- 1Rheumatology, AP-HP. Université Paris-Saclay, Hôpital Bicêtre, Le Kremlin-Bicêtre, France
- 2Faculté de Médecine, Université Paris-Saclay, Le Kremlin-Bicêtre, France
- 3Université Paris-Saclay, INSERM, CEA, Centre de Recherche en Immunologie des Infections Virales et des Maladies Auto-immunes, Le Kremlin-Bicêtre, France
- 4Biophysics and Nuclear Medicine-Molecular Imaging, AP-HP. Université Paris-Saclay, Hôpital Bicêtre, Le Kremlin-Bicêtre, France
- 5Université Paris-Saclay, CEA, CNRS, Inserm, BioMaps, Orsay, France
18F-Labeled Fluorodeoxyglucose-Positron Emission Tomography (18F-FDG PET) is a molecular imaging tool commonly used in practice for the assessment of many cancers. Thanks to its properties, its use has been progressively extended to numerous inflammatory conditions, including chronic inflammatory rheumatism (CIR) such as rheumatoid arthritis (RA), spondylarthritis (SpAs) and polymyalgia rheumatica (PMR). 18F-FDG PET is currently not recommended for the diagnostic of CIRs. However, this whole-body imaging tool has emerged in clinical practice, providing a general overview of systemic involvement occurring in CIRs. Numerous studies have highlighted the capacity of 18F-FDG PET to detect articular and extra articular involvements in RA and PMR. However, the lack of specificity of 18F-FDG limits its use for diagnosis purpose. Finally, the key question is the definition of the best way to integrate this whole-body imaging tool in the patient’s management workflow.
Introduction
Positron Emission Tomography (PET) is a whole-body, non-invasive, and highly sensitive imaging modality based on the detection of radiolabeled vectors of interest. During the last 20 years, PET using 18F-fluoro-deoxy-glucose (18F-FDG), an analog of glucose radiolabeled with Fluor 18 (18F), has become a key imaging tool to diagnose, stage, and monitor many cancers in practice. Exploiting the metabolic properties of activated cells, the use of 18F-FDG has been progressively extended to numerous inflammation and infection disorders (1). A recent report from the European league Against Rheumatisms (EULAR) highlighted the heterogeneity of the availability to PET imaging for rheumatologic purpose across 25 European countries (2), which is currently dominated for the diagnosis of large vessel vasculitis (LVV) (3, 4) or to investigate fever of unknown origin (5). EULAR has provided official recommendations for the use of imaging in LVV, rheumatoid arthritis (RA) and spondylarthritis (SpAs) in clinical practice (2, 3, 6). While the use of PET modality is clearly defined only for LVV (3), 18F-FDG PET applied to chronic inflammatory rheumatisms (CIR) has concretely emerged in clinical practice (7, 8) (Figure 1 and Table 1). In this context, the choice of the best imaging modalities in patients with suspected CIRs – and the place of PET-CT in this strategy - arises at several stages of the management: to establish a positive diagnosis, to eliminate a differential diagnosis and in particular an infectious or para-neoplastic cause and finally to monitor the response to treatment.
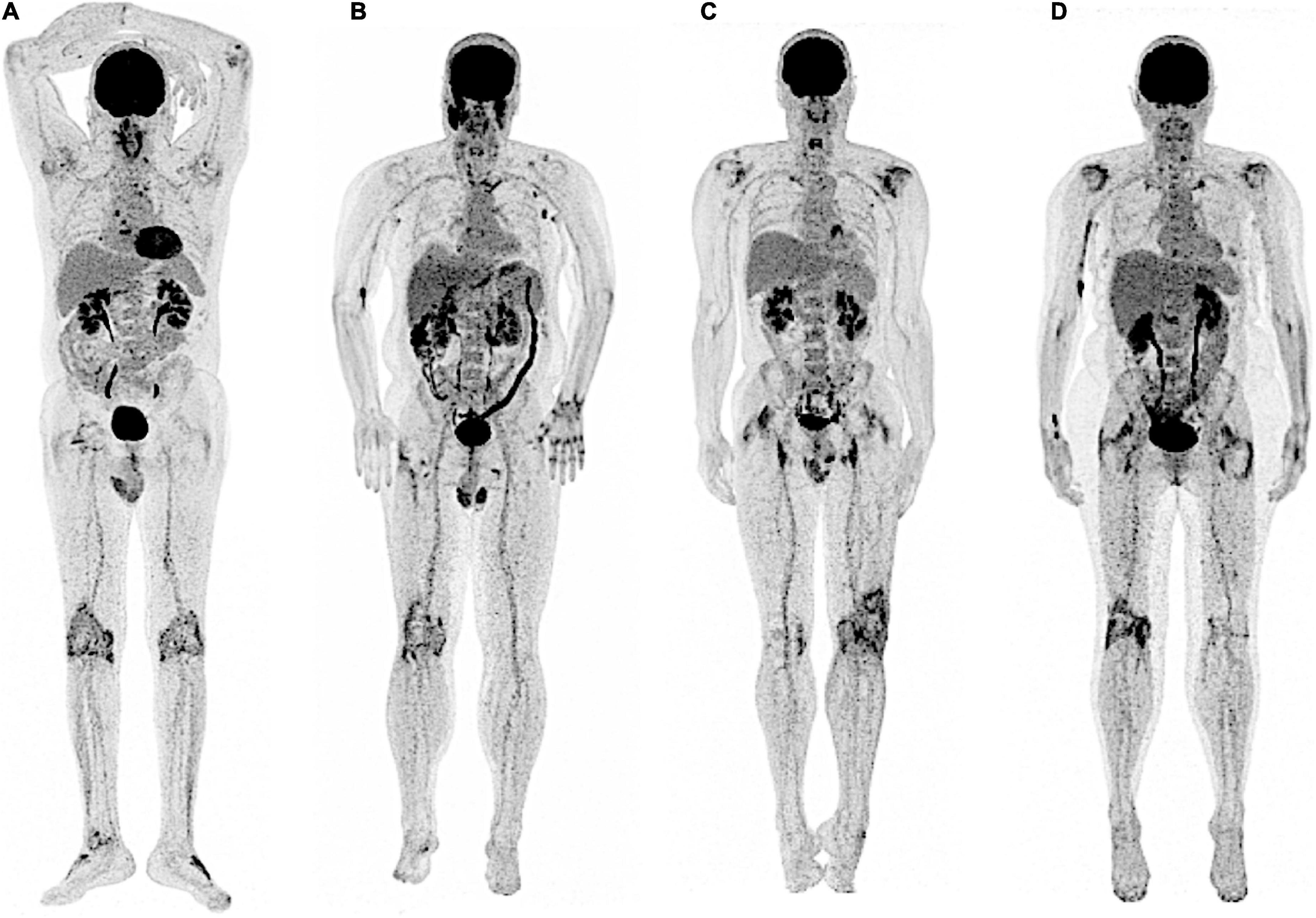
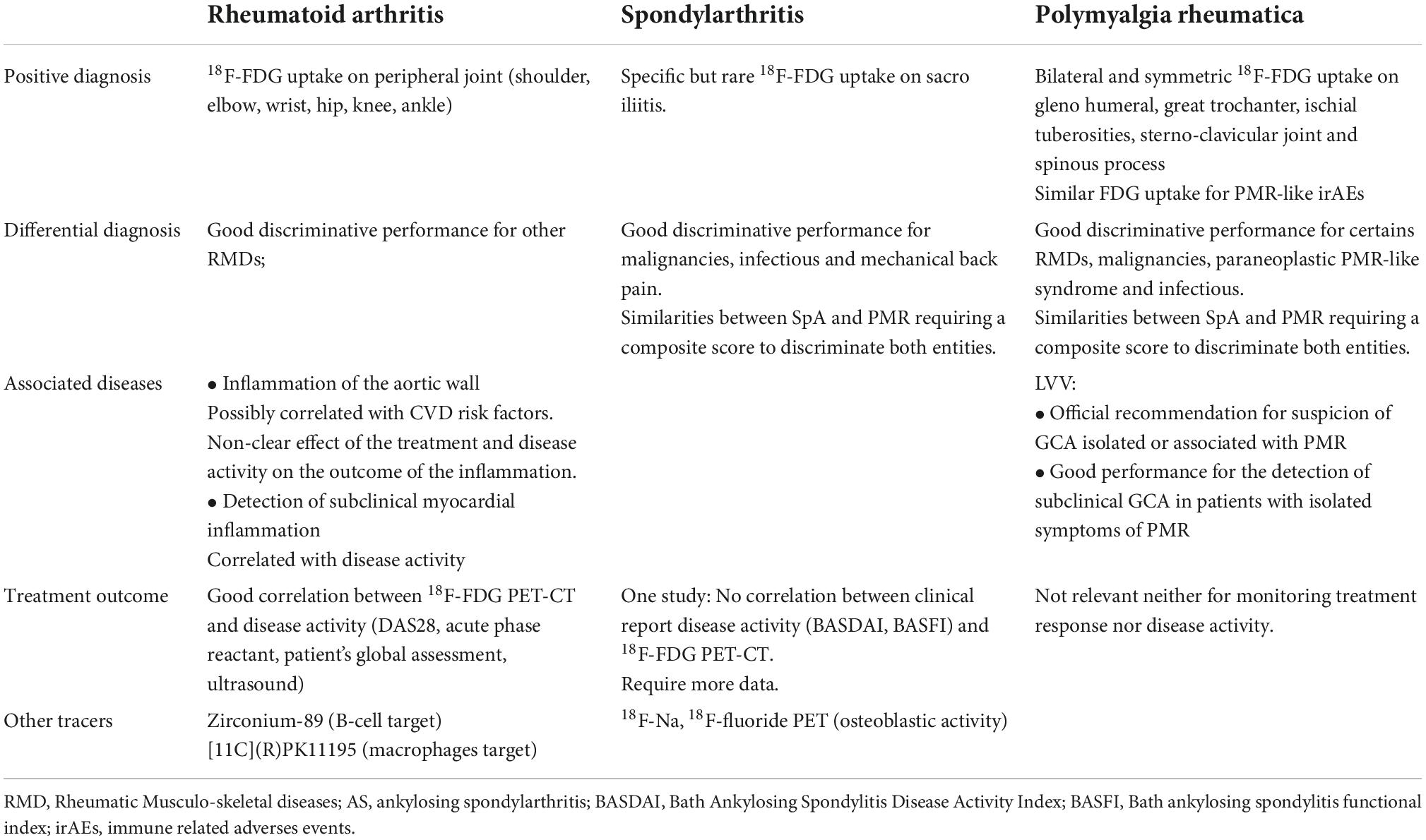
Figure 1. SpA and PMR: typical but non-specific periarticular patterns of 18F-FDG uptake at the individual whole-body level. In both SpA (A,B) and PMR (C,D), typical increase of 18F-FDG uptake is frequently observed in the scapular and pelvic girdles as illustrated here, but also at sterno-clavicular joints and interspinous processes. In both CIR, peripheric articular involvement (knees) may also be observed. Typical 18F-FDG PET findings are thus non-specific at the patient level.
The aim of this short review is to summarize the evidence-based literature on the benefits of 18F-FDG PET imaging in patients with CIR, focusing on rheumatoid arthritis (RA), spondyloarthritis (SpA) and polymyalgia rheumatica (PMR). Promising other radiotracers of interest in this field will also be discussed.
