- Affiliated Wuhan Mental Health Center, Tongji Medical College of Huazhong University of Science and Technology, Wuhan, China
Background: The ongoing COVID-19 pandemic has disproportionately affected the sleep health of older adults, but the limited number of studies on insomnia symptoms of older Chinese adults differed in terms of screener of insomnia, sample size, and prevalence, making mental health planning for this population difficult. This meta-analysis estimated the prevalence of insomnia symptoms in older Chinese adults during the COVID-19 pandemic.
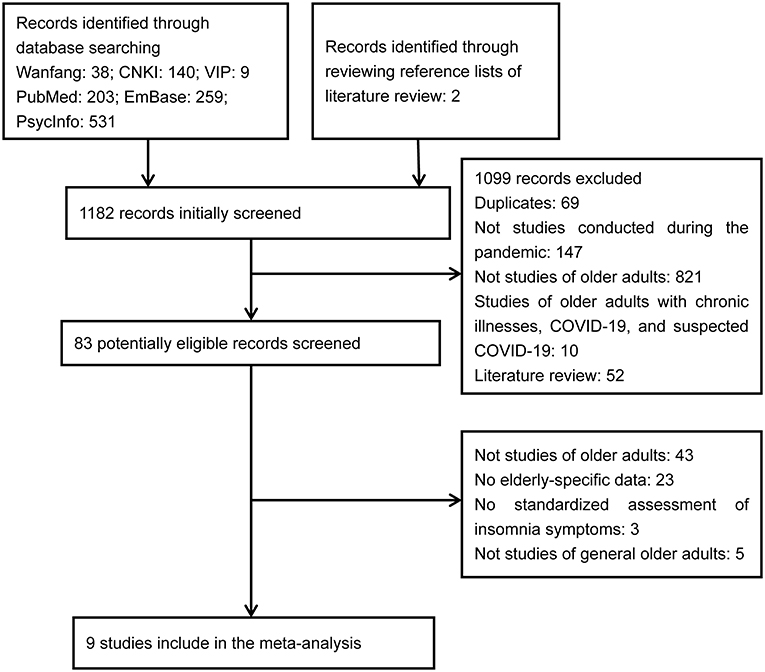
Methods: Both Chinese (CNKI, Wanfang, VIP) and English (PubMed, EmBase, PsycInfo) databases were systematically searched to identify cross-sectional studies containing data on the prevalence of insomnia symptoms in older Chinese adults during the pandemic. Risk of bias (RoB) of included studies was assessed with the Joanna Briggs Institute Critical Appraisal Checklist for Studies Reporting Prevalence Data.
Results: Nine studies with a total of 27,207 older Chinese adults were included. RoB scores of these studies ranged between zero and six. The pooled prevalence rates of insomnia symptoms and moderate and severe insomnia symptoms were 24.6% [95% confidence interval (CI): 19.5–30.5%] and 11.1% (95% CI: 7.2–16.9%), respectively. In subgroup analysis, significantly higher prevalence rates were observed in studies defining insomnia symptoms as “Insomnia Severity Index (ISI) ≥ 8” than in those defining them as “ISI ≥ 15” (32.6 vs. 15.6%, P < 0.001) and in older adults living in the COVID-19 epicenter than in those living in other places (35.2 vs. 23.3%, P = 0.006).
Conclusion: Nearly one out of every four older Chinese adults suffered from insomnia symptoms during the pandemic. Mental health services for this population during the pandemic should include supportive activities aimed at improving mental well-being, periodic assessment of insomnia symptoms, and psychiatric assessment and treatment when necessary.
Introduction
Sleep disturbances and insomnia are common among older adults. In China, 35.9% of the adults aged 60+ years suffer from sleep disturbances and 24.4–26.8% report insomnia symptoms in the most recent month, as defined by a cut-off score on the Pittsburgh Sleep Quality Index (PSQI) (1–3). Factors associated with late-life insomnia symptoms included no spouses, mental health problems, major medical conditions, negative life events, and acute or recurring psychosocial stressors (2–5).
