- 1Department of Surgery, Narita-Tomisato Tokushukai Hospital, Chiba, Japan
- 2Department of Cardiovascular Medicine, Narita-Tomisato Tokushukai Hospital, Chiba, Japan
- 3Department of Bacteriology, Nagoya University Graduate School of Medicine, Aichi, Japan
- 4Department of Radiology, Asahi General Hospital, Asahi, Japan
Emphysematous prostatic abscess (EPA) is an extremely rare but potentially fatal urinary tract infection (UTI). Here, we describe a case (a 69-year-old male with prediabetes) of ruptured EPA caused by a hypervirulent Klebsiella pneumoniae (hvKp) K1-ST23 strain, presenting as motor aphasia. Our patient presented with ruptured EPA concurrent with various severe systemic pyogenic complications (e.g., urethro-prostatic fistula, ascending UTIs, epididymal and scrotal abscesses, and liver, lung, and brain abscesses). Whole-body computed tomography (CT) and next-generation sequencing (NGS) were useful for the detection of ruptured EPA and its systemic complications, and for identification of K1-ST23 hvKp strains, respectively. Subsequently, the infections were successfully treated with aggressive antimicrobial therapy and multiple surgical procedures. This case highlights the significance of awareness of this rare entity, the clinical importance of CT for the early diagnosis of EPA and the detection of its systemic complications in view of hvKp being an important causative organism of severe community-acquired UTI, and the usefulness of NGS to identify hvKp strains.
Introduction
Prostatic abscess is an uncommon sequela of urinary tract infection (UTI). In the post-antimicrobial era, the incidence is low at approximately 0.5% (1). Among them, emphysematous prostatic abscess (EPA), characterized by gas accumulation and abscess formation within the prostate gland, is an extremely rare but life-threatening condition if left untreated (2). However, an accurate diagnosis remains challenging because of the non-specific symptoms and signs.
Case Description
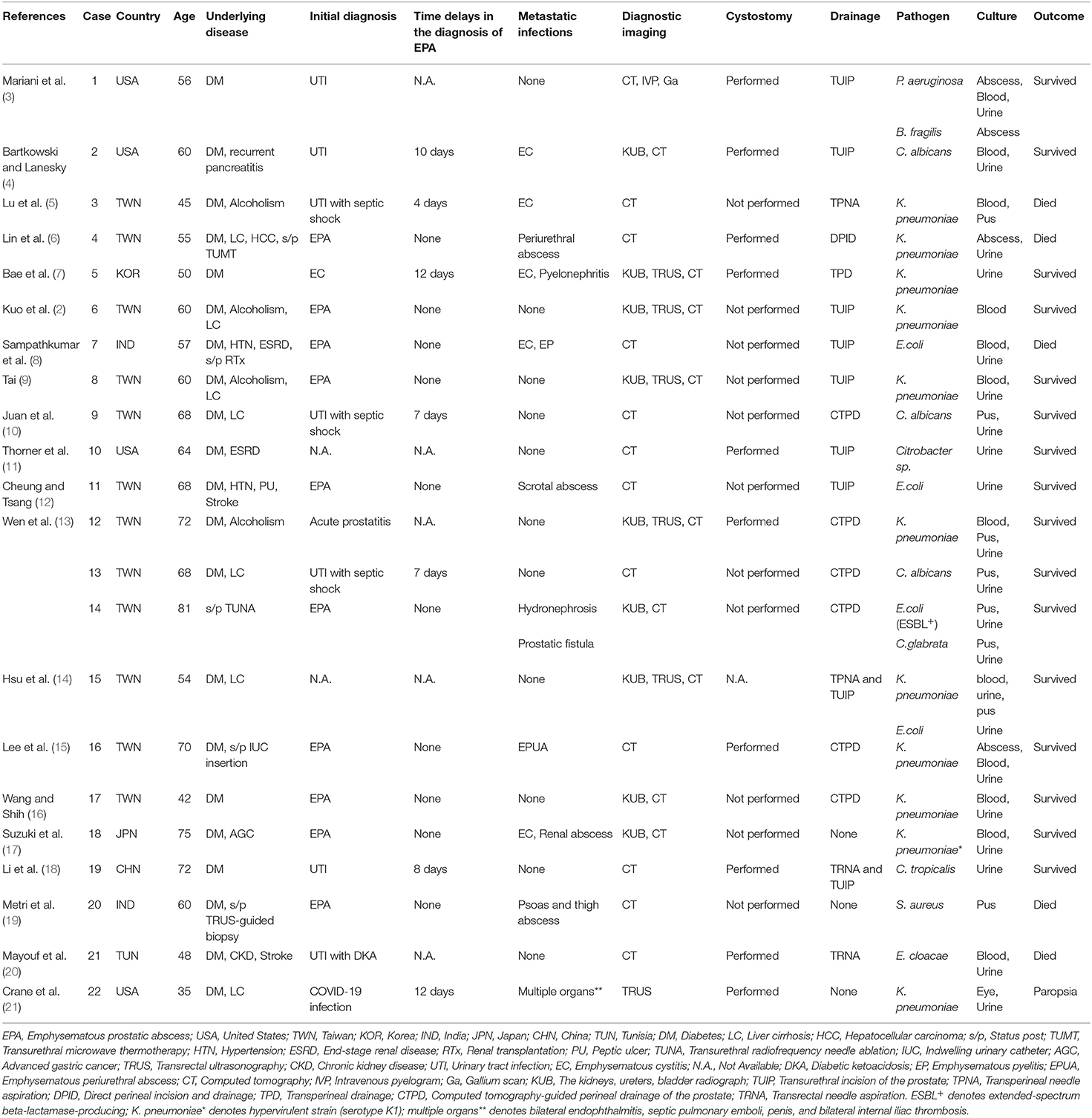
