- 1Division of Cardiology, Department of Internal Medicine, Shuang Ho Hospital, Taipei Medical University, New Taipei City, Taiwan
- 2Taipei Heart Institute, Taipei Medical University, Taipei, Taiwan
- 3Division of Cardiology, Department of Internal Medicine, School of Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan
- 4Division of Cardiovascular Surgery, Department of Surgery, Shuang Ho Hospital, Taipei Medical University, New Taipei City, Taiwan
- 5Division of Cardiovascular Surgery, Department of Surgery, School of Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan
- 6Graduate Institute of Data Science, College of Management, Taipei Medical University, Taipei, Taiwan
- 7Department of Neurosurgery, Wan-Fang Hospital, Taipei Medical University, Taipei, Taiwan
- 8Department of Medical Research Executive Secretary, Center of Human Research Protection, Shuang Ho Hospital, Taipei Medical University, New Taipei City, Taiwan
- 9Cardiovascular Center, Lo-Hsu Medical Foundation Lotung Poh-Ai Hospital, Luodong, Taiwan
- 10Department of Surgery, Lotung Poh-Ai Hospital, Luodong, Taiwan
- 11Graduate Institute of Clinical Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan
Backgrounds: The risk of stroke is higher among patients with chronic obstructive pulmonary disease (COPD) than among the healthy population. Moreover, women generally have worse long-term stroke outcomes than men.
Methods: The data of 6681 women with COPD (aged ≥ 65 years) registered in Taiwan’s National Health Insurance Research Database were retrospectively analyzed from January 1, 2001 to December 31, 2011. After 1:1 propensity score matching, the patients were divided into vaccinated and unvaccinated groups.
Results: In total, 5102 women were enrolled. The vaccinated group had a significantly lower risk of total, hemorrhagic, and ischemic stroke than the unvaccinated group (adjusted hazard ratio [aHR]: 0.60, 95% confidence interval [CI]: 0.54–0.67; aHR: 0.59, 95% CI: 0.43–0.83; and aHR: 0.59, 95% CI: 0.52–0.68, respectively). A lower risk of stroke was observed among the women aged 65–74 and ≥75 years, and the association was dose-dependent in all types of stroke (aHR: 1.08, 95% CI: 0.92–1.26; aHR: 0.70, 95% CI: 0.60–0.82; and aHR: 0.32, 95% CI: 0.26–0.38 for those vaccinated 1, 2 to 3, and ≥4 times, respectively, during the follow-up period). Women with a CHA2DS2-VASc score (conditions and characteristics included congestive heart failure, hypertension, diabetes, stroke, vascular disease, age, and sex) of 2–3 and ≥4 had a significantly lower risk of ischemic stroke while receiving more vaccinations. A smaller significant lower risk of hemorrhagic stroke after more than 4 times of vaccination was noted in the women with a CHA2DS2-VASc score of ≥4. Both interrupted and non-interrupted vaccination was associated with lower risk of stroke occurrence.
Conclusion: Influenza vaccination is associated with a lower risk of total, hemorrhagic, and ischemic stroke among women with COPD, and the association is dose-dependent. However, the findings may be limited by unmeasurable confounders. Further investigations on this subject are warranted.
Introduction
Chronic obstructive pulmonary disease (COPD) is the third leading global cause of death (1). Although COPD is primarily considered a complex respiratory tract disease characterized by irreversible airway pathological changes, it is also strongly associated with cardiovascular disease (2, 3). Common comorbidities of cardiovascular disease include heart failure, ischemic heart disease, obesity, hypertension, hyperlipidemia, and diabetes (4). Furthermore, factors contributing to the development of cardiovascular disease include systemic inflammation, hypoxemia, oxidative stress, and arterial stiffness (5).
Cardiovascular disease risk and stroke prevalence and incidence are all significantly higher in patients with COPD than in the healthy population (6). Stroke is one of the leading causes of functional disability that results in reduced quality of life in patients with COPD and increases caregiver burden. Notably, long-term stroke outcomes are less favorable in women than in men (7).
Studies have identified associations between seasonal influenza infection and an increased risk of cardiovascular mortality (8, 9). A study on influenza vaccination and reduction in hospitalization for cardiac and stroke events among older adults observed that influenza vaccination had a cardioprotective effect on patients with COPD (10). Therefore, high-risk patients should receive annual influenza vaccination (10–12). Although influenza vaccination may reduce the risk of stroke in patients at high risk for thrombogenicity (13, 14), the effect of influenza vaccination on women with COPD remains unclear. Thus, the present study explored the potential cerebroprotective association between influenza vaccination and the risk of stroke among women with COPD.
Materials and Methods
Taiwan’s National Health Insurance (NHI) program, launched in 1995, covers 98% of the population of Taiwan, which exceeds 23 million people. The NHI Research Database (NHIRD), which is maintained by the Health and Welfare Data Science Center, has been extensively analyzed and validated (13–16). In Taiwan, influenza vaccination is provided free of charge to adults aged older than 65 years with high-risk comorbidities (i.e., diabetes, chronic liver disease, cirrhosis, cardiovascular disease, and chronic pulmonary disease). All researchers using the NHIRD and its data subsets must sign a written agreement declaring that they have no intention of obtaining information that could potentially violate the privacy of patients or care providers.
Study Cohort
The patients enrolled in the present study were women recorded as having COPD between January 1, 2001 and December 31, 2011, with all diagnoses corresponding to the codes of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). The patients must have been ≥65 years of age (N = 6681) and have had at least two COPD diagnoses as inpatients or outpatients (17). The positive predictive value of the ICD-9-CM codes in COPD diagnosis was previously validated (16). Vaccination status was identified by code V048 and/or the use of vaccine (confirmed by drug codes).
