- 1Department of Urology/Institute of Urology, West China Hospital, Sichuan University, Chengdu, China
- 2West China School of Clinical Medicine, Sichuan University, Chengdu, China
- 3Department of Urology, Nanchong Central Hospital, The Second Clinical Medical College, North Sichuan Medical College, Nanchong, China
- 4Department of Urology, The First Affiliated Hospital of Kunming Medical University, Kunming, China
Background: Minimally invasive simple prostatectomy (MISP) and endoscopic enucleation of the prostate (EEP) are the two most commonly used methods for large benign prostatic hyperplasia (BPH), but it remains unclear which of the two is superior. This study aims to perform a pooled analysis to compare efficacy and safety profiles between MISP and EEP.
Methods: We conducted a comprehensive search of PubMed, Embase, Web of Science, and ClinicalTrials.gov databases to identify eligible studies comparing MISP with EEP. Parameters including efficacy and safety outcomes were compared using Stata 14.0 version.
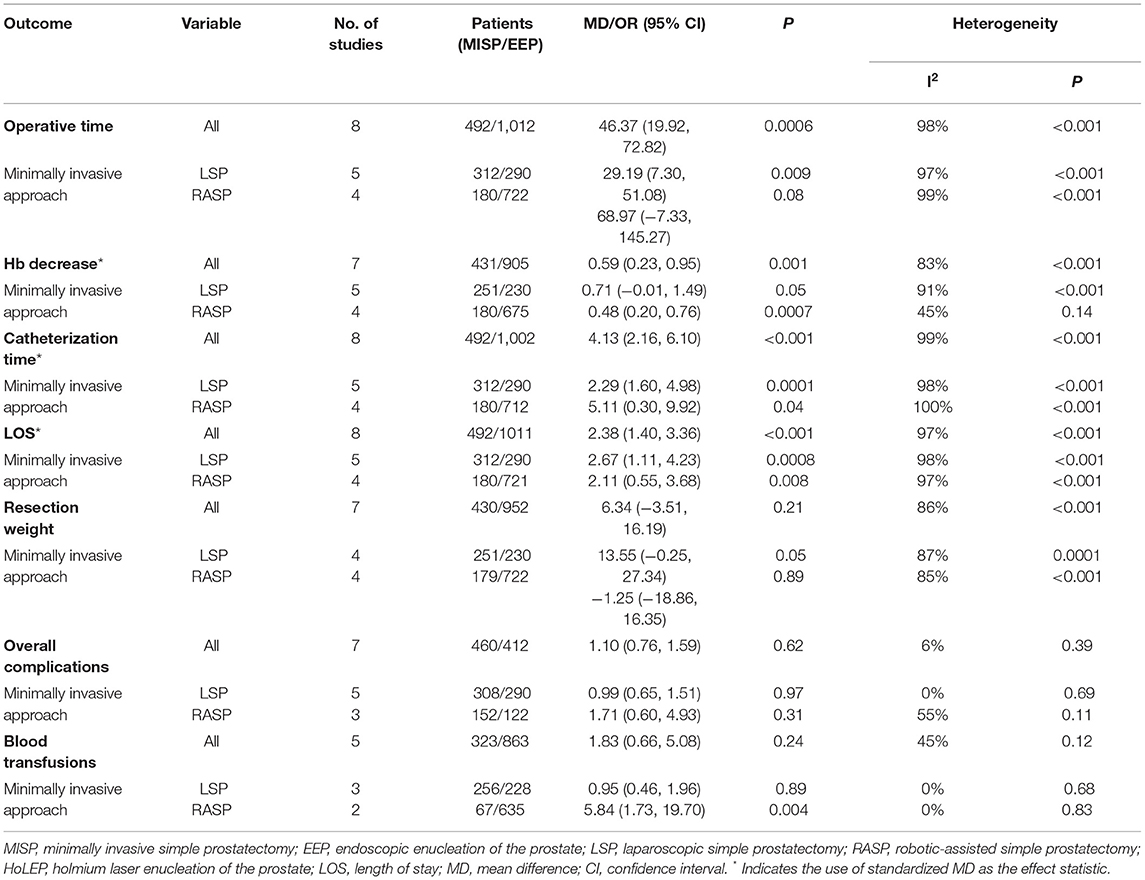
Results: Eight comparative trials with 1,504 patients were included. Compared to MISP, EEP demonstrated shorter operative time (mean difference [MD] 46.37, 95% confidence interval [CI] 19.92 to 72.82, p = 0.0006), lesser hemoglobin decrease (standardized MD [SMD] 0.59, 95% CI 0.23 to 0.95, p = 0.001), lower catheterization time (SMD 4.13, 95% CI 2.16 to 6.10, p < 0.001), and shorter length of stay (SMD 2.38, 95% CI 1.40 to 3.36, p < 0.001). However, overall complications and blood transfusions did not differ between the two groups. Moreover, EEP had better postvoid residual volume (PVR) at 6-month (MD 14.39, 95% CI 11.06 to 17.72, p < 0.001) and comparable 3- and 6-month International Prostate Symptom Score, 3- and 6-month maximum flow rate, 3-month PVR, and 3-month quality of life compared with MISP.
Conclusion: Both MISP and EEP are effective and safe surgical procedures for the treatment of large BPH. EEP appears to have a superior perioperative profile compared to MISP. This should be interpreted with caution due to the significant heterogeneity between studies. Hence, treatment selection should be based on the surgeon's experience and availability.
Introduction
Benign prostatic hyperplasia (BPH) is a common disease in elderly men, and its incidence increases gradually with age. The obstruction of the lower urinary tract caused by an enlarged prostate brings great trouble to the life of patients (1). Surgical intervention is required when patients with BPH have severe complications or non-responding well to pharmacological treatment (2). Current guidelines recommend open simple prostatectomy (OSP) as the gold standard procedure for large BPH (prostate volume > 80 mL) (3, 4), but it is related to higher postoperative complications and longer length of stay (LOS) (5, 6). For these reasons, several surgical approaches including endoscopic enucleation of the prostate (EEP) and minimally invasive simple prostatectomy (MISP) have been mentioned and introduced to reduce the morbidity associated with open surgery.
EEP based on laser or bipolar technology has proven to be a safe and efficacious treatment for BPH. A growing body of literature suggests that it has superior perioperative outcomes while providing the same clinical efficacy as OSP (7). Therefore, EEP is considered the standard therapy for treating large prostates (3). In recent years, laparoscopic and robotic techniques have been widely adopted in urological surgery because of their advantages of low trauma and quick recovery. MISP is a relatively new technique for large BPH through a laparoscopic or robot-assisted approach. This technique appears to be more attractive than OSP, as it offers less blood loss, shorter LOS, and lower perioperative complications (8). Both MISP and EEP are considered alternatives to OSP (7, 8), however, there is no common consensus as to which approach is most appropriate.
