- 1School of Medicine, Illawarra Health and Medical Research Institute, University of Wollongong, Wollongong, NSW, Australia
- 2Monash Centre for Scholarship in Health Education, Monash University, Clayton, VIC, Australia
Competency framework development in health professions has downstream implications for all relevant stakeholders, from the professionals themselves, to organisations, and most importantly end users of services. However, there is little guidance related to what stakeholders might be involved in the competency development process, and when. This review aimed to systematically review literature related to competency framework development methodology in health, to identify the breadth and purpose of key stakeholders commonly involved in the process. Studies were identified using five electronic databases (MEDLINE, PubMed, CINAHL, EMBASE, and ERIC) and a search of websites of organisations involved in curriculum or regulation using keywords related to competency frameworks. The total yield from all databases was 10,625 results, with 73 articles included in the final review. Most articles were from Australia (30%) and were conducted in the nursing (34%) profession. Unsurprisingly, practitioners (86%) and academics (75%) were typically engaged as stakeholders in competency framework development. While many competency frameworks were described as patient-focused, only 14 (19%) studies elected to include service users as stakeholders. Similarly, despite the multi-disciplinary focus described in some frameworks, only nine (12%) studies involved practitioners from other professions. Limiting the conceptualisation of competence to that determined by members of the profession itself may not provide the depth of insight required to capture the complexity of healthcare and address the needs of important stakeholder groups. Future methodology should attempt to engage a variety of relevant stakeholders such as external health professions and the community to match professional education to health service demands.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=128350
Introduction
A competent workforce is a key element for effective health care systems (1). Competency based education recognises the need to match the health workforce to priorities for population health (2), and forms the basis of academic instruction and assessment for medicine, nursing and other health professions. A competency-based approach aims to maximise skill and resource utilisation and increase labour market efficiency (3). Competency frameworks provide an architectural blueprint for workforce development, fundamental in the delivery of person-centred care (4, 5). The frameworks are an increasingly important policy tool in defining knowledge, behaviour and skill in addition to professional standing for regulation and quality improvement purposes (4). They are often the basis for curricular development in health professional education programs and are also used as standards in accreditation of programs (6). Competency standards can be used in performance evaluation, professional development and for recruitment purposes, among other uses (2). Furthermore, there is significant positive correlation between frequency of use of competencies and perceived confidence in service provision by health professionals themselves (7).
There are many approaches to developing a competency framework (8). In health professions, the process of developing a competency framework is generally guided by the professional association (organisations representing the health profession members or regulatory body), with input from others, such as academics and practitioners (8). Specifically, members of medical, nursing and other health professions have traditionally defined their own professional competencies (8). There is limited guidance on competency framework development, including which stakeholder groups to involve in the process, when to include them and to what capacity. While competency framework development might be considered a specialised process, diversity in stakeholder engagement has been shown to increase the credibility of a competency framework for end users (8, 9). Health care practise is complex, and the development of competency frameworks in health professions requires strategies to capture and represent this reality and to meet patient and community needs. The outcomes and impacts of competency frameworks have implications for all stakeholder groups including students and education providers, practitioners, employers, policy makers, credentialing and certification organisations, and importantly, service users. For example the CanMEDS framework, which describes the abilities physicians require to meet the health care needs of the people they serve, has the overarching goal to improve patient care (6). Therefore, the perspectives of multiple stakeholders regarding the conceptualisation of competency and what should constitute the roles and functions of health professionals require consideration.
The general elements of competency development processes have been previously reviewed, and the critical nature of engaging key stakeholders in this process has been established, however not summarised (8). Guidelines for competency framework development by Widdett and Hollyforde emphasise that the framework must be relevant to all those who may benefit from its use and meet the needs of a wide range of possible applications (10). To achieve this, the guidelines recommend the process involves a range of stakeholders who will be impacted by the framework. The work of Lundsgaard and colleagues explores how various stakeholders contribute to an understanding of trainee competence and illustrates that incorporating stakeholder perceptions in the development of assessment processes and tools produces a more nuanced and complete conceptualisation of competence (11). However, there has been no examination of the current breadth of stakeholder engagement in competency framework development methodology in the health professions. Understanding if, and how, stakeholders have been involved in competency framework development will identify potential gaps in process. This may further inform guidelines for the development of these frameworks in health professions such that they reflect the work required in order to improve the health and well-being of the population, which is arguably an overarching goal of health care. Educators aim to produce graduates who are cognoscente of population needs at a community and individual level, yet competency frameworks supporting student education may not have considered all aspects of care. Therefore, the aim of this work was to review literature related to competency framework development in health professions, to identify stakeholder engagement in these processes. More specifically, this review aimed to answer the research question: What stakeholders are involved in competency framework development in health professions?
Methods
Eligibility Criteria
Eligibility criteria for this review were developed using the PICOS (Participant-Intervention-Comparator-Outcomes-Study design) format (12). Inclusion criteria for the review included original research publications related to methods used to develop competency standards in registered and self-regulating health disciplines including: Aboriginal and Torres Strait Islander Health Practice, Chinese Medicine, Chiropractic, Dental, Medical, Medical Radiation Practice, Nursing and Midwifery, Occupational Therapy, Optometry, Osteopathy, Pharmacy, Physiotherapy, Podiatry, Psychology, Nutrition and Dietetics, Exercise and Sports Science, Audiology and Speech Pathology. Development of specialist competency frameworks within a health profession were included if the results included the process of development of the framework. Specialist frameworks were defined as competency frameworks for a specialist role or those that are specific to a context, population or domain of practise (13). Method papers, such as occupational analysis, were excluded unless they were part of the methodology for the development of competency frameworks.
Publications that did not relate to the methods used to develop or revise competency frameworks, but merely published a framework, were excluded. Research related to competency framework development methodology for a health discipline not included above or pertaining to competency frameworks for preceptors were also excluded.
Search Strategy
Literature was reviewed systematically to maximise rigour, and the protocol was registered on the PROSPERO International Prospective Register of Systematic Reviews under registration number CRD42019128350: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=128350. Studies published between 1996 and 2021 were identified by searching MEDLINE, Pubmed, CINAHL Plus with full text, EMBASE and ERIC during March 2019. The search was updated in April 2021 to capture any additional frameworks published up until April 2021. The following key words were used to search:
[(“Aboriginal and Torres Strait Islander Health Practice” OR “chinese medicine” OR chiropract* OR dent* OR “radiation practice” OR nurs* OR midwif* OR “occupational therap*” OR optometr* OR osteopath* OR pharmac* OR physiotherap* OR podiatr* OR psycholog* OR “social work*” OR dietetic* OR dieti#ian OR “exercise and sports science” OR audiolog* OR “speech patholog*” OR “medical education”) AND “competency standard*” OR “competency framework” OR “curriculum development”].