Data Selection Process
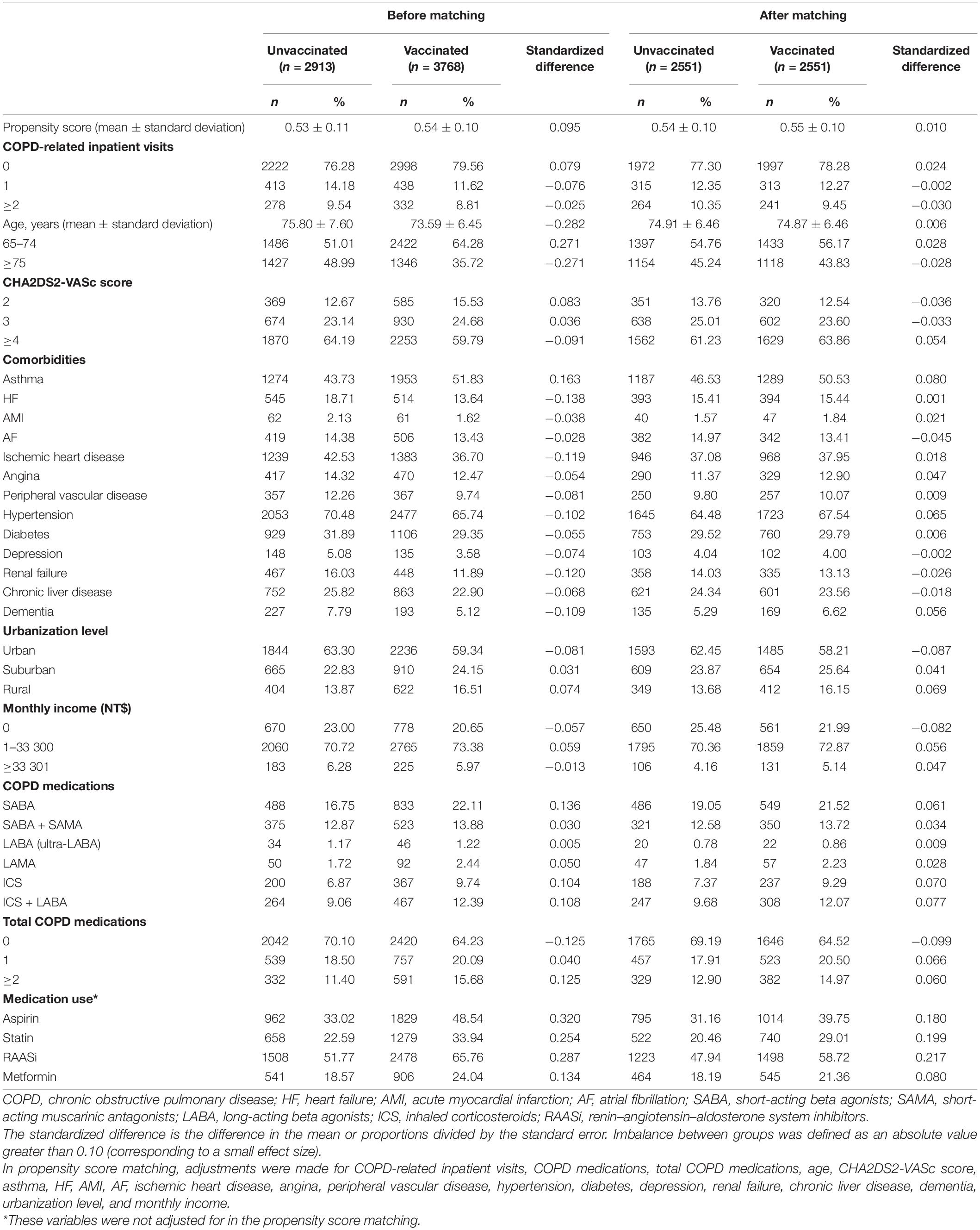
There were 3768 COPD patients who had vaccination and 2913 COPD patients who did not have vaccination. Propensity score matching (1:1) was performed and the patients were divided into vaccinated (n = 2551) and unvaccinated (n = 2551) groups (Figure 1A and Table 1).
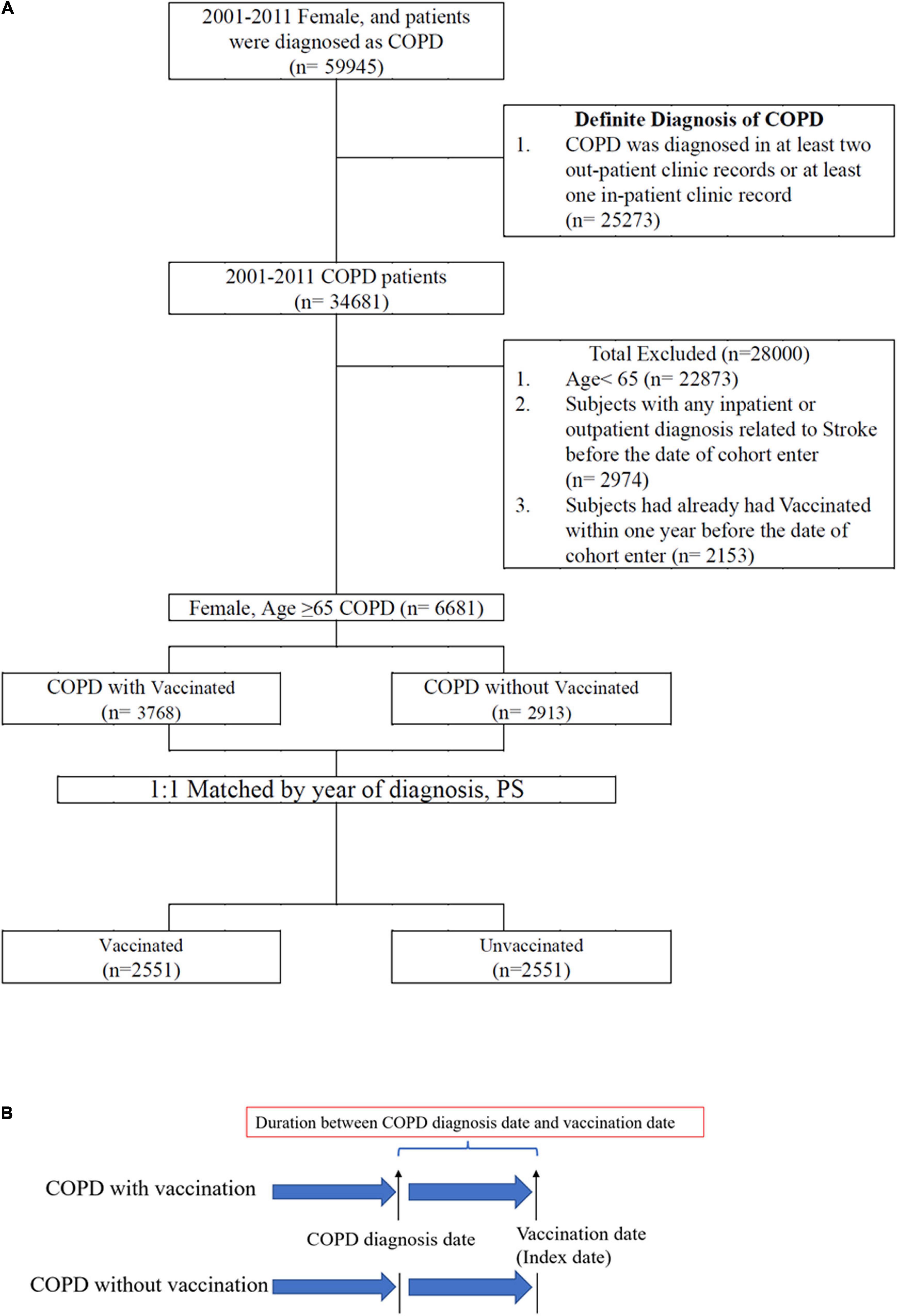
Figure 1. (A) Data selection process. (B) Definition of index date and duration between diagnosis date and vaccination date.