The ongoing COVID-19 pandemic is a significant source of stress in people's lives and has profound negative effects on the mental health of people of all ages (6). Because the majority of COVID-19-related hospitalizations and deaths occur in persons aged 65+ years, older adults have been disproportionately affected by the pandemic (7). The current public health guidelines recommend older adults to keep social distancing with others and stay indoors as much as possible, which in turn result in elevated levels of loneliness and social isolation in older adults (8, 9). Importantly, in the context of the pandemic, older adults are confronted with disruptions to the daily routines due to lockdown, difficulties in timely accessing to needed healthcare services due to the overwhelmed hospitals, financial loss due to economic recession, separation from family members due to mass quarantine, and difficulties in using digital technologies due to lack of internet access and no smartphones (10–12); these associated stressors may further exacerbate the mental health of older adults.
Mental health problems, including insomnia, are a common stress reaction following exposure to a traumatic event such as the COVID-19 pandemic. Nevertheless, compared to the numerous studies on mental health and sleep problems in general adults during the pandemic (13–15), relatively fewer have investigated sleep problems in the elderly population.
China has the world's largest population of older adults and Chinese adults aged 65+ years will rise to 366 million in 2050, accounting for 26.1% of the total population (16). Since the reform and open door policy in 1978, substantial socioeconomic–cultural changes have challenged the mental health of older adults in China. For example, the massive rural-to-urban migration of young labors has resulted in millions of left-behind older adults, the one-child policy and the erosion of the traditional family structure have resulted in millions of empty-nest elders, and the diminishing traditional value of filial piety has reduced adult children's willingness to care for older adults (17, 18). Therefore, the ongoing pandemic coupled with the rapid aging may have a much more devastating toll on the mental and sleep health of older Chinese adults.
In China, a few population-based studies have examined the prevalence of insomnia symptoms in older adults amid the pandemic, but these studies varied in terms of screener of insomnia [i.e., PSQI vs. Insomnia Severity Index (ISI)], sample size (i.e., from 35 to 13,964), and prevalence (i.e., from 13.1 to 42.9%) (19–23). Importantly, nearly all available data on older adults are derived from whole population-based studies, where elderly-specific prevalence data are not easily accessed (i.e., only shown in the main text). To facilitate the development of mental health policy aimed at preventing or reducing insomnia in older Chinese adults during the pandemic, it is necessary to systematically review available studies and estimate the prevalence of insomnia symptoms.
Materials and Methods
This systematic review and meta-analysis was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline (Supplementary Table 1). Two authors (QQ Zhang and L Li) independently searched literature, extracted data, and performed risk of bias (RoB) assessment. Any disagreements were resolved by a discussion with the correspondence author (BL Zhong). In this study, after cross-checking, no discrepancies were found in the results of literature search, study selection, and data extraction. However, the two authors had different RoB scores on two included studies. After discussion with the correspondence author, consensus was achieved across the three authors.
Literature Search
Potential studies published between January 1, 2020 and September 17, 2021 were searched in both Chinese and English databases: Chinese National Knowledge Infrastructure (CNKI), Wanfang data, VIP Information, PubMed, EmBase, and PsycInfo. The search terms were as follows: (sleep disturbance OR sleep quality OR insomnia OR sleep problem OR sleep disorder OR sleep symptom) AND (epidemiology OR cross-sectional study OR prevalence OR rate) AND (coronavirus disease 2019 OR 2019-n-CoV OR severe acute respiratory syndrome coronavirus 2 OR COVID-19 OR COVID) AND (China OR Chinese). To avoid missing studies that focused on the general population but simultaneously presented elderly-specific data in their main texts, we had no restrictions on participants in the search strategy. Further manual search was performed among the references of selected papers and related reviews.
Study Selection
Studies were included if they satisfied the following criteria: (a) participants were general older Chinese adults aged 50 years or above; (b) reported the prevalence of insomnia symptoms, as measured by validated screeners of insomnia, including PSQI, ISI, and Athens Insomnia Scale (AIS); and (c) cross-sectional or cohort studies (only the baseline data were extracted) that were conducted in China during the COVID-19 pandemic. We also included general population-based studies that separately presented elderly-specific prevalence of insomnia symptoms. We excluded studies focusing on special populations such as COVID-19 patients, older adults living in long-term care facilities, and old patients with major medical conditions, as well as those using unstandardized assessments of insomnia. Currently, there is no agreement on the cut-off age to define older adults (24). Following several previous studies (25, 26), older adults were defined as those aged 50 years or older in the present study. Because PSQI has been widely used as a screener of insomnia and it has comparable accuracy for insomnia screening compared to ISI and AIS (27, 28), PSQI is suitable for detecting the presence of insomnia symptoms.
