
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Med. , 15 February 2022
Sec. Healthcare Professions Education
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.821908
 Sabyasachi Maity1
Sabyasachi Maity1 Jadzia Wray2
Jadzia Wray2 Tamara Coffin2
Tamara Coffin2 Reetuparna Nath3
Reetuparna Nath3 Shreya Nauhria4
Shreya Nauhria4 Ramsagar Sah5
Ramsagar Sah5 Randall Waechter1
Randall Waechter1 Prakash Ramdass6
Prakash Ramdass6 Samal Nauhria7*
Samal Nauhria7*Background: The stressful academic schedule of medical students poses an obvious challenge to their daily lifestyle. Psychosomatic discomfort poses a significant risk for inaccurate self-medication for ameliorating menstrual complications and feeling better, thus directly impacting personal and academic wellbeing.
Objective: The impact of menstrual disturbances on academic life is not extensively explored. Therefore, the primary objective of this research was to probe the prevalence of menstrual disturbances and assess the academic and social impact. Finally, the authors provide an overview of pharmacological and other interventions students adopt to reduce clinical symptoms.
Methods: A database search was conducted from the year 2016 till September 2021 for the studies reporting the prevalence of menstrual disorders in all geographic locations of the world. Keywords used for searching databases included “menstrual disturbances” and “medical students,” “prevalence” OR “symptoms” of “Premenstrual syndrome” OR “Premenstrual dysphoric disorder” OR “Dysmenorrhea” in medical students. Prospero Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Meta-Analysis of Observational Studies in Epidemiology (MOOSE) protocols were followed. The protocol was registered in the International prospective register of systematic reviews (PROSPERO), the Center for Reviews and Dissemination, University of York (CRD42021277962). The quality of the methodologies used in selected studies was evaluated by a modified version of Newcastle Ottawa Scale (NOS).
Results: Initially, 1527 articles were available. After a review, 26 papers were selected for analysis. A total of 25 citations were identified for quantitative analyses, out of which 16 studies reported Pre-menstrual syndrome, 7 reported Pre-menstrual dysphoric disorder, and 13 articles reported dysmenorrhea. The pooled prevalence of Pre-menstrual syndrome was 51.30%, Pre-menstrual dysphoric disorder was 17.7%, and dysmenorrhea was 72.70%. Most common associated lifestyle factors were stress, excessive caffeine intake and lack of exercise. Painkillers, hot packs and hot beverages were amongst the common measures taken by the students to relieve their symptoms.
Conclusions: The current situation calls for action to accommodate students' needs and bridge the social gap regarding menstrual health. Proactive measures by medical educators and stakeholders are required for an inclusive, accommodating educational environment which will minimize the gender discrepancy in academic satisfaction and professional life.
Menstruation has a significant impact on a woman's physical, mental and social wellbeing. Menstrual health is defined as “a state of complete physical, mental, and social wellbeing and not merely the absence of disease or infirmity, in relation to the menstrual cycle” (1). Between menarche and menopause most women mensurate, thus menstrual health plays and integral part in women's overall heath. Cyclic discharge of blood from uterine corpus between menarche and menopause is usually how mensuration is defined. Bleeding lasts between 2 and 7 days during each cycle of 21–31 days, average 28 days. Almost 70–80% of women does not experience any disruption in carrying out their normal daily activities during or days leading to mensuration, while remaining 20–30% experiences Pre-menstrual Syndrome (PMS). Three to eight percent women experiences severe symptoms. PMS manifests as physical and emotional symptoms that occurs 1–2 weeks before actual menstruation. Common symptoms of PMS include physical symptoms such as abdominal bloating and cramp, extreme fatigue, tiredness, tendered breast and headaches; emotional symptoms like mood swings, irritability, depression, hyperphagia, and forgetfulness and difficulty with concentration (2–5).
Pre-menstrual dysphoric disorder (PMDD) is a severe form of PMS that occurs in 3–8% females resulting in serious psychological symptoms (6). PMDD is listed as pre-menstrual syndrome/pre-menstrual tension/pre-menstrual tension syndrome in the International Classification of Diseases eleventh version (ICD-11), whereas the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) and American College of Obstetricians and Gynecologists (ACOG) recognize it as pre-menstrual dysphoric disorder (7, 8). According to DSM-5 a female must possess 5 out of 11 symptoms to be categorized as PMDD, and symptom of mood swings must be present for diagnosis. Symptoms include irritability, depression, and excessive tension. These symptoms are often so severe and can lead to dysfunction and poor quality of life. The etiology of PMDD is still unknown, and studies show that being unmarried, mental distress, menstrual dysfunction and poor health can all lead to PMDD (3, 4, 9). However, there is no reported difference between women of different socio-economic status and culture (10).
Many forms of treatment and self-care are available to control the symptoms of most women, but 3 in 4 women suffer from some form of PMDD (11). Another common menstrual disorder is Dysmenorrhea (primary and secondary), which refers to pain during menstruation. Unlike primary dysmenorrhea, secondary dysmenorrhea is associated with pelvic pathology. The prevalence of dysmenorrhea has been reported to range from 15.8 to 89.5%, with ~20% experiencing condition as severe (12). Reproductive health and women's health in general is not sufficiently represented in basic and translational research. Millions of females are catastrophically affected by menstruation in terms of mental, physical, and social health. Surprisingly, previous research has shown up to 40% of women quit work and stayed home due to abnormal menstrual bleeding, thus leading to poor professional and personal life quality (13). According to a recent Lancet article all those who menstruate are being denied basic human rights, thus shaping United Nations development goals. These goals include poverty, education, health, water and sanitation, and gender equality. Addressing menstrual health problems is crucial in reaching these goals (14). It is now well-documented that educating women has a significant contribution to a more stable and resilient society, which provides all individuals equal opportunity to attain their full potential (15). Effects of menstruation on academics have been studied throughout the century. A recent systematic review established the relationship between dysmenorrhea and academic impairment such as absenteeism, lesser participation in classroom activities, lack of concentration, and degrading academic performance (16). Female students generally prefer not to seek medical attention or self-medicate using over-the-counter pain killers or other methods to control menstrual pain (6, 10, 17).
Studies suggests that female medical students around the world are also disadvantaged due to abnormal menstrual cycles. PMS, PMDD, and dysmenorrhea are leading causes of academic and personal wellbeing impairment in a medical school (3, 18–21). Moderate to severe psychosomatic menstrual symptoms are reported in the medical and health sciences students (2, 22–25).
The absence from classes and other social activities during abnormal menstruation creates anticipatory anxiety and up to 20% medical students loathe menstruation due to severe pain (21, 26, 27). A cross-sectional study on female medical students suggested 39.4% prevalence of PMS, with 14.2% reporting severe PMS. Quality of life score was reported be low in half of the students (28). The implication of abnormal menstrual cycles in female medical students is alarming. Females are more prone to depression and related symptoms compared to men (29). Abnormal menstruation further adds to the existing high stress among the medical students due to voluminous curricular content (30–33). A study of 414 medical students reported positive correlation between PMS and anxiety, depression, and stress. 11.8% students reported moderate, whereas 1.7% reported severe depression (34).
Although a few systematic reviews addressed the prevalence of menstrual disturbances among the female population (10, 17, 35), no such attempts were made in the last 5 years to explore the impact of problematic menses on the quality of life by providing evidence with meta-analysis of published studies. Thus, present research explores intrinsic inequality in the medical school curriculum, which situate female medical students a step backwards from the beginning of their academic life because of abnormal physiology. Furthermore, the current paper provides an insight on epidemiological details of menstrual disturbances.
