- 1Department of Epidemiology and Biostatistics, School of Public Health, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan-Aman, Ethiopia
- 2Department of Nutrition and Reproductive Health, School of Public Health, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan-Aman, Ethiopia
- 3Department of Public Health, School of Public Health, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan-Aman, Ethiopia
- 4Department of Nursing, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan-Aman, Ethiopia
- 5Department of Biomedical Science, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan-Aman, Ethiopia
- 6Doctoral School of Health Sciences, University of Debrecen, Debrecen, Hungary
Background: HIV-positive people can spread the virus through unprotected sex; however, HIV can be avoided if populations are educated about the risks. In underdeveloped nations, evidence suggests that the ABC method for HIV prevention is quite effective. As a result, the goal of this study was to determine the magnitude of HIV prevention behavior among adults in the Majang zone of Southwest Ethiopia, as well as the factors that influence it.
Methods: A community-based cross-sectional study was carried out from March 1st to May 31st, 2019. The data were collected through a face-to-face interview using a modified validated questionnaire among systematically selected study participants. The collected data were coded and entered using Epidata manager version 4.0.2.101 and analyzed using SPSS version 21. A logistic regression analysis was computed to determine the association using crude and adjusted odds ratios at 95% confidence intervals. The level of significance was declared at a p-value less than 0.05.
Results: Of the 772 adults interviewed, the proportion of adults who had good HIV preventive behavior was 51.8%, 95% CI [48.3–55.3%]. Two hundred forty (31.9%) were used abstinence as a type of HIV preventive behavior followed by being faithful (16.1%) and consistent condom use (7.3%). The study also found that respondents with the age group ≥27 years old (AOR = 1.56, 95% CI [1.3–3.12]), marital status (being married (AOR = 6.30, 95% CI [4.48–11.4]), and divorced/widowed (AOR = 5.50, 95% CI [2.60–12.4]) and having good knowledge of HIV prevention methods (AOR = 2.18, 95% CI [1.71–4.00]) were the factors associated with good HIV preventive behavior.
Conclusion and Recommendation: In the study area, overall HIV prevention behavior was average. The characteristics linked with successful HIV prevention behavior among adults in the Majang community included increasing age, being married or divorced/widowed, and having a solid understanding of HIV prevention approaches. As a result, policy-level and multi-sectorial intervention approaches from all stakeholders are necessary to develop short- and long-term strategies to address the problem and improve the community’s quality of life.
Introduction
Infection with the human immunodeficiency virus (HIV) is a major global public health issue that affects millions of people each year (1, 2). It is Africa’s second-biggest cause of morbidity and mortality, the fourth major cause of death overall, and the fifth leading cause of death from infectious diseases worldwide (3). The vast majority of HIV-positive people live in low- and middle-income nations (4).
The HIV epidemic, often known as AIDS, varies widely from nation to country and region to region (4), but it is particularly severe in Sub-Saharan Africa, especially Ethiopia, which accounts for more than two-thirds of the world’s HIV load (2, 5, 6). In Ethiopia, overall HIV prevalence has been fluctuating, with most regions indicating decreased trends. In 2005, Gambella, Addis Ababa, and Harari had the highest prevalence rates of 6.0 percent, 4.7 percent, and 3.5 percent, respectively. The highest frequency was observed in the regional state of Gambella, followed by Addis Ababa with 4.8 percent and 3.4 percent, respectively, in the 2016 survey (7).
HIV-positive people can spread the illness through unprotected sex (8), but the disease can be avoided if populations are educated about the risks (9). Abstain, Be Faithful, or Reduce the Number of Sexual Partners, and/or Use a Condom is an HIV/AIDS prevention strategy that is most narrowly defined as Abstain, Be Faithful, or Reduce the Number of Sexual Partners, and/or Use a Condom (10). Abstinence from sexual activity is the most efficient method of preventing pregnancy and sexually transmitted illnesses, such as HIV/AIDS (11). Peer pressure, sex myths, and misconceptions, the influence of drugs and alcohol, and the influence of media are all barriers to sexual abstinence that have become very difficult to overcome (12).
Abstinence-plus interventions emphasize the use of condoms and other safer sex practices in addition to sexual abstinence as the best approach to avoid HIV (13, 14). Being faithful to one’s sexual partner (s) is closely linked to a lower risk of contracting HIV. Couples who are not mutually faithful are more likely to contract HIV than couples who have been together for a long period (15). Condoms can help prevent HIV infection (16–18). Condoms have the greatest preventive impact when they are used frequently rather than infrequently (19). Condom use by HIV-seropositive couples results in near-zero transmission rates to the HIV-seronegative partner (6, 8, 20). Perceived susceptibility and perceived threat of HIV/AIDS showed a correlation with self-efficacy in condoms and their utilization (21).