Therefore, this study aimed to incorporate available clinical studies to systematically compare the efficacy and safety of MISP and EEP for large BPH, and provide the latest evidence for clinical practice.
Methods
This present study has been reported following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statement (9) and has been registered on PROSPERO: CRD42021239950.
Search Strategy
We conducted a comprehensive search of PubMed, Embase, Web of Science, and ClinicalTrials.gov databases to identify eligible studies comparing MISP and EEP for the treatment of large prostates and published in English from database establishment through August 2021. The database was searched using the following terms: “minimally invasive”, “laparoscopic”, “laparoscopy”, “robot”, “robotic”, “robot-assisted”, “robotic-assisted” “simple prostatectomy”, “adenomectomy”, “enucleation”, “prostate”, and “benign prostatic hyperplasia”. Moreover, relevant references for all eligible studies were also manually searched. Two authors independently reviewed the literature and any discrepancies were addressed through discussion with the third author.
Identification of Eligible Studies
The inclusion criteria for the study were defined as follows: (1) comparative studies comparing one of the minimally invasive methods (laparoscopic simple prostatectomy [LSP] and robot-assisted simple prostatectomy [RASP]) with the EEP procedure (laser or bipolar enucleation) for the treatment of patients with prostate volume > 80 mL; (2) data on efficacy or safety outcomes (or both) were provided. Non-comparative studies, reviews, case reports, letters, meeting abstracts, unpublished studies, and non-English articles were excluded.
Data Extraction
Data extraction was carried out independently by the two authors, and differences were resolved through discussion with the third author. The following data were extracted from the included studies: first author, publication year, country of study, study design, intervention, number of patients, age, body mass index (BMI), follow-up time, prostate volume, International Prostate Symptom Score (IPSS), maximum flow rate (Qmax), postvoid residual volume (PVR) quality of life (QoL), prostate-specific antigen (PSA), operative time, hemoglobin (Hb) decrease, catheterization time, LOS, resection weight, and complications. In addition, the data in the original study were converted to mean and standard deviation (SD) by computational expressions (10). If available, complications based on the Clavien-Dindo classification (CDC) system classification were analyzed.
Quality Assessment
The quality of all included studies was assessed using the Newcastle-Ottawa scale (maximum score 9) (11). In the current meta-analysis, studies with scores ≥ 7 were considered high quality. Two independent reviewers evaluated the quality of included studies, and any differences were resolved through consultation with a third reviewer.
Statistical Analysis
