- 1Department of Family Medicine, Chi Mei Medical Center, Tainan, Taiwan
- 2Department of Nursing, Chi Mei Medical Center, Tainan, Taiwan
- 3Department of Nursing, Chang Jung Christian University, Tainan, Taiwan
- 4School of Medicine, College of Medicine, National Sun Yat-sen University, Kaohsiung City, Taiwan
- 5Department of Anesthesiology, Chi Mei Medical Center, Tainan, Taiwan
Background: This meta-analysis aimed at evaluating the efficacy of cognitive behavior therapy (CBT) against osteoarthritis-associated symptoms in patients with knee/hip osteoarthritis.
Methods: Medline, PubMed, Cochrane Library, and EMBASE databases were searched from inception to July 2022 to identify randomized controlled trials (RCTs) comparing the efficacy of CBT with other treatment approaches in adults with confirmed knee/hip osteoarthritis. The pain intensity (primary outcome) and the secondary outcomes including insomnia severity, sleep efficiency, physical function as well as the severity of depression and fatigue were assessed at two time points (i.e., immediately after treatment and during the follow-up period). The effect size is expressed as standardized mean difference (SMD) with SMDs of < 0.2, 0.2–0.5, and 0.5–0.8, and > 0.8 representing negligible, small, medium, and large effect sizes, respectively.
Results: Fifteen RCTs were included for analysis. Immediately after CBT intervention, meta-analysis showed similar treatment effect in pain severity [SMD = –0.46, 95% confidence interval (CI): –0.95 to 0.04, 11 studies, 1557 participants] and other symptoms including depression (SMD = –0.26, 95% CI: –0.58 to 0.06, five studies, 735 participants), fatigue (SMD = –2.44, 95% CI:–6.53 to 1.65, two RCTs, 511 participants), and physical function (SMD = –0.11, 95% CI:–0.25 to 0.02, five RCTs, 720 participants) between CBT and control groups, while there was an improvement in insomnia severity (SMD = –0.65, 95% CI: –1.06 to –0.24, four RCTs, 639 participants, medium treatment effect) and sleep efficiency (SMD = 0.32, 95% CI: 0.04 to 0.59, three RCTs, 352 patients, small treatment effect). During follow-up, CBT improved pain severity (SMD = –0.52, 95% CI: –1.03 to –0.01, eight studies, 1447 participants, medium treatment effect), insomnia (SMD = –0.43, 95% CI: –0.85 to –0.01, three RCTs, 571 participants, small treatment effect), and depression (SMD = –0.39, 95% CI: –0.59 to –0.18, four RCTs, 791 participants, small treatment effect). Nevertheless, sleep efficiency, fatigue, and physical function were not improved in the follow-up period.
Conclusion: Our results may suggest the durability of CBT-associated treatment benefits, supporting its role as a potential promising alternative or complementary intervention for patients with knee/hip osteoarthritis, especially against pain and insomnia. Future large-scale investigations are warranted to verify our findings.
Systematic review registration: [https://www.crd.york.ac.uk/prospero/], identifier [CRD42022331165].
1. Introduction
Osteoarthritis, the most common form of arthritis, is one of the leading causes of musculoskeletal pain and disability worldwide (1). Joint pain in most patients with osteoarthritis is associated with reduced self-efficacy, depressed mood, and impaired sleep (2). Such complex psychosocial influences result in a varying range of functional limitations, psychological dysfunction, and impact on quality of life (2). Other psychosocial factors can also predict a higher degree of pain in osteoarthritis patients, including anxiety, depression, pain catastrophizing, and social isolation (3–5). Moreover, individuals with osteoarthritis also commonly report comorbid insomnia, the most prevalent form of sleep disturbance associated with chronic pain (6). Sleep deprivation is considered to interfere with cognitive function, emotion regulation, and pain sensation (7, 8), thereby aggravating their chronic pain condition (6, 9). Therefore, a comprehensive plan for the management of osteoarthritis should encompass educational, behavioral, psycho-social, and physical interventions, in addition to pharmacological treatment (10).
There is a body of literature showing the beneficial effects of non-pharmacologic treatments on pain reduction in patients with mild to moderate osteoarthritis, including pain education, manual therapy, and therapeutic exercise with or without combining with dry needling (11–14). Cognitive behavioral therapy (CBT) is a structural, time-limited, goal-oriented psychological treatment that incorporates behavioral strategies and cognitive processes for specific problems (15). Although it was primarily developed as a therapy for depression, its efficacy for various psychological (e.g., anxiety disorders, personality disorders, and eating disorders) and chronic (e.g., insomnia, chronic spinal pain, and osteoarthritis) conditions has also been reported (15–20). Therefore, several different CBT approaches have been developed, such as CBT for insomnia (CBT-I) and pain coping skills training (PCST). In patients with osteoarthritis, there have been previous meta-analytic studies showing the effectiveness of cognitive behavioral therapies for improving arthritic pain, sleep quality (e.g., insomnia severity and sleep efficiency), and psychosocial outcomes (e.g., self-efficacy, depression, and psychological distress) (20–24). On the other hand, the efficacy of CBT and the sustainability of its treatment benefits as an additive therapy for enhancing exercise adherence remain controversial in patients with osteoarthritis (24, 25). Moreover, the level of evidence was blemished by the inclusion of a limited number of studies or combination with other interventions (e.g., exercise) (21–23). To focus on the treatment effects of CBT, we excluded studies that combined CBT with other active treatments (e.g., exercise), which have been shown to be effective against osteoarthritis-associated psychosomatic comorbidities in published clinical guidelines (10, 26). Therefore, the aim of this systematic review is to investigate the efficacy of CBT without other combined treatment against osteoarthritis-associated symptoms, namely, pain, insomnia, physical function, and other psychological factors, in both the post-intervention and follow-up periods.
2. Methods
The findings of this meta-analysis were reported in accordance with the recommendations of the PRISMA statement (27). The protocol of this study was registered with the International Prospective Register of Systematic Reviews (CRD42022331165).
2.1. Search strategies
Three databases including the MEDLINE (Ovid) (from 1946 to July 2022), EMBASE (Ovid) (from 1974 to July 2022), and Cochrane library (from 1947 to July 2022) were searched. The reference lists of the acquired articles and Google scholar were also manually searched for potentially eligible studies. To access all possible MeSH terms, the following search terms were applied: “osteoarthritis” OR “osteoarthritis, hip” OR “osteoarthritis, knee.” The second group keywords were “cognitive behavioral therapy” OR “pain coping skill training” OR “behavior graded activity.” The two groups were combined using “AND.” Only randomized controlled trials (RCTs) published in English were considered eligible. We applied no restrictions to publication date and size of the sample. The information regarding the search strategies used is available in Supplementary Table 1.
2.2. Inclusion and exclusion criteria
Studies were eligible for review with reference to the following criteria: (1) Participants: adults with confirmed diagnosis of knee or/and hip osteoarthritis based on physician evaluation, radiographic evidence combined with self-reported osteoarthritis-related symptoms. Participants who underwent joint replacement surgery for knee/hip OA were excluded; (2) Intervention: any treatment which fulfilled the criteria for CBT regardless of its approach (e.g., face-to-face or internet-based) was eligible. We only included trials that adopted a combined cognitive-behavioral intervention model; (3) Control: interventions including routine care, education-only control, attention control, or no treatment were considered eligible for serving as controls; (4) Outcome measures: osteoarthritis-associated symptoms (e.g., pain severity, insomnia).
Exclusion criteria were: (1) studies which combined CBTs with any other active therapy, including exercise or physical therapy; (2) those using mindfulness- or hypnosis-based components as active treatments or as part of CBTs; (3) those without details about outcomes, and (4) studies not published as full-length original research papers such as letters, abstracts, reviews, case reports, or other forms of publication.
