
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 09 February 2022
Sec. Intensive Care Medicine and Anesthesiology
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.717477
This article is part of the Research TopicAcute Respiratory Distress Syndrome and Mechanical VentilationView all 15 articles
Objective: The present study aimed to evaluate the impact of 1.5 mg/kg succinylcholine or 1.2 mg/kg rocuronium, vs. 1.0 mg/kg succinylcholine on apnea duration in patients underwent rapid sequence induction (RSI).
Methods: This prospective cohort study was conducted in the Department of Anesthesiology in Shanghai General Hospital from July 2020 to November 2020. Apnea duration was defined as the time from apnea prompted by the PETCO2 waveform to the time the point of oxygen saturation declined to 90% (T90) and 95% (T95) after succinylcholine or rocuronium administration. The primary outcome included T90 and T95 changes in 1.5 mg/kg vs. 1.0 mg/kg succinylcholine groups and 1.5 mg/kg succinylcholine vs. 1.2 mg/kg rocuronium groups.
Results: A total of 265 participants were subjected for analysis. The succinylcholine (1.0 mg/kg) group had a significantly longer T90 (50.72, 95% confidence interval [CI, 7.60, 94.38], P = 0.015) and T95 (48.09, 95% CI [7.11, 89.07], P = 0.012) than the succinylcholine (1.5 mg/kg) group. In addition, significantly longer T90 (56.84, 95% CI [16.24, 97.44], P = 0.003) and T95 (50.57, 95% CI [12.58, 88.57], P = 0.003) were observed in the rocuronium (1.2 mg/kg) group than those in the succinylcholine (1.5 mg/kg) group. No severe side events were observed during the operation.
Conclusion: Rocuronium and the lower dose of succinylcholine may be recommended to patients underwent RSI.
Rapid sequence induction (RSI) is a special technique of anesthetic induction designed to reduce the risk of aspiration of secretions of any kind, e.g., regurgitated or vomited gastric contents. This is done by shortening the normal sequence of intubation procedures and omitting certain steps to minimize the time between loss of consciousness and swallowing reflexes until the airway is secured by tracheal intubation (1). In particular, RSI involves not using mask ventilation, at least for adults.
Neuromuscular blockade agents (NMBAs) are used to facilitate endotracheal intubation (2). Succinylcholine is a short-acting depolarizing NMBA that is the most commonly conventionally used NMBA in RSI because of its fast onset and short duration (3). Unfortunately, it can have serious side effects (4, 5). Rocuronium, a steroidal non-depolarizing NMBA, is an alternative to succinylcholine due to its fast onset (6, 7). However, the 1.0–1.2 mg/kg dose recommended for RSI has too long a duration of action that fatal hypoxia is imminent if the airway is difficult, especially if intubation and mask ventilation fail simultaneously. This disadvantage of rocuronium is not eliminated by the very rapid reversal with sugammadex (8), because this drug is often not available fast enough in emergency situations (9). Therefore, the selection of succinylcholine or rocuronium in RSI should be carefully considered and tailored to the specifics of each patient and their clinical indications and medical conditions.
Apnea caused from not using mask ventilation, however, includes the risk of hypoxemia. Therefore, “non-hypoxic apnea,” defined as duration of apnea with SpO2 > 90%, is relevant to patient safety (10). Previous studies focused mainly on increasing oxygen storage to prolong non-hypoxic apnea duration (10, 11), whereas few studies have been performed on approaches to decrease oxygen consumption. Two aspects should be considered in the assessment of the optimal dose of succinylcholine and rocuronium in RSI: prolonging the non-hypoxic apnea duration (without additional oxygen consumption) and shortening the apnea interval (fast onset and good intubation conditions). Succinylcholine may lead to increased dose-dependent oxygen consumption (12). Our previous study showed that in obese patients the non-hypoxic apnea duration in the treatment with 1.5 mg/kg succinylcholine was shorter than that in the treatment with 0.9 mg/kg rocuronium (13), we assumed that fasciculation may be a potential cause of the shorter non-hypoxic apnea. However, poor intubation conditions and repeated intubation may also increase oxygen consumption. Succinylcholine is superior to rocuronium in terms of muscle relaxation effects in both good intubation conditions and clinically acceptable intubation conditions at quantities of 2–3 times the ED95 dose (6). Similar onset times and intubation conditions were achieved at doses higher than 3 times the ED95 dose (1.0 mg/kg−1.5 mg/kg succinylcholine and 1.0 mg/kg−1.2 mg/kg rocuronium) (7, 14–16). Therefore, the optimal doses of succinylcholine and rocuronium for application in RSI are still inconclusive.