18F-FDG PET in rheumatoid arthritis
Rheumatoid arthritis is the most frequent CIR affecting 0.3–0.5% of the general population (9, 10). RA is characterized by an inflammation of synovial membrane (synovitis) resulting in bone erosion. The frequency of systemic manifestations seems to be decreasing apart from pulmonary involvement which affects about 20% of patients (11). According to the ACR/EULAR 2010 classification criteria (12), the diagnosis is based on clinical presentation and biological criteria [Acute-phase reactants, anti – cyclic citrullinated peptide2 antibodies (ACPA2) and/or rheumatoid factor (RF)]. Imaging by X-ray is required to look for structural damage (joint erosions).
Although 18F-FDG PET is not currently validated in this case, PET molecular imaging has demonstrated its diagnostic value in atypical and challenging cases. Bhattarai et al. (13) reported good performance of 18F-FDG PET combined with computed tomography (PET-CT) to discriminate 18 RA from 17 non-RA patients (SAPHO syndrome, IgG4 arthritis, psoriatic arthritis and non-specific arthritis). Compared to non-RA patients, RA patients had significantly higher metabolic visual score defined by the sum of the maximum standardized uptake value of each joint (shoulders, elbow, wrist, hip, knee, and ankle). In the same way, Yamashita et al. (14) demonstrated significant differences of 18F-FDG uptake on ischial tuberosity, great trochanter, spinous process, vertebral body and sacroiliac joint between RA, PMR, and SpA patients. Recently, Wang et al. (15) demonstrated that 18F-FDG PET could discriminate 54 suspected RA (n = 23) from PMR (n = 31) patient, based on interspinous uptake combined with rheumatoid factor (AUC = 0.892).
Concerning the assessment of disease activity, Lee et al. investigated 91 active and mainly treatment-naïve RA with a mean Disease activity score of 28, C – Reactive Protein (DAS28 CRP) of 6.4. While univariate analyses showed correlations between PET-positive joint and clinic-biological symptoms (the swollen joint and Tender Joint Counts, DAS28 CRP and Erythrocyte sedimentation rate), multivariate analyses confirmed a positive correlation between PET positive joint and DAS28 ESR and patient’s global disease score. Beckers et al. (16) supported these result and further demonstrated relationship between 18F-FDG PET and ultrasonography to detect inflamed joints. However, the use of PET-CT for this purpose of monitoring response to therapy in RA patients is not sound in clinical practice. The gold standard should be clinico-biological follow-up by DAS28 score and structural follow-up by X-ray.
As a prognosis marker in RA, few 18F-FDG PET studies have shown positive results. Roivainen et al. (17) have assessed the early predictive value of 18F-FDG PET in RA patients treated by Methotrexate/Salazopyrine/Hydroxychloroquine tri-therapy. In 17 RA patients, 18F-FDG-PET was performed at baseline, 2 and 4 weeks after the initiation of treatment. Interestingly, a decrease of disease activity on PET after 2 and 4 weeks of treatment correlated with DAS28 and CRP at 12 weeks. Elzinga et al. (18) supported these preliminary results with Infliximab, a monoclonal inhibitor of TNF, by showing a correlation between the early PET changes at 2 weeks and DAS28 at 14 and 22 weeks. Same performance was also reported with Tocilizumab, an interleukine – 6 inhibitor (19). To note, Bouman et al. did not supported this prognosis value in RA patients with low disease activity treated by TNF inhibitors (20). Again, the clinical usefulness arises. It would be useful to evaluate the economic cost and benefit-risk balance of performing 2 PET scans a few weeks apart in patients versus conventional clinical-biological monitoring.
