- 1Department of Critical Care Medicine, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
- 2Education Center, National Cheng Kung University, Tainan, Taiwan
- 3Department of Emergency Medicine, National Taiwan University Medical College and Hospital, Taipei, Taiwan
- 4Department of Critical Care Medicine, MacKay Memorial Hospital, Taipei, Taiwan
- 5Department of Medicine, Mackay Medical College, New Taipei City, Taiwan
- 6Department of Critical Care Medicine, Changhua Christian Hospital, Changhua City, Taiwan
- 7Cardiovascular Center, Taichung Veterans General Hospital, Taichung, Taiwan
- 8Institute of Clinical Medicine, National Yang-Ming Chiao-Tung University, Taipei, Taiwan
- 9Department of Physical Therapy, Fooyin University, Kaohsiung, Taiwan
- 10School of Medicine, National Yang-Ming Chiao-Tung University, Taipei, Taiwan
Background and Purpose: Targeted temperature management (TTM) is associated with decreased mortality and improved neurological function after cardiac arrest. Additionally, studies have shown that bystander cardiopulmonary resuscitation (BCPR) doubled the survival of patients with out-of-hospital cardiac arrest (OHCA) compared to patients who received no BPCR (no-BCPR). However, the outcome benefits of BCPR on patients who received TTM are not fully understood. Therefore, this study aimed to investigate the outcome differences between BCPR and no-BCPR in patients who received TTM after cardiac arrest.
Methods: The Taiwan Network of Targeted Temperature Management for Cardiac Arrest (TIMECARD) multicenter registry established a study cohort and a database for patients receiving TTM between January 2013 and September 2019. A total of 580 patients were enrolled and divided into 376 and 204 patients in the BCPR and no-BCPR groups, respectively.
Results: Compared to the no-BCPR group, the BCPR group had a better hospital discharge and survival rate (42.25 vs. 31.86%, P = 0.0305). The BCPR group also had a better neurological outcome at hospital discharge. It had a higher average GCS score (11.3 vs. 8.31, P < 0.0001) and a lower average Glasgow–Pittsburgh cerebral performance category (CPC) scale score (2.14 vs. 2.98, P < 0.0001). After undertaking a multiple logistic regression analysis, it was found that BCPR was a significant positive predictor for in-hospital survival (OR = 0.66, 95% CI: 0.45–0.97, P = 0.0363).
Conclusions: This study demonstrated that BCPR had a positive survival and neurological impact on the return of spontaneous circulation (ROSC) in patients receiving TTM after cardiac arrest.
Introduction
Post-cardiac arrest care plays a crucial role in the functional recovery of patients after cardiac arrest. Targeted temperature management (TTM) is an important post-cardiac arrest neuroprotective treatment for patients after the return of spontaneous circulation (ROSC) (1). Although the pharmacologic mechanisms are not fully understood, there is a possibility of attenuating post-arrest reperfusion injury to therapeutic hypothermia by reducing cerebral metabolism, thereby reducing the release of excitatory amino acids and the production of oxygen free radicals and restoring the mechanism of normal intracellular signaling (2). Studies have shown that TTM improves neurological outcomes in patients after cardiac arrest (3).
The neuroprotective effects of TTM can be influenced by several factors, including the initial rhythm of cardiac arrest, pre-admission ROSC, the provision of percutaneous coronary intervention, the cooling method for the maintenance phase of TTM, and bystander cardiopulmonary resuscitation (BCPR) (4, 5). BCPR provides blood circulation to vital organs after cardiac arrest, thus reducing the risk of brain damage. The survival and neurological benefits of BCPR have been rigorously investigated in existing literature (6). However, the outcome benefits of BCPR in patients receiving TTM have not been explored. This study, therefore, aimed to investigate the outcome differences between BCPR and no-BCPR (those who had not received BCPR) in patients receiving TTM after cardiac arrest.
Materials and Methods
Study Design and Setting
We conducted a retrospective observational cohort study from January 2013 to September 2019 using data from the Taiwan Network of Targeted Temperature Management for Cardiac Arrest (TIMECARD) registry, a nationwide multicenter registry for cardiac arrest patients receiving TTM in post-cardiac arrest care (7).
The TIMECARD registry was managed by the Taiwan Society of Emergency and Critical Care Medicine. In participating hospitals, TTM was provided to patients with out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest (IHCA) with a Glasgow Coma Scale (GCS) score of <8 or those who could not obey verbal commands after ROSC. A temperature range between 32 and 36°C was maintained for at least 24 h, after which the body was slowly rewarmed at a rate of 0.2–0.5°C/h. Patients aged ≥ 18 years who received TTM after ROSC were included in this study.
