- Department of Ophthalmology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, China
Purpose: To explore age- and gender-related differences of refractive and corneal astigmatism in myopic patients looking for refractive surgery.
Design: A retrospective cross-sectional study.
Materials and methods: The medical files of candidates looking for corneal refractive surgery between 2019 and 2021 were reviewed, demographic and refractive parameters including age, gender, refractive status, and corneal parameters were analyzed.
Results: A total of 1,417 eyes of 1,417 patients (453 males and 964 females) were included. Males had thicker cornea than females, while females had steeper cornea than males, there was no gender-related difference in refractive and corneal astigmatism depending on patients’ age. There was no difference in refractive astigmatism among different age group from 18 to 50 years, while corneal astigmatism had a shift from with-the rule (WTR) to against-the-rule (ATR) with increasing age. Age, central corneal thickness (CCT), sphere, refractive astigmatism (RA), and corneal curvature (Km) were correlated with corneal astigmatism (CA) (standardized coefficients of are 0.006, p = 0.011 for age, −0.001, p = 0.004 for CCT, and −0.027, p < 0.001 for sphere, 0.61, p < 0.001 for RA, −0.05, p < 0.001 for corneal curvature).
Conclusion: Refractive astigmatism is stable until the age of 50 years in myopic patients looking for refractive surgery, while corneal astigmatism showed a shift from WTR to ATR with advancing age. Age, CCT, sphere, refractive astigmatism and corneal curvature (Km) were correlated with corneal astigmatism.
Introduction
Astigmatism is a common type of refractive error, which has a significant impact on visual performance. It was first described by Tomas Young in the early 1800s, since then, a large number of studies have been conducted to evaluate various aspects of astigmatism (1–3). However, there is no single model or theory can explain the genesis of astigmatism (4). With the surge in corneal refractive surgery and toric lens implantation, it’s important to know the characteristics of refractive and corneal astigmatism as it may provide important information in making guidelines and surgical design.
It’s known that the prevalence and distribution of corneal or refractive astigmatism change according to the ethnicity and study population, it also varied with age, gender, and refractive statues (5–7). Previous studies revealed that corneal shape and astigmatism change from with-the-rule astigmatism to against-the-rule astigmatism with increasing age (8). And the amount and axis of astigmatism differ between males and females (9). But most of the studies were conducted on older population, cataract patients, or a wide range of ages (10, 11).
To our knowledge, there is no published study investigated the age- and gender-related characteristics in Chinese young myopic patients. The aim of this study is to describe the age- and gender-related difference in refractive and corneal astigmatism in this population, and its association with other corneal parameters.
Materials and methods
Subjects
This study reviewed and analyzed data of patients looking for laser refractive surgery between 2019 and 2021. The inclusion criteria were: refraction power was stable for more than 2 years (myopia increase ≤−0.5D); and no ocular and systemic disease (pterygium, keratoconus, etc.). Eyes with a history of ocular surgery, fundus disease, or other abnormal corneal disease or opacity were excluded.
Data collection
The medical files of patients were reviewed, demographic and preoperative data were collected including: age, gender, sphere, refractive astigmatism, flat K, steep K, corneal astigmatism, intraocular pressure, and central corneal thickness (CCT). Manifest and cycloplegic refraction were assessed by the same optometrist. Corneal curvature was obtained by corneal topography (Tomey, TMS-4, Japan), IOP was measured with a non-contact tonometer (Canon Full Auto Tonometer TX-F; Canon, Inc., Tokyo, Japan). CCT was measured with Sonomed Micropach 200P + (Sonomed, New Hyde Park, NY, USA). CCT, Manifest and cycloplegic refraction and corneal topography were performed by two experienced operators (L.S, YM. J). Date obtained from the right and left eye of a subject are often correlated, so the date of the right eye in this study was used for statistical analysis (12).
Refractive data were converted to minus cylinder form during analysis. The axis of astigmatism was defined for 180° ± 30° as WTR, for 90° ± 30° as ATR, whereas 45° ± 15° and 135° ± 15° were regarded as oblique astigmatism.