Correct condom knowledge, as well as favorable attitudes about condom use, is linked to the likelihood of adolescents using condoms (4). Even though most persons were aware of the facts and agreed that condoms are an effective HIV prevention tool, consistent condom use during last sex was particularly low in East Africa (17). Self-efficacy of condoms and their use has been linked to perceived vulnerability and threat of HIV/AIDS (21). The effectiveness of condoms in preventing HIV transmission may be jeopardized if they are misused. Breakage, slipping, leaking, insufficient use, and other issues during the sexual event may jeopardize the condom’s protective function (22).
HIV counseling and condom distribution, which is integrated with other healthcare services and targeted at persons with lower educational attainment, is an essential technique for preventing new HIV infections (23). In underdeveloped nations, evidence suggests that the ABC method for HIV prevention is quite effective. In Uganda, the reduction in HIV prevalence has been dramatic, and it has been connected to changes in sexual behavior (24). As a result, the goal of this study was to determine the magnitude of HIV prevention behavior among adults in the Majang zone of Southwest Ethiopia, as well as the factors that influence it.
Materials and Methods
Study Design, Area, and Period
A community-based cross-sectional study was conducted in the Majang zone of Gambella Regional State. Majang zone is found in Gambella regional state and it is among HIV high prevalent areas in Ethiopia (25). It is found 628 km from Addis Ababa, the capital of Ethiopia in the Southwest direction. It has two woredas (namely Godere, and Mangeshi) and one town administration (Meti). Based on the population projection done by the Central statistical agency (CSA) for 2014–2017, the zone had a total population of 79,041, of whom 40,896 were men (26). The study was conducted from March 1st to May 31st, 2019.
Populations
All adults in the Majang zone were used as the source population. The study population consisted of all randomly selected adults in the Majang zone. Adults between the ages of 18 and 65 were included in the study, while adults who met the inclusion criteria but were extremely ill or unable to interact verbally throughout the data collecting period were excluded.
Sample Size Determination and Sampling Method
A single population proportion formula was used by taking the following assumptions; the good HIV preventive methods to be 47.6% (27), 95% confidence level, and 5% margin of error.
After adding 10% for the non-response rate and a design effect of 2; the final computed sample size was 845.
First, we chose 30 percent of Kebeles (the smallest administrative unit) from two woredas and 1 town administration in the Majang zone to identify the calculated sample. In Mangeshi, we took 6 out of 18 kebeles, in Godere, 5 out of 14 kebeles, and in Meti, 1 out of 2 kebeles. A systematic random selection technique was used to choose the sampling unit (households) from the specified kebeles using a sampling frame derived from the health post-family folder registry. Then, if there were more than one eligible participant in the home, the household’s eligible individual was chosen by lottery (28).
Study Variables and Measurements
The dependent variable was HIV preventive behavior. The independent variables were socio-demographic characteristics (age, sex, marital status, occupation, educational status, income, and residence), and lifestyle factors (alcohol drinking and khat chewing).
Good HIV preventive behavior: A participant who used at least one of the abstinence, be faithful or consistent condom use in the last 1 year (27) and avoid sharing of sharp materials in the last 6 months and tested for HIV in the last 3 months, otherwise poor HIV preventive behavior.
Substance use (alcohol drinking/khat chewing): consuming any substance (alcohol or khat) within the last 1 month/30 days (29).
Data Collection Instrument and Procedures
The information was gathered using a standardized questionnaire that was created following a review of similar research. The questionnaire was written in English, then translated into the local language, and retranslated back into English by an independent translator to ensure consistency. Experts in the field assessed the content validity. Cronbach’s alpha test was used to determine the analysis’ reliability, and the reliability coefficient was found to be substantial (Cronbach’s alpha: 0.77). Outside of the designated kebeles, a pre-test was conducted on 10% of the sample. The data collectors and supervisors received 1-day training on the objectives and data collection techniques. Face-to-face interviews were used to gather information. The data collection method was monitored by three supervisors. Daily checks were made to confirm the completeness and uniformity of the completed questionnaires.
Data Processing and Analysis
To reduce errors during data input, the obtained data were coded and entered using Epi-data management version 4.0.2.101, and then analyzed using SPSS version 21. Frequency tables were used to display summary statistics for the independent variables. The link was determined using a binary logistic regression with crude and adjusted odds ratios at 95 percent confidence intervals. Candidates for multivariable logistic regression analysis were independent variables with p-values less than 0.25 in bivariate regression analysis. In the multivariable logistic regression analysis, a p-value of less than 0.05 was considered significant.
Ethical Consideration
Mizan-Tepi University’s Research and Community Service Directorate provided ethical approval. A letter of cooperation was issued to the relevant government bodies in the study areas. The participants were also made aware that the information they supplied would be kept private and utilized solely for research purposes. The details of the ethical consideration were better explained in a previous publication (28).
