- Quality Use of Medicines and Pharmacy Research Centre, UniSA Clinical and Health Sciences, University of South Australia, Adelaide, SA, Australia
Objectives: Large population-based studies examining frailty trajectory found a linear increase in frailty over time. The pattern in which frailty changes over time for an individual person is less well-described. We examined the frailty trajectory of older adults living in aged-care in Australia.
Materials and methods: This secondary study used data from a randomised controlled trial involving 39 aged-care facilities in Australia. The trial intervention was an on-going pharmacist-led intervention occurring every 8 weeks over 12 months aimed at preventing medicine-induced deterioration and adverse reactions. Frailty was assessed using the Frailty Index. Participants were categorised as non-frail, pre-frail and frail. Individual frailty trajectory over 12 months was visualised using the alluvial plot. Case notes were examined to explore reasons for any rapid transitions in frailty status.
Results: A total of 248 participants was included. At baseline, 40.3% were non-frail and 59.7% were pre-frail. The proportion of participants who were non-frail and pre-frail decreased over time; 15.7% were frail at 6 months and 23.4% were frail at 12 months. Overall, twenty different combinations of frailty transitions were identified over 12 months. Retrospective analysis of case notes suggest that death or transition from non-frail to frail was often preceded by hospitalisation, falls, medication change or clinically significant deterioration in grip strength or cognition.
Conclusion: The degree of frailty increased over time, but there were variations in the individual trajectories. Regular monitoring of events that precede changes in frailty status is needed to identify strategies to prevent further deterioration in residents’ conditions.
Introduction
Frailty is a state of increased vulnerability to external stressors due to a decline in reserve and function across multiple physiological systems (1, 2). The two most common operational definitions of frailty are the Frailty Index which is based on the deficit accumulation approach (3) and the frailty phenotype based primarily on physical components (4). Prevalence of frailty increases with age (5). A 2021 systematic review of 240 studies found the pooled prevalence of frailty was 11% for studies that included individuals age 50 years and above, while the pooled prevalence for studies in adults age 90 years and above was 51% (5). Frail individuals have an increased risk of adverse outcomes including mortality, hospitalisation, disability, cognitive impairment, falls and fractures, delirium, and nursing home admission (6–11). In Australia, up to one in two older adults are considered frail (11). The prevalence of frailty is expected to rise as the number of older adults in Australia continues to grow (12). In 2020, older people make up 16% of Australia’s population (12). It is estimated that by 2066, the proportion of older people in Australia will increase to about 23% (12).
The majority of population-based studies examining frailty trajectory found a linear increase in frailty over time (13–16). Studies that attempted to group frailty progression found that frailty trajectories can be broadly categorised into three types: rapidly increasing, moderately increasing, and stable frailty (14, 17). Individuals with rapidly increasing frailty were twice as likely to die within a year than those with stable frailty (14). What is less well described in the literature is the pattern in which frailty changes over time for an individual person and the frailty trajectory of older adults living in aged-care facilities. A 12-year longitudinal study in Europe reported that the rate of frailty fluctuations (i.e., up and down change in frailty) increases with age (16), meaning that the oldest in the population are likely to experience the most variations in their frailty trajectory.
In this descriptive study using data from a 12-month randomised controlled trial (18), this study aims to examine the frailty trajectory of 248 older adults living in residential aged care facilities in Australia. We graphically represent the frailty trajectory of each person according to trial arms, and explore the possible reasons for rapid changes in frailty (e.g., non-frail to death within 6 months) by examining individual case notes.
Materials and methods
This paper describes a secondary study conducted using data from the Reducing Medicine-Induced Deterioration and Adverse Reactions (ReMInDAR) Trial (18, 19). The ReMInDAR trial was a multicentre, open-label, randomised controlled trial involving 39 aged care facilities in Australia occurring between August 2018 and June 2020. The Australian government subsidises a range of aged care services including care in the home, short-term care, and residential aged care (20). The term residential aged care in Australia is synonymous with nursing homes in the USA where care is provided 24 h a day, 7 days a week to relatively frail older residents.
Participants
Residents were eligible to participate in the trial if they were taking at least four medicines or at least one medicine with anticholinergic or sedative properties. Residents were excluded if they were frail (>0.40 on the Frailty Index) (11, 21), had moderate or severe dementia [Psychogeriatric Assessment Scales < 12/21 (22) or Montreal Cognitive Assessment MoCA ≤ 17/30] (23), or were receiving palliative or respite care. The ReMInDAR trial (19) aimed to identify early onset of medicine-induced deterioration. For individuals who were already frail or with dementia, we considered it unlikely that the pharmacist intervention involving changes in medicines will have a significant impact on the person’s condition. Further, our study adopted an “opt out” approach which meant that residents needed to have the capacity to decline participation if they wish to do so. Participants who enrolled in the trial were included in this secondary study.
Intervention
The trial intervention was an on-going pharmacist-led intervention occurring every 8 weeks over 12 months aimed at preventing medicine-induced deterioration and adverse reactions.
