- 1Department of Family Medicine, Chi Mei Medical Center, Tainan, Taiwan
- 2Department of Food and Nutrition, Chung Hwa University of Medical Technology, Tainan, Taiwan
- 3Department of Nursing, Chung Hwa University of Medical Technology, Tainan, Taiwan
- 4Department of Internal Medicine, Chi Mei Medical Center, Tainan, Taiwan
- 5Institute of Biomedical Sciences, National Sun Yat-sen University, Kaohsiung, Taiwan
- 6Department of Medical Research, Chi Mei Medical Center, Tainan, Taiwan
- 7Department of Family Medicine, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, Taiwan
- 8Department of Family Medicine, College of Medicine, National Cheng Kung University, Tainan, Taiwan
- 9Institute of Gerontology, College of Medicine, National Cheng Kung University, Tainan, Taiwan
Sarcopenia is an emerging issue, but there is no universal consensus regarding its screening and diagnosis, especially regarding the influence of the Asian Working Group for Sarcopenia (AWGS) 2019 new definition on the prevalence of community-dwelling adults. To compare the prevalence of sarcopenia between the 2019 and 2014 definitions, a cross-sectional study including 606 normal nutritional status subjects (203 men/403 women; mean age 63.3 ± 10.0 years) was performed. Sarcopenic parameters, including calf circumference, grip strength, 6-m gait speed, and bioelectrical-impedance-analysis-derived skeletal mass index (SMI), were evaluated. According to the 2019 AWGS definition, the prevalence of possible sarcopenia and sarcopenia among community-dwelling adults was 7.4 and 2.8%, respectively. There were highly consistent findings regarding sarcopenia between the 2019 and 2014 AWGS definitions according to Cohen's kappa coefficient (0.668). However, the prevalence of possible sarcopenia according to 2014 and 2019 AWGS in males increased 7.9%; in contrast, sarcopenia decreased from 7.4 to 3.7% in females (p < 0.001). In conclusion, the AWGS 2019 definition is more convenient for sarcopenia case screening and remains considerably consistent in sarcopenia identification in community-dwelling adults in Taiwan. The discordance of possible sarcopenia and sarcopenia by sex is a concern.
Introduction
Sarcopenia is a progressive age-related decline of skeletal muscle (1). As the rapid growth of the elderly population, sarcopenia has become the most important issue in public health (2). As the COVID-19 outbreak began in 2020, all people were forced to stay at home and decrease their daily activity, and some gym and leisure activities were stopped (3–5). Reduced activity and subsequent weight gain cause chronic diseases (6), including frailty and sarcopenia, to worsen due to COVID-19 isolation/quarantine or hospitalization, particularly in elderly individuals (7). As much as 8% muscle strength decrease after short-term reduced physical activity for 14 days in the elderly with low muscle mass (8). The restricted quarantine also worsen the adverse consequences of sarcopenia such as functional decline, physical disability, falls, impaired quality of life, increased health care expenditures, hospitalization and death (9–12). Therefore, the finding and intervention of the possible sarcopenia as early as possible is an emerging concern during and after the COVID-19 pandemics (13, 14). The Asian Working Group for Sarcopenia (AWGS) (15, 16) recommended more attention and active intervention to enhance resilience, especially during the increase in sarcopenia owing to the aging society and COVID-19 pandemic.
The prevalence of sarcopenia varies due to differences in lifestyle habits, environment, culture, and ethnicities (17–19). In community-based studies, the prevalence of sarcopenia was 12.5% in Belgium, 7.5% in Japan, 4.8% in Brazil and 4.5% in Germany (20–24). The prevalence of sarcopenia ranges from 3.9% (2.5% in women and 5.4% in men) to 7.3% (6.5% in women and 8.2% in men) among community-dwelling elderly adults in Taiwan (25). Worldwide, the prevalence of sarcopenia in community-dwelling elderly adults is ~10.0% (26). The different operational definition is one of the major reasons of diverse prevalence (26).
Based on AWGS 2014, a new AWGS algorithm was declared in 2019. The simple, non-invasive, and inexpensive measurement of calf circumference (CC) was recommended as a first-line screening tool. Gait speed ranged from 0.8 to 1.0 m/s, and handgrip strength in males ranged from 26 to 28 kg (27).
The variation between the EWGSOP and EWGSOP2 criteria has also been reported in many studies, as a lower number of males and a lower prevalence of the combination of low muscle mass and muscle strength were found when EWGSOP2 was used (28, 29). On the other hand, a comparison between the AWGS 2019 and AWGS 2014 criteria revealed more older males who required long-term care, and the prevalence of sarcopenia was 16% in prefrail community-dwelling older adults based on the AWGS 2019 (30, 31). Even though these is no consistent conclusion about the comparison between EWGSOP1 and EWGSOP2 (32–35), most of the experts endorsed new EWGSOP2 as well (32, 36, 37). In contrast to EWGSOP series, limited studies explored the clinical utility regarding both the 2014 and new 2019 Asian Working Group for Sarcopenia. We hypothesized that the new AWGS 2019 criteria might impact sarcopenia identification. This study scrutinized the differences in the sarcopenia ratio between the AWGS 2019 and 2014 criteria for community-dwelling adults.