The search was limited to English language papers published after 1996, the year of the formal adoption of CanMEDS Roles Framework, a globally recognised physician competency framework (6). This date was deemed relevant as the development of the CanMEDS framework, along with other national frameworks, are critical to the history of competency framework development in health professions, and most standards would have undergone revision since that time. Google Scholar was searched using the same search strategy (automatically sorted by relevance) to identify any publications that did not appear in the database searches. Reference lists of included literature were also hand searched.
Predefined topic and research questions guided data collection, extraction and analysis. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guided the process of document identification, screening and eligibility assessment (14).
The electronic reference management tool EndNote X9 (Clarivate Analytics, Philadelphia, PA) was used to export and manage references. After the removal of duplicates, one author (BL) independently screened titles and abstracts and selected studies according to the pre-defined inclusion criteria. Risk of bias was managed by ensuring that the full texts of remaining papers were screened in duplicate amongst four researchers (BL, EB, KM, and CP) to identify documents and publications for inclusion. Any discrepancies were discussed in order to reach consensus. The primary author (BL) completed data extraction with oversight from EB.
Quality Appraisal
To determine quality for review, the full text of each article was assessed independently by the primary researcher (BL), with a sample (20%) checked for accuracy by a second author (EB). Given the variation in research methodologies, the Critical Appraisal Skills Programme (CASP) tool was modified for use, as adapted by Halcomb et al. (15, 16). CASP is the most frequently used tool for quality appraisal and is recommended by the Cochrane Collaboration (17). Articles that did not achieve a “yes” on all items of the checklist were not excluded from the review, but the appraisal was taken into consideration in the overall rigour of the present review. Articles were included if the process of competency framework development process was described with sufficient detail.
Data Analysis
Data was analysed using techniques of a narrative synthesis, given the heterogeneous nature of the literature (18). This process enables the researcher to construct greater meaning through a process of “re-interpretation” of published findings (19).
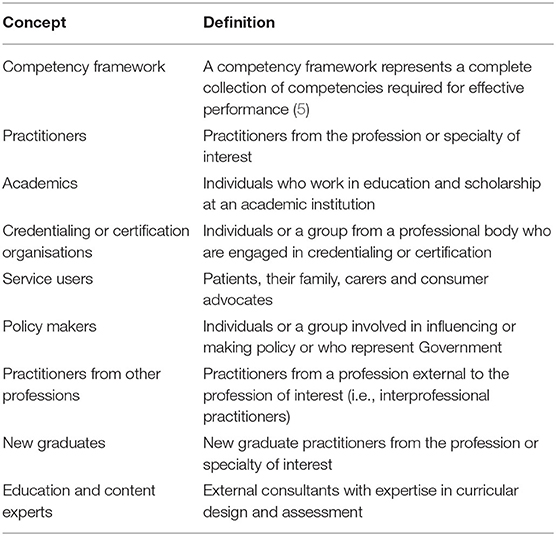
For the purposes of this review, we initially defined key concepts and stakeholder groups based on published definitions and author experience (Table 1).
Results
Search Results
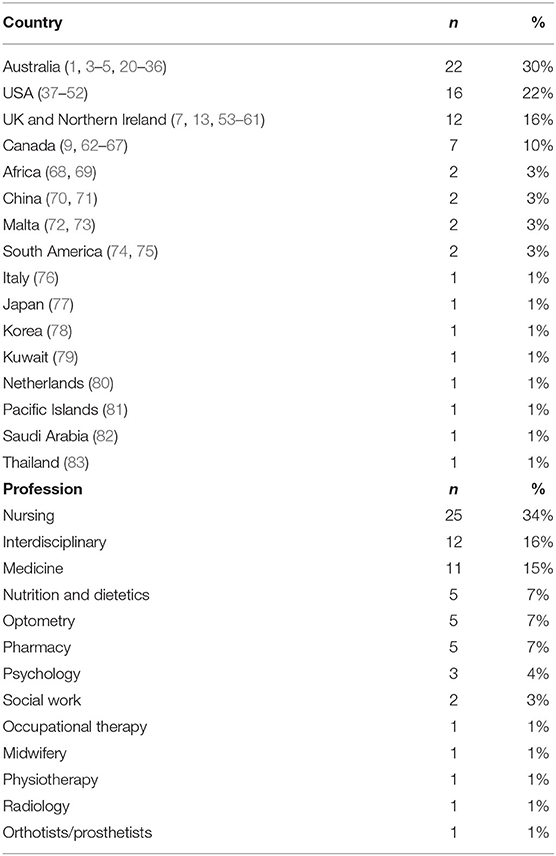
The total yield from all databases was 10,625 results, including six articles identified through hand searching of reference lists. This was reduced to 7,918 results after the removal of duplicates. Using the exclusion criteria against title and abstract, a total of 239 full-text publications were assessed for eligibility (Figure 1). Following full-text review, 73 articles were included in the review (Table 2). The reasons for exclusion included insufficient detail on methodology and papers that did not discuss methods to develop competency frameworks.
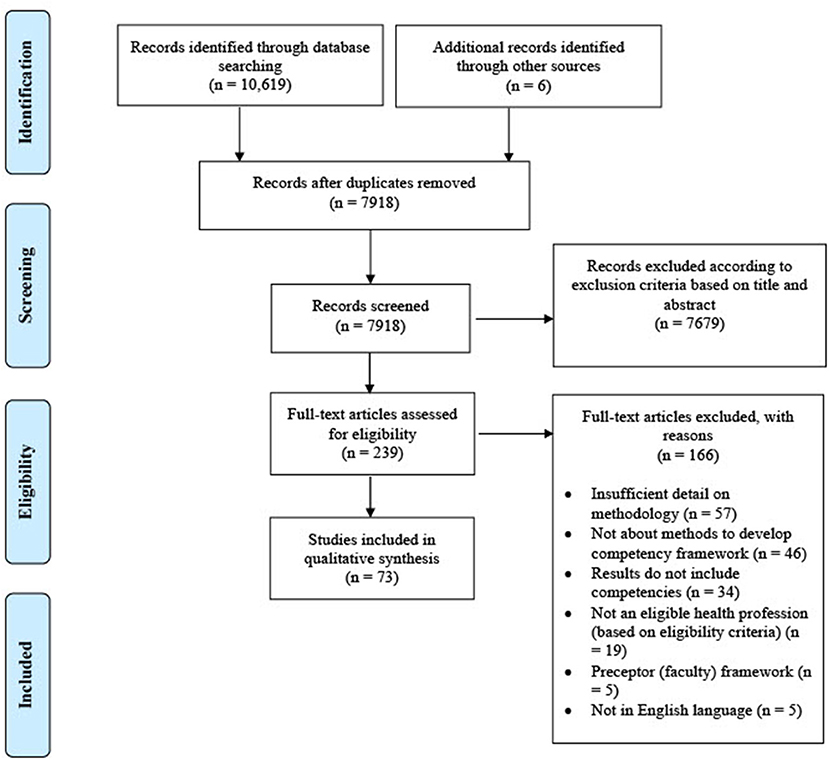
Figure 1. PRISMA flow diagram for identification of studies related to competency framework development methodology in health professions.
