- 1Department of Epidemiology and Biostatistics, School of Public Health, Peking University, Beijing, China
- 2Institute for Global Health and Development, Peking University, Beijing, China
- 3Center for Health Policy Research and Evaluation, Renmin University of China, Beijing, China
Objective: To investigate 20-year trends and disparities in quality of life among older adults in China from 1998 to 2018.
Methods: Our study was based on eight representative nationwide health surveys among older adults conducted in China from 1998 to 2018. Quality of life data were obtained from 91,993 individuals aged 65 years or above. All surveys included identical indicators of self-reported quality of life, demographic factors, socioeconomic status, lifestyle habits, and health status. The trends in the standardized prevalence of poor quality of life from 1998 to 2018 were examined by locally weighted scatterplot smoothing regression (LOWESS) analysis. We assessed the prevalence of poor quality of life and its related factors by logistic regression models after adjusting for potential confounders.
Results: The prevalence of poor quality of life was 38.2% (95% CI: 37.9–38.5%). The trends of poor quality of life showed an inverted “U” shape, that the prevalence increased from 27.8% in 1998 to 43.6% in 2008, and then decreased from 39.2% in 2011 to 32.1% in 2018. Disparities in the prevalence of poor quality of life were exacerbating among participants with low or moderate household income per capita and participants with high household income per capita from 1998 to 2018. After controlling potential confounders, living in rural areas, aged below 80 years, unmarried, living alone, low household income, current smoker, poor dietary diversity, never participating in organized social activities, with chronic diseases, functional disability, poor self-reported health, and unhealthy psychological status were risk factors related with poor quality of life in the multivariate model (all p < 0.05).
Conclusion: During the past two decades, poor quality of life in Chinese older adults showed an inverted “U” trend from 1998 to 2018 that the prevalence of poor quality of life peaked in 2008 and declined since China's deepening health system reform in 2009. However, disparities in the poor quality of life were exacerbating among participants with different socioeconomic statuses. Strengthening the health system is of great importance in improving the quality of life. More efforts are needed to reduce the disparities in the quality of life among the population at the different socioeconomic levels.
Introduction
Ensuring healthy lives and promoting well-being for all at all ages by 2030 is a global sustainable development goal (SDG) set by the United Nations. Monitoring the health status of populations is crucial for recognizing unmet population health needs, planning intervention programs, and assessing the effectiveness of health policies and strategies (1). Among all the indicators on health, quality of life is considered as a multi-dimensional and comprehensive indicator that better reflect well-being, which is affected by physical, psychological, and social factors (2, 3). Numerous studies had explored age, residence, income level, lifestyle factors, chronic disease, and social health status as factors associated with quality of life (2, 4–8).
Some studies assessed the time trends of poor quality of life (1, 6, 9, 10). However, the results were controversial because of different populations, assessment tools, locations, and periods. Audureau et al. (1) reported evidence of worsening trends and increasing demographic, socioeconomic, and regional disparities in quality of life by comparing two French population-based cross-sectional surveys in 1995 and 2003. Atlantis et al. (6) investigated the 10-year trends in quality of life among 9,059 people aged ≥15 years who participated in representative surveys of the South Australian population in 1998, 2004, and 2008. They found that scores on the physical component of SF-36 were stable and scores on the mental component were significantly decreased from 1998 to 2008 (6). Rehkopf et al. (10) found that general health improved in people aged 65 years and older in the United States from 2003 to 2017 with the percentage of poor health decreasing from 23% in 2003 to 19% in 2017.
Literature had reported the potential factors associated with poor quality of life in the general population or patients in China (3, 8, 11, 12). Zhang et al. (12) found that the prevalence and decline in quality of life of multimorbid older-aged people were severe in Shandong province, China. Aging is one of the global challenges leading high economic burden on health and social care (13). China has the largest number of older adults in the world, imposing a heavy burden on the healthcare systems. There are more than 260 million older adults in China and the proportion of people aged 60 and older continues to increase in the past decade, according to the 17 National Census in 2020. China has deepened health system reform since 2009, to reach the goal of achieving universal health coverage by 2020. Understanding the trends and disparities in quality of life among older adults in China is helpful for recognizing the achievements and gaps of health services and needs, and better making tailored interventions, strategies, and policies. However, studies examining the long-term trends of quality of life were limited in China (14). To the best of our knowledge, this is the first study that focuses on 20-year trends and disparities in quality of life among older adults in China that reflect the effect of China's deepening health system reform in 2009, which is different from previous studies made with the Chinese Longitudinal Healthy Longevity Survey (CLHLS). The study is unique due to the potential multiculturalism of the findings and its large sample size.
In the present study, we aimed to investigate the trends and disparities in quality of life among older adults aged 65 years and older in China from 1998 to 2018, using the national cross-sectional data from eight representative health surveys among older adults conducted in China in 1998, 2000, 2002, 2005, 2008, 2011, 2014, and 2018.