Participants and methods
Using the convenient sampling method, we surveyed 606 community-dwelling middle-aged and elderly Taiwanese individuals who were ambulatory and lived in Jia-Li District, southern Taiwan from May 2016 to June 2017. The exclusion criteria were uncontrolled hypertension or diabetes, stroke, severe liver or renal disease, gastrointestinal disease, neuromuscular disease, infectious disease, pulmonary disease, endocrine system disease, neurological or acute/advanced psychiatric disease, cancer, a history of seizures, and sensitivity to any study procedures. At the initial screening, recruits underwent a review of the inclusion and exclusion criteria, the validated structural questionnaires, which included basic characteristics, smoking and drinking habits, medical history, concomitant therapies, daily activity evaluation, and anthropometric and body composition measurements (38–40). We defined participants to have a smoking habit if they had smoked more than 100 cigarettes and still smoked one pack (20 cigarettes) at least per month for more than 6 months, and alcohol drinking was defined by if participants still drank one time per week for more than 6 months (39, 41). A history of hypertension, dyslipidemia or diabetes was assessed by referring to the self-reported physician's diagnosis. The short form Mini-Nutritional Assessment (MNA) was used to evaluate nutritional status (42, 43).
Bodyweight and standing height were measured using a medical weight- and height-analyzing scale (Detecto™, Webb City, MO, USA); participants were barefoot and dressed in light clothing. Body mass index (BMI) was calculated using the following formula: BMI = bodyweight in kg/height in m2. CC was measured at the greatest girth region of both calves while participants were in a seated and relaxed position with knee flexion at 90° using inelastic tape (44). Functional limitations were assessed by using the Short Physical Performance Battery (SPPB) (45). A higher summary performance score represents better performance and vice versa (46). A single-frequency 8-electrode bioelectrical impedance analysis (BIA) device (BC-418; Tanita Corp., Itabashi-ku, Tokyo, Japan) was used to measure body composition, including body fat and skeletal muscle mass (SMM) (47) [estimated using Janssen's equation (SMI = kg/m2)] (1, 41, 48). Gait speed was measured by the walking test modified to a 6-m distance (49). Grip strength [Grip-D (TKK 5401); Japan] was assessed in two separate 30-s fast-twist tests for one hand for each participant. The maximum value of grip strength was used to indicate muscle function (50). The definition of a pre-state of sarcopenia termed “presarcopenia” is low muscle mass with normal physical function and performance by EWGSOP. These varieties were compared between AWGS 2019 and AWGS 2014 (27, 51).
Ethical approval
The study (ClinicalTrials.gov Identifier: NCT03891134) was approved and monitored by the Institutional Review Board of the Chi Mei Medical Center (CMMC10504-J01). Each participant was informed of the purpose of the study, experimental procedures, and potential risks after providing signed written consent.
Statistics
All statistical analyses were performed using the Statistical Package for the Social Sciences 22 for Windows (IBM Corp., Armonk, NY, USA). Categorical and continuous variables are expressed as numbers (percentages) and as the means ± standard deviations (SDs), as indicated. Continuous variables were analyzed using unpaired t tests, and categorical variables were analyzed using the χ2 test. Significance was set at p < 0.05 for two-tailed analysis. The clinical characteristics and measurement data of males and females were compared by unpaired t tests. Regarding the comparison of the number of cases of sarcopenia and those with handgrip strength and usual gait speed measurements below the reference values between AWGS 2019 and AWGS 2014, we performed McNemar tests to compare sexes. To distinguish the corresponding reliability between the AWGS 2019 and AWGS 2014, Cohen's kappa coefficient (κ) was used to assess interrater agreement for categorical data (52). The sensitivity and specificity were calculated accordingly.
Results
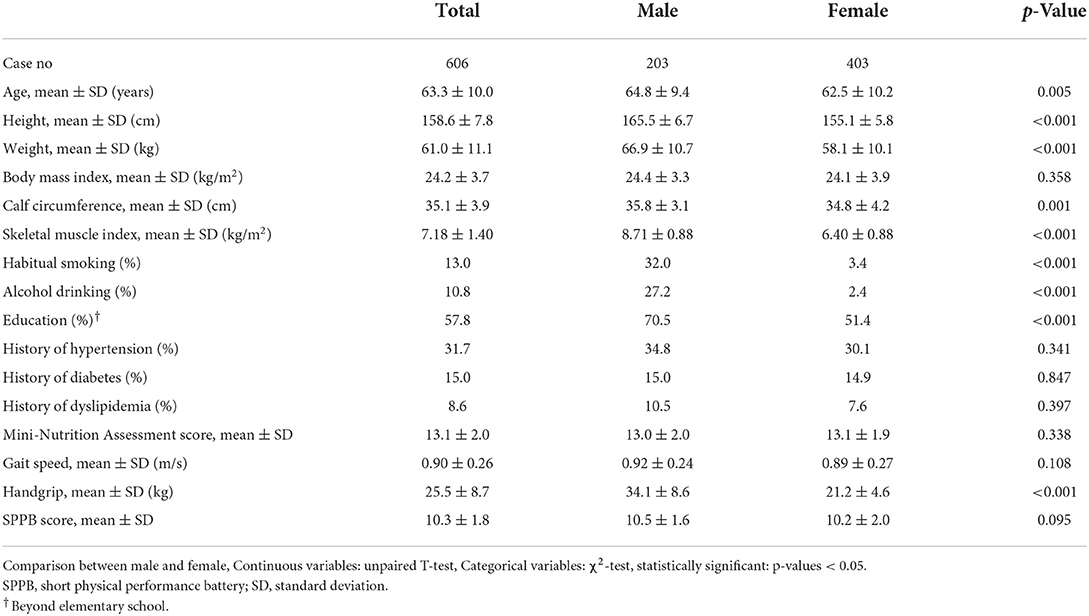
A total of 606 candidates (203 males, 403 females) with a mean age of 63.3 ± 10.0 years were identified. The distribution of sarcopenia in 2014 and 2019 is presented in Figure 1. There were 3.1% (AWGS 2014) and 2.5% (AWGS 2019) severe sarcopenia cases.