Data Collection and Definitions
The primary variable in this study was whether the patient had received BCPR. In this study, BCPR was defined as “an attempt to perform basic cardiopulmonary resuscitation by someone who is not a part of an organized emergency response system,” according to the Utstein templates for resuscitation (8). Covariates of patient-related factors such as age, sex, and comorbidities were included. Covariates of resuscitation parameters such as event time, event location, witnessed collapse, initial rhythms, cause of cardiac arrest, cardiopulmonary resuscitation (CPR) duration, electrical discharge therapy, and pre-hospital ROSC were also included.
The initial rhythm was determined using either a manual defibrillator or an automated external defibrillator (AED). Cardiac arrest is classified as cardiogenic or non-cardiogenic. Cardiogenic origin is defined as cardiac arrest caused by myocardial ischemia or infarction, hypertrophic cardiomyopathy, valvular disease, and heart failure. Non-cardiac causes include drowning, trauma, asphyxia, respiratory disease, malignancy, electrolyte imbalance, sepsis, and uncontrolled bleeding. Electrical discharge therapy included defibrillation and synchronized cardioversion with manual defibrillators or AEDs. ROSC was defined as a palpable pulse lasting >20 s. Blood pressure and heart rate were immediately measured after ROSC.
We also recorded the heart rate, mean arterial pressure, and the GCS score at ROSC, time from ROSC to targeted temperature range, the cooling method for the maintenance phase of TTM, cold saline infusion during TTM, and patients who received coronary angiography. The cooling methods for the maintenance phase of TTM were classified into external and internal cooling. External cooling included a traditional cold blanket and the Arctic Sun medical device, which modulates patient temperature by circulating cold water in pads directly adhered to the patient's skin. Internal cooling included an intravascular cooling device and extracorporeal membrane oxygenation (ECMO).
Outcomes Measures and Statistical Analysis
Results are expressed as n (%) for categorical variables. Descriptive statistics were reported as mean and standard deviation for continuous variables. The groups were compared using Pearson's chi-squared test for categorical data and Student's t-test for numerical data. We compared the survival, the GCS score, and the Glasgow–Pittsburgh cerebral performance category (CPC) scale score between the BCPR group and the no-BCPR group while transferring out of ICU and again during hospital discharge. A comparison of mortality rates between BCPR and no-BCPR patients was also analyzed in a different subgroup. The multivariate logistic regression model was used to explore independent risk factors for in-hospital mortality. Odds ratio (OR) and 95% confidence interval (CI) were identified for each