Methods
Study Population and Data Source
This is a national observational study using data from the CLHLS. The CLHLS aimed at investigating the determinants of healthy longevity among the older Chinese population and covered 22 of 31 provinces in China (15, 16). The survey was conducted randomly in about half of the cities/counties in 22 out of 31 provinces in China, covering about 85% of the national population. It began in 1998 and continued in 2000, 2002, 2005, 2008, 2011, 2014, and 2018, with about a 90% response rate for each wave (17). Nearly one-third of participants from each wave were from the previous wave, and the rest were new recruits because of the mixed longitudinal design of CLHLS. To reduce the selection bias in different waves and ensure the consistency of the study population, new recruits were selected based on the similarities in gender, age, and general characteristics with those who were lost during the follow-up. More details of the CLHLS study design can be found elsewhere (15–17).
There was a total of 1,02,864 participants in these nine waves (9,093 in 1998, 11,199 in 2000, 16,064 in 2002, 15,638 in 2005, 16,954 in 2008, 10,850 in 2011, 7,192 in 2014, and 15,874 in 2018). Among them, we excluded 10,149 participants who had missing data on quality of life and 722 participants aged below 65 years, yielding 91,993 participants (89.4%) in the final study (Figure 1).
Quality of Life
All information was obtained in the homes of participants through face-to-face questionnaire interviews and physical health examinations by trained investigators. Quality of life was assessed by asking one question as “How do you rate your quality of life at present? (Very good, good, so so, bad, very bad)”. We combined the answer “so so,” “bad,” and “very bad” as self-reported poor quality of life.
Explanatory Variables
Following previous studies (17–20), we included explanatory variable groups derived from the CLHLS in this study, such as wave indicators (investigation years), demographic factors, socioeconomic status, lifestyle habits, and health conditions variables. Demographic factors included region (urban or rural), gender (male or female), age group (65–79 years or ≥80 years), marital status (unmarried, married, or divorced or widowed), and living patterns (living with family members, living in an institution, or living alone). Socioeconomic status included years of schooling (0 years or ≥1 years), household income per capita (low, moderate, or high), and frequently going to bed hungry in childhood (yes or no). To make the household income of different years comparable, we divided the household income of each wave into three groups by tertiles according to the level of each survey year. Lifestyle habits included smoking status (never, previous, or current), alcohol intaking status (never, previous, or current), regular exercise (never, previous, or current), dietary diversity (poor, moderate, or good), participating in organized social activities (almost every day, sometimes, or never). Dietary diversity was evaluated as poor (0–3), moderate (4–6), or good (7–9) by the calculated dietary diversity score (0–9) reflecting the consumption numbers of nine types of food groups (meat, vegetables, fish, eggs, fruits, legumes, milk, tea, and nuts) (21). Health status included body mass index (BMI) (underweight, normal weight, overweight, or obesity), numbers of chronic diseases (0, 1, or ≥2), functional disability (no or yes), cognitive impairment (no or yes), self-reported health (good, general, or poor), psychological status (healthy or unhealthy). BMI was categorized as underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥30 kg/m2), according to the WHO. Functional disability was defined as the self-reported difficulty with any of the following activities of daily living (ADL) items, such as dressing, eating, bathing, continence, toileting and cleaning, or indoor movement (22). The cognitive function of participants was measured using the Chinese version of the Mini-Mental State Examination (CMMSE) in all waves of the CLHLS (18). The CMMSE consists of 24 items within six dimensions (orientation, registration, naming, attention and calculation, recall, and language). The total score of the CMMSE ranges from 0 to 30 points. Participants with CMMSE scores below 18 points were defined as cognitive impairment as previously validated (18, 23).
Statistical Analyses
Baseline characteristics of the study population were described as percentages for categorical variables (such as region) and median [interquartile range (IQR)] for continuous variables (such as age). The prevalence of poor quality of life with its 95% CI was calculated by sampling weights based on the sampling design. Pearson's χ2 test was used to compare the prevalence of poor quality of life in groups with different characteristics. The trends in the prevalence of poor quality of life from 1998 to 2018 were analyzed by the locally weighted scatterplot smoothing regression (LOWESS) analysis and estimated averaged percentage change (EAPC) were estimated (24, 25). We used univariate and multivariate logistic regression models to analyze risk factors related to poor quality of life. Crude odds ratio (COR) and adjusted odds ratio (AOR) with its 95% CI was calculated. To examine the robustness of the estimation, we did sensitivity analysis replacing categorical variables with continuous variables, such as age, education level, household income, BMI I, CMMSE scores, and ADL scores. All the analyses were performed with SPSS 26.0 and Stata 17.0. A p < 0.05 means significant.
Results
Characteristics of the Participants
Of the 91,993 participants included in the study, 73.0% were older than 80 years of age, 52.1% lived in a rural region, 55.8% were women, 81.5% lived with family members, 58.7% never went to school, and 49.2% frequently went to bed hungry in childhood. The age of participants included in the study ranged from 65 to 105 years old, with a median age of 74 years (IQR 69–81). The proportion of current smokers, current drinkers, regular exercise, diverse dietary, and regular organized social activities were 18.0, 20.6, 32.0, 30.4, and 14.8%, respectively. About 30.3% of the participants were underweight, 24.3% had a functional disability, 20.2% had cognitive impairment, 50.5% had self-reported poor or general health, and 42.7% reported unhealthy psychological status (Table 1).
