
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Med., 10 March 2022
Sec. Obstetrics and Gynecological Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.817029
 Shuangshuang Lu1,2†
Shuangshuang Lu1,2† Xinyu Yao2†
Xinyu Yao2† Jun Shi2†
Jun Shi2† Jian Huang2
Jian Huang2 Shaohua Zhuang2
Shaohua Zhuang2 Junfang Ma2
Junfang Ma2 Yan Liu2
Yan Liu2 Wei Zhang2
Wei Zhang2 Lifei Yu2
Lifei Yu2 Ping Zhu2
Ping Zhu2 Qiuwei Zhu2
Qiuwei Zhu2 Ruxia Shi2
Ruxia Shi2 Hong Zheng2
Hong Zheng2 Dong Shao2
Dong Shao2 Yuyan Pan2
Yuyan Pan2 Shizhen Bao2
Shizhen Bao2 Li Qin2
Li Qin2 Lijie Huang2
Lijie Huang2 Wenjia Liu1,2*
Wenjia Liu1,2* Jin Huang1,2*
Jin Huang1,2*Background: Intrauterine devices (IUDs) are commonly used as a contraceptive method. IUD migration and colon perforation are rare but serious complications occurring sometimes years after insertion.
Case: A 42-year-old woman with complaints of slight abdominal pain underwent a colonoscopy. Colonoscopy showed that a “nail” had penetrated the ascending colon wall and that an arm of the “nail” was embedded in the colon wall. We did not remove the “nail” rashly under colonoscopy. Considering the safety and effectiveness of the patient's operation, we were able to remove the “nail” easily by performing laparoscopic-endoscopic cooperative surgery (LECS) combined with hysteroscopy at the same time.
Conclusion: We report a case of successful removal of a colonic perforation device by colonoscopy, laparoscopy, and hysteroscopy, which is the first method used.
The intrauterine device (IUD) is one of the most effective measures of contraception available today, with its use increasing yearly. However, they may cause rare but potentially serious complications such as migration through the uterine wall and gastrointestinal perforation (1). Ideal treatment of IUD migration remains controversial (2).
We report a case of ectopic migration of an IUD with perforation of the ascending colon along with a literature review. This case has been reported in line with the SCARE criteria (3).
A 42-year-old female presented in our hospital with slight abdominal pain. On admission, the patient's vital signs were normal. In abdominal examination, tenderness without rebound tenderness was felt in the lower abdomen. She had no previous disease history, and her fertility history was 3-0-0-3. We arranged a colonoscopy for the patient, and intestinal preparation was carried out according to the 2015 ASGE guidelines. The whole intestinal preparation process is smooth. During the colonoscopy examination, a small nail was observed protruding through the intestinal wall (Figure 1A). It was firmly adherent to the colon wall. To avoid causing any damage to the intestine, we decided to discontinue the examination to confirm the source of the nail. The rest of the colonoscopy was eventless. Abdominal computed tomography (CT) was performed and showed a foreign body through the wall of the colon (Figure 1). We inquired about the patient's medical history in detail. The patient denied a history of foreign body swallowing. She underwent IUD implantation 6 months after her first delivery 18 years ago. Surprisingly, 2 years after IUD placement, she became pregnant and gave birth smoothly. At that time, uterine ultrasound did not show the IUD ring, so it was thought to have fallen out naturally. Then, the patient conceived naturally again and gave birth. Considering this reproductive history, we believe that the nail in the intestinal cavity is likely to be the IUD.

Figure 1. Colonoscopy and abdominal CT findings. Colonoscopy showed a foreign body similar to a nail in the ascending colon, and a local ulcer was formed (A). CT showed a foreign body through the wall of the colon (B,C).