risk factor. Important significant risk factors were identified using the stepwise logistic regression model. All data were processed using SAS software (version 9.4; SAS Institute Inc., Cary, NC). A P < 0.05 was considered statistically significant.
Results
Study Population
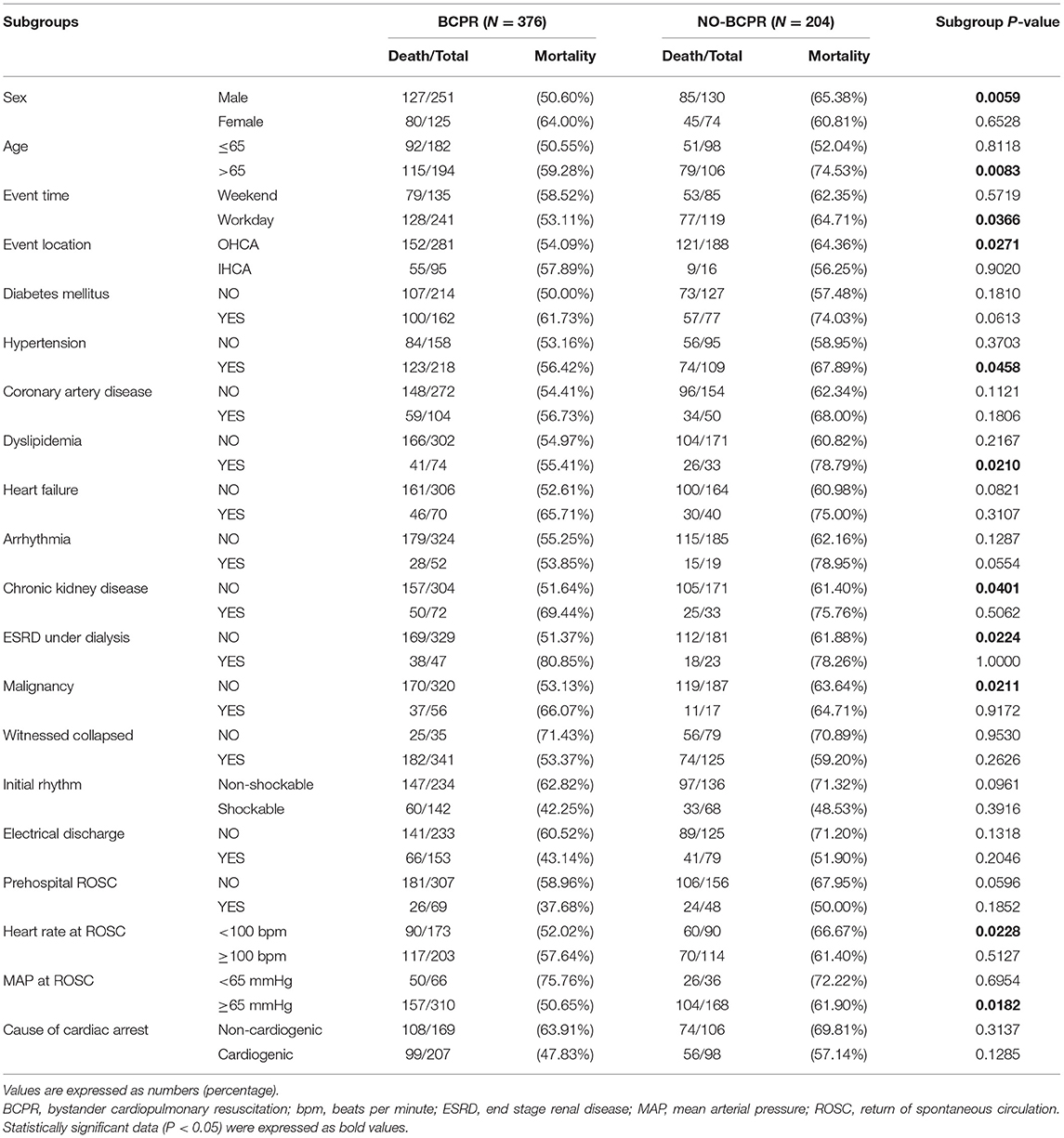
A total of 580 patients were enrolled in this study, of which 376 were in the BCPR group, and the remaining 204 were in the no-BCPR group. The basic characteristics of cardiac arrest patients who received TTM in the BCPR and no-BCPR groups are listed in Table 1. The mean age was 62.1 in the BCPR group and 67.3 in the no-BCPR group (Table 1).
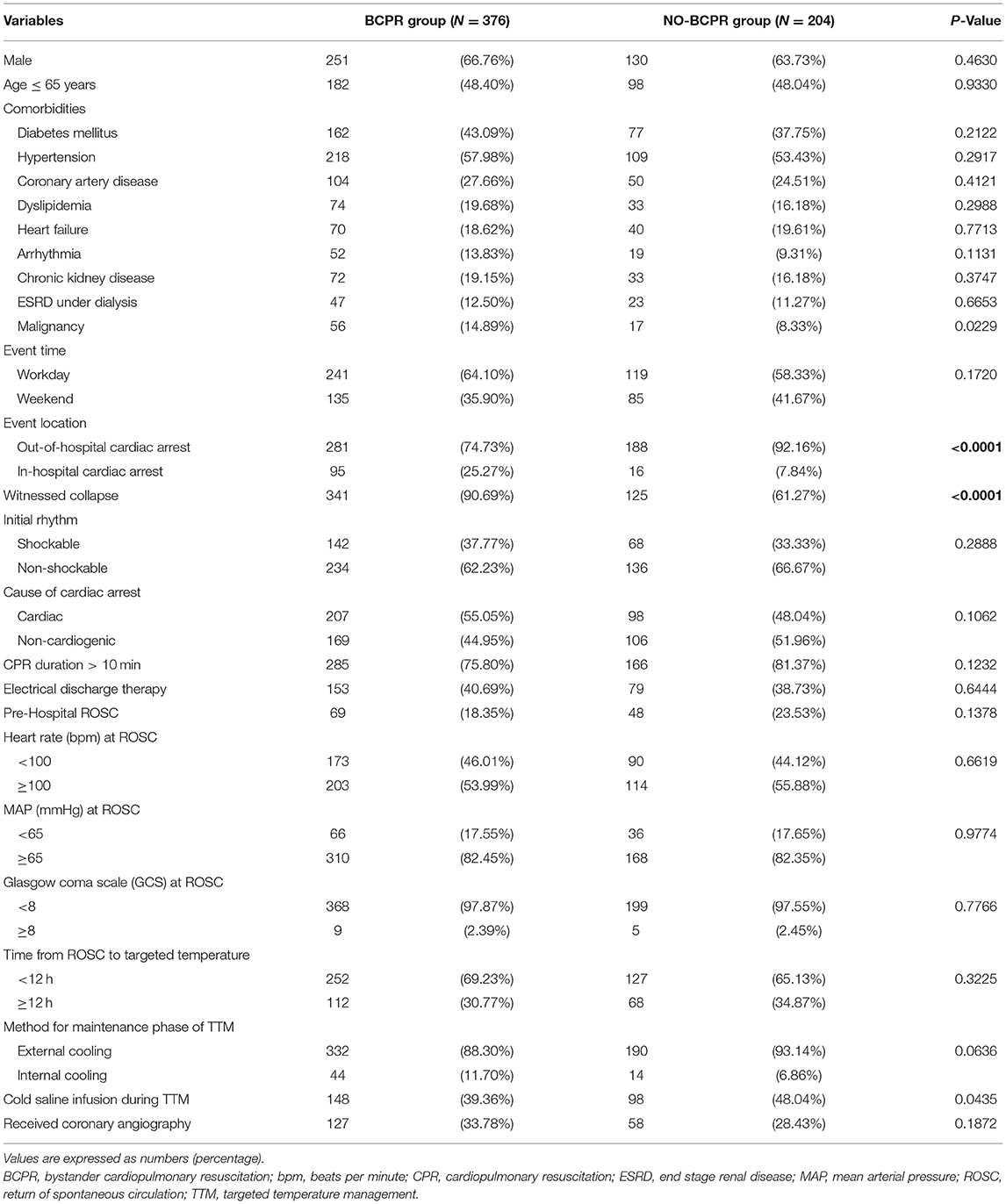
Table 1. Basic characteristics for cardiac arrest patients receiving TTM between BCPR group and NO-BCPR group.
Effect of BCPR on Survival and Neurological Outcomes in ROSC Patients Post-TTM
A survival benefit was found in the BCPR group. Compared to those in the no-BCPR group, BCPR patients who received TTM after ROSC had a higher survival rate at hospital discharge (42.25 vs. 31.86%, P = 0.0305, Table 2). However, there was no significant difference in the survival rate of patients in the BCPR and no-BCPR groups (52.66 vs. 49.51%, P = 0.4686, Table 2) while transferring out of ICU.
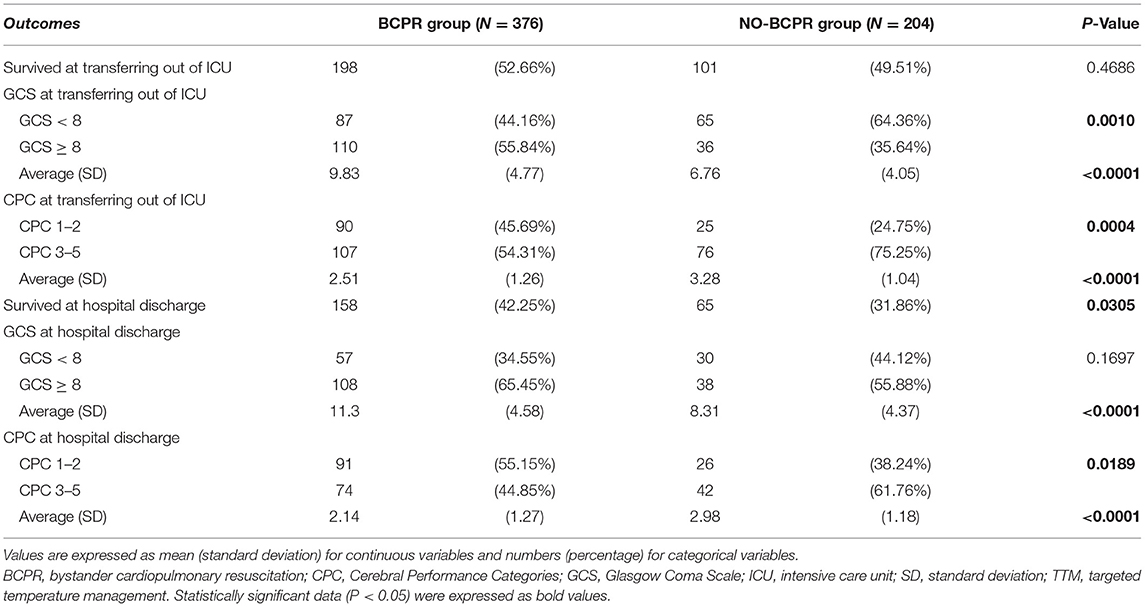
Table 2. Survival and neurological outcomes for cardiac arrest patients receiving TTM between BCPR group and NO-BCPR group.