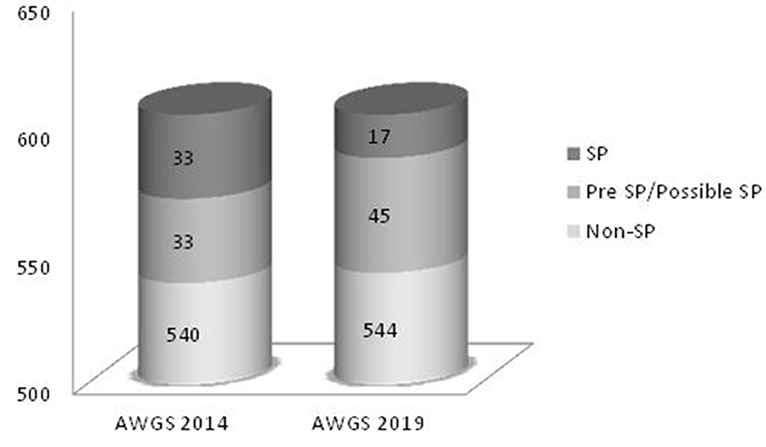
Figure 1. Conceptual distribution of sarcopenia. SP, sarcopenia; Possible Sarcopenia on 2019 AWGS, Pre-Sarcopenia on 2014 AWGS.
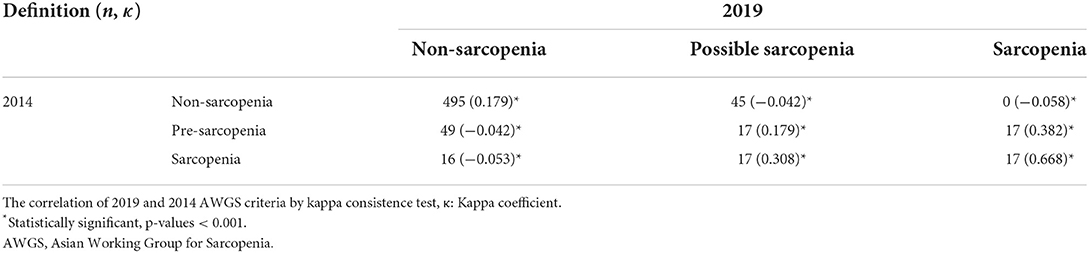
Table 1 shows the demographic characteristics and measurements of the study participants according to the definition of 2019 AWGS. The mean MNA and SPPB scores indicated the participants with normal nutritional status and without physical function limitation. Table 2 outlines the ratios of overall participants and participants grouped by sex according to the AWGS 2014 and 2019 definitions. The mean prevalence of possible sarcopenia and sarcopenia was 7.4 and 2.8% according to the 2019 criteria, compared to, 5.4 and 5.4% using the 2014 definition, respectively. In males, on average, 7.9% of participants had possible sarcopenia based on the 2019 criteria, compared to 0% using the 2014 definition (presarcopenia). In females, on average, 7.2 and 3.7% of participants had possible sarcopenia and sarcopenia based on the 2019 criteria, compared to 8.2 and 7.4% using the 2014 definition. There was slight agreement on nonsarcopenia and possible sarcopenia (κ: 0.179) but substantial agreement on sarcopenia (κ: 0.668; Table 3). Compared to the 2014 criteria, the 2019 AWGS criteria sensitivity and specificity were 51.5 and 100%, respectively (Supplementary Table 1).