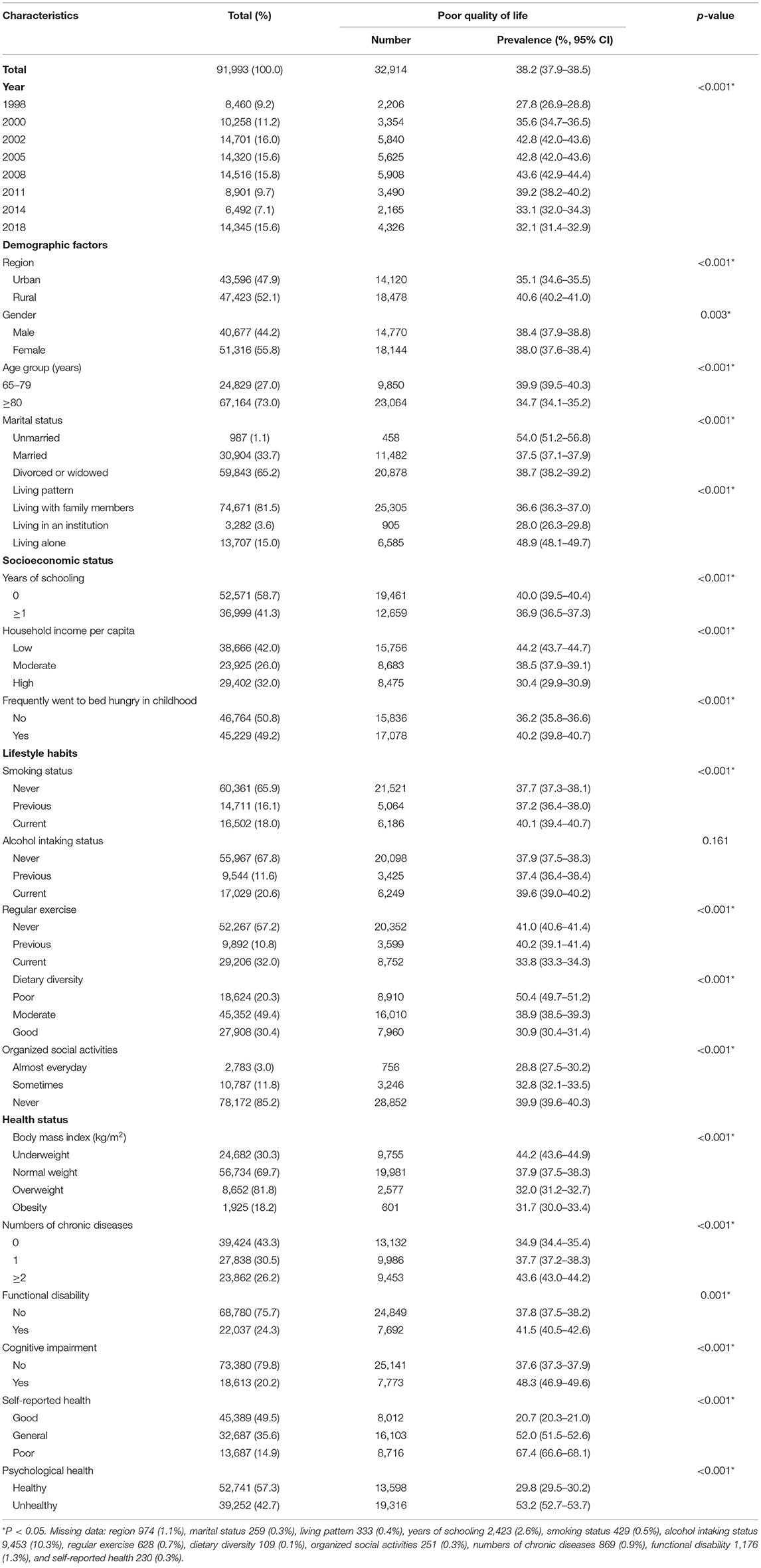
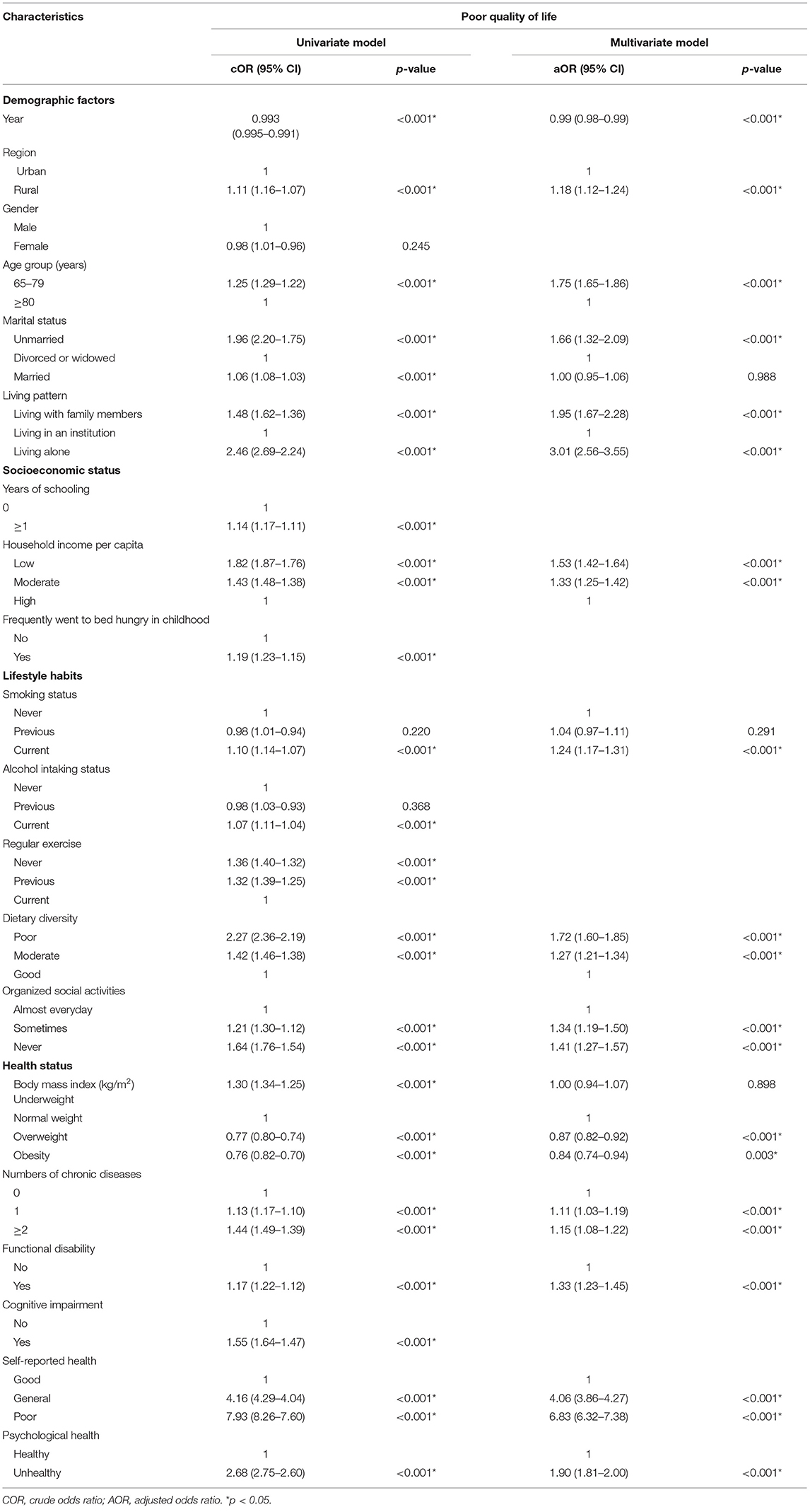
Table 1. Prevalence of poor quality of life by the survey year, demographic factors, socioeconomic status, lifestyle habits, and health status (N = 91,993).
Trends and Disparities in the Prevalence of Poor Quality of Life From 1998 to 2018
The prevalence of poor quality of life was 38.2% (95% CI: 37.9–38.5%, Table 1). The trends of poor quality of life showed an