The BCPR group also had a better neurological outcome while transferring out of ICU. The BCPR group had more patients with GCS ≥8 than the no-BCPR group (55.84 vs. 35.64%, P = 0.0010, Table 2). Their average GCS score was higher (9.83 vs. 6.76, P < 0.0001, Table 2), and more patients in BCPR group were scored 1–2 on the CPC scale (45.69 vs. 24.75%, P = 0.0004, Table 2). The average CPC scale was also lower in the BCPR group (2.51 vs. 3.28, P < 0.0001, Table 2).
The data collected at hospital discharge also showed neurological benefits in patients in the BCPR group. The group had a higher average GCS score (11.3 vs. 8.31, P < 0.0001, Table 2) and a lower average CPC scale score (2.14 vs. 2.98, P < 0.0001, Table 2).
Effect of BCPR on Survival in Different Subgroups in ROSC Patients Post-TTM
The effect of BCPR on post-TTM survival in various subgroups is presented in Table 3. Compared to the patients in the no-BCPR group, the BCPR group had a lower mortality rate in male patients (50.60 vs. 65.38%, P = 0.0059), patients aged >65 (59.28 vs. 74.53%, P = 0.0083), patients with cardiac arrest on workday (53.11 vs. 64.71%, P = 0.0366), and patients with OHCA (54.09 vs. 64.36%, P = 0.0271). While studying BCPR patients with co-morbidities, a survival benefit was also found among patients with hypertension (56.42 vs. 67.89%, P = 0.0458), patients with dyslipidemia (55.41 vs. 78.79%, P = 0.0210), patients without chronic kidney disease (CKD) (51.64 vs. 61.40%, P = 0.0401), patients without end-stage renal disease (ESRD) under dialysis (51.37 vs. 61.88%, P = 0.0224), and patients without malignancy (53.13 vs. 63.64%, P = 0.0211). Two resuscitation-related parameters, heart rate <100 bpm at ROSC (52.02 vs. 66.67%, P = 0.0228) and mean arterial pressure (MAP) ≥65 mmHg at ROSC (50.65 vs. 61.90%, P = 0.0182), were associated with a lower mortality rate in the BCPR group.
Independent Risk Factors of In-Hospital Mortality in Patients With Cardiac Arrest Receiving TTM
We performed a multivariate logistic regression analysis to explore independent risk factors for in-hospital mortality. The adjusted odds ratio and 95% confidence interval of each risk factor are shown in Table 4. Bystander CPR was a significant positive predictor, with an adjusted odds ratio (OR) of 0.66 (95% CI: 0.45–0.97, P = 0.0363, Table 4) for in-hospital mortality. On the other hand, the unadjusted odds ratio of bystander CPR was 0.697 (95% CI 0.49–0.99, P = 0.0436).
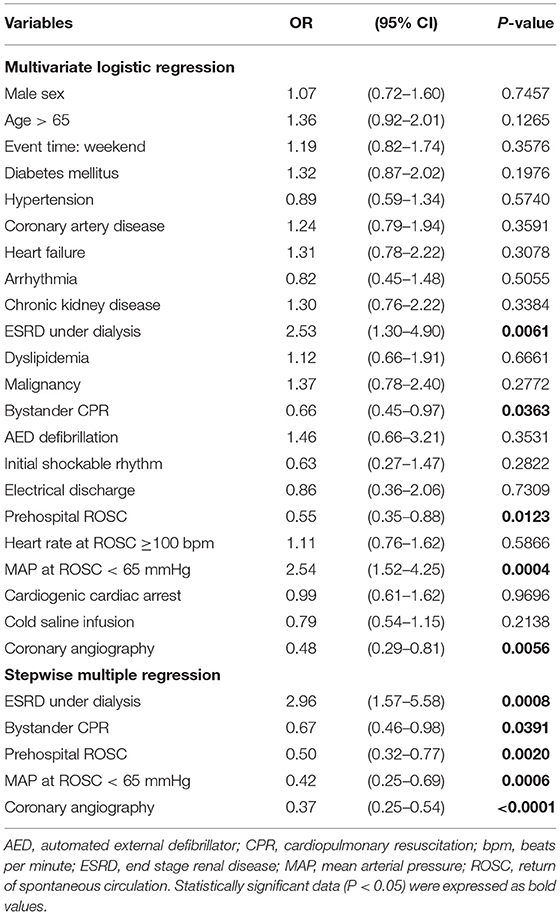
Table 4. Independent risk factors of in-hospital mortality in cardiac arrest patients receiving TTM.