Statistical analysis
Student t-test was used to compare the difference between male and female. One-way analysis of variance (ANOVA) was used for comparison among multiple groups. Multiple linear regression analyses were used to assess the contribution of age, gender, central corneal thickness, refractive error, and corneal curvature to the corneal astigmatism. P < 0.05 were considered statistically significant. Statistical analyses were performed using SPSS and Excel.
Results
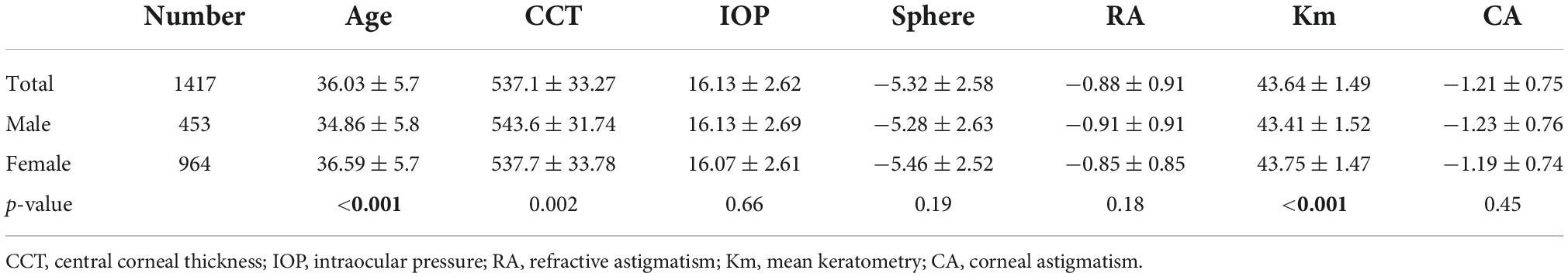
This study enrolled 1,417 eyes of 1,417 Chinese patients (453 males and 964 females) with a mean age of 36.03 ± 5.7 years (18∼50 years). The mean central corneal thickness (CCT) was 537.1 ± 33.27 μm, the mean intraocular pressure (IOP) was 16.13 ± 2.62 mmHg, the mean sphere power and astigmatism was −5.32 ± 2.58D, −0.88 ± 0.91D, the mean corneal power, and corneal astigmatism was 43.64 ± 1.49D, −1.21 ± 0.75D. The male eyes had greater CCT than female eyes (543.6 μm vs. 537.7 μm, p < 0.01), while females had slightly steeper corneal curvature (43.75 vs. 43.41, p < 0.01). There was no statistical sex-related difference in IOP, sphere, refractive astigmatism (RA), and corneal astigmatism (CA) as shown in Table 1.
In the total population, 974 (68.73%) eyes had refractive astigmatism (RA) over 0.5D, the mean magnitude of RA was 0.88 ± 0.91D, 1,210 (85.39%) of all eyes had corneal astigmatism (CA) over 0.5D, the mean magnitude of CA was 1.21 ± 0.75D. The mean magnitude of RA and CA did not have a significant difference between the men and women groups in any age group. The magnitude of RA did not change significantly among age groups, while the CA in male eyes decreased significantly with advancing age (p = 0.008) (Table 2).
