- 1Department of Orthopedics, Taichung Veterans General Hospital, Taichung, Taiwan
- 2Department of Post-Baccalaureate Medicine, College of Medicine, National Chung Hsing University, Taichung, Taiwan
- 3Department of Computer Science and Information Engineering, Providence University, Taichung, Taiwan
- 4Department of Rehabilitation Science, Jenteh Junior College of Medicine, Nursing and Management, Miaoli, Taiwan
- 5Division of Endocrinology and Metabolism, Department of Internal Medicine, Taichung Veterans General Hospital, Taichung, Taiwan
- 6Ph.D. Program in Translational Medicine, National Chung Hsing University, Taichung, Taiwan
- 7Department of Food Science and Technology, Hung Kuang University, Taichung, Taiwan
Purpose: We investigated the association between pre-operative anemia and long-term all-cause mortality in patients with vertebral fracture who underwent a vertebroplasty.
Materials and methods: We retrospectively selected patients who were admitted for vertebroplasty for vertebral compression fracture between 2013 and 2020. Patients who had pathologic fractures or had no assessment of bone mineral density were excluded. Relevant information was collected from electronic medical records. Patients’ survival status was confirmed at the end of March 2021. Cox-proportional hazard models were conducted to examine the effects of anemia (<12 g/dL vs. ≥12 g/dL) and pre-operative hemoglobin levels (as a continuous variable) on all-cause mortality with multivariate adjustments.
Results: A total of 167 patients were analyzed (mean age 75.8 ± 9.3 years, male 25.7%). After a median follow-up duration of 2.1 years, pre-operative anemia (hemoglobin <12 g/dL vs. ≥12 g/dL) was independently associated with a higher risk of all-cause mortality (hazard ratio 2.762, 95% CI 1.184 to 6.442, p = 0.019). An increase in pre-operative hemoglobin was associated with a lower risk of all-cause mortality after multivariate adjustment (hazard ratio 0.775, 95% CI 0.606 to 0.991, p = 0.042).
Conclusion: Pre-operative anemia (<12 g/dL) was independently associated with survival outcome among patients with vertebral compression fractures who underwent vertebroplasty. Our findings highlight anemia as a risk factor of long-term mortality in this elderly surgical population.
Introduction
Osteoporotic vertebral compression fracture is common in elderly populations (1, 2). Moreover, symptomatic vertebral compression fracture is associated with an increase in mortality risk (3) and an impairment of quality of life (4). These may result in substantial healthcare expenditures (5). Patients with persistent symptoms despite medical treatment are often treated with vertebroplasty, which has become a common orthopedic procedure. However, its effects on symptom relief, functional outcomes, and risk of mortality in the elderly are not yet clear (6–8).
Older aged individuals often have multiple morbidities which may further increase their susceptibility to post-operative complications and risk of long-term mortality. For example, anemia is prevalent in elderly people, especially hospitalized patients (9). Furthermore, anemia is an independent risk factor for all-cause mortality in people aged ≥65 years (10). Pre-operative anemia (defined as a hemoglobin <12 g/dL) has been associated with a higher risk of short-term mortality in patients with hip fracture (mortality within 60 days) (11) and in those who underwent primary total knee arthroplasty (mortality within 30 days) (12).
Given that anemia is frequently observed in elderly inpatients (9), and in light of the fact that patients who undergo vertebroplasty are often aged more than 70 years (13), pre-operative anemia might have an effect on long-term outcomes in this population. In this study, we investigated the association between pre-operative anemia and long-term all-cause mortality in patients with vertebral fracture who underwent vertebroplasty.
Materials and methods
This study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the Institutional Review Board of Taichung Veterans General Hospital, Taichung, Taiwan (approval number: CE22167A). We retrospectively selected patients who presented to our Department of Orthopedics with a vertebral compression fracture between 2013 and 2020. These patients were admitted for a vertebroplasty after pre-operative assessment. We excluded patients who had pathologic fractures or history of blood transfusion within 3 months, and those with no assessment of bone mineral density from the analysis. Pathological fractures were confirmed by pathological reports and discharge diagnosis. The requirement for informed consent was waived due to the retrospective study design.
We collected relevant information, including anthropometric data, medical history, and laboratory test results, from electronic medical records. Patients’ survival status was confirmed at the end of March 2021 using data obtained from the Ministry of Health and Welfare, R.O.C. Thereafter, de-identified data were used for analyses. Hemoglobin levels were measured as a routine pre-operative assessment. The study population was divided into two groups according to their pre-operative hemoglobin levels (<12 g/dL vs. ≥12 g/dL) to examine the association between pre-operative anemia and long-term all-cause mortality. The cutoff value 12 g/dL was determined because that it is the lower limit of normal, and a hemoglobin level less than 12 g/dL has been associated with risk of mortality in patients receiving an orthopedic surgery (11, 12, 14).