Data Extraction
We extracted the following information from included studies: first author, publication year, study site, survey date, survey method, sampling approach, sample size, insomnia screener, and rate of insomnia symptoms.
RoB Assessment of Included Studies
The Joanna Briggs Institute Critical Appraisal Checklist for Studies Reporting Prevalence Data (“JBI checklist” hereafter) was used to measure the level of RoB of included studies (29). The JBI checklist has nine methodology domains: sample frame, sampling, sample size, description of participants and setting, sample coverage of the data analysis, validity of the instrument for assessing the outcome, standardization and reliability of the instrument for assessing outcome, statistical analysis, and response rate (30). Each domain has four options (yes, no, unclear, or not applicable) and one point is assigned to a “yes” answer. The total RoB score ranges between zero and nine, with a higher score denoting a lower RoB.
Statistical Analysis
We used the “metaprop” package of R, version 4.0.2, to conduct the meta-analysis. I2 statistic was used to test heterogeneity between studies and, when there was evidence of heterogeneity (I2 > 50%), a random-effect model was used to generate the pooled estimate of prevalence. Subgroup analysis was used to explore the source of heterogeneity in the prevalence estimate of insomnia symptoms. Publication bias was assessed by funnel plots, Egger's regression model, and Begg's test. Because Generalized Linear Mixed Models (GLMMs) perform better than the conventional two-step approach when small-sample studies are included for synthesizing proportions, GLMMs were used to directly model event counts without data transformation within studies (31). Sensitivity analysis was conducted by removing each study individually to assess the robustness of pooled estimate of prevalence. P < 0.05 (two-sided) was deemed as statistically significant.
Results
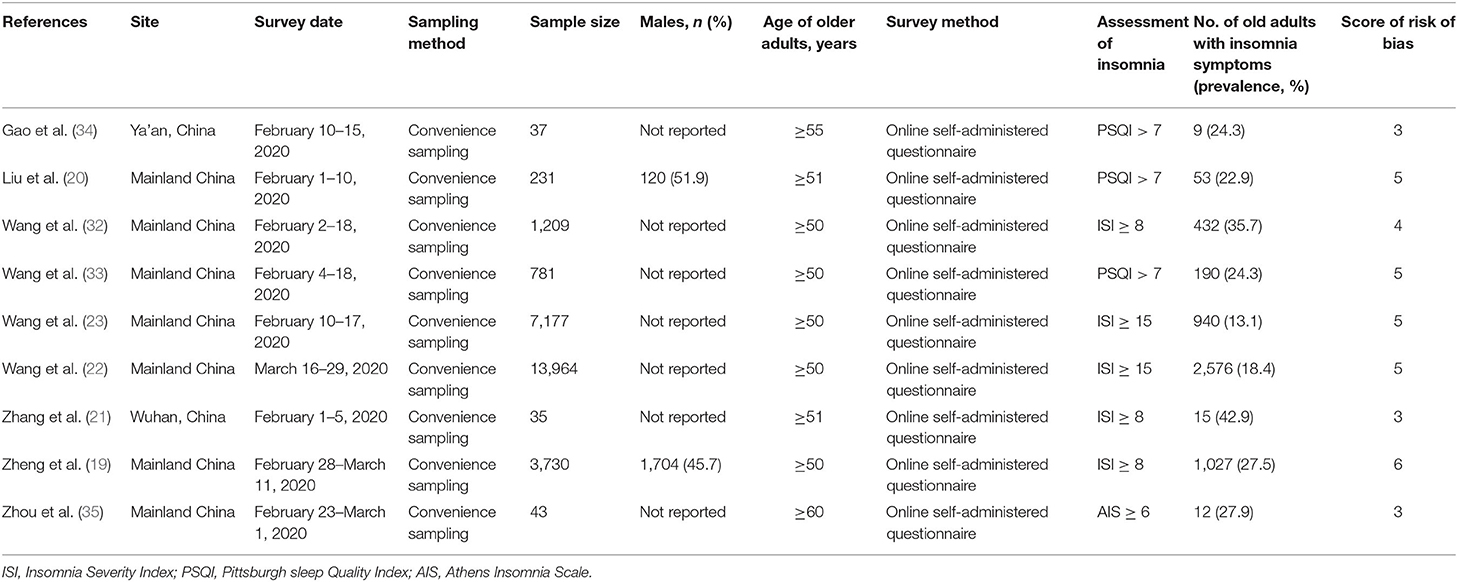
Altogether, nine studies with 27,207 older Chinese adults were eligible and included (Figure 1) (19–23, 32–35). All studies assessed the presence of insomnia symptoms in convenient samples of older adults during the outbreak period of COVID-19 in China. With regard to the insomnia screener, five studies used ISI, three used PSQI, and one used AIS. Detailed characteristics of included studies are displayed in Table 1.