A 69-year-old Japanese man was admitted to our hospital with a 7-day history of slurred speech. He had no past history of prostatic manipulation. On admission, the patient had a low-grade fever of 37.8°C, tachycardia of 109 beats/min, blood pressure of 122/90 mmHg, and oxygen saturation of 97% on ambient air. Motor aphasia was recognized on neurologic examination. Digital rectal examination revealed a soft and non-tender enlarged prostate. Laboratory testing revealed neutrophilic leukocytosis, elevated levels of C-reactive protein (20.86 mg/dL; reference: <0.15 mg/dL), fasting blood glucose (135 mg/dL; reference: <110 mg/dL), and HbA1c (6.3%; reference: <6.0%). Mild hepatorenal dysfunction was also observed. Urinalysis was positive for bacteriuria and pyuria. Cerebrospinal fluid analysis was unremarkable. Brain computed tomography (CT) and magnetic resonance imaging (MRI) revealed a lesion in the left lenticular nucleus, suggestive of a brain abscess (Figures 1A,B). We subsequently searched for the cause of the brain abscess on a whole-body CT. Pelvic CT revealed an enlarged multilobular prostate gland characterized by capsulized fluid cavities and multiple gas bubbles, suggesting EPA caused by anaerobic bacteria (Figures 2A,B). We also recognized severe pyogenic complications of EPA, which were different from Fournier's gangrene. We classified a wide spectrum of complications into four predominant categories according to the route of spread of infection. We found direct extension as the 1st route, which involved spread into the left seminal vesicle and extraperitoneal space of the ischioanal fossa (Figures 2A,B), and an ascending infection of the ipsilateral urinary tract as the 2nd route, which caused left hydronephrosis, acute focal bacterial nephritis, and thrombophlebitis of the adjacent left iliac vein (Figures 2C,D). We also found a retrograde infection of the ipsilateral spermatic duct as the 3rd route, which led to an epididymal abscess (Figure 2A), and hematogenous spread to the liver (Figure 2E) and lungs (Figure 2F) as the 4th route. Pelvic MRI further characterized the pelvic infection and revealed active prostatic inflammation involving the urinary bladder and left seminal vesicles, which ruptured into the extraperitoneal perivesicular space, and subsequent fistula formation of the bulbar urethra with the prostate (Figure 3). Based on these findings, we concluded that brain abscess was highly likely due to hematogenous seeding of the primary prostate infection. We started to treat the pelvic infection with the insertion of a transurethral Foley catheter and commencement of empiric antimicrobial therapy (meropenem, 4 g/day IV).