inverted “U” shape (Figure 2), that the prevalence increased from 27.8% in 1998 to 43.6% in 2008 (EAPC 5.5%, 95% CI: 5.0–6.0%), and then decreased from 39.2% in 2011 to 32.1% in 2018 (EAPC −4.0%, 95% CI: −3.3 to −4.8%).
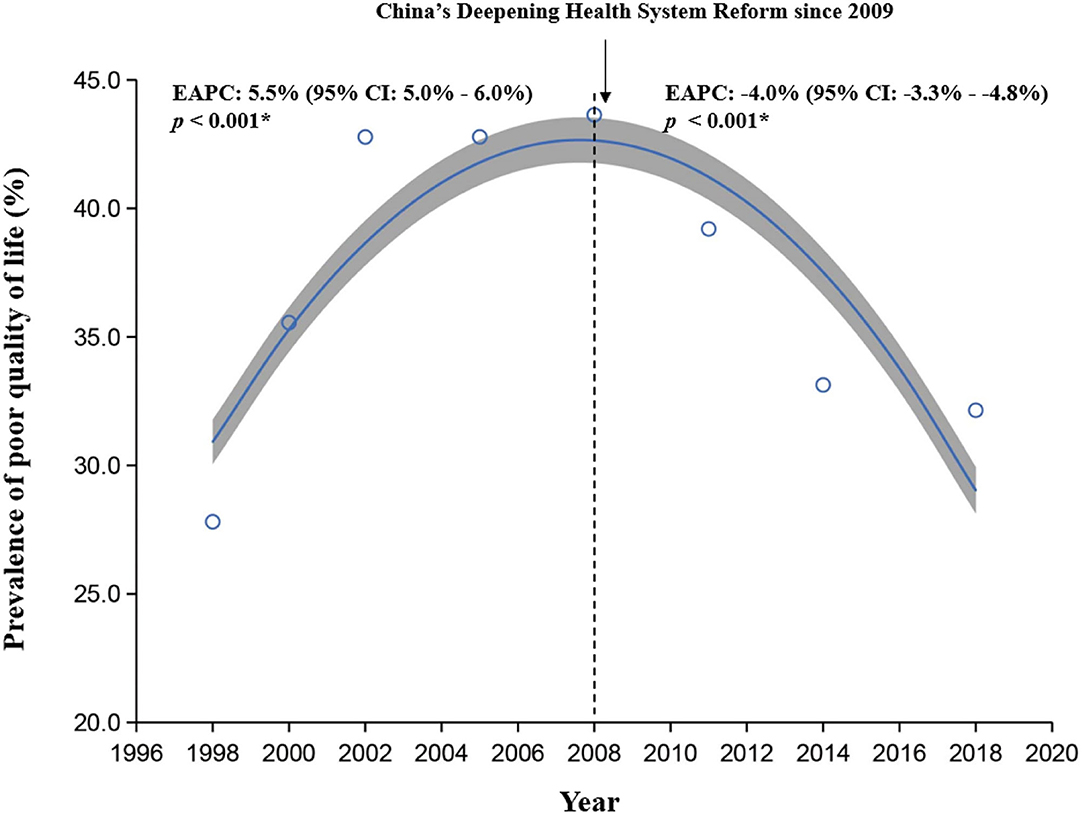
Figure 2. The trends in the prevalence of poor quality of life from 1998 to 2018 by locally weighted scatterplot smoothing regression analysis. EAPC, estimated averaged percentage change.