In addition to bystander CPR, prehospital ROSC (OR = 0.55, 95% CI: 0.35–0.88, P = 0.0123, Table 4) and coronary angiography (OR = 0.48, 95% CI: 0.29–0.81, P = 0.0056, Table 4) were significant positive predictors in multivariate logistic regression model. On the contrary, ESRD under dialysis (OR = 2.53, 95% CI: 1.30–4.90, P = 0.0061, Table 4) and mean arterial pressure at ROSC <65 mmHg (OR = 2.54, 95% CI: 1.52–4.25, P = 0.00004, Table 4) were significant negative predictors. Stepwise logistic regression for important factors was also analyzed. The odds ratio for each important factor is demonstrated in Table 4.
Discussion
BCPR Improved Survival in Patients Post-TTM
This study aimed to investigate the outcome differences between BCPR and no-BCPR patients receiving TTM after cardiac arrest. Among patients who received TTM, BCPR was associated with a higher survival rate until hospital discharge than those who did not receive BCPR (42.25 vs. 31.86%, P = 0.0305, Table 2). The positive effects of BCPR on OHCA patients have been extensively investigated. According to a meta-analysis of 16 cohort studies, BCPR was associated with an ~2-fold chance of survival of patients with OHCA compared to patients who received no-BCPR (OR = 1.95; 95% CI: 1.66–2.30) (6). Notably, our study proved the survival benefit of BCPR in patients with cardiac arrest, specifically in those receiving TTM. During cardiac arrest, the cerebral blood flow is extremely low (9). If patients with cardiac arrest received BCPR, they could have better cerebral blood flow, which consequently contributes to improved survival outcomes after TTM.
The positive survival impact of BCPR was significant among older patients (aged > 65 years) undergoing TTM (59.28 vs. 74.53%, P = 0.0083, Table 3). In a previous study, BCPR had a higher OR for 1-month survival in patients aged >71 years (OR = 5.1, 95% CI: 3.8–7.1) than in those aged ≤71 years (OR = 2.5, 95% CI: 1.9–3.3) (10). In terms of their response to TTM, a previous study showed that TTM was significantly associated with good neurologic outcomes in patients aged <65 years but had no association with outcomes in older patients (65–74 years: OR 1.49, 95% CI: 0.90–2.47; >75 years: OR 1.44, 95% CI: 0.79–2.34) (11). Although older patients may not benefit much from TTM, they can have better survival outcomes after receiving BCPR.
Our study showed that patients who received BCPR had a better chance of survival in post-TTM care when they did not have CKD (51.64 vs. 61.40%, P = 0.0401, Table 3), ESRD on dialysis (51.37 vs. 61.88%, P = 0.0224, Table 3), and malignancy (53.13 vs. 63.64%, P = 0.0211, Table 3). A previous study also suggested that BCPR had a stronger survival impact on patients with less severe comorbidities (12). One possible explanation is that additional comorbidities may hasten the electrical, hemodynamic, and metabolic decline in patients with cardiac arrest, making BCPR less effective in rescuing a patient (13).
Our findings showed that BCPR improved survival in patients with OHCA (54.09 vs. 64.36%, P = 0.0271, Table 3) but did not show a survival benefit in patients with IHCA. In patients who did not receive BCPR, the interval time between OHCA and EMS arrival was longer than the interval time between IHCA and CPR provided by the healthcare team. BCPR could significantly reduce the time from arrest to first CPR in patients with OHCA but not in patients with IHCA. This could be a possible reason why BCPR has different effects on survival between patients with OHCA and IHCA.
BCPR Preserved Pre-arrest Neurological Status in Patients Post-TTM
The result of our study demonstrated that BCPR was associated with better neurological outcomes. Similar results were reported in a previous study. According to a meta-analysis in 2018, favorable neurological outcomes were associated with a significantly higher odds ratio of BCPR (OR, 1.44; 95% CI: 1.14–1.82) in patients treated with TTM after cardiac arrest (14). Given that immediate CPR provides crucial blood flow to the brain and shortens ischemia time, BCPR has a positive impact on neurological outcomes in cardiac arrest patients treated with TTM. Therefore, community interventions to encourage BCPR should be undertaken to improve the functional outcomes of patients with cardiac arrest.
Other Independent Risk Factors of In-Hospital Mortality in Patients Post-TTM
Preexisting comorbidities in patients with cardiac arrest influenced their survival after TTM therapy. When adjusted for other variables, ESRD under dialysis (OR = 2.53, 95% CI: 1.30–4.90, Table 4) was an independent negative predictive factor for survival. Hirlekar et al. also demonstrated that renal disease (OR = 0.53, 95% CI: 0.53–0.72) reduced the chance of 30-d survival of patients with OHCA (15).
Pre-hospital ROSC (OR = 0.55, 95% CI: 0.35–0.88, Table 4) was also an independent prognostic factor for survival in our study. Since chest compressions only generate 25–30% of the normal cardiac output (16), prolonged CPR increases cerebral damage (17). Therefore, a pre-hospital ROSC could result in good survival among TTM recipients by reducing the levels of brain damage prior to TTM.