Index Date Definition
To avoid immortal time bias (18), the vaccination date of the patients in the vaccinated group was defined as the index or cohort entry date. In the matched pairs, the participants who did and did not receive vaccination were assigned the same index date (i.e., the vaccination date) for follow-up (Figure 1B).
Definition of Interrupted and Non-interrupted Vaccination
Patients who received more than two vaccinations were divided into interrupted and non-interrupted groups. Interrupted vaccination was defined as receiving more than two vaccinations with any interruption during the follow-up period. Non-interrupted vaccination was defined as receiving more than two yearly vaccinations without any interruption during the follow-up period.
Study Endpoint
The study endpoint was the initial diagnosis of hemorrhagic stroke (ICD-9-CM codes 430, 431, or 432), ischemic stroke (ICD-9-CM codes 433 or 434), or undefined stroke (ICD-9-CM code 436). All patients were followed until stroke diagnosis, withdrawal from NHI, loss to follow-up, death, or December 31, 2012. Except for those patients diagnosed with stroke, the other data were censored.
Potential Confounders
The potential confounders of the cohort were based on sociodemographic characteristics (age, urbanization level, and monthly income), comorbidities [asthma, heart failure [HF], acute myocardial infarction [AMI], atrial fibrillation [AF], ischemic heart disease, angina, peripheral vascular disease, hypertension, diabetes, depression, renal failure, chronic liver disease, dementia, and CHA2DS2-VASc score (19)], COPD severity and treatment (COPD-related inpatient visits, COPD medications, total number of COPD medications) and medication use (aspirin, statins, renin–angiotensin–aldosterone system inhibitors [RAASi], and metformin). These confounders have been implicated as possible risk factors in stroke (19–21).
Matching Factors
Propensity score matching, which involves assigning levels of 0 and 1 to a treatment variable, given a set of known variables, is used to adjust for potential selection bias, confounding, and differences between treatment groups in observational studies (22). In the present study, the propensity score of each vaccinated patient was estimated by logistic regression with the following 25 potential confounders associated with vaccine introduction: sociodemographic characteristics (age, urbanization level, and monthly income), comorbidities [asthma, HF, AMI, AF, ischemic heart disease, angina, peripheral vascular disease, hypertension, diabetes, depression, renal failure, chronic liver disease, dementia, and CHA2DS2-VASc score (19)], and COPD severity and treatment (COPD-related inpatient visits, COPD medications, and total number of COPD medications). The vaccinated and unvaccinated patients were then matched using propensity scores and a 1:1 nearest neighbor algorithm. As previously suggested (23), the caliper width was set as 0.03 of the pooled standard deviation of the logit of the propensity scores. Finally, the patients were divided into vaccinated (n = 2551) and unvaccinated (n = 2551) groups.
Statistical Analysis
In the present study, categorical data are expressed as numbers and percentages, whereas quantitative data are presented as the means ± standard deviations. The balance of characteristics was assessed by estimating the standardized differences (StDiffs) between the vaccinated and unvaccinated groups. Empirically, an absolute value of StDiffs that exceeds 0.1 (10%) represents a meaningful imbalance in a given variable between two groups. A Cox proportional hazards model was used to calculate the hazard ratios (HRs) to determine the differences in the risk of stroke between the groups. The adjusted HRs (aHRs) were HRs that were adjusted according to the confounder propensity score. In addition to the previously mentioned confounders, the duration between the COPD diagnosis date and index date was also included in the Cox proportional hazard model for aHR analysis. Fine and Gray’s (F&G) survival and regression analyses were used to determine the risk of stroke while competing with death. In this way the F&G method models the subdistribution hazards. The effect estimated using the F&G model shows the current and real differences between the treatment groups in terms of subdistribution hazards ratios. The assumption of proportionality of hazards is still a requirement, but of course it refers to the subdistribution hazards. The F&G model can accommodate time dependent coefficients to model the non-proportionality of hazards. This model can be applied to both the event of interest (stroke) or the competing risk (death). Sensitivity analysis can improve the understanding of the effects of drugs and biologics in epidemiologic database studies (24). Thus, in the present sensitivity analysis, the patients were stratified to estimate the association of age, CHA2DS2-VASc score, COPD-related inpatient visits, asthma, HF, AF, ischemic heart disease, angina, peripheral vascular disease, hypertension, diabetes, renal failure, and chronic liver disease with the incidence of stroke in different models. The cumulative incidence of stroke in the vaccinated and unvaccinated patients with COPD was calculated using the cumulative incidence function. All analyses were performed using SAS, version 9.4 (SAS Institute Inc., Cary, NC, United States). A two-tailed P-value of <0.05 was considered significant.
Results
The baseline characteristics of both groups of patients after propensity score matching are presented in Table 1. As mentioned, 6681 patients were enrolled, and after 1:1 propensity score matching, we divided the patients into vaccinated and unvaccinated groups (each group, n = 2551).