Statistical analysis
We conducted the statistical analyses using the Statistical Package for the Social Sciences (IBM SPSS version 22.0; International Business Machines Corp., NY, USA). Categorical and continuous variables were examined for statistically significant between-group differences using the chi-square test and independent t-test, respectively. Kaplan–Meier survival curves were plotted for the study population according to their pre-operative hemoglobin levels (<12 g/dL vs. ≥12 g/dL). Cox-proportional hazard models were conducted to examine the effects of anemia (<12 g/dL vs. ≥12 g/dL) and pre-operative hemoglobin levels (as a continuous variable) on all-cause mortality with adjustments for age, sex, and concomitant chronic diseases. Cubic spline of pre-operative hemoglobin levels vs. risk of all-cause mortality by a Cox proportional hazards model was conducted as a sensitivity test. A two-sided p-value of less than 0.05 was considered statistical significance.
Results
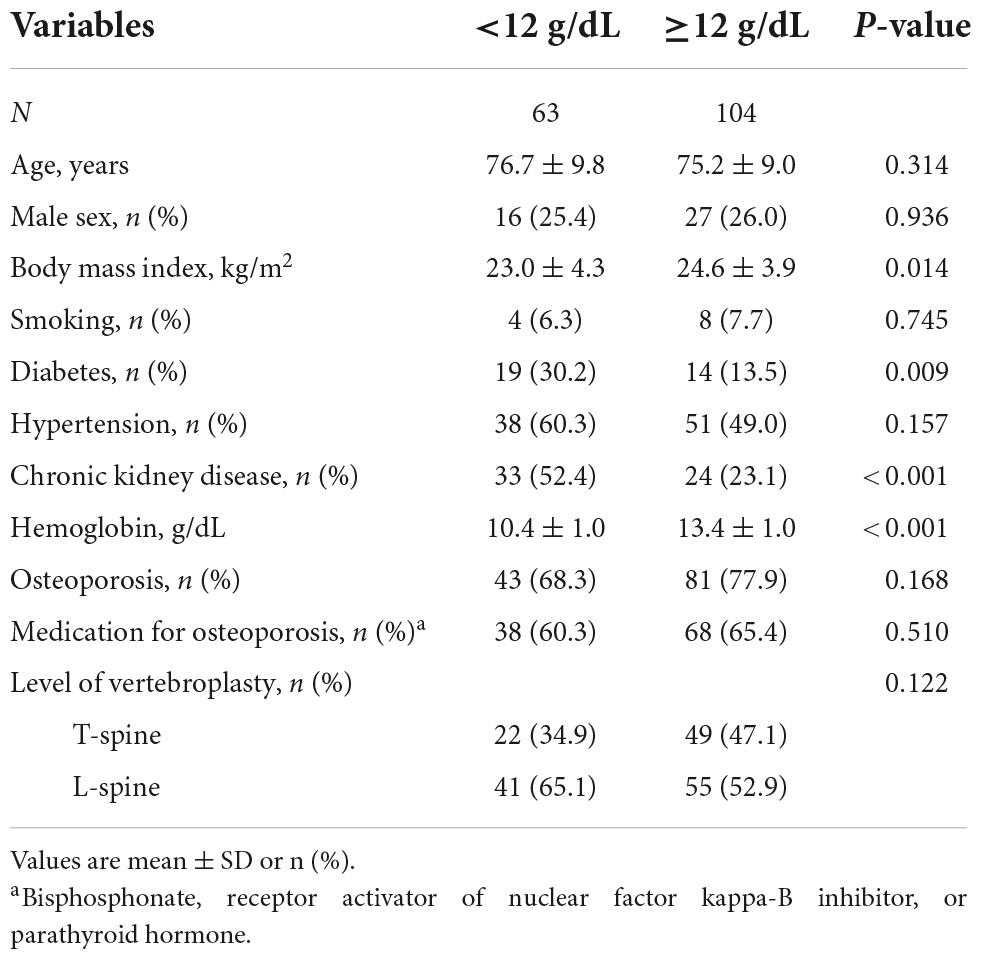
A total of 167 patients were analyzed (mean age 75.8 ± 9.3 years, male 25.7%). Table 1 shows the characteristics of the study population according to their pre-operative hemoglobin levels (<12 g/dL vs. ≥12 g/dL). Patients who had a pre-operative hemoglobin <12 g/dL (mean 10.4 ± 1.0 g/dL) had a lower body mass index (23.0 ± 4.3 vs. 24.6 ± 3.9 kg/m2, p = 0.014), and a higher proportion of diabetes (30.2 vs. 13.5%, p = 0.009) and chronic kidney disease (52.4 vs. 23.1%, p < 0.001), compared with those who had a pre-operative hemoglobin ≥12 g/dL (mean 13.4 ± 1.0 g/dL). There were no significant between-group differences in the other variables.