The JBI checklist scores of the studies ranged between three and six. No studies were rated as low RoB (JBI checklist score = 9) (Table 1). The three most common limitations were inappropriate way of sampling of participants (9/9), unclear response rates of study samples (9/9), and unclear information for assessing whether the outcome was measured in a standard, reliable way for all participants (9/9).
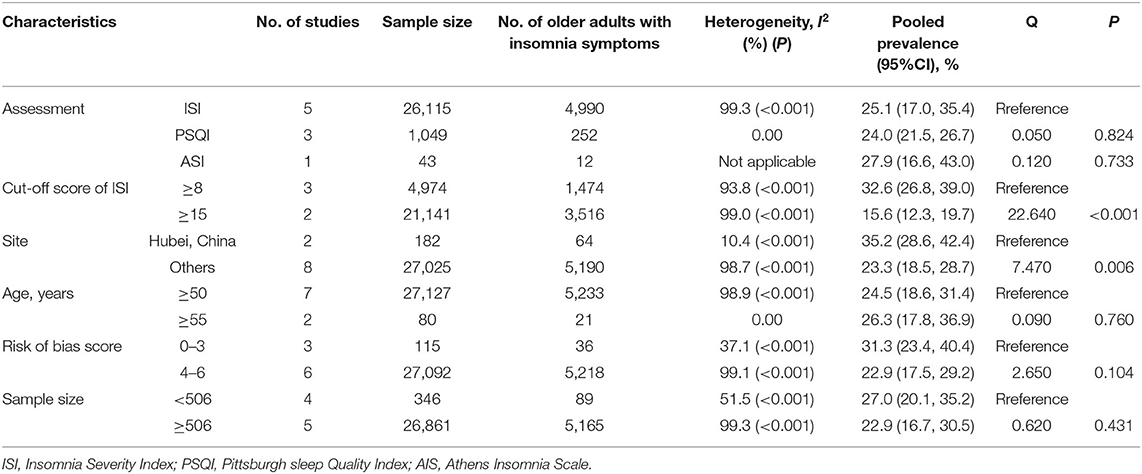
The pooled prevalence rates of insomnia symptoms and moderate and severe insomnia symptoms were 24.6% [95% confidence interval (CI): 19.5–30.5%] and 11.1% (95% CI: 7.2–16.9%), respectively (Figure 2). Results of subgroup analysis showed that significantly higher prevalence rates were observed in studies defining the presence of insomnia symptoms as “ISI ≥ 8” than in those defining it as “ISI ≥ 15” (32.6 vs. 15.6%, P < 0.001) and in studies carried out in the COVID-19 epicenter than in those in other places (35.2 vs. 23.3%, P = 0.006) (Table 2).
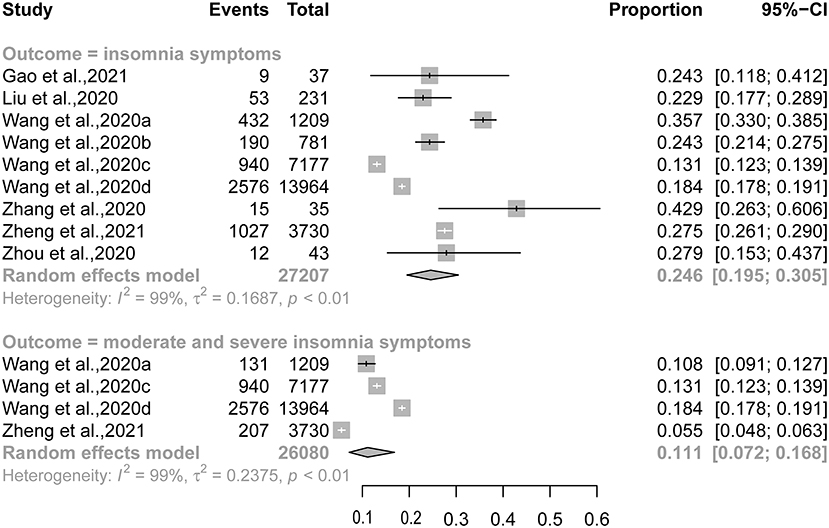
Figure 2. Forest plot of the prevalence of insomnia symptoms and moderate and severe insomnia symptoms.