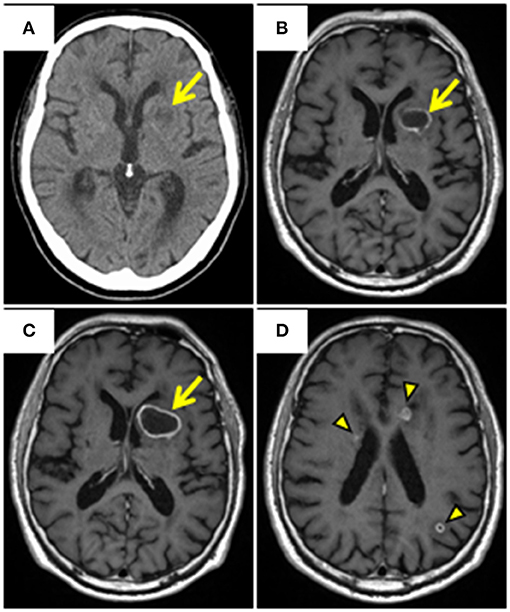
Figure 1. Brain CT and MRI. (A) Axial plain CT reveals a round low-attenuation area with slightly high-attenuation rim in the left lenticular nucleus (arrow). (B) Axial gadolinium-enhanced T1-weighted MRI reveals ring enhancement in the area (arrow). (C, D) MRI following the initial treatment reveals enlargement of the existing abscess (arrow), and new ring enhancement (arrowheads) in the bilateral periventricular and subcortical areas. CT, Computed tomography; MRI, Magnetic resonance imaging.
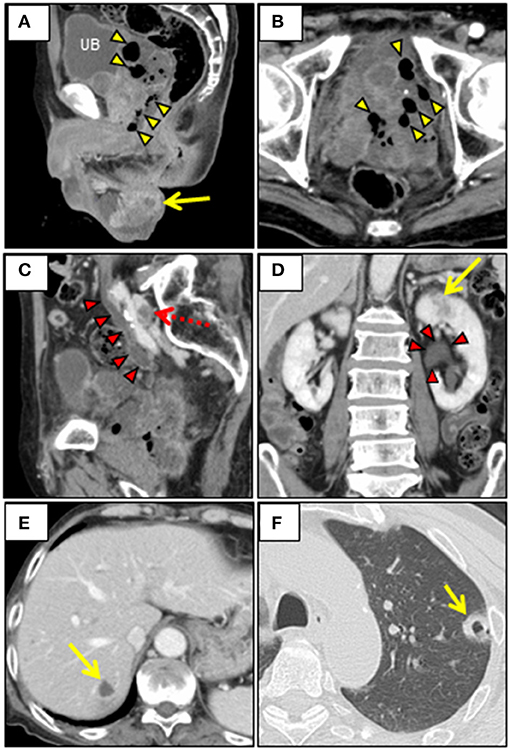
Figure 2. Contrast-enhanced whole-body CT. (A, B) Pelvic CT reveals the irregularly-shaped enlarged prostate and the left seminal vesicle, which are replaced by encapsulated fluid cavities containing multiple gas bubbles (arrowheads), with spread of infection into extraperitoneal perivesicular space in the small pelvis. Note the left epididymal abscess (arrow). (C, D) Abdominal/pelvic CT shows marked dilatation of the left ureteral and renal pelvis (arrowheads), and multiple hypoenhancement foci in the left renal parenchyma (arrow). Note the thrombus in the left common iliac vein parallel to the dilated ureter (dotted arrow). (E) Abdominal CT reveals a centrally hypoattenuating lesion with peripheral heterogeneous enhancement in liver S7 (arrow). (F) Chest CT (lung window) reveals peripheral thick-walled cavitary nodule in the left upper lobe (arrow). CT, Computed tomography; UB, Urinary bladder.
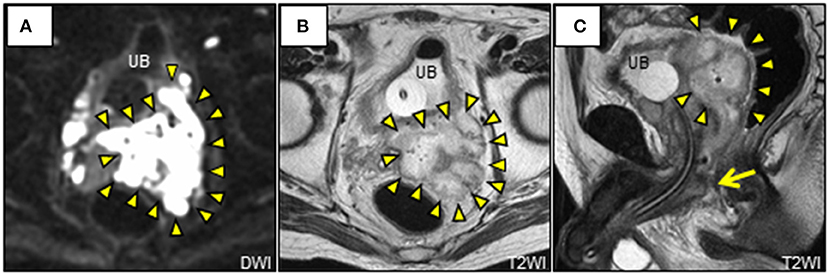
Figure 3. Pelvic magnetic resonance imaging. (A) Axial DWI shows characteristic restricted diffusion on the left lobe of the prostate extending to the opposite lobe and bilateral perivesicular extraperitoneal spaces (arrowheads). (B, C) Axial and sagittal T2WI shows obviously multilocular abscess of both prostate and left seminal vesicle (arrowheads), with a fistulous communication of the bulbar urethra (arrow). DWI, diffusion-weighted image; T2WI, T2-weighted image; UB, urinary bladder.