The Association Between Influenza Vaccination and Stroke Occurrence in Different Age Groups and Patients With Varying CHA2DS2-VASc Scores
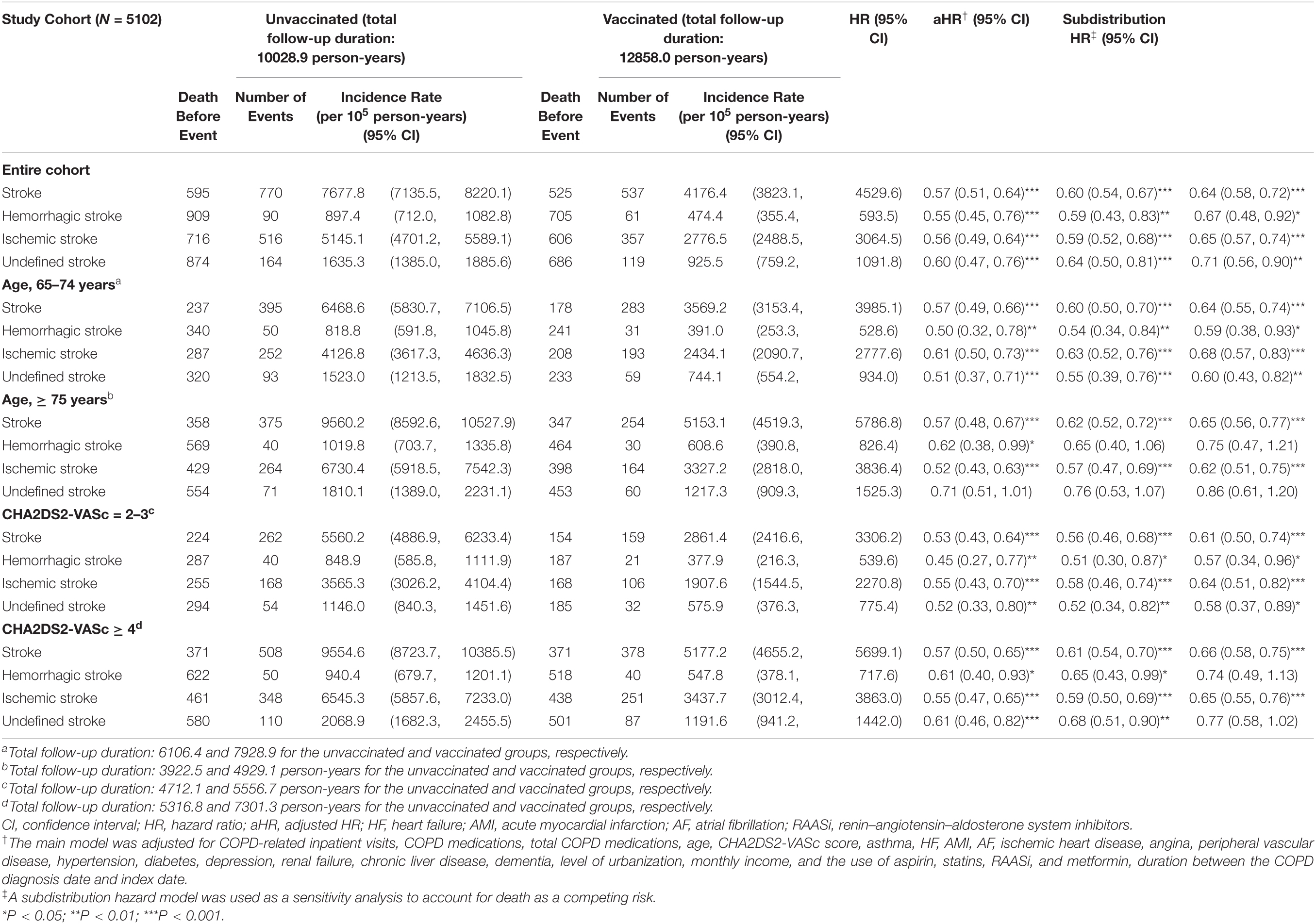
Table 2 shows the association between influenza vaccination and the risk of stroke in the present cohort, stratified by age and CHA2DS2-VASc score. Ischemic stroke was higher in incidence than hemorrhagic stroke during the follow-up period. Overall, the occurrence of all strokes, hemorrhagic, ischemic, and undefined were significantly lower in the vaccinated group (aHR: 0.60, 95% confidence interval [CI]: 0.54–0.67; aHR: 0.59, 95% CI: 0.43–0.83; aHR: 0.59, 95% CI: 0.52–0.68; and aHR: 0.64, 95% CI: 0.50–0.81, respectively) than in the unvaccinated group (Figures 2A–D). In the Fine and Gray competing risk model, the risk of all strokes remained significantly lower in the vaccinated group while competing with death (Table 2). Influenza vaccination was also associated with a lower risk of hemorrhagic, ischemic, and undefined stroke in patients aged 65 to 74 years. Vaccinated patients aged ≥75 years had a lower risk of all strokes and ischemic stroke than their unvaccinated counterparts.
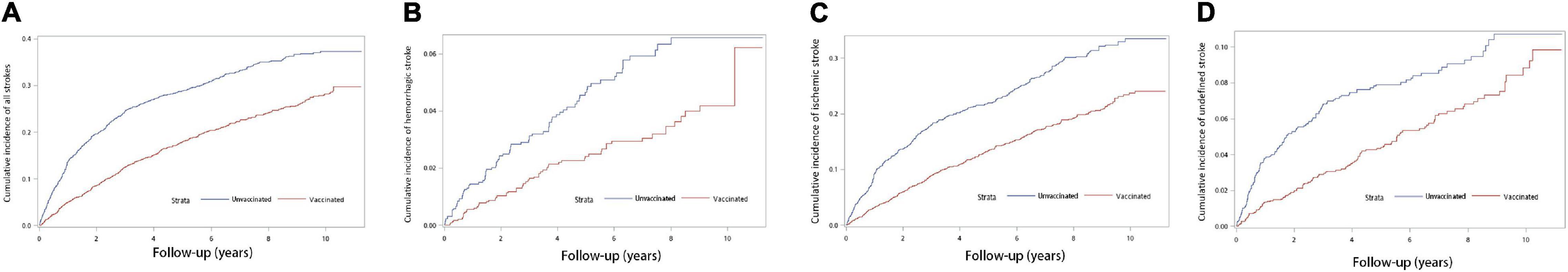
Figure 2. Cumulative incidence rates of different types of strokes estimated by the cumulative incidence function competing risk analysis between patients with and without vaccination. (A) Overall stroke events (χ2 = 79.308; df = 1; P < 0.001). (B) Hemorrhagic stroke events (χ2 = 13.466; df = 1; P < 0.001). (C) Ischemic stroke events (χ2 = 81.272; df = 1; P < 0.001). (D) Undefined stroke events (χ2 = 18.660; df = 1; P < 0.001).
The occurrence of hemorrhagic, ischemic, and undefined stroke was considerably lower in women with COPD and a CHA2DS2-VASc score of 2–3 after they were vaccinated. Compared with that of women with a CHA2DS2-VASc score of 2–3, the risk of ischemic stroke was significantly lower in vaccinated women with COPD who had higher CHA2DS2-VASc scores.
Association Between the Total Number of Influenza Vaccinations and Stroke Risk
In the main model, a higher number of influenza vaccinations over the follow-up period was associated with a lower risk of stroke occurrence in women with COPD overall (aHR: 1.08, 95% CI: 0.92–1.26; aHR: 0.70, 95% CI: 0.60–0.82; and aHR: 0.32, 95% CI: 0.26–0.38 for patients vaccinated 1, 2 to 3, and ≥4 times, respectively; Table 3 and Figure 3A). Patients with a history of asthma, HF, AF, ischemic heart disease, angina, hypertension, diabetes, renal failure, and chronic liver disease had a reduced risk of developing all types of stroke after they received more vaccinations. Notably, a considerably lower risk of all types of stroke was detected in patients without such history after they received more vaccinations. In patients with a CHA2DS2-VASc score 2–3, significantly lower risk of stroke after receiving more than four times of vaccination was observed. In patients with a CHA2DS2-VASc score ≥ 4, a substantially lower risk of all types of stroke was observed after more than two vaccinations, and further reductions in risk were noted in subsequent vaccinations, with a significant trend (Table 3). The patients with no COPD-related inpatient visits had a substantially lower risk of all types of strokes after receiving more than two vaccinations. The same results were noted in the patients with one COPD-related inpatient visit. Among patients with two or more COPD-related inpatient visits, the risk of all types of strokes only decreased after they received four or more vaccinations (Table 3). In patients who did not have influenza during the follow-up period, a substantially lower risk of all types of stroke was observed after vaccination. In patients who had influenza infection during the follow-up period, a significant trend of lower risk of all types of stroke was observed after vaccination (Table 3).