Outcome
The trial primary outcome was change in Frailty Index from baseline to 12 months (11). The Frailty Index is a multi-dimensional assessment encompassing physical, medical, psychological, and social factors to measure frailty. The Frailty Index consists of 39 variables and ranges from 0 to 1 with 0 being the least frail.
The secondary outcomes were changes in cognition as measured using the Montreal Cognitive Assessment (23), 24-h movement behaviour measured using the GENEActiv accelerometer (24), grip strength measured using a handheld dynamometer, weight extracted from the resident serial weight chart, adverse events (e.g., falls, delirium, hospitalisation) and quality of life measured using the EQ-5D (25). Outcome assessments for all participants were conducted by independent research assistants at baseline, 6 and 12 months.
Analysis
For the purpose of this secondary study, only the primary outcome (Frailty Index), which was of interest to understand frailty trajectory, was analysed. Participants were categorised at baseline as non-frail (Frailty Index < 0.25), pre-frail (≥0.25 to 0.4), and frail (>0.40) using previously validated Frailty Index cut-offs (21).
Descriptive statistics were used to summarise participants’ baseline characteristics. Baseline characteristics were presented as means (standard deviation) for continuous variables and as counts (percentage) for categorical variables. Individual frailty trajectory was visualised using the alluvial plot from the R package “ggalluvial.” Analyses were performed using the R statistical program, version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria) (26).
For participants who had a rapid progression in frailty (e.g., from non-frail to frail or non-frail to death within 6 months), we retrospectively examined individual case notes recorded by the trial pharmacists and research assistants to identify possible reasons for the change, and whether the pharmacists’ review and assessment using validated tools identified deterioration in participants’ health.
Results
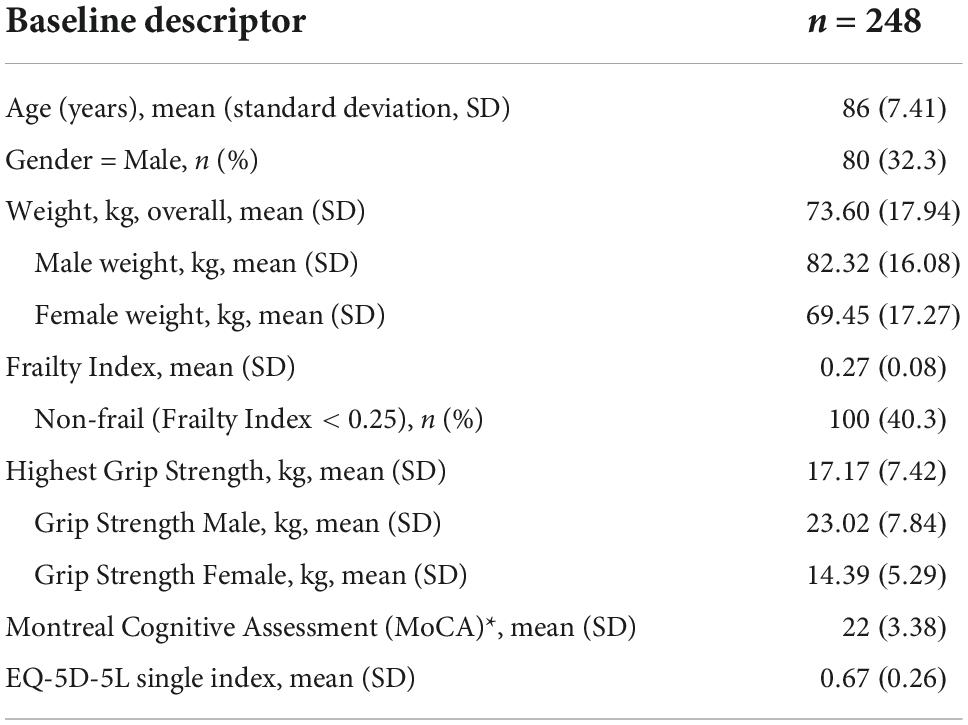
A total of 248 participants were included in this secondary study. The mean age of participants was 86 years and a third (32%) of the participants were men. The baseline characteristics of all participants included in this study is shown in Table 1.
At baseline, 40.3% of participants were non-frail (Frailty Index < 0.25) and 59.7% were pre-frail (0.25 ≥ Frailty Index ≤ 0.4) (Figure 1). No participants were frail at baseline, consistent with the trial exclusion criterion whereby residents with Frailty Index > 0.4 were excluded. The proportion of participants who were non-frail and pre-frail decreased over time; 15.7% of participants became frail at 6 months and 23.4% were frail at 12 months. Approximately 10% of participants died by 6 months and 16.1% by 12 months.
