
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 15 February 2022
Sec. Obstetrics and Gynecological Surgery
Volume 8 - 2021 | https://doi.org/10.3389/fmed.2021.800180
This article is part of the Research Topic Changing Backgrounds and Groundbreaking Changes: Gynecological surgery in the third decade of the 21st century View all 11 articles
Objective: Single-port laparoscopy has become a feasible and safe approach for the management of benign adnexal masses during pregnancy. To our knowledge, there are few reports on the feasibility and safety of single-port laparoscopy for adnexal mass removal during pregnancy. Our study reports the use of single-port laparoscopy in adnexal mass removal during pregnancy in our hospital.
Methods: We included 10 cases of single-port laparoscopic surgery for adnexal mass removal during pregnancy in the West China Second University Hospital between January 2017 and March 2020. Median values were found using SPSS20. When the p-value was <0.05, the median and interquartile range were used. All patients provided informed consent.
Results: The following median values were recorded: surgical time, 112.50 min; blood loss, 25 ml; postoperative hospital stay, 3 days; postoperative pain [visual analog scale (VAS)] at 6 h, 3; and postoperative pain (VAS) at 24 h, 2. Our study reported no postoperative spontaneous abortions. There was one preterm birth.
Conclusion: Single-port laparoscopy appears to be safe for both the mother and the fetus.
Conventional laparoscopy has been widely used as a gold standard surgical method for adnexal mass removal. It is associated with shorter hospital stays, less operative pain, and fewer intraoperative complications when compared with laparotomy. Between 1:500 and 1:635, women require non-obstetric surgery during pregnancy (1). The most common gynecological non-obstetric surgery is adnexal mass removal, with an incidence rate between 0.1 and 2.4% (2). Single-port laparoscopic surgery (SPLS) has become a feasible and safe approach for the management of benign adnexal masses when compared with conventional laparoscopy (3). With the development of surgical experience in laparoscopic technology, it has been used more in pregnant patients. However, to our knowledge, there are few reports on the feasibility and safety of SPLS used in adnexal mass removal during pregnancy. Given the lack of consensus on adnexal mass treatment during pregnancy, we aimed to compile evidence regarding the safety and efficacy of SPLS as a treatment. Our study reports the use of SPLS in adnexal mass removal during pregnancy in our hospital.
We included 10 cases of SPLS for adnexal mass removal during pregnancy in the West China Second University Hospital between January 2017 and March 2020. The inclusion criteria were as follows: (1) adnexal torsion or rupture was suspected during surgery and (2) the adnexal mass was continually increasing in size during the second trimester of pregnancy and was > 6 cm in diameter.
First, we made a 2–3 cm umbilical incision longitudinally. We then inserted the single-port wound retractor into the incision and the port cap was fixed to the wound retractor. The single-port cap contained a gas inlet and four access ports (Kangji Medical). The other laparoscopic instruments were the same as those conventionally used, such as 30°, 10 mm laparoscopes that are placed into the pelvic cavity through the 10 mm port. Then, a pneumoperitoneum was established using CO2 insufflation of up to 10–15 mmHg, and the abdominal pressure was maintained at around 12 mmHg during surgery. The entire surgical procedure of ovarian cystectomy and suturing of the ovarian tissue within the abdomen was carried out through the single-port. The ovarian tissue was sutured with 2–0 absorbable suture materials, and topical hemostats, such as oxidized cellulose and bipolar hemostat forceps, were used when necessary to reduce the risk of bleeding and to shorten the surgical time if suturing was difficult. Finally, the cyst was retrieved through the umbilical incision and placed in a bag before the umbilical incision was sutured.
Larger adnexal masses were removed using the single-port assisted extracorporeal method. In the single-port assisted extracorporeal method surgical procedure, after puncture and aspiration of the content of the ovarian mass, the cyst was extracted from the abdominal cavity through an umbilical incision. Ovarian cystectomy and suturing of the ovarian tissue were then performed outside of the abdomen (Figure 1).