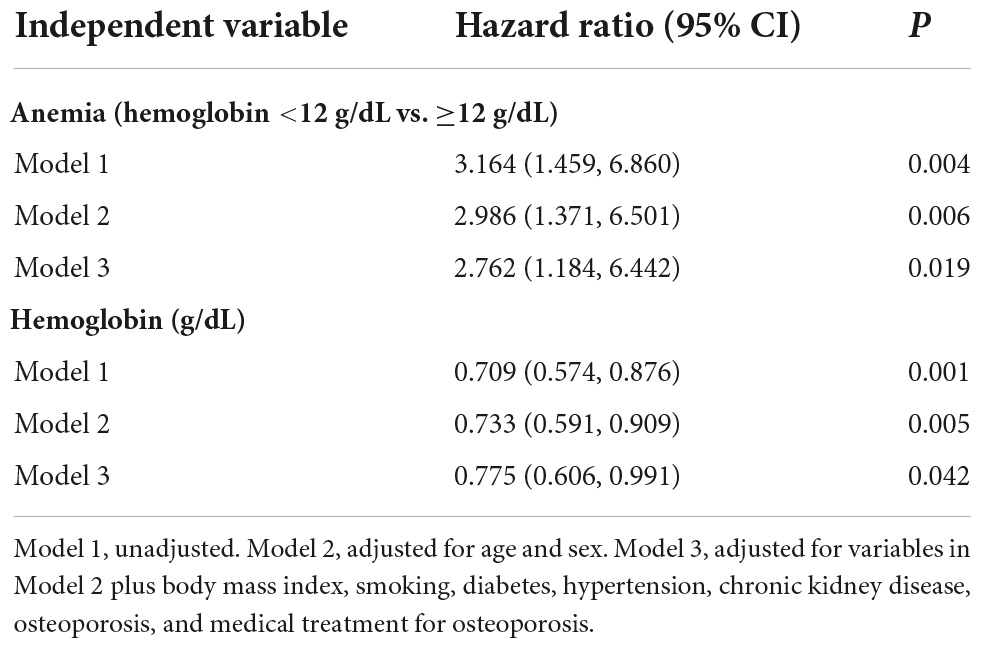
After a median follow-up duration of 2.1 years, patients with a pre-operative hemoglobin <12 g/dL had a lower survival rate than those who had a pre-operative hemoglobin ≥12 g/dL (Figure 1, Log-rank p = 0.002). The associations of pre-operative anemia (hemoglobin <12 g/dL vs. ≥12 g/dL) and hemoglobin levels with all-cause mortality are shown in Table 2. Pre-operative anemia (hemoglobin <12 g/dL vs. ≥12 g/dL) was associated with a significantly higher risk of all-cause mortality (hazard ratio 3.164, 95% CI 1.459 to 6.860, p = 0.004). This association remained significant after multivariate adjustment (hazard ratio 2.762, 95% CI 1.184 to 6.442, p = 0.019).