Finally, the holistic nature of 18F-FDG as a biomarker of cellular metabolic activity makes 18F-FDG PET an intrinsic “swiss-knife” to evaluate multidimensional aspects of the same disease, even at a subclinical level. Due to vascular wall and/or systemic chronic inflammation condition, RA patients had an increased risk of cardiovascular diseases (CVD) (21, 22), up to 2–3-fold excess of mortality in comparison with general population (23). In their recent study, Geraldino-Pardilla et al. (22) showed in 91 RA patients without clinical evidence of CVD a significant relationship between 18F-FDG PET vascular uptake of the aortic wall and both CVD risk factors (arterial hypertension and body mass index) and RA disease features (rheumatoid nodules and Disease activity score) (22). In the same way, Trang et al. (24) showed in 64 RA patients increased 18F-FDG uptake of the aortic wall after 6 months of biologic therapies (TNF inhibitors, IL6 blockers and Ig CTLA4), even in RA patients with low disease activity or in clinical remission. Moreover, Amigues et al. reported subclinical myocardial 18F-FDG uptake in 39% of their 119 RA patients without known CVD (25). For 8 patients requiring an step-up of their treatment, the longitudinal follow-up showed substantial decrease of myocardial 18F-FDG uptake over 6 months, together with the clinical disease activity index. In a controlled study including 33 RA and age/gender matched controls with neither RA nor CVD, a significant correlation between synovial (acromioclavicular and acetabulo-femoral joints) and aortic 18F-FDG uptake was observed only in the RA group (26). These results are interesting. Nevertheless, it would be necessary to define the pathological value of vascular abnormalities in RA patients and to be able to determine whether their detection should result in therapeutic intervention.
In summary, there are abnormalities specific to RA on PET CT. However, it is not clear whether this examination has a place in the diagnostic or follow-up strategy of patients.
18F-FDG PET in spondylarthritis
Spondylarthritis is a composite spectrum of rheumatism disorders sharing common clinical and genetic features, including ankylosing spondylitis (AS), reactional arthritis, arthritis associated to bowel inflammatory diseases, psoriatic arthritis, undifferentiated SpA and Synovitis – Arthritis – Palmoplantar pustulosis - Hyperostosis – Osteitis syndrome (SAPHO). SpA affects 0.2 to 0.3% of the general population and typically concerns young males below 40 years old. Musculoskeletal manifestations include pelvic and axial inflammatory pain, peripheral joint involvement and enthesis (27). SpA had no specific biologic marker contrary to RA. Conventional radiography and ultrasonography typically lack of sensitivity (28). Magnetic resonance imaging (MRI) remains the gold standard to assess spine and sacroiliac joint (SIJ), SIJ involvement being critical according to the diagnostic criteria of the 2009 Assessment of Spondyloarthritis international Society classification (29).
Despite the lack of clinical validation, 18F-FDG PET-CT showed interesting results as a diagnostic tool in SpA (Figure 2). In a challenging clinical context mixing 21 SpA, 16 RA and 16 PMR patients, Yamashita et al. found higher 18F-FDG uptake in sacroiliac joint of SpA patients compared to other CIR (14). To note, only 60% of the sacroiliitis diagnosed with MRI were identified on PET-CT, and no inter-groups difference of 18F-FDG uptake was observed for the other joints (ischiatic tuberosity, greater trochanter, spinous process, and vertebral body). These data are supported by Strobel et al. (30) who found moderate diagnostic performance of 18F-FDG PET-CT to detect sacroiliitis in 28 patients with active AS (n = 15) or mechanical low back pain (MLBP, n = 13), especially for grades II (localized erosions or scleroses, no alteration in the joint width, Se = 40%) and IV (ankylosis, Sen = 50%). Recently, Pean de Ponfilly-Sotier et al. (31) evaluated 18F-FDG PET-CT in a particular population of 27 atypical SpA mixing late onset SpA patients, patients refractory to TNF inhibitors and/or with general manifestations. In this specific challenging population, 18F-FDG PET-CT showed rare but higher 18F-FDG uptake in SIJ compared to PMR patients. Other 18F-FDG uptake locations (ischial tuberosity, great trochanter, hips, shoulders, interspinous process) were significantly associated with PMR. At the patient level, 18F-FDG PET could not discriminate PMR from atypical SpA (Figure 1). In another study by Toussirot et al. (32), 18F-FDG PET-CT demonstrated a good concordance with MRI to detect sacroiliitis and spinal inflammatory lesions in AS. However, in non-radiographic axial SpA patient, 18F-FDG-PET-CT showed no metabolic activity and did not seem to be helpful in this specific population, suggesting 18F-FDG PET-CT to be relevant in patients with active SpA. In summary, PET CT may have value in the diagnostic approach to atypical presentations in patients with suspected SpA.

Figure 2. 18F-FDG PET of SpA. In SpA, sacro-iliitis is a highly specific pattern of 18F-FDG uptake, as illustrated here in the right sacro-iliac joint, but is rarely observed in practice. As for PMR, 18F-FDG uptake of the sterno-clavicular joints, scapular and pelvic girdles is also observed.
Monitoring the disease independently from the self-reported clinical score Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and Bath ankylosing spondylitis functional index (BASFI) remains an important issue in SpA. In this perspective, Wendling et al. evaluated three AS patients with 18F-FDG PET-CT at baseline and after 6–8 weeks of TNF inhibitors (33). No decrease in 18F-FDG uptake was observed under treatment, highlighting the need of further large cohort investigations in this particular field.
18F-FDG PET in polymyalgia rheumatica
Polymyalgia rheumatic (PMR) is an inflammatory disease of unknown origin affecting patients over 50 years old, causing arthromyalgia of the pelvic and/or scapular girdle, systemic manifestations and sometimes peripheral arthritis (34, 35). A biologic inflammatory syndrome is classical. As well as SpA, PMR has no specific biomarkers. The diagnosis is based on clinical and laboratory evidence and the exclusion of the numerous differential diagnosis (e.g., late onset SpA, rheumatoid arthritis with rhizomelic presentation, remittive symmetrical seronegative synovitis with pitting edema (RS3PE), inflammatory myositis ….) with plain radiography and exhaustive biologic tests. In 15 to 20% of cases, PMR is associated with giant cell arteritis (GCA), an inflammatory disease of the vascular wall of large arteries (Figure 3). Corticosteroids are the cornerstone of treatment both for GCA and PMR.