Quality Assessment
Quality assessment identified variability in the reporting of study methodology. Rigor of data analysis was the main factor delineating methodological quality between included publications (Supplementary Material). We classified the sampling generously in the first instance, however even with this consideration, the sample size and participant profile were unclear in some publications. In many publications, while significant numbers of stakeholders may have taken part in the competency framework development process, often they were a very homogenous group. Few publications acknowledged study limitations or weaknesses.
Characteristics of Included Publications
Studies published between 1997 and 2021 were primarily peer-reviewed articles (n = 72), with one thesis (n = 1). Most publications related to specialty or context-specific competencies (n = 55), with 18 pertaining to occupational or professional practise competencies. The majority of studies were from Australia (n = 22, 30%), followed by the USA (n = 16, 22%), the United Kingdom and Northern Ireland (n = 12, 16%), and Canada (n = 7, 10%) (Table 2). Nursing competencies accounted for the majority (n = 25, 34%), followed by interdisciplinary frameworks (n = 12, 16%) and medicine (n = 11, 15%) and (Table 2).
Summary of Results
Studies most frequently engaged four (n = 21, 29%) groups of stakeholders in the competency framework development process, albeit this varied considerably from one (n = 14, 19%) to seven groups (n = 1, 1%). There was considerable variation in the combination of stakeholder groups involved in the competency framework development process. None of the included studies provided a rationale for the number of stakeholder groups engaged in the competency framework development process.
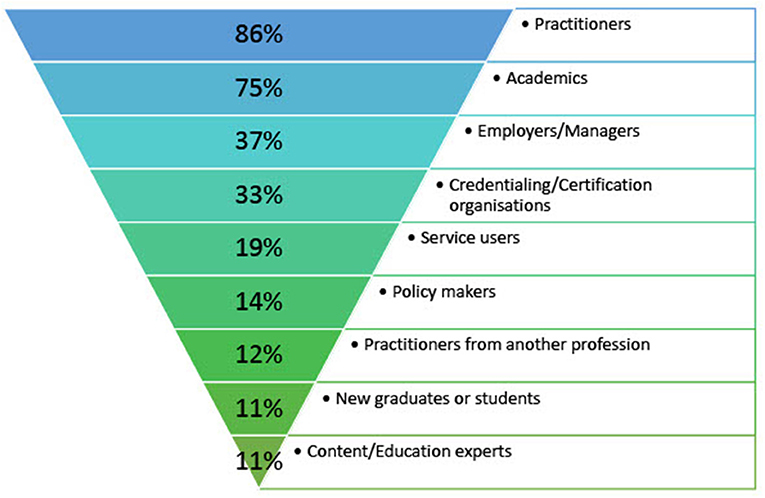
Practitioners and academics were the most frequently engaged stakeholder groups in the development of competency frameworks in health professions outlined in the search strategy (Figure 2). Less than 20% of papers involved service users and only 14% considered the perspective of policy makers in the reported process to develop a competency framework. The least frequently involved stakeholder groups in competency framework development methodology in health professions include practitioners from other professions, new graduates or students and content and/or education experts (Figure 2). Few of the included studies provided a rationale for the stakeholder groups engaged in the competency framework development process in health professions. The findings for each stakeholder group are elaborated on below, with examples to illustrate a critical lack of diversity in stakeholder engagement in competency framework development in health professions.
Practitioners
Practitioners from the profession were the most frequently engaged stakeholder group in the development of competency frameworks in health professions (Figure 2). Researchers sought practitioner input across a number of methods used to develop a competency framework, in the development of a competency framework, to gather input on an existing framework and to revise, validate or reach consensus on a draught competency framework (Table 3). Practitioners were most frequently involved in studies which reported using the Delphi technique (n = 24), interviews, focus groups or a workshop (n = 17) as methods to develop competency frameworks. Though there were a small number of papers which reported using values clarification and the nominal group technique as methods to develop a competency framework, all of the papers which utilised these methods engaged with practitioners in the process (Table 3). Practitioners were often selected as Delphi panellists based on clinical expertise; with the assumption they had the necessary experience to be considered “experts” in their field (20, 37, 38, 53, 54, 72). In studies which utilised observation of practise in competency development methodology, there was little effort made to undertake observations in non-clinical settings (settings which do not include one-on-one care), such as roles in public health, management, academia, and policy.
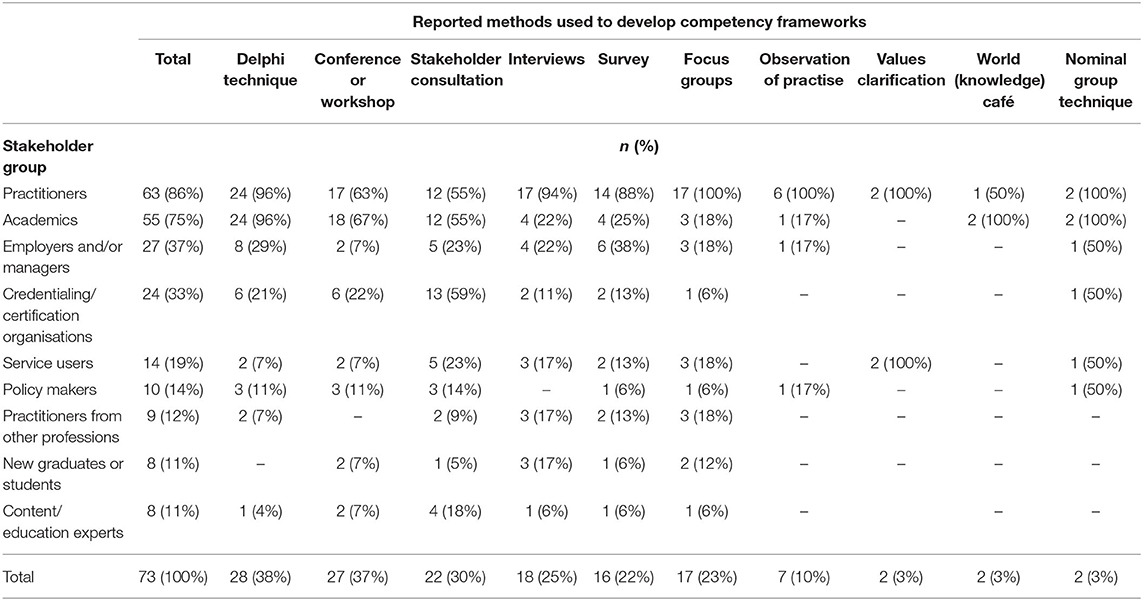
Table 3. Stakeholder engagement across reported methods used to develop a competency framework in health professions.