Over time, medical education has reformed itself to accommodate students' needs by including students with learning disabilities (31, 32). An inclusive medical school curriculum considering the students with any menstrual disturbance is essential for equality (18). Medical educators are in an advantageous position to reframe the negative attitude or eliminate the negative emotions associated with menstruation in medical students. It is time for medical educators to address the gender divide regarding access to education resources and better-quality life (36). Due to lack of awareness and initiatives among medical educators there is still have a long way to go to address this issue. Keeping up with the opposite gender and not experiencing equality can be detrimental, the psychosomatic complications of menstrual disturbances, thus, are a significant concern for female medical students in the current competitive world where gender equality has seen great uprising (14, 18, 31, 32, 37, 38). Thus, the aims of current study are-
a) Probe the prevalence of PMS, PMDD and dysmenorrhea using meta-analysis among medical students.
b) To assess the effect of this prevalence on class absenteeism and overall quality of life.
c) To provide an overview of pharmacological and other modes of interventions adopted by female medical students worldwide to reduce the clinical symptoms of menstrual disturbances.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Meta-Analysis of Observational Studies in Epidemiology (MOOSE) protocols were followed by the researchers (39, 40). The protocol used in this study was registered in International prospective register of systematic reviews (PROSPERO), the Center for Reviews and Dissemination, University of York (CRD42021277962) prior to the commencement of the project.
Published studies were searched in electronic databases namely, PubMed (US National Library of Medicine, National Institutes of Health), Scopus, Embase, and Web of Science for potentially relevant studies from inception up to September 2021. Articles published in English from selected databases were included. The authors were required to reach a consensus among themselves on the final search strategy. The medical subject headings (MeSH) search terms included “menstrual disorder,” “Premenstrual Syndrome” and “Premenstrual Dysphoric Disorder” including all subheadings. The following search strategy was used to identify studies in PubMed: (“Menstruation Disturbances” [Mesh]) AND “Students” [Mesh]. Using simple search terms “Menstruation Disturbances AND Students,” search was conducted through PubMed in addition to our MESH search. For Scopus, the following search strategy was used: ALL (Menstruation disturbances and students) AND [LIMIT-TO (DOCTYPE, “ar”) OR LIMIT-TO (DOCTYPE, “re”)] AND [LIMIT-TO (LANGUAGE, “English”)]. For EMBASE, we used: (“menstruation disorder”/exp OR “menstruation disorder”) AND “medical students.” Finally, the relevant articles were also included by adopting the snowball method which involves searching the bibliographic list of selected articles.
Two independent reviewers (SM and SN) screened the retrieved papers based on titles and abstracts. Criteria for examination of full text of the relevant paper after the initial database screening were as follows:
• Articles reporting data on impact and prevalence of PMS, PMDD, and/or dysmenorrhea that could be extracted for statistical analysis were only included
• Studies conducted in any geographical location but on medical/health sciences/nursing students
• All the studies that include cross-sectional studies, or cohort based
• Studies published from 2016 till September 2021 (last 5 years) and the female population studied adequately
• The non-peer-reviewed editorials, letters, commentaries, incomplete data, reviews, conference posters, preprints, and thesis were excluded
Any confusion or doubts regarding the study selection were resolved by reaching a consensus. Figure 1 represents the process of study selections for the systematic review and meta-analysis as per the PRISMA protocol.
Two independent reviewers (SM and SaN) evaluated the quality of the methodologies used in selected studies by a modified version of Newcastle Ottawa Scale (NOS) (41). Five segments of the NOS scale were included with offering of one (*) to each with a positive evaluation regarding any of the assigned point as per the criteria. The five segments for assessing quality of each study article were: “sample representativeness,” “sample size,” “ascertainment of any of the inclusion menstrual disorder,” “comparability between respondents and nonrespondents,” and “statistical quality.” According to the resultant number of points assigned, each study was judged to be at high (≥3 *) or low (<3 *) quality. Any discrepancies concerning the author's judgments were resolved by consensus and by discussing with another reviewer PR. Supplementary Table 1 represents the raw data of quality assessment using the modified NOS.
Author SM extracted the relevant data, and the data was crosschecked by SaN and others. In a blank excel sheet, data on author and year of publication, geographical location, duration of the study, age range of the study participants, total number of populations, diagnosis and scale used as diagnosis criteria, and reported prevalence for each eligible study were extracted. The included study authors were contacted for clarification and assistance with incomplete study and non-response was considered as exclusion. Any disagreement amongst authors was resolved by consensus and discussion with PR.
Meta-analysis of quantitative data was performed to estimate the cumulative prevalence from individual studies. The summary estimates of prevalence were reported along with their 95% confidence intervals (CI) for PMS, PMDD, and dysmenorrhea. The pooled prevalence data was presented in a Forest plot. All the analyses were done using “Comprehensive meta-analysis” software version 3. Presence of publication bias was examined by the visual inspection of funnel plot. The “one-study-removed” procedure was used as a sensitivity analysis to determine whether the overall estimates of menstrual disorders in female medical students were influenced by outlier studies.
Our search through the databases finally identified 26 articles on prevalence of menstrual disturbances including PMS, PMDD, dysmenorrhea that were included in the systematic review from 2016 till 2021. The article exclusion criteria included the following reasons:
• Not relevant to the objective
• Not in line with the inclusion criteria
• The studies were not conducted on medical students
• The full text pdf was not available
• Not original research
• No availability of statistical results
All the included studies were of cross-sectional design across the world at varied number and time frames. Although most of the studies were on medical students however, a few reported prevalence from non-medical students too with a reasonable statical comparison of prevalence. The total number of female medical student from the included studies was 4,874. Although most of the studies exclusively reported the prevalence of either PMS or PMDD or dysmenorrhea however, a few studies do indicate prevalence of two menstrual disturbances in a single population. Therefore, the prevalence data were calculated accordingly. A detailed synthesis of included studies is provided in Table 1.
The final included articles were predominantly of cross-sectional design. Therefore, a modified NOS was used as explained in the methods section. To evaluate each study, a (*) was assigned to the any of the criteria of the NOS. Only one study (34) was rated as low (<3 *). Other included studies were rated as high. Table 2 represents the summary of quality assessment using modified NOS.
SM and RN individually assessed the impact of menstrual disturbances and the lifestyle factor associations.
The high prevalence of menstrual disturbances impacted the academic and social life. Students were missing classes and some reported lower grades compared to others. In addition, many reported impairments of various aspects of the quality of life such as meeting friends and co-workers, relationships with their family and partners, etc. What alarming is the intervention by the medical students to reduce the symptoms of menstrual disturbances. Most of the students reported to self-medicate by using painkillers such as NSAID's and other hot drinks. A very few consulted doctors for treatment. Some medical students preferred not to share the menstrual discomfort and perceived it as taboo. The details of academic and health impact of the respective studies and frequent measures adopted by the students are listed in Table 3.