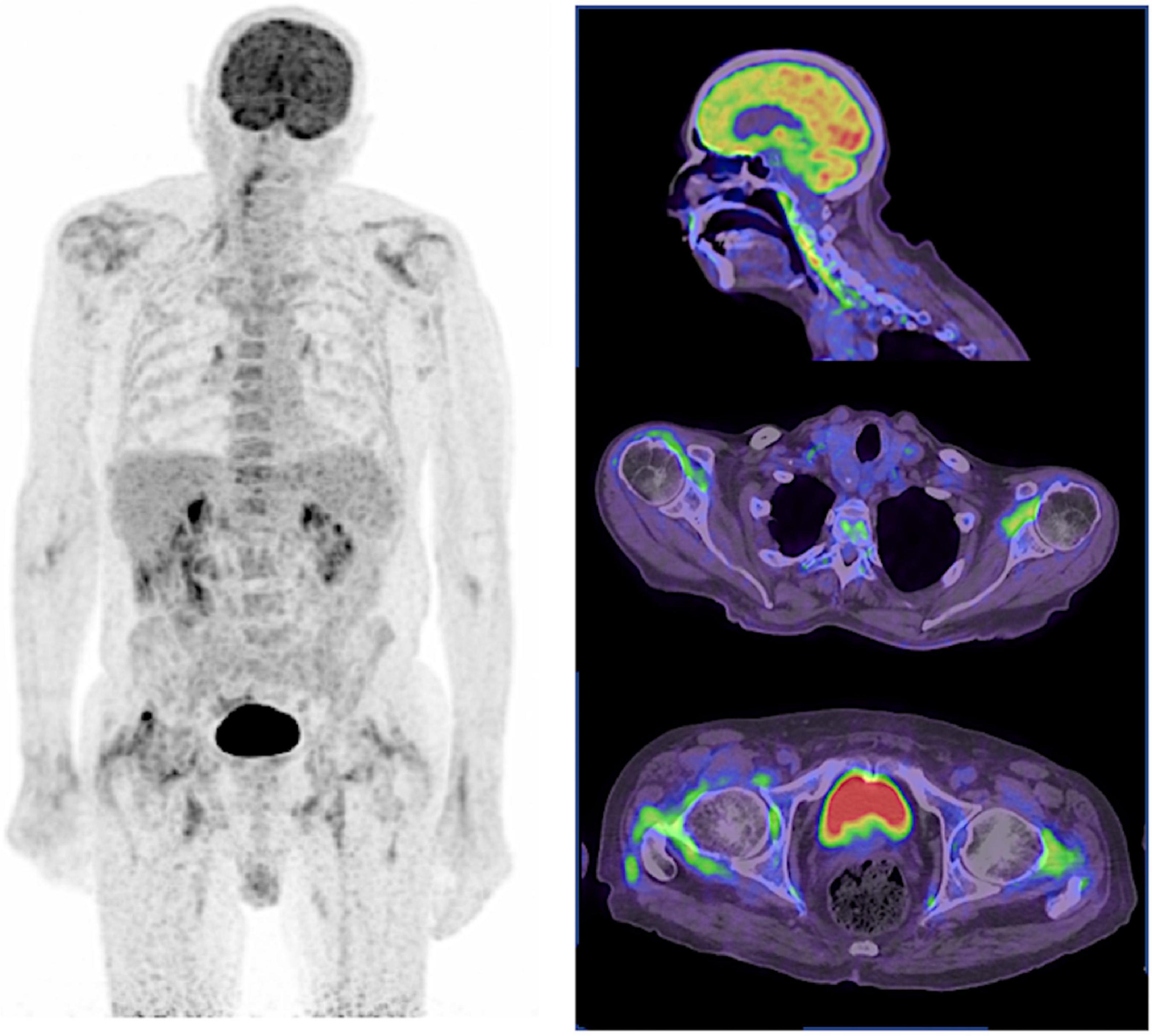
Figure 3. 18F-FDG PET of PMR. In PMR, active LVV frequently overlaps, as illustrated here with the long linear and smooth 18F-FDG uptake of the right vertebral artery in this corticosteroid resistant PMR patient. As for SpA, 18F-FDG uptake of the sterno-clavicular joints, scapular, and pelvic girdles is also typically observed.
Although 18F-FDG-PET-CT is not recommended to diagnose isolated PMR, 18F-FDG PET-CT is now indicated as a first line imaging procedure in the case of suspected GCA (3). Historically, Blockmans et al. were the first to apply 18F-FDG PET on isolated PMR patients (36). In their seminal paper, the authors reported the currently well-known reference pattern of 18F-FDG uptake in this RIC: a bilateral and symmetrical increase of 18F-FDG uptake in the shoulders and pelvic girdles, frequently associated with multi-tiered increase of 18F-FDG uptake of spinous process. During the last 15 years, several studies reported these typical 18F-FDG uptake, but also sternoclavicular joints (14, 31, 37). At the population level, the intensity of 18F-FDG uptake in these locations appears higher in PMR patients compared to RA, SpA and other inflammatory condition (38). A recent meta-analysis by van der Geest et al. showed that combining these targeted anatomic sites of 18F-FDG uptake improved the diagnosis performance of PET in PMR (37). These data were later confirmed by other studies (31, 39), highlighting the fact that 18F-FDG-PET-CT could be a relevant tool to discriminate PMR from other inflammatory rheumatisms, even in challenging case-mix populations. Steroid treatment prior to PET-CT reduces the scan’s ability to demonstrate inflammation in PMR patients. This should be kept in mind when interpreting PET-CT in patients already exposed to steroids (40). PMR-like syndrome have been reported in patients receiving immune check point inhibitors (ICIs) for cancers (41, 42). Rheumatic and Musculo-skeletal immune-related adverse events (irAes) often do not fulfill to the traditional classification criteria (42). Compared with classical PMR, PMR-like syndromes showed higher prevalence of peripheral arthritis and the biologic inflammation can be lacking (43). Previous report (44) and van der Geest et al. (45) assessed the role of 18F-FDG PET-CT before the initiation of corticosteroid in 6 patients with PMR – like syndrome. He found the same symmetric 18F-FDG uptake locations than those in classical PMR, without LVV associated. One third exhibited peripheral 18F-FDG uptake. These results were confirmed recently by Ponce et al. (44). To note, patients experienced irAEs induced by ICI had a better cancer prognosis than those in non – irAEs patients (46).
Monitoring the response to treatment with 18F-FDG PET-CT may be tempting (Figure 4). However, standard clinical and biological biomarkers are currently sufficient in most practical cases. Nevertheless, Palard-Novello et al. assessed the value of 18F-FDG PET-CT to monitor 18 PMR patients receiving Tocilizumab as first line treatment (TENOR trial) (47). The PET-CT were performed at baseline, two and 12 weeks. Between baseline and 12 weeks, the authors observed significant improvement of the PMR activity score and biological markers, together with a decrease of 18F-FDG uptake in targeted joints (hips, ischial tuberosity, lumbar spinous process). During follow-up, no correlation was found between PET, clinical and biological biomarkers. Devauchelle-Pensec et al. confirmed these results in a cohort of 20 glucocorticoid-free PMR onset receiving Tocilizumab as first line treatment (48). Thus 18F-FDG PET-CT may not appear relevant neither for monitoring treatment response nor disease activity in PMR patients.