Academics
The majority of studies (75%) involved academics in the competency framework development process. Academics participated in the initial development of a competency framework, to solicit input for changes to an existing competency framework and frequently, in the review process. Academics were most often participants in papers which reported using the Delphi technique (n = 24), or in a workshop (n = 18), and were infrequently engaged in papers which reported utilising observation of practise (n = 1). Academics were less likely to be engaged in the process via focus groups and interviews than practitioners (Table 3). In some articles, the development process was limited to the input of a small sample of local, and mostly senior, academics (39–41, 73, 82).
Employers
Healthcare employers were inconsistently (37%) involved in the competency framework development process. They were most frequently involved as a stakeholder in studies that reported use of the Delphi technique (n = 8) or a survey (n = 6), though considerably less frequently than practitioners and academics (Table 3). The perspective of healthcare employers or management was sought in the development of an initial competency framework and to revise or validate a preliminary framework. Jie and Wanyi reported including this stakeholder group to provide breadth of perspective on workforce expectation and development (70). The views of employers in the focus group methodology used by Palermo et al. were included to ensure that the competency framework conveyed the professionalism required of the future dietetic workforce (21). Vardanyan et al. reported using interview methodology to explore the perspective of medical co-ordinators on the personal and managerial skills required of pharmacists (74).
Credentialing and/or Certification Organisation Representatives
Representatives from credentialing and/or certification organisations were involved in the competency framework development process in thirty-three percent (33%) of papers, mostly via a stakeholder consultation process in the end-stages (review and validation) of competency framework development (59%) (13, 42–44, 55, 77). In some studies, the competency framework development process was limited to input from members of the working group, which often comprised of senior representatives from professional bodies engaged in credentialing (40, 56, 75).
Service Users
Service users such as patients and their family, or consumer advocates were infrequently engaged (19%) in competency framework development, despite many authors claiming a focus on “patient-centred care” (Figure 2). Service users were most frequently engaged in the latter stages of the development process, via a stakeholder consultation (n = 5) to review or validate a framework and its application (Table 3). In observation of practise, there were no studies that utilised observation of interactions between clinicians and patients. Authors reported including service users, such as patient representatives and carers, in the development process to ensure that the resulting competency framework encompassed the needs of patients, families and carers (7, 9, 57). Framed as “experts by experience,” Carter et al. note that a focus group with service users helped to shape the content of the admiral nurse competency framework, based on their unique experience and expectations of care (57), though the sample was small (n = 5). Cashin et al. (4) state that partnering with service users is fundamental to the development of standards for practise for registered nurses providing person-centred health care. Yet, out of close to 10,000 stakeholders engaged in the redesign of the standards, only seven were patients or consumers. Similarly, Yates et al. (22) circulated a discussion paper outlining key roles and broad competency domains that constitute the specialist breast nursing role in Australia to 60 stakeholders for review, but only one was a representative from a consumer advocacy organisation and no other service users were engaged in the process. In the development of core competencies in cancer genetics for advanced practise oncology nurses, Calzone et al. (38) utilised the Delphi technique with an expert panel, which reportedly included consumer participants (n = 9). In this case the “consumers” were graduates of an advanced practise nursing oncology degree, selected to represent “novices in genetics” who are experienced in all aspects of oncology nursing care (38). In some studies, it was not clear how many service users were engaged in the competency framework development process (13, 68, 77). Few papers utilised values clarification as a method in the development of a competency framework, though Davis et al. (13) engaged users of diabetes services in this exercise to develop a competency framework for diabetes nursing. Kirk et al. note that engagement with patient representatives (n = 4) via a nominal group process validated the application of the competency framework to patient and family needs, and the role of the profession in meeting these needs (7).
Policy Makers
Policy makers were rarely (14%) engaged as a stakeholder in competency framework development, despite the output of many studies containing competency items related to policy (40, 55, 62, 63). The input of policy makers was sought primarily to review a competency framework, via a workshop or consultation process, and less frequently in the initial construction of such frameworks (Table 3). Lehane et al. purposively included national policy makers (Department of Health) in focus groups in a “creative collaborative process” to develop a competency framework for clinical effectiveness education for health and social care professionals (84).
Practitioners From Other Professions
Only 12% of papers engaged practitioners from other professions in the process of development, despite competency frameworks containing competency items related to multi-disciplinary care or the ability to work in a team (22, 42, 55). The perspective of practitioners from other professions was most frequently sought using qualitative methods such as focus groups (n = 3) and interviews (n = 3) in the development of a competency framework (Table 3). Moaveni et al. (64) engaged interprofessional colleagues throughout the framework development process who were able to identify attributes essential for multidisciplinary care. In addition, these same authors reported utilising an interdisciplinary Delphi panel to provide a consensus on what the role of a family practise registered nurse might look like based on multiple perspectives (64). Similarly, Chen et al. interviewed providers from different disciplines, for variety of perspective on clinical experiences and educational needs for the in-patient provider workforce (9).
New Graduates and Students
Only eight papers (11%) elected to include new graduates or students in the development of competency frameworks, most often using focus group methodology (n = 3) (Table 3). Authors reported sampling students or new graduates to capture the evolution of the profession, or to identify competencies required to work in emerging roles (1, 21).
Content/Education Experts
Content or education experts (also referred to as educationalists) were engaged in 11% of publications, particularly in the end-stages of competency framework development, such as via stakeholder consultation to refine or validate a framework (Table 3). More specifically, authors reported consulting content and education experts to review a competency framework for scope, and to assist with consistency in style, language, and format of the framework. Dressler et al. note that a multiple review process including education experts brought consistency and cohesion to an initially disparate preliminary competency framework (42). Jidkov et al. interviewed stakeholders from a range of expert backgrounds, including educationalists, for diversity in attitude and perspective and to reduce bias in the development of health informatics competencies for postgraduate medical education and training in the UK (58).
Discussion
There is little existing guidance on stakeholder involvement for competency framework development processes. This study aimed to identify the key stakeholders commonly involved in the competency framework development process in health professions. Our findings build on a previous scoping review of competency framework development (8) by synthesising the evidence and highlighting a lack of diversity in participation of stakeholders in this process. Across methods used to develop competency frameworks, there was a focus on the views of the profession, including practitioners and academics. This is unsurprising, however there is no indication that this is best practise, but rather a reflection on the current status of competency-based education (22). Patients today expect healthcare professionals to not only be experts in their field, but also to work successfully in a team, provide patient-centred care and communicate effectively with patients and colleagues (85, 86). Limiting the conceptualisation of competence to that determined by members of the profession itself may not provide the depth of insight required to capture the complexity of healthcare and address the needs of key stakeholder groups, such as service users (9).
It is well-established that coordinated, team-based health care leads to improvements in health outcomes and patient satisfaction (87). Despite this, only 12% of papers in the present review involved practitioners from other professions in the process of competency framework development. While it is recognised that competency frameworks are limited in terms of describing team competence (88), the application of competencies related to team-based care has been shown to limit re-admissions, improve health outcomes and improve the efficiency and effectiveness of care (87, 89). Poorly structured stakeholder identification and participation, risks the exclusion of valuable perspectives (90). Practitioners from other professions are likely able to identify attributes required to support other key members of the health care team, in order to deliver effective and coordinated health care. Therefore, the participation of interprofessional colleagues in competency framework development may increase the likelihood that the competency framework will encompass standards for team-based health care. Given that coordination of care is a critical component of an effective health system (87), competency framework development should engage other health professions as a stakeholder in order to maximise multidisciplinary understanding and practise (2).