On day 5, all the urine culture and two sets of blood cultures collected on admission yielded Klebsiella pneumoniae, which was susceptible to conventional antimicrobials, yet naturally resistant to ampicillin. Although the K. pneumoniae isolate was negative for the string test, we performed next-generation sequencing (NGS) for capsular genotyping, virulence factors, and multilocus sequencing typing (MLST). The isolate was found to belong to a sequence type (ST) 23 serotype K1 strain harboring virulence-associated genes, including kfuA (an iron uptake system), magA (specific to K1 capsule serotype), rmpA (regulator of mucoid phenotype), ybtS (yersiniabactin gene), iroN (gene for the outer membrane receptor, FepA, of Fe3+-bound salmochelin), and mrkD (type 3 fimbrial adhesin gene). Based on the antimicrobial susceptibility test results, antimicrobial de-escalation was performed (ciprofloxacin, 1,200 mg/day IV). On day 14, a left scrotal abscess developed progressively, presumably originating from the adjacent epididymal abscess, and required surgical drainage. On day 21, follow-up CT showed a decrease in the size of the EPA, and multiple intrapelvic abscesses, liver abscess, and pulmonary septic emboli.
However, on day 24, we performed an additional brain abscess drainage on a CT-guided stereotactic procedure because follow-up brain MRI confirmed a gradual progression of the existing brain abscess and multiple new ones (Figures 1C,D). Subsequently, the treatment was replaced with a 3-week course of intravenous ceftriaxone (3 g/day) and ciprofloxacin (1,200 mg/day). On follow-up CT/MRI, the brain abscesses gradually reduced in size. The patient continued rehabilitation for disuse syndrome and motor aphasia, and these improved with training. Fasting blood glucose levels after control of infection were in the range of 110–125 mg/dL, suggesting prediabetes. The patient was discharged on day 88. He remained clinically stable at 1-year follow-up. The timeline of the case presentation and clinical course is presented in Supplementary Figure 1.
Discussion
Herein, we describe a rare case of EPA caused by a hypervirulent K. pneumoniae (hvKp) K1-ST23 strain. Within a few days, the patient developed abscess rupture concurrent with various serious systemic pyogenic complications successfully treated with aggressive antimicrobial therapy and multiple surgical interventions. Our case illustrates several valuable clinical pearls.
First, our patient with EPA exhibited abscess rupture, leading to a variety of serious systemic pyogenic complications. We conducted an updated systematic review of case reports to investigate the characteristics and epidemiology of EPA (Table 1). The literature search was performed with English language restriction using electronic databases of PubMed from January 1, 1983, until July 28, 2021. The following search terms were used: “emphysematous prostatic abscess” (Mesh) or “emphysematous prostatic abscess” (tiab) or “emphysematous prostatitis” (Mesh) or “emphysematous prostatitis” (tiab). Consequently, 22 cases were included (2–21). EPA is most often diagnosed in Asia (68%), with an average age of 60 years (range, 35–75 years). The underlying disease was diabetes mellitus (96%), followed by liver cirrhosis (27%), recent urological surgery (23%), and alcoholism (18%). Unlike prostatic abscess, in which Escherichia coli is the main causative organism; the most common causative organism of EPA is K. pneumoniae (50%), followed by Escherichia coli (18%) and Candida albicans (14%). EPA is often misdiagnosed as the usual type of UTI, leading to time delay (range, 4–12 days) in the accurate diagnosis and proper treatment. EPA can have a variable presentation, ranging from asymptomatic to lethal. Frequent complications of EPA include localized spread of infection to adjacent areas, ascending infections, or disseminated hematogenous spread. Although rare, the most feared sequelae include a urethro-prostatic fistula or abscess rupture into the urethra, perineum, bladder, or rectum (13, 22). Metastatic infections are common (55%), with a high mortality rate of 23%. CT is the most useful diagnostic imaging tool. The mainstay of treatment includes adequate antimicrobial therapy and drainage; in 86% of cases, surgical drainage was performed using a transperineal (45%), transurethral (41%), or transrectal (9%) approach. Suprapubic cystostomy is often performed for urinary diversion (45.4%).