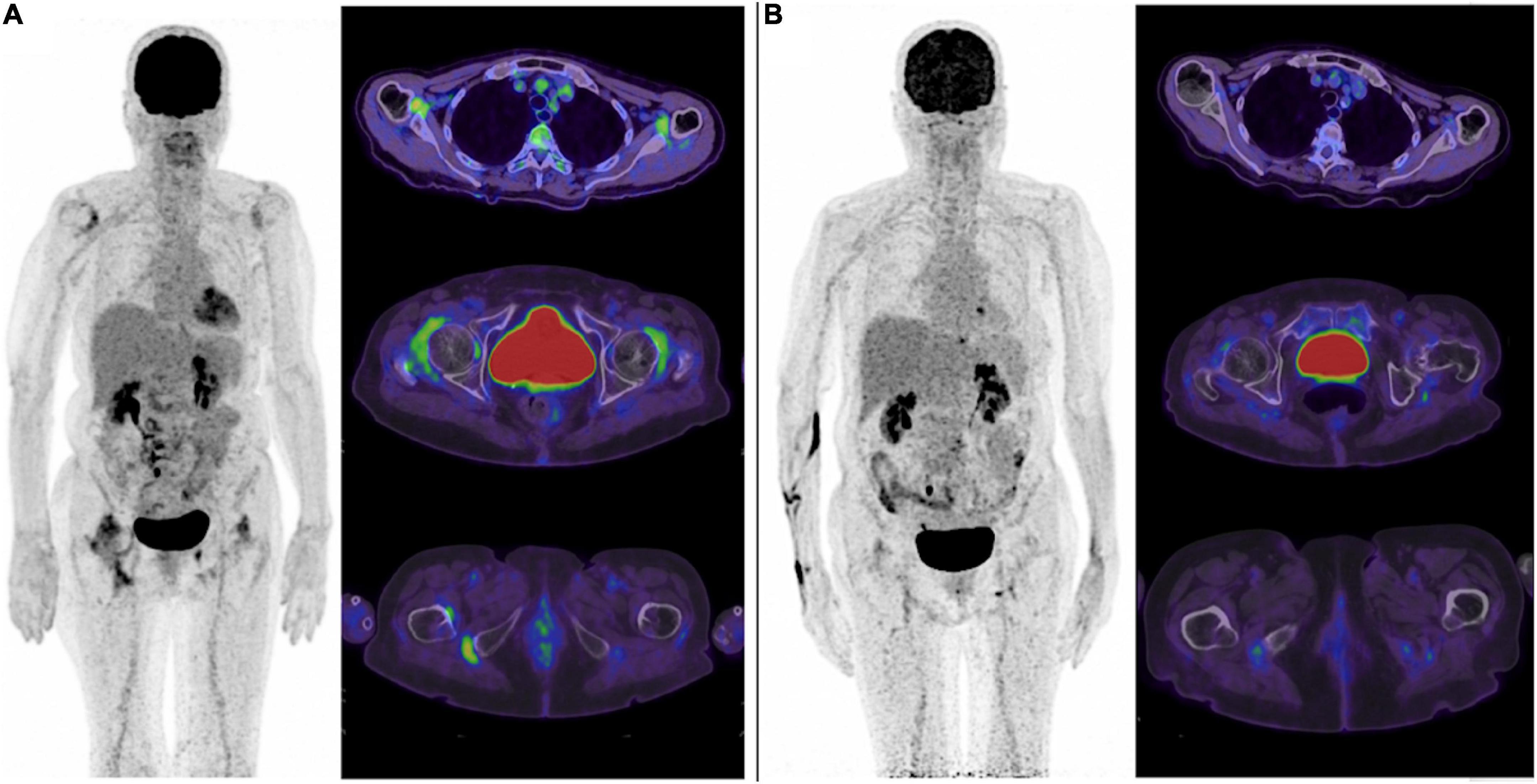
Figure 4. 18F-FDG PET changes under treatment: typical but no current benefit over standard biomarkers. In this case of PMR, significant decrease of 18F-FDG uptake is observed in the targeted joints (here the scapular and pelvic girdles, ischial tuberosities) under treatment (A) baseline scan, and (B) after several lines of treatment). Although metabolic changes assessed with 18F-FDG are frequently observed, the clinical benefit of such imaging biomarker over standard clinical and biological biomarkers for disease monitoring remains to be defined.
Whether 18F-FDG-PET-CT could be a relevant tool or not to predict response to treatment is poorly evaluated. In 2007, the seminal paper by Blockman et al. (36) found no difference of 18F-FDG uptake between relapsers and non-relapsers at 3 and 6 months, and 18F-FDG PET uptake was not correlated with the risk of relapse. In a recent study, Prieto-Peña et al. (49) identified predictive factor of 18F-FDG PET positivity for LVV in a population of 84 isolated PMR patient with persistent of classical PMR symptoms and/or unusual symptoms (inflammatory low back pain, diffuse lower limb pain). Among 84 patients, 51 (61%) patients had evidence of LVV on 18F-FDG PET. In multivariate analysis, diffuse lower limb pain, pelvic girdle pain and inflammatory low back pain were the best set of predictors of PET positivity for LVV in patients with initially isolated PMR. Finally, a take home message of this study is the potential existence of LVV signs in PMR patients in whom GCA was not clinically suspected. The presence of predictive signs could raise the question of systematically searching for GCA by PET CT given the therapeutic and prognostic impact. This work will therefore need to be confirmed in a new cohort. As mentioned previously, caution should be made in patients already exposed to glucocorticoids. Because glucocorticoids rapidly reduce the 18F-FDG uptake of the vascular wall in LVV patients, withdraw or delay therapy until after 18F-FDG PET when possible (i.e., no risk of ischemic complications) or 18F-FDG PET acquisition within the first days of therapy are currently recommended to reduce the risk of false negative results (4).
Finally, 18F-FDG PET could be used for differential diagnosis including cancers revealed by musculoskeletal manifestations including PMR-like symptoms. In this perspective, Moya-Alvarado et al. (50) assessed the added value of 18F-FDG PET-CT to diagnose other underlying conditions in a cohort of 103 onset and steroid resistant PMR patients. The final diagnosis of PMR, LVV, malignancies and other (small vessel vasculitis, osteoarthritis, elderly onset of RA, Sjögren’s syndrome) were retained in 73, 16, 5, and 9 patients, respectively. In the case of bio-clinical flare after glucocorticoid tapering in GCA patients with or without PMR, Camellino et al. promote the use of 18F-FDG PET-CT to rule-out cancer and detect subclinical LVV (35).
Time for new tracers?
PET imaging is characterized by its vectorized imaging capabilities. Beyond 18F-FDG we have focused on here, other tracers have been investigated in CIRs (51). In SpA, several studies reported the relevance of 18F-Na (18F-fluoride PET) to evaluate osteoblastic activity in chronic AS, and diagnose new bone formation in spine and SIJ which were misjudged by MRI and delayed by plain radiography (52–54). Son et al. (55) evaluated 18F-Na in a retrospective cohort of 68 patients with suspected AS. Among 68 patients, 72% reach ASAS criteria for SpA. Eighty percent in AS group exhibited higher frequency of 18F-Na uptake (enthesopathy, syndesmophyte, symmetric sacroiliitis), in comparison with the control group. In 2018, in a pilot study, Bruijnen et al. (53) suggested that AS activity was better reflected by bone activity assessed by 18F-Na than inflammation assessed by 18F-FDG and [11C](R)PK11195, a radiotracer of inflammation targeting the mitochondrial outer membrane translocator protein of activated macrophages (TSPO PET). In RA, TSPO PET radiotracers have also been assessed (56, 57). In their study including 29 RA patients without clinical arthritis, Gent et al. showed increased TSPO PET uptake in metacarpophalangeal, proximal interphalangeal, and wrist joints in 55% of cases, of whom 69% developed a flare within the 3-years of follow-up (56). More recently, the baseline PET assessment of B-cell load by using radiolabeled Rituximab (Zirconium-89) showed independent value of PET to prognose therapeutic response, with positive and negative predictive values for clinical response at 24 weeks of 90 and 75%, respectively (58).