Health 2020 calls for a people-centred health system (91). It is increasingly acknowledged that attention to patients, their family and the community results in improved health outcomes and treatment compliance (92, 93). Here we identified a lack of patient, or service user, perspective as a limitation to competency framework development, with <20% of papers electing to engage patients or consumer advocates in the process. Traditionally, competency frameworks may be heavily reflective of traditional health care settings, which may not have emphasised person-centred care. While person-centred care has become a key aspect of any clinical encounter, the evolution of competency frameworks for health professions appears to lag behind (94). For example, in the development of competency frameworks, only five papers in this review published before 2010 included service users (13, 22, 38, 43). Engagement with patient and family advocacy groups broadens the conceptualisation of competency, particularly given the recent increase in consumer participation in health care (4, 65). Service user participation in health care research may provide unique information about the effectiveness of health care systems including how to improve patient experience and outcomes (95). Patients, and their carers, are intimate with the realities of health system operations and can identify required competencies, from the perspective of those who receive care. Furthermore, consumer involvement, particularly in qualitative methods, such as interviews, focus groups and the nominal group technique, can provide rich insight and reinforce the application of the competency framework to patient and family needs (7). Future competency framework development research should ideally involve a range of stakeholders including service users, such as patients, their family and the wider community.
Previous work has highlighted a need for a wider interpretation of employability, and therefore, of what constitutes professional competence (96). Less than 40% of papers in this review included employers in the competency framework development process. The massification of higher education, a largely stratified and shrinking graduate labour market and an increasing onus on students to improve their own employability skills makes the professional transition to employment a significant challenge (97). Graduate perceptions of employment suggest there is considerable pressure for each individual to develop their own employability relative to others in the post-graduate landscape (97). Without a benchmark, namely, a competency framework, which encompasses professionalism required of the workforce, it is unreasonable to expect an individual to be responsible for their own employability. Collet et al. suggest that competency-based education needs to shift towards enabling graduates to perform in a variety of workplace contexts, and competency centred on organisational purpose (98). Given the complexity of the employment sector described above, the perspective of healthcare employers in the development process is essential in re-shaping the conceptualisation of employability, based on their unique perspective of workforce expectation and demand (21). Ultimately, employability benefits the individual, the workforce, the community and the economy (98). It is therefore in the best interests of all to engage with a variety of stakeholders, including employers in methodologies for competency framework development. Specifically, greater involvement of employers, patients/end users and others in the interdisciplinary team is needed to ensure high quality competency framework development in health professions.
Strengths and Limitations
This review offers a synthesis of stakeholder engagement in competency framework development in defined health professions and highlights a critical lack of diversity in perspective, however, needs to be considered in the context of its limitations. As healthcare systems are heterogeneous internationally, articles set in other countries, may have used different terms than those used by the authors, resulting in exclusion. Another limitation is that the grey literature included in this review may not be representative of all unpublished studies. Furthermore, the included articles belong to professions across the health care spectrum, where the involvement of stakeholders may vary. There is future scope to directly compare the results of this review to the development of well-established competency frameworks for health professions, such as the CanMEDS Physician Competency Framework (6). Future research should explore shifts in stakeholder engagement in competency framework development in health professions over time and evaluate the downstream implications of a critical lack of diversity in stakeholder engagement on current health care practises.
Conclusion
A well-defined competency framework serves as a framework to advance the profession, retain practitioners, support growth and development and improve health and safety outcomes for patients. A range of stakeholders may be involved in competency framework development, but to date, there has been a focus only on the views of the profession. Competence in the workforce is a shared responsibility. Therefore, methodologies in future competency framework development should aim to involve a range of stakeholders including other health professions and end-users in competency framework development to match professional education to health service demands.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
BL, EB, KM, and CP contributed to the design of the review. BL did the literature search, performed data analysis, and drafted the manuscript. EB contributed to quality appraisal. All authors contributed to the literature search, revision of the manuscript, and approval of the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.759848/full#supplementary-material
References
1. Ash S, O'Connor J, Anderson S, Ridgewell E, Clarke L. A mixed-methods research approach to the review of competency standards for orthotist/prosthetists in Australia. Int J Evid Based Healthc. (2015) 13:93–103. doi: 10.1097/XEB.0000000000000038
2. Langins M. Strengthening a Competency Health Workforce for the Provision of Coordinated/Integrated Health Services. Copenhagen: World Health Organisation (WHO) (2015).
3. Kiely PM, Chakman J. Competency standards for entry-level to the profession of optometry 1993. Clin Exp Optomet. (1993) 75:150–61. doi: 10.1111/j.1444-0938.1993.tb02968.x
4. Cashin A, Heartfield M, Bryce J, Devey L, Buckley T, Cox D, et al. Standards for practice for registered nurses in Australia. Collegian. (2017) 24:255–66. doi: 10.1016/j.colegn.2016.03.002
5. Hughes R. Competencies for effective public health nutrition practice: a developing consensus. Public Health Nutr. (2004) 7:683–91. doi: 10.1079/PHN2003574
6. Frank JR, Snell L, Sherbino L. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada (2015).
7. Kirk M, Tonkin E, Skirton H. An iterative consensus-building approach to revising a genetics/genomics competency framework for nurse education in the UK. J Adv Nurs. (2014) 70:405–20. doi: 10.1111/jan.12207
8. Batt AM, Tavares W, Williams B. The development of competency frameworks in healthcare professions: a scoping review. Adv Health Sci Educ. (2019) 25:913–87. doi: 10.1007/s10459-019-09946-w
9. Chen SP, Krupa T, Lysaght R, McCay E, Piat M. The development of recovery competencies for in-patient mental health providers working with people with serious mental illness. Admin Policy Ment Health. (2013) 40:96–116. doi: 10.1007/s10488-011-0380-x
10. Whiddett S, Hollyforde S. A Practical Guide to Competencies: How to Enhance Individual and Organisational Performance. 2nd ed. London: Chartered Institute of Personnel and Development (2003).
11. Lundsgaard K, Tolsgaard M, Mortensen O, Mylopoulos MDø. Embracing multiple stakeholder perspectives in defining trainee competence. Acad Med. (2019) 94:838–46. doi: 10.1097/ACM.0000000000002642
12. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ionnidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. doi: 10.1136/bmj.b2700
13. Davis R, Turner E, Hicks D, Tipson M. Developing an integrated career and competency framework for diabetes nursing. J Clin Nurs. (2008) 17:168–74. doi: 10.1111/j.1365-2702.2006.01866.x
14. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
15. Halcomb E, Stephens M, Bryce J, Foley E, Ashley C. Nursing competency standards in primary health care: an integrative review. J Clin Nurs. (2016) 25:1193–205. doi: 10.1111/jocn.13224
16. CASP. CASP (Qualitative) Checklist. Critical Appraisal Skills Programme (CASP). Oxford, UK (2018).
17. Noyes J, Popay J, Pearson A, Hannes K, Booth A. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane: John Wiley & Sons (2015). p. 571–92.