Similar trends of poor quality of life were observed in rural and urban areas, different age groups, and socioeconomic statuses. However, disparities in the prevalence of poor quality of life were exacerbating among participants with low or moderate household income per capita and participants with high household income per capita from 1998 to 2018 (Figure 3).
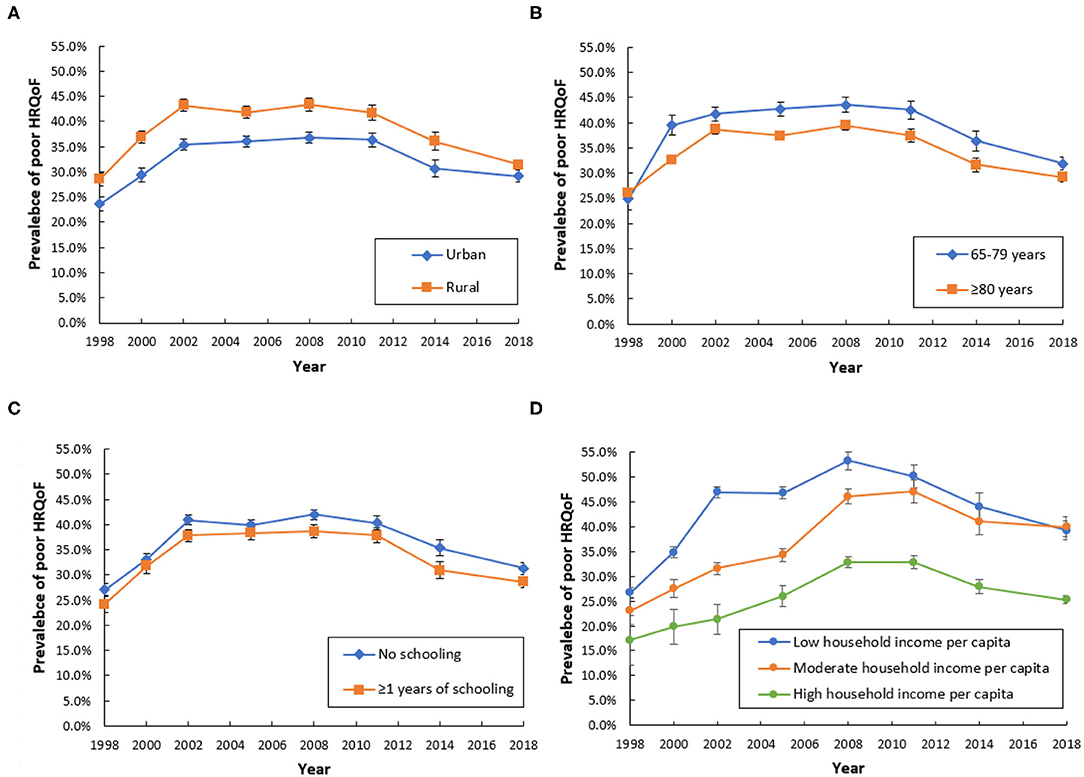
Figure 3. Trends of poor quality of life from 1998 to 2018 by region (A), age (B), education (C), and household income per capita (D).
In the univariate models, participants living in rural areas, male, with young age, unmarried, living alone, no schooling, low household income, frequently went to bed hungry in childhood, current smoker, current alcohol intaking, no regular exercise, poor dietary diversity, never participating in organized social activities, underweight, with chronic diseases, functional disability, cognitive impairment, poor self-reported health, and unhealthy psychological status were more likely to have a poor quality of life (all p < 0.05, (Tables 1, 2).