In this study, Stata 14.0 version (Stata Corp, College Station, TX, US) was used for statistical analysis. The mean difference (MD) or the standardized MD (SMD) and odds ratio (OR) were used as effect analysis statistics for continuous and dichotomous variables, respectively. The random-effects model was adopted in the analyses. Heterogeneity among studies was measured using the Chi-square (χ2) and inconsistency index (I2) tests, and P < 0.10 or I2 > 50% was regarded as significant heterogeneity. 95% confidence intervals (CIs) were calculated for all statistics. P < 0.05 was considered statistically significant. Furthermore, the sensitivity analysis was performed by excluding one or more studies that might have contributed to heterogeneity. Funnel plot and Begg's test were used to assess potential publication bias.
Results
Literature Search and Study Characteristics
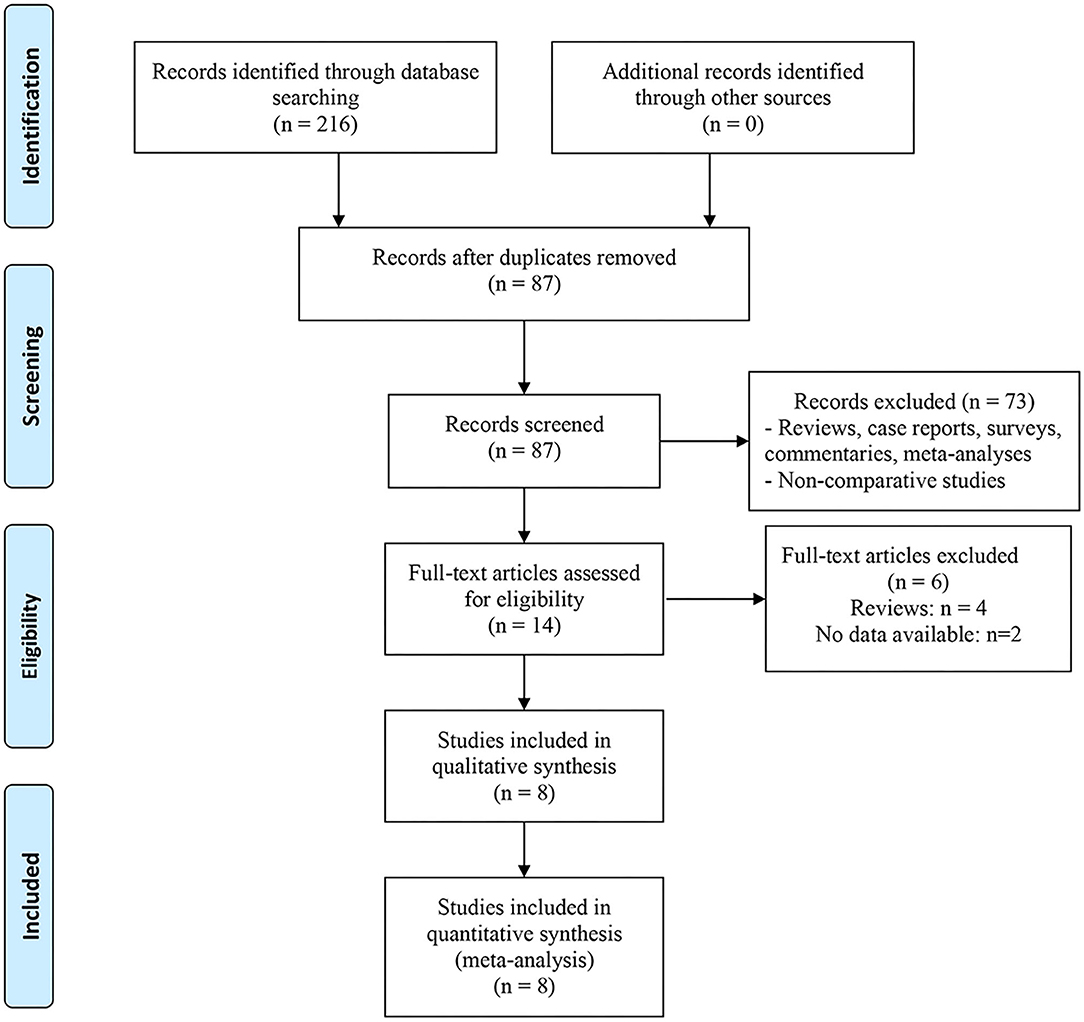
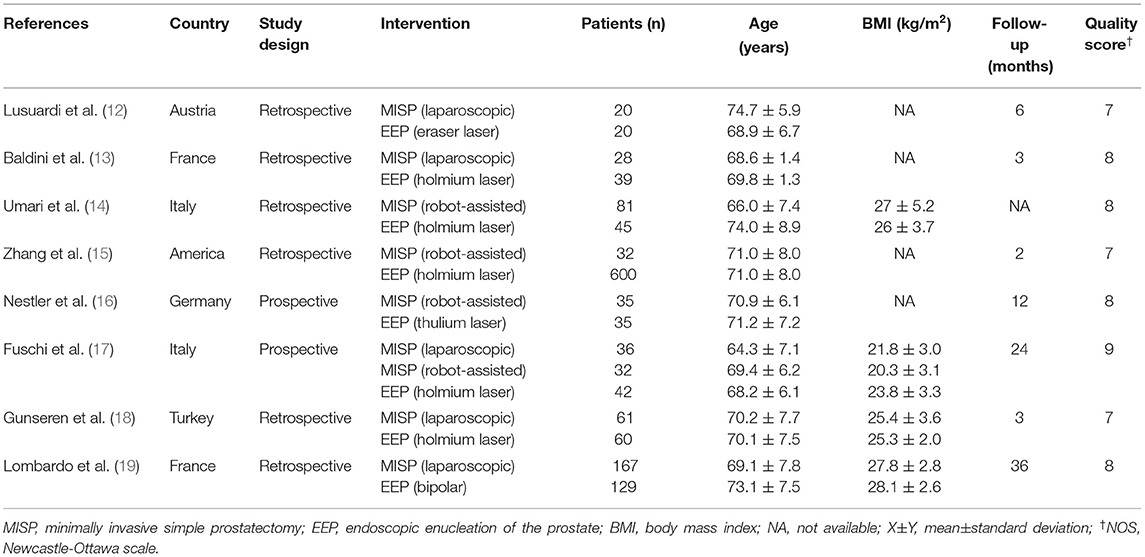
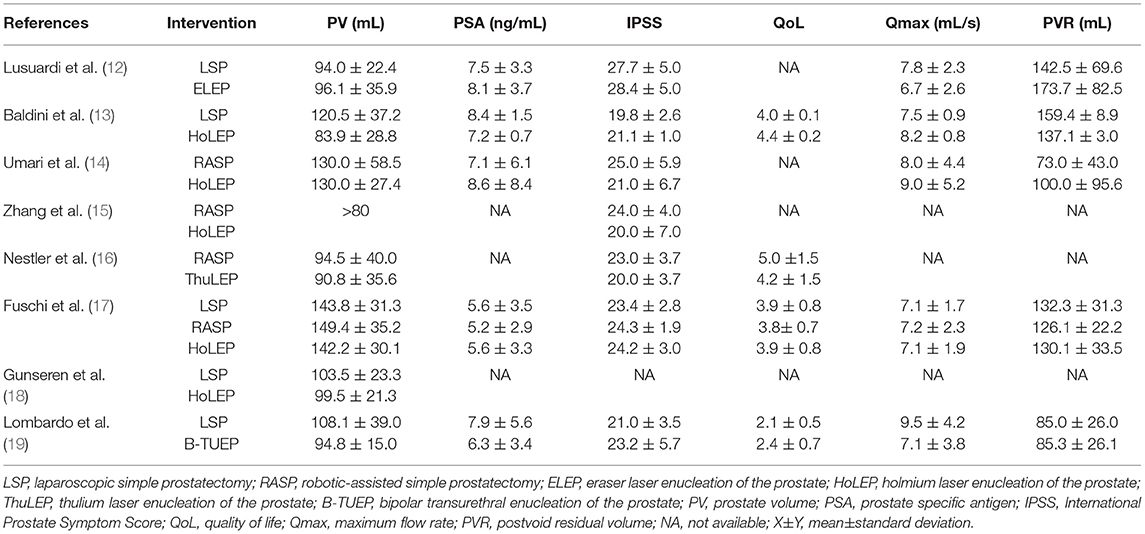
The screening process is presented in Figure 1, 216 studies were preliminarily retrieved, and 87 remained after duplicates were removed. We excluded 73 studies after reviewing abstracts and titles, and 6 articles after reading the full text. Finally, 8 studies involving 1,504 patients (492 MISP vs. 1,012 EEP) were included in the present meta-analysis (12–19). These studies were published between 2015 and 2021. Among them, one was a prospective study (16), six were retrospective studies (12–15, 18, 19), and one was a prospective randomized study (17). Four studies (12, 13, 18, 19) focused on the comparison of LSP and EEP, three studies (14–16) focused on the comparison of RASP and EEP, and only one study (17) analyzed the comparison of LSP, RASP, and EEP. Additionally, since Fuschi et al. (17) reported the comparison of two MISP technologies (LSP and RASP) with EEP, we divided their results into two parts and presented them as Fuschi 2020a (LSP vs. EEP) and Fuschi 2020b (RASP vs. EEP) during data analysis. The characteristics of all patients in each study are presented in Tables 1, 2. The quality evaluation results indicated that all the studies were rated as high quality, and detailed scores for each study are shown in Supplementary Material 1.
Efficacy Outcomes
The short-term efficacy outcomes of MISP and EEP were evaluated in the meta-analysis. Five studies (12–14, 17, 19) showed that there were no significant differences in 3-month (MD −0.89, 95% CI −2.02 to 0.25, p = 0.13) and 6-month (MD 0.28, 95% CI −0.39 to 0.94, p = 0.42) IPSS between MISP and EEP groups (Figure 2). Five trials (12–14, 17, 19) reported postoperative Qmax data (Figure 2), and no significant differences were observed regarding Qmax between groups at 3-month (MD 1.04, 95% CI −0.63 to 2.71, p = 0.22) and 6-month (MD 0.95, 95% CI −5.00 to 6.89, p = 0.76). Postoperative PVR was obtained from 4 studies (12, 13, 17, 19) (Figure 3). The 3-month (MD−1.22, 95% CI −9.73 to 7.30, p = 0.78) PVR was similar between the groups. However, the MISP group had higher 6-month PVR (MD 14.39, 95% CI 11.06 to 17.72, p < 0.001) than the EEP group. Three trials (13, 17, 19) compared postoperative QOL in the MISP and EEP groups (Figure 3). There was no difference in 3-month QoL (MD −0.13, 95% CI −0.79 to 0.52, p = 0.69). Furthermore, four studies (13, 14, 17, 19) reported the postoperative PSA (Figure 3), and MISP had the same PSA as the EEP group during short-term follow-up (MD −0.19, 95% CI −0.55 to 0.18, p = 0.33). Of note, there was significant heterogeneity among studies (p < 0.10) for each metric.