To ensure the safety and effectiveness of the operation, we performed laparoscopic-endoscopic cooperative surgery (LECS) and hysteroscopy at the same time. During the operation (Figure 2), granulomas formed in the anterior wall of the ascending colon, protruding on the surface. A nail-like foreign body was removed from the intestine by foreign body forceps under enteroscopy. A clip was used for hemostasis and closure of wounds. As seen by laparoscopy during the operation, the wounds on the lateral intestine were eroded after removal of the IUD. Silk thread was used for preventive sutures at the weak part of the intestinal wall to prevent secondary perforation. Three laparoscopic ports were used. The intraoperative blood loss was minimal. Examination of the posterior wall of the uterus showed hyperemia and erosion, with a diameter of 1.5 cm, surrounding granulation tissue. No obvious abnormality was found during hysteroscopy (Figure 2; Supplementary Video 1). The operation (Figure 3) was carried out smoothly, and there was no special discomfort after the operation. She was discharged after 5 days of postoperative recovery. One month after the operation, the patient went to the clinic for follow-up and a re-check abdominal CT, and no abnormality was found.
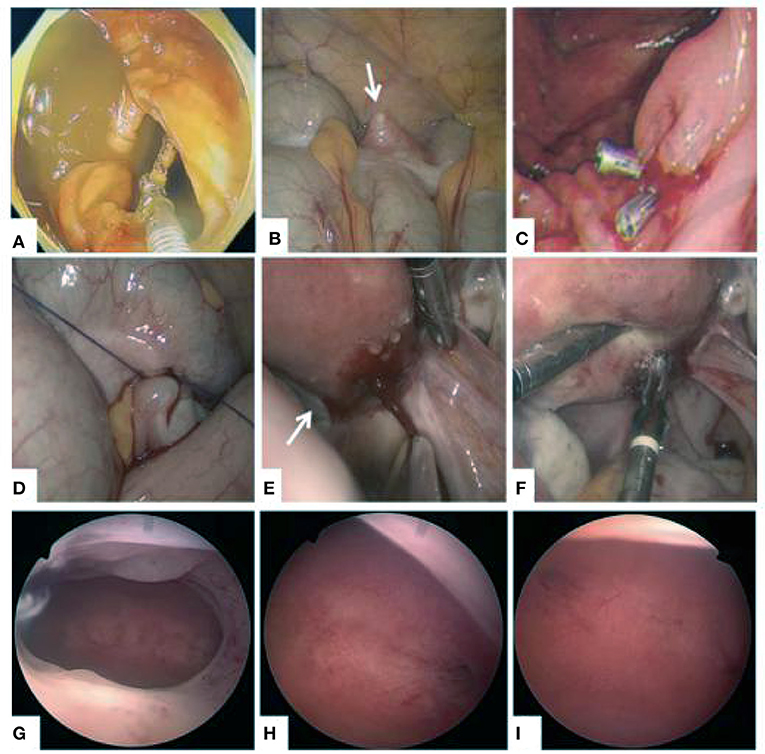
Figure 2. Laparoscopic-endoscopic cooperative surgery and no obvious abnormality were found during hysteroscopy. (A) The IUD was removed under laparoscope. (B) The IUD embedded in the colon wall showed a white protuberance outside the cavity (arrow). (C) Haemoclips at the wound site to prevent perforation of the colon. (D) The weak intestinal wall was sutured to prevent perforation. (E) Localized erosion at the posterior wall of the uterus and dense adhesions between the uterus and colon. (F) Bipolar coagulation to stop bleeding. (G) Morphology of uterine cavity. (H) Opening of right fallopian tube. (I) Opening of left fallopian tube.
In this case report, the patient underwent IUD placement after initial production but did not go to the gynecological clinic regularly thereafter. In the case of accidental pregnancy, an IUD was not found in the uterine cavity by ultrasonography, and it was mistakenly considered that the IUD had fallen out of the vagina and was excreted from the body. After the patient's second delivery, the contraceptive method used was safe period contraception, and the effect of this method was not good. Later, the patient became pregnant again and gave birth for a third time.
A literature search was conducted in PubMed on the 1st of August 2021 using the search terms “IUD perforation” and “colon”, covering 1969 to the present. There were 38 matches in total. After removing non-colon and incomplete data-related issues, 26 articles were included from the literature (1, 4–28). We reviewed 31 cases of IUD-related uterine and subsequent intestinal penetrations.