Results
Socio-Demographic Characteristics
Of 844 respondents recruited, 772 responded to the interview yielding a response rate of 91.5%. Four hundred fifty-one (58.4%) of the respondents were aged less than 27 years. More than two-thirds (67.7%) and more than half (54.8%) of the respondents were male and protestant religious followers, respectively. More than half (59.6%) and about three-fourths (75.5%) of the respondents were Majang in ethnicity and from rural residences, respectively (Table 1).
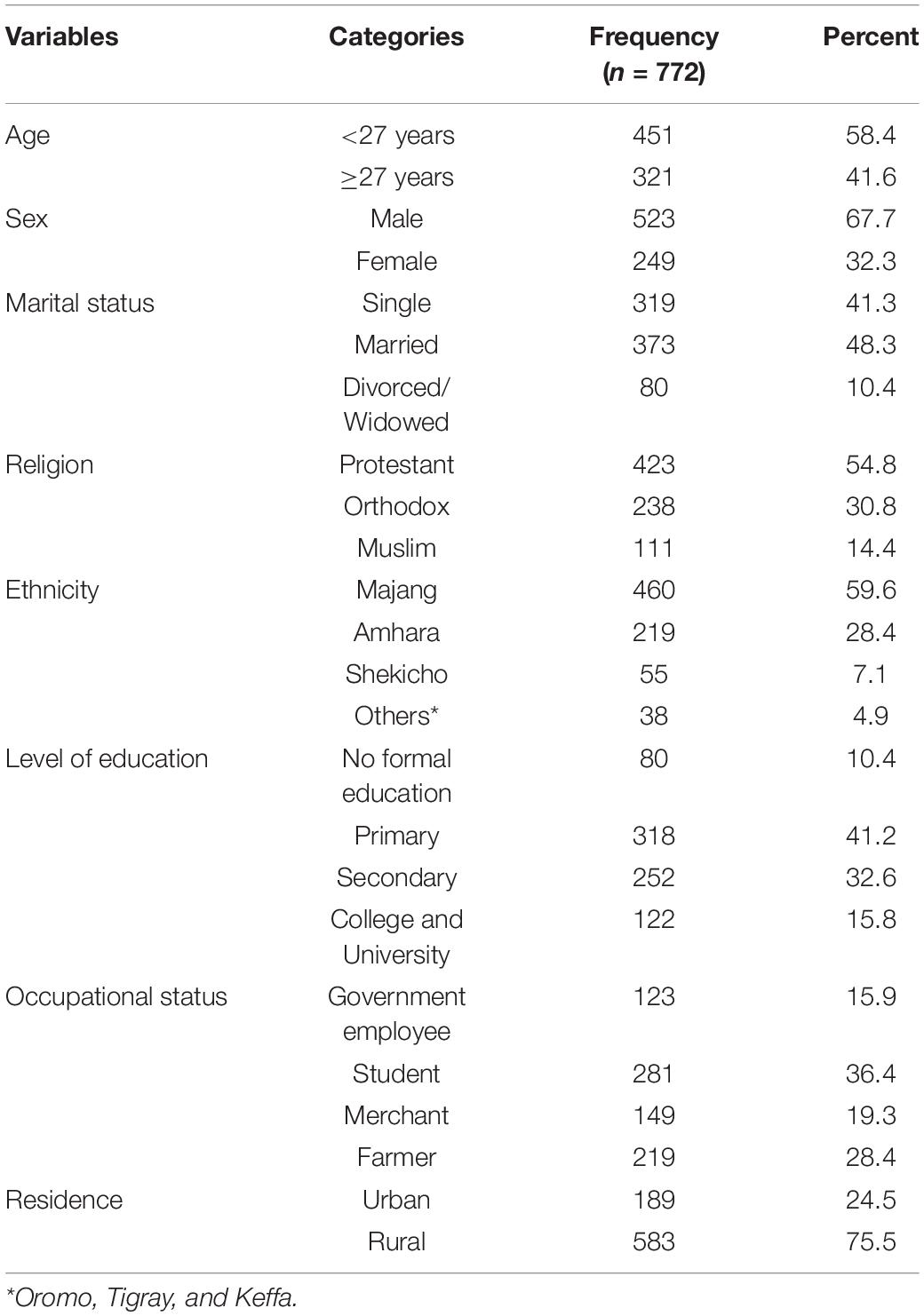
Table 1. Socio-demographic characteristics of the respondents at Majang zone in Southwest Ethiopia, 2019.
Behavioral Profiles and HIV Preventive Behavior
More than one-fourth (27.8%) and 176 (22.8%) of the respondents were alcohol drinkers and khat chewers, respectively. Of 772 respondents, 400 (51.8%) respondents had good HIV preventive behavior. Two hundred forty (31.9%) were used abstinence as a type of HIV preventive behavior followed by being faithful (16.1%) and consistent condom use (7.3%). Almost all (95.6%) didn’t share sharp materials in the last 6 months and 56.9% (439) were tested for HIV in the last 3 months (Table 2).