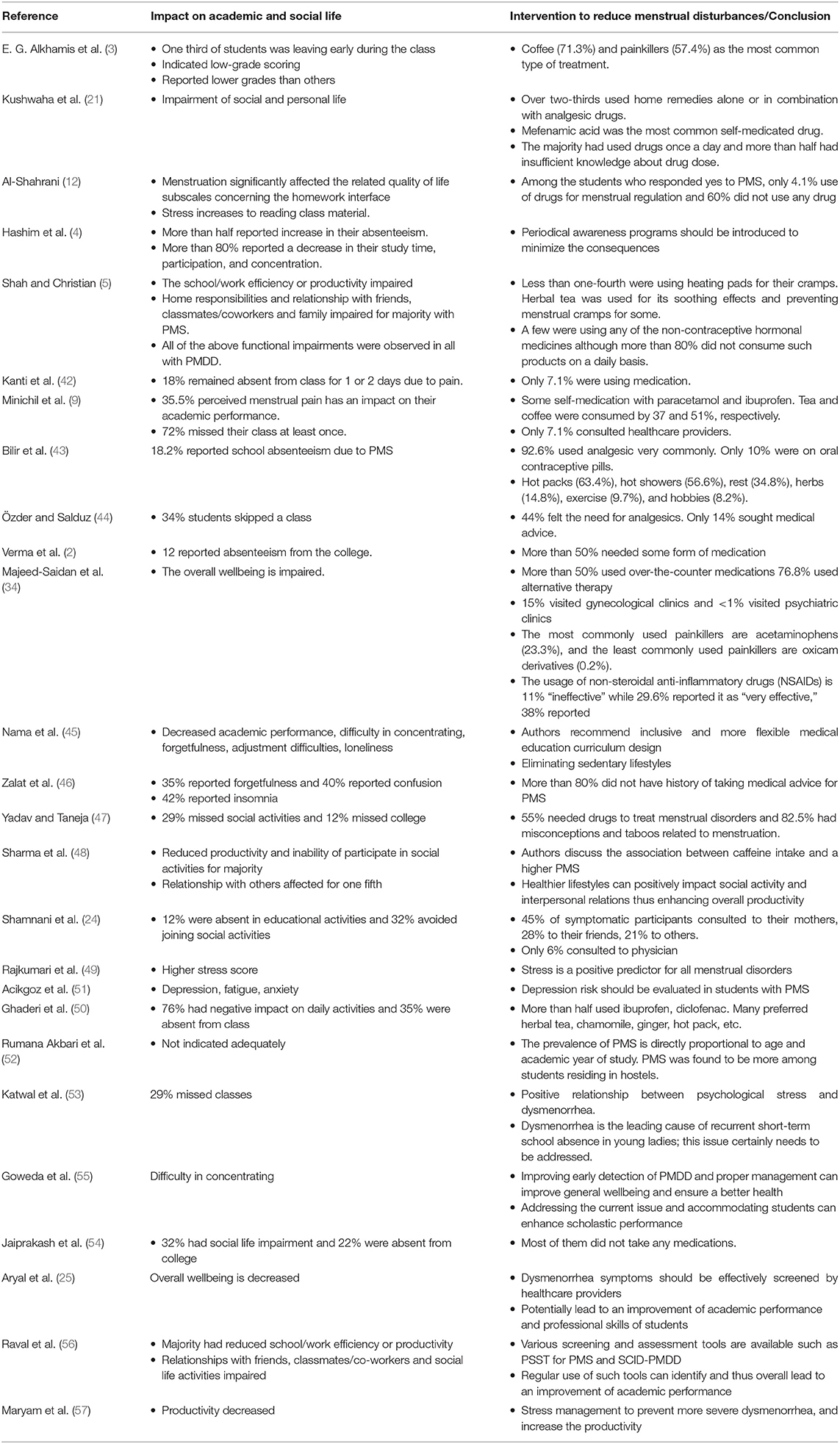
Table 3. Academic and social impact of menstrual abnormalities and the adopted intervention by the medical students to reduce complications.
The lifestyle factors associated with menstrual disturbances found in our study are shown in Supplementary Table 2 which represents some characteristics of everyday life which potentially lead to menstrual disturbances. For example, anticipatory stress or family history of other psychologic disorders are prone to have menstrual problems. Likewise, lack of exercise, excessive caffeine and tea intake, smoking, unhealthy dietary habits, and abnormal body weights are lifestyle factors associated with the development of menstrual complications. Figure 2 depicts the graphical representations of the factors leading to the menstrual abnormalities in medical students.
Among the total female medical students of the included studies (n = 4,874) across the continents, the prevalence of PMS was reported by 16 studies (n = 3,192). The pooled prevalence of PMS was 51.30% (95% CI: 0.396–0.629). The studies of PMS prevalence have been conducted mostly in Asia, Middle East and partly from European countries. Table 1 of the extracted data shows the country wise distribution of menstrual disturbances. Figure 3 shows the overall PMS prevalence with a high level of heterogeneity. Supplementary Figure 1 represents the pooled prevalence of PMS after excluding one study to minimize the heterogeneity. The highest prevalence of PMS was found from New Delhi, India (2), estimated at 85.20% (95% CI: 0.792–0.897) and lowest was from Gujarat, India (56) at 7% (95% CI: 0.030–0.158). This observation was in line with previous studies (17). The publication bias is indicated through the visual inspection of the funnel plot (Figure 4).
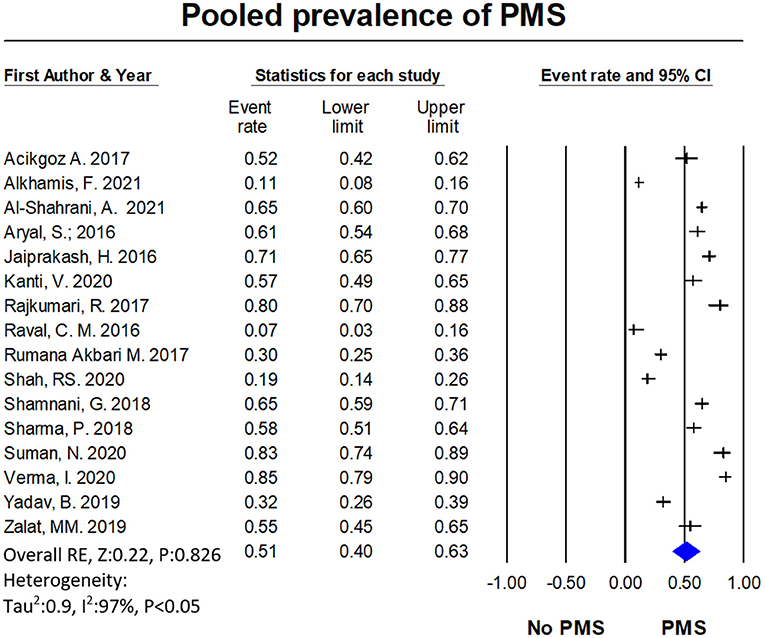
Figure 3. The forest plot of PMS prevalence. The diamond represents the overall results and 95% confidence interval of the random effect of the meta-analysis. Model: Random, overall effect size: 0.513, 95%CI: [0.396–0.629] (z-value: 0.220, p-value: 0.826), I2:96.93. Tau2: 0.901, s.e: 0.384, variance: 0.147, tau: 0.949.
