- 1Stomatological Hospital, Southern Medical University, Guangzhou, China
- 2Department of Cariology, Endodontology and Periodontology, University Leipzig, Leipzig, Germany
- 3Dr. D. Y. Patil Dental College and Hospital, Dr. D. Y. Patil Vidyapeeth, Pune, India
- 4Shenzhen Stomatological Hospital, Southern Medical University, Shenzhen, China
Background: This systematic review evaluates the oral health-related quality of life (OHRQoL) of patients with chronic respiratory diseases.
Methods: A systematic literature search was performed based on the PubMed, Medline, Web of Science, and Scopus, using the search terms: “oral health-related quality of life” and “respiratory disease” or “lung” and “oral health-related quality of life.” Full-text articles published until June 30, 2021 and reporting any OHRQoL measurement in children or adults with a chronic respiratory disease or condition were included and analyzed qualitatively.
Results: A total of seven out of 44 studies were included, of which four studies examined adults and three studies investigated children. The respective diseases were chronic obstructive pulmonary disease (COPD) (n = 2), sleep apnea (n = 2), severe asthma (n = 1), cystic fibrosis (n = 1), and lung transplantation (n = 1). Four studies confirmed a worse OHRQoL in the respiratory diseased group compared to healthy controls. The overall OHRQoL was reduced in the included studies. Oral health, health-related quality of life, and disease-related parameters were rarely examined with regard to OHRQoL.
Conclusion: Patients with chronic respiratory diseases show a reduced OHRQoL. Oral health should be fostered in these individuals to support their OHRQoL.
Background
Chronic diseases affecting the respiratory system cover a broad variety of different conditions; thereby, lifestyle or risk factor-associated, high prevalent diseases, such as chronic obstructive pulmonary disease (COPD), exist (1) alongside with very rare genetic diseases, such as cystic fibrosis (2). Other examples of respiratory diseases are asthma, which is a highly prevalent condition with primarily an autoimmune cause (3) or sleep apnea or sleep-disordered breathing as a complex and multifactorial condition (4). Especially, if breathlessness occurs, chronic respiratory diseases can be related to a high morbidity and a negative impact on the quality of life of affected patients (5). Additionally, chronic respiratory diseases, such as COPD, can lead to different comorbidities and physical deconditioning, decreasing the health-related quality of life (HRQoL) of patients suffering from these diseases (6).
Oral health is often reported to be affected by respiratory diseases in respective patients; a recent meta-analysis showed that patients with asthma as well as COPD showed an association to the presence of periodontal diseases (7). Besides a direct association, medications, e.g., asthma medication including bronchodilators, corticosteroids, or anticholinergic drugs inhaled by the patients can increase the risk of dry mouth, dental caries, dental erosion, periodontal diseases, and oral candidiasis (8, 9). Especially for severely diseased patients, such as patients with cystic fibrosis or COPD, oral bacteria related to dental and periodontal diseases can also colonize the lungs, increasing the risk for complications (10, 11). Additionally, patients with obstructive sleep apnea, which is completely different from the other respiratory diseases described here, show affected oral health conditions as well as the relationship between oral diseases and the underlying disorder; this is heterogeneous, but obvious for both the children and adults (12). In the complex relationship between oral and respiratory health, the multifactorial character of oral diseases, as well as the anatomic proximity of the oropharyngeal and respiratory tract could be relevant.
A particular issue of interest in this context is the oral HRQoL (OHRQoL). As a part of the general HRQoL, the OHRQoL reflects the perceived affection of HRQoL by conditions related to the oral cavity including teeth, mouth, or dentures (13, 14). In other groups of systemically diseased patients, the OHRQoL showed interesting and clinically relevant results. For example, patients with rheumatic diseases show an impaired OHRQoL, whereby rheumatic disease-related parameters might be major influential factors (15). On the other hand, patients after solid organ transplantation were supposed to undergo a “response shift” of the perception of OHRQoL, i.e., reduced awareness of their insufficient oral health status (16). Considering the impaired oral health, reduced general HRQoL alongside the anatomic proximity between the oral cavity and the respiratory system, the OHRQoL of patients with different respiratory diseases appears a topic of clinical interest. Therefore, this study evaluates the OHRQoL of patients with chronic respiratory diseases. It was hypothesized that these patients would show a reduced OHRQoL.