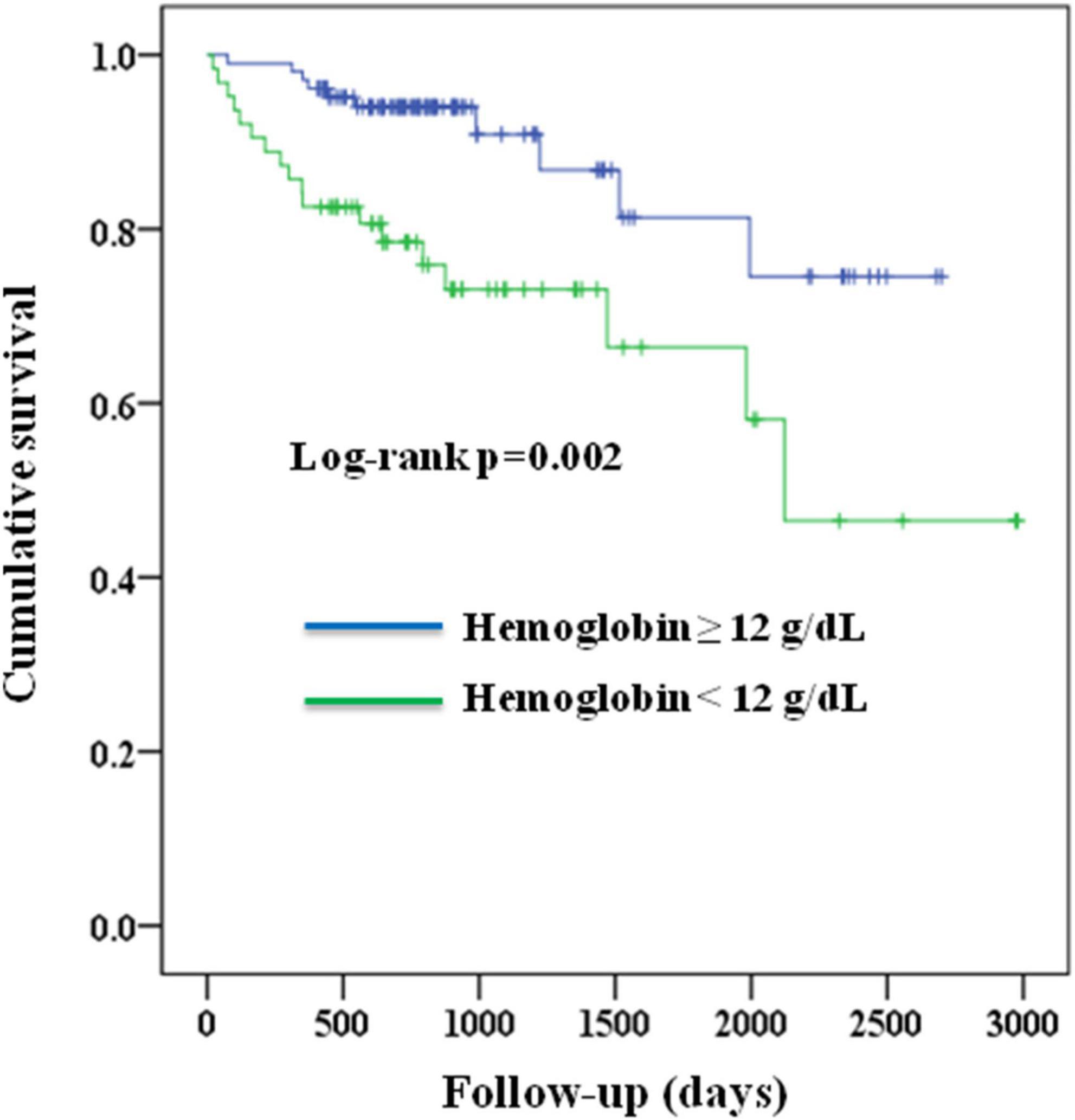
Figure 1. Kaplan–Meier survival curves of the study population according to their pre-operative hemoglobin levels (<12 g/dL vs. ≥12 g/dL).
Similar findings were noted when pre-operative hemoglobin levels were examined as a continuous variable. An increase in pre-operative hemoglobin was associated with a lower risk of all-cause mortality (hazard ratio 0.709, 95% CI 0.574 to 0.876, p = 0.001, Table 2). This association was independent of age, sex, body mass index, and other clinical variables (hazard ratio 0.775, 95% CI 0.606 to 0.991, p = 0.042). Figure 2 shows the cubic spline of pre-operative hemoglobin levels vs. risk of all-cause mortality in the overall population. The point of hemoglobin level below which the risk of mortality started to increase was approximately 12 g/dL.