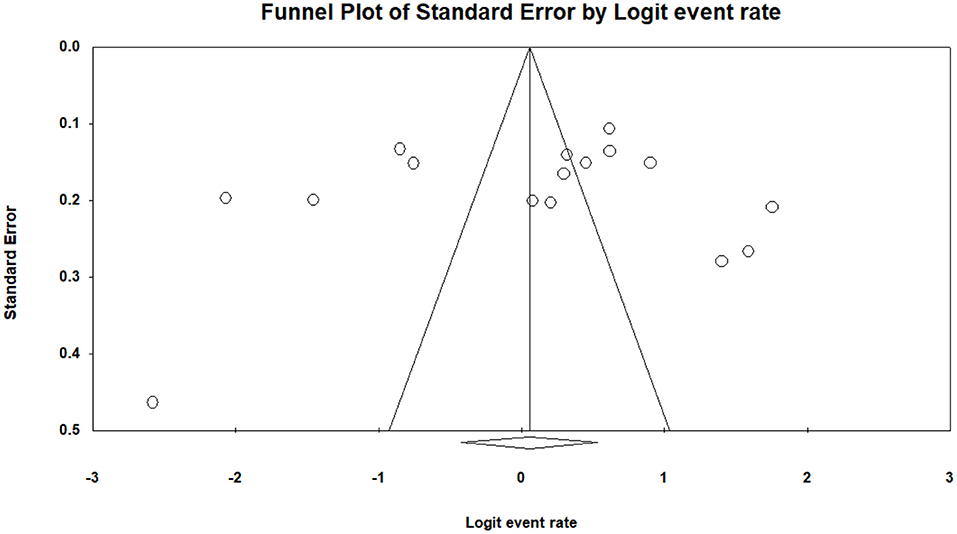
Figure 4. The funnel plot of pooled prevalence of PMS is asymmetry and suggest that overall effect of the analysis is biased. In this case the intercept (B0) is 1.06576, 95% confidence interval (−7.59403, 9.72556), with t = 0.27088, df = 11. The 1-tailed p-value (recommended) is 0.39575, and the 2-tailed p-value is 0.79150.
A total of 7 studies with a total of 1,487 female medical students were included in the meta-analysis for the prevalence of PMDD. Prevalence reported by individual studies ranged between 1 and 38%. The pooled estimate of PMDD was 17% (95% CI: 0.102–0.289). Figure 5 shows the overall PMDD prevalence. The heterogeneity test was not performed since the total number of PMDD studies were <10. Supplementary Figure 2 represents the pooled prevalence of PMS with exclusion of one study to minimize the heterogeneity.
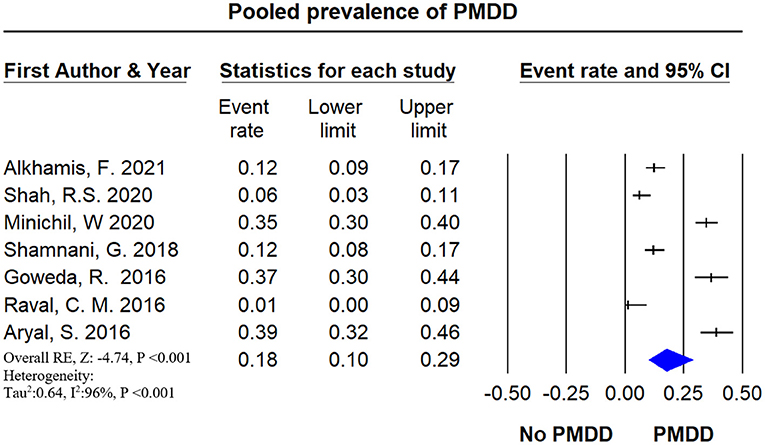
Figure 5. The forest plot of PMDD prevalence. The diamond represents the overall results and 95% confidence interval of the random effect of the meta-analysis. The prevalence of PMDD was reported in 6 studies including 1,487 participants. The estimated prevalence, pooled from all included studies for PMDD was found to be 17.7% (95% CI: 0.102–0.289) with a high level of heterogeneity (I2 = 95.12%), p-value: <0.001, Results: significant.
A total of 13 studies with a total of 2,497 female medical students, were included in the meta-analysis for the prevalence of dysmenorrhea. Prevalence reported by individual studies ranged between 24 and 98%. The pooled estimate of dysmenorrhea was 72.7% (95% CI: 0.634–0.804) with a high level of heterogeneity (I2 = 94.7%). Figure 6 shows the overall dysmenorrhea prevalence. Supplementary Figure 3 represents the pooled prevalence of dysmenorrhea with exclusion of one study to minimize the heterogeneity. The publication bias is indicated through the visual inspection of the funnel plot (Figure 7) asymmetry.
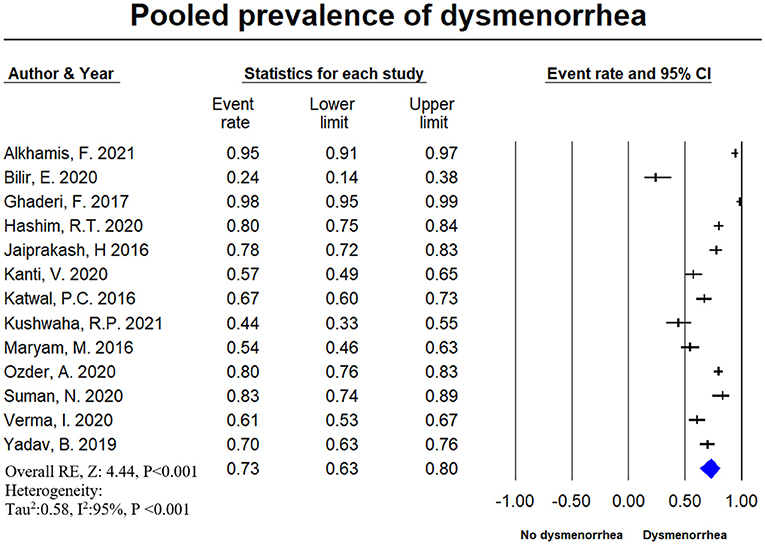
Figure 6. The forest plot of dysmenorrhea prevalence. The diamond represents the overall results and 95% confidence interval of the random effect of the meta-analysis. The prevalence of dysmenorrhea was reported in 13 studies including 2,497 participants. The estimated prevalence, pooled from all included studies for dysmenorrhea was found to be 17.7% (95% CI: 0.102–0.289) with a high level of heterogeneity (I2 = 94.7%), p-value: <0.001. Model name: Random, z value: 4.444, p-value <0.001, I2: 94.7%, tau2: 0.578, S.E: 0.283, variance: 0.08, Tau: 0.76.
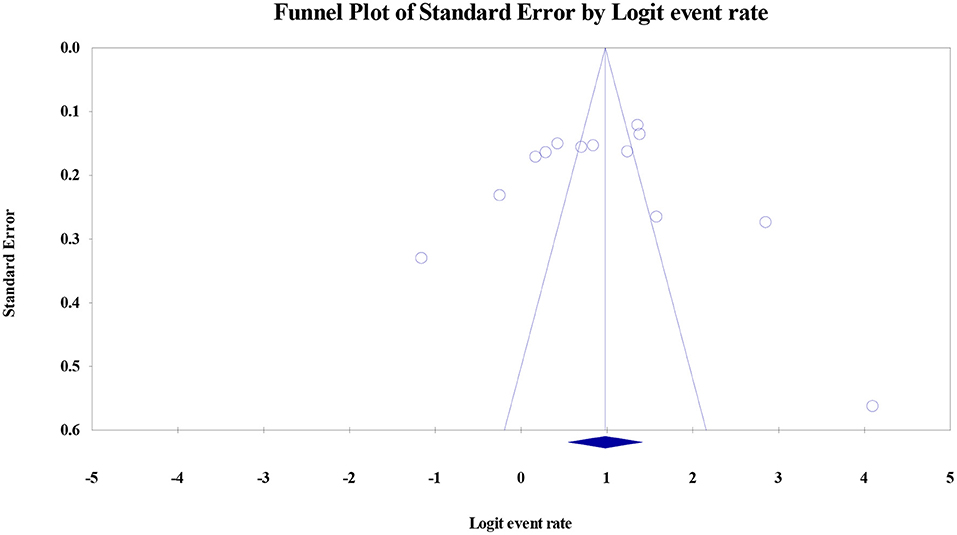
Figure 7. The funnel plot of pooled prevalence of dysmenorrhea is asymmetry and suggest that overall effect of the analysis is biased. In this case the intercept (B0) is 1.06576, 95% confidence interval (−7.59403, 9.72556), with t = 0.27088, df = 11. The 1-tailed p-value (recommended) is 0.39575, and the 2-tailed p-value is 0.79150.