Therefore, the aim of the present study was to compare the non-hypoxic apnea duration of the administration of 1.5 mg/kg succinylcholine, 1.0 mg/kg succinylcholine, and 1.2 mg/kg rocuronium during RSI.
This prospective cohort study was conducted in the Department of Anesthesiology in Shanghai General Hospital from July 2020 to November 2020. This study was approved by the Ethics Committee of Shanghai General Hospital ([2020]54) and was registered in the Chinese Clinical Trial Registration Center (http://www.chictr.org.cn/index.aspx) with the registration number ChiCTR2000034769. Written informed consent was obtained from all individual participant.
Patients who underwent elective surgery requiring RSI were enrolled. The following inclusion criteria were used: (1) American Society of Anesthesiologists (ASA) physical status I or II and (2) Age between 18 and 65 years. The exclusion criteria were as follows: (1) Unwilling to provide written informed consent; (2) Pregnancy; (3) Patients with a history of difficulty in intubation or failed intubation; (4) Obstructive sleep apnea syndrome; (5) A history of respiratory tract infection within a month; (6) Smoking cessation <2 months before surgery; (7) History of alcohol or drug abuse; (8) Cerebrovascular disease and increased intracranial pressure; (9) Drugs antagonists of rocuronium (such as phenytoin, carbamazepine, or protease inhibitors). In case one of the following conditions was present, the observation was to be suspended and the participant withdrawn from the study: (1) After preoxygenation, the end-tidal oxygen concentration was <90%; (2) Coughing during tracheal intubation; (3) Failed tracheal intubation twice times or more; (4) Recovery from spontaneous breathing before mechanical ventilation; (5) Severe allergic reactions; (6) Patients with circulatory fluctuations that were difficult to correct after 5 min of using vasoactive drugs. The participants were not compensated for their study participation.
General anesthesia drugs and treatment strategies were selected based on clinical needs. The choice of a muscle relaxant was jointly decided by the anesthetist and the participants. As an observational exploratory study, no blindness was applied.
All subjects fasted for more than 8 h before surgery. After entering the operation room, a 20G indwelling vein cannula was placed in the median vein of the left antecubital fossa, and 10 mL/kg of sodium lactate Ringer's solution was infused to substitute for the fasting-induced fluid deficit. Then, 2% local lidocaine anesthesia was administered for the puncture and the placement of the left radial artery. Next, a pressure sensor was connected to the patient to measure the direct arterial pressure and perform blood gas analysis. If the left radial artery puncture and placement failed, the right forearm was used to measure the non-invasive blood pressure with a measurement interval of 1 min. Further, the subjects were connected to a GE CARESCAPE Monitor B650 (GE Healthcare Finland OY, Helsinki, Finland) to monitor the heart rate (HR), mean arterial pressure (MAP), finger pulse oxygen saturation (SpO2), bispectral index (BIS) and nasopharyngeal temperature (Temp). The subject lied in the supine position and was kept warm using a medical insulation blanket. The oxygen flow rate used was 10 L/min; the oxygen concentration reached was 100%. The airway pressure-limiting valve of the anesthesia machine was fully opened, the breathing circuit was pre-filled, and the subject was instructed to breathe calmly under a closed mask for 3 min. Then, an intravenous injection of fentanyl 3 μg/kg and propofol 2 mg/kg was administered. After the eyelash reflex disappeared and the subject ceased respond to the patting call, the muscle relaxant was administered (following the decision previously made by the anesthetist and the participants). Before the spontaneous breathing disappeared, the subject was to fasten the mask to avoid inhaling