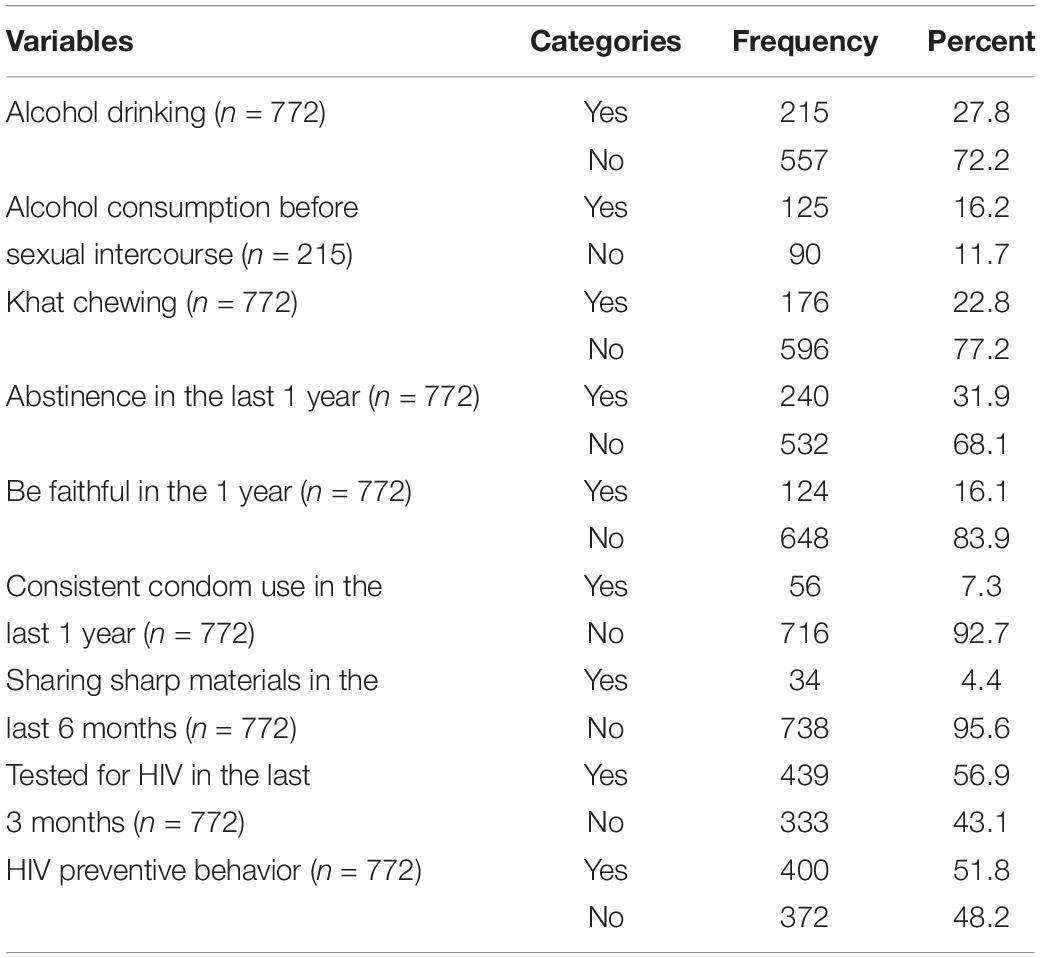
Table 2. Behavioral profiles and HIV preventive behavior of the respondents at Majang Zone in Southwest Ethiopia, 2019.
Factors Associated With the HIV Preventive Behavior
After adjusting for age, marital status, khat chewing, and knowledge of HIV preventive methods as confounding variables, age group ≥27 years old (AOR = 1.56, 95% CI [1.3–3.12]), marital status (being married (AOR = 6.30, 95% CI [4.48–11.4]), and divorced/widowed (AOR = 5.50, 95% CI [2.60–12.4]) and having good knowledge of HIV prevention methods (AOR = 2.18, 95% CI [1.71–4.00]) were the factors associated with good HIV preventive behavior (Table 3).