In most cases (Table 1), the patient placed an IUD during lactation after the initial delivery. At that time, the uterus was soft, and it was likely that a rare complication of placing an IUD occurred, which was that it was freed from the uterus and penetrated into the intestinal cavity, resulting in sterile perforation. The IUD is one of the most effective, safe, and economical contraceptive methods (4). However, IUDs have been associated with serious complications such as bleeding, uterine perforation, and bowel perforation (29). Perforation usually occurs immediately after insertion. However, it can occur years later. A possible mechanism for colonic penetration is adherence of the copper IUD to the pericolonic fat, followed by local inflammation and eventual penetration into the colon (5). Another less likely mechanism is uterine enlargement during the patient's pregnancy, physically displacing the IUD into the colon (30).
When the literature was analyzed (Table 2), most IUDs were perforated in the sigmoid colon. Chronic abdominal pain was the main manifestation of IUD migration, and acute abdominal pain was another main manifestation. Most patients could have the IUD removed by laparoscopy. In most cases, adhesions and bowel perforation were thought to have led to the abandonment of attempts at laparoscopy and subsequent laparotomy. Laparoscopy combined with hysteroscopy was used to remove the IUD in 2 cases (7, 26), which was related to the direction and shape of the IUD insertion. Two cases had the IUD removed without operation (9, 11). One patient did not receive treatment because she was older and had no clinical symptoms (9), and another died soon after due to other malignancies (11). In one case, there was imperfect removal because the 1-cm right arm of the IUD was suspected to have been left in the lumen of the colon (12). More rarely, there was a case (9) in which two different IUDs were found penetrating the colorectal wall. Although it is a general recommendation to remove all migrated uterine devices to avoid complications (8), leaving the device in place in asymptomatic patients should also be considered.
We report a case of IUD perforation found in the ascending colon that was successfully removed by colonoscopy, laparoscopy, and hysteroscopy. This operation is minimally invasive, safe, and effective. Injury to the intestine, abdominal cavity and uterine cavity were evaluated at the same time. This case was analyzed retrospectively. It was suggested that the patient should have regular re-examination 6 weeks after IUD placement (4). When the IUD is found to disappear in the uterine cavity, it should not be excluded that there is the possibility of ectopic migration, and physicians should be vigilant for the potential for intestinal perforation. Because there is a risk of perforation when removing intestinal foreign bodies under endoscopy, laparoscopy can be used to observe the abdominal side of the intestinal wall when removing intestinal foreign bodies under endoscopy to improve the safety and success rate of the operation.
The diagnosis of and operation for IUD perforations are complicated and difficult and may require the combined operation of digestive physicians, gastrointestinal surgeons, and gynecologists. However, due to the extensive use of IUDs (25), the diagnosis and treatment of this issue cannot be ignored. The combination of laparoscopy and colonoscopy, and even hysteroscopy, may increase the economic burden on patients, but it is helpful to identify the location, degree, and scope of the lesions. IUDs can be taken out accurately to reduce unnecessary damage to achieve minimal invasiveness and reduce the role of recurrence. In addition, the treatment can also identify uterine cavity injury to increase the probability of pregnancy and improve gastrointestinal tract healing and quality of life. It is an effective method in clinical practice. However, due to the complexity and intersection of surgery and specialty, it is suggested that it should be popularized gradually under the condition of fully evaluating the patient's condition and coordinating with relevant specialists.
We report a case of successful removal of a colonic perforation device by colonoscopy, laparoscopy, and hysteroscopy, which is the first method used. With the popularity of minimally invasive concepts and the continuous development of minimally invasive technology, multimirror combined technology will have high application value in the treatment of intestinal foreign body removal.
YL found intestinal foreign bodies in the renamed patient during the initial colonoscopy. WL, JinH, XY, JiaH, SL, WZ, LY, SZ, and JM have done a lot of work in colonoscopy, treatment, and postoperative follow-up. JS, PZ, and QZ participated in the laparoscopic operation. RS and HZ performed hysteroscopy for the patient. SB, LH, and LQ made contributions to intraoperative cooperation and postoperative nursing. DS performed intraoperative anesthesia for the patient. YP gave guidance on the treatment and medication of patients. SL sorted out all the materials and wrote a paper with XY and JS. JinH and WL finally revised the manuscript. The manuscript was written through the contributions of all authors. All authors have given approval to the final version of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.817029/full#supplementary-material
Supplementary Video 1. Hysteroscopy went well.