Coronary angiography (OR = 0.48, 95% CI: 0.29–0.81, Table 4) had a positive effect on in-hospital survival in BCPR patients. Acute coronary syndrome is a major cause of OHCAs, requiring emergency coronary angiography for immediate diagnosis and treatment. Although immediate coronary angiography could delay TTM therapy for ~1 h (18), current guidelines recommend immediate coronary angiography and percutaneous coronary intervention in resuscitated OHCA patients whose ECGs show ST-elevation myocardial infarction (19). Given that hemodynamic instability and cardiac dysfunction could worsen during TTM, percutaneous coronary intervention could provide better outcomes in TTM recipients by allowing revascularization of the coronary artery and supporting the hemodynamic status during post-resuscitation care (4).
Mean arterial pressure at ROSC <65 mmHg was an independent negative predictor of in-hospital mortality in patients post-TTM. A previous retrospective cohort study also found that post-ROSC hypotension was an independent predictor of survival among patients who had ROSC after OHCA (20).
Study Limitations
Our study is subject to certain limitations. First, this was a retrospective, non-randomized study. Potential selection bias may exist due to differences in basic patient characteristics between the control and experimental groups. However, selection bias was limited by the large sample size in this study. Second, our analyses were based on observational data. Therefore, although our study showed correlations between BCPR, survival, and neurological outcomes, we could not prove causality. Third, TTM duration, targeted temperature, and cooling methods differed between hospitals due to their differing protocols. This may be an unknown bias that influences the overall survival and neurological outcomes.
Study Strengths
This is the first nationwide multicenter registry project to compare survival and neurological outcomes between cardiac patients under TTM care who had received BCPR with those who did not receive BCPR. A significant positive survival impact of BCPR was found in multiple subsets in the subgroup analysis. This study also identified independent risk and protective factors and their odds ratio for in-hospital mortality among patients who received TTM. Since this study proved that BCPR increases the neuroprotective effects of TTM, the public should be encouraged to offer more BCPR, which will improve post-TTM outcomes in cardiac patients.
Conclusions
This study demonstrated that BCPR had a positive survival and neurological outcome on the return of spontaneous circulation in patients post-TTM.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board (IRB) of the Kaohsiung Veterans General Hospital approved this study (No. VGHKS18-EM3-02). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
W-CH: conception, study design, and critical revision of the manuscript. M-ST, L-KK, H-HH, C-HL, and K-CL: data acquisition, analysis, and interpretation, F-YL: drafting of the manuscript. All authors have read and approved the final manuscript.
Funding
This study was supported by grants from the Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan (VGHKS19-EM12-01).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Mr. Chiu Yong Chih for his expert statistical assistance.
References
1. Kirkegaard H, Taccone FS, Skrifvars M, Søreide E. Postresuscitation care after out-of-hospital cardiac arrest: clinical update and focus on targeted temperature management. Anesthesiology. (2019) 131:186–208. doi: 10.1097/ALN.0000000000002700
2. Chiu WT, Lin KC, Tsai MS, Hsu CH, Wang CH, Kuo LK, et al. Post-cardiac arrest care and targeted temperature management: a consensus of scientific statement from the Taiwan society of emergency & critical care medicine, Taiwan society of critical care medicine and Taiwan society of emergency medicine. J Formos Med Assoc. (2021) 120 (1 Pt. 3):569–87. doi: 10.1016/j.jfma.2020.07.036
3. Dumas F, Grimaldi D, Zuber B, Fichet J, Charpentier J, Pe ne F, et al. Is hypothermia after cardiac arrest effective in both shockable and nonshockable patients?: insights from a large registry. Circulation. (2011) 123:877–86. doi: 10.1161/CIRCULATIONAHA.110.987347
4. Kim JG, Shin H, Choi HY, Kim W, Kim J, Moon S, et al. Prognostic factors for neurological outcomes in Korean targeted temperature management recipients with return of spontaneous circulation after out-of-hospital cardiac arrests: a nationwide observational study. Medicine. (2020) 99:e19581. doi: 10.1097/MD.0000000000019581
5. Mader TJ, Westafer LM, Nathanson BH, Villarroel N, Coute RA, McNally BF. Targeted temperature management effectiveness in the elderly: insights from a large registry. Ther Hypothermia Temp Manag. (2017) 7:222–30. doi: 10.1089/ther.2017.0015
6. Song J, Guo W, Lu X, Kang X, Song Y, Gong D. The effect of bystander cardiopulmonary resuscitation on the survival of out-of-hospital cardiac arrests: a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med. (2018) 26:86. doi: 10.1186/s13049-018-0552-8
7. Chang HC, Tsai MS, Kuo LK, Hsu HH, Huang WC, Lai CH, et al. Factors affecting outcomes in patients with cardiac arrest who receive target temperature management: the multi-center TIMECARD registry. J Formos Med Assoc. (2021) 121 (1 Pt. 2):294–303. doi: 10.1016/j.jfma.2021.04.006
8. Chamberlain D, Cummins RO. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the 'Utstein style'. European resuscitation council, American heart association, heart and stroke foundation of Canada and Australian resuscitation council. Eur J Anaesthesiol. (1992) 9:245–56.