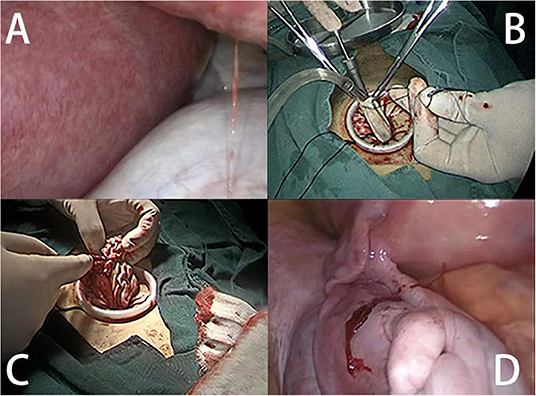
Figure 1. Extracorporeal cystectomy procedure. (A) The intraoperative view shows the enlarged uterus and left ovarian mass. (B) The puncture and aspiration of the contents of the ovarian mass. (C) Cystectomy was performed and sutured extracorporeally. (D) The ovarian tissue was returned to the abdomen.
Basic patient data was recorded. This included age, body mass index (BMI), surgical history, parity, method of conception, gestational week, maximum diameter of the ovarian mass, location of the ovarian tumors, and tumor pathology. The perioperative parameters included the diagnosis, such as the cause of the surgery, duration of the surgery, blood loss, postoperative hospital stay, axillary trocar insertion, intraoperative complications such as blood vessel injury, ileus injury, and postoperative complications such as ileus, fever, and wound infection. Postoperative pain was assessed at 6 and 24 h. All patients were contacted to determine the mode of delivery and the gestational week of delivery. Data on the duration of surgery, blood loss, postoperative hospital stay, postoperative pain [visual analog scale (VAS)] at 6 h, and postoperative pain (VAS) at 24 h were analyzed using SPSS20. When the p-value was < 0.05, the median and interquartile range were used.
A total of 10 cases of SPLS for adnexal mass removal during pregnancy were included in our study. Table 1 describes the basic characteristics of the included patients. Three of the ten procedures were performed because of torsion of the ovarian mass. The rest of the procedures were performed because of persistent enlarged ovarian masses which were >6 cm in the second trimester of pregnancy.
Table 2 presents the perioperative data of the patients. The median surgical time was 112.50 min (interquartile range, 88.75, 185). The median blood loss value was 25 ml (interquartile range, 20, 57.5). The median postoperative hospital stay was 3 days (interquartile range, 3, 4). The median postoperative pain score (VAS) at 6 h was 3 (interquartile range, 2, 3). The median postoperative pain score (VAS) at 24 h was 2 (interquartile range, 1.75, 2). The final histological pathology is included in Table 2. Mature teratomas accounted for 40% of the included cases. Hemorrhagic corpus luteal cysts were found in 30% of patients. Mucinous cystadenomas accounted for 20% of cases and only one borderline ovarian serous papillary cystadenoma occurred in the study.
Table 3 reports the obstetric outcomes of the patients. Seven patients delivered after a full-term pregnancy. One patient delivered at 34 + 4 gestational weeks, four patients delivered naturally, and six had a cesarean section delivery.
In the past, the laparoscopic approach to treat adnexal masses in the second and third trimesters of pregnancy has been discouraged. The main concerns were the risk of uterine perforation when using a Veres needle, the impact of intraabdominal pressure and CO2 on the feto-maternal circulation, longer surgical times compared to laparotomy, and potential harm from the use of monopolar current. Based on these concerns, open surgical techniques have been preferred during pregnancy. Pearl et al. (4) commissioned the guideline for laparoscopy in pregnancy which recommends that (1) End-tidal CO2 (ETCO2) be used as a surrogate marker for maternal arterial CO2 monitoring, (2) CO2 insufflation be performed to 10–15 mmHg, and (3) that the abdominal operating pressure of 12 mmHg be observed to maintain feto-maternal perfusion and optimal utero-placental blood flow. Additionally, bipolar hemostasis has been reported to be safe to use in the course of laparoscopic surgery performed during pregnancy (5). Further studies have since reported maternal and fetal safety using a laparoscopic surgical approach in pregnant patients (5, 6). Laparoscopic surgery in pregnant women has also been associated with faster recovery, shorter hospital stays, and fewer wound infections compared with laparotomy (7). Single-port laparoscopy also has the advantages of conventional laparoscopy without the risk of Veres needle injury and with less postoperative incision pain, shorter hospital stays, and ease of specimen extraction through the umbilical incision (8).