This study is a first-of-its-kind prevalence study in medical students where a systematic review and meta-analysis of included studies were provided clearly. We searched the databases comprehensively and extracted the relevant data on menstrual disturbances in female medical students worldwide.
Although all humans experience some hormonal surges at puberty, women are predominantly susceptible to physical and mental stress caused by endocrinal changes associated with the menstrual cycle. Throughout the active reproductive life of a female (from menarche→regular menstrual cycle→pregnancy→menopause), the body goes through hormonal fluctuations, leading to stress and mood alterations. A high level of stress and mood disturbances can further complicate the menstrual cycle. The hypothalamic-pituitary-gonadal/adrenal (HPG/HPA) axis provides essential feedback and regulatory influence to maintain physiological homeostasis. Therefore, abnormality of either HPG or HPA is a major contributing factor for menstrual disturbances (58). Emotional stress could modulate these powerful feedback mechanisms by the HPA and HPG axis. For example, overactivation of HPA because of psychological stressors increases cortisol's plasma level to meet the increased energy demand in stressful situations (59, 60). Eventually, the higher cortisol concentration and the associated increase in metabolism disrupts the typical cyclical pattern of hormonal fluctuation leading to menstrual abnormalities such as PMS, PMDD, and dysmenorrhea.
Pre-menstrual symptoms include a spectrum of psychosomatic symptoms arising in the luteal phase of the menstrual cycle affecting the typical lifestyle of a female and getting resolved after the menstruation cycle begins. The American Congress of Obstetricians and Gynecologists (ACOG) and the American Psychiatric Association (APA) both have a set of diagnostic criteria based on physical and psychological symptoms for diagnosing PMS and PMDD, respectively (7, 8). The physical and psychological symptoms generally occur between menarche and menopause anytime throughout the reproductive life. Pain during menstruation (period pain), known as dysmenorrhea, is widespread in young women. Dysmenorrhea affects approximately three-quarters of all women in their teens and early adult life. Women with menstrual disturbances have higher rates of negative impact on academic performance, work absences, higher medical expenses, and overall, lower quality of life (61).
We searched the databases comprehensively and extracted the relevant data on menstrual disturbances in female medical students worldwide. Our study found common complaints of PMS, PMDD, and dysmenorrhea in female medical students. Some studies have also reported a combination of menstrual disturbances (3, 5, 54). The calculated pooled prevalence of PMS was 51.30% (95% CI: 0.396–0.629), PMDD was 17.7% (95% CI: 0.102–0.289), and dysmenorrhea was 72.7% (95% CI: 0.102–0.289), respectively. The highest report of PMS was from New Delhi, India (2), and the lowest was from Gujarat, India (56). The highest report of PMDD was from Nepal (25), and the lowest was from Gujarat, India (56). The highest report of dysmenorrhea was from Iran (50), and the lowest was from Turkey (43). Could it be due to the food habit and lifestyle patterns? It would be interesting to explore this avenue further for targeted therapeutic interventions.
Although we searched comprehensively, we did not find a suitable study from the USA, Canada, UK, Australia, and other western countries. However, studies are available on the impact of therapeutic interventions for treatment of PMS and PMDD (62, 63). Likewise, Armour et al. provide a systematic review and meta-analysis of the prevalence of dysmenorrhea among 21,573 young women worldwide but the study does not focus on medical students (61). Medical students across the globe have been found to have higher levels of perceived stress and emotional distress. The higher stress level is due inability of students to tackle a challenging medical curriculum with a higher course load along with frequency of exams (64). Comparative research data indeed shows a higher level of perceived stress in medical students than the general population and students from another academic field (65, 66). Researchers have assessed perceived stress in medical students by specific questionnaires such as the Perceived Medical School Stress (PMSS) (64, 67). Rationally, menstrual disturbances and the associated discomfort add to the already increased perceived stress in medical students.
An exciting aspect of this review was to investigate root causes of the menstrual disturbances in medical students and the impact on academic and social life. Although we did not quantify the causal statistical data, our study highlights behavioral and lifestyle factors such as food and drink preferences, lack of exercise, smoking, caffeine intake, etc., may have a strong association with menstrual disturbances. It is also interesting to notice a trend of traditional interventions such as over-the-counter pain killers, drinking hot tea, etc., to reduce the symptoms of menstrual disturbances in medical students. This study supports evidence from previous observations by Kushwaha et al., who reported a lower incidence (19 vs. 48%) of moderate to severe dysmenorrhea in students who had been exercising regularly vs. students who did not. Most respondents adopted home remedies to manage painful menstruation without medical consultation. In addition, 61% respondents used analgesic drugs out of which 51% used Mefenamic acid as the most common self-medicated drug. The more concerning fact is that 78% had used drugs once a day, but 68% had insufficient knowledge about drug dosage (21). Long-term misuse of pain medications may lead to an additional burden of disease among medical students.
In accordance with the present results, a previous study by Alkhamis et al., reported a 23.3% prevalence of PMS and PMDD. Fifty-six percent of medical student respondents in the study were not involved in any exercise, and 21% did not sleep for 6 h or more. Sixty-five percent reported consuming caffeine regularly, and 26% reported eating junk food more often than others. Although no precise statistical analysis was shown between lifestyle behaviors and the prevalence of PMS and PMDD, a national association is possible. It was also reported that female students left early from the class because of PMS. Consequentially, 29.1% of the female medical students indicated low-grade scoring, and 22.5% reported lower grades than males. Among students with PMS or PMDD, 71.3% used hot drinks such as coffee, 57.4% used traditional pain killers as a mode to reduce pain. Only 11.2% opted for medical treatment (3). Therefore, a proper health policy and intervention should be implemented by all medical universities worldwide to provide female medical students with equal opportunity as their peers.
These results corroborate the ideas of Al-Shahrani et al., who reported that 50% students who experienced PMS did not exercise and 25% had a family history of menstrual problems. The quality of life was also significantly impaired in medical students because of menstruation disorder. More than 60% of the respondents did not use any medication or medical consultation to reduce the discomfort during the menstrual cycle (27).
Overall, this research paper shows direct and significant impact of menstrual disorders on the academic and personal quality of life of female medical students. Moreover, the academic disadvantage may lead to an unequal platform for success compared to other medical students. Therefore, this gap should be considered for a critical intervention by the medical universities, all stakeholders and government agencies.
One of the early studies in 1971 by Kantero and Widholm on over 5,000 female adolescents reported a 43% irregular menstrual cycle rate with 20% having irregular menses 5 years after menarche (68). Furthermore, studies on non-medical college and school students reported chief complaints of oligomenorrhea or amenorrhea (16, 69). These early studies generated a considerable clinical interest to explore further the variability of menstrual patterns and associated symptoms such as PMS, PMDD, and dysmenorrhea. Early studies of menstrual patterns in medical students, however, report conflicting results. A study examined physical discomfort during menses in medical students and found no evidence to support the hypothesis that a higher perceived stress level was associated with a change of a menstrual function (70). On the contrary, an Indian study on medical students reported a PMS (67%) and dysmenorrhea (33%) as the most distressing problems associated with menstruation (48). These results seem to be consistent with other research which found that 16% had a positive correlation of irregular menses and examination stress (69). As discussed previously, in most of these early studies, the academic and quality of life were impaired because of menstrual disturbances.