The present case presented with systemic complications via all the aforementioned routes of infection. Despite fatal complications (e.g., urethro-prostatic fistula, epididymal and scrotal abscesses, and metastatic hepatic/pulmonary/brain abscesses), CT/MRI screening was useful for early detection, and the infection was successfully controlled by aggressive antimicrobial therapy and multiple surgical drainage procedures.
Second, our case underscores the significance of early diagnosis of invasive K. pneumoniae infections in healthy subjects. The hvKp is a major causative agent in invasive community-acquired infections characterized by pyogenic liver abscess (PLA) with a high mortality, and has been reported in the Asian Pacific Rim, starting in Taiwan since the 1980s, and is now spreading worldwide (23). The hvKp strain has a much more vicious phenotype than the classical K. pneumoniae (cKp) strain due to its high toxicity and metastatic potential, resulting in grave secondary infections such as endophthalmitis, meningitis, and septic pulmonary emboli. Thus, early diagnosis and prompt treatment are required; however, the following three clinical issues for hvKp infection were exemplified by our case.
As the first clinical issue, hvKp-related primary extrahepatic genitourinary infections are increasingly being reported. Although the exact pathogenesis of hvKp remains unknown, many studies have indicated that hvKp initially colonizes the gastrointestinal tract, from where it preferentially infects other organs, mainly the liver. Therefore, UTI caused by hvKp has been considered secondary to hematogenous spread from preceding bacteremia. In fact, there are several reported cases of PLA with hematogenous spread to the kidney, perirenal tissues, and prostate, leading to local abscess formation (23). Conversely, several hvKp cases with community-acquired UTIs without PLA have also been reported (24–26). Similarly, the main source of infection in our case was the prostate gland, and concomitant liver abscess was highly likely secondary to the primary prostatic infection. Thus, our case underscores the importance of considering the possibility of hvKp infection even in patients with community-acquired UTIs.
The second clinical issue concerns the significance of serotype K1 K. pneumoniae in our case. To our knowledge, the present case is the first case of EPA caused by serotype K1 hvKp infection presenting with a brain abscess. The K1 strain has a strong propensity to cause metastatic ocular and neurologic complications. In a single-center, retrospective study of 177 patients with PLA in Taiwan, the incidence of metastatic complications was 13% (27). The frequency of metastatic complications was significantly higher in patients with K1 strains than in patients with non-K1 strains (19 vs. 5%, p = 0.007). Multivariate logistic regression analyses demonstrated that the K1 strain was the sole significant risk factor for metastatic complications (adjusted odds ratio, 4.8; 95% confidence interval, 1.5–15.7, p = 0.009), strongly suggesting that the K1 strains should be recognized as a distinct virulent organism. In addition, such metastatic complications have been reported in patients with K1 strains without hepatic involvement, suggesting that their development is unrelated to the presence of PLA (25, 26). Thus, our case highlights the importance of considering serotype K1 hvKp as a rare causative agent of community-acquired brain abscess and of screening for the primary site of infection.