air; the mandible had to be unsupported before intubation, and any manual or mechanical ventilation was not to be applied. Fifty seconds after the administration of the muscle relaxant, the mask was removed, and a video laryngoscope (UETDC-K3) was utilized to perform a laryngoscopy to expose the glottis. Next, 60 s after the administration of the muscle relaxant, endotracheal intubation was conducted (7.5-mm cuffed tracheal tube for men and 7-mm cuffed tracheal tube for women). The insertion depth of the tracheal tube was 1 cm after the cuff was fully inserted into the glottis. After the tracheal intubation, a fiberoptic bronchoscope (UESCOPETIC-I1) was used to check whether the tracheal tube position is correct. The tracheal tube was opened in the air, without mechanical ventilation, and the end-expiratory carbon dioxide output was observed to monitor the recovery of spontaneous breathing. After tracheal intubation, to prevent the recovery of spontaneous breathing, intravenous bolus of rocuronium (0.6 mg/kg) was given to maintain muscle relaxation in the succinylcholine (1.5 mg/kg) and succinylcholine bromide (1.0 mg/kg) groups. To prevent consciousness restoration during anesthesia, propofol was intravenously injected at a rate of 5 mg /kg/h (Willi's Ark CONCERT-III infusion pump). In case BIS was >60, intravenous injection of 20 mg of propofol was applied. When SpO2 dropped to 90%, the tracheal tube was immediately connected to the anesthesia machine (GE Carestation 620) for mechanically controlled mechanical ventilation (parameter settings: oxygen concentration 100%, oxygen flow 1 L/min, tidal volume 8 mL/kg, frequency 16 beats/min, inhale-to-exhale ratio 1:2).
During the anesthesia, the hemodynamic parameters were monitored in real time. If HR > 110 beats/min, intravenous bolus of 1 mg of esmolol was administrated; if HR <50 beats/min, an intravenous bolus injection of atropine 0.5 mg was given. If SBP > 170 mmHg, intravenous bolus injection of 1 mg perdipine was administered, and if SBP <80 mmHg or MAP dropped more than 25% of the baseline value, 50 μg oxypinephrine was applied as an intravenous bolus injection.
The primary outcome was the non-hypoxic apnea duration. That is, the time interval between PETCO2 waveform area prompts apnea to oxygen saturation declined to 95% (T95) and 90% (T90) of 1.5 mg/kg succinylcholine vs. 1.0 mg/kg succinylcholine groups, and 1.5 mg/kg succinylcholine vs. 1.2 mg/kg rocuronium groups.
Prespecified secondary outcomes included the T95 and T90 of the 1.0 mg/kg succinylcholine and 1.2 mg/kg rocuronium groups and adverse events. The exploratory outcomes included the exploration of factors that correlated with T90, and the variation of blood gas analysis, BIS, temperature, HR, MAP, SpO2, ETO2, and PETCO2.
Any adverse reactions, such as laryngospasm, bronchospasm, and masseter spasm, or muscle rigidity during intubation, were recorded during the surgery operation. Any adverse events found were followed up before improvement or discharge.
The data collected included gender, age, ASA classification, preoperative hemoglobin (Hb), hematocrit (Hct), weight, height, body-mass index (BMI, kg/m2), smoking history, Mallampati score, T95, T90, duration of muscle fibrillation (TF, the time from the onset of muscle fibrillation to the disappearance of muscle fibrillation after intravenous injection of muscle relaxants), classification of the degree of muscle fibrillation, and the conditions of tracheal intubation. In addition, the laryngoscope exposure classification, number of intubation attempts, HR, MAP, SpO2, Temp, BIS, ETO2, as well as for at room entry, 3 min after oxygen inhalation, 30 s after muscle relaxant administration, 50 s after muscle relaxant administration, 2 min after intubation, SpO2 reduction to 95%, SpO2 decrease to 90%, SpO2 increase to 96%. Moreover, blood gas analysis was performed of pH, pO2, pCO2, cLac at room entry, 3 min after oxygen inhalation, and SpO2 decrease to 90%.