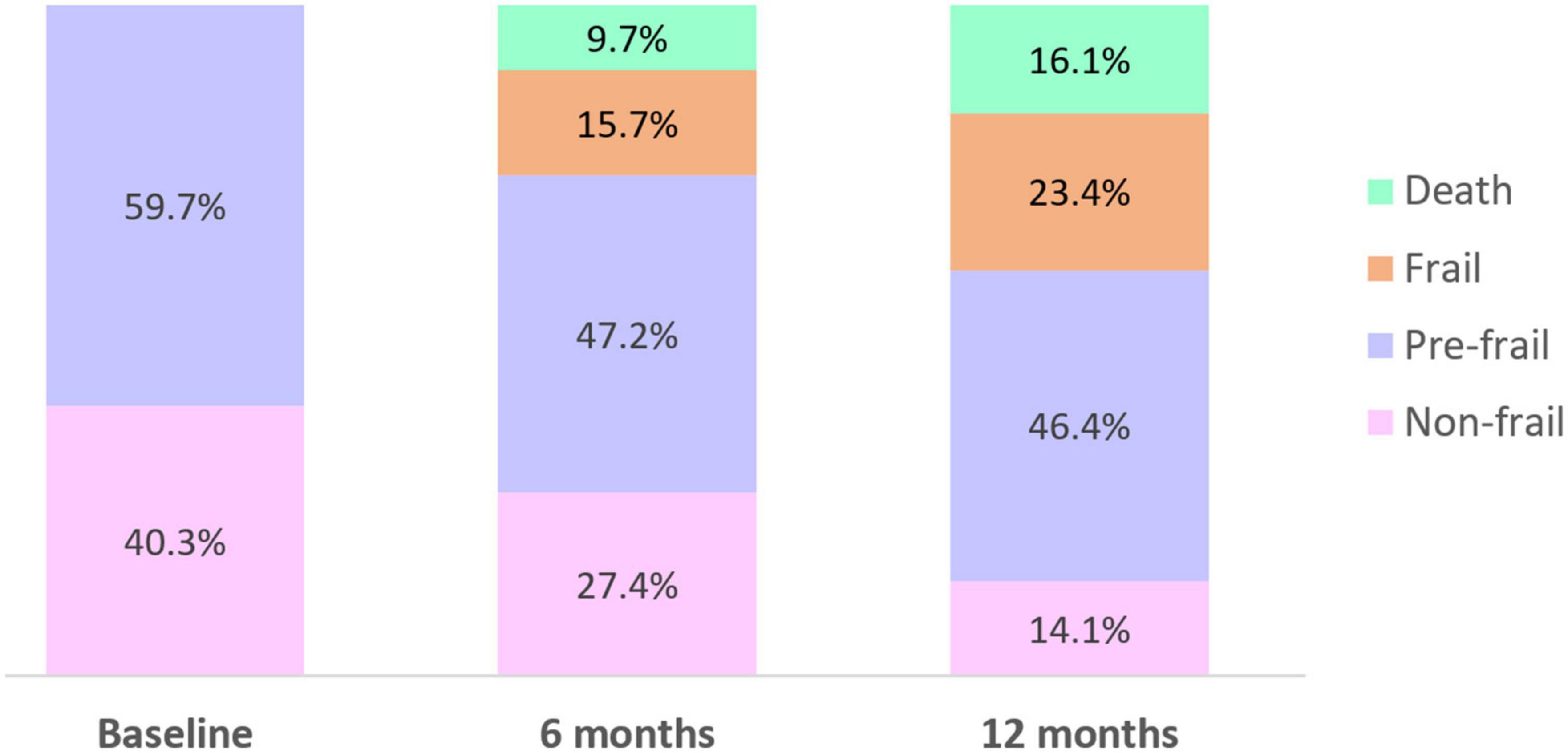
Figure 1. Proportion of participants who were non-frail, pre-frail, frail, or died over the 12-month study period.
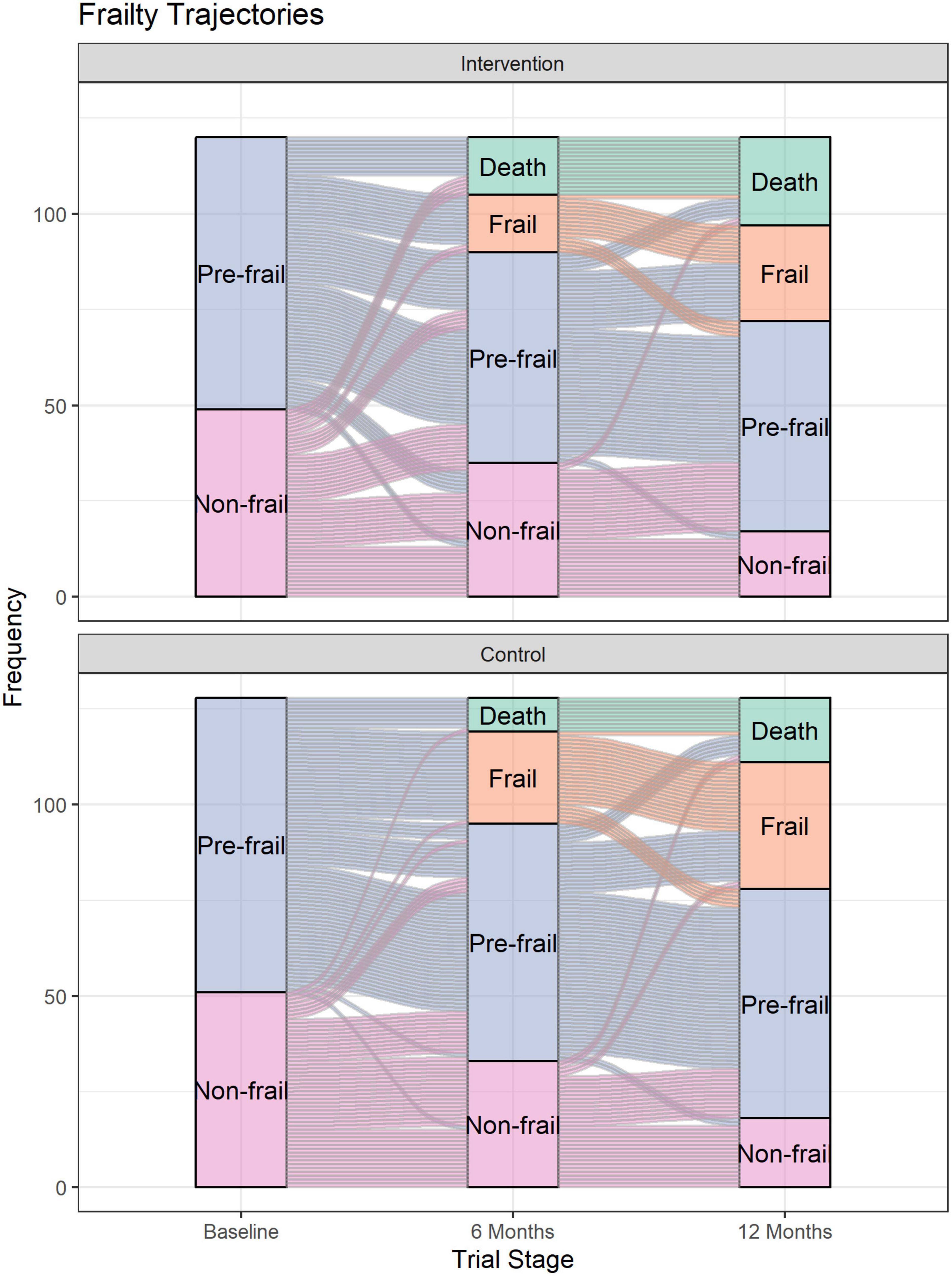
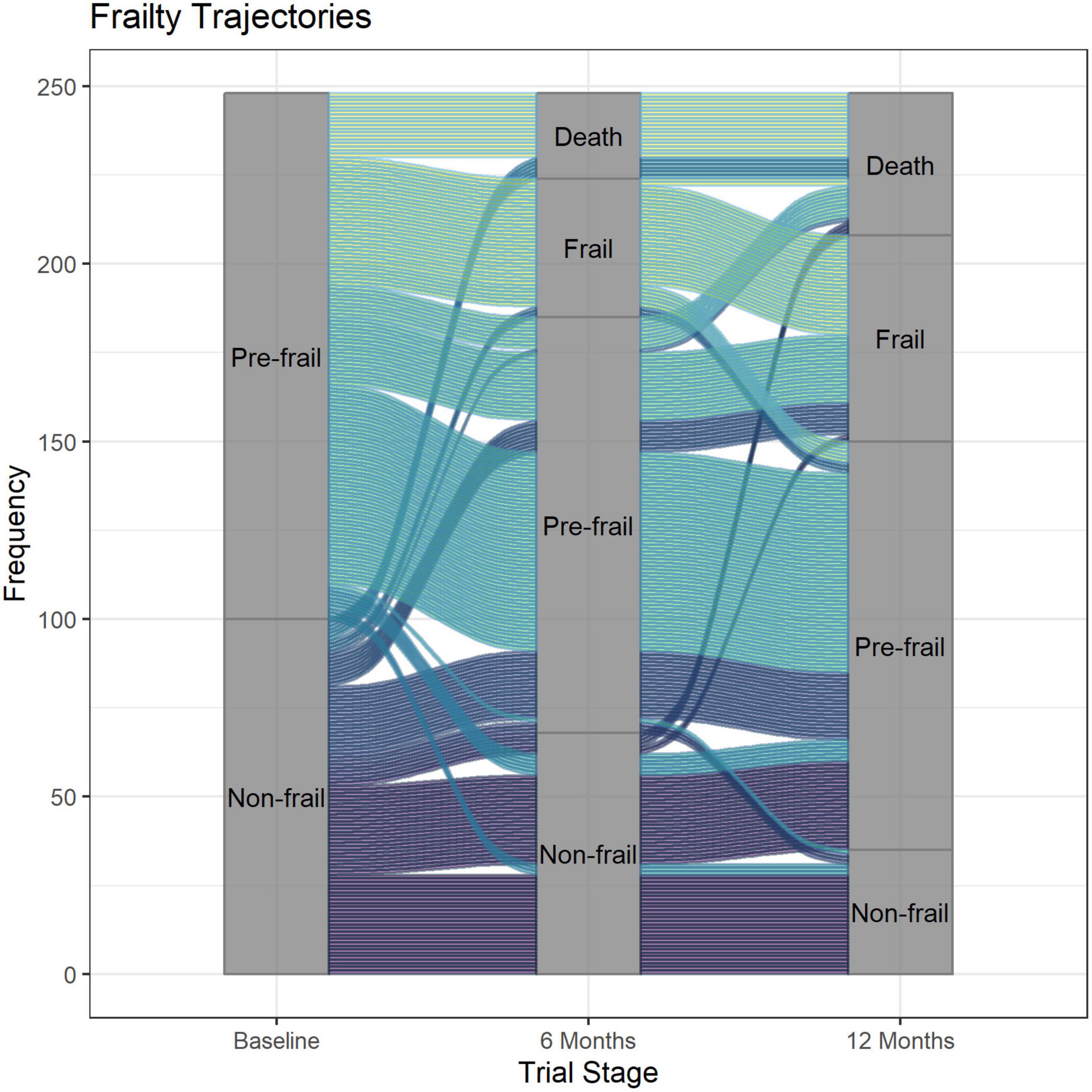
Figure 2 shows the individual trajectories for each participant from baseline to 12 months according to trial arm, while Figure 3 shows the trajectories of all participants from baseline to 12 months. There was an imbalance in the number of withdrawals due to death between the two trial groups. At the 6 months assessment, there were 15 (out of 120) and 9 (out of 128) deaths in the intervention and control groups, respectively. However, the imbalance in deaths predominantly occurred in the first 2 months, prior to the first intervention visit in the trial, with 5/120 deaths (4%) for intervention arm and 2/128 deaths (2%) for the control group.