The third clinical issue is to identify a hvKp strain definitely. Although numerous studies have been conducted to differentiate hvKp strains from cKp strains in terms of epidemiologic and genetic differences, there are still no clear microbiological and molecular diagnostic criteria for hvKp strains. A positive string test, indicating a hypermucoviscous colony phenotype on the agar plate, is widely believed to be a unique characteristic of hvKp strains. However, hypermucoviscosity and hypervirulence do not always coincide, as shown by the fact that there are both string test-negative hvKp strains and string test-positive cKp strains. A study evaluating 140 cases of K. pneumoniae bloodstream infections revealed that the string test alone is not adequate to differentiate hvKp strains from cKp strains (69.2% sensitivity, 89.5% specificity, 60.0% positive predictive value, and 92.7% negative predictive value), supporting this notion (28). The hvKp strains have some capsular types necessary for their virulence, with K1/K2 capsular serotypes being the most prevalent and virulent reported to date. Regarding virulence-associated genes, rmpA is remarkably related to the hvKp strain (29). Type 1 and type 3 fimbriae are deeply involved in bacterial resistance to phagocytosis, adhesion to biological/non-biological surfaces, and altered antibiotic permeability. Iron is a metal necessary for bacterial growth and plays an important role in infection spread, and siderophores (aerobactin, enterobactin, salmochelin, and yersiniabactin), secreted by K. pneumoniae, have the ability to sequester iron, contributing to their high virulence. However, while all the factors described above play important roles in the process of increased virulence, no single causal risk factor alone is the sole determinant of hypervirulence. Recently, a new genotype/phenotype approach for the comprehensive detection of a specific set of biomarkers has been proposed for the successful identification of hvKp strains (30). Further investigation is expected to accumulate in the future. In our case, NGS was useful for identifying the hvKp strain because it allows simultaneous analysis of MLST and virulence-associated genes, belongs to a K1-ST23 hvKp strain, and has the same profile of virulence-associated genes as the K1-ST23 hvKp strains previously identified in Japan, suggesting high genetic similarity (31). In our case review, only one case of EPA caused by the serotype K1 hvKp strain has been reported (Table 1). Given the high incidence of K. pneumoniae pathogens in EPA patients and the highly invasive nature of EPA, a thorough investigation of these strains is warranted.
Untreated glucose intolerance might have contributed to the virulent phenotype observed in our case, since hyperglycemia impairs neutrophil phagocytosis of K1/K2 capsular serotypes (32).
Conclusions
Herein, we report a case of ruptured EPA secondary to K1-ST23 hvKp infection with serious systemic pyogenic complications that was successfully treated with aggressive antimicrobial therapy and multiple surgical procedures. CT is useful for the accurate diagnosis and early detection of complications. EPA is an extremely rare, yet potentially fatal sequela of UTI, which can be curable if treated properly at an early stage. Therefore, clinicians should recognize this rare clinical entity and perform systemic CT screening in patients with potentially severe UTI. In addition, our case highlights the clinical importance of keeping in mind hvKp infections as a possible cause of community-acquired UTI in immunocompromised individuals including prediabetes, and of NGS to identify hvKp strains for appropriate treatment.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
HY was responsible for the clinical study design and conceptualization of the study. KK, TS, HM, HY, and HO were involved in the acquisition of clinical data. YT, JI, and YA analyzed and interpreted the data. HY, JI, and YA wrote the manuscript. All authors contributed to the article and approved the submitted version.
Funding
Next-generation sequencing experiments were funded by the Nagoya University Graduate School of Medicine, under Grant [Japan Agency for Medical Research and Development (AMED)/16fk0108307h0402]. Other parts of this study were not funded by any institution.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.768042/full#supplementary-material
Abbreviations
UTI, urinary tract infection; EPA, emphysematous prostatic abscess; CT, computed tomography; MRI, magnetic resonance imaging; NGS, next-generation sequencing; MLST, multilocus sequencing typing; ST, sequence type; kfuA, an iron uptake system; magA, specific to K1 capsule serotype; rmpA, regulator of mucoid phenotype; ybtS, Yersiniabactin gene; iroN, Gene for the outer membrane receptor; FepA, of Fe3+-bound salmochelin; mrkD, type 3 fimbrial adhesin gene; hvKp, Hypervirulent K. pneumoniae; PLA, Pyogenic liver abscesses; cKp, Classical K. pneumoniae.