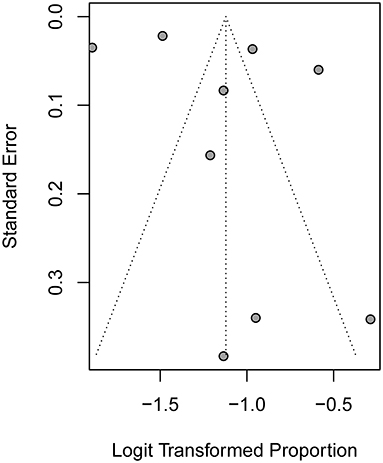
The Egger's test (t = 0.97, P = 0.365) and Begg's test (z = 0.210, P = 0.835) revealed no statistically significant publication bias (Figure 3).
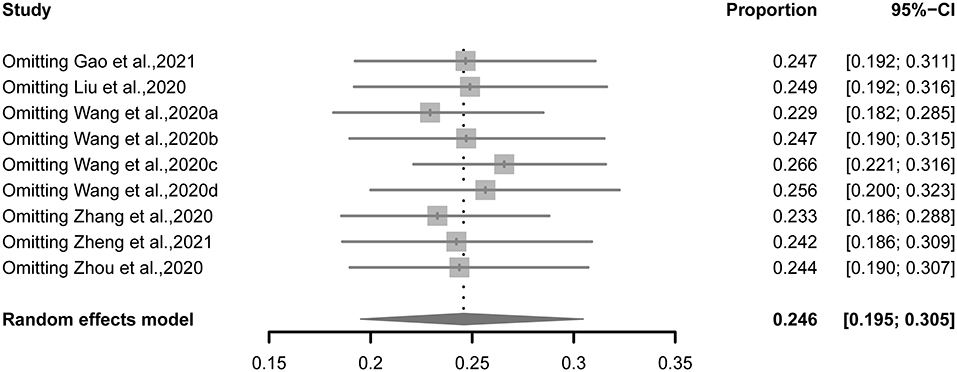
When each study was excluded sequentially, the pooled estimate of prevalence (22.9–26.6%) and heterogeneity across studies (I2: 97.7–98.8%) were not altered significantly, suggesting that no outlying study could influence the overall results of the meta-analysis (Figure 4).
Discussion
This meta-analysis quantitatively summarized studies estimating the prevalence of insomnia symptoms in older adults in China amid the COVID-19 pandemic. We found an overall prevalence rate of 24.6% of insomnia symptoms in older Chinese adults and significantly higher rates in studies defining insomnia symptoms as “ISI ≥ 8” (vs. “ISI ≥ 15”) and older adults living within the COVID-19 epicenter (vs. other places). In addition, 11.1% of the older Chinese adults had moderate and severe insomnia symptoms.
Compared to the 24.4–26.8% prevalence of insomnia symptoms among older Chinese adults during the non-pandemic era (1–3), a comparable prevalence of insomnia symptoms (24.6%) was found in older Chinese adults during the pandemic. This estimate seems to not support the additional risk of insomnia exerted by the pandemic. Nevertheless, we argue that the result from this direct comparison should be considered cautiously owing to the significant heterogeneity in the methodologies of included studies. For example, most studies included in this meta-analysis defined older adults as those aged 50 years or over but the aforementioned 24.4–26.8% prevalence estimate was derived from studies of older adults aged 60 years or above (1–3). Because there is evidence showing an increasing prevalence of insomnia symptoms with increasing age in older Chinese adults (3, 36), our study should have a higher prevalence estimate of insomnia symptoms in older adults during the pandemic if older adults were those aged 60+ years. Moreover, as displayed in Table 2, when studies were limited to those defining the presence of insomnia symptoms as “ISI ≥ 8,” the synthesized prevalence rose to 32.6%, which is higher than the aforementioned 24.4–26.8% prevalence in older adults during the non-pandemic era (1–3). In addition, in our study the 11.1% prevalence of moderate and severe insomnia symptoms indicates that nearly a half (11.1/24.6%) of the older adults with insomnia symptoms are severe enough for clinical attention. These data may suggest an elevated risk of insomnia symptoms in older Chinese adults during the COVID-19 pandemic.