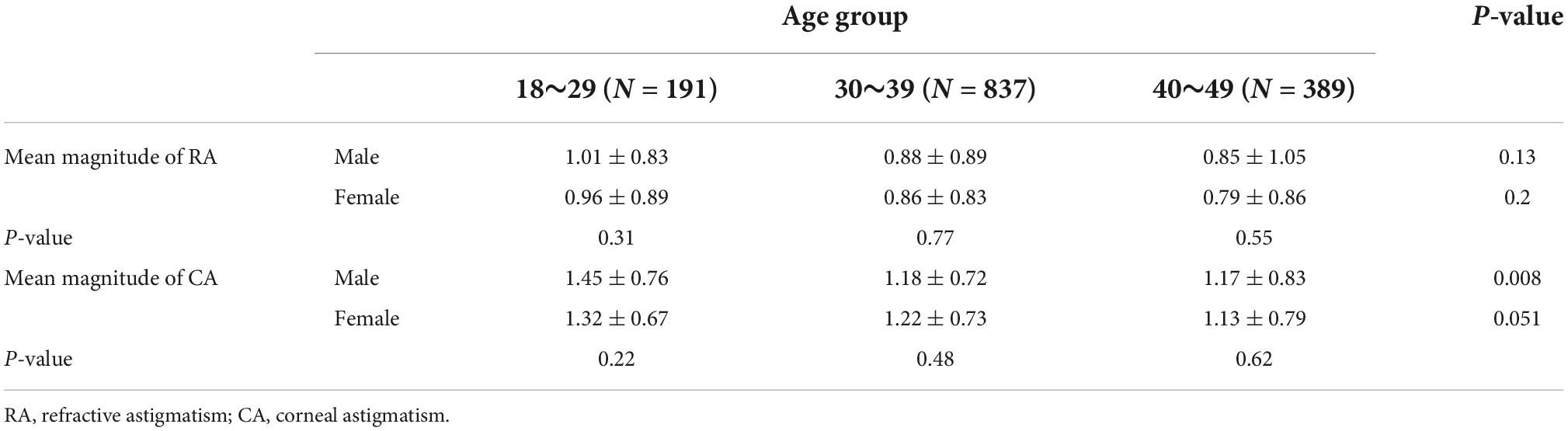
Table 2. Univariate comparison of the mean magnitude of refractive astigmatism and corneal astigmatism stratified by age and gender.
Most cases had with-the rule (WTR) astigmatism, followed by against-the rule (ATR) and oblique. Regarding to refractive astigmatism, 878 (88.15%) eyes had WTR astigmatism, 84 (8.43%) eyes had ATR astigmatism, 36 (3.61%) eyes had oblique astigmatism. The distribution was similar in corneal astigmatism, in which 1,203 (86.92%) eyes had WTR astigmatism, 99 eyes (7.15%) had ATR astigmatism, and 82 eyes (5.92%) had oblique astigmatism. Figure 1 are double-angle plots of RA and CA, data are scattered mostly to the left of the center, indicating that RA and CA tend to have a with the rule pattern.