Methods
This study was performed in full accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (17).
Patients, Intervention, Comparison, and Outcome (PICO) Question
The PICO question was as follows: “Do patients with severe respiratory diseases show a reduced OHRQoL?”. Thereby, “patients” were individuals with chronic respiratory diseases. The aspect “intervention” was not defined because it was expected to primarily include cross-sectional studies. “Comparison” was a healthy control group, if applicable. Otherwise, values should be compared to reference values or other groups of patients with systemic diseases. Finally, “outcome” was any applied OHRQoL measurement. The hypothesis was formed that the OHRQoL of patients with chronic respiratory diseases would be worse than in healthy individuals.
Eligibility Criteria
For inclusion in this study, several inclusion criteria were formulated:
- Publication until 30th of June, 2021.
- Examination of children or adults with a chronic respiratory disease or condition.
- Reporting of any OHRQoL measurement.
- Full text in English language.
Search Strategy
In July 2021, a systematic literature search was performed by two different and independent reviewers. As databases for literature search, the PubMed, Medline, Web of Science, and Scopus were chosen, using the search terms: “oral health-related quality of life” and respiratory disease or lung and “oral health-related quality of life.” A manual search based on the references of findings complemented the systematic literature search. All the findings were checked and screened for their eligibility.
Data Extraction
After all the articles were screened and checked, qualitative data extraction was applied. Thereby, different issues were extracted from the respective articles.
• Form of respiratory disease, year of publication, number of participants, study type, age, gender, and smoking.
• Presence and characteristics of a healthy control group.
• Oral health findings, if applicable.
• Oral HRQoL assessment including the form of measurement and results.
• Potential relationship between OHRQoL and general parameters, disease-related parameters, or oral health findings, if applicable.
• Subscales of the OHRQoL measurements, if applicable.
Two independent reviewers executed the whole process of systematic search and study selection as well as qualitative analysis. Only studies explicitly reporting OHRQoL of patients with chronic respiratory diseases were considered within this study.
Quality Assessment
The 11-item checklist from the Agency for Healthcare Research and Quality (AHRQ) for cross-sectional studies was applied for quality assessment of the included studies (18). The answers “no” or “unclear” were rated as 0 and the answer “yes” was rated as 1 point for each question to estimate a score for the respective quality of the studies. A sum score of all the questions of 0–3 indicated low quality, 4–7 indicated moderate quality, and a score of 8–11 indicated high quality of this study. The quality appraisal was conducted by two independent reviewers, whereby any disagreements were discussed and resolved in the whole author group.
Results
Search Findings
The PRISMA diagram, reflecting the findings of the systematic search, is given in Figure 1. Out of 44 database search findings, 26 full-text articles were assessed for their eligibility. During this, 19 articles were excluded (Supplementary Table 1). Finally, seven studies were included in the qualitative analysis.