2.3. Studies selection and data collection
Two independent reviewers selected the eligible studies by examining their titles and abstracts based on the inclusion and exclusion criteria. An independent third reviewer resolved any disagreements that arose between the two reviewers. A specially designed data extraction tool (using a set of templates) was used by the two authors for independent data extraction from the studies. In the case that disagreements could not be settled through discussion, a third review author was consulted.
2.4. Outcomes and definitions
The primary outcome was the degree of pain relief following CBT intervention. The secondary outcomes included insomnia severity, sleep efficiency, physical function, depression, and fatigue. The definitions of primary and secondary outcome assessments were in accordance with those adopted in individual studies regardless of the tools being applied [e.g., Visual Analogue Scale (VAS) or Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale for pain severity; Insomnia Severity Index or Wake After Sleep Onset Diary for insomnia]. In the current meta-analysis, we evaluated the efficacy of CBT against the related symptoms at two time points, namely, immediately after treatment and during the follow-up period. If data from multiple follow-up time points were available in a study, we selected the latest time point for data extraction.
2.5. Risk of bias assessment and certainty of evidence
Two independent reviewers assessed the risk of bias of each included trial. Disagreements were resolved by discussion till a consensus was reached, otherwise a third review author acted as arbiter. According to RoB 2.0 (28), we assessed the risk of bias for each study based on the key criteria: randomization process, deviation from intended intervention, missing outcome date, measurement of the outcome, selection of the report result, and overall bias. We judged the risk of bias according to each of the domains as: low, some concerns, and high.
The overall certainty of evidence for each outcome was investigated using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework (29). Disagreements regarding overall certainty of evidence were resolved by discussion.
2.6. Data analysis
Due to a variation in assessment scales for the same outcome, the effect sizes are expressed as standardized MD (SMD) including 95% confidence interval (CI) in the current study. The effect sizes were considered minimal, small, medium, and large for SMD with values of < 0.2, 0.2–0.5, 0.5–0.8, and > 0.8, respectively (30). Meta-analysis of the data was performed if more than two trials that reported the same outcome of interest. I-squared (I2) test was used to assess heterogeneity among the RCTs with thresholds being set at > 50% for defining significant heterogeneity as previously reported (31, 32). Assuming a high heterogeneity across the included trials, we applied a priori a random-effects model regardless of the outcomes of statistical heterogeneity. The likelihood of publication bias was investigated by inspection of a funnel plot when there are ten or more studies reporting the same outcome. To evaluate the influence of an individual study on the pooled results, leave-one-out sensitivity analysis was performed (31). Meta-regression was performed to identify the origin of heterogeneity by using the comprehensive Meta-Analysis (CMA) V3 software (Biostat, Englewood, NJ, USA). The following covariates were included for meta-regression analysis, including age, proportion of female, sample size, and follow-up time. Other analyses were conducted with the Cochrane Review Manager (RevMan 5.3; Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2014). Two-tailed statistical tests with a significant level set at p < 0.05 were applied.
3. Results
3.1. Characteristics and quality of studies
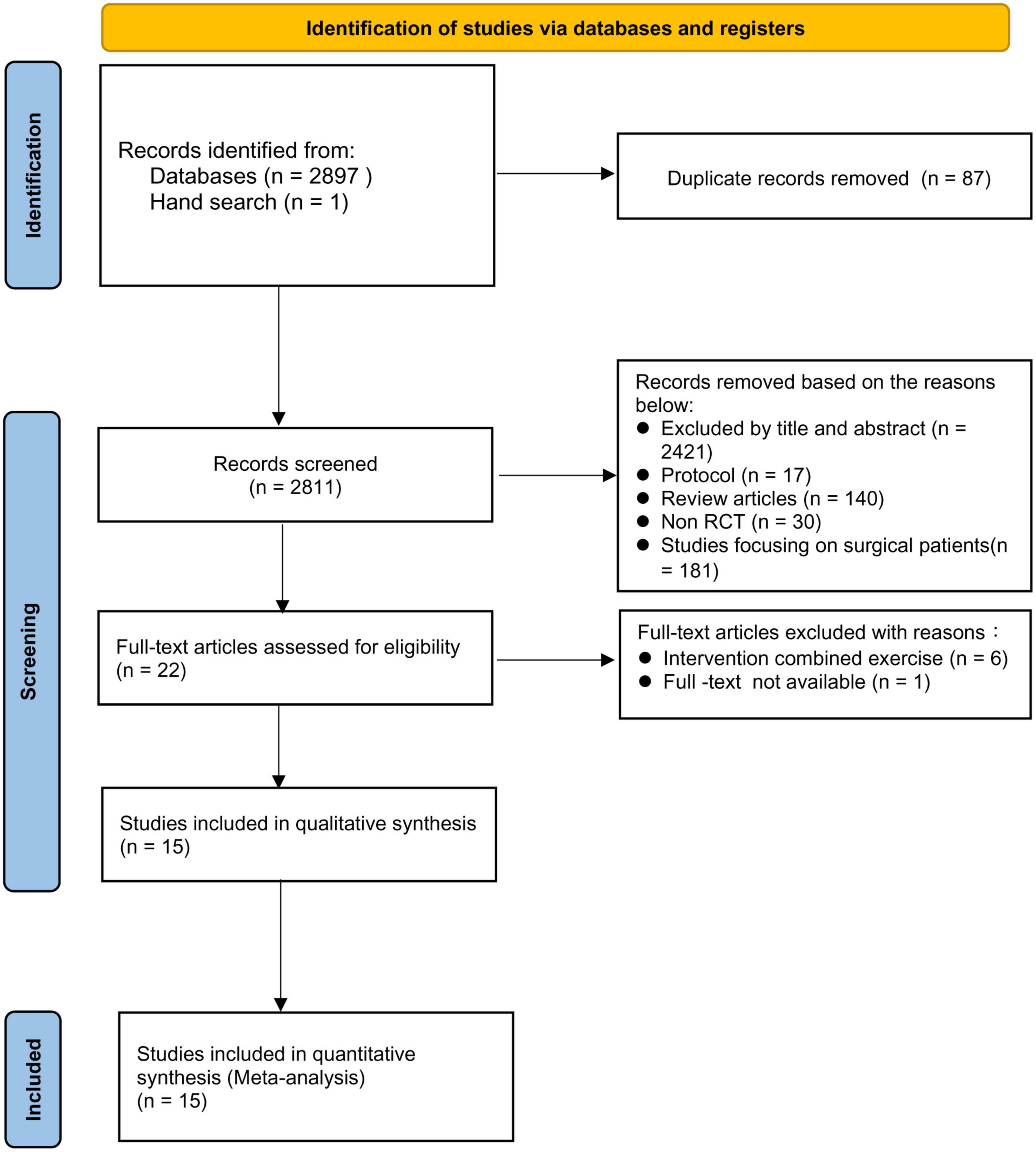
A total of 2,898 relevant records were identified through electronic database and manual literature search. After removal of duplicate records, 2,821 records were available. After eliminating 2,799 articles after screening based on title and abstract as well as exclusion criteria, 22 studies were eligible for full-text screening. Seven studies were further excluded because of a combination with exercise (n = 6) in their intervention groups and unavailability of full-text (n = 1). Finally, 15 RCTs published between 1990 and 2021 were included in this systematic review and meta-analysis (33–47). A detailed flow diagram is presented in Figure 1.