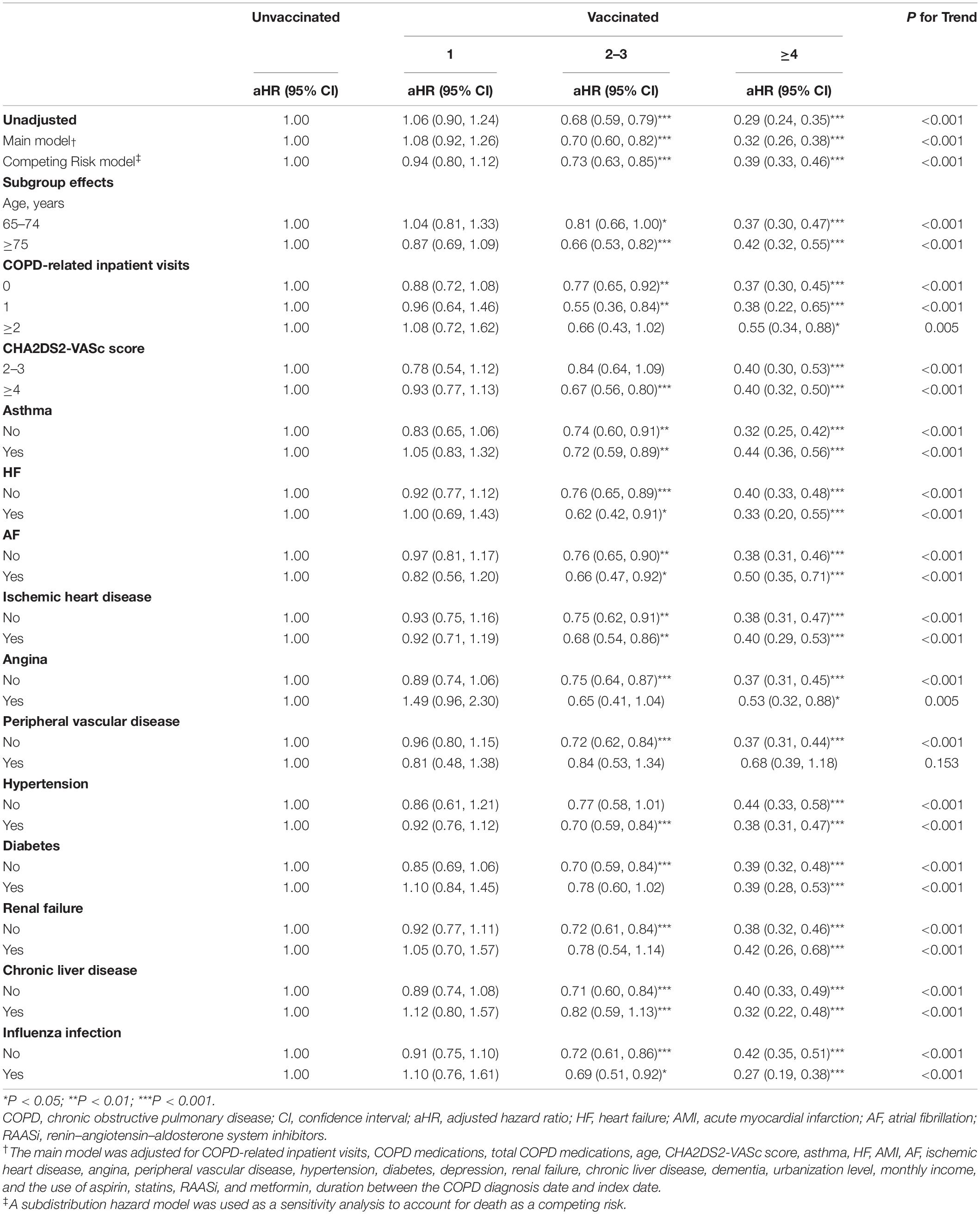
Table 3. Sensitivity analysis of the adjusted hazard ratios of vaccination in stroke risk reduction.
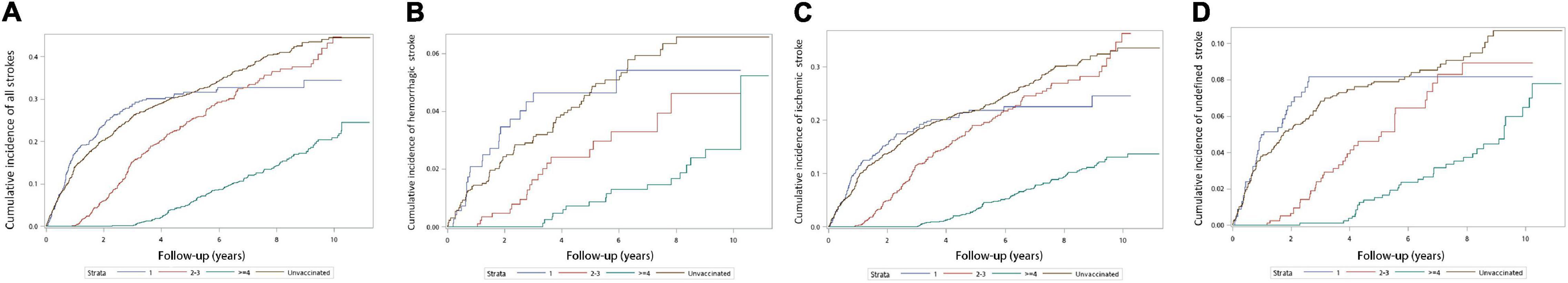
Figure 3. Cumulative incidence rates of different types of strokes estimated by the cumulative incidence function competing risk analysis between patients total number of vaccinations (A) Overall stroke events (χ2 = 217.451; df = 3; P < 0.001). (B) Hemorrhagic stroke events (χ2 = 27.725; df = 3; P < 0.001). (C) Ischemic stroke events (χ2 = 153.256; df = 3; P < 0.001). (D) Undefined stroke events (χ2 = 39.481; df = 3; P < 0.001).
Supplementary Tables 1–3 present the sensitivity analysis results of the total number of vaccinations in patients with hemorrhagic, ischemic, and undefined stroke, respectively. The main model analysis revealed that patients who received 2 to 3 and ≥ 4 vaccinations had a lower risk of developing these types of strokes (Supplementary Tables 1–3 and Figures 3B–D). Among patients with no COPD-related inpatient visits, the risk of hemorrhagic stroke decreased after they received more than 4 vaccinations. Following multiple vaccinations, patients without HF, ischemic heart disease, angina, peripheral vascular disease, diabetes, renal failure, or chronic liver disease were less likely to develop hemorrhagic stroke. After receiving more than four vaccinations, patients with hypertension had a reduced risk of hemorrhagic stroke. All the patients had a reduced risk or developed ischemic stroke after receiving a higher number of vaccinations, regardless of the presence of those comorbidities, except patients with angina. Among women with a CHA2DS2-VASc score ≥ 4, the risk of hemorrhagic stroke decreased following more than 4 times of vaccinations, but the risk of ischemic stroke decreased after receiving more than two times of vaccinations. Among patients with a CHA2DS2-VASc score 2–3, the risk of hemorrhagic stroke did not decrease despite receiving more than four times of vaccination. A lower risk of ischemic stroke and undefined stroke occurrence was observed in patients with a CHA2DS2-VASc score of 2 to 3, or ≥4 after they received 4 or more vaccinations.