9. Hoedemaekers CW, Ainslie PN, Hinssen S, Aries MJ, Bisschops LL, Hofmeijer J, et al. Low cerebral blood flow after cardiac arrest is not associated with anaerobic cerebral metabolism. Resuscitation. (2017) 120:45–50. doi: 10.1016/j.resuscitation.2017.08.218
10. Holmberg M, Holmberg S, Herlitz J. Factors modifying the effect of bystander cardiopulmonary resuscitation on survival in out-of-hospital cardiac arrest patients in Sweden. Eur Heart J. (2001) 22:511–9. doi: 10.1053/euhj.2000.2421
11. Wallmu ller C, Spiel A, Sterz F, Schober A, Hubner P, Stratil P, et al. Age-dependent effect of targeted temperature management on outcome after cardiac arrest. Eur J Clin Invest. (2018) 48:e13026. doi: 10.1111/eci.13026
12. Hirlekar G, Jonsson M, Karlsson T, Ba ck M, Rawshani A, Hollenberg J, et al. Comorbidity and bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest. Heart. (2020) 106:1087–93. doi: 10.1136/heartjnl-2019-315954
13. Carew HT, Zhang W, Rea TD. Chronic health conditions and survival after out-of-hospital ventricular fibrillation cardiac arrest. Heart. (2007) 93:728–31. doi: 10.1136/hrt.2006.103895
14. Zhang Q, Qi Z, Liu B, Li C. Predictors of survival and favorable neurological outcome in patients treated with targeted temperature management after cardiac arrest: a systematic review and meta-analysis. Heart Lung. (2018) 47:602–9. doi: 10.1016/j.hrtlng.2018.07.005
15. Hirlekar G, Jonsson M, Karlsson T, Hollenberg J, Albertsson P, Herlitz J. Comorbidity and survival in out-of-hospital cardiac arrest. Resuscitation. (2018) 133:118–23. doi: 10.1016/j.resuscitation.2018.10.006
16. Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American heart association. Circulation. (2013) 128:417–35. doi: 10.1161/CIR.0b013e31829d8654
17. Matos RI, Watson RS, Nadkarni VM, Huang HH, Berg RA, Meaney PA, et al. Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation. (2013) 127:442–51. doi: 10.1161/CIRCULATIONAHA.112.125625
18. Lemkes JS, Janssens GN, van der Hoeven NW, Jewbali LSD, Dubois EA, Meuwissen M, et al. Coronary Angiography after cardiac arrest without ST-468 segment elevation. N Engl J Med. (2019) 380:1397–407. doi: 10.1056/NEJMoa1816897
19. Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, et al. Part 8: Post-Cardiac Arrest Care: 2015. American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2015) 132 (18 Suppl. 2):S465–82. doi: 10.1161/CIR.0000000000000262
Keywords: cardiac arrest, targeted temperature management, bystander cardiopulmonary resuscitation, witnessed collapse, electrical discharge, coronary intervention
Citation: Liou F-Y, Tsai M-S, Kuo L-K, Hsu H-H, Lai C-H, Lin K-C and Huang W-C (2022) A Study on the Outcome of Targeted Temperature Management Comparing Cardiac Arrest Patients Who Received Bystander Cardiopulmonary Resuscitation With Those Who Did Not, Using the Nationwide TIMECARD Multicenter Registry. Front. Med. 9:779781. doi: 10.3389/fmed.2022.779781
Received: 19 September 2021; Accepted: 07 March 2022;
Published: 13 April 2022.
Edited by:
Björn Tampe, University Medical Center Göttingen, GermanyCopyright © 2022 Liou, Tsai, Kuo, Hsu, Lai, Lin and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei-Chun Huang, d2NodWFuZ2x1bHVAZ21haWwuY29t
 Fang-Yu Liou1,2
Fang-Yu Liou1,2 Min-Shan Tsai
Min-Shan Tsai Hsin-Hui Hsu
Hsin-Hui Hsu Chih-Hung Lai
Chih-Hung Lai Kun-Chang Lin
Kun-Chang Lin Wei-Chun Huang
Wei-Chun Huang