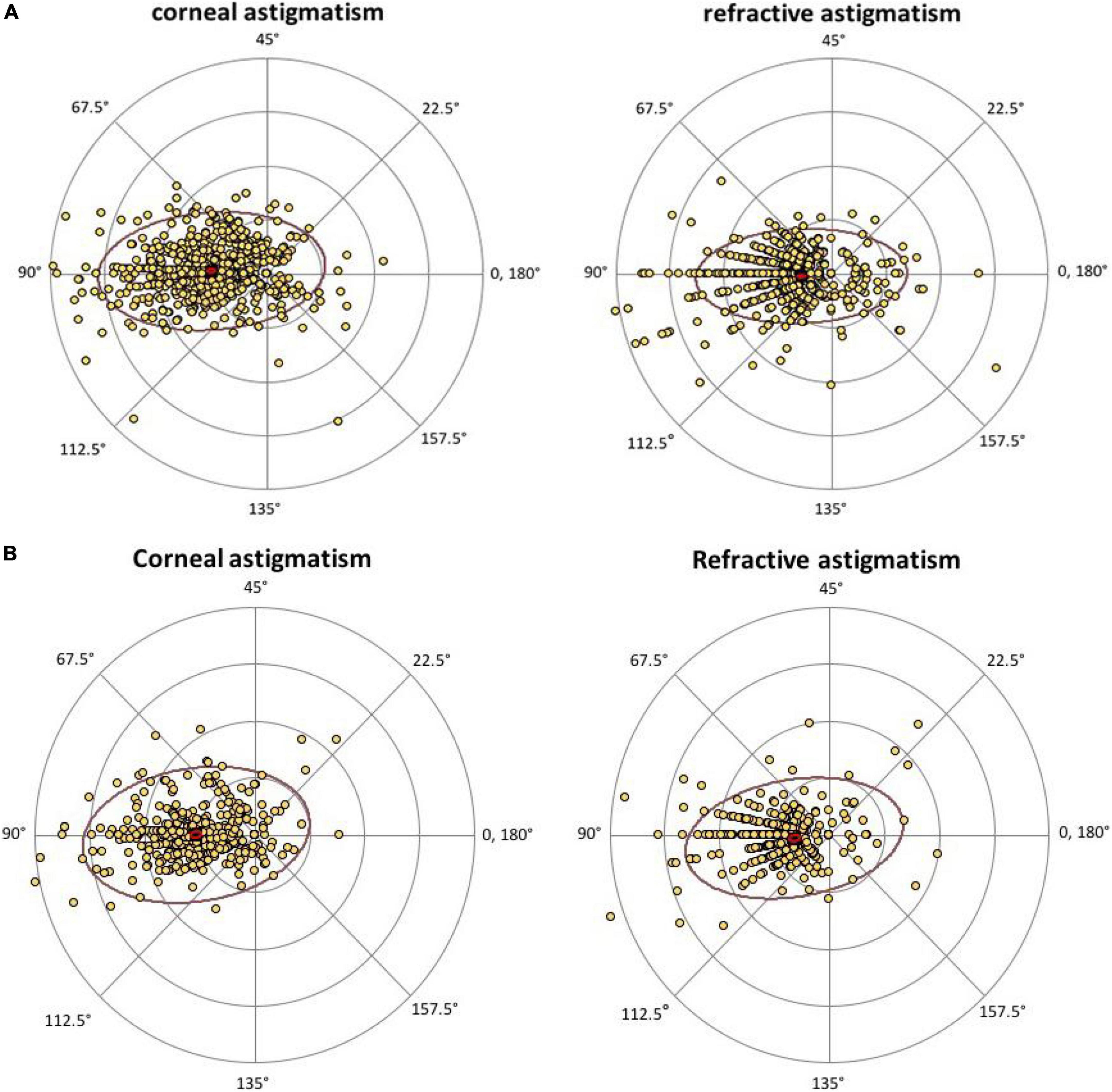
Figure 1. Double-angle plot of refractive astigmatism and corneal astigmatism in male (A) and female (B). Data are scattered mostly to the left of the center, indicating that RA and CA tend to have a with-the-rule pattern. RA, refractive astigmatism; CA, corneal astigmatism.
For the axis of refractive astigmatism and corneal astigmatism, there was no significant difference between men and women eyes in the percentage of WTR, ATR, and oblique at any age group. While the percentage of WTR, ATR, and oblique astigmatism was significantly different among different age groups, there was a shift in astigmatism from WTR to ATR with advancing age (Figure 2).
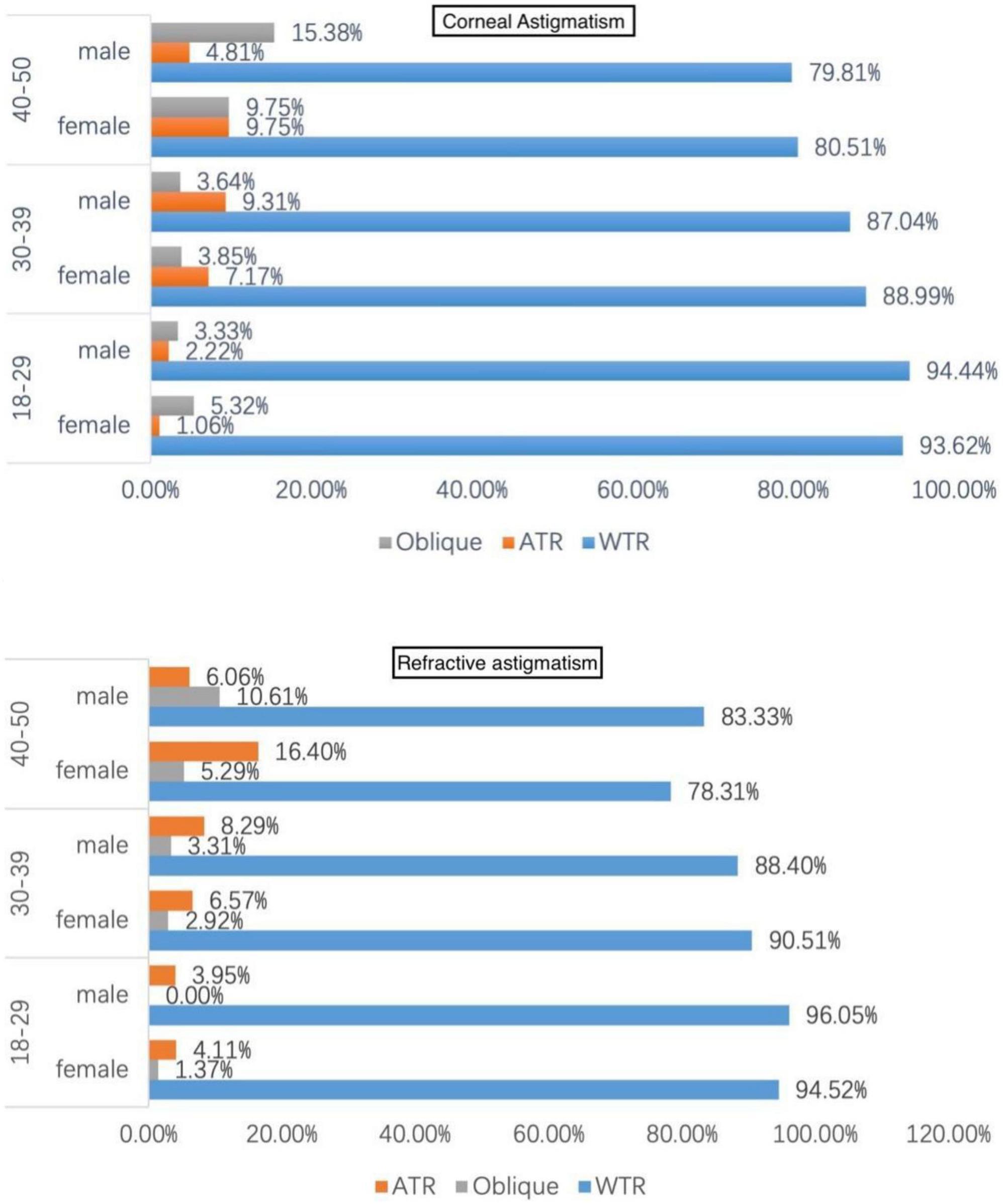
Figure 2. Distribution of astigmatism axis stratified by gender and age. WTR, with-the-rule; ATR, against-the-rule.