Analysis revealed that both interrupted and non-interrupted influenza vaccinations (Supplementary Tables 4–6) were associated with a lower risk of all strokes. In the sensitivity analysis, the risk of stroke was significantly lower after receiving more vaccination regardless of influenza infection (Table 3 and Supplementary Tables 1–3). In mediator analysis of present study, there were no significant decreasing influenza infection after influenza vaccination (β = −0.129) nor significant occurrence of stroke after influenza infection (β = 0.127). However, there was a significant stroke risk reduction after influenza vaccination (β = −0.567***, p < 0.001). The results of mediator analysis suggested that influenza infection was not a mediator effect in the present study (Supplementary Figure).
Discussion
Main Findings
The main findings of the present nationwide population-based propensity-matched cohort study are as follows: (1) Overall, women with COPD had a potentially lower risk of developing any of the types of stroke after receiving influenza vaccination. A similar association between a lower risk of stroke and influenza vaccination was found in elderly (≥65 years-old) and late elderly (≥75 years-old) women (2). The association between influenza vaccination and a lower risk of stroke in women with COPD appeared to be dose-dependent and consistent across all types of stroke (3). Regardless of the presence of comorbidities, women with COPD had a significantly lower risk of ischemic stroke after receiving more than four influenza vaccinations. However, only women with COPD without comorbidities except hypertension had a lower risk of hemorrhagic stroke after receiving more than four influenza vaccinations during the follow-up period (4). Among women with COPD and a CHA2DS2-VASc score of 2 to 3, receiving more than four vaccinations was associated with a significantly lower risk of stroke. Women with COPD and CHA2DS2-VASc scores of ≥4 all had a significantly lower risk of stroke after receiving more than two influenza vaccinations.
Association Between Influenza Vaccination and Stroke in Women With Chronic Obstructive Pulmonary Disease
Influenza vaccination is strongly associated with a reduced risk of ischemic and hemorrhagic stroke (10, 13, 14, 25). In a recent nationwide observational study from Spain (26), a significantly higher risk of in-hospital mortality and mechanical ventilation usage was noted among women with COPD who were admitted because of ischemic stroke. Therefore, decreasing the risk of stroke in women with COPD is important. However, few studies have addressed the benefits of influenza vaccination in women with COPD.
The literature indicates the existence of sex differences in stroke. In general, women who have had a stroke are older and have more disabilities (7). Experimental studies have demonstrated the potential cardioprotective effect of estrogen (27). Therefore, postmenopausal women have a higher risk of stroke than premenopausal women (28). In Taiwan, influenza vaccination is provided free of charge to patients aged ≥65 years with high-risk comorbidities, which explains why the majority of the patients in the present study were postmenopausal. After adjustment for comorbidities, medications, urbanization level, monthly income, COPD-related inpatient visits, duration between COPD diagnosis date and vaccination date and age, influenza vaccination remained associated with a lower risk of all types of stroke. Furthermore, the risk of stroke remained significantly lower among older adults aged ≥75 years after receiving vaccination. In addition, a potential protective association was observed in both patients who did and did not have influenza.
Possible explanations are as follows: First, viral infection may trigger the thrombogenic process and induce coagulopathy (29). Influenza vaccination prevents postviral infection thrombus and hemorrhage. In addition, influenza infection may contribute to carotid atherosclerotic plaque inflammation and the eventual development of acute vascular events (30). Furthermore, lowering the risk of influenza infection prevents relevant consequences such as elevated sympathetic tone, hypoxemia, and endothelial dysfunction (31). Second, in a study on apoE knockout mice, influenza vaccination promoted the formation of smaller and more stable atherosclerotic plaques through an immunoresponse (32). Moreover, decreasing levels of interferon gamma, interleukin 2, and tumor necrosis factor alpha, as well as the activation of the bradykinin 2 receptor signaling pathway, constitute potential mechanisms underlying the stabilization of atherosclerotic plaques by influenza vaccination (32, 33).
As mentioned, the association between vaccination and a lower risk of stroke observed in the present study appeared to be dose-dependent and did not differ depending on whether multiple vaccinations were administered consecutively or were interrupted. A higher number of vaccinations was significantly associated with a reduction in all types of stroke, a result in line with that of another study (34). A systematic review and meta-analysis indicated that the protective effects of the influenza vaccine against different types of viruses may be less notable following repeated vaccinations (35). However, annual vaccination is still recommended for the prevention and control of influenza infections (36). The fact that vaccine effectiveness in the United States during the 2017–2018 influenza season was only 38% (37) suggests that receiving vaccination only once may not be sufficient to prevent contracting the virus. With more than one vaccination, the risk of influenza infection may also decrease, as may the risk of further cardiovascular complications, including stroke.
We further investigated the effect of the CHA2DS2-VASc score in women with COPD. Higher CHA2DS2-VASc scores were associated with a higher risk of ischemic stroke in patients with COPD, even those without AF (19). Notably, although the sensitivity analysis yielded significant results for both ischemic and hemorrhagic stroke, vaccination had a stronger risk reduction effect on ischemic stroke in the patients with CHA2DS2-VASc scores of ≥2. Because most hemorrhagic strokes are caused by ruptured cerebral vessels resulting from uncontrolled hypertension and abnormal cerebrovascular structure, the protective effect of influenza vaccination with plaque stabilization (32, 33) may be diminished in patients with these conditions. However, among female COPD patients with hypertension, the potentially risk reduction of hemorrhagic stroke was observed in the present study. Prospective studies are warranted to confirm these suppositions.
In addition, a significantly lower risk of stroke was observed in the patients with more inpatient visits because of the acute deterioration of their condition after they received four vaccinations, which is a greater number of vaccinations than that required for a protective effect against stroke in the patients with fewer inpatient visits. Thus, acute exacerbation in patients with COPD must be prevented to reduce complications.
In Taiwan, annual influenza vaccination constitutes a preventive strategy against an influenza epidemic. Previous nationwide studies conducted in Taiwan have indicated that influenza vaccination has benefits on cardiovascular and neurological outcomes (10, 14, 38). Overall, the present findings serve as a reference for policy-making with regard to annual influenza vaccination, especially in individuals with high-risk comorbidities.