18. Sandelowski M, Barroso J. Creating metasummaries of qualitative findings. Nurs Res. (2003) 52:226–33. doi: 10.1097/00006199-200307000-00004
19. Britten N, Campbell R, Pope C, Donovan J, Morgan M, Pill R. Using meta ethnography to synthesis qualitative research: a worked example. J Health Serv Res Policy. (2002) 7:209–15. doi: 10.1258/135581902320432732
20. Hughes R, Begley A, Yeatman H. Aspirational competency expectations for public health nutritionists in Australia: a consensus study. Nutr Dietetics. (2015) 72:122–31. doi: 10.1111/1747-0080.12098
21. Palermo C, Conway J, Beck EJ, Dart J, Capra S, Ash S. Methodology for developing competency standards for dietitians in Australia. Nurs Health Sci. (2016) 18:130–7. doi: 10.1111/nhs.12247
22. Yates P, Evans A, Moore A, Heartfield M, Gibson T, Luxford K. Competency standards and educational requirements for specialist breast nurses in Australia. Collegian. (2007) 14:11–5. doi: 10.1016/S1322-7696(08)60542-9
23. Albarqouni L, Hoffman T, Straus S, Olsen N, Young T, Ilic D, et al. Core competencies in evidence-based practice for health professionals: consensus statement based on a systematic review and Delphi survey. JAMA Netw Open. (2018) 1:w180281. doi: 10.1001/jamanetworkopen.2018.0281
24. Canning D, Rosenberg J, Yates P. Therapeutic relationships in specialist palliative care nursing practice. Int J Palliat Nurs. (2007) 13:222–9. doi: 10.12968/ijpn.2007.13.5.23492
25. Halcomb E, Stephens M, Bryce J, Foley E, Ashley C. The development of professional practice standards for Australian general practice nurses. J Adv Nurs. (2017) 73:1958–69. doi: 10.1111/jan.13274
26. Dunn SV, Lawson D, Robertson S, Underwood M, Clark R, Valentine T, et al. The development of competency standards for specialist critical care nurses. J Adv Nurs. (2000) 31:339–46. doi: 10.1046/j.1365-2648.2000.01292.x
27. Ford L, McIntyre G. Competency standards for occupational therapy assistants: outline of the development process and applications. Aust Occup Ther J. (2004) 51:49–52. doi: 10.1111/j.1440-1630.2004.00426.x
28. Gill FJ, Kendrick T, Davies H, Greenwood M. A two phase study to revise the Australian practice standards for specialist critical care nurses. Aust Crit Care. (2017) 30:173–81. doi: 10.1016/j.aucc.2016.06.001
29. Phillips S, Ash S, Tapsell L. Relevance of the competency standards to entry level dietetic practice. Aust J Nutr Dietetics. (2000) 57:198–207. doi: 10.1111/j.1747-0080.2011.01552.x
30. Harding P, Pearce A. Advanced musculoskeletal physiotherapy in public hospitals: utilizing a competency based training and assessment approach. Physiotherapy. (2015) 101:E1184. doi: 10.1016/j.physio.2015.03.2107
31. Homer CS, Passant L, Kildea S, Pincombe J, Thorogood C, Leap N, et al. The development of national competency standards for the midwife in Australia. Midwifery. (2007) 23:350–60. doi: 10.1016/j.midw.2006.03.008
32. Kiely PM, Chakman J, Horton P. Optometric therapeutic competency standards 2000. Clin Exp Optom. (2000) 83:300–14. doi: 10.1111/j.1444-0938.2000.tb04918.x
33. Kiely PM. Optometrists association australia universal (entry-level) and therapeutic competency standards for optometry 2008. Clin Exp Optom. (2009) 92:362-5:6–86. doi: 10.1111/j.1444-0938.2009.00383.x
34. Kiely PM, Slater J. Optometry Australia entry-level competency standards for optometry 2014. Clin Exp Optom. (2015) 98:65–89. doi: 10.1111/cxo.12216
35. Williams C, Hill V. Review of the competency standards for perioperative nursing. ACORN. (2007) 20:22.
36. Zupanc CM, Burgess-Limerick R, Hill A, Riek S, Wallis GM, Plooy AM, et al. A competency framework for colonoscopy training derived from cognitive task analysis techniques and expert review. BMC Med Educ. (2015) 15:216. doi: 10.1186/s12909-015-0494-z
37. Burns C, Lachat AM, Gordon K, Ryan MG, Gruden M, Barker DP, et al. Respiratory protection competencies for the occupational health nurse. Workplace Health Safety. (2014) 62:96–104. doi: 10.1177/216507991406200303
38. Calzone KA, Jenkins J, Masny A. Core competencies in cancer genetics for advanced practice oncology nurses. Oncol Nurs Forum. (2002) 29:1327–33. doi: 10.1188/02.ONF.1327-1333
39. Kruszewski BD, Spell NO 3rd. A consensus approach to identify tiered competencies in quality improvement and patient safety. J Grad Med Educ. (2018) 10:646–50. doi: 10.4300/JGME-D-18-00210.1
40. McDaniel SH, Grus CL, Cubic BA, Hunter CL, Kearney LK, Schuman CC, et al. Competencies for psychology practice in primary care. Am Psychol. (2014) 69:409–29. doi: 10.1037/a0036072
41. Clark L, Calvillo E, Cruz FD, Fongwa M, Kools S, Lowe J, et al. Cultural competencies for graduate nursing education. J Prof Nurs. (2011) 27:133–9. doi: 10.1016/j.profnurs.2011.02.001
42. Dressler DD, Pistoria MJ, Budnitz TL, McKean SCW, Amin AN. Core competencies in hospital medicine: development and methodology. J Hosp Med. (2006) 1(Suppl. 1):48–56. doi: 10.1002/jhm.85
43. Jenkins J, Calzone KA. Establishing the essential nursing competencies for genetics and genomics. J Nurs Scholarship. (2007) 39:10–6. doi: 10.1111/j.1547-5069.2007.00137.x
44. Leipzig RM, Granville L, Simpson D, Anderson MB, Sauvigne K, Soriano RP. Keeping granny safe on July 1: a consensus on minimum geriatrics competencies for graduating medical students. Acad Med. (2009) 84:604–10. doi: 10.1097/ACM.0b013e31819fab70
45. Bobonich M, Nolen M. Competencies for dermatology nurse practitioners. J Am Assoc Nurse Pract. (2018) 30:606–13. doi: 10.1097/JXX.0000000000000137
46. Carrico R, Rebmann T, English J, Mackey J, Cronin S. Infection prevention and control competencies for hospital-based health care personnel. Am J Infect Control. (2008) 36:691–701. doi: 10.1016/j.ajic.2008.05.017
47. Carrougher GJ, Hollowed KA, Sproul JL, Wiggins BJ, Mann-Salinas E. Burn nurse competencies: developing consensus using E-Delphi methodology. J Burn Care Res. (2018) 39:751–9. doi: 10.1093/jbcr/irx036