Muscle fibrillation was classified using the scale scores described in a previous report (17): 0 = No muscle tremor; 1 = Mild: slight muscle tremor in eyes, neck, face, or fingers, no limb movement; 2 = Moderate: moderate muscle tremor or obvious limb movement on both sides; 3 = Severe: severe or continuous and extensive muscle fibrillation. Endotracheal intubation condition was evaluated by Copenhagen score (18): 1 = excellent; 2 = good, and 3 = poor. Laryngoscope exposure classification (Cormack-Lehane classification) was defined as follows: 1 = the glottis was mostly visible; 2 = only the posterior union of the glottis could be seen, but not the glottis; 3 = only the epiglottis was visible; 4 = no glottal epiglottis could be seen. We used the World Health Organization classification for BMI: <18.5 (underweight), 18.5–24.9 (normal range), 25–29.9 (overweight), and >30 (obesity).
Preliminary analysis revealed that T90 in the succinylcholine (1.5 mg/kg), succinylcholine (1.0 mg/kg), and rocuronium (1.2 mg/kg) groups was 475.9 ± 64.7, 534.7 ± 64.7, and 528.7 ± 52.5, respectively. Therefore, an estimated sample size of 91 patients per group could provide 80% power to detect a between-group difference, assuming a two-sided significance level of 2.5%. Considering a loss of follow-up of 10%, a number of 101 subjects per group are required.
Continuous variables that follow normal distribution was expressed with mean ± Standard deviation (SD), otherwise presented as median and interquartile range (IQR). Categorical variables were displayed using number and percentages. For multiple demographic characteristics comparison, nonparametric test was applied for continuous variables that not conformed to normal distribution. The comparison between the 1.5 mg/kg succinylcholine vs. 1.0 mg/kg succinylcholine and 1.5 mg/kg succinylcholine vs. 1.2 mg/kg rocuronium groups were analyzed using student t test. Two-way repeated measurement ANOVA was used to detect the effects of treatment and time interaction on HR and MAP. In addition, categorical variable comparison was conducted using Chi-square or Fisher exact tests. Pearson correlation analysis was employed to assess the correlation between T90 and the interested variables. All data were analyzed using SPSS 22.0 (IBM Corp., Armonk, NY, USA). P < 0.05 was considered statistically significant.
Not applicable.
A total of 471 patients were assessed for eligibility, of which 162 failed to meet the inclusion criteria, and 6 refused to participate. Of the enrolled 303 patients, 38 were excluded because of incomplete data for T90 and T95. Therefore, a total number of 265 subjects were analyzed: 90 cases in the 1.5 mg/kg succinylcholine, 83 in the 1.0 mg/kg succinylcholine, and 92 in the 1.2 mg/kg rocuronium groups (Figure 1). The demographic data are presented in Table 1.
T90 in the 1.2 mg/kg rocuronium group was significantly longer (56.84 [95% CI 16.24–97.44], P = 0.003) than that in the 1.5 mg/kg succinylcholine group. Additionally, T90 in the 1.0 mg/kg succinylcholine group was statistically significantly longer (50.72 [95% CI 7.06–94.38], P = 0.015) than that in the 1.5 mg/kg succinylcholine group. Compared with the 1.5 mg/kg succinylcholine group, the 1.2 mg/kg rocuronium group had a significant longer T95 (50.57 [95% CI 12.58–88.57], P = 0.003). When compared with the succinylcholine (1.5 mg/kg) group, the succinylcholine (1.0 mg/kg) exhibited a significant longer T90 (48.09 [95% CI 7.11–89.07], P = 0.012).