In the literature, living in Hubei or its capital city, Wuhan, was significantly associated with insomnia symptoms in both the general population and older adults in China (19, 37). In accordance with these studies, our meta-analysis confirmed the significantly higher risk of insomnia symptoms in older adults living within the COVID-19 epicenter than in those living in other places. This may be ascribed to the longer duration of mass quarantine, more strict social distancing measures, and higher risk of exposure to COVID-19 in persons living within than those living outside the epicenter (12).
The strength of this meta-analysis is the large sample size of older Chinese adults, which provided an overall and reliable estimate of the prevalence of insomnia symptoms in this vulnerable population during the COVID-19 pandemic. Nevertheless, this study also has a few limitations. First, none of the included studies were of low RoB. Because subgroup analysis according to RoB score revealed a trend toward lower prevalence of insomnia symptoms in studies with higher RoB scores (Table 2), we may have overestimated the true prevalence of insomnia symptoms in older Chinese adults during the pandemic. However, as we argued above, several included studies used strict criteria to define the presence of insomnia symptoms (i.e., “ISI ≥ 15”), so we may have underestimated the true prevalence of insomnia symptoms. Given the two limitations, it is difficult to evaluate the extent and direction of bias in the prevalence estimate. Second, since sex-specific and region-specific (i.e., urban vs. rural) prevalence data were available in only one of the included studies (19), this meta-analysis was not able to provide data on the demographic characteristics of insomnia symptoms in older adults. Third, all of the included studies were conducted during the COVID-19 outbreak period, so it remains unclear whether the sleep quality of older adults improves or worsens during the post-outbreak period. Finally, data on healthcare services utilization of older adults with moderate and severe insomnia symptoms are important for mental health policy-making during the pandemic, but the included studies had no such data.
In summary, nearly one out of every four older Chinese adults suffered from insomnia symptoms, suggesting a high level of mental healthcare need in this population in the context of COVID-19 pandemic. Insomnia has been associated with a range of physical and mental morbidities and elevated mortality in older adults (4). Given the high prevalence of insomnia symptoms, mental health services for this population during the pandemic should include supportive activities aimed at improving mental well-being, periodic assessment of insomnia symptoms to ensure early recognition of older adults who meet the diagnostic criteria for clinical insomnia, and psychiatric assessment and treatment when necessary. The higher prevalence rate of insomnia symptoms in older adults living in the epicenter indicates that more mental health resources should be assigned to older adults in the COVID-19 epicenter. In addition, prospective studies are warranted to understand the longitudinal changes of insomnia symptoms in older Chinese adults during the post-outbreak era.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Author Contributions
Q-QZ: acquisition and analysis of data for the study, drafting the paper, and interpretation of data for the study. LL: design and acquisition of data for the study. B-LZ: drafting the paper, revising the paper for important intellectual content, and interpretation of data for the study. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by National Natural Science Foundation of China (Grant Number: 71774060) and 2015 Irma and Paul Milstein Program for Senior Health Awards from the Milstein Medical Asian American Partnership Foundation. The two funding sources listed had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.779914/full#supplementary-material
1. Lu L, Wang SB, Rao W, Zhang Q, Ungvari GS, Ng CH, et al. The prevalence of sleep disturbances and sleep quality in older chinese adults: a comprehensive meta-analysis. Behav Sleep Med. (2019) 17:683–97. doi: 10.1080/15402002.2018.1469492
2. Zhang J, Lu C, Tang J, Qiu H, Liu L, Wang S, et al. A sleep quality investigation of the people aged 60 and above of Shandong province. Chin J Behav Med Brain Sci. (2008) 17:41–4. doi: 10.3760/cma.j.issn.1674-6554.2008.01.017
3. Wu X, Chen X, Jiang X, Yang S, Lu H, Feng Y, et al. Sleep quality and its associated factors in Chinese elderly in Chengdu. Chin J Gerontol. (2021) 41:189–91.