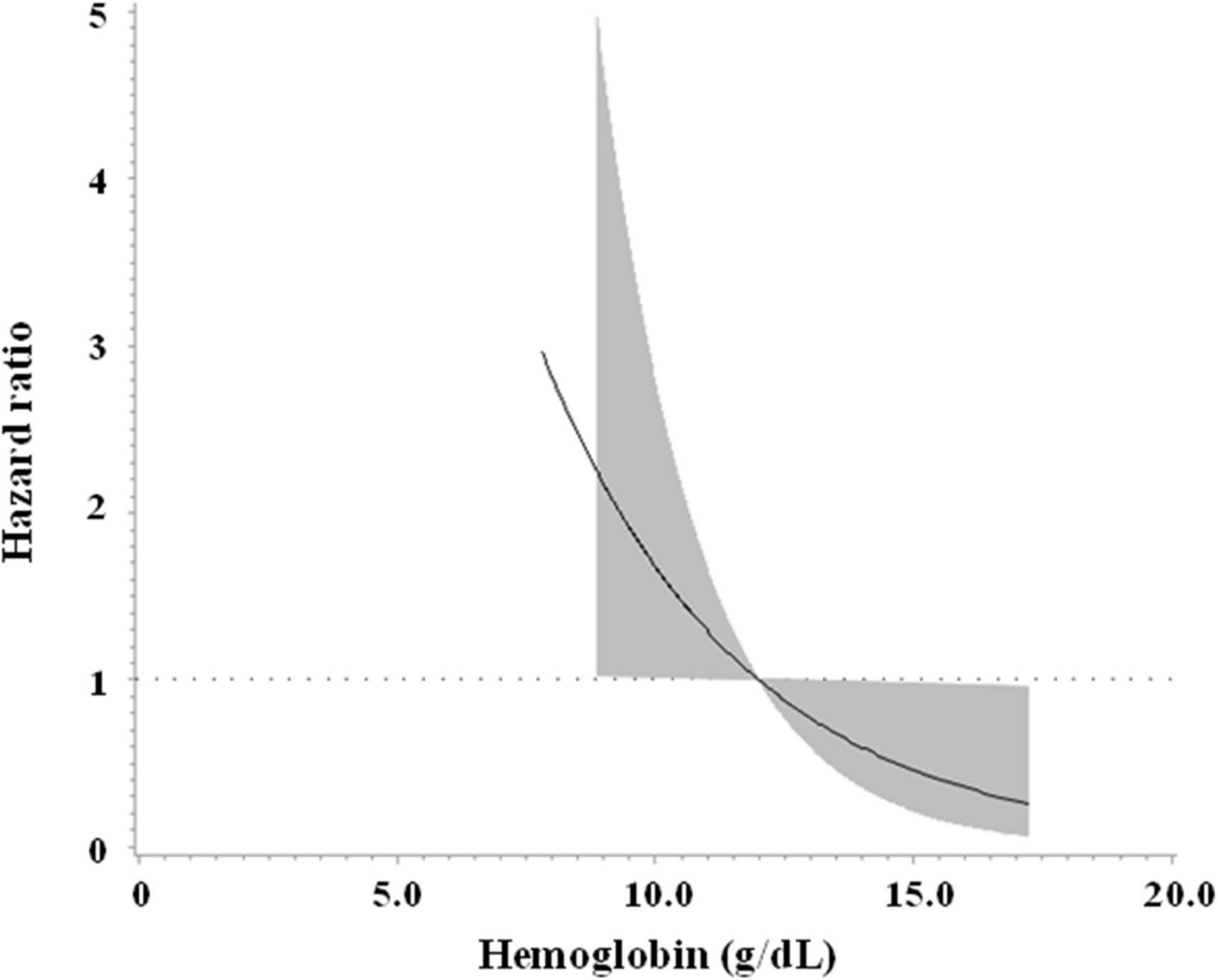
Figure 2. Cubic spline of pre-operative hemoglobin levels vs. risk of all-cause mortality in the overall population.
Discussion
In this study, we demonstrated that pre-operative anemia (hemoglobin <12 g/dL) was associated with a higher risk of all-cause mortality in patients with vertebral compression fracture who underwent percutaneous vertebroplasty after a median follow-up duration of more than 2 years. The findings were consistent when pre-operative hemoglobin was examined as an independent continuous variable (Table 2). Our results highlight the importance of pre-operative anemia as a risk factor for long-term mortality in patients with vertebral compression fracture who underwent a surgical intervention.
The incidence of vertebral fracture substantially increases in an aging population (15, 16). Furthermore, there is a significant increase in mortality rate after vertebral fracture (16, 17). In a recent report (18), anemia was associated with an approximately twofold increased risk of osteoporotic fractures in elderly men. Hence, anemia may be associated with adverse outcomes in that population (19, 20). In this context, anemia has been associated with complications after some orthopedic surgeries (21, 22). Moreover, a low pre-operative hemoglobin level was associated with an increase in in-hospital and 30-days mortality after surgical procedures (23). Similar findings were noted in patients who underwent total knee arthroplasty (12) and in those with hip fractures (11). However, data on the association between pre-operative anemia and long-term mortality after orthopedic procedures are scarce (14). Since the prevalence of anemia may be as high as 40% in elderly inpatients (9), our findings are important and could be used to identify patients who are at a high risk of post-operative long-term mortality in those who underwent percutaneous vertebroplasty (24–26), which has become a common orthopedic procedure for treatment of compression vertebral fractures.