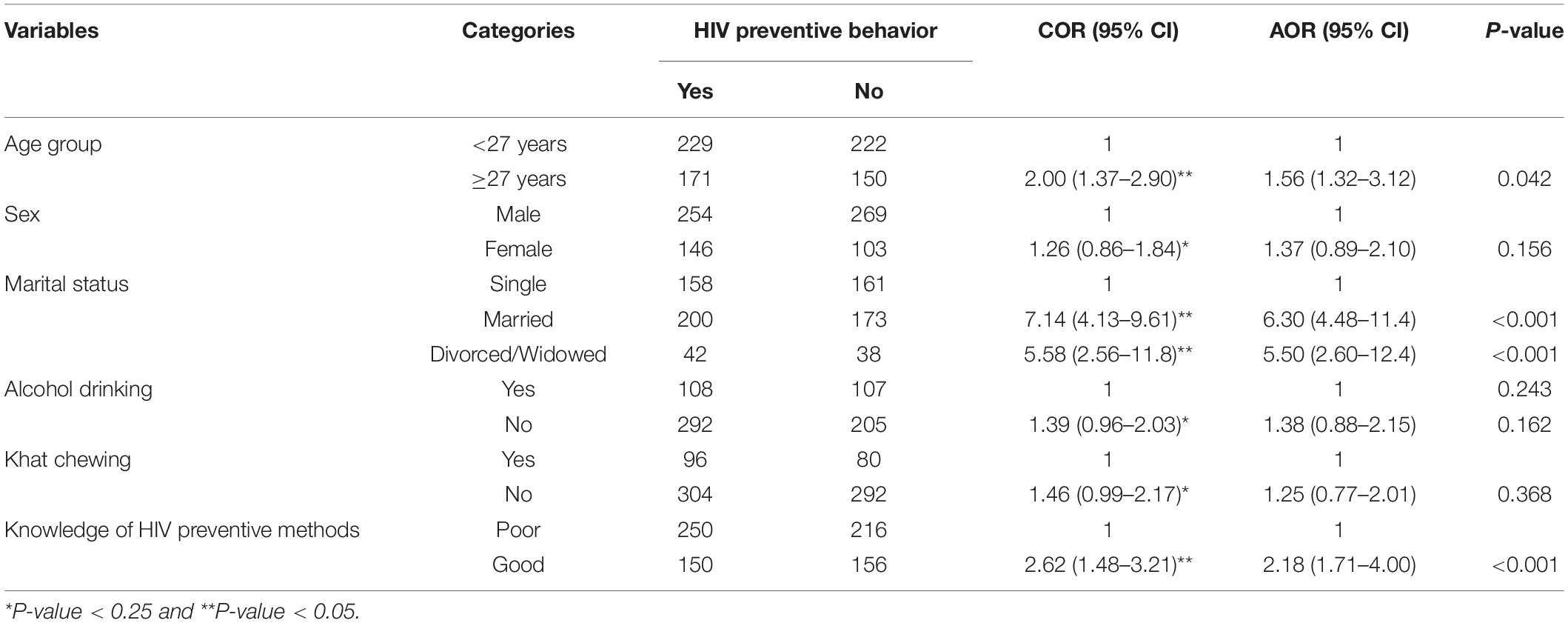
Table 3. Factors associated with HIV preventive behavior in the Majang zone, Southwest Ethiopia, 2019.
Discussion
HIV can be avoided if people are educated about the disease (9). ABCs is an HIV/AIDS prevention strategy (10). The adoption of an intervention focused on increasing condom usage, cleaner needle use, and a combination of abstinence, faithfulness, and condom use (ABC) significantly reduced HIV prevalence (9). The goal of this study was to determine the magnitude of HIV prevention behavior among adults in the Majang zone in Southwest Ethiopia, as well as the factors that influence it.
The magnitude of HIV preventive behavior was 51.8%, 95% CI [48.3–55.3%]. This finding was in line with 54.1% in Bale Zone, Ethiopia (30). It was higher than 47.6% in Bench-Sheko Zone (27) and 46.4% in West Gojjam Zone (31) studies in Ethiopia. But, it was lower than 61.1% in the Afar region, Ethiopia (32). The use of a condom regularly can help to minimize the spread of HIV and other sexually transmitted illnesses. Condom use is a cost-effective and cost-saving intervention (every €1 spent on condom distribution saves €5.51) (33). The magnitude of consistent condom use was 7.3%, 95% CI [5.5–9.2%]. It was lower than 46% in the Bench-Sheko Zone (27) and 16.8% in Hawassa (34) studies in Ethiopia, 60% in Cameroon (35), 16.7% in Iran (8), and 53% in the United States (18).
Individuals who had one or no sexual partner were had good knowledge of sexually transmitted infections (36), which is very good for applying good HIV preventive behavior. The magnitude of sexual abstinence was 31.9%, 95% CI [27.6–35.2%]. It was higher than 7.9% in the Bench-Sheko Zone, Ethiopia (27). It was lower than 37.1% in Côte d’Ivoire (11). The magnitude of be faithful was 16.1%, 95% CI [13.5–18.7%]. It was lower than 23.5% in the Bench-Sheko Zone, Ethiopia (27), 52% in Cameroon, and 74% in Zimbabwe (15). The magnitude of tested for HIV in the last 3 months was 56.9%, 95% CI [53.4–60.4%]. It was higher than 43.5% in the Bench-Sheko Zone, Ethiopia (27). Multiple factors contributed to the disparity between this and other research. It could be due to the sample size disparity, the operational definition utilized, or the approach as a whole. Furthermore, economical, behavioral, and sociocultural variables may all play a role in the observed variation.