4. Patel D, Steinberg J, Patel P. Insomnia in the elderly: a review. J Clin Sleep Med. (2018) 14:1017–24. doi: 10.5664/jcsm.7172
5. Kamel NS, Gammack JK. Insomnia in the elderly: cause, approach, and treatment. Am J Med. (2006) 119:463–9. doi: 10.1016/j.amjmed.2005.10.051
6. Wand APF, Zhong BL, Chiu HFK, Draper B, De Leo D. COVID-19: the implications for suicide in older adults. Int Psychogeriatr. (2020) 32:1225–30. doi: 10.1017/S1041610220000770
7. Vahia IV, Jeste DV, Reynolds CF 3rd. Older adults and the mental health effects of COVID-19. JAMA. (2020) 324:2253–4. doi: 10.1001/jama.2020.21753
8. Bao L, Li WT, Zhong BL. Feelings of loneliness and mental health needs and services utilization among Chinese residents during the COVID-19 epidemic. Global Health. (2021) 17:51. doi: 10.1186/s12992-021-00704-5
9. Wu B. Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Glob Health Res Policy. (2020) 5:27. doi: 10.1186/s41256-020-00154-3
10. Yang Y, Li W, Zhang Q, Zhang L, Cheung T, Xiang YT. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e19. doi: 10.1016/S2215-0366(20)30079-1
11. Weil J, Kamber T, Glazebrook A, Giorgi M, Ziegler K. Digital inclusion of older adults during COVID-19: lessons from a case study of older adults technology services (OATS). J Gerontol Soc Work. (2021) 64:643–55. doi: 10.1080/01634372.2021.1919274
12. Zhong BL, Zhou DY, He MF, Li Y, Li WT, Chee HN, et al. Mental health problems, needs, and service use among people living within and outside Wuhan during the COVID-19 epidemic in China. Ann Transl Med. (2020) 8:1392. doi: 10.21037/atm-20-4145
13. Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. (2021) 1486:90–111. doi: 10.1111/nyas.14506
14. Zhao YJ, Jin Y, Rao WW, Li W, Zhao N, Cheung T, et al. The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: a systematic review and meta-analysis of observational studies. J Affect Disord. (2021) 287:145–57. doi: 10.1016/j.jad.2021.03.016
15. Lin YN, Liu ZR, Li SQ, Li CX, Zhang L, Li N, et al. Burden of sleep disturbance during COVID-19 pandemic: a systematic review. Nat Sci Sleep. (2021) 13:933–66. doi: 10.2147/NSS.S312037
16. Han Y, He Y, Lyu J, Yu C, Bian M, Lee L. Aging in China: perspectives on public health. Global Health J. (2020) 4:11–7. doi: 10.1016/j.glohj.2020.01.002
17. Zhong BL, Chen SL, Tu X, Conwell Y. Loneliness and cognitive function in older adults: findings from the Chinese longitudinal healthy longevity survey. J Gerontol B Psychol Sci Soc Sci. (2017) 72:120–8. doi: 10.1093/geronb/gbw037
18. Zhong BL, Liu XJ, Chen WC, Chiu HF, Conwell Y. Loneliness in Chinese older adults in primary care: prevalence and correlates. Psychogeriatrics. (2018) 18:334–42. doi: 10.1111/psyg.12325
19. Zheng YB, Shi L, Lu ZA, Que JY, Yuan K, Huang XL, et al. Mental health status of late-middle-aged adults in china during the coronavirus disease 2019 pandemic. Front Public Health. (2021) 9:643988. doi: 10.3389/fpubh.2021.643988
20. Liu C, Liu D, Huang N, Fu M, Ahmed JF, Zhang Y, et al. The combined impact of gender and age on post-traumatic stress symptoms, depression, and insomnia during COVID-19 outbreak in China. Front Public Health. (2020) 8:620023. doi: 10.3389/fpubh.2020.620023
21. Zhang L, Zhang B, Hu L. The relationship between perceived stress and sleep quality of Wuhan residents during COVID-19 outbreak: psychological resilience as a moderator. Chin J Dis Contr Prev. (2020) 24:638–42. doi: 10.16462/j.cnki.zhjbkz.2020.06.004
22. Wang S, Zhang Y, Guan Y, Ding W, Meng Y, Hu H, et al. A nationwide evaluation of the prevalence of and risk factors associated with anxiety, depression and insomnia symptoms during the return-to-work period of coronavirus disease 2019 in China. Soc Psychiatry Psychiatr Epidemiol. (2021). doi: 10.1007/s00127-021-02046-4. [Epub ahead of print].