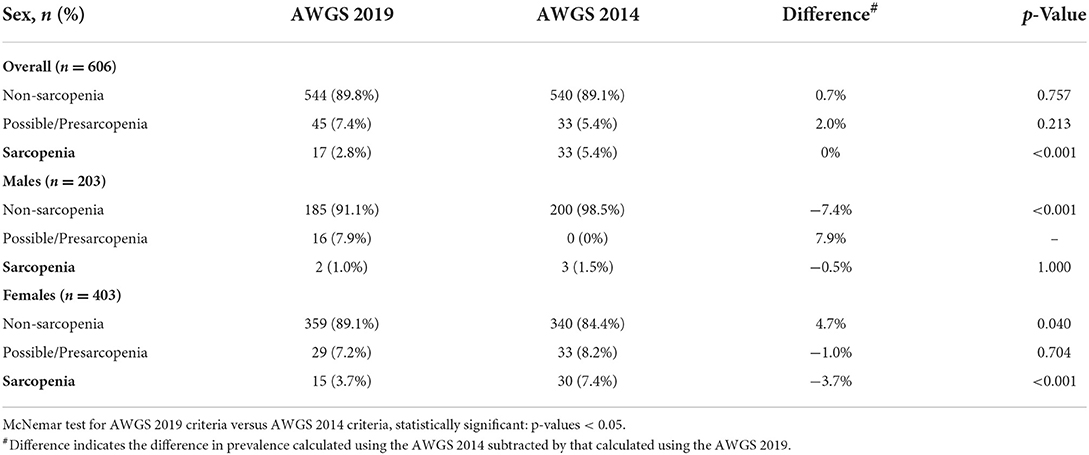
Table 2. Prevalence and difference of non-sarcopenia, pre/possible sarcopenia, and sarcopenia in Taiwanese community-dwelling adults using the cut-of values from the 2014 and 2019 Asian Working Group for Sarcopenia (AWGS) definition, stratified by sex.
Discussion
When the AWGS 2019 algorithm was announced, the prevalence of sarcopenia varied since the handgrip strength of males and gait speed increased. When we used the 2019 AWGS definition, the prevalence of sarcopenia was 2.8% within the range of community settings (1–30%) (16, 27) but lower than that when the 2014 definition was used (5.4%). The decrease in the prevalence of sarcopenia cases was predominantly observed among females (3.7%). Sex-based differences of a lower prevalence in females and a higher prevalence in males were found for possible sarcopenia according to the AWGS 2019 definition. There was higher relative consistency in sarcopenia between the 2019 and 2014 AWGS definitions in South Taiwanese community-dwelling adults.
The prevalence of pre-sarcopenia according to AWGS was 8.4% in Chinese T2DM elderly (53). However, some studies reported the prevalence of possible sarcopenia based on the 2019 AWGS criteria widely ranged from 2.9 to 38.5% in Asian (54–56). During the COVID-19 pandemic, one study demonstrated the skeletal muscle mass decrease by life space assessment (57). The pooled prevalence of sarcopenia in COVID-19 was 48.0% in one meta-analysis study (58). As the subjects at risk of sarcopenia would increase rapidly in post COVID-19 pandemic era, it is plausible to ascertain the utility of case finding by 2019 AWGS.
In the present study, we found no significant statistical difference in the prevalence of non-sarcopenia and pre-sarcopenia/possible sarcopenia between 2014 and 2019 AWGS algorithm, but higher possible sarcopenia as revealed in previous study with EWGSOP2 (59). The 2019 AWGS algorithm initiated the case finding from calf circumference, SAR-F or SARF-CALF coordinated with muscle strength instead of muscle mass in 2014 AWGS for initial identifying subjects at risk of sarcopenia. That is, the new 2019 algorithm reached the purpose of case finding in community-dwelling middle aged and old adults at risk of sarcopenia in a more user-friendly manner. The AWGS 2019 algorithm recommended either calf circumference or the SARC-F or the SARC-Calf questionnaires as an initial screening tool for case finding in the community or primary health care (27). When the subjects' CC was below the standard values (male: 34 cm, female: 33 cm), further assessment and diagnostic procedures were arranged. Screening for sarcopenia using CC is an accurate and easy (60) and has moderate-to-high sensitivity and specificity (61–65). We found that CC alone as initial case finding may result in underestimation in women of possible sarcopenia. In one trial of cadavers (66), CC showed a higher correlation with muscle mass in males but not in females because of the higher fat mass among females (67). CC adjusted for BMI was proposed to predict sarcopenia (68). Lower sensitivity and higher specificity were calculated in our assessment, and the result was similar to that of J Reiss et al. about EWGSOP2 (28) and consistent with a lower Kappa coefficient in possible/presarcopenia. Some studies found low sensitivity but high specificity for SARC-F (69, 70); however, SARC-Calf (SARC-F combined with CC) with improved sensitivity (71) would be a clinical practice tool for identifying sarcopenia but would require more time completing questionnaires. Ethnic differences in sarcopenia and the difference between EWGSOP1 and EWGSOP2 have been reported (28, 29), and more trials analyzing AWGS 2019 will be helpful for sarcopenia early detection and intervention (30, 31).
Our study had limitations. First, this cross-sectional study was initiated before the announcement of the EWGSOP2 and 2019 AWGS. Additionally, the SARC-F and SARC-Calf were not recommended for identifying sarcopenia. The lack of consistent analysis could occur in the absence of SARC-F and SARC-Calf information. In our study, although the non-sarcopenia and possible sarcopenia rates were similar between the 2014 and 2019 definitions, sex differences and female predominance in our study might affect the prevalence and limit generalizability to other trials (72). Second, the enrolled adults were engaged in agricultural work in rural areas of south Taiwan. There might be a difference compared to adults living in the city. We believe the most valuable finding is that when subjects are judged as having sarcopenia according to the 2019 definition, the possibility of severe sarcopenia may be higher. More comparisons are needed to confirm our findings and investigate the bias.