References
1. Ackerman AL, Parameshwar PS, Anger JT. Diagnosis and treatment of patients with prostatic abscess in the post-antibiotic era. Int J Urol. (2018) 25:103–10. doi: 10.1111/iju.13451
2. Kuo PH, Huang KH, Lee CW, Lee WJ, Chen SJ, Liu KL. Emphysematous prostatitis caused by Klebsiella pneumoniae. J Formos Med Assoc. (2007) 106:74–7. doi: 10.1016/S0929-6646(09)60219-9
3. Mariani AJ, Jacobs LD, Clapp PR, Hariharan A, Stams UK, Hodges CV. Emphysematous prostatic abscess: diagnosis and treatment. J Urol. (1983) 129:385–6. doi: 10.1016/S0022-5347(17)52112-6
4. Bartkowski DP, Lanesky JR. Emphysematous prostatitis and cystitis secondary to Candida albicans. J Urol. (1988) 139:1063–5. doi: 10.1016/S0022-5347(17)42774-1
5. Lu DC, Lei MH, Chang SC. Emphysematous prostatic abscess due to Klebsiella pneumoniae. Diagn Microbiol Infect Dis. (1998) 31:559–61. doi: 10.1016/S0732-8893(98)00032-7
6. Lin DC, Lin YM, Tong YC. Emphysematous prostatic abscess after transurethral microwave thermotherapy. J Urol. (2001) 166:625. doi: 10.1097/00005392-200108000-00059
7. Bae GB, Kim SW, Shin BC, Oh JT, Do BH, Park JH, et al. Emphysematous prostatic abscess due to Klebsiella pneumoniae: report of a case and review of the literature. J Korean Med Sci. (2003) 18:758–60. doi: 10.3346/jkms.2003.18.5.758
8. Sampathkumar K, Murali TR, Sooraj YS, Mahaldar AR. Emphysematous prostatitis in renal transplant. Indian J Urol. (2007) 23:476–8. doi: 10.4103/0970-1591.36728
9. Tai HC. Emphysematous prostatic abscess: a case report and review of literature. J Infect. (2007) 54:e51–4. doi: 10.1016/j.jinf.2006.03.033
10. Juan YS, Huang CH, Chang K, Wang CJ, Chuang SM, Shen JT, et al. Emphysematous prostatic abscess due to candidiasis: a case report. Kaohsiung J Med Sci. (2008) 24:99–102. doi: 10.1016/S1607-551X(08)70104-9
11. Thorner DA, Sfakianos JP, Cabrera F, Lang EK, Colon I. Emphysematous prostatitis in a diabetic patient. J Urol. (2010) 183:2025. doi: 10.1016/j.juro.2010.01.084
12. Cheung WK, Tsang YM. Emphysematous infections of the prostate and scrotum in an older adult in a nursing home. J Am Geriatr Soc. (2011) 59:2378–9. doi: 10.1111/j.1532-5415.2011.03710.x
13. Wen SC, Juan YS, Wang CJ, Chang Ko, Shih MCP, Shen JT, et al. Emphysematous prostatic abscess: case series study and review. Int J Infect Dis. (2012) 16:e344–9. doi: 10.1016/j.ijid.2012.01.002
14. Hsu LN, Chiang PH, Kang CH. Emphysematous prostatic abscess: rare case and systematic review. J Formos Med Assoc. (2015) 114:292–3. doi: 10.1016/j.jfma.2013.07.002
15. Lee CY, Tsai HC, Lee SSJ, Chen YS. Concomitant emphysematous prostatic and periurethral abscesses due to Klebsiella pneumoniae: a case report and review of the literature. Southeast Asian J Trop Med Public Health. (2014) 45:1099–106.
16. Wang HS, Shih MC. Images in clinical medicine. Emphysematous prostatitis. N Engl J Med. (2016) 375:879. doi: 10.1056/NEJMicm1507124
17. Suzuki K, Yamaguchi T, Yanai M. Simultaneous occurrence of hypermucoviscous Klebsiella pneumoniae emphysematous prostatic abscess, emphysematous cystitis, and renal abscess. ID Cases. (2018) 14:e00464. doi: 10.1016/j.idcr.2018.e00464
18. Li Z, Wen J, Zhang N. Emphysematous prostatic abscess due to candidiasis: a case report and review of the literature. Medicine. (2020) 99:e19391. doi: 10.1097/MD.0000000000019391
19. Metri M, Kalra S, Narayanan DL, Ramanitharan M, Ks S. Emphysematous prostatitis with secondary psoas abscess-a lethal outcome following prostate biopsy. Urology. (2020) 142:e45–6. doi: 10.1016/j.urology.2020.04.085