We reported 10 cases of adnexal mass removal during pregnancy using SPLS and the obstetric outcomes for each patient were optimal. We have also summarized the literature about the single port approach during pregnancy in Table 4 (8–16). To our knowledge, only seven studies have reported the use of SPLS for adnexal mass removal during pregnancy (8–14). Jiang et al. (8) reported 15 cases of cystectomy during pregnancy with no instances of missed abortion or preterm birth. Lee et al. (9) reported 14 women with intrauterine pregnancies who underwent SPLS for adnexal disease during pregnancy with good obstetric outcomes. Takeda et al. (10) reported 29 cases of adnexal mass removal during pregnancy, four of which resulted in preterm birth. Scheib et al., Kim et al., Dursun et al., and Xiao et al. (11–14) detailed two, one, nine, and six case reports, respectively, where SPLS was performed on an adnexal mass during pregnancy, and the obstetric outcomes were also good.
According to the American College of Obstetrics and Gynecology committee (17), performing non-urgent laparoscopic surgery in the second trimester is the best option for adnexal mass removal during pregnancy. In women with persistent masses in pregnancy, the reported malignancy rate is 3.6 to 6.8% and the rate of torsion of adnexal masses during pregnancy is 10% (2). Persistently growing ovarian masses >6 cm in diameter in the second trimester can be considered for removal via elective surgery in cases of emergencies and malignancies (17). Diagnostic laparoscopy in the management of adnexal masses during pregnancy is safe unless clinical severity warrants laparotomy or malignancy is strongly suspected (4). In our study, we performed three emergency surgeries and seven elective surgeries.
Chong et al. (18) reported using a single-port assisted extracorporeal approach for the removal of an ovarian cyst that measured > 8 cm in diameter on preoperative imaging. Kim et al. (12) first reported the safety of this method in adnexal mass during pregnancy. We adopted a single-port assisted extracorporeal approach for Case 9. The remaining patients underwent single-port laparoscopy. Ancillary trocar insertion was performed in two patients.
A meta-analysis reported by Liu et al. (19) showed that using laparoscopy for ovarian cyst removal is associated with better maternal and obstetric outcomes when compared with laparotomy. Three studies have reported on the safety and feasibility of single-port laparoscopy for adnexal masses when compared to conventional laparoscopy (3, 20, 21). Wang et al., Lee et al. (3, 20) compared the perioperative outcomes of single-port laparoscopy and conventional laparoscopy in adnexal mass removals and reported no difference in the median operation time, the median decreased level of hemoglobin from preoperative to postoperative day, or the median duration of postoperative hospital stay. Furthermore, Yim et al. (21) reported no difference in postoperative pain scores, operative time, perioperative complications, intraoperative blood loss, or duration of hospital stay between single-port laparoscopy and conventional laparoscopy in adnexal disease. However, only two reports have compared the use of single-port laparoscopy for ovarian mass removal during pregnancy with the use of conventional laparoscopy, but they both concluded that the techniques had comparable perioperative surgical and pregnancy outcomes (8, 10). We report a median surgical time of 112.50 min, a median blood loss of 25 ml, a median postoperative hospital stay of 3 days, a median postoperative pain (VAS) score of 3 at 6 h, and a median postoperative pain (VAS) score of 2 at 24 h. These results are similar to those detailed by Liu et al. (19) in their report on the perioperative data of laparoscopy used in adnexal masses during pregnancy. Our study reported no postoperative spontaneous abortions and one preterm birth. SPLS seems to be a safe alternative to conventional laparoscopy in treating patients with adnexal masses that require removal during pregnancy. However, there are still some shortcomings and challenges of SPLS compared to conventional laparoscopy during pregnancy. The ability to maneuver instruments in one port is limited and the enlarged uterus influences the view and operating space. As a result, the British Society for Gynecological Endoscopy (BSGE) recommends that laparoscopic surgery during pregnancy be performed by advanced laparoscopic surgeons with appropriate training and competencies (4).
There are two possible areas of future improvement for this technique. Minilaparoscopy uses 2–5 mm diameter laparoscopic instruments that can improve the cosmetic outcomes of surgery (22, 23). Minilaparoscopic single-site surgery is a new surgical procedure that combines the advantage of minilaparoscopic and single-site surgery. Casarin et al. (24) reported on this procedure to perform bilateral salpingo-oophorectomy. It is possible that this technique can be applied to the treatment of adnexal mass during pregnancy. In addition, it has been suggested that Endo Bags be used to extract suspected malignant masses to prevent spillage and the chance of spillage is rarely existed (25). In single-port laparoscopy, the cyst can be placed in a bag after cystectomy and retracted through the umbilical incision. However, if the cyst is ruptured during the cystectomy, the spillage cannot be avoided. In this case, the ovarian mass can be placed in the Endo Bag before the cystectomy is performed to reduce the spillage as suggested by Laganà et al. (26).