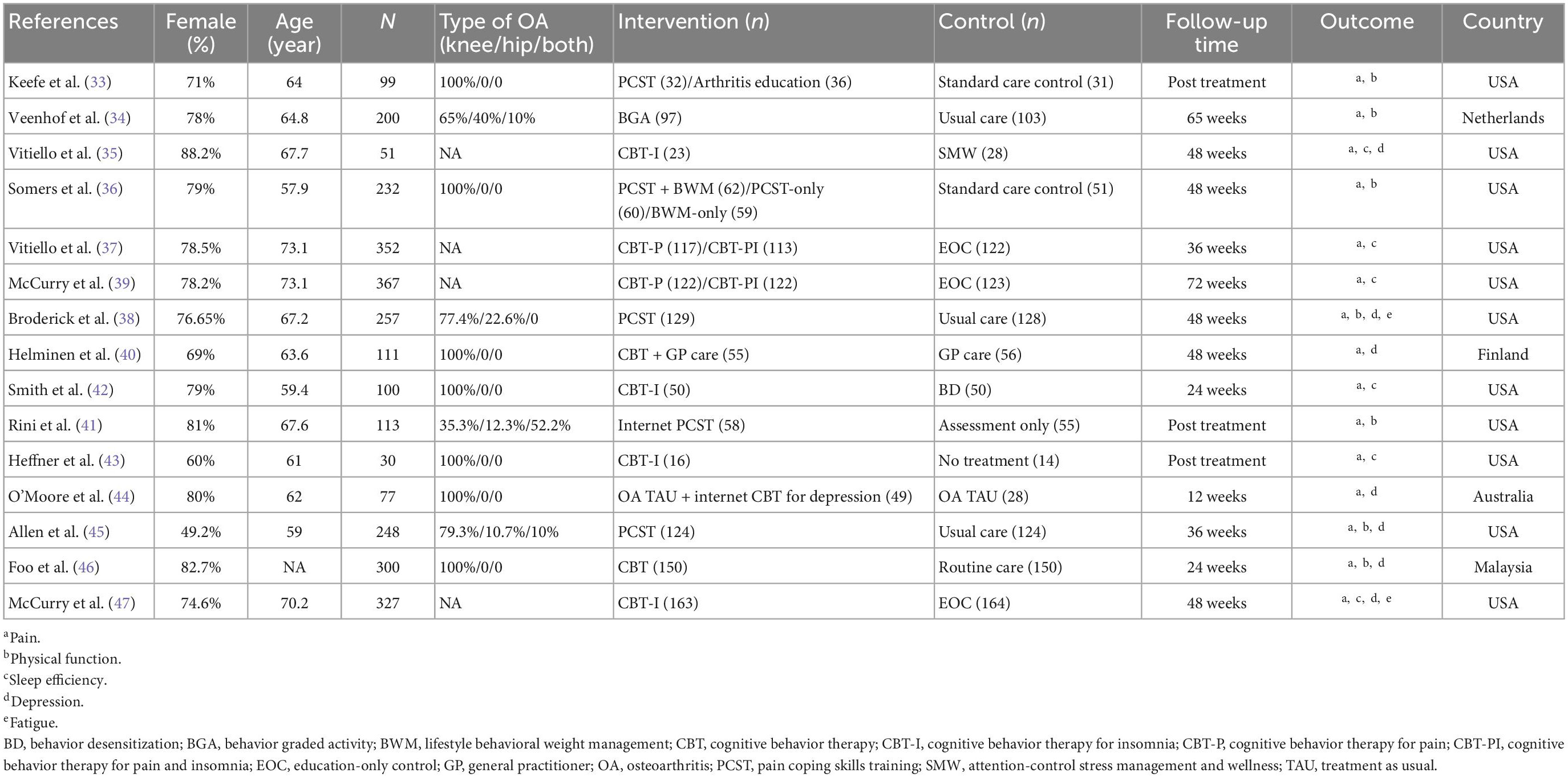
Characteristics of the included studies are summarized in Table 1. In our systematic review, a total of 2,864 patients were included. The mean age of the participants was between 57.9 and 73.1 years, while one study did not provide relevant details (46). Of the 15 analyzed studies, seven recruited only patients with knee osteoarthritis (33, 36, 40, 42–44, 46), four included patients with knee/hip osteoarthritis (34, 38, 41, 45), and four did not mention the location of osteoarthritis (35, 37, 39, 47). The sample sizes ranged from 30 to 367. The methods for diagnosis of osteoarthritis are shown in Supplementary Table 2. The diagnosis of osteoarthritis was confirmed by physician or radiographic findings combined with osteoarthritis-related symptoms in all studies (33–47). The types of interventions included CBT for insomnia (CBT-I) (four RCTs) (35, 42, 43, 47), CBT for pain (CBT-P)/CBT for pain and insomnia (CBT-PI) (two RCTs) (37, 39), CBT for depression (one RCT) (44), CBT (two RCTs) (40, 46), pain coping skills training (PCST) (five RCTs) (33, 36, 38, 41, 45), and behavioral graded activity (BGA) (one RCT) (34). The CBT protocol and components of the included studies are detailed in Supplementary Table 3. Delivery of interventions included face-to-face approach (within a group or individually) in 11 studies, telephone-approach in four studies, and internet-based approach in two studies (Supplementary Table 3). The duration of intervention sessions varied from 6 to 24 weeks, with a frequency ranging from every week to every 2 weeks (Supplementary Table 3).
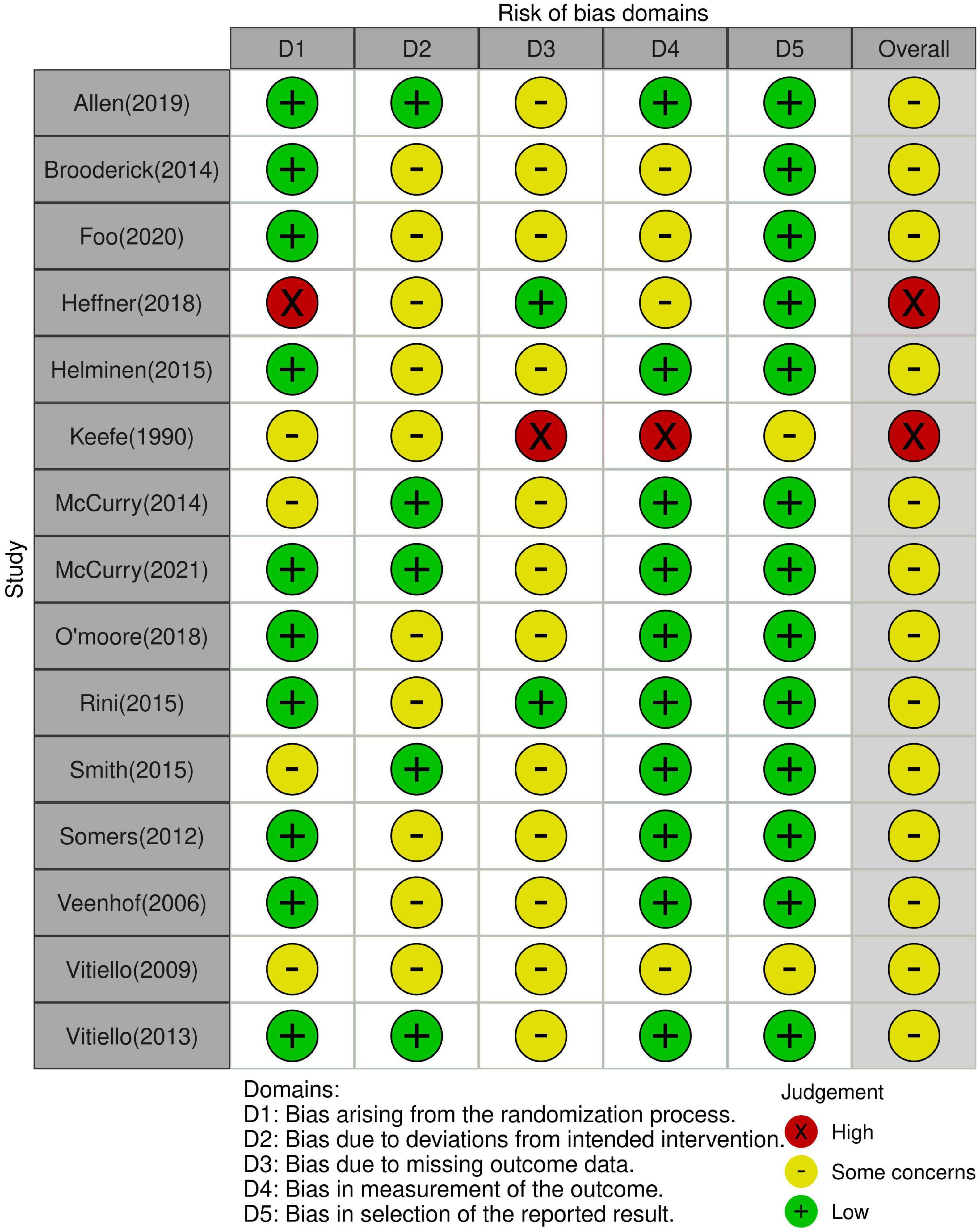
The risks of bias of the included studies are summarized in Figure 2. The risks of bias were mostly related to the randomization process, deviations from intended intervention, and missing outcome data. The overall risk of bias was judged to be of some concerns in two studies and high in the other 13 studies. The overall certainty of evidence was demonstrated in Supplementary Table 4. The overall certainty of evidence was graded as high in two outcomes (i.e., depression symptom during the follow-up period and physical function immediately after treatment), while other outcomes were considered as moderated.