For secondary outcome comparison, the T90 (6.12 [95% CI −34.58–46.82], P = 0.48) and T95 (2.48 [95% CI 35.74–40.70], P = 0.54) values were comparable between the 1.0 mg/kg succinylcholine and 1.2 mg/kg rocuronium groups (Table 2). No severe adverse events were observed during the surgery and during follow-up in all groups. A total number of 23, 13, and 19 mild adverse reactions occurred in the 1.5 mg/kg succinylcholine, 1.2 mg/kg rocuronium, and 1.0 mg/kg succinylcholine groups, respectively. Among them, sore throat and myalgia were the most common side effects (Table 3).
One incubation attempt was successfully performed in all patients. Tracheal intubation evaluation revealed that the incubation conditions, C-L classification, and incubation number were comparable among the groups. The time for muscle fibrillation was comparable between the 1.5 mg/kg and 1.0 mg/kg succinylcholine groups (P = 0.73) (Supplementary Table 1). The degrees of muscle fibrillation in these two groups were also similar (P = 0.11) (Supplementary Table 2).
Moreover, the variation ratio of MAP and HR were within 30% at each time point (Figures 2A,B). In addition, the BIS variation among the three groups showed no clinical significance (Supplementary Table 3). The temperature during RSI was relatively stable, ranging from 36.0 °C to 37.1 °C.
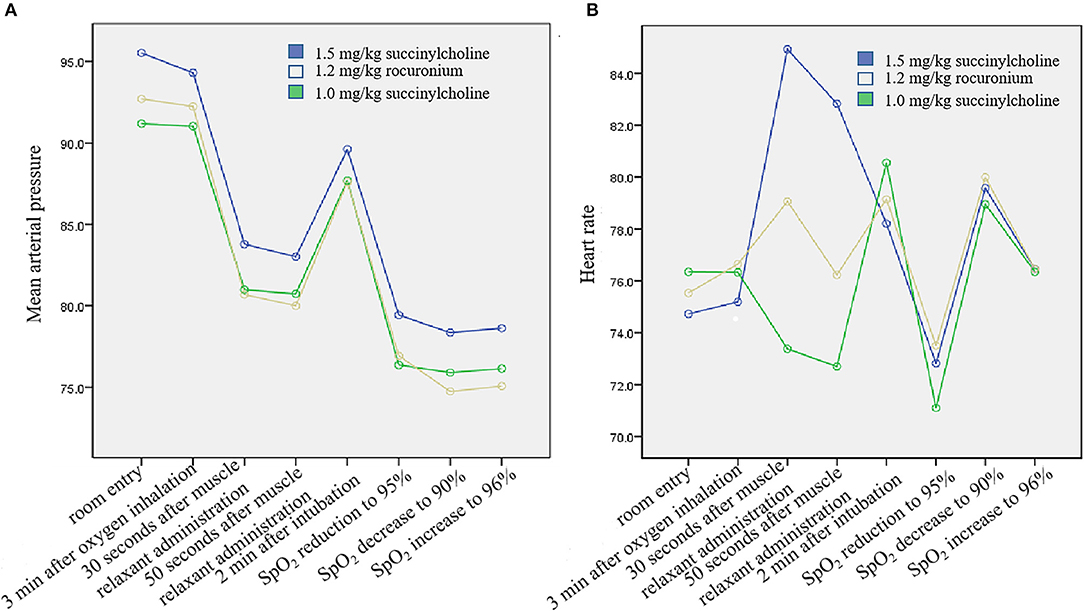
Figure 2. Mean arterial pressure and heart rate variation. (A) Mean arterial pressure. Two-way repeated measurement ANOVA suggested that time and treatment interaction was comparable (P = 0.279). (B) Heart rate. Two-way repeated measurement ANOVA suggested that time and treatment interaction showed statistical significance among the groups (P < 0.001), though no clinical significance was observed.
Blood gas analysis showed a significantly different pH between room entry and 3 min after oxygen inhalation (P < 0.01) among the groups, despite no clinical significance. pO2 at 3 min after oxygen inhalation time point was highest in the 1.0 mg/kg succinylcholine group (P = 0.005). The pCO2 and cLac values significantly differed among the groups at room entry, 3 min after oxygen inhalation, and SpO2 decrease to 90% time points (all P < 0.01) (Table 4). The SpO2 in room entry and the minimum SpO2 time points were comparable among the groups (all P > 0.05). In addition, ETO2 was comparable among the groups, and PETCO2 at 3 min after oxygen inhalation (P = 0.013) and SpO2 increase to 96% time points (P = 0.002) were significantly differed (Supplementary Table 4).