Medical education has evolved in recent times not just to follow the government guidelines but also to fulfill the motto of education for all. Education trends have debunked the myth that only students of science background can apply and get into medical school. Many institutions have additional pre-medical programs tailored for non-medical students who wish to learn and practice medicine. In addition, a significant number of medical students in the USA require additional accommodations due to learning disabilities. Providing equal opportunities to all the sections of the students is advantageous for society and a fulfilling experience for a medical school. Currently, the USA has several practicing doctors who completed their medical studies with learning disabilities like ADHD (71). Therefore, medical educators should recognize the gap in academic performance and social index in the female medical students also as compared to their male peers and provide additional accessibility as required. The need of the hour is to recognize and urgently implement a knowledge-based program with additional measures to provide equal platforms for both male and female students.
The current study is the first systematic review and meta-analysis of three predominant menstruation disturbances among female medical students worldwide. Present study adds value to the existing body of literature on female reproductive and personal wellbeing. The review also provides an overview of the traditional lifestyle factors leading to menstruation disturbances among medical students. In addition, the review also sheds light on the impact of menstrual disturbances in the academic and personal life. The present systematic review and meta-analysis may have overlooked some studies that could have been included in our review despite comprehensive search strategy. The present study could not find enough relevant studies from USA, UK, and Australia. Since the gray literature of the thesis and another non-peer-reviewed article were excluded, a piece of valuable information may have been lost because of this. The subgroup analysis of PMS, PMDD, and dysmenorrhea, could have been more in-depth, but that would also be too much information for a busy reader. A significant limitation of our study is the presence of a considerable level of heterogeneity. This could be due to the diverse geographical population with different cultures and differences in methodologies of the study protocol. The heterogeneity of results and different outcomes posed a major problem and could be resolved in the future by introducing a core outcome set but we still have to work on that. Present study includes Supplementary Figures 1–3 with more refined versions of forest plots by eliminating the one data to reduce the heterogeneity. Finally, the impact of menstrual disturbances on education and quality of life was not analyzed because of inadequate data. Therefore, the report may be underestimating the prevalence of the impact of menstrual disturbances.
The current systematic review and meta-analysis shows a high prevalence of PMS and dysmenorrhea among female medical students. However, the prevalence of PMDD is relatively low in the same population. Most reproductive age group female students have impairment of academic and social quality of life because of menstrual symptoms. Lifestyle, socio-demographic, genetic, and psychological factors may contribute to the menstrual disturbances. Since there are a smaller number of studies and sharp variation of estimates in worldwide research data, it would be interesting in future to compare the prevalence of menstrual disturbances and associated factors between the female medical students of USA, UK, and Australia to the rest of the world in a large-scale study to find out the personal, professional, and economic impact of menstrual disturbances. Since a significant population of the studies either miss classes or have impairment of the academic performance, all stakeholders should step up the formulation of guidelines to increase our medical student population's overall quality of life. Early intervention in the medical universities and formulation of strategies to improve pain, mood, depression, and associated symptoms of menstrual disturbances would increase educational opportunities and foster a better quality of life. Finally, further studies are needed to evaluate and assess the cause of the menstrual disturbances and therapeutic interventions to bridge the gender gap in our society for a better tomorrow.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
SM and SaN: conceptualizing, literature search and screening, methodology selection, data extraction, project administration, supervising and writing, and manuscript preparation. TC, JW, SaN, and RN: conceptualizing, data extraction and analysis, validation, writing, and reviewing and editing. RS: meta-analysis validation and data curation. RW and PR: conceptualizing, supervision, interpretation, and review and editing. RN, ShN, and SaN: final review and editing, data visualization, and project administration. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to acknowledge the efforts of Suzanne Paparo, Faculty Librarian, St. George's University School of Medicine, Grenada in assisting with database access.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.821908/full#supplementary-material
1. Hennegan J, Winkler IT, Bobel C, Keiser D, Hampton J, Larsson G, et al. Menstrual health: a definition for policy, practice, and research. Sex Reprod Health Matters. (2021) 29:1911618. doi: 10.1080/26410397.2021.1911618
2. Verma I, Joshi G, Sood D, Soni RK. Menstrual problems in undergraduate medical students: a cross-sectional study in a medical college of North India. J South Asian Federation Obstetr Gynaecol. (2020) 12:85–90. doi: 10.5005/jp-journals-10006-1774
3. Alkhamis F, Almzraq LAA, Alshayeb ZK, AL-Jaziri ZY. Prevalence of premenstrual syndrome among medical students in King Faisal University in Alahssa-Saudi Arabia. Med Sci. (2021) 25:1971–83. Available online at: http://www.discoveryjournals.org/medicalscience/current_issue/v25/n114/A23.pdf
4. Hashim RT, Alkhalifah SS, Alsalman AA, Alfaris DM, Alhussaini MA, Qasim RS, et al. Prevalence of primary dysmenorrhea and its effect on the quality of life amongst female medical students at King Saud University, Riyadh, Saudi Arabia. Saudi Med J. (2020) 41:283–9. doi: 10.15537/smj.2020.3.24988
5. Shah R, Christian D. Association of socio-demographic, dietary and lifestyle factors with Premenstrual Syndrome (PMS) among undergraduate medical students of a tertiary care institute in Ahmedabad, Gujarat. J Family Med Prim Care. (2020) 9:5719–24. doi: 10.4103/jfmpc.jfmpc_1553_20
6. Dilbaz B, Aksan A. Premenstrual syndrome, a common but underrated entity: review of the clinical literature. J Turk German Gynecol Assoc. (2021) 22:139–48. doi: 10.4274/jtgga.galenos.2021.2020.0133
7. American College of Obstetricians and Gynecologists. Guidelines for Women's Health Care: A Resource Manual. 4th ed. Washington, DC: The American College of Obstetricians and Gynecologists, Women's Health Care Physicians (2014). p. 889.