3.2. Results
3.2.1. Primary outcome: Impact of CBT on pain severity
Analysis of 11 RCTs that reported immediate post-treatment pain relief demonstrated comparable treatment effect on pain severity between the CBT and control groups (SMD = –0.46, 95% CI: –0.95 to 0.04, P = 0.07, I2 = 95%, 11 studies, 1557 patients) (Figure 3A) (33, 35–38, 40–42, 44, 46, 47) with an unstable result on sensitivity analysis. During post-treatment follow-up, pooled result from a total of eight RCTs revealed a medium treatment effect of CBT on pain severity (SMD = –0.52, 95% CI: –1.03 to –0.01, P = 0.04, I2 = 95%, eight studies, 1447 patients) (Figure 3B) (34, 38, 39, 42, 44–47) with an unstable finding on sensitivity analysis. An inspection of the funnel plot showed a low risk of publication bias on pain severity immediately after treatment (Supplementary Figure 1).
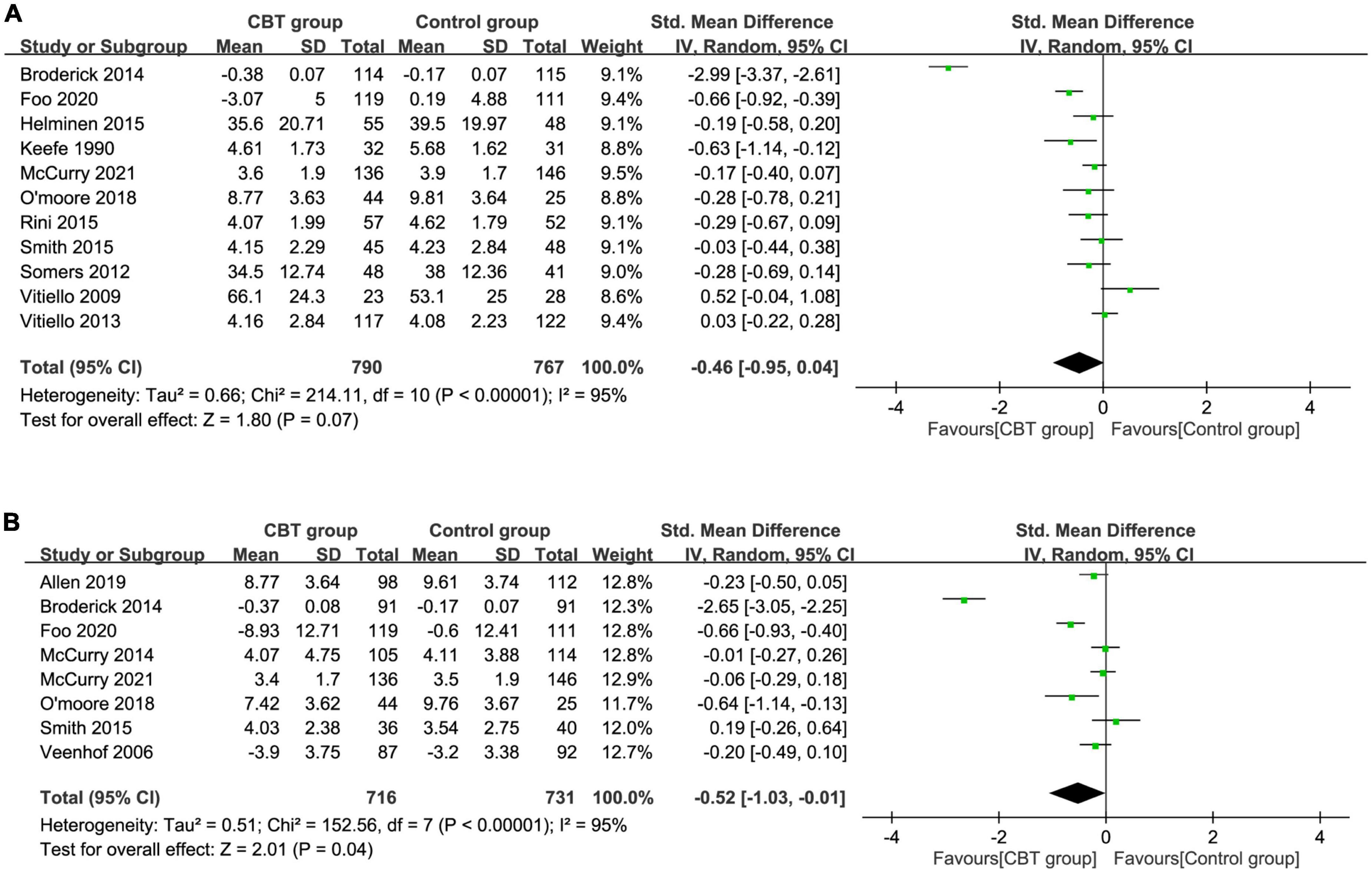
Figure 3. Forest plot comparing pain severity (A) immediately after treatment and (B) during follow-up period between the cognitive behavior therapy (CBT) and control groups. Std, standardized; iv, inverse variance; CI, confidence interval.
3.2.2. Secondary outcomes: Insomnia severity
Analysis of a total of four RCTs with information about insomnia showed a medium treatment effect of CBT on severity of insomnia immediately after treatment (SMD = –0.65, 95% CI: –1.06 to –0.24, P = 0.002, I2 = 81%, four RCTs, 639 patients) (Supplementary Figure 2) (37, 42, 43, 47) with a consistent finding on sensitivity analysis. In the follow-up period, the beneficial effects of CBT on insomnia severity demonstrated a small treatment effect (SMD = –0.43, 95% CI: –0.85 to –0.01, P = 0.04, I2 = 82%, three RCTs, 571 patients), suggesting an association between CBT and a lower severity of insomnia (Figure 4A) (39, 42, 47). However, sensitivity analysis revealed an instability of the result.