Limitations
This study has several limitations. First, its retrospective nature limits the generalizability of the findings; prospective randomized controlled trials are required to confirm the present results. Second, the NHIRD does not contain definite information on the severity classification of COPD as indicated by physical activity, smoking status, alcohol intake, body mass index, spirometry test results, and other laboratory data. We performed propensity matching to minimize the impact of this limitation (22). Third, healthy user bias may have been present (39). Therefore, we adjusted for sociodemographic characteristics, such as urbanization and monthly income, as potential confounders. In addition, because influenza vaccination in Taiwan was provided free of charge to the members of our cohort, vaccination refusal caused by the inability to pay for the procedure seems unlikely; as mentioned, the influenza vaccine coverage rate among older adults in Taiwan has reached 49% in recent years (40). Fourth, the data of the present study were collected until the end of 2011, and future studies enrolled more recent data to validate the results of the present study. Moreover, although we controlled for and minimized the bias by propensity score matching and sensitivity analysis, the bias from the residual unmeasured confounders and healthy user bias could still present. Fifth, the patients enrolled in the present study were based on the ICD-9 diagnosis. Although the positive predictive rate and accuracy had been validated before (16, 17), the potential bias from patient selection process remained exist, which could influence the result of the present study.
In conclusion, influenza vaccination was associated with a considerably lower risk of ischemic, hemorrhagic, and undefined stroke in women with COPD, and the association appeared to be dose-dependent. Among women with a CHA2DS2-VASc score of ≥2, the association between vaccination and hemorrhagic stroke risk was not as substantial as ischemic stroke. Further investigations are required to determine the potential mechanism of influenza vaccination against stroke in this patient population.
Data Availability Statement
The data supporting the findings of this research were sourced from NHIRD in Taiwan. Owing to the legal restrictions imposed by the Government of Taiwan related to the Personal Information Protection Act, the database cannot be made publicly available.
Ethics Statement
The present study protocol was approved by the NHIRD research committee and the Taipei Medical University Joint Institutional Review Board (TMU-JIRB No. N201804043).
Author Contributions
W-RH and J-CL are the guarantors of the content of the manuscript and including the data and analysis. C-CChen conceived and designed the study and drafted the manuscript. Y-AF was responsible for data collection. Y-AF, C-HL, W-RH, C-CChiu, T-YY, M-HH, M-HL, H-TY, and Y-HW analyzed and interpreted the data. All authors reviewed the manuscript and approved its submission.
Funding
This work was financially supported of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan, and granted by the Taiwan Ministry of Health and Welfare (MOHW109-TDU-B-212-114007 and MOHW110-TDU-B-212-124007), and 109FRP-07 from the Taipei Medical University-Shuang Ho Hospital, Ministry of Health and Welfare.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.811021/full#supplementary-material
References
1. López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology. (2016) 21:14–23. doi: 10.1111/resp.12660
2. Rabe KF, Hurst JR, Suissa S. Cardiovascular disease and COPD: dangerous liaisons? Eur Respir Rev. (2018) 27:180057. doi: 10.1183/16000617.0057-2018
3. Donaldson GC, Hurst JR, Smith CJ, Hubbard RB, Wedzicha JA. Increased risk of myocardial infarction and stroke following exacerbation of COPD. Chest. (2010) 137:1091–7. doi: 10.1378/chest.09-2029
4. Smith MC, Wrobel JP. Epidemiology and clinical impact of major comorbidities in patients with COPD. Int J Chron Obstruct Pulmon Dis. (2014) 9:871–88. doi: 10.2147/copd.S49621
5. Maclay JD, MacNee W. Cardiovascular disease in COPD: mechanisms. Chest. (2013) 143:798–807. doi: 10.1378/chest.12-0938
6. Kim YR, Hwang IC, Lee YJ, Ham EB, Park DK, Kim S. Stroke risk among patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Clinics (Sao Paulo). (2018) 73:e177.
7. Bushnell CD. Stroke and the female brain. Nat Clin Pract Neurol. (2008) 4:22–33. doi: 10.1038/ncpneuro0686
8. Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL. Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol. (2016) 1:274–81. doi: 10.1001/jamacardio.2016.0433
9. Barnes M, Heywood AE, Mahimbo A, Rahman B, Newall AT, Macintyre CR. Acute myocardial infarction and influenza: a meta-analysis of case-control studies. Heart. (2015) 101:1738–47. doi: 10.1136/heartjnl-2015-307691
10. Nichol KL, Nordin J, Mullooly J, Lask R, Fillbrandt K, Iwane M. Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly. N Engl J Med. (2003) 348:1322–32. doi: 10.1056/NEJMoa025028
11. Phrommintikul A, Kuanprasert S, Wongcharoen W, Kanjanavanit R, Chaiwarith R, Sukonthasarn A. Influenza vaccination reduces cardiovascular events in patients with acute coronary syndrome. Eur Heart J. (2011) 32:1730–5. doi: 10.1093/eurheartj/ehr004
12. Bekkat-Berkani R, Wilkinson T, Buchy P, Dos Santos G, Stefanidis D, Devaster JM, et al. Seasonal influenza vaccination in patients with COPD: a systematic literature review. BMC Pulmon Med. (2017) 17:79. doi: 10.1186/s12890-017-0420-8
13. Kao PF, Liu JC, Hsu YP, Sung LC, Yang TY, Hao WR, et al. Influenza vaccination might reduce the risk of ischemic stroke in patients with atrial fibrillation: a population-based cohort study. Oncotarget. (2017) 8:112697–711. doi: 10.18632/oncotarget.22352
14. Liu JC, Wang TJ, Sung LC, Kao PF, Yang TY, Hao WR, et al. Influenza vaccination reduces hemorrhagic stroke risk in patients with atrial fibrillation: a population-based cohort study. Int J Cardiol. (2017) 232:315–23. doi: 10.1016/j.ijcard.2016.12.074
15. Sung LC, Chen CI, Fang YA, Lai CH, Hsu YP, Cheng TH, et al. Influenza vaccination reduces hospitalization for acute coronary syndrome in elderly patients with chronic obstructive pulmonary disease: a population-based cohort study. Vaccine. (2014) 32:3843–9. doi: 10.1016/j.vaccine.2014.04.064