8. Vahia V. Diagnostic and statistical manual of mental disorders 5: a quick glance. Indian J Psychiatry. (2013) 55:20–3. doi: 10.4103/0019-5545.117131
9. Minichil W, Eskindir E, Demilew D, Mirkena Y. Magnitude of premenstrual dysphoric disorder and its correlation with academic performance among female medical and health science students at University of Gondar, Ethiopia, 2019: a cross-sectional study. BMJ Open. (2020) 10:e034166. doi: 10.1136/bmjopen-2019-034166
10. Duko B, Mekuriaw B, Molla A, Ayano G. The prevalence of premenstrual dysphoric disorder among adolescents in Ethiopia: a systematic review and meta-analysis. Irish J Med Sci. (2020) 190:419–27. doi: 10.1007/s11845-020-02275-7
11. Osborn E, Wittkowski A, Brooks J, Briggs PE, O'Brien PMS. Women's experiences of receiving a diagnosis of premenstrual dysphoric disorder: a qualitative investigation. BMC Womens Health. (2020) 20:242. doi: 10.1186/s12905-020-01100-8
12. Alshahrani MS. Dysmenorrhea and its effects among female students at health colleges in Najran University, Saudi Arabia: a cross-sectional study. J Women's Health Care. (2020) 9:484. doi: 10.35248/2167-0420.20.9.484
13. Karlsson TS, Marions LB, Edlund MG. Heavy menstrual bleeding significantly affects quality of life. Acta Obstetric Gynecol Scand. (2014) 93:52–7. doi: 10.1111/aogs.12292
14. Babbar K, Martin J, Ruiz J, Parray AA, Sommer M. Menstrual health is a public health and human rights issue. Lancet Public Health. (2021). 7:e10–e11. doi: 10.1016/S2468-2667(21)00212-7
15. Bayeh E. The role of empowering women and achieving gender equality to the sustainable development of Ethiopia. Pac Sci Rev B Hum Soc Sci. (2016) 2:37–42. doi: 10.1016/j.psrb.2016.09.013
16. Munro AK, Hunter EC, Hossain SZ, Keep M. A systematic review of the menstrual experiences of University students and the impacts on their education: a global perspective. PLoS ONE. (2021) 16:e0257333. doi: 10.1371/journal.pone.0257333
17. Dutta A, Sharma A. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in India: a systematic review and meta-analysis. Health Prom Perspect. (2021) 11:161–70. doi: 10.34172/hpp.2021.20
18. Hashimoto K, Fukushima K, Fukushima N, Sato H, Yokota J, Uchida K. Association between nutritional level, menstrual-related symptoms, and mental health in female medical students. Plos One (2020) 15(7). doi: 10.1371/journal.pone.0235909
19. Strine TW, Chapman DP, Ahluwalia IB. Menstrual-related problems and psychological distress among women in the United States. J Womens Health. (2005) 14:316–23. doi: 10.1089/jwh.2005.14.316
20. Sahin N, Kasap B, Kirli U, Yeniceri N, Topal Y. Assessment of anxiety-depression levels and perceptions of quality of life in adolescents with dysmenorrhea. Reprod Health. (2018) 15:13. doi: 10.1186/s12978-018-0453-3
21. Sah B, Yadav P, Sitaula S, Sinha P, Rai DS, Sarraf DP, et al. Evaluation of the severity and self-management practice in primary dysmenorrhea in medical and dental students: A cross-sectional study in a teaching hospital. Asian J Med Sci. (2021) 12:59–65. doi: 10.3126/ajms.v12i3.32687
22. Yesuf TA, Eshete NA, Sisay EA. Dysmenorrhea among University health science students, Northern Ethiopia: impact and associated factors. Int J Reprod Med. (2018) 2018:9730328. doi: 10.1155/2018/9730328
23. Rafique N, Al-Sheikh MH. Prevalence of menstrual problems and their association with psychological stress in young female students studying health sciences. Saudi Med J. (2018) 39:67–73. doi: 10.15537/smj.2018.1.21438
24. Shamnani G, Gupta V, Jiwane R, Singh S, Tiwari S, Bhartiy S. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder among medical students and its impact on their academic and social performance. Natl J Physiol Pharm Pharmacol. (2018) 8:1205–8. doi: 10.5455/njppp.2018.8.0415728042018
25. Aryal S, Thapa B, Pant SB. Premenstrual syndrome and premenstrual dysphoric disorder in medical and nursing students of a tertiary care teaching hospital in Nepal. J Obstetr Gynaecol. (2017) 12:12–6. doi: 10.3126/njog.v12i1.18975
26. Lee LK, Chen PC, Lee KK, Kaur J. Menstruation among adolescent girls in Malaysia: a cross-sectional school survey. Singapore Med J. (2006) 47:869–74. Available online at: http://www.sma.org.sg/smj/4710/4710a6.pdf
27. Al-Shahrani AM, Miskeen E, Shroff F, Elnour S, Algahtani R, Youssry I, et al. Premenstrual syndrome and its impact on the quality of life of female medical students at Bisha University, Saudi Arabia. J Multidiscipl Healthc. (2021) 14:2373–9. doi: 10.2147/JMDH.S327893
28. Farrokh-Eslamlou H, Oshnouei S, Heshmatian B, Akbari E. Premenstrual syndrome and quality of life in Iranian medical students. Sex Reprod Healthc. (2015) 6:23–7. doi: 10.1016/j.srhc.2014.06.009
29. Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: META-analyses of diagnoses and symptoms. Psychol Bull. (2017) 143:783–822. doi: 10.1037/bul0000102
30. Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students. JAMA. (2016) 316:2214–36. doi: 10.1001/jama.2016.17324
31. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. (2006) 81:354–73. doi: 10.1097/00001888-200604000-00009
32. Mirza AA, Baig M, Beyari GM, Halawani MA, Mirza AA. Depression and anxiety among medical students: a brief overview. Adv Med Educ Pract. (2021) 12:393–8. doi: 10.2147/AMEP.S302897
33. Neufeld A, Malin G. How medical students cope with stress: a cross-sectional look at strategies and their sociodemographic antecedents. BMC Med Educ. (2021) 21:299. doi: 10.1186/s12909-021-02734-4
34. Majeed-Saidan MMA, AlKharraz N, Kaaki K, AlTawil N, Alenezy S, Ahamed SS. Prevalence of premenstrual syndrome levels and its management among female students of medical and non-medical colleges in Riyadh. Cureus. (2020) 12:e11595. doi: 10.7759/cureus.11595
35. Erbil N, Geta TG, Woldeamanuel GG, Dassa TT. Prevalence and associated factors of premenstrual syndrome among women of the reproductive age group in Ethiopia: systematic review and meta-analysis. PLoS ONE. (2020) 15:e0241702. doi: 10.1371/journal.pone.0241702
36. Lempp H, Seale C. Medical students' perceptions in relation to ethnicity and gender: a qualitative study. BMC Med Educ. (2006) 6:17. doi: 10.1186/1472-6920-6-17
37. Blanch DC, Hall JA, Roter DL, Frankel RM. Medical student gender and issues of confidence. Patient Educ Couns. (2008) 72:374–81. doi: 10.1016/j.pec.2008.05.021
39. Stroup DF. Meta-analysis of observational studies in epidemiology. A proposal for reporting. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
40. Moher D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. (2009) 151:264–9, W64. doi: 10.7326/0003-4819-151-4-200908180-00135
41. Luchini C, Stubbs B, Solmi M, Veronese N. Assessing the quality of studies in meta-analyses: advantages and limitations of the Newcastle Ottawa Scale. World J Meta Analy. (2017) 5:80–4. doi: 10.13105/wjma.v5.i4.80
42. Kanti V, Verma V, Singh NP. Study of menstrual abnormalities and its association with demographic factors among female medical students. J Clin Diagn Res. (2020). 14:QC06–QC09. doi: 10.7860/JCDR/2020/44086.13957
43. Bilir E, Yildiz S, Yakin K, Ata B. The impact of dysmenorrhea and premenstrual syndrome on academic performance of college students, and their willingness to seek help. J Turk Soc Obstetr Gynecol. (2020) 17:196–201. doi: 10.4274/tjod.galenos.2020.97266
44. Özder A, Salduz Z. The prevalence of dysmenorrhea and its effects on female University students- quality of life: what can we do in primary care? Int J Clin Exp Med. (2020) 13:6496–505. Avialable online at: https://avesis.bezmialem.edu.tr/yayin/0028d8c5-6383-4b2d-a032-fd3ec6ee6e5d/the-prevalence-of-dysmenorrhea-and-its-effects-on-female-university-students-quality-of-life-what-can-we-do-in-primary-care/document.pdf
45. Nama S, Gaddala A, Matli P, Rajamouli J, Gurnule S, Tejaswi U. A Cross sectional study to assess the prevalence of menstrual abnormalities in medical students of Karimnagar. Eur J Mol Clin Med. (2021) 7:6959–65. Available online at: https://ejmcm.com/pdf_9633_480e2ed047eb0e0f57a2977672250686.html
46. Zalat MM, Azam AN, Aahmadi HG, Alhazmi NO, Alshaya RA. Prevalence of premenstrual syndrome among Taibah University female medical students, KSA. Int J Health Med Curr Res. (2019) 4:1469–77. doi: 10.22301/IJHMCR.2528-3189.1469
47. Yadav B, Taneja P. Questionnaire based study on menstrual patterns among female medical University students of rural North India. J Evol Med Dent Sci. (2019) 8:1232. doi: 10.14260/jemds/2019/273
48. Sharma P, Patro A, Ibrahim S, Reddy TSK, Jain N, Mallya SD. Premenstrual symptoms and lifestyle Factors Associated with it among Medical students. Indian J Public Health Res. Dev. (2018) 9:39–45. doi: 10.5958/0976-5506.2018.01312.8
49. Rajkumari R, Keithellakpam S, Thiyam J, Devi NM. Relationship between psychosocial stress and menstrual function-related abnormalities among the female undergraduate medical students. J Evol Med Dent Sci. (2017) 6:3103–7. doi: 10.14260/Jemds/2017/669
50. Ghaderi F, Asghari Jafarabadi M, Mohseni Bandpei MA. Dysmenorrhea and self-care strategies in Iranian female students: a regression modeling of pain severity and underlying factors. Int J Adolesc Med Health. (2017) 29:20160017. doi: 10.1515/ijamh-2016-0017
51. Acikgoz A, Dayi A, Binbay T. Prevalence of premenstrual syndrome and its relationship to depressive symptoms in first-year University students. Saudi Med J. (2017) 38:1125–31. doi: 10.15537/smj.2017.11.20526
52. Rumana A, Sudharani M, Kallupurackal S, Ramya V, Nagendra G, Suryakantha A. Prevalence of premenstrual syndrome among medical students. Natl J Community Med. (2017) 8:292–4. Availble online at: http://www.njcmindia.org/uploads/8-6_292-294.pdf
53. Katwal PC, Karki NR, Sharma P, Tamrakar SR. Dysmenorrhea and stress among the nepalese medical students. Kathmandu Univ Med J. (2016) 14:318–21.