To conclude, the place of 18F-PET-CT in the management of patients with RA, SpA and PMR remains to be defined. In classical presentations, 18F-FDG PET does not appear useful in the diagnostic process. It should be reserved for atypical presentations or in case of poor response to treatment in order to ensure the absence of a differential diagnosis. Its relevance for the assessment of associated manifestations - cardiovascular complications of RA - GCA associated with PMR appears promising, deserving dedicated lines of research. Finally, the use of new tracers is to be followed to improve the diagnostic and prognostic performance of this whole-body imaging modality.
Author contributions
All authors contributed to design and acquisition analysis, revising for intellectual content, final approval, and agreement to be accountable for all aspects of this work (accuracy and integrity of any part of the work).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
18F-FDG PET-CT, 18F-labeled fluorodeoxyglucose-positron emission tomography/computed tomography; CIR, chronic inflammatory rheumatism; RA, rheumatoid arthritis; SpAs, spondylarthris; PMR, polymyalgia rheumatica; ACPA2, anti – cyclic citrullinated peptide2 antibodies; RF, rheumatoid factor; SUVmax, maximum standardized uptake value; DAS28 CRP, Disease activity score 28 C – Reactive Protein; SJC, Swollen joint count; TJC, Tender Joint Count; CVD, cardiovascular diseases; RLDA, Remission or low disease activity; MHDA, Moderate or high disease activity; AS, ankylosing spondylitis; SAPHO, Synovitis – Arthritis – Palmoplantar pustulosis - Hyperostosis – Osteitis syndrome; SIJ, sacroiliac joint; MLBP, mechanical low back pain; BASDAI, Bath Ankylosing Spondylitis Disease Activity Index; BASFI, Bath ankylosing spondylitis functional index; ROC, Receiver Operating Characteristic Curve; MRI, Magnetic resonance imaging; AUC, Area Under the Curve; SpA, Spondylarthritis; TNFi, TNF inhibitors; PMR, Polymyalgia rheumatic; GCA, giant cell arteritis; LVV, Live vessel vasculitis; RS3PE, remittive symmetrical seronegative synovitis with pitting edema; ICIs, immune check point inhibitors; irAes, immune-related adverse events; RMDs, Rheumatologic and Musculo-skeletal Disorders.
References
1. Manhas NS, Salehi S, Joyce P, Guermazi A, Ahmadzadehfar H, Gholamrezanezhad A. PET/computed tomography scans and PET/MR imaging in the diagnosis and management of musculoskeletal diseases. PET Clin. (2020) 15:535–45. doi: 10.1016/j.cpet.2020.06.005
2. Mandl P, Ciechomska A, Terslev L, Baraliakos X, Conaghan PG, D’Agostino MA, et al. Implementation and role of modern musculoskeletal imaging in rheumatological practice in member countries of EULAR. RMD Open. (2019) 5:e000950. doi: 10.1136/rmdopen-2019-000950
3. Dejaco C, Ramiro S, Duftner C, Besson FL, Bley TA, Blockmans D, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann Rheum Dis. (2018) 77:636–43. doi: 10.1136/annrheumdis-2017-212649
4. Slart RHJA, Writing group, Reviewer group, Members of EANM Cardiovascular, Members of EANM Infection & Inflammation, Members of Committees,, et al. FDG-PET/CT(A) imaging in large vessel vasculitis and polymyalgia rheumatica: joint procedural recommendation of the EANM, SNMMI, and the PET Interest Group (PIG), and endorsed by the ASNC. Eur J Nucl Med Mol Imaging. (2018) 45:1250–69. doi: 10.1007/s00259-018-3973-8
5. Besson FL, Chaumet-Riffaud P, Playe M, Noel N, Lambotte O, Goujard C, et al. Contribution of (18)F-FDG PET in the diagnostic assessment of fever of unknown origin (FUO): a stratification-based meta-analysis. Eur J Nucl Med Mol Imaging. (2016) 43:1887–95. doi: 10.1007/s00259-016-3377-6
6. Colebatch AN, Edwards CJ, Østergaard M, van der Heijde D, Balint PV, D’Agostino MA, et al. EULAR recommendations for the use of imaging of the joints in the clinical management of rheumatoid arthritis. Ann Rheum Dis. (2013) 72:804–14. doi: 10.1136/annrheumdis-2012-203158
7. Yamashita H, Kubota K, Mimori A. Clinical value of whole-body PET/CT in patients with active rheumatic diseases. Arthritis Res Ther. (2014) 16:423. doi: 10.1186/s13075-014-0423-2
8. Kubota K, Yamashita H, Mimori A. Clinical value of FDG-PET/CT for the evaluation of rheumatic diseases: rheumatoid arthritis, polymyalgia rheumatica, and relapsing polychondritis. Semin Nucl Med. (2017) 47:408–24. doi: 10.1053/j.semnuclmed.2017.02.005
9. Smolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet. (2016) 388:2023–38. doi: 10.1016/S0140-6736(16)30173-8
10. Roux CH, Saraux A, Le Bihan E, Fardellone P, Guggenbuhl P, Fautrel B, et al. Rheumatoid arthritis and spondyloarthropathies: geographical variations in prevalence in France. J Rheumatol. (2007) 34:117–22.
11. Juge PA, Granger B, Debray MP, Ebstein E, Louis-Sidney F, Kedra J, et al. A risk score to detect subclinical rheumatoid arthritis-associated interstitial lung disease. Arthritis Rheumatol. (2022) 74:1755–65. doi: 10.1002/art.42162
12. Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO, et al. 2010 Rheumatoid arthritis classification criteria: an American college of rheumatology/European league against rheumatism collaborative initiative. Arthritis Rheum. (2010) 62:2569–81. doi: 10.1002/art.27584
13. Bhattarai A, Nakajima T, Sapkota S, Arisaka Y, Tokue A, Yonemoto Y, et al. Diagnostic value of 18F-fluorodeoxyglucose uptake parameters to differentiate rheumatoid arthritis from other types of arthritis. Medicine. (2017) 96:e7130. doi: 10.1097/MD.0000000000007130
14. Yamashita H, Kubota K, Takahashi Y, Minamimoto R, Morooka M, Kaneko H, et al. Similarities and differences in fluorodeoxyglucose positron emission tomography/computed tomography findings in spondyloarthropathy, polymyalgia rheumatica and rheumatoid arthritis. Joint Bone Spine. (2013) 80:171–7. doi: 10.1016/j.jbspin.2012.04.006
15. Wang G, Liu X, Chen J, Zhang F, Xu X, Wang Y, et al. The combination of 18F-fluorodeoxyglucose positron emission tomography metabolic and clinical parameters can effectively distinguish rheumatoid arthritis and polymyalgia rheumatic. Contrast Media Mol Imaging. (2022) 2022:9614678. doi: 10.1155/2022/9614678
16. Beckers C, Ribbens C, André B, Marcelis S, Kaye O, Mathy L, et al. Assessment of disease activity in rheumatoid arthritis with (18)F-FDG PET. J Nucl Med. (2004) 45:956–64.