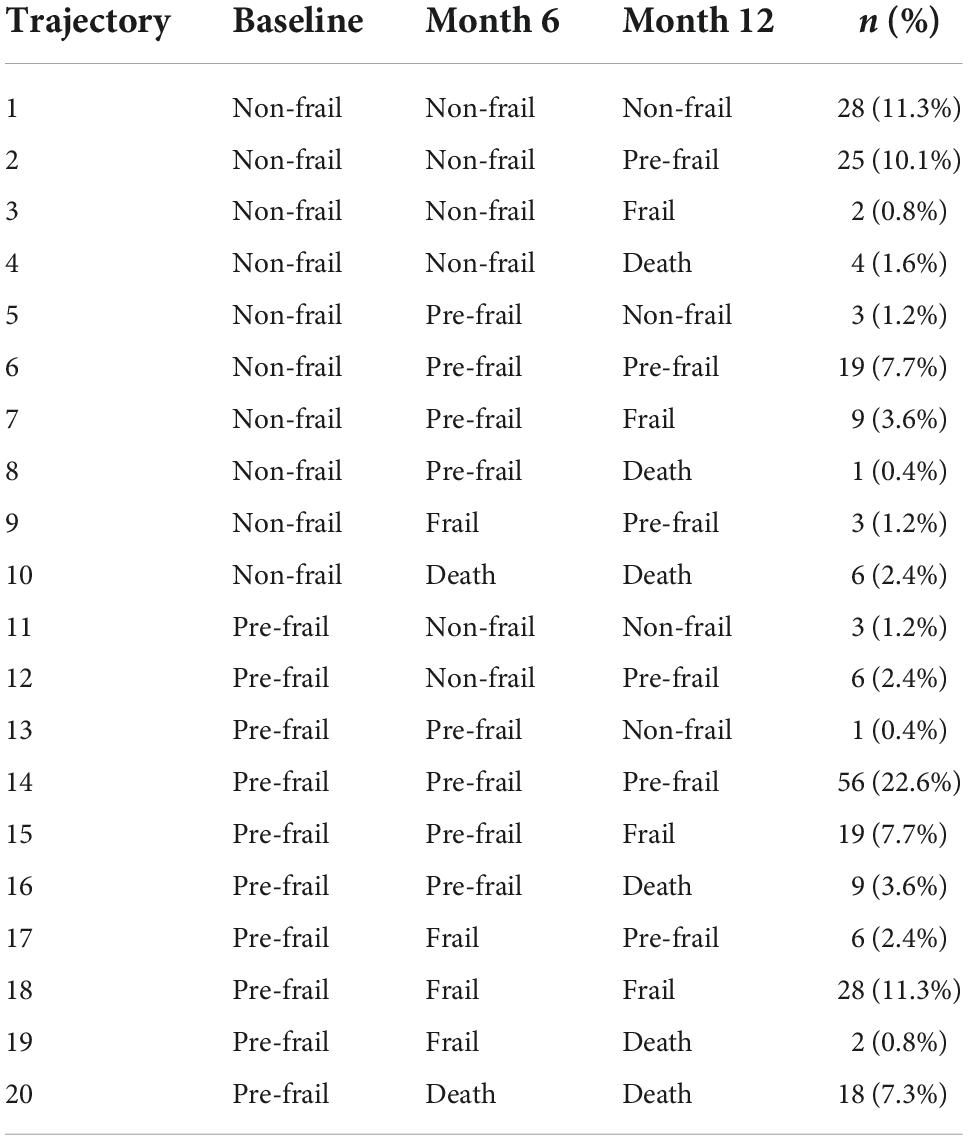
Overall, twenty different combinations of frailty transitions were identified over 12 months (Table 2). The two common combinations of frailty transitions for non-frail participants were “stable frailty” (i.e., participants who were non-frail at baseline continued to be non-frail at 6- and 12-months) and “moderately increasing frailty” (i.e., participants moved from being non-frail to pre-frail at 6- or 12 months). The three common combinations for participants who were pre-frail at baseline were “stable frailty” (i.e., participants who were pre-frail at baseline and continued to be pre-frail at 6- and 12-months), “moderately increasing frailty” (i.e., moved from being pre-frail to frail at 6- or 12 months) and “pre-frail to death.” Ten percent (n = 10) of all participants who were non-frail at baseline died by 12 months, while 20% (n = 30) of all participants who were pre-frail at baseline died by 12 months.