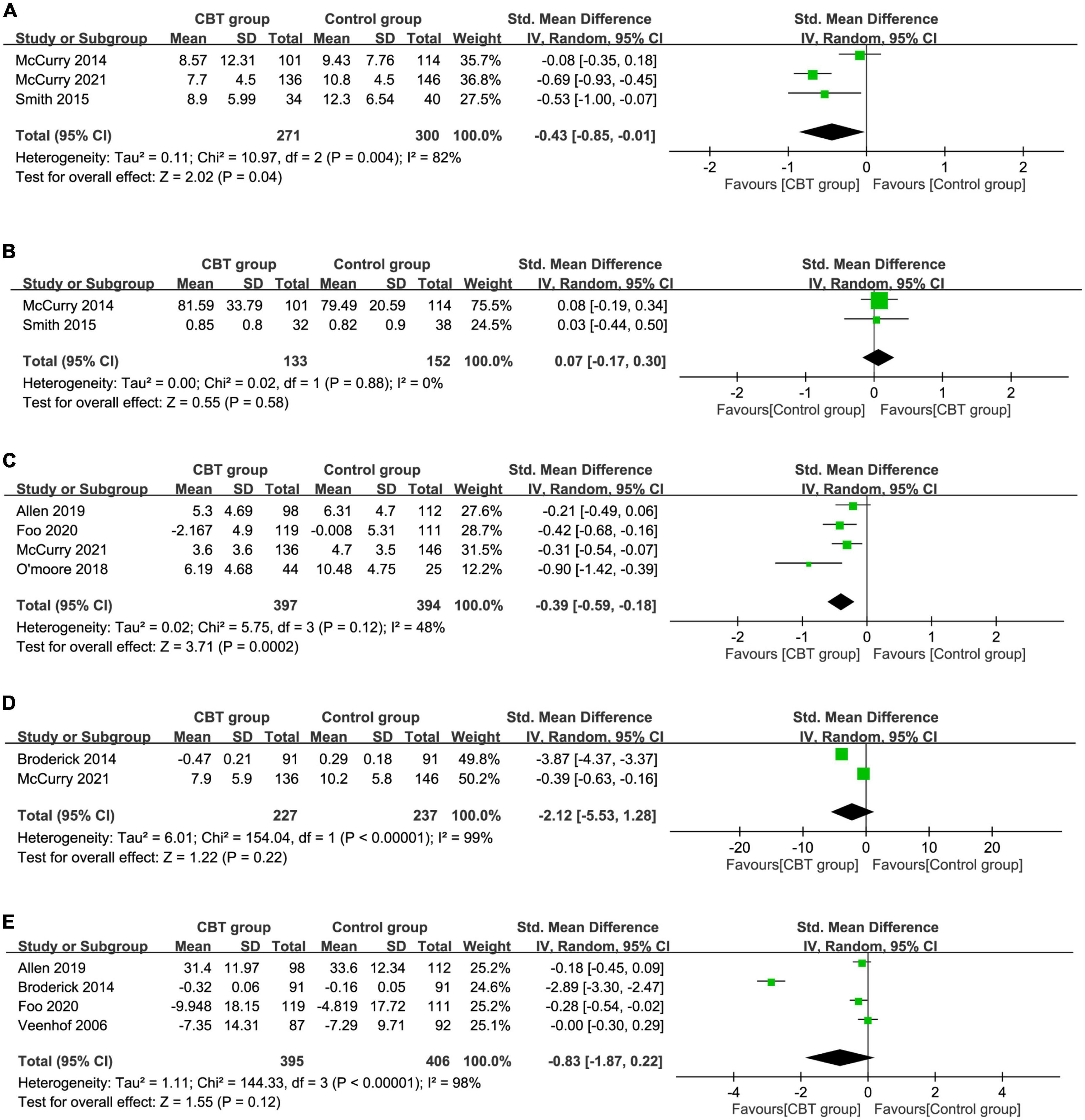
Figure 4. Forest plot comparing (A) insomnia severity, (B) sleep efficiency, (C) depression severity, (D) fatigue severity, and (E) physical function during the follow-up period between the cognitive behavior therapy (CBT) and control groups. Std, standardized; iv, inverse variance; CI, confidence interval.
3.2.3. Sleep efficiency
Three studies provided the details regarding the impact of CBT on sleep efficiency immediately after treatment (35, 37, 42) while two RCTs reported this information in the follow-up period (39, 42). The use of CBT had a small treatment effect on sleep efficiency immediately after treatment (SMD = 0.32, 95% CI: 0.04 to 0.59, P = 0.03, I2 = 32%, three RCTs, 352 patients) (Figure 4B) (35, 37, 42) with an unstable finding on sensitivity analysis. However, there was a similar treatment effect on sleep efficiency between the two groups during the follow-up period (SMD = 0.07, 95% CI: –0.17 to 0.3, P = 0.58, two studies, 285 patients) (Supplementary Figure 3) (39, 42) with a consistent result on sensitivity analysis.
3.2.4. Severity of depression symptom
The pooled results immediately after treatment and during follow-up period were available in five (35, 40, 44, 46, 47) and four RCTs (44–47), respectively. Immediately after intervention, there was comparable treatment effect of CBT in depression symptoms (SMD = –0.26, 95% CI: –0.58 to 0.06, p = 0.12, I2 = 75%, five studies, 735 patients) (Supplementary Figure 4) (35, 40, 44, 46, 47). During the follow-up period, there was a small treatment effect of CBT on depression severity (SMD = –0.39, 95% CI: –0.59 to –0.18, p = 0.0002, I2 = 48%, four RCTs, 791 patients) (Figure 4C) (44–47). Sensitivity analysis supported the stability of these two outcomes.
3.2.5. Fatigue symptom and physical function
Regarding the severity of fatigue, there was similar treatment effect on this outcome immediately after treatment (SMD = –2.44, 95% CI:-6.53 to 1.65, P = 0.24, I2 = 100%, two RCTs, 511 patients) (Supplementary Figure 5) (38, 47) and during the follow-up period (SMD = –2.12, 95% CI:-5.53 to 1.28, P = 0.22, I2 = 99%, two RCTs, 464 patients) (Figure 4D) (38, 47). In respect of physical function, there was comparable treatment effect in the CBT group compared with the controls immediately after treatment (SMD = –0.11, 95% CI:-0.25 to 0.02, P = 0.09, I2 = 20%, five RCTs, 720 patients) (Supplementary Figure 6) (33, 36, 38, 41, 46) and during the follow-up period (SMD = –0.83, 95% CI:-1.87 to 0.22, P = 0.12, I2 = 98%, four RCTs, 801 patients) (Figure 4E) (34, 38, 45, 46). Sensitivity analysis of the outcomes of fatigue and physical function demonstrated unstable results regardless of the timing of evaluation (i.e., during immediate post-treatment or follow-up periods).
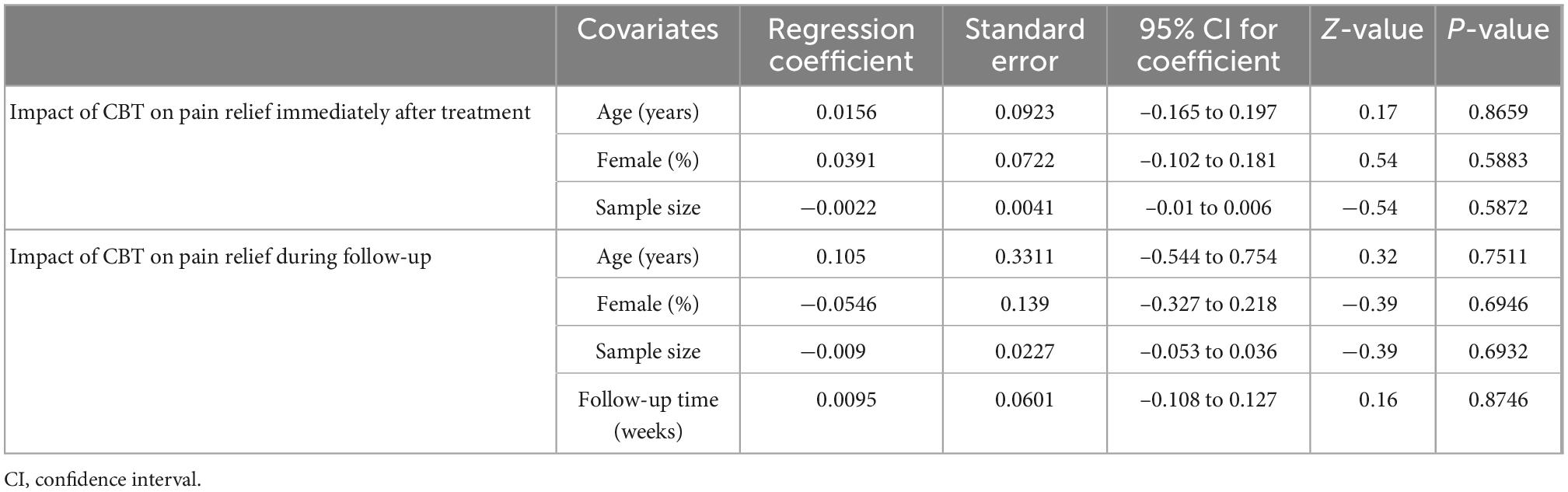
3.3. Meta-regression
Meta-regression analyses demonstrated no significant association of the included covariates (i.e., age, female ratio, sample size, and follow-up time) with the impact of CBT on pain severity (i.e., two-sided p > 0.05) (Table 2).