In conclusion, this study revealed that the AWGS 2019 algorithm was convenient and efficient in sarcopenia case identification for community-dwelling adults in Taiwan. However, sex differences in possible sarcopenia/sarcopenia should not be ignored when conducting comparisons with the 2014 criteria, and the sarcopenia rate remained considerably consistent.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the correspondingauthor.
Ethics statement
The studies involving human participants were reviewed and approved by Chi Mei Medical Center (CMMC10504-J01). The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conception and design of the study: C-HK, H-YC, C-SC, and C-HW. Statistical analyses: C-HK, S-CY, and C-SC. Acquisition of data: S-JW, Y-FC, and C-SC. Drafting the article: C-HK and C-HW. Research data interpretation, suggestions and discussion, critical revision of the manuscript, and final approval of the manuscript: all authors.
Funding
We are grateful to Taiwanese Osteoporosis Association, the Taiwan Ministry of Science and Technology (MOST No. 106-2314-B-006-064-MY2), Chi Mei Hospital (Holistic Health Care No. JCHCR 10510), and National Cheng Kung University Hospital (No. NCKUH-10709012) for the listed grants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.1041186/full#supplementary-material
References
1. Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. (2002) 50:889–9. doi: 10.1046/j.1532-5415.2002.50216.x
2. Wu Y-H, Hwang A-C, Liu L-K, Peng L-N, Chen L-K. Sex differences of sarcopenia in Asian populations: the implications in diagnosis and management. J Clin Gerontol Geriatr. (2016) 7:37.e43. doi: 10.1016/j.jcgg.2016.04.001
3. Parmet WE, Sinha MS. Covid-19 - the law and limits of quarantine. N Engl J Med. (2020) 382:e28. doi: 10.1056/NEJMp2004211
4. Sun S, Folarin A, Ranjan Y, Rashid Z, Conde P, Cummins N, et al. Using smartphones and wearable devices to monitor behavioural changes during COVID-19. arXiv. (2020). doi: 10.2196/19992
5. Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. (2020) 28:12. doi: 10.3390/nu12061583
6. Patterson R, McNamara E, Tainio M, de Sá TH, Smith AD, Sharp SJ, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. (2018) 33:811–29. doi: 10.1007/s10654-018-0380-1
7. English KL, Paddon-Jones D. Protecting muscle mass and function in older adults during bed rest. Curr Opin Clin Nutr Metab Care. (2010) 13:34–9. doi: 10.1097/MCO.0b013e328333aa66
8. Reidy PT, McKenzie AI, Mahmassani Z, Morrow VR, Yonemura NM, Hopkins PN, et al. Skeletal muscle ceramides and relationship with insulin sensitivity after 2 weeks of simulated sedentary behaviour and recovery in healthy older adults. J Physiol. (2018) 596:5217–36. doi: 10.1113/JP276798
9. Kirwan R, McCullough D, Butler T, Perez, de Heredia F, Davies IG, Stewart C. Sarcopenia during COVID-19 lockdown restrictions: long-term health effects of short-term muscle loss. GeroScience. (2020) 42:1547–78. doi: 10.1007/s11357-020-00272-3
10. Liu P, Hao Q, Hai S, Wang H, Cao L, Dong B. Sarcopenia as a predictor of all-cause mortality among community-dwelling older people: a systematic review and meta-analysis. Maturitas. (2017) 103:16–22. doi: 10.1016/j.maturitas.2017.04.007
11. Sousa AS, Guerra RS, Fonseca I, Pichel F, Ferreira S, Amaral T, et al. Financial impact of sarcopenia on hospitalization costs. Eur J Clin Nutr. (2016) 70:1046–51. doi: 10.1038/ejcn.2016.73
12. Goates S, Du K, Arensberg MB, Gaillard T, Guralnik J, Pereira S, et al. Economic impact of hospitalizations in US adults with sarcopenia. J Frailty Aging. (2019) 8:93–9. doi: 10.14283/jfa.2019.10
13. Xie WQ, Xiao GL, Hu PW, He YQ, Lv S, Xiao WF. Possible sarcopenia: early screening and intervention-narrative review. Ann Palliat Med. (2020) 9:4283–93. doi: 10.21037/apm-20-967
14. Kwan RYC, Liu JYW, Yin YH, Lee PH, Ng SY, Cheung DSK, et al. Sarcopenia and its association with objectively measured life-space mobility and moderate-to-vigorous physical activity in the oldest-old amid the COVID-19 pandemic when a physical distancing policy is in force. BMC Geriatr. (2022) 22:250. doi: 10.1186/s12877-022-02861-7
15. Lim WS, Wong SF, Leong I, Choo P, Pang WS. Forging a frailty-ready healthcare system to meet population ageing. Int J Environ Res Public Health. (2017) 14:1448. doi: 10.3390/ijerph14121448