The mechanisms by which pre-operative anemia was related to risk of mortality are not yet clear. In a prospective cohort study (14), pre-operative anemia (<12 g/dL) was associated with a higher risk of mortality (adjusted relative risk 1.68, 95% CI 1.22 to 2.30, p = 0.001) in elderly people with hip fracture. Anemia may impede functional mobility (27, 28) after surgery for fracture in the elderly, which could be associated with subsequent complications (29–32), such as pneumonia, and deep vein thrombosis. Anemia is frequently observed in aging populations. In light of this phenomenon, our findings highlight the effects of pre-operative anemia on adverse outcomes (33) in patients who underwent vertebroplasty, which is commonly conducted in elderly patients with vertebral fracture. The same scenario should be carefully considered in patients undergoing other orthopedic surgeries. In a retrospective cohort study including patients with femoral neck fracture aged 65 years and above treated with hemi-arthroplasty (34), pre-operative anemia (on-admission hemoglobin <10 g/dL) was associated with a higher risk of 2-years mortality (hazard ratio 3.3, 95% CI 1.3 to 8.3, p < 0.01). Similar findings were noted in another study conducted in patients over 60 years old who underwent hip fracture surgery (35). These results are in line with a recent report (36) in which hemoglobin was selected as a predictor for 1-year post-operative mortality in geriatric patients with hip fractures using an artificial intelligence approach. According to the aforementioned findings, pre-operative anemia should be evaluated carefully in aging surgical populations. These patients’ outcomes might be improved after optimal diagnosis and management of anemia.
It is not clear if various causes of anemia would affect the association between pre-operative anemia and patients outcomes. Although we did not have differential diagnosis of anemia for all patients, some of them (n = 132, 79%) had data on mean corpuscular volume (MCV). Among these, 17 (12.9%) had an MCV < 80 fL and 17 (12.9%) had an MCV > 100 fL. The association between anemia and all-cause mortality remained significant (HR 2.806, 95% CI 1.132 to 6.957, p = 0.026) after adjustment for MCV in the multivariate analysis. Similar finding was noted when hemoglobin was analyzed as a continuous variable (HR 0.772, 95% CI 0.598 to 0.996, p = 0.047). Based on these findings, we consider that the causes of anemia might be unlikely to affect the association between anemia and long-term all-cause mortality in our study population.
The strength of this study is that the association between pre-operative anemia and mortality after vertebroplasty was examined with a median follow-up duration of more than 2 years. Nevertheless, there are several limitations. First, the number of our patients was relatively small. Second, the data were retrospectively collected in a single medical center. Although we had adjusted for some concomitant chronic diseases (such as hypertension and diabetes) in the analytical models, missing data on the status of disease control (e.g., blood pressure and blood glucose levels) and nutrition might have confounded our results. Third, the effect of a blood transfusion on the association between pre-operative anemia and long-term mortality risk was not examined. Some of the aforementioned issues need to be addressed in prospective studies.
In conclusion, pre-operative anemia (<12 g/dL) was independently associated with survival outcome among patients with vertebral compression fractures who underwent vertebroplasty. Our findings highlight anemia as a risk factor for long-term mortality in this aging surgical population.
Data availability statement
The datasets presented in this article are not readily available because privacy/ethical restrictions. Requests to access the datasets should be directed to J-SW, anN3YW5nQHZnaHRjLmdvdi50dw==.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of Taichung Veterans General Hospital, Taichung, Taiwan. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
Y-CW, J-SW, and C-HL designed and conducted the research. Y-CW, Y-HL, Y-TL, W-CW, K-HC, C-CP, and C-HL contributed to data curation. Y-CW and J-SW analyzed data and wrote the first draft of the manuscript. Y-HL, Y-TL, W-CW, K-HC, C-CP, and C-HL revised the manuscript critically for important intellectual content. All authors approved the final draft of the manuscript.
Funding
This work was supported by the Taichung Veterans General Hospital, Taichung, Taiwan (Grant Numbers TCVGH-1103504C, 2021 and TCVGH-1113502C, 2022).