The respondents’ age was statistically linked to their HIV prevention practice. Respondents under the age of 27 were 1.6 times more likely than those above the age of 27 to use HIV prevention strategies. This research matched that of a study conducted in Ethiopia’s Afar region (32). Individuals appear to be more aware of numerous approaches to avoid HIV/AIDS as they get older (27), which leads to better implementation of HIV preventive behavior.
Married and divorced/widowed respondents had 6.3 and 5.5 times higher probabilities of implementing HIV prevention activity than single respondents, respectively. Being married and being divorced/widowed were both substantially linked to HIV prevention behavior. Fontes MB et al. endorsed this study, which found that being married was linked to HIV prevention practices (37). Yosef T (38) revealed that being single or unmarried had a high chance of acquiring sexually transmitted infections due to the application of poor preventive behavior. This could be because married people are more likely to be faithful to their partners, which could lead to the usage of an HIV prevention strategy. Divorced and bereaved people are also more prone to refrain from sex because they feel demoralized as a result of their sexual partner’s separation.
Good knowledge about STIs including HIV/AIDS was associated with a positive attitude toward condom use (39). Knowing about the disease and the techniques for preventing it is beneficial to HIV prevention. Respondents with a good understanding of HIV prevention behavior were 2.2 times more likely to practice HIV prevention behavior than those with poor knowledge of HIV prevention behavior. Individuals who have comprehensive knowledge about HIV were more likely to practice HIV preventive behaviors than an individual lacking comprehensive knowledge about the disease (40, 41). This could be attributed to the respondent’s degree of practice, which is largely determined by their knowledge level. However, this result was incongruent with Nuked et al., there is no link between knowledge and behaviors/practices (35).
Limitation of the Study
Participants’ preventative habits were assessed by asking them to recall their previous preventive activities. As a result, there was a chance that recalling bias would be incorporated into the data, necessitating caution when interpreting and applying the findings of this study.
Conclusion
In the study area, overall HIV prevention behavior was average. The characteristics linked with successful HIV prevention behavior among adults in the Majang community included increasing age, being married or divorced/widowed, and having a solid understanding of HIV prevention approaches. As a result, policy-level and multi-sectorial intervention approaches from all stakeholders are necessary to develop short- and long-term strategies to address the problem and improve the community’s quality of life.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Research and Community service directorate of Mizan-Tepi University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
TY was involved in the conception, design, and acquisition of data, analysis, interpretation of the results, and drafted the manuscript. WW, TN, AA, QQ, BM, GM, NS, HA, and BB were involved in the design, acquisition of data, and analysis of the results. All authors approved it for publication.
Funding
This study was funded by the Mizan-Tepi University.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We acknowledge the study participants for their valuable participation and the Mizan-Aman town administration for their full collaboration and support by providing important data during the study. We would like to acknowledge data collectors and supervisors for their valuable contributions during data collection.
References
1. Joint United Nations Programme on HIV/AIDS [UNAIDS]. Miles to Go: Closing Gaps, Breaking Barriers, Righting Injustices. Geneva: Joint United Nations Programme on HIV/AIDS (2018).
2. Joint United Nations Programme on HIV/AIDS [UNAIDS]. UNAIDS Data 2017. Geneva: Joint United Nations Programme on HIV/AIDS (2017).
3. Ali MHM, Osman OB, Ibrahim MAM, Ahmed W. The effect of HIV/AIDS peer health education on knowledge, attitudes, and practices of secondary school students in Khartoum, Sudan. AIMS Public Health. (2015) 2:718–26. doi: 10.3934/publichealth.2015.4.718
4. Kayiki SP, Forste R. HIV/AIDS related knowledge and perceived risk associated with condom use among adolescents in Uganda. Afr J Reprod Health. (2011) 15:57–63.
5. Ali MS, Tesfaye Tegegne E, Kassa Tesemma M, Tesfaye Tegegne K. Consistent condom use and associated factors among HIV-positive clients on antiretroviral therapy in North West Ethiopian health center, 2016 GC. AIDS Res Treat. (2019) 2019:7134908.
6. Shewamene Z, Legesse B, Tsega B, Bhagavathula AS, Endale A. Consistent condom use in HIV/AIDS patients receiving antiretroviral therapy in Northwestern Ethiopia: implication to reduce transmission and multiple infections. HIV/AIDS Res Palliat Care. (2015) 7:119–24. doi: 10.2147/HIV.S79122
7. Kibret GD, Ferede A, Leshargie CT, Wagnew F, Ketema DB, Alebel A. Trends and spatial distributions of HIV prevalence in Ethiopia. Infect Dis Poverty. (2019) 8:90. doi: 10.1186/s40249-019-0594-9
8. Moazen B, Hajizadeh S, Nedjat S, Setayesh HR, Mohraz M, Gouya MM, et al. Determinants of consistent condom use among Iranians living with HIV/AIDS: implication for prevention. Int J High Risk Behav Addict. (2017) 6:e63237.