Factors Related to Poor Quality of Life in the Multivariate Model
After controlling potential confounders, living in rural areas (AOR 1.18, 95% CI: 1.12–1.24), aged below 80 years (AOR 1.75, 95% CI: 1.65–1.86), unmarried (AOR 1.66, 95% CI: 1.32–2.09), living alone (AOR 3.01, 95% CI: 2.56–3.55), low household income (AOR 1.53, 95% CI: 1.42–1.64), current smoker (AOR 1.24, 95% CI: 1.17–1.31), poor dietary diversity (AOR 1.72, 95% CI: 1.60–1.85), never participated in organized social activities (AOR 1.41, 95% CI: 1.27–1.57), with chronic diseases (AOR 1.15, 95% CI: 1.08–1.22), functional disability (AOR 1.33, 95% CI: 1.23–1.45), poor self-reported health (AOR 6.83, 95% CI: 6.32–7.38), and unhealthy psychological status (AOR 1.90, 95% CI: 1.81–2.00) were risk factors related with the poor quality of life in the multivariate model (all p < 0.05, Table 2). In the sensitivity analysis, the results were stable.
Discussion
To our knowledge, this was the first study that assessed the 20-year trends and disparities in quality of life among older adults in China from 1998 to 2018. In the present study, we found that overall, more than one-third of the older adults (38.2%) perceived poor quality of life in the past two decades, and the time trends of poor quality of life showed an inverted “U” shape, with an increasing trend during 1998–2008 and a decreasing trend during 2009–2018. China started the first round of health system reform in 1996, but the effectiveness of the reform was questioned after several years of implementation for complaints from the public about access to and affordability of healthcare increased (26). According to the national health services survey in 2008, a large proportion of the population in China could not afford the needed healthcare (26, 27). As the outbreak of severe acute respiratory syndrome (SARS) in 2003 in China highlighted the importance of health for human development, the Chinese government began to recognize the contribution of the health system to entire social and economic development and started to plan another round of health system reform in 2007 (26). The failure of the first round of health system reform might be one possible explanation for the increasing trends of poor quality of life.
The decreasing trend of quality of life after 2008 might be related to the achievement of China's deepening health system reform on healthcare since 2009 (26). After 2008, the Central Committee of the Communist Party of China and the State Council issued the Opinions on Deepening Health System Reform in 2009, with the aim of establishing an equitable and effective health system for all people (universal health coverage) by 2020, by strengthening the provision of essential medicines, healthcare delivery, and health security (26, 28). Since 2009, China's deepening health system reform on healthcare was conducted. Yao et al. compared the 2008 and 2013 national health services surveys in China and reported decreased problems in the quality of life (14). Our findings were consistent with the results in the general population.
It is well-known that subjective quality of life is a construct determined by multiple factors (29). Sociodemographic, physical, and psychological factors could influence the subjective quality of life (7). In the multivariate model, we found that aged below 80 years, living in rural areas, unmarried, living alone, low household income, current smoker, poor dietary diversity, never participated in organized social activities, with chronic diseases, functional disability, poor self-reported health, unhealthy psychological status were risk factors related with the poor quality of life, after controlling potential confounders. The findings were consistent with previous studies (2, 4, 5, 7). It is well-reported that cognition and behavior change significantly, along with the associated brain function and organization as humans age (30). Age-dependent physical and psychological dependence might be related to the poor quality of life (31). Living alone, smoking habits, poor dietary diversity, and social isolation were all modifiable risk factors, which could be intervened.
We found that the quality of life in participants with low socioeconomic status was much worse than participants with high socioeconomic status, which was consistent with previous studies (7, 32). Previous studies had reported that differences in socioeconomic status were a significant factor in explaining the different health statuses among the Chinese older people (32–34). The relationship between socioeconomic status and quality of life might be explained by the difference in living standards and the access to healthcare services (12). Gross domestic product (GDP) per capita has increased more than 10 times in China in the past 20 years, from $ 828.58 in 1998 to $ 9,976.68 in 2018. However, we found that disparities in the prevalence of poor quality of life were exacerbating among participants with different socioeconomic statuses, despite the rapid development of China's socioeconomic level in the past two decades. The underlying reason behind this phenomenon is worthy of further research in the future.
As for practical recommendations, our findings highlighted the importance of strengthening the health system on improving the multidimensional quality of life among older adults. More operationalized policies are needed to improve the current situation of health inequities among the different socioeconomic statuses in China and to address the health equity problem in a more systematic way. Currently, insufficient integration of medical treatment and public health hampered the equity of health, equity of health service utilization, and equity of accessibility of older adults in China. Chinese health departments should take advantage of China's development paradigm shift in recent years from efficiency-orientation to sustainability and equality-orientation in the construction of Healthy China 2030. Quality of life should also be added as one of the main health indicators in monitoring the progress in the Healthy China 2030 plan.
There were several limitations in this study. First, the measurement of quality of life was not based on complex tools, such as SF-36, because of the original study design on the questionnaire in the CLHLS. Second, recall bias could not be avoided when we did the survey among older adults, compared with youngsters. Third, some confounding factors (e.g., major life stress events) may affect the quality of life. However, the CLHLS did not collect the information on these potential confounders. Thus, we could not include these factors in the multivariable models. Finally, the results of this study only represent the quality of life of the elderly population in mainland China. In the future, it is necessary to carry out longitudinal tracking of quality of life around the world and carry out multi-country comparative studies.