Correlation analysis was used to explore the potential factors that might affect T90. As depicted in Supplementary Table 5, BMI, age, and hemoglobin were significantly correlated with T90 (all P < 0.001). Gender, smoking, muscle fibrillation time period, and muscle fibrillation degree were not correlated with T90.
In the present study, compared with 1.5 mg/kg succinylcholine group, both 1.0 mg/kg succinylcholine and 1.2 mg/kg rocuronium groups had significantly longer T90 and T95. These findings may provide evidence that lower dose succinylcholine and 1.2 mg/kg rocuronium may be feasible in clinical practice.
RSI is a critical medical measure that facilitates intubation. The selection of neuromuscular relaxants has been extensively studied, but there is no consensus. One of the highest risks of RSI comes from hypoxemia and reducing hypoxemia risk should be considered in the choice of muscle relaxants. Nevertheless, the available evidence on non-hypoxic apnea duration is limited. A meta-analysis showed that succinylcholine was superior to rocuronium in achieving excellent clinically acceptable intubation conditions (6). However, no statistical difference in the intubation conditions achieved was found between rocuronium and succinylcholine (19). In terms of non-hypoxic apnea duration, it was suggested that 1.0 mg/kg succinylcholine and 1.2 mg/kg rocuronium were superior to 1.5 mg/ kg succinylcholine in T90 and T95. These findings suggested that the administration of 1.0 mg/kg succinylcholine may be safer than higher doses. We noted that apneic oxygenation during the apnea period in RSI did not prevent desaturation as compared with conventional care measures in cardiac or traumatic arrest patients (20).
In the present study, the T95 and T90 in the 1.0 mg/kg succinylcholine and 1.2 mg/kg rocuronium groups were significantly longer than that in the 1.5 mg/kg succinylcholine group. In a previous study, Taha et al. reported that the T95 value in 1.5 mg/kg rocuronium-treated patients was 378 (370–393), which was lower than that in the present study. This discrepancy may be attributed to the differences in the fentanyl dose, start time points, and sample sizes (21). Our previous study compared the time of oxygen saturation decline to 92% (T92) in 0.9 mg/kg rocuronium- and 1.5 mg/kg succinylcholine-treated obese patients, in which rocuronium showed a significantly longer T92 (13), which in agreement with the present study.
Succinylcholine can trigger muscle fibrillation and increase muscle fibrillation-related metabolism. In this study, the degree and duration in the 1.5 mg/kg succinylcholine and 1.0 mg/kg succinylcholine groups were comparable, which may be explained with the supply of oxygen by myoglobin, which minimized its effect on systemic oxygen reservation (22). Moreover, the heart rate was significantly accelerated in the 1.5 mg/kg succinylcholine group, whereas mild effect was observed in the 1.0 mg/kg succinylcholine and 1.2 mg/kg rocuronium groups. Previous study suggested that succinylcholine increased anaerobic metabolism and disturbed the tissue oxygen supply and demand balance, and that high-dose succinylcholine elevated the risk of hemoglobin desaturation (12). In animal experiments, continuous infusion of succinylcholine augmented oxygen consumption (23). These previous results together with our findings suggest that a high dose of succinylcholine during RSI may need to be avoided.
This study is not without limitations. Although there were no significant differences in the intubation conditions, due to the observational nature of the study, we could not conclude whether they showed comparable effects. Additionally, elder adults and obese patients, as well as such with lung-related diseases were not included, which limited the representativeness of the conclusion. We noted that gender and height significantly differed among the three groups, and whether these two parameters affect oxygenation desaturation needs further investigation. Moreover, patients failed to complete RSI, coughing during intubation, or spontaneous breathing before mechanical ventilation were excluded for analysis, which may introduce selection bias, so the interpretation of results should be cautious.