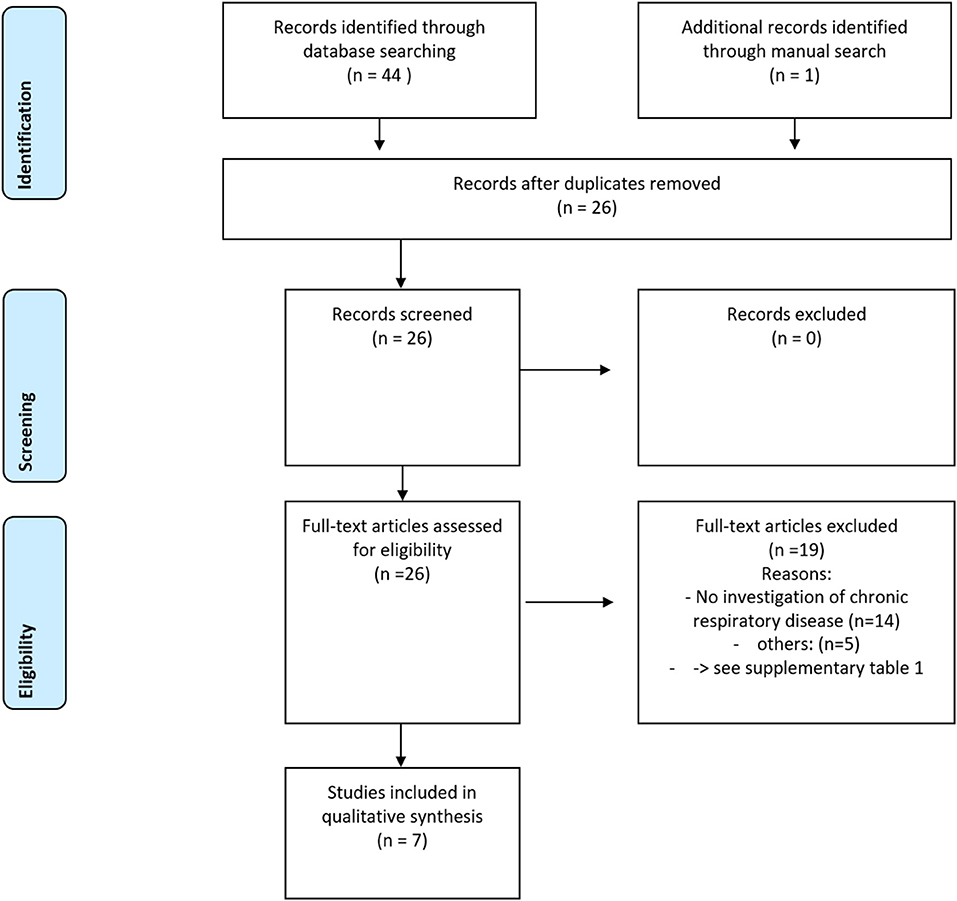
Figure 1. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram for the systematic review process in this study (17).
Characteristics of the Included Studies
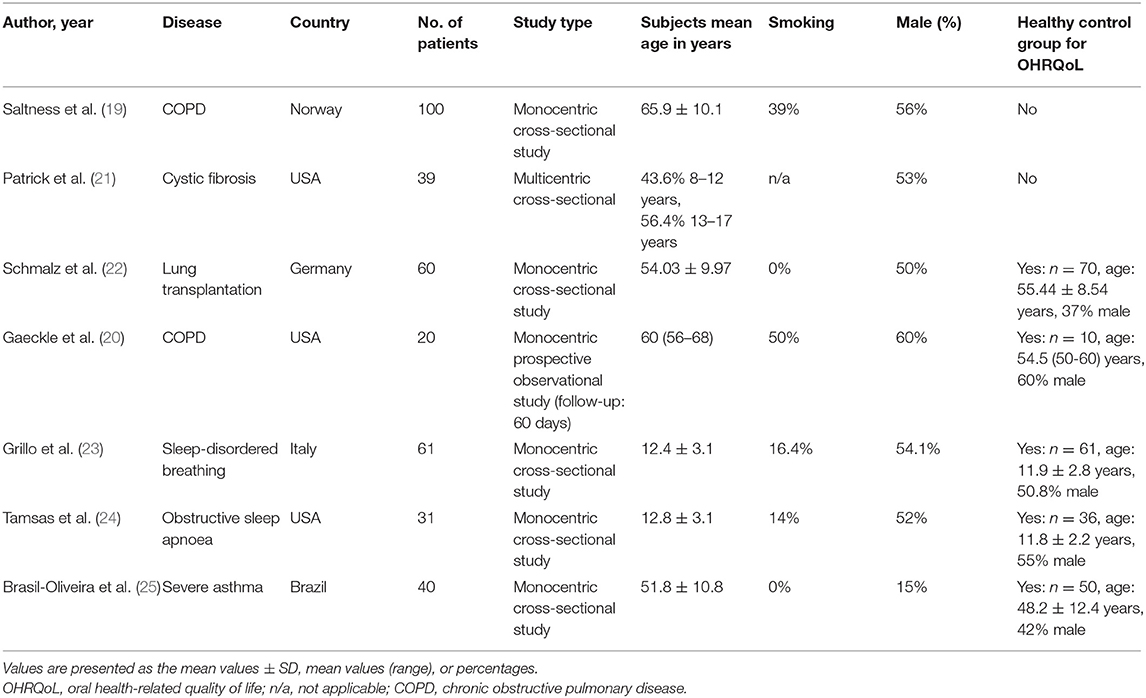
Out of the seven studies, two studies were on patients with COPD (19, 20), while each one study was on cystic fibrosis (21), lung transplantation (22), sleep-disordered breathing (23), obstructive sleep apnea (24), and severe asthma (25). Three studies were performed in children (21, 23, 24), while four studies were conducted in adult patients (19, 20, 22, 25). All the included studies had either a cross-sectional or an observational design. The healthy control group was examined in five of the included studies (20, 22–25). A full overview of the study characteristics is shown in Table 1.