48. Curl AL, Tompkins CJ, Rosen AL, Zlotni KJ. A case study of professional change: the impact of the national gerontological social work competencies survey. Gerontol Geriatr Educ. (2010) 31:256–73. doi: 10.1080/02701960.2010.503135
49. Greco KE, Tinley S, Seibert D. Development of the essential genetic and genomic competencies for nurses with graduate degrees. Annu Rev Nurs Res. (2011) 29:173–90. doi: 10.1891/0739-6686.29.173
50. Misener TR, Alexander JW, Blaha AJ, Clarke PN, Cover CM, Felton GM, et al. National Delphi study to determine competencies for nursing leadership in public health. Image J Nurs Sch. (1997) 29:47–51. doi: 10.1111/j.1547-5069.1997.tb01139.x
51. Wilson L, Callender B, Hall TL, Jogerst K, Torres H, Velji A. Identifying global health competencies to prepare 21st century global health professionals: report from the global health competency subcommittee of the consortium of universities for global health. J Law Med Ethics. (2014) 42(Suppl. 2):26–31. doi: 10.1111/jlme.12184
52. Campbell LA, Harmon MJ, Joyce BL, Little SH. Quad Council Coalition community/public health nursing competencies: building consensus through collaboration. Public Health Nursing. (2020) 37:96–112. doi: 10.1111/phn.12666
53. Galbraith K, Ward A, Heneghan C. A real-world approach to evidence-based medicine in general practice: a competency framework derived from a systematic review and Delphi process. BMC Med Educ. (2017) 17:78. doi: 10.1186/s12909-017-0916-1
54. Liddell AE, Allan S, Goss K. Therapist competencies necessary for the delivery of compassion-focused therapy: a Delphi study. Psychol Psychother. (2017) 90:156–76. doi: 10.1111/papt.12105
55. Santy J, Rogers J, Davis P, Jester R, Kneale J, Knight C, et al. A competency framework for orthopaedic and trauma nursing. J Orthop Nurs. (2005) 9:81–6. doi: 10.1016/j.joon.2005.02.003
56. Tipson M, Turner E. Career and competency framework for diabetes nursing. J Diabetes Nurs. (2002) 6:179–81.
57. Carter C, Bray J, Read K, Harrison-Dening K, Thompson R, Brooker D. Articulating the unique competencies of admiral nurse practice. Working Older People. (2018) 22:139–47. doi: 10.1108/WWOP-02-2018-0007
58. Jidkov L, Alexander M, Bark P, Williams JG, Kay J, Taylor P, et al. Health informatics competencies in postgraduate medical education and training in the UK: a mixed methods study. BMJ Open. (2019) 9:e025460. doi: 10.1136/bmjopen-2018-025460
59. Courtenay M, Lim R, Castro-Sanchez E, Deslandes R, Hodson K, Morris G, et al. Development of consensus-based national antimicrobial stewardship competencies for UK undergraduate healthcare professional education. J Hosp Infect. (2018) 100:245–56. doi: 10.1016/j.jhin.2018.06.022
60. Forsyth P, Warren A, Thomson C, Bateman J, Greenwood E, Williams H, et al. A competency framework for clinical pharmacists and heart failure. Int J Pharm Pract. (2018) 27:424–35. doi: 10.1111/ijpp.12465
61. Hay EM, Campbell A, Linney S, Wise E. Development of a competency framework for general practitioners with a special interest in musculoskeletal/rheumatology practice. Rheumatology. (2007) 46:360–2. doi: 10.1093/rheumatology/kel357
62. Schofield R, Chircop A, Baker C, Dietrich Leurer M, Duncan S, Wotton D. Entry-to-practice public health nursing competencies: a Delphi method and knowledge translation strategy. Nurse Educ Today. (2018) 65:102–7. doi: 10.1016/j.nedt.2018.03.001
63. Charles L, Triscott JAC, Dobbs BM, McKay R. Geriatric core competencies for family medicine curriculum and enhanced skills: care of elderly. Can Geriatr J. (2014) 17:53–62. doi: 10.5770/cgj.17.95
64. Moaveni A, Gallinaro A, Conn LG, Callahan S, Hammond M, Oandasan I. A Delphi approach to developing a core competency framework for family practice registered nurses in Ontario. Nurs Leadership. (2010) 23:45–60. doi: 10.12927/cjnl.2011.22142
65. Jacono B, Young L, Baker C, Richardson HR, Cable-Williams B, Jewers H, et al. Developing palliative care competencies for the education of entry level baccalaureate prepared Canadian nurses. Int J Nurs Educ Scholarship. (2011) 8:21. doi: 10.2202/1548-923X.2251
66. Wood V, Flavell A, Vanstolk D, Bainbridge L, Nasmith L. The road to collaboration: developing an interprofessional competency framework. J Interprof Care. (2009) 23:621–9. doi: 10.3109/13561820903051477
67. Esplen MJ, Hunter J, Maheu C, Rosberger Z, Wong J, McGillicuddy P, et al. de Souza interprofessional practice cancer competency framework. Support Care Cancer. (2020) 28:797–808. doi: 10.1007/s00520-019-04823-z
68. Kiguli S, Mubuuke R, Baingana R, Kijjambu S, Maling S, Waako P, et al. A Consortium approach to competency based undergraduate medical education in Uganda: process, opportunities and challenges. Educ Health. (2014) 27:163–9. doi: 10.4103/1357-6283.143774
69. Shah K, Naidoo K, Loughman J. Development of socially responsive competency frameworks for ophthalmic technicians and optometrists in Mozambique. Clin Exp Optomet. (2016) 99:173–82. doi: 10.1111/cxo.12282
70. Jie L, Wanyi H. Pragmatic professionalism: a Fuzzy Delphi study on the competencies of social workers in Guangzhou, China. Br J Soc Work. (2018) 48:505–24. doi: 10.1093/bjsw/bcx035
71. Zhang X, Meng K, Chen S. Competency framework for specialist critical care nurses: a modified Delphi study. Nurs Crit Care. (2020) 25:45–52. doi: 10.1111/nicc.12467
72. Attard DJ, Ross DL, Weeks KW. Developing a spiritual care competency framework for pre-registration nurses and midwives. Nurse Educ Pract. (2019) 40:102604. doi: 10.1016/j.nepr.2019.07.010
73. Attard J, Ross L, Weeks KW. Design and development of a spiritual care competency framework for pre-registration nurses and midwives: a modified Delphi study. Nurse Educ Pract. (2019) 39:96–104. doi: 10.1016/j.nepr.2019.08.003