Twelve participants transitioned from non-frail to frail or death within a 6-month period. Retrospective analysis of case notes of the 12 participants suggest that death or transition from non-frail to frail was often preceded by hospitalisation, falls, medication change, or clinically significant deterioration as measured using grip strength or cognitive function test (Supplementary Table 1). Three participants who went from non-frail at baseline to frail at 6 months, transitioned back to pre-frail at 12 months (Supplementary Table 2). Similarly, the transition from non-frail to frail in the three participants were preceded by events such as falls, medication change or clinically significant deterioration in grip strength or cognition.
Discussion
Our results showed that frailty increased over time as the proportion of residents who were pre-frail and frail increased over the 12-month study period, consistent with findings from previous research (13–16). A higher proportion of participants who were pre-frail at baseline died at 12 months compared to those who were non-frail at baseline. In contrast to only three trajectories that are commonly reported (14, 17), our study adds to the existing literature by graphically representing the individual trajectory of older adults living in residential aged care facilities. By visualising the individual trajectory, we were able to show that individuals who seemed “stable” (i.e., had similar baseline and 12-month Frailty Index) did actually experience transient changes in frailty in between follow-ups.
Although most residents either remained stable or had worsening frailty over time, our visualisation shows that a small number of residents had initial worsening of frailty but subsequently experienced improvement in frailty (e.g., non-frail at baseline, frail at 6 months and pre-frail at 12 months). This supports the notion that frailty can, to some degree, be reversed (16, 27–29). For example, a longitudinal cohort study involving 1,735 participants in five European countries found that participants who increased their physical activity over a 12-month period have lower frailty compared to baseline (28). By analysing individual case notes, we found that residents who had initial worsening frailty (at 6-month follow up) followed by improvement in frailty at 12 months experienced sudden stressors (falls and infection), and subsequent recovery leading to improved frailty. Frailty can also potentially be reversed by interventions to reduce frailty; however, previous systematic reviews found mixed results regarding the effectiveness of interventions to reduce or prevent frailty (27, 30). In our randomised controlled trial which involved a pharmacist-led intervention, we found no statistically significant difference in the change in Frailty Index between the intervention and the control groups (18). Our final sample for the trial was short of our required sample size of 354 persons, leaving the study under-powered for its primary endpoint (change in Frailty Index). The recruitment shortfall in the trial was in part due to the high proportion of residents in aged-care in Australia that are already frail. Despite using a Frailty Index cut off of 0.4, only 8% of the Australian aged-care population in the facilities recruited were eligible for our intervention.
One could argue that the within-individual change in frailty over time observed in our study was due to inter-operator variability in the assessment of Frailty Index, and not due to an actual change due to incidents with temporary harm such as infections and injury. However, we found similar fluctuations in scores measured using other validated tools (grip strength and cognition) for those in the intervention arm (19), suggesting that the within-individual changes in frailty are likely a true effect rather than inconsistency in measurement. Research has also shown that grip strength is correlated with frailty index (31), thus providing further support that that within-individual changes are a true effect.
To the best of our knowledge, this is the first study to visualise individual frailty trajectories and investigate reasons behind rapid changes in frailty among older adults living in aged care facilities (mean age 86). A recent study using the Irish Longitudinal Study of Ageing (TILDA) dataset similarly visualised frailty trajectories using the alluvial plot; however, the study included a younger cohort living in the community with a mean age of 63.8 years at baseline (32). The large number of frailty trajectories suggests that older adults in late life should be assessed regularly for signs and symptoms of deterioration, so that interventions can be implemented to prevent further deterioration. Interventions such as exercise and muscle strength training have been shown to be effective to delay or reverse frailty (33, 34). Our study had some limitations. We included a less frail population within the aged-care setting in our trial and therefore our results may not be generalisable to all aged care residents. The latter part of the trial (March to June 2020) was impacted by the COVID pandemic, which affected some of our 12 month data collection as our research assistants could not attend the facilities during that time. Frailty assessment was therefore delayed for a small number of participants.
Conclusion
The degree of frailty increased over time in the aged care population, but there were variations in the individual trajectories experienced by residents. Regular monitoring of events that precede changes in frailty status is needed to identify strategies to prevent further deterioration in residents’ conditions. Future studies could consider visualising frailty trajectory for all residents and understanding the impact of COVID-19 including any restrictions due to the pandemic on frailty trajectories in aged care residents.