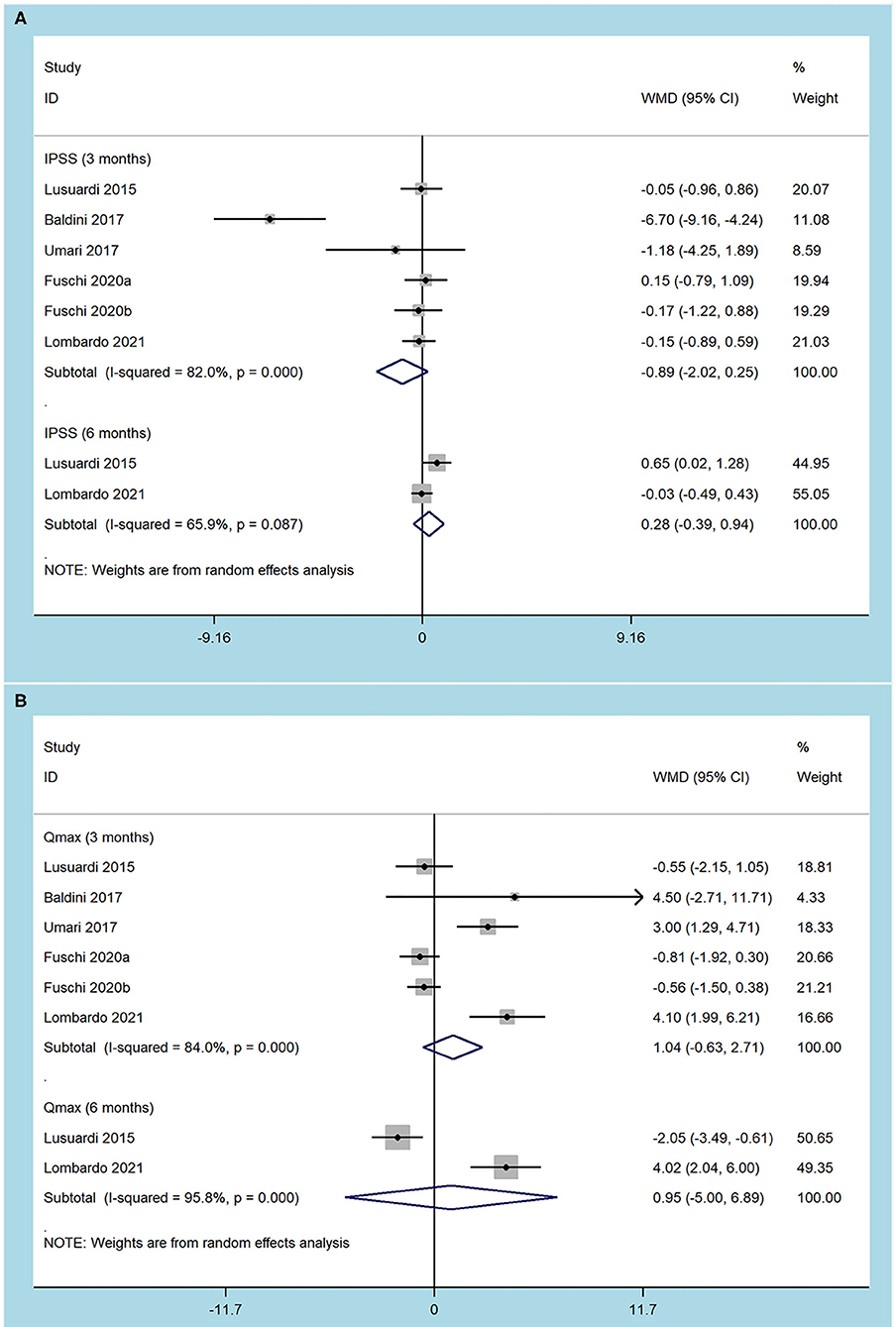
Figure 2. Forest plots of efficacy outcomes. (A) International prostate symptom score; (B) maximum flow rate.
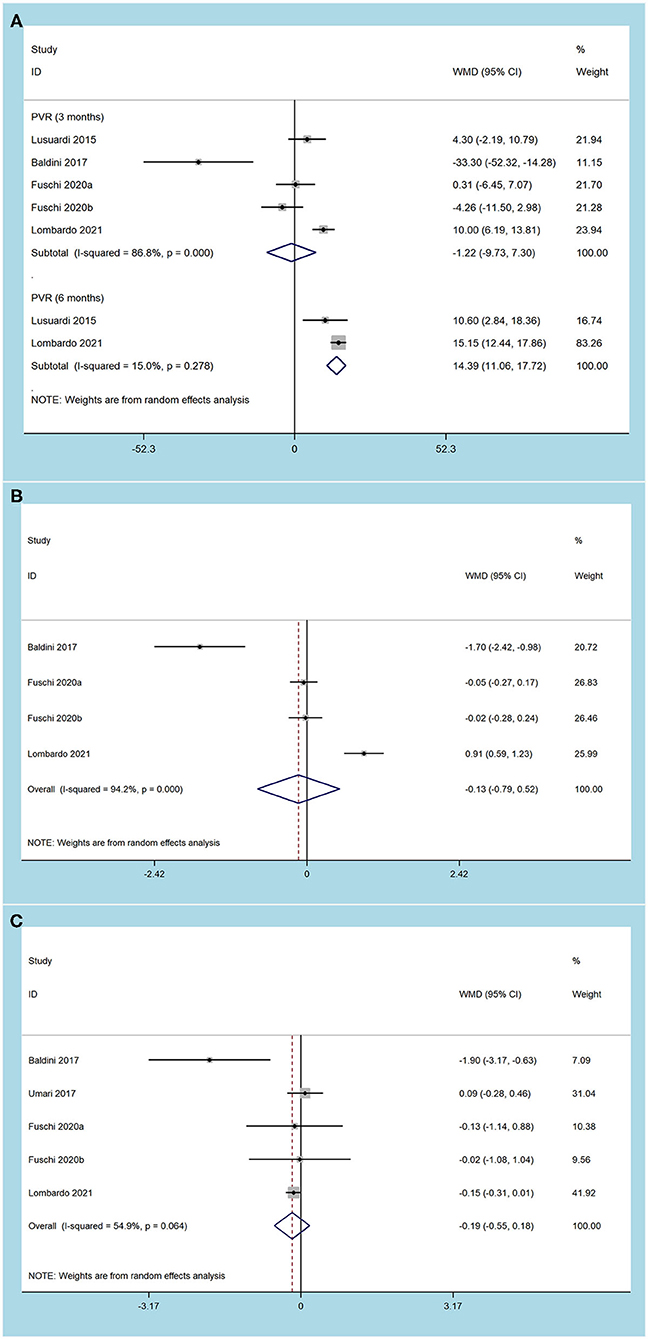
Figure 3. Forest plots of efficacy outcomes. (A) postvoid residual volume; (B) quality of life; (C) prostate specific antigen).