The limitation of our study was the small number of patients included; therefore, we did not compare our findings with those of traditional laparoscopy performed in our hospital. We intend to include more cases and conduct large randomized trials with long-term follow-up in the future. However, based on the data we included, SPLS appears to be safe for the mother and fetus.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The study was approved by the Ethics Committee of the West China Second University Hospital and informed consent was taken from all the patients. The patients/participants provided their written informed consent to participate in this study.
LH and YC were responsible for the conception of the study and manuscript drafting. AZ, QW, and LH contributed to the revision and final approval of the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank editors for providing language help.
1. Kort B. Katz VL,Watson WJ. The effect of nonobstetric operation during pregnancy. Surg Gynecol Obstet. (1993) 177:371–6.
2. Webb KE, Sakhel K, Chauhan SP, Abuhamad AZ. Adnexal mass during pregnancy: a review. Am J Perinatol. (2015) 32:1010–6. doi: 10.1055/s-0035-1549216
3. Wang SY, Yin L, Guan XM, Xiao BB, Zhang Y, Delgado A. Single port transumbilical laparoscopic surgery versus conventional laparoscopic surgery for benign adnexal masses: a retrospective study of feasibility and safety. Chin Med J. (2016) 129:1305–10. doi: 10.4103/0366-6999.182829
4. Pearl J Price R Richardson W Fanelli R Society Society of American Gastrointestinal Endoscopic Surgeons. Society of American gastrointestinal endoscopic surgeons guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy. Surg Endosc. (2011) 25:3479–92. doi: 10.1007/s00464-011-1928-2
5. Ball E, Waters N, Cooper N, Talati C, Mallick R, Rabas S, et al. Evidence-based guideline on laparoscopy in pregnancy: commissioned by the british society for gynaecological endoscopy (BSGE) endorsed by the royal college of obstetricians & gynaecologists (RCOG). Facts Views Vis Obgyn. (2019) 11:5–25.
6. Sedaghat N, Cao AM, Eslick GD, Cox MR. Laparoscopic versus open cholecystectomy in pregnancy: a systematic review and meta-analysis. Surg Endosc. (2017) 31:673–9. doi: 10.1007/s00464-016-5019-2
7. Cox TC, Huntington CR, Blair LJ, Prasad T, Lincourt AE, Augenstein VA, et al. Laparoscopic appendectomy and cholecystectomy versus open: a study in 1999 pregnant patients. Surg Endosc. (2016) 30:593–602. doi: 10.1007/s00464-015-4244-4
8. Jiang D, Yang Y, Zhang X, He F, Wu Y, Niu J, et al. Laparoendoscopic single-site compared with conventional laparoscopic surgery for gynaecological acute abdomen in pregnant women. J Int Med Res. (2021) 49:3000605211053985. doi: 10.1177/03000605211053985
9. Lee JH, Lee JR, Jee BC, Suh CS, Kim SH. Safety and feasibility of a single-port laparoscopic adnexal surgery during pregnancy. J Minim Invasive Gynecol. (2013) 20:864–70. doi: 10.1016/j.jmig.2013.06.002
10. Takeda A, Imoto S, Nakamura H. Gasless laparoendoscopic single-site surgery for management of adnexal masses during pregnancy. Eur J Obstet Gynecol Reprod Biol. (2014) 180:28–34. doi: 10.1016/j.ejogrb.2014.06.019
11. Scheib SA, Jones HH, Boruta DM, Simpson K, Bedaiwy M, Grumbine FC, et al. Laparoendoscopic single-site surgery for management of adnexal masses in pregnancy: case series. J Minim Invasive Gynecol. (2013) 20:701–7. doi: 10.1016/j.jmig.2013.02.024
12. Kim WC, Kwon YS. Laparoendoscopic single-site surgery for exteriorization and cystectomy of an ovarian tumor during pregnancy. J Minim Invasive Gynecol. (2010) 17:386–9. doi: 10.1016/j.jmig.2009.12.024