The correlations between corneal astigmatism and demographic and ocular parameters were analyzed by multivariate linear regression. Age, CCT, sphere, RA, and corneal curvature (Km) were correlated with CA (standardized coefficients of are 0.006, p = 0.011 for age, −0.001, p = 0.004 for CCT, and −0.027, p < 0.001 for sphere, 0.61, p < 0.001 for TA, −0.05, p < 0.001 for mean corneal curvature), as shown in Table 3. RA had the most significant correlation with CA, followed by corneal curvature, sphere, age, and CCT.
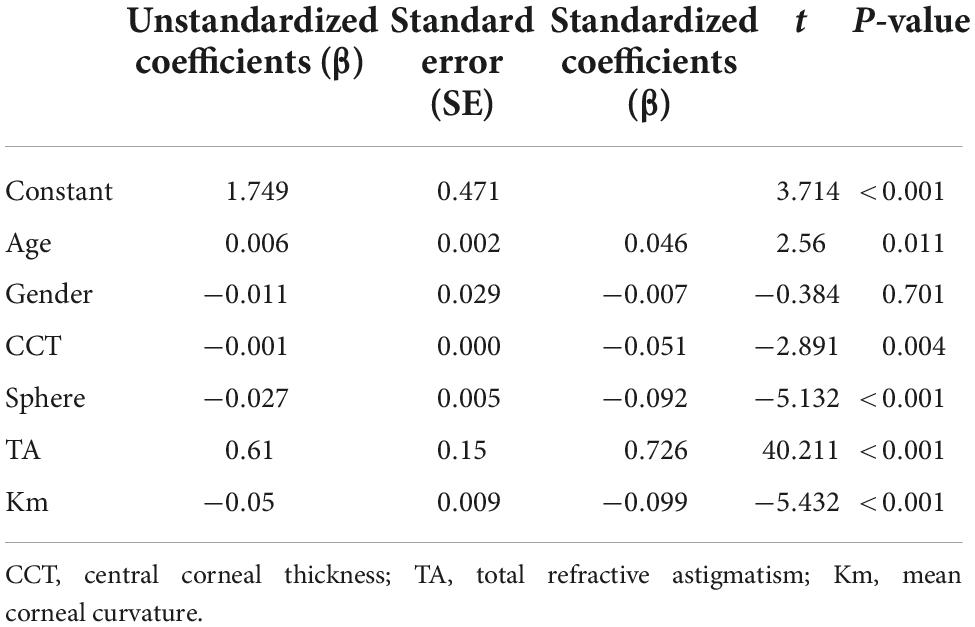
Table 3. Multiple linear regression model estimating the correlation between age, gender, central corneal thickness, sphere, corneal curvature, and corneal astigmatism.