In conclusion, the prevalence of poor quality of life in Chinese older adults showed an inverted “U” trend from 1998 to 2018 during the past two decades. It peaked in 2008 and declined since China's deepening health system reform in 2009. However, disparities in the poor quality of life were exacerbating among participants with different socioeconomic statuses. Quality of life was affected by physical—psychological—social multidimensional factors. Strengthening the health system is of great importance in improving the quality of life. More efforts are needed to promote quality of life among Chinese older adults, especially for reducing the disparities in quality of life among population different socioeconomic levels.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethical Review Committee of Peking University (IRB00001052-13074). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JL contributed to the conceptualization, formal analysis, writing the original draft, writing review and editing, and funding acquisition. JW contributed to the writing review and editing. All the authors have made substantial contributions to the conception, design of the study, or the acquisition, analysis, or interpretation of data for the study. They have participated in drafting the manuscript and approval of the version to be published.
Funding
This study was supported by the National Natural Science Outstanding Youth Foundation of China (Grant Numbers: 72122001) and the National Natural Science Foundation of China (Grant Numbers: 72042002 and 72061160491). The funding body had no role in the design or conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the members of the CLHLS study group for data collection and all the participants.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.796208/full#supplementary-material
References
1. Audureau E, Rican S, Coste J. Worsening trends and increasing disparities in health-related quality of life: evidence from two French population-based cross-sectional surveys, 1995–2003. Quality of life Research. (2013) 22:13–26. doi: 10.1007/s11136-012-0117-7
2. Taype-Rondan A, Abbs ES, Lazo-Porras M, Checkley W, Gilman RH, Smeeth L, et al. Association between chronic conditions and health-related quality of life: differences by level of urbanization in Peru. Quality of life Research. (2017) 26:3439–47. doi: 10.1007/s11136-017-1649-7
3. Zheng S, He A, Yu Y, Jiang L, Liang J, Wang P. Research trends and hotspots of health-related quality of life: a bibliometric analysis from 2000 to 2019. Health Qual Life Outcomes. (2021) 19:130. doi: 10.1186/s12955-021-01767-z
4. Lu J, Yu Z, Zhang X, Wu M, Lin S, Zhu Y, et al. Association between social health status and health-related quality of life among community-dwelling elderly in Zhejiang. Health Qual Life Outcomes. (2020) 18:110. doi: 10.1186/s12955-020-01358-4
5. Brown DR, Carroll DD, Workman LM, Carlson SA, Brown DW. Physical activity and health-related quality of life: US adults with and without limitations. Quality of life Research. (2014) 23:2673–80. doi: 10.1007/s11136-014-0739-z
6. Atlantis E, Goldney RD, Eckert KA, Taylor AW. Trends in health-related quality of life and health service use associated with body mass index and comorbid major depression in South Australia, 1998-2008. Qual Life Res. (2012) 21:1695–704. doi: 10.1007/s11136-011-0101-7
7. Kim J, Park E. Impact of socioeconomic status and subjective social class on overall and health-related quality of life. BMC Public Health. (2015) 15:783. doi: 10.1186/s12889-015-2014-9
8. Li S, Cui G, Yin Y, Wang S, Liu X, Chen L. Health-promoting behaviors mediate the relationship between eHealth literacy and health-related quality of life among Chinese older adults: a cross-sectional study. Qual Life Res. (2021) 30:2235–43. doi: 10.1007/s11136-021-02797-2
9. Bretschneider J, Janitza S, Jacobi F, Thom J, Hapke U, Kurth T, et al. Time trends in depression prevalence and health-related correlates: results from population-based surveys in Germany 1997–1999 vs. 2009–2012. BMC Psychiatry. (2018) 18:394. doi: 10.1186/s12888-018-1973-7
10. Rehkopf DH, Furstenberg FF, Rowe JW. Trends in mental and physical health-related quality of life in low-income older persons in the United States, 2003 to 2017. JAMA Network Open. (2019) 2:e1917868. doi: 10.1001/jamanetworkopen.2019.17868
11. Garrison LP, Schepman P, Bushmakin AG, Robinson RL, Tive L, Hall J, et al. Concern about addiction is associated with lower quality of life in patients with osteoarthritis: an exploratory, real-world data analysis. Qual Life Res. (2021). doi: 10.1007/s11136-021-02907-0. [Epub ahead of print].
12. Zhao Q, Wang J, Nicholas S, Maitland E, Sun J, Jiao C, et al. Health-related quality of life and health service use among multimorbid middle-aged and older-aged adults in china: a cross-sectional study in Shandong province. Int J Environ Res Public Health. (2020) 17:9261. doi: 10.3390/ijerph17249261
13. Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the global burden of disease study 2017. Lancet Public Health. (2019) 4:e159–67. doi: 10.1016/S2468-2667(19)30019-2
14. Yao Q, Liu C, Zhang Y, Xu L. Changes in health-related quality of life of Chinese populations measured by the EQ-5D-3 L: a comparison of the 2008 and 2013 National Health Services Surveys. Health Qual Life Outcomes. (2019) 17:43. doi: 10.1186/s12955-019-1109-x
15. Zeng Y. Introduction to the Chinese Longitudinal Healthy Longevity Survey (CLHLS). Dordrecht, Netherlands: Springer (2008).