1. Zeino MY, Wietfeldt ED, Advani V, Ahad S, Younkin C, Hassan I. Laparoscopic removal of a copper intrauterine device from the sigmoid colon. JSLS. (2011) 15:568–70. doi: 10.4293/108680811X13176785204661
2. Gill RS, Mok D, Hudson M, Shi X, Birch DW, Karmali S. Laparoscopic removal of an intra-abdominal intrauterine device: case and systemic review. Contraception. (2012) 85:15–8. doi: 10.1016/j.contraception.2011.04.015
3. Agha RA, Fowler AJ, Saeta A, Barai I, Rajmohan S, Orgill DP, for the SCARE Group. The SCARE statement: consensus-based surgical case report guidelines. Int J Surg. (2016) 34:180–6. doi: 10.1016/j.ijsu.2016.08.014
4. Taras AR, Kaufman JA. Laparoscopic retrieval of intrauterine device perforating the sigmoid colon. JSLS. (2010) 14:453–5. doi: 10.4293/108680810X12924466006684
5. Takahashi H, Puttler KM, Hong C, Ayzengart AL. Sigmoid colon penetration by an intrauterine device: a case report and literature review. Mil Med. (2014) 179:e127–9. doi: 10.7205/MILMED-D-13-00268
6. Almarhabi Y. Asymptomatic cecal perforation and ileocecal fistula after intrauterine device migration: a case report. J Surg Case Rep. (2020) 2020:rjaa015. doi: 10.1093/jscr/rjaa015
7. Huang X, Zhong R, Zeng L, He X, Deng Q, Peng X, et al. Chronic nodules of sigmoid perforation caused by incarcerated intrauterine contraception device. Medicine. (2019) 98:e14117. doi: 10.1097/MD.0000000000014117
8. Huh JM, Kim KS, Cho YS, Suh DK, Lee JU, Baek SD, et al. Colonoscopic removal of an intrauterine device that had perforated the rectosigmoid colon. Ann Coloproctol. (2018) 34:106–8. doi: 10.3393/ac.2017.10.30
9. Tavecchia M, Burgos García A, de María Pallares P. Colorectal penetration by two intrauterine devices. Revista Española de Enfermedades Digestivas. (2019) 111:320–1. doi: 10.17235/reed.2019.5974/2018
10. Tabatabaei F, Masoumzadeh M. Dislocated intrauterine devices: clinical presentations, diagnosis and management. Eur J Contracept Reprod Health Care. (2021) 26:160–6. doi: 10.1080/13625187.2021.1874337
11. Sentilhes L, Lefebvre-Lacoeuille C, Poilblanc M, Descamps P. Incidental finding of an intrauterine device in the sigmoid colon. Eur J Contracept Reprod Health Care. (2009) 13:212–4. doi: 10.1080/13625180801892868
12. Lee J, Oh JH, Kim J, Lim C, Jung SH. Incomplete removal of an intrauterine device perforating the sigmoid colon. Korean J Gastroenterol. (2021) 78:48–52. doi: 10.4166/kjg.2021.041
13. Aliukonis V, Lasinskas M, Pilvelis A, Gradauskas A. Intrauterine device migration into the lumen of large bowel: a case report. Int J Surg Case Rep. (2020) 72:306–8. doi: 10.1016/j.ijscr.2020.06.011
14. Maroni ES, Genton CY. IUD-associated ovarian actinomycosis causing bowel obstruction. Arch Gynecol. (1986) 239:59–62. doi: 10.1007/BF02134289
15. Bitterman A, Lefel O, Segev Y, Lavie O. Laparoscopic removal of an intrauterine device following colon perforation. J Soc Laparoendosc Surg. (2010) 14:456–8. doi: 10.4293/108680810X12924466006963
16. Vekemans M, Verougstraete A. Late uterine perforation with an anchored IUD, the Gynefix: a case report. Contraception. (1999) 60:55–6. doi: 10.1016/S0010-7824(99)00055-4
17. Nceboz US, Ozcakir HT, Uyar Y, Caglar H. Migration of an intrauterine contraceptive device to the sigmoid colon: a case report. Eur J Contracept Reprod Health Care. (2003) 8:229–32. doi: 10.1080/ejc.8.4.229.232