In conclusion, this study revealed that a relatively low dose of succinylcholine and rocuronium led to a longer non-hypoxic apnea duration. Therefore, 1.0 mg/kg succinylcholine or 1.2 mg/kg rocuronium may be recommended for RSI to satisfy the required intubation conditions. Further large-scale randomized control studies are needed to validate these findings.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Shanghai General Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
LT and XZ conceived and coordinated the study, designed, performed and analyzed the experiments, and wrote the paper. SL, LH, JL, LC, and SH carried out the data collection, data analysis, and revised the paper. All authors reviewed the results and approved the final version of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.717477/full#supplementary-material
1. H.J. Morton, and W.D. Wylie. Anaesthetic deaths due to regurgitation or vomiting. Anaesthesia. (1951) 6:190–201. doi: 10.1111/j.1365-2044.1951.tb01388.x
2. Gray TC, Halton JA. Milestone in Anaesthesia?: (d-Tubocurarine Chloride). Proc R Soc Med. (1946) 39:400–10. doi: 10.1177/003591574603900716
3. Foldes FF, McNall PG, Borrego-Hinojosa JM. Succinylcholine: a new approach to muscular relaxation in anesthesiology. N Engl J Med. (1952) 247:596–600. doi: 10.1056/NEJM195210162471603
4. G.A. Gronert. A possible mechanism of succinylcholine-induced hyperkalemia. Anesthesiology. (1980) 53:356. doi: 10.1097/00000542-198010000-00027
5. J.M. Hunter. Adverse effects of neuromuscular blocking drugs. Br J Anaesth. (1987) 59:46–60. doi: 10.1093/bja/59.1.46
6. Tran DTT, Newton EK, Mount VAH, Lee JS, Mansour C, Wells GA. et al. Rocuronium vs succinylcholine for rapid sequence intubation: a Cochrane systematic review. Anaesthesia. (2017) 72:765–77. doi: 10.1111/anae.13903
7. Guihard B, Chollet-Xémard C, Lakhnati P, Vivien B, Broche C, Savary D. et al. Effect of Rocuronium vs Succinylcholine on Endotracheal Intubation Success Rate Among Patients Undergoing Out-of-Hospital Rapid Sequence Intubation: A Randomized Clinical Trial. JAMA. (2019) 322:2303–12. doi: 10.1001/jama.2019.18254
8. Lee C, Jahr JS, Candiotti KA, Warriner B, Zornow MH, Naguib M. Reversal of profound neuromuscular block by sugammadex administered three minutes after rocuronium: a comparison with spontaneous recovery from succinylcholine. Anesthesiology. (2009) 110:1020–5. doi: 10.1097/ALN.0b013e31819dabb0
9. Bisschops MM, Holleman C, Huitink JM. Can sugammadex save a patient in a simulated 'cannot intubate, cannot ventilate' situation? Anaesthesia. (2010) 65:936–41. doi: 10.1111/j.1365-2044.2010.06455.x
10. Herriger A, Frascarolo P, Spahn DR, Magnusson L. The effect of positive airway pressure during pre-oxygenation and induction of anaesthesia upon duration of non-hypoxic apnoea. Anaesthesia. (2004) 59:243–7. doi: 10.1111/j.1365-2044.2004.03615.x
11. Dixon BJ, Dixon JB, Carden JR, Burn AJ, Schachter LM, Playfair JM, et al. Preoxygenation is more effective in the 25 degrees head-up position than in the supine position in severely obese patients: a randomized controlled study. Anesthesiology. (2005) 102:1110–5. doi: 10.1097/00000542-200506000-00009
12. Naguib M, Samarkandi AH, Abdullah K, Riad W, Alharby SW. Succinylcholine dosage and apnea-induced hemoglobin desaturation in patients. Anesthesiology. (2005) 102:35–40. doi: 10.1097/00000542-200501000-00009