Perioperative Outcomes
The current analysis suggested that EEP had a shorter operative time (MD 46.37, 95% CI 19.92 to 72.82, p = 0.0006), lower Hb decrease (SMD 0.59, 95% CI 0.23 to 0.95, p = 0.001), shorter catheterization time (SMD 4.13, 95% CI 2.16 to 6.10, p < 0.001) and lower LOS (SMD 2.38, 95% CI 1.40 to 3.36, p < 0.001) compared to MISP. However, no difference was observed in the resection weight (MD 6.34, 95% CI −3.51 to 16.19, p = 0.21) between the groups. The heterogeneity test indicated that there was significant heterogeneity among studies of each outcome (p < 0.10) (Table 3).
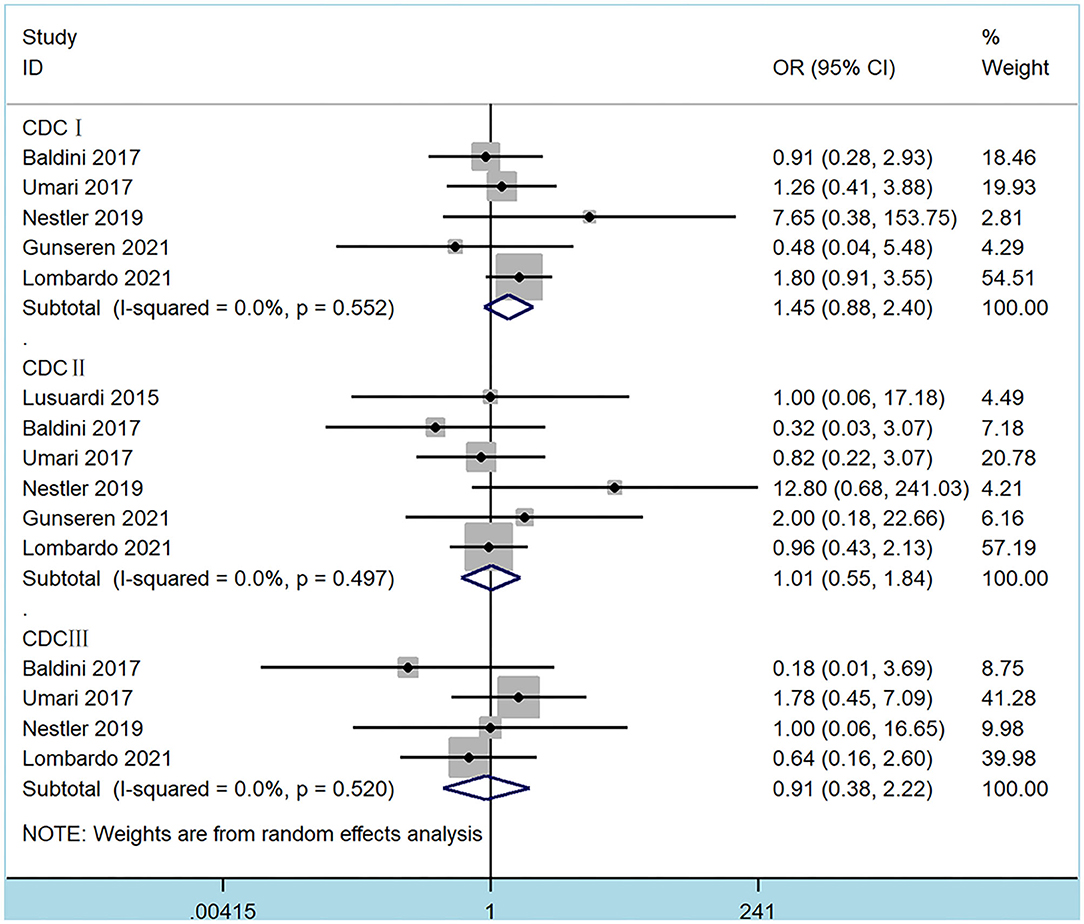
Complications
The pooled results demonstrated that MISP and EEP techniques had similar overall complications (OR 1.10, 95% CI 0.76 to 1.59, p = 0.62) and blood transfusions (OR 1.83, 95% CI 0.66 to 5.08, p = 0.24) (Table 3). Moreover, complications of CDC grade I (OR 1.45, 95% CI 0.88 to 2.40, p = 0.14), grade II (OR 1.01, 95% CI 0.55 to 1.84, p = 0.98) and grade III (OR 0.91, 95% CI 0.38 to 2.22, p = 0.84) were analyzed from 6 studies (Figure 4). No significant differences were found between MISP and EEP (all p > 0.05). Statistical heterogeneity between these studies was not significant (p > 0.10).
Subgroup Analysis
Due to the limited number of studies available for meta-analysis, we only performed subgroup analyses for perioperative outcomes and complications and stratified by minimally invasive approaches (Table 3). For subgroup with LSP, the pooled results indicated that LSP was associated with longer operative time (p = 0.009), catheterization time (p = 0.0001) and LOS (p = 0.0008) compared with EEP. However, there were no significant differences in Hb decrease, resection weight, overall complications, and blood transfusions between the groups (all p ≥ 0.05). In terms of the RASP subgroup, patients undergoing RASP had higher Hb decrease (p = 0.0007), longer catheterization time (p = 0.04), longer LOS (p = 0.008) and higher blood transfusions (p = 0.004) compared to the EEP group. However, no differences were observed regarding operative time, resection weight, and overall complications between the groups (all p ≥ 0.05).