Acknowledgments
We thank the Osteoporosis Prevention Center of Taichung Veterans General Hospital, Taichung, Taiwan, for help data management.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chen AT, Cohen DB, Skolasky RL. Impact of nonoperative treatment, vertebroplasty, and kyphoplasty on survival and morbidity after vertebral compression fracture in the medicare population. J Bone Joint Surg Am. (2013) 95:1729–36. doi: 10.2106/JBJS.K.01649
2. Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. (2019) 393:364–76. doi: 10.1016/S0140-6736(18)32112-3
3. McDonald RJ, Achenbach SJ, Atkinson EJ, Gray LA, Cloft HJ, Melton LJ III, et al. Mortality in the vertebroplasty population. AJNR Am J Neuroradiol. (2011) 32:1818–23. doi: 10.3174/ajnr.A2616
4. Greendale GA, Barrett-Connor E, Ingles S, Haile R. Late physical and functional effects of osteoporotic fracture in women: the Rancho Bernardo study. J Am Geriatr Soc. (1995) 43:955–61. doi: 10.1111/j.1532-5415.1995.tb05557.x
5. Ray NF, Chan JK, Thamer M, Melton LJ III. Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone Miner Res. (1997) 12:24–35. doi: 10.1359/jbmr.1997.12.1.24
6. Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. (2009) 361:557–68. doi: 10.1056/NEJMoa0900429
7. Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. (2009) 361:569–79. doi: 10.1056/NEJMoa0900563
8. McCullough BJ, Comstock BA, Deyo RA, Kreuter W, Jarvik JG. Major medical outcomes with spinal augmentation vs conservative therapy. JAMA Intern Med. (2013) 173:1514–21. doi: 10.1001/jamainternmed.2013.8725
9. Gaskell H, Derry S, Andrew Moore R, McQuay HJ. Prevalence of anaemia in older persons: systematic review. BMC Geriatr. (2008) 8:1. doi: 10.1186/1471-2318-8-1
10. Galbussera AA, Mandelli S, Rosso S, Zanetti R, Rossi M, Giacomin A, et al. Mild anemia and 11- to 15-year mortality risk in young-old and old-old: results from two population-based cohort studies. PLoS One. (2021) 16:e0261899. doi: 10.1371/journal.pone.0261899
11. Halm EA, Wang JJ, Boockvar K, Penrod J, Silberzweig SB, Magaziner J, et al. The effect of perioperative anemia on clinical and functional outcomes in patients with hip fracture. J Orthop Trauma. (2004) 18:369–74. doi: 10.1097/00005131-200407000-00007
12. Neuwirth AL, Boddapati V, Held MB, Grosso MJ, Shah RP, Geller JA, et al. Preoperative anemia is associated with 30-day morbidity in total knee arthroplasty. Orthopedics. (2022) 45:e86–90. doi: 10.3928/01477447-20211227-06
13. Staples MP, Kallmes DF, Comstock BA, Jarvik JG, Osborne RH, Heagerty PJ, et al. Effectiveness of vertebroplasty using individual patient data from two randomised placebo controlled trials: meta-analysis. BMJ. (2011) 343:d3952. doi: 10.1136/bmj.d3952
14. Yombi JC, Putineanu DC, Cornu O, Lavand’homme P, Cornette P, Castanares-Zapatero D. Low haemoglobin at admission is associated with mortality after hip fractures in elderly patients. Bone Joint J. (2019) 101-B:1122–8. doi: 10.1302/0301-620X.101B9.BJJ-2019-0526.R1
15. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. (2002) 359:1761–7. doi: 10.1016/S0140-6736(02)08657-9
16. Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. (2009) 301:513–21. doi: 10.1001/jama.2009.50
17. Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. (1999) 353:878–82. doi: 10.1016/S0140-6736(98)09075-8
18. Kristjansdottir HL, Mellström D, Johansson P, Karlsson M, Vandenput L, Lorentzon M, et al. Anemia is associated with increased risk of non-vertebral osteoporotic fractures in elderly men: the MrOS Sweden cohort. Arch Osteoporos. (2022) 17:85. doi: 10.1007/s11657-022-01130-9
19. Potter LJ, Doleman B, Moppett IK. A systematic review of pre-operative anaemia and blood transfusion in patients with fractured hips. Anaesthesia. (2015) 70:483–500. doi: 10.1111/anae.12978
20. Puckeridge G, Terblanche M, Wallis M, Fung YL. Blood management in hip fractures; are we leaving it too late? A retrospective observational study. BMC Geriatr. (2019) 19:79. doi: 10.1186/s12877-019-1099-x
21. Grosso MJ, Boddapati V, Cooper HJ, Geller JA, Shah RP, Neuwirth AL. The effect of preoperative anemia on complications after total hip arthroplasty. J Arthroplasty. (2020) 35:S214–8. doi: 10.1016/j.arth.2020.01.012