4. Discussion
The results of the current studies had several striking clinical implications. Given that chronic pain associated with osteoarthritis is a major factor contributing to an impaired quality of life and socioeconomic burden (48–50), our results may suggest the effectiveness of psychological intervention as an alternative or complementary treatment strategy to the recommended pharmacological treatment (e.g., NSAIDs) (10, 26) in this setting. The lack of adverse side effects of medications may be another merit. To the best of our knowledge, this is the most comprehensive systematic review and meta-analysis focusing on the efficacy of CBT alone against osteoarthritis-associated symptoms with the inclusion of a recently published large-scale RCT of telephone CBT-I. The current meta-analysis of 15 RCTs showed an association of the implementation of CBT only with an improvement in the severity of insomnia and sleep efficiency immediately after intervention, but not in other symptoms including pain severity, depression, fatigue, and physical function in the immediate post-treatment period. During the follow-up period, we found that the use of CBT improved the severity of pain, insomnia, and depression. Nevertheless, sleep efficiency, fatigue, and physical function were not improved in the follow-up period.
In terms of the efficacy of CBT for osteoarthritis-related pain relief, the evidence reported in individual RCTs was mixed. The discrepancy may result from the use of different CBT approaches. For instance, instead of the application of CBT for pain, some studies used CBT for insomnia or CBT for depression. In this regard, previous published trials focusing on the effectiveness of pain coping skills training (PCST) in the population with osteoarthritis reported significant pain improvement during the immediate post-treatment period as well as during 12-month follow-ups, despite variation in intervention delivery (33, 38, 41). Regarding CBT for insomnia (CBT-I), the relevant trials also demonstrated mixed findings (35, 37, 39, 42, 47) probably attributable to the small sample sizes and less rigorous control groups in those reporting negative findings (6). On the other hand, another study demonstrated an improvement in osteoarthritis-related pain through internet CBT for depression at 3-month follow-up but not during the immediate post-treatment period (44). Nevertheless, the results of those trials need to be judiciously interpreted because of their inclusion of pain-related measurements mainly as secondary outcomes.
Our findings in patients with knee/hip osteoarthritis showed a medium treatment effect of CBT on pain severity during the follow-up period despite only a similar treatment effect immediately after intervention. The result is consistent with that of a prior review article that demonstrated the effectiveness of CBT for pain relief during long-term follow-up in the chronic pain population with fibromyalgia syndrome (16). On the other hand, different from our findings, another meta-analysis comprising participants with chronic non-cancer pain comorbid with insomnia revealed a correlation between CBT-I and short-term pain improvement but not in the follow-up period (51). Nevertheless, the use of CBT-I, a therapeutic tool primarily designed for insomnia, in that meta-analysis (51) may not accurately reflect the efficacy of the general CBT approach for chronic pain treatment. In contrast with previous systematic reviews that investigated the efficacy of CBT for a variety of chronic non-cancer pain (17, 51), one of the merits of the current study was our focusing on the knee/hip osteoarthritis population. Regarding the characteristics of our included studies, we found a tendency of increased utilization of internet- or telephone-based CBTs in the last decade compared to prior studies that mainly used face-to-face approaches. Technological evolution, which has overhauled the mode of communication in the recent decade, may be a possible explanation.
Focusing on the secondary outcomes, our results suggested small to medium treatment effect of CBTs on insomnia severity during both the immediate post-treatment and follow-up periods. A previous study has shown an association between sleep disturbance and osteoarthritis-induced pain (52). In addition, a recent systematic review demonstrated a correlation of the diagnosis of temporomandibular joint osteoarthritis with sleep quality and sleep disorders (e.g., obstructive sleep apnea) (53), further highlighting the adverse impact of osteoarthritis on the normal sleep cycle. Our findings were consistent with those of a prior meta-analysis (51) that demonstrated a significant and sustained therapeutic efficacy of CBT-I against insomnia in patients with chronic pain. It was noteworthy that the improvement in insomnia remained significant after the inclusion of a large-scale telephone CBT trial (47). However, our study showed a comparable treatment effect of CBT on sleep efficiency during follow-ups. In addition to the limited number of studies available for analysis, reliance on retrospective self-reported data (6) may introduce bias to the outcome. Despite the established effectiveness of CBT-I against comorbid insomnia from previous meta-analyses (54, 55), the current investigation was the first to focus on patients with knee/hip osteoarthritis.
Regarding the efficacy of CBT for depression among patients diagnosed with knee osteoarthritis, a previous trial including 300 participants failed to show significant treatment benefits immediately after CBT despite the demonstration of improvements at post-treatment one and six months (46). In contrast, another relatively small-scale trial on 69 individuals with knee osteoarthritis investigating the effectiveness of CBT against depression demonstrated significant improvement in depression during both immediate post-treatment and follow-up periods (44). Nevertheless, examination of the pooled evidence in the current study revealed a small treatment effect of CBT on depressive symptoms during follow-ups, while no benefit was noted in the immediate post-treatment period. The absence of a significant improvement during the immediate post-treatment period may be attributed to a variation in therapeutic protocols [e.g., group CBT (46) vs. internet CBT for depression (44)] across the included studies.
With respect to the other secondary outcomes, the current study revealed no significant benefit of CBT in the treatment of fatigue. Our finding was consistent with that of a previous meta-analysis focusing on the effectiveness of CBT-I for chronic pain with insomnia that showed no therapeutic effect against fatigue both during the immediate post-treatment and follow-up periods (51). Regarding physical function, the present investigation demonstrated no therapeutic benefit of CBT in both periods. Consistently, another meta-analysis investigating the use of pain coping skills training in patients with osteoarthritis also failed to reveal a positive impact of CBT on physical function (56). The small numbers of studies available for analysis may contribute to the lack of significant treatment benefits regarding the two outcomes in the current study. While the outcome on fatigue was derived from only two studies, the result on physical function was based on five and four trials for the immediate post-treatment and follow-up periods, respectively. Therefore, further studies are warranted to verify our findings.
There are several limitations in the current study. First, the high heterogeneities across our included studies attributable to the diversity in therapeutic protocols, modes of delivery, therapist (e.g., trained nurse vs. physical therapist) as well as the number of treatment sessions and duration (Supplementary Table 3) may introduce bias to our outcomes. Besides, the use of different pain assessment tools (e.g., AIMS pain subscale, WOMAC pain subscale, and VAS scale), the recruitment of a mixed population of patients diagnosed with knee or hip osteoarthritis, and variations in follow-up periods may be potential sources of bias. Second, publication bias may arise from our inclusion of English literature for analysis. Third, the risk of bias assessment in the current meta-analysis showed that the overall risk of bias was high and of some concerns in two and 13 studies, respectively. The risk of bias may mostly be attributed to the randomization process, deviations from intended intervention, and missing outcome data. Therefore, our results may be biased due to the poor quality of those studies. Finally, despite our demonstration of the effectiveness of CBT against pain, insomnia, and depression during the follow-up periods, the selection of different cut-off points and follow-up periods as well as the merging of results from different time points (36, 38) across the included studies precluded our elucidation of the durability of its efficacy.