23. Wang S, Zhang Y, Ding W, Meng Y, Hu H, Liu Z, et al. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: a nationwide multicenter cross-sectional study. Eur Psychiatry. (2020) 63:e77. doi: 10.1192/j.eurpsy.2020.78
24. Singh S, Bajorek B. Defining 'elderly' in clinical practice guidelines for pharmacotherapy. Pharm Pract. (2014) 12:489. doi: 10.4321/S1886-36552014000400007
25. Rubin DS, Huisingh-Scheetz M, Ferguson MK, Nagele P, Peden CJ, Lauderdale DS. U.S. trends in elective and emergent major abdominal surgical procedures from 2002 to 2014 in older adults. J Am Geriatr Soc. (2021) 69:2220–30. doi: 10.1111/jgs.17189
26. Sabharwal S, Wilson H, Reilly P, Gupte CM. Heterogeneity of the definition of elderly age in current orthopaedic research. Springerplus. (2015) 4:516. doi: 10.1186/s40064-015-1307-x
27. Chiu HY, Chang LY, Hsieh YJ, Tsai PS. A meta-analysis of diagnostic accuracy of three screening tools for insomnia. J Psychosom Res. (2016) 87:85–92. doi: 10.1016/j.jpsychores.2016.06.010
28. Ali RM, Zolezzi M, Awaisu A. A systematic review of instruments for the assessment of insomnia in adults. Nat Sci Sleep. (2020) 12:377–409. doi: 10.2147/NSS.S250918
29. Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. (2014) 3:123–8. doi: 10.15171/ijhpm.2014.71
30. Luo W, Zhong BL, Chiu HF. Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: a systematic review and meta-analysis. Epidemiol Psychiatr Sci. (2021) 30:e31. doi: 10.1017/S2045796021000202
31. Lin L, Chu H. Meta-analysis of proportions using generalized linear mixed models. Epidemiology. (2020) 31:713–7. doi: 10.1097/EDE.0000000000001232
32. Wang M, Liu X, Guo H, Fan H, Jiang R, Tan S. Mental health of middle-aged and elderly population during outbreak of coronavirus disease 2019. Chin J Mult Organ Dis Elderly. (2020) 19:241–5.
33. Wang J, Gong Y, Chen Z, Wu J, Feng J, Yan S, et al. Sleep disturbances among Chinese residents during the coronavirus disease 2019 outbreak and associated factors. Dermatol Ther. (2020) 74:199–203. doi: 10.1016/j.sleep.2020.08.002
34. Gao R, Zhang B, Peng S, Bai J, Xu L, Wang D, et al. Mental health status of the general population during the COVID-19 epidemic in Ya'an city. Chin Mental Health J. (2021) 35:79–84. doi: 10.3969/j.issn.1000-6729.2021.01.014
35. Zhou Q, Hu Z, Bian G, Yu H, Li X, Lu Y, et al. Mental health and psychosocial function of general population during the COVID-19 epidemic in China. Clin Transl Med. (2020) 10:e103. doi: 10.1002/ctm2.103
36. Zhu Q, Jian W, Yang L, Wu Z, Zhuo L, Wang H. Sleep quality and its associated factors in community-dwelling Chinese older adults. Chin J Gerontol. (2019) 39:606–11.
Keywords: insomnia, older adults, prevalence, COVID-19, China
Citation: Zhang Q-Q, Li L and Zhong B-L (2021) Prevalence of Insomnia Symptoms in Older Chinese Adults During the COVID-19 Pandemic: A Meta-Analysis. Front. Med. 8:779914. doi: 10.3389/fmed.2021.779914
Received: 20 September 2021; Accepted: 12 October 2021;
Published: 15 November 2021.
Edited by:
Tzvi Dwolatzky, Technion Israel Institute of Technology, IsraelReviewed by:
Yu Jin, Beijing Normal University, ChinaYuan Yang, Southern Medical University, China
Modesto Leite Rolim Neto, Universidade Federal do Cariri, Brazil
Copyright © 2021 Zhang, Li and Zhong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bao-Liang Zhong, aGFpemhpbGFuQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
 Qian-Qian Zhang
Qian-Qian Zhang Lan Li†
Lan Li† Bao-Liang Zhong
Bao-Liang Zhong