20. Mayouf S, Fourati M, Bchir S, Kammoun O, Mseddi MA, Slimen MH. Emphysematous prostatitis: a case report. Urol Case Rep. (2020) 34:101459. doi: 10.1016/j.eucr.2020.101459
21. Crane AB, Diaz MCA, Jiang Y, Pergament KM. Rare case of endogenous Klebsiella endophthalmitis associated with emphysematous prostatitis in a patient with diabetes, cirrhosis and COVID-19. BMJ Case Rep. (2021) 14:e240425. doi: 10.1136/bcr-2020-240425
22. Garg PK, Hadke NS. Prostato-ano-cutaneous fistula: unusual complication of prostatic abscess. ANZ J Surg. (2008) 78:1032–3. doi: 10.1111/j.1445-2197.2008.04727.x
23. Russo TA, Marr CM. Hypervirulent Klebsiella pneumoniae. Clin Microbiol Rev. (2019) 32:e00001–19. doi: 10.1128/CMR.00001-19
24. Suzuki K, Nakamura A, Enokiya T, Iwashita Y, Tomatsu E, Muraki Y, et al. Septic arthritis subsequent to urosepsis caused by hypermucoviscous Klebsiella pneumoniae. Intern Med. (2013) 52:1641–5. doi: 10.2169/internalmedicine.52.0175
25. Dubey D, Raza FS, Sawhney A, Pandey A. Klebsiella pneumoniae renal abscess syndrome: a rare case with metastatic involvement of lungs, eye, and Brain. Case Rep Infect Dis. (2013) 2013:685346. doi: 10.1155/2013/685346
26. Hyun JI, Kim YJ, Jeon YH, Kim SI, Park YJ, Kang MW, et al. A case of ventriculitis associated with renal abscess caused by serotype K1 Klebsiella pneumoniae. Infect Chemother. (2014) 46:120–4. doi: 10.3947/ic.2014.46.2.120
27. Fang CT, Lai SY, Yi WC, Hsueh PR, Liu KL, Chang SC. Klebsiella pneumoniae genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess. Clin Infect Dis. (2007) 45:284–93. doi: 10.1086/519262
28. Harada S, Aoki K, Yamamoto S, Ishii Y, Sekiya N, Kurai H, et al. Clinical and molecular characteristics of klebsiella pneumoniae isolates causing bloodstream infections in Japan: occurrence of hypervirulent infections in health care. J Clin Microbiol. (2019) 57:e01206–19. doi: 10.1128/JCM.01206-19
29. Yu WL, Ko WC, Cheng KC, Lee HC, Ke DS, Lee CC, et al. Association between rmpA and magA genes and clinical syndromes caused by Klebsiella pneumoniae in Taiwan. Clin Infect Dis. (2006) 42:1351–8. doi: 10.1086/503420
30. Russo TA, Olson R, Fang CT, Stoesser N, Miller M, MacDonald U, et al. Identification of biomarkers for differentiation of hypervirulent Klebsiella pneumoniae from Classical K. pneumoniae. J Clin Microbiol. (2018) 56:e00776–18. doi: 10.1128/JCM.00776-18
31. Harada S, Ishii Y, Saga T, Aoki K, Tateda K. Molecular epidemiology of Klebsiella pneumoniae K1 and K2 isolates in Japan. Diagn Microbiol Infect Dis. (2018) 91:354–9. doi: 10.1016/j.diagmicrobio.2018.03.010
Keywords: Klebsiella pneumoniae, hypervirulent, EPA, brain abscess, K1-ST23, NGS
Citation: Konagaya K, Yamamoto H, Suda T, Tsuda Y, Isogai J, Murayama H, Arakawa Y and Ogino H (2022) Ruptured Emphysematous Prostatic Abscess Caused by K1-ST23 Hypervirulent Klebsiella pneumoniae Presenting as Brain Abscesses: A Case Report and Literature Review. Front. Med. 8:768042. doi: 10.3389/fmed.2021.768042
Received: 31 August 2021; Accepted: 06 December 2021;
Published: 03 January 2022.
Edited by:
Kai Zhou, First Affiliated Hospital of Southern University of Science and Technology, ChinaCopyright © 2022 Konagaya, Yamamoto, Suda, Tsuda, Isogai, Murayama, Arakawa and Ogino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hiroyuki Yamamoto, aHlhbWFtb3RvMTk3MDA5MDhAZ21haWwuY29t
†Present address: Yoshichika Arakawa, Department of Medical Technology, Faculty of Medical Sciences, Shubun University, Aichi, Japan
 Kensuke Konagaya1
Kensuke Konagaya1 Hiroyuki Yamamoto
Hiroyuki Yamamoto Yusuke Tsuda
Yusuke Tsuda