74. Vardanyan H, Mosegui GBG, Miranda ES. Skills and core competencies of pharmacists in humanitarian assistance. Prehosp Disaster Med. (2018) 33:266–72. doi: 10.1017/S1049023X18000304
75. Pastrana T, Wenk R, De Lima L. Consensus-based palliative care competencies for undergraduate nurses and physicians: a demonstrative process with Colombian universities. J Palliative Med. (2016) 19:76–82. doi: 10.1089/jpm.2015.0202
76. Hoxhaj I, Tognetto A, Acampora A, Stojanovic J, Boccia S. Core competencies in cancer genomics for healthcare professionals: results from a systematic literature review and a Delphi process. J Cancer Educ. (2021). doi: 10.1007/s13187-021-01956-w
77. Haruta J, Sakai I, Otsuka M, Yoshimoto H, Yoshida K, Goto M, et al. Development of an interprofessional competency framework in Japan. J Interprof Care. (2016) 30:675–7. doi: 10.1080/13561820.2016.1192588
78. Lim CS, Lee YS, Lee YD, Kim HS, Jin GH, Choi SY, et al. The job competency of radiological technologists in Korea based on specialists opinion and questionnaire survey. J Educ Eval Health Professions. (2017) 14:9. doi: 10.3352/jeehp.2017.14.9
79. Al-Haqan A, Smith F, Bader L, Bates I. Competency development for pharmacy: adopting and adapting the Global Competency Framework. Res Social Adm Pharm. (2020) 17:771–85. doi: 10.1016/j.sapharm.2020.06.023
80. Keijser WA, Handgraaf HJM, Isfordink LM, Janmaat VT, Vergroesen P-PA, Verkade JMJS, et al. Development of a national medical leadership competency framework: the Dutch approach. BMC Med Educ. (2019) 19:441. doi: 10.1186/s12909-019-1800-y
81. Brown AN, Gilbert BJ, Bruno AF, Cooper GM. Validated competency framework for delivery of pharmacy services in pacific-island countries. J Pharm Pract Res. (2012) 42:268–72. doi: 10.1002/j.2055-2335.2012.tb00186.x
82. Zaini RG, Bin Abdulrahman KA, Al-Khotani AA, Al-Hayani AM, Al-Alwan IA, Jastaniah SD. Saudi Meds: a competence specification for Saudi medical graduates. Med Teacher. (2011) 33:582–4. doi: 10.3109/0142159X.2011.578180
83. Suwannaprom P, Suttajit S, Eakanunkul S, Supapaan T, Kessomboon N, Udomaksorn K, et al. Development of pharmacy competency framework for the changing demands of Thailand's pharmaceutical and health services. Pharm Pract. (2020) 18:2141. doi: 10.18549/PharmPract.2020.4.2141
84. Lehane E, Agreli H, O' Connor S, Hegarty J, Leahy Warren P, Bennett D, et al. Building capacity: getting evidence-based practice into healthcare professional curricula. BMJ Evid Based Med. (2020) 26:246. doi: 10.1136/bmjebm-2020-111385
85. Gillam S, Siriwardena A. Evidence-based healthcare and quality improvement. Qual Prim Care. (2014) 22:125–32.
86. van der Aa J, Aabakke A, Andersen B, Settnes A, Hornnes P, Teunissen P, et al. From prescription to guidance: a European framework for generic competencies. Adv Health Sci Educ. (2020) 25:173–87. doi: 10.1007/s10459-019-09910-8
87. Antonelli R, McAllister J, Popp J. Making Care Coordination a Critical Component of the Paediatric Health System: A Multidisciplinary Framework. New York, NY: The Commonwealth Fund (2009).
88. Hodges BD, Lingard L. The Question of Competence: Reconsidering Medical Education in the Twenty-First Century. New York, NY: Cornell University Press (2013).
89. WHO. HEARTS Technical Package for Cardiovascular Disease Management in Primary Health Care: Team-Based Care. Geneva: World Health Organisation (WHO) (2018).
90. Virgolesi M, Marchetti A, Pucciarelli G, Valentina B, Pulimeno AML, Piredda M, et al. Stakeholders' perspective about their engagement in developing a competency-based nursing baccalaureate curriculum: a qualitative study. J Prof Nurs. (2019) 36:141–6. doi: 10.1016/j.profnurs.2019.09.003
91. WHO. Health 2020: A European Policy Framework Supporting Action Across Government and Society for Health and Well-Being. Copenhagen: World Health Organisation (WHO) (2013).
92. Gruppen LD, Mangrulkar RS, Kolars JC. The promise of competency-based education in the health professions for improving global health. Hum Resources Health. (2012) 10:43. doi: 10.1186/1478-4491-10-43
93. WHO. Preparing a Health Care Workforce for the 21st Century: The Challenge of Chronic Conditions. Geneva: World Health Organisation (WHO) (2005).
94. Little P, Everitt H, Williamson I, Warner G, Gould C, Ferrier K, et al. Preferences of patients for patient centred approach to consultation in primary care: observational study. BMJ. (2001) 322:468–72. doi: 10.1136/bmj.322.7284.468
95. Santana MJ, Manalili K, Jolley RJ, Zelinksy S, Quan H, Mingshan L. How to practice person-centred care: a conceptual framework. Health Expect. (2017) 21:429–40. doi: 10.1111/hex.12640
96. Williams S, Dodd LJ, Steele C, Randall R. A systematic review of current understandings of employability. J Educ Work. (2016) 29:877–901. doi: 10.1080/13639080.2015.1102210
97. O'Connor H, Bodicoat M. Exploitation or opportunity? Student perceptions of internships in enhancing employability skills. Br J Sociol Educ. (2016) 38:435–49. doi: 10.1080/01425692.2015.1113855
Keywords: competency frameworks, health professions, stakeholder engagement, education, competency development
Citation: Lepre B, Palermo C, Mansfield KJ and Beck EJ (2021) Stakeholder Engagement in Competency Framework Development in Health Professions: A Systematic Review. Front. Med. 8:759848. doi: 10.3389/fmed.2021.759848
Received: 17 August 2021; Accepted: 22 October 2021;
Published: 12 November 2021.
Edited by:
Madawa Chandratilake, University of Kelaniya, Sri LankaReviewed by:
Shaista S. Guraya, Royal College of Surgeons in Ireland, BahrainBhavani Veasuvalingam, Newcastle University Medicine Malaysia, Malaysia
Copyright © 2021 Lepre, Palermo, Mansfield and Beck. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Breanna Lepre, Ymw3NzhAdW93bWFpbC5lZHUuYXU=
 Breanna Lepre
Breanna Lepre Claire Palermo
Claire Palermo Kylie J. Mansfield
Kylie J. Mansfield Eleanor J. Beck
Eleanor J. Beck