Quality Assessment
Quality appraisal revealed that three studies were of high quality (19, 20, 23), while four studies were elevated with moderate quality (21, 22, 24, 25) according to the AHRQ criteria for cross-sectional studies (18) (Table 2).
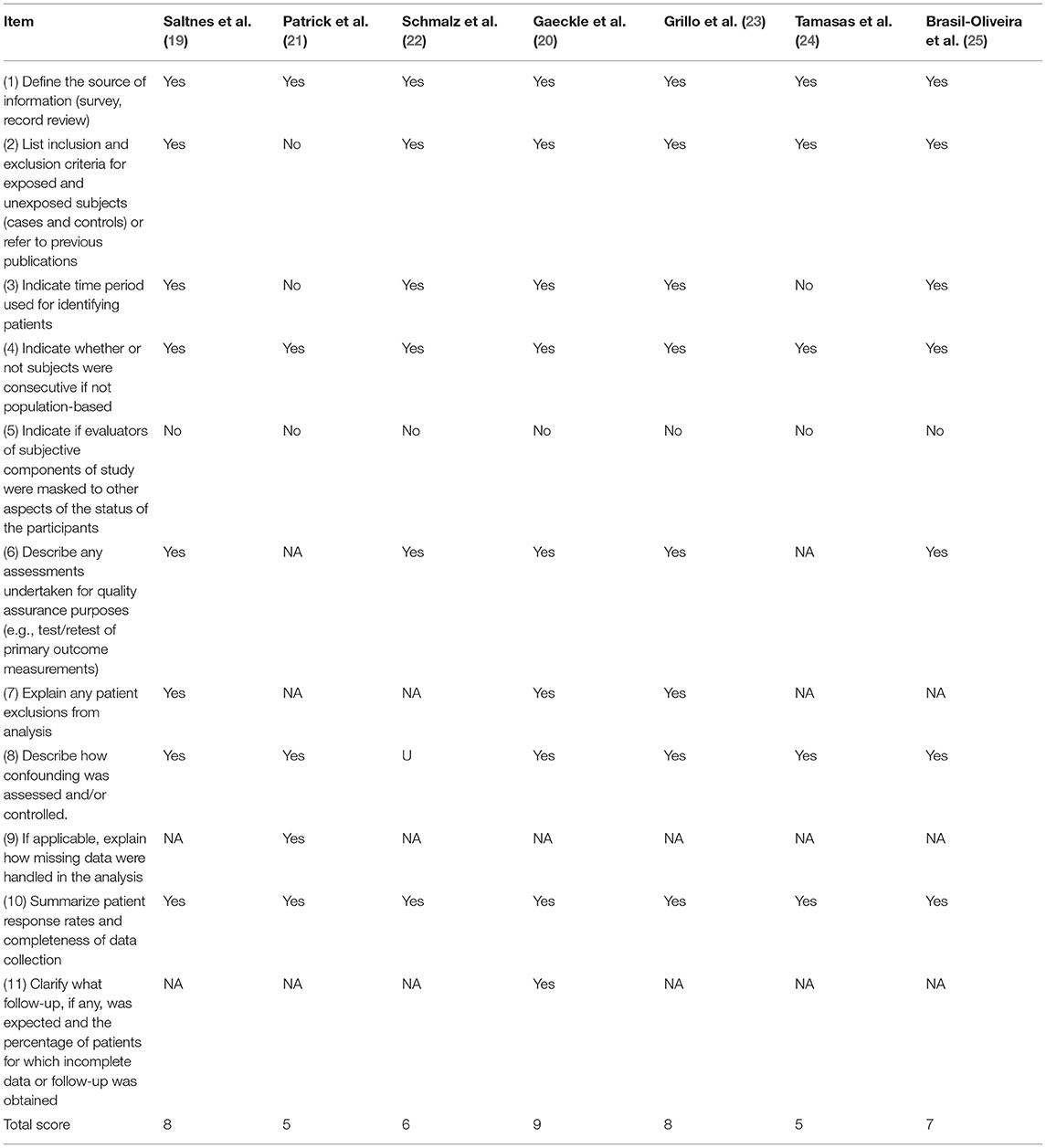
Table 2. Quality assessment of the included studies according to the Agency for Healthcare Research and Quality (ARHQ) (18).