16. John SJ, Anna Z, Chen B, Chih-Da W, Lijing Y, Shenglan T, et al. Residential greenness and mortality in oldest-old women and men in China: a longitudinal cohort study. Lancet Planet Health. (2019) 3:e17–e25. doi: 10.1016/S2542-5196(18)30264-X
17. Gao M, Kuang W, Qiu P, Wang H, Lv X, Yang M. The time trends of cognitive impairment incidence among older Chinese people in the community: based on the CLHLS cohorts from 1998 to 2014. Age Ageing. (2017) 46:787–93. doi: 10.1093/ageing/afx038
18. Du M, Tao L, Zhu L, Liu J. Association between biomass fuel use and the risk of cognitive impairment among older populations in China: a population-based cohort study. Environ Health. (2021) 20:21. doi: 10.1186/s12940-021-00706-1
19. Du M, Tao L, Liu M, Liu J. Tourism experiences and the lower risk of mortality in the Chinese elderly: a national cohort study. BMC Public Health. (2021) 21:996. doi: 10.1186/s12889-021-11099-8
20. Du M, Liu M, Liu J. The association between sleep duration and the risk of mortality in the Chinese older adults: a national cohort study. J Clin Sleep Med. (2021) 17:1821–9. doi: 10.5664/jcsm.9278
21. Tao L, Xie Z, Tao H. Dietary diversity and all-cause mortality among Chinese adults aged 65 or older: a community-based cohort study. Asia Pac J Clin Nutr. (2020) 29:152–60. doi: 10.6133/apjcn.202003_29(1).0020
22. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. (1963) 185:914–19. doi: 10.1001/jama.1963.03060120024016
23. Zhang Z, Zahner G, Román G, Liu X, Wu C, Hong Z, et al. Socio-demographic variation of dementia subtypes in china: methodology and results of a prevalence study in Beijing, Chengdu, Shanghai, and Xian. Neuroepidemiology. (2006) 27:177–87. doi: 10.1159/000096131
24. Tao L, Wang R, Han N, Liu J, Yuan C, Deng L, et al. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: a multi-center cross-sectional study based on Health Belief Model. Hum Vaccin Immunother. (2021) 17:2378–88. doi: 10.1080/21645515.2021.1892432
25. Liu Q, Jing W, Kang L, Liu J, Liu M. Trends of the global, regional and national incidence of malaria in 204 countries from 1990 to 2019 and implications for malaria prevention. J Travel Med. (2021) 28:taab046. doi: 10.1093/jtm/taab046
26. Meng Q, Mills A, Wang L, Han Q. What can we learn from China's health system reform? BMJ. (2019) 365:l2349. doi: 10.1136/bmj.l2349
27. Center for Health Statistics and Information National Health and Family Planning Commission. An analysis report of national health services survey 2008. Beijing: Peking Union Medical College Press (2009).
28. Central Central Committee of the Communist Party of China State, Council (2009). Opinions on deepening health system reform. Zhongfa 2009 No. 6. Available online at: http://www.china.org.cn/government/scio-pressconferences/2009-04/09/content_17575378.htm.
29. Taylor JE, Poston WS, Haddock CK, Blackburn GL, Heber D, Heymsfield SB, et al. Psychometric characteristics of the general well-being schedule (GWB) with African-American women. Qual Life Res Int J Qual Life Asp Treat Care Rehab. (2003) 12:31–9. doi: 10.1023/A:1022052804109
30. Schlesinger KJ, Turner BO, Lopez BA, Miller MB, Carlson JM. Age-dependent changes in task-based modular organization of the human brain. Neuroimage. (2017) 146:741–62 doi: 10.1016/j.neuroimage.2016.09.001
31. Mohammadian J, Miladi-Gorji H. Age- and sex-related changes in the severity of physical and psychological dependence in morphine-dependent rats. Pharmacol Biochem Behav. (2019) 187:172793. doi: 10.1016/j.pbb.2019.172793
32. Wang HCK, Chen K, Zhou B, Wang JF. Study on social determinants and health-related quality of life among the 'empty nest' (lonely) elderly Chinese people. Zhonghua Liu Xing Bing Xue Za Zhi. (2010) 31:400–4. doi: 10.3760/cma.j.issn.0254-6450.2010.04.009
33. Ying M, Wang S, Bai C, Li Y. Rural-urban differences in health outcomes, healthcare use, and expenditures among older adults under universal health insurance in China. PLoS ONE. (2020) 15:e240194. doi: 10.1371/journal.pone.0240194
Keywords: quality of life, prevalence, observational study, older adults, China
Citation: Liu J and Wang J (2022) Trends and Disparities in Quality of Life Among Older Adults From 1998 to 2018 in China: A National Observational Study. Front. Med. 8:796208. doi: 10.3389/fmed.2021.796208
Received: 16 October 2021; Accepted: 28 December 2021;
Published: 28 January 2022.
Edited by:
Redhwan Ahmed Al-Naggar, National University of Malaysia, MalaysiaReviewed by:
Liyuan Tao, Peking University Third Hospital, ChinaInbar Levkovich, Oranim Academic College, Israel
Copyright © 2022 Liu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jue Liu, anVlbGl1JiN4MDAwNDA7YmptdS5lZHUuY24=; Jun Wang, Y2ZkcmtpbmcmI3gwMDA0MDsxMjYuY29t
 Jue Liu
Jue Liu Jun Wang3*
Jun Wang3*