Discussion
Sex difference exists in a wide range of the eye. For instance, a large number of studies found that males have different axil length and anterior chamber depth with females (5, 13, 14). In this study, we found that males had thicker corneal thickness than females, and females had steeper corneal curvature than males, Wang’s study also represented the same results (15). Therefore, it’s of importance to take sex effect into consideration when setting up the eye’s “average” values.
Regarding the myopic population, previous literature has focused on the characteristics of astigmatism and its correlation with other ocular parameters, while differences in age and sex of myopic populations have been rarely reported (16, 17). The prevalence of refractive astigmatism in our study was 68.73%, one study conducted in school students of eastern China found the prevalence of refractive astigmatism was 7∼25% and increased with grade (18). The prevalence of corneal astigmatism in our study was 85.39%. Other studies reported the prevalence of corneal astigmatism was around 60% (10, 19), this inconsistency was due to the definition of astigmatism used and the age and ethnicity of population examined. Although previous studies described a sex-related difference for the magnitude of astigmatism, this wasn’t shown in our study. But those studies were conducted in European (20) or African population (21), other studies in Asian population didn’t observe the sex difference either (22, 23).
Regarding to age-related difference, the magnitude of total refractive astigmatism did not appear to be age dependent in our study, while the magnitude of corneal astigmatism decreased with age, previous studies also found that patients age was negatively correlated with the magnitude of corneal astigmatism (9, 24, 25). One explanation is that the intraocular astigmatism increased with age, which comprise the effect of corneal astigmatism on the total refractive astigmatism. The age-related changes in the axis of the refractive and corneal astigmatism have been described in several studies (26–28), they found that there was a shift in astigmatism from with-the-rule to against-the-rule with increase in age, which was also presented in our study. Although the exact mechanism of astigmatism is still unknown, this age-related change is thought to be related to changes in the collagen orientation and the position and extension of the lid, and extraocular muscles (4, 29, 30).
It’s well known that corneal astigmatism is the leading cause of refractive astigmatism. In our study, we found that corneal astigmatism was strongly positive correlated with refractive astigmatism, which was consistent with previous studies (31). We also found that central corneal thickness and corneal curvature have a weak but significant correlation with corneal astigmatism. This relationship between corneal astigmatism and corneal thickness and corneal curvature was rarely reported before. Yuta Ueno and associates found that the difference between horizontal and vertical corneal thickness was correlated with the posterior corneal astigmatism (32), Zhou X etc., discovered that the front and back curvatures and the back astigmatism correlate with the distribution of corneal thickness (33). In addition, we also found that myopia is associated with increased astigmatism, which was also found in a large German population-based study (34).
There are several limitations in our study. First, we are unable to measure intraocular astigmatism, therefore, we were not able to describe the changes of posterior cornea or lens astigmatism. Second, our data only included cases with an age range from 18 to 50 years, therefore we can’t describe characteristics of astigmatism during childhood or the elderly population. Third, we didn’t include anterior chamber depth and axial length in the association analysis of astigmatism, which needs further investigation.