13. Tang L, Li S, Huang S, Ma H, Wang Z. Desaturation following rapid sequence induction using succinylcholine vs. rocuronium in overweight patients. Acta anaesthesiologica Scandinavica. (2011) 55:203–8. doi: 10.1111/j.1399-6576.2010.02365.x
14. Stourac P, Adamus M, Seidlova D, Pavlik T, Janku P, Krikava I, et al. Low-dose or high-dose rocuronium reversed with neostigmine or sugammadex for cesarean delivery anesthesia: a randomized controlled noninferiority trial of time to tracheal intubation and extubation. Anesth Analg. (2016) 122:1536–45. doi: 10.1213/ANE.0000000000001197
15. Andrews JI, Kumar N, van den Brom RH, Olkkola KT, Roest GJ, Wright PM. A large simple randomized trial of rocuronium vs. succinylcholine in rapid-sequence induction of anaesthesia along with propofol. Acta anaesthesiologica Scandinavica. (1999) 43:4–8. doi: 10.1034/j.1399-6576.1999.430102.x
16. Sluga M, Ummenhofer W, Studer W, Siegemund M, Marsch SC. Rocuronium vs. succinylcholine for rapid sequence induction of anesthesia and endotracheal intubation: a prospective, randomized trial in emergent cases. Anesth Analg. (2005) 101:1356–61. doi: 10.1213/01.ANE.0000180196.58567.FE
17. Kararmaz A, Kaya S, Turhanoglu S, Ozyilmaz MA. Effects of high-dose propofol on succinylcholine-induced fasciculations and myalgia. Acta anaesthesiologica Scandinavica. (2003) 47:180–4. doi: 10.1034/j.1399-6576.2003.00052.x
18. Fuchs-Buder T, Claudius C, Skovgaard LT, Eriksson LI, Mirakhur RK, Viby-Mogensen J. Good clinical research practice in pharmacodynamic studies of neuromuscular blocking agents II: the Stockholm revision. Acta anaesthesiologica Scandinavica. (2007) 51:789–808. doi: 10.1111/j.1399-6576.2007.01352.x
19. Tran DT, Newton EK, Mount VA, Lee JS, Wells GA, Perry JJ. Rocuronium vs. succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. (2015) 2015:Cd002788. doi: 10.1002/14651858.CD002788.pub3
20. Caputo N, Azan B, Domingues R, Donner L, Fenig M, Fields D. et al. Emergency department use of apneic oxygenation vs. usual care during rapid sequence intubation: a randomized controlled trial (The ENDAO Trial) academic emergency medicine: official journal of the society for academic emergency. Medicine. (2017) 24:1387–94. doi: 10.1111/acem.13274
21. Taha SK, El-Khatib MF, Baraka AS, Haidar YA, Abdallah FW, Zbeidy RA, et al. Effect of suxamethonium vs rocuronium on onset of oxygen desaturation during apnoea following rapid sequence induction. Anaesthesia. (2010) 65:358–61. doi: 10.1111/j.1365-2044.2010.06243.x
22. Erbguth PH, Bergman NA. The effect of a single dose of succinylcholine on oxygen consumption and carbon dioxide production in man. Anesthesiology. (1973) 39:447–9. doi: 10.1097/00000542-197310000-00023
Keywords: rapid sequence induction intubation, succinylcholine, rocuronium, apnea duration, oxygen saturation
Citation: Tang L, Zhao X, Li S, Huang L, Li J, Chen L and Huang S (2022) Impact of Succinylcholine vs. Rocuronium on Apnea Duration for Rapid Sequence Induction: A Prospective Cohort Study. Front. Med. 9:717477. doi: 10.3389/fmed.2022.717477
Received: 31 May 2021; Accepted: 17 January 2022;
Published: 09 February 2022.
Edited by:
Chunbo Chen, Maoming People's Hospital, ChinaReviewed by:
Manfred Blobner, Technical University of Munich, GermanyCopyright © 2022 Tang, Zhao, Li, Huang, Li, Chen and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lianhua Chen, Y2hlbmxpYW5odWFAYWxpeXVuLmNvbQ==; Shiwei Huang, aHVhbmdzaGl3ZWlAc2luYS5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.