Data availability statement
The data analysed in this study is subject to the following licences/restrictions: Requests for de-identified data can be made to the Principal Investigator. Requests to access these datasets should be directed to bGliYnkucm91Z2hlYWRAdW5pc2EuZWR1LmF1.
Ethics statement
The studies involving human participants were reviewed and approved by University of South Australia Human Research Ethics Committee. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
RL, T-LK, RB, and EER: acquisition, analysis or interpretation of data, and statistical analysis. RL: drafting of the manuscript. All authors contributed to the study concept and design and critical revision of the manuscript for important intellectual content, contributed to the article, and approved the submitted version.
Funding
This study used data from the ReMInDAR trial. This trial was funded by the Australian Government Department of Health as part of the Sixth Community Pharmacy Agreement. RL was supported by a National Health and Medical Research Council (NHMRC) fellowship APP1156368. EER was supported by an NHMRC Senior Principal Research Fellowship APP1110139.
Acknowledgments
We thank the trial participants, pharmacists, general practitioners and the staff of residential aged-care facilities, and research assistants for their support and participation. We also thank members of the stakeholder advisory group and the consumer advisory committee for their valuable advice and support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.1010444/full#supplementary-material
References
1. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. (2013) 381:752–62. doi: 10.1016/S0140-6736(12)62167-9
2. Xue Q-L. The frailty syndrome: definition and natural history. Clin Geriatr Med. (2011) 27:1–15. doi: 10.1016/S0140-6736(12)62167-9
3. Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal. (2001) 1:323–36. doi: 10.1100/tsw.2001.58
4. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A Biol Sci Med Sci. (2001) 56:M146–56. doi: 10.1093/gerona/56.3.M146
5. O’Caoimh R, Sezgin D, O’Donovan MR, Molloy DW, Clegg A, Rockwood K, et al. Prevalence of frailty in 62 countries across the world: a systematic review and meta-analysis of population-level studies. Age Ageing. (2021) 50:96–104. doi: 10.1093/ageing/afaa219
6. Hubbard RE, Peel NM, Samanta M, Gray LC, Mitnitski A, Rockwood K. Frailty status at admission to hospital predicts multiple adverse outcomes. Age Ageing. (2017) 46:801–6. doi: 10.1093/ageing/afx081
7. Kojima G. Quick and simple FRAIL scale predicts incident activities of daily living (ADL) and instrumental ADL (IADL) disabilities: a systematic review and meta-analysis. J Am Med Direct Assoc. (2018) 19:1063–8. doi: 10.1016/j.jamda.2018.07.019
8. Ekram A, Woods RL, Britt C, Espinoza S, Ernst ME, Ryan J. The association between frailty and all-cause mortality in community-dwelling older individuals: an umbrella review. J Frailty Aging. (2021) 10:320–6.
9. Fompeyrine C, Abderhalden LA, Mantegazza N, Hofstetter N, Bieri-Brüning G, Bischoff-Ferrari HA, et al. Frailty is associated with increased mortality in older adults 12 months after discharge from post-acute care in Swiss nursing homes. J Frailty Aging. (2021) 10:233–6. doi: 10.14283/jfa.2020.58
10. Kiiti Borges M, Oiring de Castro Cezar N, Silva Santos Siqueira A, Yassuda M, Cesari M. Aprahamian I. The relationship between physical frailty and mild cognitive impairment in the elderly: a systematic review. J Frailty Aging. (2019) 8:192–7. doi: 10.14283/jfa.2019.29
11. Widagdo IS, Pratt N, Russell M, Roughead EE. Predictive performance of four frailty measures in an older Australian population. Age Ageing. (2015) 44:967–72. doi: 10.1093/ageing/afv144
12. Australian Institute of Health and Welfare. Older Australians. (2021). Available online at: https://www.aihw.gov.au/reports/older-people/older-australians/contents/demographic-profile (accessed October 5, 2022).
13. Welstead M, Jenkins ND, Russ T, Luciano M, Muniz-Terrera G. A systematic review of frailty trajectories: their shape and influencing factors. Gerontologist. (2020) 61:e463–e475. doi: 10.1093/geront/gnaa061
14. Stow D, Matthews FE, Hanratty B. Frailty trajectories to identify end of life: a longitudinal population-based study. BMC Med. (2018) 16:171. doi: 10.1186/s12916-018-1148-x
15. Hoogendijk EO, Rockwood K, Theou O, Armstrong JJ, Onwuteaka-Philipsen BD, Deeg DJH, et al. Tracking changes in frailty throughout later life: results from a 17-year longitudinal study in the Netherlands. Age Ageing. (2018) 47:727–33. doi: 10.1093/ageing/afy081