54. Jaiprakash H, Myint K, Chai L, Nasir B. Prevalence of dysmenorrhea and its sequel among medical students in a Malaysian University. Br J Med Med Res. (2016) 16:1–8. doi: 10.9734/BJMMR/2016/25135
55. Goweda RA, Alkot MM, Alturkistani FA, Alhajaji RJ, Aljebali SS, Baashr ZA. Prevalence of premenstrual dysphoric disorder among medical students of Umm Al-Qura University, Makkah Al-Mukaramah, Kingdom of Saudi Arabia. Middle East J Family Med. (2016) 14:14–20. doi: 10.5742/MEWFM.2015.92785
56. Raval C, Panchal B, Tiwari D, Vala A, Bhatt R. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder among college students of Bhavnagar, Gujarat. Indian J Psychiatry. (2016) 58:164–70. doi: 10.4103/0019-5545.183796
57. Ritonga MA. Relationship between menstrual profile and psychological stress with dysmenorrhea. Althea Med J. (2016) 3:382–7. doi: 10.15850/amj.v3n3.884
58. Oyola MG, Handa RJ. Hypothalamic–pituitary–adrenal and hypothalamic–pituitary–gonadal axes: sex differences in regulation of stress responsivity. Stress. (2017) 20:476–94. doi: 10.1080/10253890.2017.1369523
59. Juruena MF. Early-life stress and HPA axis trigger recurrent adulthood depression. Epilepsy Behav. (2014) 38:148–59. doi: 10.1016/j.yebeh.2013.10.020
60. Herman JP, McKlveen JM, Ghosal S, Kopp B, Wulsin A, Makinson R, et al. Regulation of the hypothalamic-pituitary-adrenocortical stress response. Compreh Physiol. (2016) 6:603–21. doi: 10.1002/cphy.c150015
61. Armour M, Parry K, Manohar N, Holmes K, Ferfolja T, Curry C, et al. The prevalence and academic impact of dysmenorrhea in 21,573 young women: a systematic review and meta-analysis. J Womens Health. (2019) 28:1161–71. doi: 10.1089/jwh.2018.7615
62. Kleinstauber M, Witthoft M, Hiller W. Cognitive-behavioral and pharmacological interventions for premenstrual syndrome or premenstrual dysphoric disorder: a meta-analysis. J Clin Psychol Med Settings. (2012) 19:308–19. doi: 10.1007/s10880-012-9299-y
63. Shah NR, Jones JB, Aperi J, Shemtov R, Karne A, Borenstein J. Selective serotonin reuptake inhibitors for premenstrual syndrome and premenstrual dysphoric disorder: a meta-analysis. Obstet Gynecol. (2008) 111:1175–82. doi: 10.1097/AOG.0b013e31816fd73b
64. Heinen I, Bullinger M, Kocalevent R-D. Perceived stress in first year medical students - associations with personal resources and emotional distress. BMC Med Educ. (2017) 17:4. doi: 10.1186/s12909-016-0841-8
65. Dyrbye LN, Harper W, Durning SJ, Moutier C, Thomas MR, Massie FS Jr, et al. Patterns of distress in US medical students. Med Teach. (2011) 33:834–9. doi: 10.3109/0142159X.2010.531158
66. Dyrbye LN, Shanafelt TD. Commentary: medical student distress: a call to action. Acad Med. (2011) 86:801–3. doi: 10.1097/ACM.0b013e31821da481
67. Fasoro AA, Oluwadare T, Ojo TF, Oni IO. Perceived stress and stressors among first-year undergraduate students at a private medical school in Nigeria. J Taibah Univ Med Sci. (2019) 14:425–30. doi: 10.1016/j.jtumed.2019.08.003
68. Widholm O, Kantero R-L. III Menstrual patterns of adolescent girls according to chronological and gynecological ages. Acta Obstetric Gynecol Scand. (1971) 50:19–29. doi: 10.3109/00016347109155077
69. Demir SC, Kadayýfçý TO, Vardar MA, Atay Y. Dysfunctional uterine bleeding and other menstrual problems of secondary school students in Adana, Turkey. J Pediatr Adolesc Gynecol. (2000) 13:171–5. doi: 10.1016/S1083-3188(00)00061-9
70. Clarvit SR. Stress and menstrual dysfunction in medical students. Psychosomatics. (1988) 29:404–9. doi: 10.1016/S0033-3182(88)72341-5
Keywords: menstrual disturbances, pre-menstrual syndrome, pre-menstrual dysphoric disorder, dysmenorrhea, prevalence, medical students, undergraduate students
Citation: Maity S, Wray J, Coffin T, Nath R, Nauhria S, Sah R, Waechter R, Ramdass P and Nauhria S (2022) Academic and Social Impact of Menstrual Disturbances in Female Medical Students: A Systematic Review and Meta-Analysis. Front. Med. 9:821908. doi: 10.3389/fmed.2022.821908
Received: 26 November 2021; Accepted: 14 January 2022;
Published: 15 February 2022.
Edited by:
Pentti Nieminen, University of Oulu, FinlandReviewed by:
Hannu Vähänikkilä, University of Oulu, FinlandCopyright © 2022 Maity, Wray, Coffin, Nath, Nauhria, Sah, Waechter, Ramdass and Nauhria. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samal Nauhria, c2FtYWxuYXVocmlhQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.