9. Setswe G. Abstinence and faithfulness programmes for prevention of HIV/AIDS among young people: what are the current debates? S Afr Fam Pract. (2007) 49:5–10. doi: 10.1080/20786204.2007.10873610
10. Murphy EM, Greene ME, Mihailovic A, Olupot-Olupot P. Was the “ABC” approach (abstinence, being faithful, using condoms) responsible for Uganda’s decline in HIV? PLoS Med. (2006) 3:e379. doi: 10.1371/journal.pmed.0030379
11. Koffi AK, Kawahara K. Sexual abstinence behavior among never-married youths in a generalized HIV epidemic country: evidence from the 2005 Cte d’Ivoire AIDS indicator survey. BMC Public Health. (2008) 8:408. doi: 10.1186/1471-2458-8-408
12. Mokwena K, Morabe M. Sexual abstinence: what is the understanding and views of secondary school learners in a semi-rural area of North West Province, South Africa? Sahara J. (2016) 13:81–7. doi: 10.1080/17290376.2016.1195281
13. Underhill K, Operario D, Montgomery P. Systematic review of abstinence-plus HIV prevention programs in high-income countries. PLoS Med. (2007) 4:e275. doi: 10.1371/journal.pmed.0040275
14. Underhill K, Montgomery P, Operario D. Abstinence-plus programs for HIV infection prevention in high- income countries (Review). Cochrane Database Syst Rev. (2008) 22:93–114.
15. Mishra V, Hong R, Assche SB, Barrere B. The Role of Partner Reduction and Faithfulness in HIV Prevention in Sub-Saharan Africa: Evidence from Cameroon, Rwanda, Uganda, and Zimbabwe. Calverton, MD: Macro International Inc (2009).
16. Rodrigues V, Pinheiro F, Onofrio CD, Barcelos P, Costa NDS, Amorim CM, et al. Factors associated with condom use among young men who have sex with men. Enferm Glob. (2017) 46:80–93.
17. Emmanuel W, Edward N, Moses P, William R, Geoffrey O, Monicah B, et al. Condom use determinants and practices among people living with HIV in Kisii County, Kenya. Open AIDS J. (2015) 9:104–11. doi: 10.2174/1874613601509010104
18. Gursahaney PR, Cordes S, Ofotokun I, Wall KM, Jamieson DJ, Haddad LB. Factors associated with condom use among HIV-positive women living in Atlanta, Georgia. PLoS One. (2019) 14:e0225406. doi: 10.1371/journal.pone.0225406
19. Gitau M, Siyan YI. Determinants ofinconsistent condom use among sero discordant couples in Cambodia. Am J Public Health Res. (2016) 4:69–74.
20. Feldblum PJ, Welsh MJ, Steiner MJ. Don’t overlook condoms for HIV prevention. Sex Transm Infect. (2002) 79:268–9. doi: 10.1136/sti.79.4.268
21. Ndabarora E, Mchunu G. Factors that influence utilisation of HIV/AIDS prevention methods among university students residing at a selected university campus. SAHARA J. (2014) 11:202–10. doi: 10.1080/17290376.2014.986517
22. Jabr AM, Di Stefano M, Greco P, Santantonio T, Fiore JR. Errors in condom use in the setting of HIV transmission: a systematic review. Open AIDS J. (2020) 14:16–26. doi: 10.2174/1874613602014010016
23. Gelaw YA, Magalhães RJS, Assefa Y, Williams G. Spatial clustering and socio-demographic determinants of HIV infection in Ethiopia, 2015–2017. Int J Infect Dis. (2019) 82:33–9. doi: 10.1016/j.ijid.2019.02.046
24. Alonso A, de Irala J. Strategies in HIV prevention: the A-B-C Rights were not granted to include this image in electronic media. Lancet. (2007) 364:1033–4.
25. Mekdim Ethiopia National Association. HIV/AIDS was Responsible for 17,181 Deaths in Ethiopia in 2017. Addis Ababa: Mekdim Ethiopia National Association (2019).
26. Federal Democratic Republic of Ethiopia Central Statistical Agency. Population projection of Ethiopia for All Regions at Wereda Level from 2014–2017. Addis Ababa: Federal Democratic Republic of Ethiopia Central Statistical Agency (2013).