16. Legido-Quigley H, Asgari N, Teo YY, Leung GM, Oshitani H, Fukuda K, et al. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet. (2020) 395:848–50. doi: 10.1016/S0140-6736(20)30551-1
17. Barbieri E, Agostini D, Polidori E, Potenza L, Guescini M, Lucertini F, et al. The pleiotropic effect of physical exercise on mitochondrial dynamics in aging skeletal muscle. Oxid Med Cell Longev. (2015) 2015:917085. doi: 10.1155/2015/917085
18. Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. (2018) 6:e1077–86. doi: 10.1016/S2214-109X(18)30357-7
19. Lee JE, McLerran DF, Rolland B, Chen Y, Grant EJ, Vedanthan R, et al. Meat intake and cause-specific mortality: a pooled analysis of Asian prospective cohort studies. Am J Clin Nutr. (2013) 98:1032–41. doi: 10.3945/ajcn.113.062638
20. Legrand D, Vaes B, Matheï C, Swine C, Degryse JM. The prevalence of sarcopenia in very old individuals according to the European consensus definition: insights from the BELFRAIL study. Age Ageing. (2013) 42:727–34. doi: 10.1093/ageing/aft128
21. Yoshida D, Suzuki T, Shimada H, Park H, Makizako H, Doi T, et al. Using two different algorithms to determine the prevalence of sarcopenia. Geriatr Gerontol Int. (2014) 14(Suppl 1):46–51. doi: 10.1111/ggi.12210
22. Alexandre TDS, Duarte YAO, Santos JLF, Lebrão ML. Prevalence and associated factors of sarcopenia, dynapenia, and sarcodynapenia in community-dwelling elderly in São Paulo - SABE Study. Rev Bras Epidemiol. (2019) 21:e180009. doi: 10.1590/1980-549720180009.supl.2
23. Yamada M, Nishiguchi S, Fukutani N, Tanigawa T, Yukutake T, Kayama H, et al. Prevalence of sarcopenia in community-dwelling Japanese older adults. J Am Med Dir Assoc. (2013) 14:911–5. doi: 10.1016/j.jamda.2013.08.015
24. Kemmler W, Teschler M, Goisser S, Bebenek M, von Stengel S, Bollheimer LC, et al. Prevalence of sarcopenia in Germany and the corresponding effect of osteoarthritis in females 70 years and older living in the community: results of the FORMoSA study. Clin Interv Aging. (2015) 10:1565–73. doi: 10.2147/CIA.S89585
25. Wu IC, Lin CC, Hsiung CA, Wang CY, Wu CH, Chan DC, et al. Epidemiology of sarcopenia among community-dwelling older adults in Taiwan: a pooled analysis for a broader adoption of sarcopenia assessments. Geriatr Gerontol Int. (2014) 14:52–60. doi: 10.1111/ggi.12193
26. Shafiee G, Keshtkar A, Soltani A, Ahadi Z, Larijani B, Heshmat R. Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J Diabetes Metab Disord. (2017) 16:21. doi: 10.1186/s40200-017-0302-x
27. Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. (2020) 21:300–307.e2. doi: 10.1016/j.jamda.2019.12.012
28. Reiss J, Iglseder B, Alzner R, Mayr-Pirker B, Pirich C, Kässmann H, et al. Consequences of applying the new EWGSOP2 guideline instead of the former EWGSOP guideline for sarcopenia case finding in older patients. Age Ageing. (2019) 48:719–24. doi: 10.1093/ageing/afz035
29. Costanzo L, De Vincentis A, Di Iorio A, Bandinelli S, Ferrucci L, Antonelli Incalzi R, et al. Impact of low muscle mass and low muscle strength according to EWGSOP2 and EWGSOP1 in community dwelling older people. J Gerontol A Biol Sci Med Sci. (2020) 75:1324–30. doi: 10.1093/gerona/glaa063
30. Sawaya Y, Ishizaka M, Kubo A, Shiba T, Hirose T, Onoda K, et al. The Asian working group for sarcopenia's new criteria updated in 2019 causing a change in sarcopenia prevalence in Japanese older adults requiring long-term care/support. J Phys Ther Sci. (2020) 32:742–7. doi: 10.1589/jpts.32.742
31. Lim JY, Low NA, Merchant RA. Prevalence of sarcopenia in pre-frail community dwelling older adult and utility of SARC-F, SARC-CalF and calf circumference in case finding. J Frailty Sarcopenia Falls. (2020) 5:53–6. doi: 10.22540/JFSF-05-053
32. Locquet M, Beaudart C, Petermans J, Reginster JY, Bruyere O. EWGSOP2 versus EWGSOP1: impact on the prevalence of sarcopenia and its major health consequences. J Am Med Dir Assoc. (2019) 20:384–5. doi: 10.1016/j.jamda.2018.11.027
33. Yang M, Liu Y, Zuo Y, Tang H. Sarcopenia for predicting falls and hospitalization in community-dwelling older adults: EWGSOP versus EWGSOP2. Sci Rep. (2019) 9:17636. doi: 10.1038/s41598-019-53522-6
34. Shafee G, Heshmat R, Ostovar A, Khatami F, Fahimfar N, Arzaghi SM, et al. Comparison of EWGSOP-1and EWGSOP-2 diagnostic criteria on prevalence of and risk factors for sarcopenia among Iranian older people: the Bushehr Elderly Health (BEH) program. J Diabetes Metab Dis. (2020) 19:727–34. doi: 10.1007/s40200-020-00553-w