Conclusion
In summary, our study found that there was a sex-related difference in corneal thickness and corneal power, but not in refractive and corneal astigmatism in young adults. In addition, corneal astigmatism was associated with age, corneal thickness, corneal power, and spherical refraction. We confirmed that there was a change from with-the-rule astigmatism to against-the-rule astigmatism in young adults.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Peking Union Medical College Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lopes MC, Hysi PG, Verhoeven VJ, Macgregor S, Hewitt AW, Montgomery GW, et al. Identification of a candidate gene for astigmatism. Invest Ophthalmol Vis Sci. (2013) 54:1260–7. doi: 10.1167/iovs.12-10463
2. Feizi S, Naderan M, Ownagh V, Sadeghpour F. Distribution of the anterior, posterior, and total corneal astigmatism in healthy eyes. Int Ophthalmol. (2018) 38:481–91. doi: 10.1007/s10792-017-0483-9
3. Kim JH, Kim M, Lee SJ, Han SB, Kong YT, Yang HK, et al. Age-related differences in ocular biometry in adult Korean population. BMC Ophthalmol. (2016) 16:146. doi: 10.1186/s12886-016-0328-8
4. Read SA, Collins MJ, Carney LG. A review of astigmatism and its possible genesis. Clin Exp Optom. (2007) 90:5–19. doi: 10.1111/j.1444-0938.2007.00112.x
5. Kenneth J, Hoffer GS. Effect of gender and race on ocular biometry. Int Ophthalmol. (2017) 57:137–42.
6. Sawada A, Tomidokoro A, Araie M, Iwase A, Yamamoto T. Refractive errors in an elderly Japanese population: the Tajimi study. Ophthalmology. (2008) 115:363–70.e3. doi: 10.1016/j.ophtha.2007.03.075
7. Logan NS, Davies LN, Mallen EA, Gilmartin B. Ametropia and ocular biometry in a U.K. university student population. Optom Vis Sci. (2005) 82:261–6. doi: 10.1097/01.opx.0000159358.71125.95
8. Naeser K, Savini G, Bregnhoj JF. Age-related changes in with-the-rule and oblique corneal astigmatism. Acta ophthalmologica. (2018) 96:600–6.
9. Hayashi K, Sato T, Sasaki H, Hirata A, Yoshimura K. Sex-related differences in corneal astigmatism and shape with age. J Cataract Refract Surg. (2018) 44:1130–9. doi: 10.1016/j.jcrs.2018.06.020
10. Prasher P, Sandhu JS. Prevalence of corneal astigmatism before cataract surgery in Indian population. Int Ophthalmol. (2017) 37:683–9.
11. Wajuihian SO. Characteristics of astigmatism in Black South African high school children. Afr Health Sci. (2017) 17:1160–71. doi: 10.4314/ahs.v17i4.25
12. Armstrong RA. Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic Physiol Optics. (2013) 33:7–14.
13. Gaurisankar ZS, van Rijn GA, Lima JEE, Ilgenfritz AP, Cheng Y, Haasnoot GW, et al. Correlations between ocular biometrics and refractive error: a systematic review and meta-analysis. Acta Ophthalmol. (2019) 97:735–43. doi: 10.1111/aos.14208
14. Sng CC, Foo LL, Cheng CY, Allen JC Jr., He M, Krishnaswamy G, et al. Determinants of anterior chamber depth: the Singapore Chinese eye study. Ophthalmology. (2012) 119:1143–50.
15. Wang Q, Liu W, Wu Y, Ma Y, Zhao G. Central corneal thickness and its relationship to ocular parameters in young adult myopic eyes. Clin Exp Optom. (2017) 100:250–4.
16. Wang J, Cheng QE, Fu X, Zhang R, Meng J, Gu F, et al. Astigmatism in school students of eastern China: prevalence, type, severity and associated risk factors. BMC Ophthalmol. (2020) 20:155. doi: 10.1186/s12886-020-01425-w
17. Hoffmann PC, Hutz WW. Analysis of biometry and prevalence data for corneal astigmatism in 23,239 eyes. J Cataract Refract Surg. (2010) 36:1479–85. doi: 10.1016/j.jcrs.2010.02.025
18. Williams KM, Verhoeven VJ, Cumberland P, Bertelsen G, Wolfram C, Buitendijk GH, et al. Prevalence of refractive error in Europe: the European Eye Epidemiology (E(3)) Consortium. Eur J Epidemiol. (2015) 30:305–15. doi: 10.1007/s10654-015-0010-0
19. Mashige KP, Jaggernath J, Ramson P, Martin C, Chinanayi FS, Naidoo KS. Prevalence of refractive errors in the INK Area, Durban, South Africa. Optom Vis Sci. (2016) 93:243–50. doi: 10.1097/OPX.0000000000000771
20. Varma R, Torres M, McKean-Cowdin R, Rong F, Hsu C, Jiang X. Prevalence and risk factors for refractive error in adult Chinese Americans: The Chinese American Eye Study. Am J Ophthalmol. (2017) 175:201–12.