17. Roivainen A, Hautaniemi S, Möttönen T, Nuutila P, Oikonen V, Parkkola R, et al. Correlation of 18F-FDG PET/CT assessments with disease activity and markers of inflammation in patients with early rheumatoid arthritis following the initiation of combination therapy with triple oral antirheumatic drugs. Eur J Nucl Med Mol Imaging. (2013) 40:403–10. doi: 10.1007/s00259-012-2282-x
18. Elzinga EH, van der Laken CJ, Comans EFI, Boellaard R, Hoekstra OS, Dijkmans BAC, et al. 18F-FDG PET as a tool to predict the clinical outcome of infliximab treatment of rheumatoid arthritis: an explorative study. J Nucl Med. (2011) 52:77–80. doi: 10.2967/jnumed.110.076711
19. Okamura K, Yonemoto Y, Okura C, Higuchi T, Tsushima Y, Takagishi K. Evaluation of tocilizumab therapy in patients with rheumatoid arthritis based on FDG-PET/CT. BMC Musculoskelet Disord. (2014) 15:393. doi: 10.1186/1471-2474-15-393
20. Bouman CAM, van Herwaarden N, Blanken AB, Van der Laken CJ, Gotthardt M, Oyen WJG, et al. 18F-FDG PET-CT in rheumatoid arthritis patients tapering TNFi: reliability, validity and predictive value. Rheumatology. (2022) 61:SI6–13. doi: 10.1093/rheumatology/keab842
21. Alavi A, Saboury B, Nardo L, Zhang V, Wang M, Li H, et al. Potential and most relevant applications of total body PET/CT imaging. Clin Nucl Med. (2022) 47:43–55. doi: 10.1097/RLU.0000000000003962
22. Geraldino-Pardilla L, Zartoshti A, Bag Ozbek A, Giles JT, Weinberg R, Kinkhabwala M, et al. Arterial inflammation detected with 18 F-fluorodeoxyglucose-positron emission tomography in rheumatoid arthritis. Arthritis Rheumatol. (2018) 70:30–9. doi: 10.1002/art.40345
23. Avina-Zubieta JA, Thomas J, Sadatsafavi M, Lehman AJ, Lacaille D. Risk of incident cardiovascular events in patients with rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis. (2012) 71:1524–9. doi: 10.1136/annrheumdis-2011-200726
24. Trang DAMT, Okamura K, Suto T, Sakane H, Yonemoto Y, Nakajima T, et al. Do biologic therapies reduce aortic inflammation in rheumatoid arthritis patients? Arthritis Res Ther. (2021) 23:206. doi: 10.1186/s13075-021-02585-w
25. Amigues I, Tugcu A, Russo C, Giles JT, Morgenstein R, Zartoshti A, et al. Myocardial inflammation, measured using 18-fluorodeoxyglucose positron emission tomography with computed tomography, is associated with disease activity in rheumatoid arthritis. Arthritis Rheumatol. (2019) 71:496–506. doi: 10.1002/art.40771
26. Emami H, Vijayakumar J, Subramanian S, Vucic E, Singh P, MacNabb MH, et al. Arterial 18F-FDG uptake in rheumatoid arthritis correlates with synovial activity. JACC Cardiovasc Imaging. (2014) 7:959–60. doi: 10.1016/j.jcmg.2014.03.018
27. Taurog JD, Chhabra A, Colbert RA. Ankylosing spondylitis and axial spondyloarthritis. N Engl J Med. (2016) 374:2563–74. doi: 10.1056/NEJMra1406182
28. van Tubergen AM, Landewé RBM. Tools for monitoring spondyloarthritis in clinical practice. Nat Rev Rheumatol. (2009) 5:608–15. doi: 10.1038/nrrheum.2009.207
29. Rudwaleit M, van der Heijde D, Landewé R, Akkoc N, Brandt J, Chou CT, et al. The assessment of spondyloarthritis international society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann Rheum Dis. (2011) 70:25–31. doi: 10.1136/ard.2010.133645
30. Strobel K, Fischer DR, Tamborrini G, Kyburz D, Stumpe KDM, Hesselmann RGX, et al. 18F-fluoride PET/CT for detection of sacroiliitis in ankylosing spondylitis. Eur J Nucl Med Mol Imaging. (2010) 37:1760–5. doi: 10.1007/s00259-010-1464-7
31. Pean de Ponfilly-Sotier M, Besson FL, Gomez L, Ottaviani S, Dieudé P, Pavy S, et al. Use of 18F FDG PET-CT to discriminate polymyalgia rheumatica and atypical spondylarthritis in clinical practice. Joint Bone Spine. (2022) 89:105325.
32. Toussirot E, Caoduro C, Ungureanu C, Michel F, Runge M, Boulahdour H. 18F- fluoride PET/CT assessment in patients fulfilling the clinical arm of the ASAS criteria for axial spondyloarthritis. A comparative study with ankylosing spondylitis. Clin Exp Rheumatol. (2015) 33:588.
33. Wendling D, Blagosklonov O, Streit G, Lehuédé G, Toussirot E, Cardot JC. FDG-PET/CT scan of inflammatory spondylodiscitis lesions in ankylosing spondylitis, and short term evolution during anti-tumour necrosis factor treatment. Ann Rheum Dis. (2005) 64:1663–5. doi: 10.1136/ard.2005.040345
34. Salvarani C, Cantini F, Boiardi L, Hunder GG. Polymyalgia rheumatica and giant-cell arteritis. N Engl J Med. (2002) 347:261–71. doi: 10.1056/NEJMra011913
35. Camellino D, Matteson EL, Buttgereit F, Dejaco C. Monitoring and long-term management of giant cell arteritis and polymyalgia rheumatica. Nat Rev Rheumatol. (2020) 16:481–95. doi: 10.1038/s41584-020-0458-5
36. Blockmans D, De Ceuninck L, Vanderschueren S, Knockaert D, Mortelmans L, Bobbaers H. Repetitive 18-fluorodeoxyglucose positron emission tomography in isolated polymyalgia rheumatica: a prospective study in 35 patients. Rheumatology. (2007) 46:672–7. doi: 10.1093/rheumatology/kel376
37. van der Geest KSM, Treglia G, Glaudemans AWJM, Brouwer E, Jamar F, Slart RHJA, et al. Diagnostic value of [18F]FDG-PET/CT in polymyalgia rheumatica: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging. (2021) 48:1876–89. doi: 10.1007/s00259-020-05162-6
38. Yuge S, Nakatani K, Yoshino K, Koyama T. Diagnosing polymyalgia rheumatica on 18F-FDG PET/CT: typical uptake patterns. Ann Nucl Med. (2018) 32:573–7. doi: 10.1007/s12149-018-1269-5
39. van der Geest KSM, van Sleen Y, Nienhuis P, Sandovici M, Westerdijk N, Glaudemans AWJM, et al. Comparison and validation of FDG-PET/CT scores for polymyalgia rheumatica. Rheumatology. (2022) 61:1072–82. doi: 10.1093/rheumatology/keab483
40. Lund Petersen A, Voss A, Laustrup H. PET-CT findings in patients with polymylagia rheumatica without symptoms of cranial ischaemia. Dan Med J. (2017) 64:A5410.