5. Conclusion
This systematic review and meta-analysis showed the efficacy of CBTs against osteoarthritis-related pain, insomnia, and depression during the follow-up period but without significant benefit in the treatment of sleep efficiency, fatigue, and physical function. Our results may suggest the durability of CBT-associated treatment effects, supporting its role as a potential promising alternative or complementary intervention for patients with knee/hip osteoarthritis, especially against pain and insomnia. Nevertheless, the high heterogeneity across the included studies warrants future large-scale investigations to verify our findings.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
H-ML and P-SH: conceptualization. N-CC: methodology. C-HT: software. N-CC and W-FK: formal analysis. N-CC and H-ML: data curation. H-ML, P-SH, and K-CH: writing—original draft preparation. K-CH and Y-LL: writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.1083095/full#supplementary-material
References
1. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1211–59. doi: 10.1016/S0140-6736(17)32154-2
2. National Clinical Guideline C. National Institute for Health and Clinical Excellence: Guidance. Osteoarthritis: Care and Management in Adults. London: National Institute for Health and Care Excellence (2014).
3. Smith B, Zautra A. The effects of anxiety and depression on weekly pain in women with arthritis. Pain. (2008) 138:354–61.
4. Rosemann T, Laux G, Szecsenyi J, Wensing M, Grol R. Pain and osteoarthritis in primary care: factors associated with pain perception in a sample of 1,021 patients. Pain Med. (2008) 9:903–10. doi: 10.1111/j.1526-4637.2008.00498.x
5. Somers T, Keefe F, Pells J, Dixon K, Waters S, Riordan P, et al. Pain catastrophizing and pain-related fear in osteoarthritis patients: relationships to pain and disability. J Pain Symptom Manage. (2009) 37:863–72. doi: 10.1016/j.jpainsymman.2008.05.009
6. Finan P, Buenaver L, Coryell V, Smith M. Cognitive-behavioral therapy for comorbid insomnia and chronic pain. Sleep Med Clin. (2014) 9:261–74.
7. Weiner D, Rudy T, Morrow L, Slaboda J, Lieber S. The relationship between pain, neuropsychological performance, and physical function in community-dwelling older adults with chronic low back pain. Pain Med. (2006) 7:60–70.
8. Yoo S, Gujar N, Hu P, Jolesz F, Walker M. The human emotional brain without sleep–a prefrontal amygdala disconnect. Curr Biol. (2007) 17:R877–8. doi: 10.1016/j.cub.2007.08.007
9. Lautenbacher S, Kundermann B, Krieg J. Sleep deprivation and pain perception. Sleep Med Rev. (2006) 10:357–69.
10. Kolasinski S, Neogi T, Hochberg M, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis foundation guideline for the management of osteoarthritis of the hand, Hip, and Knee. Arthritis Care Res. (2020) 72:149–62.
11. Sánchez Romero E, Fernández-Carnero J, Calvo-Lobo C, Ochoa Sáez V, Burgos Caballero V, Pecos-Martín D. Is a Combination of Exercise and Dry Needling Effective for Knee OA? Pain Med. (2020) 21:349–63.
12. Sinatti P, Sánchez Romero E, Martínez-Pozas O, Villafañe J. Effects of patient education on pain and function and its impact on conservative treatment in elderly patients with pain related to hip and knee osteoarthritis: a systematic review. Int J Environ Res Public Health. (2022) 19:6194. doi: 10.3390/ijerph19106194
13. Alonso Pérez J, Martín Pérez S, Battaglino A, Villafañe J, Alonso-Sal A, Sánchez Romero E. An Up-Date of the muscle strengthening exercise effectiveness in postmenopausal women with osteoporosis: a qualitative systematic review. J Clin Med. (2021) 10:2229. doi: 10.3390/jcm10112229
14. Sánchez-Romero E, González-Zamorano Y, Arribas-Romano A, Martínez-Pozas O, Fernández Espinar E, Pedersini P, et al. Efficacy of manual therapy on facilitatory nociception and endogenous pain modulation in older adults with knee osteoarthritis: a case series. Appl Sci. (2021) 11:1895.
15. Keith Hawton P, Kirk J, Clark DM. Cognitive Behaviour Therapy for Psychiatric Problems: A Practical Guide. Oxford: Oxford University Press (1989).
16. Bernardy K, Klose P, Welsch P, Häuser W. Efficacy, acceptability and safety of cognitive behavioural therapies in fibromyalgia syndrome – A systematic review and meta-analysis of randomized controlled trials. Eur J Pain. (2018) 22:242–60.
17. Hajihasani A, Rouhani M, Salavati M, Hedayati R, Kahlaee A. The influence of cognitive behavioral therapy on pain, quality of life, and depression in patients receiving physical therapy for chronic low back pain: a systematic review. PM R. (2019) 11:167–76. doi: 10.1016/j.pmrj.2018.09.029
18. Pardos-Gascón E, Narambuena L, Leal-Costa C, van-der Hofstadt-Román C. Differential efficacy between cognitive-behavioral therapy and mindfulness-based therapies for chronic pain: systematic review. Int J Clin Health Psychol. (2021) 21:100197. doi: 10.1016/j.ijchp.2020.08.001
19. Thoma N, Pilecki B, McKay D. Contemporary cognitive behavior therapy: a review of theory, history, and evidence. Psychodyn Psychiatry. (2015) 43:423–61.
20. Ho K, Ferreira P, Pinheiro M, Aquino Silva D, Miller C, Grunstein R, et al. Sleep interventions for osteoarthritis and spinal pain: a systematic review and meta-analysis of randomized controlled trials. Osteoarthr Cartilage. (2019) 27:196–218. doi: 10.1016/j.joca.2018.09.014
21. Ismail A, Moore C, Alshishani N, Yaseen K, Alshehri M. Cognitive behavioural therapy and pain coping skills training for osteoarthritis knee pain management: a systematic review. J Phys Ther Sci. (2017) 29:2228–35.
22. Pitsillides A, Stasinopoulos D, Giannakou K. The effects of cognitive behavioural therapy delivered by physical therapists in knee osteoarthritis pain: a systematic review and meta-analysis of randomized controlled trials. J Bodyw Mov Ther. (2021) 25:157–64. doi: 10.1016/j.jbmt.2020.11.002
23. Briani R, Ferreira A, Pazzinatto M, Pappas E, De Oliveira Silva D, Azevedo F. What interventions can improve quality of life or psychosocial factors of individuals with knee osteoarthritis? A systematic review with meta-analysis of primary outcomes from randomised controlled trials. Br J Sports Med. (2018) 52:1031–8.
24. Hawley D. Psycho-educational interventions in the treatment of arthritis. Bailliere’s Clin Rheumatol. (1995) 9:803–23.
25. Jordan J, Holden M, Mason E, Foster N. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. (2010) 2010:Cd005956.
26. Bannuru R, Osani M, Vaysbrot E, Arden N, Bennell K, Bierma-Zeinstra S, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr Cartilage. (2019) 27:1578–89. doi: 10.1016/j.joca.2019.06.011
27. Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. (2021) 134:178–89.
28. Sterne J, Savović J, Page M, Elbers R, Blencowe N, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898.
29. Guyatt G, Oxman A, Vist G, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. (2008) 336:924–6.
30. Kesten J, Griffiths P, Cameron N. A systematic review to determine the effectiveness of interventions designed to prevent overweight and obesity in pre-adolescent girls. Obesity Rev. (2011) 12:997–1021. doi: 10.1111/j.1467-789X.2011.00919.x
31. Hung K, Chang Y, Chen I, Soong T, Ho C, Hsing C, et al. Efficacy of high flow nasal oxygenation against hypoxemia in sedated patients receiving gastrointestinal endoscopic procedures: a systematic review and meta-analysis. J Clin Anesth. (2022) 77:110651.