27. Abdissa HG, Lemu YK, Nigussie DT. HIV preventive behavior and associated factors among mining workers in Sali traditional gold mining site bench Maji zone, Southwest Ethiopia: a cross sectional study. BMC Public Health. (2014) 14:1003. doi: 10.1186/1471-2458-14-1003
28. Wondimu W, Asefa A, Qanche Q, Nigussie T, Yosef T. Determinants of the community knowledge and attitude towards HIV prevention methods in Majang Zone, Southwest Ethiopia. HIV AIDS (Auckl). (2021) 13:21–9. doi: 10.2147/HIV.S289379
29. Yosef T, Getachew D, Bogale B, Wondimu W, Shifera N, Negesse Y, et al. Psychoactive substance use and its associated factors among truck drivers in Ethiopia. Biomed Res Int. (2021) 2021:1604245. doi: 10.1155/2021/1604245
30. Mohammed AY. Knowledge, attitude and practice on HIV/AIDS prevention among batu terara preparatory school students in Goba Town, Bale Zone, Southeast Ethiopia. Prim Health Care Open Access. (2015) 05:192.
31. Kassie AA, Gudayu TW, Araya BM. Knowledge, attitude, and preventive practices towards sexually transmitted infections among preparatory school students in West Gojjam Zone, Ethiopia. Adv Public Health. (2020) 2020:6894394.
32. Tadesse AW, Chernet W, Ahmed O, Tadesse W. HIV/AIDS preventive practice and associated factors among female sex workers in Afar Region, Ethiopia: a community based study. Ethiop J Health Sci. (2020) 30:45–54. doi: 10.4314/ejhs.v30i1.7
33. Bom RJM, Van Der Linden K, Matser A, Poulin N, Schim Van Der Loeff MF, Bakker BHW, et al. The effects of free condom distribution on HIV and other sexually transmitted infections in men who have sex with men. BMC Infect Dis. (2019) 19:222. doi: 10.1186/s12879-019-3839-0
34. Mekonnen M, Behailu T, Wakgari N. Knowledge, attitude, and practice regarding HIV/AIDS among people with disability in Hawassa City, Southern Ethiopia. Adv Public Health. (2018) 2018:9649610.
35. Nubed CK, Akoachere JFTK. Knowledge, attitudes and practices regarding HIV/AIDS among senior secondary school students in Fako Division, South West Region, Cameroon. BMC Public Health. (2016) 16:847. doi: 10.1186/s12889-016-3516-9
36. Nigussie T, Yosef T. Knowledge of sexually transmitted infections and its associated factors among polytechnic college students in Southwest Ethiopia. Pan Afr Med J. (2020) 37:68. doi: 10.11604/pamj.2020.37.68.22718
37. Fontes MB, Campos Crivelaro R, Scartezini AM, Lima DD, Garcia A, Fujioka RT. Determinant factors of knowledge, attitudes and practices regarding STD/AIDS and viral hepatitis among youths aged 18 to 29 years in Brazil. Cien Saude Colet. (2017) 22:1343–52. doi: 10.1590/1413-81232017224.12852015
38. Yosef T. Sexually transmitted infection associated syndromes among pregnant women attending antenatal care clinics in Southwest Ethiopia. Heliyon. (2021) 7:e07576. doi: 10.1016/j.heliyon.2021.e07576
39. Yosef T, Nigussie T. Behavioral profiles and attitude toward condom use among college students in Southwest Ethiopia. Biomed Res Int. (2020) 2020:9582139. doi: 10.1155/2020/9582139
40. Yuliza WT, Hardisman H, Nursal DGA. Factors related to HIV/AIDS prevention behavior among female sex workers in Padang in 2018. Sains Med J Kedokt dan Kesehat. (2019) 10:18–25.
Keywords: HIV/AIDS, preventive behavior, Majang zone, Gambella region, Ethiopia
Citation: Yosef T, Wondimu W, Nigussie T, Asefa A, Qanche Q, Mekonnen B, Mesafint G, Shifera N, Amsalu H and Bekele BB (2022) Factors Associated With HIV Preventive Behavior Among Adults in Majang Zone of Gambella Region, Southwest Ethiopia. Front. Med. 9:807730. doi: 10.3389/fmed.2022.807730
Received: 02 November 2021; Accepted: 17 March 2022;
Published: 19 April 2022.
Edited by:
Claudio Fenizia, University of Milan, ItalyReviewed by:
Agegnehu Bante, Arba Minch University, EthiopiaAbel Sinshaw, University of Gondar, Ethiopia
Copyright © 2022 Yosef, Wondimu, Nigussie, Asefa, Qanche, Mekonnen, Mesafint, Shifera, Amsalu and Bekele. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tewodros Yosef, dGV3b2Ryb3N5b3NlZjQ3QG10dS5lZHUuZXQ=, orcid.org/0000-0002-3173-6753
 Tewodros Yosef
Tewodros Yosef Wondimagegn Wondimu1
Wondimagegn Wondimu1 Tadesse Nigussie
Tadesse Nigussie Adane Asefa
Adane Asefa Besufekad Mekonnen
Besufekad Mekonnen Gebremeskel Mesafint
Gebremeskel Mesafint Nigusie Shifera
Nigusie Shifera Hailemariam Amsalu
Hailemariam Amsalu Bayu Begashaw Bekele
Bayu Begashaw Bekele