41. Braaten TJ, Brahmer JR, Forde PM, Le D, Lipson EJ, Naidoo J, et al. Immune checkpoint inhibitor-induced inflammatory arthritis persists after immunotherapy cessation. Ann Rheum Dis. (2020) 79:332–8. doi: 10.1136/annrheumdis-2019-216109
42. Kostine M, Finckh A, Bingham CO, Visser K, Leipe J, Schulze-Koops H, et al. EULAR points to consider for the diagnosis and management of rheumatic immune-related adverse events due to cancer immunotherapy with checkpoint inhibitors. Ann Rheum Dis. (2021) 80:36–48. doi: 10.1136/annrheumdis-2020-217139
43. Martin de Fremont G, Belkhir R, Henry J, Voisin AL, Lambotte O, Besson FL, et al. Features of polymyalgia rheumatica-like syndrome after immune checkpoint inhibitor therapy. Ann Rheum Dis. (2022) 81:e52. doi: 10.1136/annrheumdis-2020-217225
44. Ponce A, Frade-Sosa B, Sarmiento-Monroy JC, Sapena N, Ramírez J, Azuaga AB, et al. Imaging findings in patients with immune checkpoint inhibitor-induced arthritis. Diagnostics. (2022) 12:1961. doi: 10.3390/diagnostics12081961
45. van der Geest KSM, Sandovici M, Rutgers A, Hiltermann TJN, Oosting SF, Slart RHJA, et al. Management of immune checkpoint inhibitor-induced polymyalgia rheumatica. Ann Rheum Dis. (2020) 81:e263. doi: 10.1136/annrheumdis-2020-218276
46. Zhong L, Wu Q, Chen F, Liu J, Xie X. Immune-related adverse events: promising predictors for efficacy of immune checkpoint inhibitors. Cancer Immunol Immunother. (2021) 70:2559–76. doi: 10.1007/s00262-020-02803-5
47. Palard-Novello X, Querellou S, Gouillou M, Saraux A, Marhadour T, Garrigues F, et al. Value of (18)F-FDG PET/CT for therapeutic assessment of patients with polymyalgia rheumatica receiving tocilizumab as first-line treatment. Eur J Nucl Med Mol Imaging. (2016) 43:773–9. doi: 10.1007/s00259-015-3287-z
48. Devauchelle-Pensec V, Berthelot JM, Cornec D, Renaudineau Y, Marhadour T, Jousse-Joulin S, et al. Efficacy of first-line tocilizumab therapy in early polymyalgia rheumatica: a prospective longitudinal study. Ann Rheum Dis. (2016) 75:1506–10. doi: 10.1136/annrheumdis-2015-208742
49. Prieto-Peña D, Martínez-Rodríguez I, Loricera J, Banzo I, Calderón-Goercke M, Calvo-Río V, et al. Predictors of positive 18F-FDG PET/CT-scan for large vessel vasculitis in patients with persistent polymyalgia rheumatica. Semin Arthritis Rheum. (2019) 48:720–7. doi: 10.1016/j.semarthrit.2018.05.007
50. Moya-Alvarado P, Fernandez Leon A, Corica ME, Camacho Marti V, López-Mora DA, Castellví I, et al. The added value of 18f-FDG PET/CT in the assessment of onset and steroid resistant polimyalgia rheumatica. PLoS One. (2021) 16:e0255131. doi: 10.1371/journal.pone.0255131
51. van der Krogt JMA, van Binsbergen WH, van der Laken CJ, Tas SW. Novel positron emission tomography tracers for imaging of rheumatoid arthritis. Autoimmun Rev. (2021) 20:102764. doi: 10.1016/j.autrev.2021.102764
52. Idolazzi L, Salgarello M, Gatti D, Viapiana O, Vantaggiato E, Fassio A, et al. 18F-fluoride PET/CT for detection of axial involvement in ankylosing spondylitis: correlation with disease activity. Ann Nucl Med. (2016) 30:430–4. doi: 10.1007/s12149-016-1080-0
53. Bruijnen STG, van der Weijden MAC, Klein JP, Hoekstra OS, Boellaard R, van Denderen JC, et al. Bone formation rather than inflammation reflects ankylosing spondylitis activity on PET-CT: a pilot study. Arthritis Res Ther. (2012) 14:R71. doi: 10.1186/ar3792
54. Raynal M, Bouderraoui F, Ouichka R, Melchior J, Morel O, Blum A, et al. Performance of 18F-sodium fluoride positron emission tomography with computed tomography to assess inflammatory and structural sacroiliitis on magnetic resonance imaging and computed tomography, respectively, in axial spondyloarthritis. Arthritis Res Ther. (2019) 21:119. doi: 10.1186/s13075-019-1903-1
55. Son SM, Kim K, Pak K, Kim SJ, Goh TS, Lee JS. Evaluation of the diagnostic performance of 18F-NaF positron emission tomography/computed tomography in patients with suspected ankylosing spondylitis according to the assessment of spondyloarthritis international society criteria. Spine J. (2020) 20:1471–9. doi: 10.1016/j.spinee.2020.03.011
56. Gent YYJ, Ahmadi N, Voskuyl AE, Hoetjes N, van Kuijk C, Britsemmer K, et al. Detection of subclinical synovitis with macrophage targeting and positron emission tomography in patients with rheumatoid arthritis without clinical arthritis. J Rheumatol. (2014) 41:2145–52. doi: 10.3899/jrheum.140059
57. Bruijnen STG, Verweij NJF, Gent YYJ, Huisman MC, Windhorst AD, Kassiou M, et al. Imaging disease activity of rheumatoid arthritis by macrophage targeting using second generation translocator protein positron emission tomography tracers. PLoS One. (2019) 14:e0222844. doi: 10.1371/journal.pone.0222844
58. Bruijnen S, Tsang-A-Sjoe M, Raterman H, Ramwadhdoebe T, Vugts D, van Dongen G, et al. B-cell imaging with zirconium-89 labelled rituximab PET-CT at baseline is associated with therapeutic response 24 weeks after initiation of rituximab treatment in rheumatoid arthritis patients. Arthritis Res Ther. (2016) 18:266. doi: 10.1186/s13075-016-1166-z
Keywords: 18F-FDG, PET, rheumatoid arthritis, spondylarthropathy, polymyalgia rheumatica
Citation: Pean De Ponfilly – Sotier M, Seror R, Nocturne G and Besson FL (2022) 18F-FDG PET molecular imaging: A relevant tool to investigate chronic inflammatory rheumatisms in clinical practice? Front. Med. 9:1070445. doi: 10.3389/fmed.2022.1070445
Received: 14 October 2022; Accepted: 15 November 2022;
Published: 30 November 2022.
Edited by:
Giorgio Treglia, Ente Ospedaliero Cantonale (EOC), SwitzerlandReviewed by:
Ryogo Minamimoto, National Center For Global Health and Medicine, JapanCopyright © 2022 Pean De Ponfilly – Sotier, Seror, Nocturne and Besson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gaetane Nocturne, Z2FldGFuZS5ub2N0dXJuZUBhcGhwLmZy; Florent L. Besson, ZmxvcmVudC5iZXNzb25AYXBocC5mcg==
†These authors share last authorship
 Marie Pean De Ponfilly – Sotier
Marie Pean De Ponfilly – Sotier Raphaële Seror1,2,3
Raphaële Seror1,2,3 Gaetane Nocturne
Gaetane Nocturne Florent L. Besson
Florent L. Besson