Sensitivity Analysis
Due to the limited number of articles included in the study, we performed a sensitivity analysis of perioperative outcomes and complications. No significant change in the combined effect was observed by eliminating each study one by one, which demonstrates the stability of our results (Supplementary Material 2).
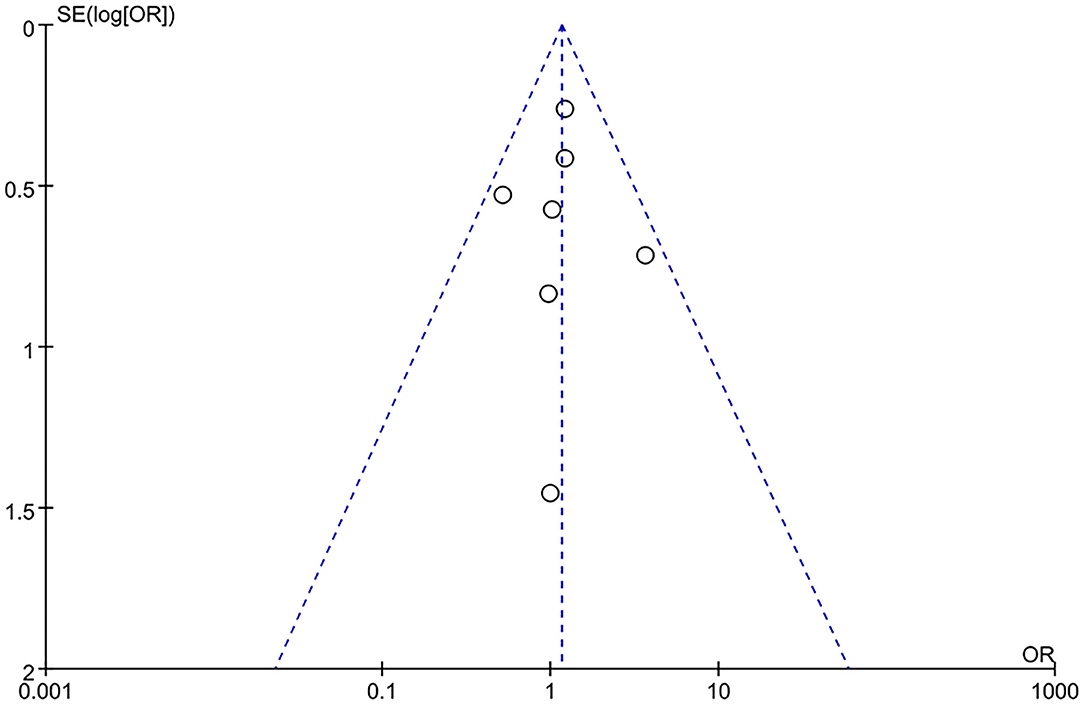
Publication Bias
Publication bias analysis was performed based on overall complications index, no significant publication bias was observed in the analysis with a funnel plot (Figure 5) and in Begg's test (p > 0.1).
Discussion
Over the past several decades, OSP has been the surgical method of choice for treating large BPH, and it may disappear as minimally invasive methods continue to advance (18). EEP and MISP are currently the preferred alternative procedures, but the superiority of these two approaches remains controversial. A previous meta-analysis of comparatives studies by Abi (20) aimed at comparing MISP with laser enucleation revealed that the two methods had similar postoperative IPSS (p = 0.23) and major complications (p = 0.41). They also concluded that laser enucleation had a shorter operative time (p = 0.006), LOS (p < 0.001) and catheterization time (p < 0.001) than MISP. One problem with the Abi study is that although five studies were included for analysis, only two or three were available for comparison of postoperative functional outcomes. Therefore, with the publication of new studies related to this topic, further evaluation of the efficacy and safety of MISP and EEP is necessary.
We conducted a meta-analysis of clinical studies comparing MISP and EEP in terms of short-term efficacy, perioperative outcomes, and complications. According to the review criteria, 8 comparative trials involving 1,504 patients with large BPH were determined. The quantitative analysis demonstrated that the two surgical procedures had similar 3- and 6-month IPSS, 3- and 6-month Qmax, 3-month PVR, and 3-month QoL. Our findings are broadly consistent with previously published literature. This suggests that even though there are some differences between the different surgical procedures, they appear to be equally effective for treatment of large BPH (19). Furthermore, it should be noted that we also observed that EEP had a superior 6-month PVR (only two studies involved), but this conclusion needs to be confirmed in high-quality randomized controlled trials (RCTs) with longer follow-up.
In this meta-analysis, we found that EEP might have superior perioperative outcomes. Compared with the MISP group, the EEP group had a shorter operation time, less Hb decrease, shorter catheterization time, lower LOS, and comparable resection weight. Our results are consistent with the existing evidence comparing the two surgical methods (12, 15, 19). Interestingly, subgroup analysis revealed that when the two minimally invasive techniques were separately compared with endoscopic surgery, the operative time was higher for LSP (p = 0.009) and comparable for RASP (p = 0.08). Nevertheless, there was significant heterogeneity in these studies. Baldini et al. (13) and Fuschi et al. (17) reported that there was no difference in operative time between LSP and endoscopic procedure. In contrast, Gunseren et al. (18) observed that LSP was associated with higher operative time. They claimed that closing bladder incisions could lead to a partial increase in operative time, even in the hands of surgeons with laparoscopic experience. Further correlation line demonstrated that the operative time advantage of holmium laser enucleation of the prostate (HoLEP) might disappear in huge prostates. For comparison of RASP and endoscopic procedure, Zhang et al. (15) found that RASP had a higher operative time, while a prospective randomized study by Fuschi et al. (17) showed no difference in operative time between the two procedures. On the side, Fuschi et al. (17) also reported that RASP had comparable operative time to LSP.
The technical proficiency of the surgeon appears to be a factor affecting the duration of operation (8). Johnson et al. (21) found that the median operative time of RASP improved significantly as surgeons became more skilled (early cohort 160 mins vs. late cohort 134 mins). In addition, they also claimed that a physician with experience with robotic radical prostatectomy might need only 10–12 cases to become proficient with RASP. Nevertheless, surgeries that involve EEP, such as the HoLEP technique, still have a steep learning curve for even experienced surgeons (22). Brunckhorst et al. (23) reported that HoLEP required 40–60 cases to achieve a proficient efficiency platform. In consequence, the “learning curve” factor might be more favorable to RASP rather than HoLEP, but it still needs to be validated in high-quality, multicenter RCTs.