21. Kato K, Kondo M, Takeuchi M, Hirano K. Refractive error and biometrics of anterior segment of eyes of healthy young university students in Japan. Sci Rep. (2019) 9:15337. doi: 10.1038/s41598-019-51920-4
22. Naeser K, Savini G, Bregnhøj JF. Age-related changes in with-the-rule and oblique corneal astigmatism. Acta Ophthalmol. (2018) 96:600–6.
23. Shao X, Zhou KJ, Pan AP, Cheng XY, Cai HX, Huang JH, et al. Age-related changes in corneal astigmatism. J Refract Surg. (2017) 33:696–703.
24. Rozema JJ, Hershko S, Tassignon MJ. The components of adult astigmatism and their age-related changes. Ophthalmic Physiol Optics. (2019) 39:183–93.
25. Kim H, An Y, Joo CK. Gender-differences in age-related changes of corneal astigmatism in Korean cataract patients. BMC Ophthalmol. (2019) 19:31. doi: 10.1186/s12886-018-1001-1
26. Ueno Y, Hiraoka T, Beheregaray S, Miyazaki M, Ito M, Oshika T. Age-related changes in anterior, posterior, and total corneal astigmatism. J Refract Surg. (2014) 30:192–7.
27. Niederer RL, Perumal D, Sherwin T, McGhee CN. Age-related differences in the normal human cornea: a laser scanning in vivo confocal microscopy study. Br J Ophthalmol. (2007) 91:1165–9. doi: 10.1136/bjo.2006.112656
28. Bagheri A, Farahi A, Guyton DL. Astigmatism induced by simultaneous recession of both horizontal rectus muscles. J AAPOS. (2003) 7:42–6. doi: 10.1067/mpa.2003.S1091853102420071
29. Jaime Tejedor AG. Agreement between refractive and corneal stigmatism in psuedopjakic eyes. Cornea. (2013) 32:783–90.
30. Ueno Y, Hiraoka T, Miyazaki M, Ito M, Oshika T. Corneal thickness profile and posterior corneal astigmatism in normal corneas. Ophthalmology. (2015) 122:1072–8.
31. Zhou X, Wang L, Chu R, Yu Z. [Corneal thickness distribution and its relationship with corneal topography in ametropic population]. Zhonghua Yan Ke Za Zhi. (2014) 50:658–64.
32. Schuster AK-G, Pfeiffer N, Schulz A, Hoehn R, Ponto KA, Wild PS, et al. Refractive, corneal and ocular residual astigmatism: distribution in a German population and age-dependency - the Gutenberg health study. Graefes Arch Clin Exp Ophthalmol. (2017) 255:2493–501.
33. Hu Y, Zhu S, Xiong L, Fang X, Liu J, Zhou J, et al. A multicenter study of the distribution pattern of posterior corneal astigmatism in Chinese myopic patients having corneal refractive surgery. Sci Rep. (2020) 10:16151. doi: 10.1038/s41598-020-73195-w
Keywords: age, gender, astigmatism, cornea, myopia
Citation: Yang S, Jiang Y, Cui G and Li Y (2022) Age- and gender-related characteristics of astigmatism in a myopic population. Front. Med. 9:1011743. doi: 10.3389/fmed.2022.1011743
Received: 06 August 2022; Accepted: 26 September 2022;
Published: 13 October 2022.
Edited by:
Jinhai Huang, Fudan University, ChinaReviewed by:
Haijiang Lin, Massachusetts Eye and Ear and Harvard Medical School, United StatesMatteo Nioi, Università di Cagliari, Italy
Zhao Shaozhen, Tianjin Medical University Eye Hospital, China
Copyright © 2022 Yang, Jiang, Cui and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Li, bGl5aW5ncHVtY2hAMTI2LmNvbQ==
 Shan Yang
Shan Yang Yang Jiang
Yang Jiang Ge Cui
Ge Cui Ying Li*
Ying Li*