18. Park JM, Lee CS, Kim MS, Kim DY, Kim CY, Lim YB, et al. Penetration of the descending colon by a migrating intrauterine contraceptive device. J Korean Soc Coloproctol. (2010) 26:433. doi: 10.3393/jksc.2010.26.6.433
19. Browning JJ, Bigrigg MA. Recovery of the intrauterine contraceptive device from the sigmoid colon. Three case reports. Br J Obstet Gynaecol. (1988) 95:530–2. doi: 10.1111/j.1471-0528.1988.tb12813.x
20. Akpinar F, Ozgur EN, Yilmaz S, Ustaoglu O. Sigmoid colon migration of an intrauterine device. Case Rep Obstet Gynecol. (2014) 2014:1–3. doi: 10.1155/2014/207659
21. Mederos R, Humaran L, Minervini D. Surgical removal of an intrauterine device perforating the sigmoid colon: a case report. Int J Surg. (2008) 6:e60–2. doi: 10.1016/j.ijsu.2007.02.006
22. Vandaele N, Iwanicki-Caron I, Piat M, Hervé S, Ducrotté P. Translocation of an intra-uterine contraceptive device with sigmoid penetration through an endometriosic nodule. Gastroentérologie Clinique et Biologique. (2009) 33:488–90. doi: 10.1016/j.gcb.2009.03.004
23. Sanlikan F, Arslan O, Avci ME, Göçmen A. Laparoscopic removal of an intrauterine device from the sigmoid colon. Pak J Med Sci. (2015) 31:214–6. doi: 10.12669/pjms.311.6096
24. Carson SA, Gatlin A, Mazur M. Appendiceal perforation by Copper-7 intrauterine contraceptive device. Am J Obstet Gynecol. (1981) 141:586–7. doi: 10.1016/S0002-9378(15)33284-1
25. Toumi O, Ammar H, Ghdira A, Chhaidar A, Trimech W, Gupta R, et al. Pelvic abscess complicating sigmoid colon perforation by migrating intrauterine device: a case report and review of the literature. Int J Surg Case Rep. (2018) 42:60–3. doi: 10.1016/j.ijscr.2017.10.038
26. Le A, Shan L, Xiao T, Zhuo R, Wang Z. Removal of an incarcerated intrauterine device in the sigmoid colon under the assistance of hysteroscope and laparoscope: a case report. Clin Exp Obstet Gyn. (2015) 42:531–4.
27. Nohuz E, Battista R, Tamburro S, Leonenko M, Bayeh S, Varga J, et al. A more and more painful intrauterine device… where it is not enough to see the wires to exclude malposition! Gynecol Obstet Fertil. (2014) 42:261–4. doi: 10.1016/j.gyobfe.2011.08.019
28. Brinth LS, Holte K, Andersen J. Penetrated IUD as the cause of stricture in the sigmoid colon. Ugeskr Laeger. (2007) 169:143–4.
29. Narayanamoorthy S, Christensen A, Apostol R. Intrauterine device perforation and adhesion formation. Obstet Gynecol. (2019) 133:110S–1S. doi: 10.1097/01.AOG.0000558830.72397.4e
Keywords: intrauterine devices, colon perforation, migration, laparoscopic-endoscopic cooperative surgery, hysteroscopy
Citation: Lu S, Yao X, Shi J, Huang J, Zhuang S, Ma J, Liu Y, Zhang W, Yu L, Zhu P, Zhu Q, Shi R, Zheng H, Shao D, Pan Y, Bao S, Qin L, Huang L, Liu W and Huang J (2022) Is It a “Colon Perforation”? A Case Report and Review of the Literature. Front. Med. 9:817029. doi: 10.3389/fmed.2022.817029
Received: 17 November 2021; Accepted: 04 February 2022;
Published: 10 March 2022.
Edited by:
Wenxian Guan, Nanjing University, ChinaReviewed by:
Wan Ahmad Hazim Wan Ghazali, MOH Putrajaya, MalaysiaCopyright © 2022 Lu, Yao, Shi, Huang, Zhuang, Ma, Liu, Zhang, Yu, Zhu, Zhu, Shi, Zheng, Shao, Pan, Bao, Qin, Huang, Liu and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenjia Liu, MTM4MTMwMTYyOTBAMTI2LmNvbQ==; Jin Huang, aGowNDIxNTNAaG90bWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.