13. Dursun P, Gülümser C, Caglar M, Araz C, Zeyneloglu H, Haberal A. Laparoendoscopic single-site surgery for acute adnexal pathology during pregnancy: preliminary experience. J Matern Fetal Neonatal Med. (2013) 26:1282–6. doi: 10.3109/14767058.2013.783799
14. Xiao J, Fu K, Duan K, Wang J, Sunkara S, Guan X. Pregnancy-preserving laparoendoscopic single-site surgery for gynecologic disease: a case series. J Minim Invasive Gynecol. (2020) 27:1588–97. doi: 10.1016/j.jmig.2020.02.009
15. Koh AR, Lee JH, Choi JS, Eom JM, Hong JH. Single-port laparoscopic appendectomy during pregnancy. Surg Laparosc Endosc Percutan Tech. (2012) 22:e83–6. doi: 10.1097/SLE.0b013e31824444a9
16. Cho IS, Bae SU, Jeong WK. Single-port laparoscopic appendectomy for acute appendicitis during pregnancy. J Minim Access Surg. (2021) 17:37–42. doi: 10.4103/jmas.JMAS_193_19
17. Committee Opinion No. 696. American College of obstetricians and gynecologists. nonobstetric surgery during pregnancy. Obstet Gynecol. (2017) 129:777–8. doi: 10.1097/AOG.0000000000002014
18. Chong GO, Hong DG, Lee YS. Single-port (OctoPort) assisted extracorporeal ovarian cystectomy for the treatment of large ovarian cysts: compare to conventional laparoscopy and laparotomy. J Minim Invasive Gynecol. (2015) 22:45–9. doi: 10.1016/j.jmig.2014.06.003
19. Liu YX, Zhang Y, Huang JF, Wang L. Meta-analysis comparing the safety of laparoscopic and open surgical approaches for suspected adnexal mass during the second trimester. Int J Gynaecol Obstet. (2017) 136:272–9. doi: 10.1002/ijgo.12069
20. Lee YY, Kim TJ, Kim CJ, Park HS, Choi CH, Lee JW, et al. Single port access laparoscopic adnexal surgery versus conventional laparoscopic adnexal surgery: a comparison of peri-operative outcomes. Eur J Obstet Gynecol Reprod Biol. (2010) 151:181–4. doi: 10.1016/j.ejogrb.2010.03.010
21. Yim GW, Lee M, Nam EJ, Kim S, Kim YT, Kim SW. Is single-port access laparoscopy less painful than conventional laparoscopy for adnexal surgery? a comparison of postoperative pain and surgical outcomes. Surg Innov. (2013) 20:46–54. doi: 10.1177/1553350612439632
22. Gencdal S, Aydogmus H, Aydogmus S, Kolsuz Z, Kelekci S. Mini-Laparoscopic versus conventional laparoscopic surgery for benign adnexal masses. J Clin Med Res. (2017) 9:613–7. doi: 10.14740/jocmr3060w
23. Laganà AS, Garzon S, D'Alterio MN, Noventa M, Stabile G, Naem A, et al. Mini-laparoscopy or single-site robotic surgery in gynecology? let's think out of the box. J Invest Surg. (2020) 35:440–1. doi: 10.1080/08941939.2020.1857480
24. Casarin J, Laganà AS, Pinelli C, Cromi A, Ghezzi F. Minilaparoscopic single-site bilateral salpingo-oophorectomy: a scarless prophylactic procedure. Minim Invasive Ther Allied Technol. (2020) 16:1–6. doi: 10.1080/13645706.2020.1790391
25. Feghali EJ, Laganà AS, Daccache A, Bitar R, Garzon S, Uccella S, et al. Endobag use in laparoscopic gynecological surgeries: a systematic review. Minim Invasive Ther Allied Technol. (2021) 3:1–6. doi: 10.1080/13645706.2021.1982727
Keywords: single-port laparoscopy, adnexal mass, pregnancy, obstetric outcome, ovarian mass
Citation: Han L, Wan Q, Chen Y and Zheng A (2022) Single-Port Laparoscopic Surgery for Adnexal Mass Removal During Pregnancy: The Initial Experience of a Single Institute. Front. Med. 8:800180. doi: 10.3389/fmed.2021.800180
Received: 22 October 2021; Accepted: 27 December 2021;
Published: 15 February 2022.
Edited by:
Rafał Watrowski, University of Freiburg, GermanyReviewed by:
Polat Dursun, Consultant, Ankara, TurkeyCopyright © 2022 Han, Wan, Chen and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yali Chen, WWFsaWNoZW4xODJAMTYzLmNvbQ==; Ai Zheng, YWl6aGVuZzcxNkAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.