35. Franzon K, Zethelius B, Cederholm T, Kilander L. The impact of muscle function, muscle mass and sarcopenia on independent ageing in very old Swedish men. BMC Geriatr. (2019) 19:153. doi: 10.1186/s12877-019-1142-y
36. Petermann-Rocha F, Chen M, Gray SR, Ho FK, Pell JP, Celis-Morales C. New versus old guidelines for sarcopenia classification: what is the impact on prevalence and health outcomes? Age Ageing. (2020) 49:300–4. doi: 10.1093/ageing/afz126
37. Phu S, Vogrin S, Zanker J, Bani Hassan E, Al Saedi A, Duque G. Agreement between initial and revised European working group on sarcopenia in older people definitions. J Am Med Dir Assoc. (2019) 20:382–3.e1. doi: 10.1016/j.jamda.2018.11.026
38. Chang CS, Chang YF, Wang MW, Chen CY, Chao YJ, Chang HJ, et al. Inverse relationship between central obesity and osteoporosis in osteoporotic drug naive elderly females: the Tianliao Old People (TOP) Study. J Clin Densitom. (2013) 16:204–11. doi: 10.1016/j.jocd.2012.03.008
39. Chang CS, Chang YF, Liu PY, Chen CY, Tsai YS, Wu CH. Smoking, habitual tea drinking and metabolic syndrome in elderly men living in rural community: the Tianliao old people (TOP) study 02. PLoS ONE. (2012) 7:e38874. doi: 10.1371/journal.pone.0038874
40. Ko CH, Wu SJ, Wang ST, Chang YF, Chang CS, Kuan TS, et al. Effects of enriched branched-chain amino acid supplementation on sarcopenia. Aging. (2020) 12:15091–103. doi: 10.18632/aging.103576
41. Wu CH, Chen KT, Hou MT, Chang YF, Chang CS, Liu PY, et al. Prevalence and associated factors of sarcopenia and severe sarcopenia in older Taiwanese living in rural community: the Tianliao old people study 04. Geriatr Gerontol Int. (2014) 14:69–75. doi: 10.1111/ggi.12233
42. Young AM, Kidston S, Banks MD, Mudge AM, Isenring EA. Malnutrition screening tools: comparison against two validated nutrition assessment methods in older medical inpatients. Nutrition. (2013) 29:101–06. doi: 10.1016/j.nut.2012.04.007
43. Wyka J, Biernat J, Mikołajczak J, Piotrowska E. Assessment of dietary intake and nutritional status (MNA) in polish free-living elderly people from rural environments. Arch Gerontol Geriatr. (2012) 54:44–9. doi: 10.1016/j.archger.2011.02.001
44. Berg HE, Tedner B, Tesch PA. Changes in lower limb muscle cross-sectional area and tissue fluid volume after transition from standing to supine. Acta Physiol Scand. (1993) 148:379–85. doi: 10.1111/j.1748-1716.1993.tb09573.x
45. Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. (1994) 49:M85–94. doi: 10.1093/geronj/49.2.M85
46. Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. (1995) 332:556–61. doi: 10.1056/NEJM199503023320902
47. Pietrobelli A, Rubiano F, St-Onge MP, Heymsfield SB. New bioimpedance analysis system: improved phenotyping with whole-body analysis. Eur J Clin Nutr. (2004) 58:1479–84. doi: 10.1038/sj.ejcn.1601993
48. Janssen I, Heymsfield SB, Baumgartner RN, Ross R. Estimation of skeletal muscle mass by bioelectrical impedance analysis. J Appl Physiol. (2000) 89:465–71. doi: 10.1152/jappl.2000.89.2.465
49. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. (2010) 39:412–23. doi: 10.1093/ageing/afq034
50. Hamilton A, Balnave R, Adams R. Grip strength testing reliability. J Hand Ther. (1994) 7:163–70. doi: 10.1016/S0894-1130(12)80058-5
51. Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, et al. Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc. (2014) 15:95–101. doi: 10.1016/j.jamda.2013.11.025
52. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med. (2012) 22:276–82. doi: 10.11613/BM.2012.031
53. Wang T, Feng X, Zhou J, Gong H, Xia S, Wei Q, et al. Type 2 diabetes mellitus is associated with increased risks of sarcopenia and pre-sarcopenia in Chinese elderly. Sci Rep. (2016) 6:38937. doi: 10.1038/srep38937
54. Miura H, Sakaguchi K, Ogawa W, Tamori Y. Clinical features of 65-year-old individuals in Japan diagnosed with possible sarcopenia based on the Asian Working Group for Sarcopenia 2019 criteria. Geriatr Gerontol Int. (2021) 21:689–96. doi: 10.1111/ggi.14182
55. Kurose S, Nishikawa S, Nagaoka T, Kusaka M, Kawamura J, Nishioka Y, et al. Prevalence and risk factors of sarcopenia in community-dwelling older adults visiting regional medical institutions from the Kadoma Sarcopenia Study. Sci Rep. (2020) 10:19129. doi: 10.1038/s41598-020-76185-0