16. Su VY, Yang KY, Yang YH, Tsai YH, Perng DW, Su WJ, et al. Use of ICS/LABA combinations or LAMA is associated with a lower risk of acute exacerbation in patients with coexistent COPD and Asthma. J Allergy Clin Immunol Pract. (2018) 6:1927–1935.e3. doi: 10.1016/j.jaip.2018.01.035
17. Ho TW, Ruan SY, Huang CT, Tsai YJ, Lai F, Yu CJ. Validity of ICD9-CM codes to diagnose chronic obstructive pulmonary disease from national health insurance claim data in Taiwan. Int J Chron Obstruct Pulmon Dis. (2018) 13:3055–63. doi: 10.2147/copd.S174265
18. Lévesque LE, Hanley JA, Kezouh A, Suissa S. Problem of immortal time bias in cohort studies: example using statins for preventing progression of diabetes. BMJ. (2010) 340:b5087. doi: 10.1136/bmj.b5087
19. Hu WS, Lin CL. CHA2DS2-VASc score for ischaemic stroke risk stratification in patients with chronic obstructive pulmonary disease with and without atrial fibrillation: a nationwide cohort study. Europace. (2018) 20:575–81. doi: 10.1093/europace/eux065
20. Mirzaei H. Stroke in women: risk factors and clinical biomarkers. J Cell Biochem. (2017) 118:4191–202. doi: 10.1002/jcb.26130
21. Söderholm M, Inghammar M, Hedblad B, Egesten A, Engström G. Incidence of stroke and stroke subtypes in chronic obstructive pulmonary disease. Eur J Epidemiol. (2015) 31:159–68. doi: 10.1007/s10654-015-0113-7
22. D’Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. (1998) 17:2265–81. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b
23. Heinze G, Jüni P. An overview of the objectives of and the approaches to propensity score analyses. Eur Heart J. (2011) 32:1704–8. doi: 10.1093/eurheartj/ehr031
24. Schneeweiss S. Sensitivity analysis and external adjustment for unmeasured confounders in epidemiologic database studies of therapeutics. Pharmacoepidemiol Drug Saf. (2006) 15:291–303. doi: 10.1002/pds.1200
25. Grau AJ, Fischer B, Barth C, Ling P, Lichy C, Buggle F. Influenza vaccination is associated with a reduced risk of stroke. Stroke. (2005) 36:1501–6. doi: 10.1161/01.Str.0000170674.45136.80
26. de Miguel-Díez J, López-de-Andrés A, Jiménez-García R, Hernández-Barrera V, Jiménez-Trujillo I, Ji Z, et al. Sex differences in the incidence and outcomes of COPD patients hospitalized with ischemic stroke in Spain: a population-based observational study. Int J Chron Obstruct Pulmon Dis. (2021) 16:1851–62. doi: 10.2147/copd.S311826
27. Mendelsohn ME, Karas RH. The protective effects of estrogen on the cardiovascular system. N Engl J Med. (1999) 340:1801–11. doi: 10.1056/nejm199906103402306
28. Bogousslavsky J, Pierre P. Ischemic stroke in patients under age 45. Neurol Clin. (1992) 10:113–24. doi: 10.1016/s0733-8619(18)30236-6
29. Goeijenbier M, van Wissen M, van de Weg C, Jong E, Gerdes VE, Meijers JC, et al. Review: Viral infections and mechanisms of thrombosis and bleeding. J Med Virol. (2012) 84:1680–96. doi: 10.1002/jmv.23354
30. Keller TT, van der Meer JJ, Teeling P, van der Sluijs K, Idu MM, Rimmelzwaan GF, et al. Selective expansion of influenza A virus-specific T cells in symptomatic human carotid artery atherosclerotic plaques. Stroke. (2008) 39:174–9. doi: 10.1161/strokeaha.107.491282
31. Vardeny O, Solomon SD. Influenza vaccination: a one-shot deal to reduce cardiovascular events. Eur Heart J. (2016) 38:334–7. doi: 10.1093/eurheartj/ehw560
32. Bermúdez-Fajardo A, Oviedo-Orta E. Influenza vaccination promotes stable atherosclerotic plaques in apoE knockout mice. Atherosclerosis. (2011) 217:97–105. doi: 10.1016/j.atherosclerosis.2011.03.019
33. Veljkovic V, Glisic S, Veljkovic N, Bojic T, Dietrich U, Perovic VR, et al. Influenza vaccine as prevention for cardiovascular diseases: possible molecular mechanism. Vaccine. (2014) 32:6569–75. doi: 10.1016/j.vaccine.2014.07.007
34. Ahmed AE, Nicholson KG, Nguyen-Van-Tam JS. Reduction in mortality associated with influenza vaccine during 1989-90 epidemic. Lancet. (1995) 346:591–5. doi: 10.1016/s0140-6736(95)91434-x
35. Ramsay LC, Buchan SA, Stirling RG, Cowling BJ, Feng S, Kwong JC, et al. The impact of repeated vaccination on influenza vaccine effectiveness: a systematic review and meta-analysis. BMC Med. (2019) 17:9. doi: 10.1186/s12916-018-1239-8
36. Grohskopf LA, Alyanak E, Broder KR, Blanton LH, Fry AM, Jernigan DB, et al. Prevention and Control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices – United States, 2020-21 influenza season. MMWR Recomm Rep. (2020) 69:1–24. doi: 10.15585/mmwr.rr6908a1
37. Rolfes MA, Flannery B, Chung JR, O’Halloran A, Garg S, Belongia EA, et al. Effects of influenza vaccination in the United States during the 2017-2018 influenza season. Clin Infect Dis. (2019) 69:1845–53. doi: 10.1093/cid/ciz075
38. Liu JC, Hsu YP, Kao PF, Hao WR, Liu SH, Lin CF, et al. Influenza vaccination reduces dementia risk in chronic kidney disease patients: a population-based cohort study. Medicine (Baltimore). (2016) 95:e2868. doi: 10.1097/MD.0000000000002868
39. Shrank WH, Patrick AR, Brookhart MA. Healthy user and related biases in observational studies of preventive interventions: a primer for physicians. J Gen Intern Med. (2011) 26:546–50. doi: 10.1007/s11606-010-1609-1
Keywords: women, COPD, influenza vaccination, ischemic stroke, hemorrhagic stroke
Citation: Chen C-C, Lin C-H, Chiu C-C, Yang TY, Hsu M-H, Wang Y-H, Lei M-H, Yeh HT, Fang Y-A, Hao W-R and Liu J-C (2022) Influenza Vaccination and Risk of Stroke in Women With Chronic Obstructive Pulmonary Disease: A Nationwide, Population-Based, Propensity-Matched Cohort Study. Front. Med. 9:811021. doi: 10.3389/fmed.2022.811021
Received: 08 November 2021; Accepted: 11 April 2022;
Published: 19 May 2022.
Edited by:
Anastassia Angelopoulou, University of Westminster, United KingdomReviewed by:
Jun-Jun Yeh, Ditmanson Medical Foundation Chia-Yi Christian Hospital, TaiwanLiang-Yu Chen, Taipei Veterans General Hospital, Taiwan
Copyright © 2022 Chen, Lin, Chiu, Yang, Hsu, Wang, Lei, Yeh, Fang, Hao and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen-Rui Hao, Yjg1MDEwNDNAdG11LmVkdS50dw==; Ju-Chi Liu, bGl1bWRjdkB0bXUuZWR1LnR3
 Chun-Chao Chen
Chun-Chao Chen Cheng-Hsin Lin2,4,5
Cheng-Hsin Lin2,4,5 Yu-Ann Fang
Yu-Ann Fang Ju-Chi Liu
Ju-Chi Liu