We found that the EEP had a lower Hb decrease compared to MISP. In fact, both procedures rely on direct application of energy to achieve intraoperative hemostasis, but the endoscopic method can control the bleeding rapidly during the enucleation and thus has a better hemostasis effect (15). In most cases, fewer bleeding may be associated with surgical parameters such as shorter catheterization time and lower LOS, so the EEP group might have shorter catheterization time and LOS (24). However, there were significant differences in the results of different studies. Lusuardi et al. (12) reported a lower Hb decrease in endoscopic surgery, whereas Umari et al. (14) and Lombardo et al. (19) did not observe such a significant difference. In addition, higher hemoglobin reduction did not translate into higher blood transfusions. We observed similar blood transfusions between the groups (7.4 vs. 3.1%, p = 0.24). Interestingly, the RASP subgroup had a higher rate of transfusion (P = 0.004). However, the transfusion rate may not be a good indicator for evaluating the outcome of minimally invasive surgery as they vary from among hospitals, according to patient comorbidities and surgeon preferences (25).
The present study also expanded the pooled evidence to show that the MISP group had comparable overall complications (p = 0.62) compared to the EEP group. Our subgroup analysis also indicated that there was no difference in overall complications between minimally invasive techniques (LSP and RASP) and endoscopic procedures. These results are consistent with the available evidence. In most studies, the incidence of related complications was low and appeared to be evenly distributed in the MISP and EEP groups. Overall, both MISP and EEP are safe surgical procedures for the treatment of large BPH, and no clear conclusions can be drawn in favor of endoscopic therapy.
Another major constraint on the widespread use of surgical techniques is cost. Juaneda et al. (26) observed an average savings of €1835 for HoLEP compared to LSP (€2871 vs. €4706), and proposed that the reduced cost of the HoLEP was associated with shorter LOS. Unfortunately, no studies have reported a cost comparison between RASP and HoLEP, but in the comparison between RASP and OSP, Matei et al. (27) found that the average cost of RASP was €3940. Besides, Sotelo et al. (28) noted that the mean cost of the RASP was $1627 more expensive than LSP. These results suggest that endoscopic procedures appear to be cheaper than MISP. However, cost-benefit analysis is extremely complex and is influenced by many factors, such as hospital costs, complications, and reimbursement issues, which vary widely between countries and healthcare systems (25). Therefore, carefully designed studies are needed before definitive conclusions can be drawn.
Compared with the study of Abi Chebel et al. (20), the present meta-analysis has the advantage of including three recent comparative trials and then analyzing more parameters related to the effectiveness and safety of these two methods. In addition, the previous study only provided 3-month IPSS data, whereas our study expanded the sample size and further evaluated functional outcomes at 6-month. Another strength of the current study was our subgroup analyses, which for the first time systematically compared RASP with EEP outcomes.
Limitations should be noted before interpreting our findings. First, this study was unable to analyze the learning curves and costs of the two processes because of the lack of data. Second, significant heterogeneity was observed in perioperative outcomes and complications, which may limit the strength of our evidence. For this, we conducted a subgroup analysis of each outcome indicator based on the minimally invasive approach, hoping that this has increased some robustness to our analysis and interpretation. Third, the follow-up time was mostly less than 6 months. Therefore, our results can only compare the short-term efficacy and safety of MISP and EEP. Finally, due to the inconsistent follow-up time in this study, there may be deviations in the reports of complications.
Conclusion
The current study suggested that the short-term efficacy and safety were comparable between MISP and EEP procedures for large prostates. However, EEP may have a more favorable perioperative profile with shortened operative time, reduced Hb decrease, shortened reduced catheterization time, and reduced LOS. Based on these results, both surgical procedures could be offered to patients, which should understand the advantages and disadvantages of each method to make a suitable decision.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the Corresponding Author/s.
Author Contributions
QW is responsible for manuscript conceptualization. JL, DC, and CM are responsible for manuscript writing and data analysis. LP and ZX are responsible for data analysis. YL and QW are responsible for manuscript editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (Grant Number 82000721), Post-Doctor Research Project, West China Hospital, Sichuan University (Grant Number 2019HXBH089), Health commission of Sichuan province (Grant Number 20PJ036), and Sichuan Province Science and Technology Planning Project (Grant Number 2020YJ0054 and 2020YFS0320).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Ms. Mengqi Chen for providing continuous encouragement to JL to pursue his career in medicine.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.773257/full#supplementary-material
References
1. Xu XF, Liu GX, Guo YS, Zhu HY, He DL, Qiao XM, et al. Global, regional, and national incidence and year lived with disability for benign prostatic hyperplasia from 1990 to 2019. Am J Mens Health. (2021) 15:15579883211036786. doi: 10.1177/15579883211036786
2. Lokeshwar SD, Harper BT, Webb E, Jordan A, Dykes TA, Neal DE, et al. Epidemiology and treatment modalities for the management of benign prostatic hyperplasia. Transl Androl Urol. (2019) 8:529–39. doi: 10.21037/tau.2019.10.01
3. Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. (2015) 67:1099–109. doi: 10.1016/j.eururo.2014.12.038
4. Lerner LB, McVary KT, Barry MJ, Bixler B, Dahm P, Das AK, et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline part II-surgical evaluation and treatment. J Urol. (2021) 206:806–17. doi: 10.1097/JU.0000000000002183
5. Pariser JJ, Pearce SM, Patel SG, Bales GT. National trends of simple prostatectomy for benign prostatic hyperplasia with an analysis of risk factors for adverse perioperative outcomes. Urology. (2015) 86:721–5. doi: 10.1016/j.urology.2015.06.048
6. Bhanvadia R, Ashbrook C, Gahan J, Mauck R, Bagrodia A, Margulis V, et al. Perioperative outcomes and cost of robotic vs open simple prostatectomy in the modern robotic era: results from the National Inpatient Sample. BJU Int. (2021) 128:168–77. doi: 10.1111/bju.15258
7. Lin Y, Wu X, Xu A, Ren R, Zhou X, Wen Y, et al. Transurethral enucleation of the prostate versus transvesical open prostatectomy for large benign prostatic hyperplasia: a systematic review and meta-analysis of randomized controlled trials. World J Urol. (2016) 34:1207–19. doi: 10.1007/s00345-015-1735-9
8. Li J, Cao D, Peng L, Ren Z, Gou H, Li Y, et al. Comparison between minimally invasive simple prostatectomy and open simple prostatectomy for large prostates: a systematic review and meta-analysis of comparative trials. J Endourol. (2019) 33:767–76. doi: 10.1089/end.2019.0306
9. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71.
10. Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. (2018) 27:1785–805. doi: 10.1177/0962280216669183
11. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
12. Lusuardi L, Hruby S, Janetschek G, Mitterberger M, Sieberer M, Colleselli D, et al. Laparoscopic adenomectomy versus Eraser laser enucleation of the prostate. World J Urol. (2015) 33:691–6. doi: 10.1007/s00345-014-1476-1
13. Baldini A, Fassi-Fehri H, Duarte RC, Crouzet S, Ecochard R, Abid N, et al. Holmium laser enucleation of the prostate versus laparoscopic transcapsular prostatectomy: perioperative results and three-month follow-up. Curr Urol. (2017) 10:81–6. doi: 10.1159/000447156
14. Umari P, Fossati N, Gandaglia G, Pokorny M, De Groote R, Geurts N, et al. Robotic assisted simple prostatectomy versus holmium laser enucleation of the prostate for lower urinary tract symptoms in patients with large volume prostate: a comparative analysis from a high volume center. J Urol. (2017) 197:1108–14. doi: 10.1016/j.juro.2016.08.114
15. Zhang MW, El Tayeb MM, Borofsky MS, Dauw CA, Wagner KR, Lowry PS, et al. Comparison of perioperative outcomes between holmium laser enucleation of the prostate and robot-assisted simple prostatectomy. J Endourol. (2017) 31:847–50. doi: 10.1089/end.2017.0095
16. Nestler S, Bach T, Herrmann T, Jutzi S, Roos FC, Hampel C, et al. Surgical treatment of large volume prostates: a matched pair analysis comparing the open, endoscopic (ThuVEP) and robotic approach. World J Urol. (2019) 37:1927–31. doi: 10.1007/s00345-018-2585-z
17. Fuschi A, Al Salhi Y, Velotti G, Capone L, Martoccia A, Suraci PP, et al. Holmium laser enucleation of prostate versus minimally invasive simple prostatectomy for large volume (≥ 120 ml) prostate glands: a prospective multicenter randomized study. Minerva Urol Nefrol. (2020). doi: 10.23736/S0393-2249.20.04043-6. [Epub ahead of print].
18. Gunseren KO, Akdemir S, Çiçek MC, Yildiz A, Arslan M, Yavaşcaoglu I, et al. Holmium laser enucleation, laparoscopic simple prostatectomy, or open prostatectomy: the role of the prostate volume in terms of operation time. Urol Int. (2021) 105:285–90. doi: 10.1159/000511637
19. Lombardo R, Zarraonandia Andraca A, Plaza Alonso C, González-Dacal JA, Rodríguez Núñez H, Barreiro Mallo A, et al. Laparoscopic simple prostatectomy vs bipolar plasma enucleation of the prostate in large benign prostatic hyperplasia: a two-center 3-year comparison. World J Urol. (2021) 39:2613–9. doi: 10.1007/s00345-020-03512-5
20. Abi Chebel J, Sarkis J, El Helou E, Hanna E, Abi Tayeh G, Semaan A. Minimally invasive simple prostatectomy in the era of laser enucleation for high-volume prostates: a systematic review and meta-analysis. Arab J Urol. (2020) 19:123–9. doi: 10.1080/2090598X.2020.1789809
21. Johnson B, Sorokin I, Singla N, Roehrborn C, Gahan JC. Determining the learning curve for robot-assisted simple prostatectomy in surgeons familiar with robotic surgery. J Endourol. (2018) 32:865–70. doi: 10.1089/end.2018.0377
22. Robert G, Cornu JN, Fourmarier M, Saussine C, Descazeaud A, Azzouzi AR, et al. Multicentre prospective evaluation of the learning curve of holmium laser enucleation of the prostate (HoLEP). BJU Int. (2016) 117:495–9. doi: 10.1111/bju.13124
23. Brunckhorst O, Ahmed K, Nehikhare O, Marra G, Challacombe B, Popert R. Evaluation of the learning curve for holmium laser enucleation of the prostate using multiple outcome measures. Urology. (2015) 86:824–9. doi: 10.1016/j.urology.2015.07.021
24. Gu C, Zhou N, Gurung P, Kou Y, Luo Y, Wang Y, et al. Lasers versus bipolar technology in the transurethral treatment of benign prostatic enlargement: a systematic review and meta-analysis of comparative studies. World J Urol. (2020) 38:907–18. doi: 10.1007/s00345-019-02852-1
25. Kordan Y, Canda AE, Köseoglu E, Balbay D, Laguna MP, de la Rosette J. Robotic-assisted simple prostatectomy: a systematic review. J Clin Med. (2020) 9:1798. doi: 10.3390/jcm9061798
26. Juaneda R, Thanigasalam R, Rizk J, Perrot E, Theveniaud PE, Baumert H. Holmium laser enucleation versus laparoscopic simple prostatectomy for large adenomas. Actas Urol Esp. (2016) 40:43–8. doi: 10.1016/j.acuroe.2015.11.007
27. Matei DV, Brescia A, Mazzoleni F, Spinelli M, Musi G, Melegari S, et al. Robot-assisted simple prostatectomy (RASP): does it make sense? BJU Int. (2012) 110:E972–9. doi: 10.1111/j.1464-410X.2012.11192.x
Keywords: minimally invasive simple prostatectomy, endoscopic enucleation, benign prostatic hyperplasia, outcomes, meta-analysis
Citation: Li J, Cao D, Meng C, Xia Z, Peng L, Li Y and Wei Q (2021) Comparison of the Efficacy and Safety of Minimally Invasive Simple Prostatectomy and Endoscopic Enucleation of Prostate for Large Benign Prostatic Hyperplasia. Front. Med. 8:773257. doi: 10.3389/fmed.2021.773257
Received: 09 September 2021; Accepted: 13 October 2021;
Published: 05 November 2021.
Edited by:
Xiulin Zhang, Second Hospital of Shandong University, ChinaReviewed by:
Meng Gu, Shanghai Ninth People's Hospital, ChinaCristoforo Pomara, University of Catania, Italy
Copyright © 2021 Li, Cao, Meng, Xia, Peng, Li and Wei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yunxiang Li, bGl5dW54aWFuZzM2OUAxMjYuY29t; Qiang Wei, d2VpcWlhbmczMzlAMTI2LmNvbQ==
†These authors have contributed equally to this work
 Jinze Li
Jinze Li Dehong Cao
Dehong Cao Chunyang Meng
Chunyang Meng Zhongyou Xia3,4
Zhongyou Xia3,4 Yunxiang Li
Yunxiang Li Qiang Wei
Qiang Wei