16. Stolz E, Mayerl H, Freidl W. Fluctuations in frailty among older adults. Age Ageing. (2019) 48:547–52.
17. Hsu HC, Chang WC. Trajectories of frailty and related factors of the older people in Taiwan. Exp Aging Res. (2015) 41:104–14. doi: 10.1080/0361073X.2015.978219
18. Lim R, Bereznicki L, Corlis M, Kalisch Ellett LM, Kang AC, Merlin T, et al. Reducing medicine-induced deterioration and adverse reactions (ReMInDAR) trial: study protocol for a randomised controlled trial in residential aged-care facilities assessing frailty as the primary outcome. BMJ Open. (2020) 10:e032851. doi: 10.1136/bmjopen-2019-032851
19. Roughead EE, Pratt NL, Parfitt G, Rowett D, Kalisch-Ellett LM, Bereznicki L, et al. Effect of an ongoing pharmacist service to reduce medicine-induced deterioration and adverse reactions in aged-care facilities (nursing homes): a multicentre, randomised controlled trial (the ReMInDAR trial). Age Ageing. (2022) 51:afac092. doi: 10.1093/ageing/afac092
20. Australian Government Department of Health and Aged Care. What is Aged Care?. (2020). Available online at: https://www.health.gov.au/health-topics/aged-care/about-aged-care/what-is-aged-care#types-of-aged-care-services (accessed October 5, 2022).
21. Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol Ser A. (2007) 62:722–7. doi: 10.1093/gerona/62.7.722
22. Australian Government Department of Health. Psychogeriatric Assessment Scales (PAS) User Guide. (2016). Available online at: https://agedcare.health.gov.au/aged-care-funding/residential-care-subsidy/basic-subsidy-amount-aged-care-funding-instrument/psychogeriatric-assessment-scales-pas-user-guide (accessed December 12, 2016).
23. Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. (2005) 53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x
24. Esliger DW, Rowlands AV, Hurst TL, Catt M, Murray P, Eston RG. Validation of the GENEA accelerometer. Med Sci Sports Exerc. (2011) 43:1085–93. doi: 10.1080/0361073X.2015.978219
25. Rabin R, Charro FD. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. (2009) 33:337–43. doi: 10.3109/07853890109002087
26. R Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing (2013).
27. Puts MTE, Toubasi S, Andrew MK, Ashe MC, Ploeg J, Atkinson E, et al. Interventions to prevent or reduce the level of frailty in community-dwelling older adults: a scoping review of the literature and international policies. Age Ageing. (2017) 46:383–92. doi: 10.1093/ageing/afw247
28. Zhang X, Tan SS, Franse CB, Bilajac L, Alhambra-Borrás T, Garcés-Ferrer J, et al. Longitudinal association between physical activity and frailty among community-dwelling older adults. J Am Geriatr Soc. (2020) 68:1484–93. doi: 10.1111/jgs.16391
29. Arrieta H, Rezola-Pardo C, Gil SM, Virgala J, Iturburu M, Antón I, et al. Effects of multicomponent exercise on frailty in long-term nursing homes: a randomized controlled trial. J Am Geriatr Soc. (2019) 67:1145–51. doi: 10.1111/jgs.15824
30. Apóstolo J, Cooke R, Bobrowicz-Campos E, Santana S, Marcucci M, Cano A, et al. Effectiveness of interventions to prevent pre-frailty and frailty progression in older adults: a systematic review. JBI Database System Rev Implement Rep. (2018) 16:140–232. doi: 10.11124/JBISRIR-2017-003382
31. Sternäng O, Reynolds CA, Finkel D, Ernsth-Bravell M, Pedersen NL, Dahl Aslan AK. Factors associated with grip strength decline in older adults. Age Ageing. (2015) 44:269–74. doi: 10.1093/ageing/afu170
32. Romero-Ortuno R, Kenny RA, Hartley P, Halloran AMO, Knight SP editors. Alluvial visualization and computation of probabilities of transitions in frailty index states over an 8-year period using multi-state Markov models. In: Proceedings of the 29th European Signal Processing Conference (EUSIPCO). Dublin (2021). doi: 10.23919/EUSIPCO54536.2021.9616100
33. Travers J, Romero-Ortuno R, Bailey J, Cooney M-T. Delaying and reversing frailty: a systematic review of primary care interventions. Br J Gen Pract. (2019) 69:e61–9. doi: 10.3399/bjgp18X700241
Keywords: cognition, frail older adult, mortality, physical activity, nursing home
Citation: Lim R, Kelly T-L, Andrade AQ, Kalisch Ellett LM, Bilton R, Dorj G, Pratt NL and Roughead EE (2022) Frailty trajectory over one year among residential aged care (nursing home) residents. Front. Med. 9:1010444. doi: 10.3389/fmed.2022.1010444
Received: 04 August 2022; Accepted: 20 October 2022;
Published: 03 November 2022.
Edited by:
Tzvi Dwolatzky, Technion - Israel Institute of Technology, IsraelReviewed by:
Susanna Gentili, University of Rome “Tor Vergata”, ItalyChihJung Yeh, Chung Shan Medical University, Taiwan
Copyright © 2022 Lim, Kelly, Andrade, Kalisch Ellett, Bilton, Dorj, Pratt and Roughead. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Renly Lim, cmVubHkubGltQHVuaXNhLmVkdS5hdQ==
 Renly Lim
Renly Lim Thu-Lan Kelly
Thu-Lan Kelly Nicole L. Pratt
Nicole L. Pratt