32. Hung K, Wu S, Hsu C, Ko C, Chen J, Huang P, et al. Efficacy of laryngeal mask airway against postoperative pharyngolaryngeal complications following thyroid surgery: a systematic review and meta-analysis of randomized controlled studies. Sci Rep. (2022) 12:18210. doi: 10.1038/s41598-022-21989-5
33. Keefe F, Caldwell D, Williams D, Gil K, Mitchell D, Robertson C, et al. Pain coping skills training in the management of osteoarthritic knee pain: a comparative study. Behav Therapy. (1990) 21:49–62.
34. Veenhof C, Köke A, Dekker J, Oostendorp R, Bijlsma J, van Tulder M, et al. Effectiveness of behavioral graded activity in patients with osteoarthritis of the hip and/or knee: a randomized clinical trial. Arthritis Rheum. (2006) 55:925–34.
35. Vitiello M, Rybarczyk B, Von Korff M, Stepanski E. Cognitive behavioral therapy for insomnia improves sleep and decreases pain in older adults with co-morbid insomnia and osteoarthritis. J Clin Sleep Med. (2009) 5:355–62.
36. Somers T, Blumenthal J, Guilak F, Kraus V, Schmitt D, Babyak M, et al. Pain coping skills training and lifestyle behavioral weight management in patients with knee osteoarthritis: a randomized controlled study. Pain. (2012) 153:1199–209. doi: 10.1016/j.pain.2012.02.023
37. Vitiello M, McCurry S, Shortreed S, Balderson B, Baker L, Keefe F, et al. Cognitive-behavioral treatment for comorbid insomnia and osteoarthritis pain in primary care: the lifestyles randomized controlled trial. J Am Geriatr Soc. (2013) 61:947–56.
38. Broderick J, Keefe F, Bruckenthal P, Junghaenel D, Schneider S, Schwartz J, et al. Nurse practitioners can effectively deliver pain coping skills training to osteoarthritis patients with chronic pain: a randomized, controlled trial. Pain. (2014) 155:1743–54.
39. McCurry S, Shortreed S, Von Korff M, Balderson B, Baker L, Rybarczyk B, et al. Who benefits from CBT for insomnia in primary care? Important patient selection and trial design lessons from longitudinal results of the Lifestyles trial. Sleep. (2014) 37:299–308. doi: 10.5665/sleep.3402
40. Helminen E, Sinikallio S, Valjakka A, Väisänen-Rouvali R, Arokoski J. Effectiveness of a cognitive-behavioural group intervention for knee osteoarthritis pain: a randomized controlled trial. Clin Rehabil. (2015) 29:868–81. doi: 10.1177/0269215514558567
41. Rini C, Porter L, Somers T, McKee D, DeVellis R, Smith M, et al. Automated Internet-based pain coping skills training to manage osteoarthritis pain: a randomized controlled trial. Pain. (2015) 156:837–48. doi: 10.1097/j.pain.0000000000000121
42. Smith M, Finan P, Buenaver L, Robinson M, Haque U, Quain A, et al. Cognitive-behavioral therapy for insomnia in knee osteoarthritis: a randomized, double-blind, active placebo-controlled clinical trial. Arthritis Rheumatol. (2015) 67:1221–33. doi: 10.1002/art.39048
43. Heffner K, France C, Ashrafioun L, Quiñones M, Walsh P, Maloney M, et al. Clinical pain-related outcomes and inflammatory cytokine response to pain following insomnia improvement in adults with knee osteoarthritis. Clin J Pain. (2018) 34:1133–40. doi: 10.1097/AJP.0000000000000644
44. O’Moore KA, Newby J, Andrews G, Hunter D, Bennell K, Smith J, et al. Internet cognitive-behavioral therapy for depression in older adults with knee osteoarthritis: a randomized controlled trial. Arthritis Care Res. (2018) 70:61–70. doi: 10.1002/acr.23257
45. Allen K, Somers T, Campbell L, Arbeeva L, Coffman C, Cené C, et al. Pain coping skills training for African Americans with osteoarthritis: results of a randomized controlled trial. Pain. (2019) 160:1297–307.
46. Foo C, Arumugam M, Lekhraj R, Lye M, Mohd-Sidik S, Jamil Osman Z. Effectiveness of health-led cognitive behavioral-based group therapy on pain, functional disability and psychological outcomes among knee osteoarthritis patients in Malaysia. Int J Environ Res Public Health. (2020) 17:6179. doi: 10.3390/ijerph17176179
47. McCurry S, Zhu W, Von Korff M, Wellman R, Morin C, Thakral M, et al. Effect of telephone cognitive behavioral therapy for insomnia in older adults with osteoarthritis pain: a randomized clinical trial. JAMA Intern Med. (2021) 181:530–8. doi: 10.1001/jamainternmed.2020.9049
48. Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr Cartilage. (2013) 21:1145–53.
49. Bartley E, Palit S, Staud R. Predictors of osteoarthritis pain: the importance of resilience. Curr Rheumatol Rep. (2017) 19:57.
50. Rosemann T, Laux G, Szecsenyi J. Osteoarthritis: quality of life, comorbidities, medication and health service utilization assessed in a large sample of primary care patients. J Orthopaedic Surg Res. (2007) 2:12. doi: 10.1186/1749-799X-2-12
51. Selvanathan J, Pham C, Nagappa M, Peng P, Englesakis M, Espie C, et al. Cognitive behavioral therapy for insomnia in patients with chronic pain – A systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. (2021) 60:101460. doi: 10.1016/j.smrv.2021.101460
52. Parmelee P, Tighe C, Dautovich N. Sleep disturbance in osteoarthritis: linkages with pain, disability, and depressive symptoms. Arthritis Care Res. (2015) 67:358–65. doi: 10.1002/acr.22459
53. Sánchez Romero E, Martínez-Pozas O, García-González M, de-Pedro M, González-Álvarez M, Esteban-González P, et al. Association between sleep disorders and sleep quality in patients with temporomandibular joint osteoarthritis: a systematic review. Biomedicines. (2022) 10:2143. doi: 10.3390/biomedicines10092143
54. van der Zweerde T, Bisdounis L, Kyle S, Lancee J, van Straten A. Cognitive behavioral therapy for insomnia: a meta-analysis of long-term effects in controlled studies. Sleep Med Rev. (2019) 48:101208.
55. Geiger-Brown J, Rogers V, Liu W, Ludeman E, Downton K, Diaz-Abad M. Cognitive behavioral therapy in persons with comorbid insomnia: a meta-analysis. Sleep Med Rev. (2015) 23:54–67.
Keywords: cognitive behavior therapy, osteoarthritis, meta-analysis, pain, insomnia
Citation: Lin H-M, Hsieh P-S, Chen N-C, Tsai C-H, Kuo W-F, Lee Y-L and Hung K-C (2023) Impact of cognitive behavior therapy on osteoarthritis-associated pain, insomnia, depression, fatigue, and physical function in patients with knee/hip osteoarthritis: A systematic review and meta-analysis of randomized controlled trials. Front. Med. 9:1083095. doi: 10.3389/fmed.2022.1083095
Received: 28 October 2022; Accepted: 15 December 2022;
Published: 06 January 2023.
Edited by:
Elisa Belluzzi, University of Padua, ItalyReviewed by:
Adewale Adebajo, The University of Sheffield, United KingdomEleuterio A. Sánchez Romero, European University of Madrid, Spain
Nicola Luigi Bragazzi, York University, Canada
Copyright © 2023 Lin, Hsieh, Chen, Tsai, Kuo, Lee and Hung. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying-Li Lee,  bjkzMDk2OUBtYWlsLmNoaW1laS5vcmcudHc=; Kuo-Chuan Hung,
bjkzMDk2OUBtYWlsLmNoaW1laS5vcmcudHc=; Kuo-Chuan Hung,  ZWQxMDI2MDVAZ21haWwuY29t
ZWQxMDI2MDVAZ21haWwuY29t
†These authors have contributed equally to this work
‡These authors share first authorship
 Hong-Min Lin1‡
Hong-Min Lin1‡ Ying-Li Lee
Ying-Li Lee Kuo-Chuan Hung
Kuo-Chuan Hung