22. Kashanchi KI, Nazemi AK, Komatsu DE, Wang ED. The impact of preoperative anemia on complications after total shoulder arthroplasty. J Am Acad Orthop Surg Glob Res Rev. (2021) 5:e20.00136. doi: 10.5435/JAAOSGlobal-D-20-00136
23. Fowler AJ, Ahmad T, Phull MK, Allard S, Gillies MA, Pearse RM. Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg. (2015) 102:1314–24. doi: 10.1002/bjs.9861
24. Maravic M, Taupin P, Roux C. Hospital burden of vertebral fractures in France: influence of vertebroplasty. Osteoporos Int. (2013) 24:2001–6. doi: 10.1007/s00198-012-2264-7
25. Buchbinder R, Johnston RV, Rischin KJ, Homik J, Jones CA, Golmohammadi K, et al. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev. (2018) 11:CD006349. doi: 10.1002/14651858.CD006349.pub4
26. Cazzato RL, Bellone T, Scardapane M, De Marini P, Autrusseau PA, Auloge P, et al. Vertebral augmentation reduces the 12-month mortality and morbidity in patients with osteoporotic vertebral compression fractures. Eur Radiol. (2021) 31:8246–55. doi: 10.1007/s00330-021-07985-9
27. Foss NB, Kristensen MT, Kehlet H. Anaemia impedes functional mobility after hip fracture surgery. Age Ageing. (2008) 37:173–8. doi: 10.1093/ageing/afm161
28. Lawrence VA, Silverstein JH, Cornell JE, Pederson T, Noveck H, Carson JL. Higher Hb level is associated with better early functional recovery after hip fracture repair. Transfusion. (2003) 43:1717–22. doi: 10.1046/j.0041-1132.2003.00581.x
29. Han SB, Kim SB, Shin KH. Risk factors for postoperative pneumonia in patients undergoing hip fracture surgery: a systematic review and meta-analysis. BMC Musculoskelet Disord. (2022) 23:553. doi: 10.1186/s12891-022-05497-1
30. Feng L, Xu L, Yuan W, Xu Z, Feng Z, Zhang H. Preoperative anemia and total hospitalization time are the independent factors of preoperative deep venous thromboembolism in Chinese elderly undergoing hip surgery. BMC Anesthesiol. (2020) 20:72. doi: 10.1186/s12871-020-00983-2
31. Mathis MR, Naik BI, Freundlich RE, Shanks AM, Heung M, Kim M, et al. Preoperative risk and the association between hypotension and postoperative acute kidney injury. Anesthesiology. (2020) 132:461–75. doi: 10.1097/ALN.0000000000003063
32. Vlisides P, Mashour GA. Perioperative stroke. Can J Anaesth. (2016) 63:193–204. doi: 10.1007/s12630-015-0494-9
33. Guralnik J, Ershler W, Artz A, Lazo-Langner A, Walston J, Pahor M, et al. Unexplained anemia of aging: etiology, health consequences, and diagnostic criteria. J Am Geriatr Soc. (2022) 70:891–9. doi: 10.1111/jgs.17565
34. Sayed-Noor A, Al-Amiry B, Alwan A, Knutsson B, Barenius B. The association of on-admission blood hemoglobin, C-reactive protein, and serum creatinine with 2-year mortality of patients with femoral neck fractures. Geriatr Orthop Surg Rehabil. (2021) 12:21514593211037758. doi: 10.1177/21514593211037758
35. Duque-Sánchez JD, Toro LÁ, González-Gómez FI, Botero-Baena SM, Duque G, Gómez F. One-year mortality after hip fracture surgery: urban-rural differences in the Colombian Andes. Arch Osteoporos. (2022) 17:111. doi: 10.1007/s11657-022-01150-5
Keywords: anemia, fracture, mortality, vertebral fracture, vertebroplasty
Citation: Wu Y-C, Lin Y-H, Lin Y-T, Wang W-C, Chen K-H, Pan C-C, Wang J-S and Lee C-H (2022) Pre-operative anemia was associated with all-cause mortality in patients with vertebral fracture who underwent percutaneous vertebroplasty. Front. Med. 9:1058636. doi: 10.3389/fmed.2022.1058636
Received: 30 September 2022; Accepted: 07 November 2022;
Published: 21 November 2022.
Edited by:
Tzvi Dwolatzky, Technion - Israel Institute of Technology, IsraelReviewed by:
I. G. P. Suka Aryana, Udayana University, IndonesiaWeiyang Zhong, The First Affiliated Hospital of Chongqing Medical University, China
Copyright © 2022 Wu, Lin, Lin, Wang, Chen, Pan, Wang and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun-Sing Wang, anN3YW5nQHZnaHRjLmdvdi50dw==; Cheng-Hung Lee, bGVlY2hlbmdodW5nMDExNUBnbWFpbC5jb20=
†These authors have contributed equally to this work and share senior authorship
 Yun-Che Wu
Yun-Che Wu Yu-Hsien Lin
Yu-Hsien Lin Yu-Tsung Lin
Yu-Tsung Lin Wen-Chien Wang
Wen-Chien Wang Kun-Hui Chen1,2,3
Kun-Hui Chen1,2,3 Chien-Chou Pan
Chien-Chou Pan Jun-Sing Wang
Jun-Sing Wang