56. Wu X, Li X, Xu M, Zhang Z, He L, Li Y. Sarcopenia prevalence and associated factors among older Chinese population: findings from the China Health and Retirement Longitudinal Study. PLoS ONE. (2021) 16:e0247617. doi: 10.1371/journal.pone.0247617
57. Perracini MR, de Amorim JSC, Lima CA, da Silva A, Trombini-Souza F, Pereira DS, et al. Impact of COVID-19 pandemic on life-space mobility of older adults living in Brazil: REMOBILIZE study. Front Public Health. (2021) 9:643640. doi: 10.3389/fpubh.2021.643640
58. Xu Y, Xu JW, You P, Wang BL, Liu C, Chien CW, et al. Prevalence of sarcopenia in patients with COVID-19: a systematic review and meta-analysis. Front Nutr. (2022) 9:925606. doi: 10.3389/fnut.2022.925606
59. Lampignano L, Bortone I, Castellana F, Donghia R, Guerra V, Zupo R, et al. Impact of different operational definitions of sarcopenia on prevalence in a population-based sample: the Salus in Apulia Study. Int J Environ Res Public Health. (2021) 18:12979. doi: 10.3390/ijerph182412979
60. Chen CY, Tseng WC, Yang YH, Chen CL, Lin LL, Chen FP, et al. Calf circumference as an optimal choice of four screening tools for sarcopenia among ethnic Chinese older adults in assisted living. Clin Interv Aging. (2020) 15:2415–22. doi: 10.2147/CIA.S287207
61. Kawakami R, Murakami H, Sanada K, Tanaka N, Sawada SS, Tabata I, et al. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr Gerontol Int. (2015) 15:969–76. doi: 10.1111/ggi.12377
62. Kusaka S, Takahashi T, Hiyama Y, Kusumoto Y, Tsuchiya J, Umeda M. Large calf circumference indicates non-sarcopenia despite body mass. J Phys Ther Sci. (2017) 29:1925–8. doi: 10.1589/jpts.29.1925
63. McIntosh EI, Smale KB, Vallis LA. Predicting fat-free mass index and sarcopenia: a pilot study in community-dwelling older adults. Age. (2013) 35:2423–34. doi: 10.1007/s11357-012-9505-8
64. Hwang AC, Liu LK, Lee WJ, Peng LN, Chen LK. Calf circumference as a screening instrument for appendicular muscle mass measurement. J Am Med Dir Assoc. (2018) 19:182–4. doi: 10.1016/j.jamda.2017.11.016
65. Kim S, Kim M, Lee Y, Kim B, Yoon TY, Won CW. Calf circumference as a simple screening marker for diagnosing sarcopenia in older korean adults: the Korean Frailty and Aging Cohort Study (KFACS). J Korean Med Sci. (2018) 33:e151. doi: 10.3346/jkms.2018.33.e151
66. Tresignie J, Scafoglieri A, Pieter Clarys J, Cattrysse E. Reliability of standard circumferences in domain-related constitutional applications. Am J Hum Biol. (2013) 25:637–42. doi: 10.1002/ajhb.22423
67. Nindl BC, Scoville CR, Sheehan KM, Leone CD, Mello RP. Gender differences in regional body composition and somatotrophic influences of IGF-I and leptin. J Appl Physiol. (2002) 92:1611–8. doi: 10.1152/japplphysiol.00892.2001
68. Bahat G. Measuring calf circumference: a practical tool to predict skeletal muscle mass via adjustment with BMI. Am J Clin Nutr. (2021) 113:1398–9. doi: 10.1093/ajcn/nqab107
69. Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc. (2013) 14:531–2. doi: 10.1016/j.jamda.2013.05.018
70. Kim S, Kim M, Won CW. Validation of the Korean version of the SARC-F questionnaire to assess sarcopenia: Korean Frailty and Aging Cohort Study. J Am Med Dir Assoc. (2018) 19:40–5.e1. doi: 10.1016/j.jamda.2017.07.006
71. Lim WS, Chew J, Lim JP, Tay L, Hafizah N, Ding YY. Letter to the editor: Case for validated instead of standard cut-offs for SARC-CalF. J Nutr Health Aging. (2019) 23:393–5. doi: 10.1007/s12603-019-1177-y
Keywords: Asian Working Group for Sarcopenia, sarcopenia, gait speed, hand grip, skeletal muscle index, calf circumference
Citation: Ko C-H, Chuang H-Y, Wu S-J, Yu S-C, Chang Y-F, Chang C-S and Wu C-H (2022) Changes of sarcopenia case finding by different Asian Working Group for Sarcopenia in community indwelling middle-aged and old people. Front. Med. 9:1041186. doi: 10.3389/fmed.2022.1041186
Received: 10 September 2022; Accepted: 24 October 2022;
Published: 07 November 2022.
Edited by:
Tino Prell, University Hospital in Halle, GermanyReviewed by:
Atsumu Yuki, Kochi University, JapanKornanong Yuenyongchaiwat, Thammasat University, Thailand
Copyright © 2022 Ko, Chuang, Wu, Yu, Chang, Chang and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chih-Hsing Wu, cGF1bG9AbWFpbC5uY2t1LmVkdS50dw==
†These authors have contributed equally to this work
 Chun-Hung Ko
Chun-Hung Ko Hua-Ying Chuang3,4†
Hua-Ying Chuang3,4† Chin-Sung Chang
Chin-Sung Chang Chih-Hsing Wu
Chih-Hsing Wu