Oral Health Records and Findings
Reporting of oral health data was not very comprehensive in the majority of included studies. One study did not report on any oral health conditions of the participants (21). The four studies including adults reported on remaining teeth (19, 20, 22, 25). Moreover, four studies reported on dental as well as periodontal conditions, whereby the assessment method was quite different (22–25). The detailed oral health findings, if applicable, are shown in Table 3.
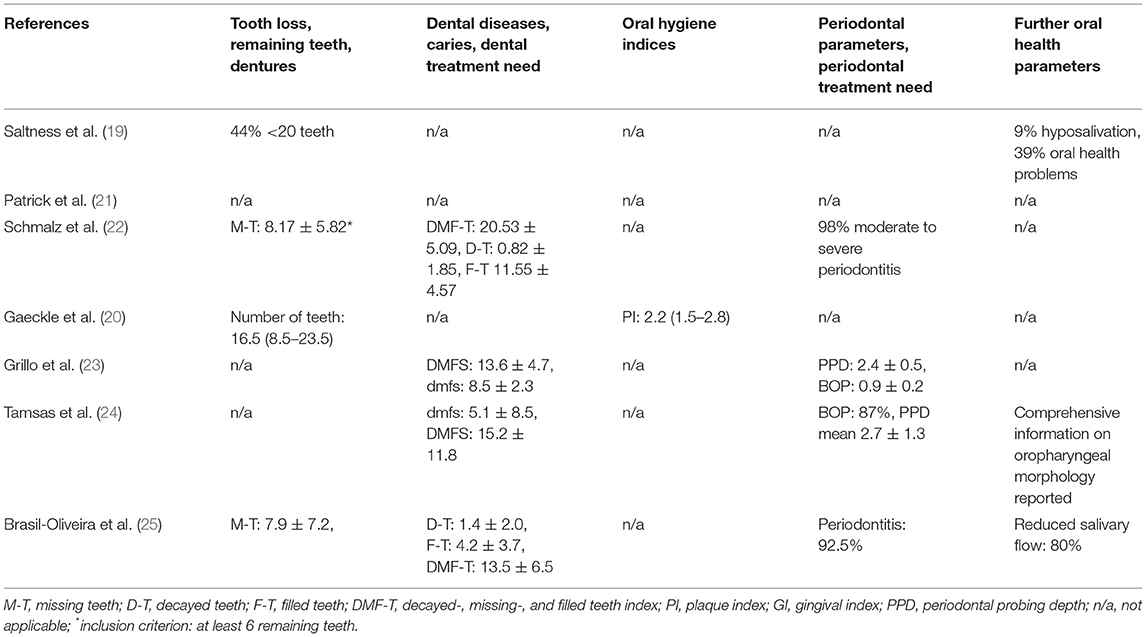
Table 3. Oral health parameters and respective main results if they presented as the mean values ± SD, means (range), or percentages in the included studies.
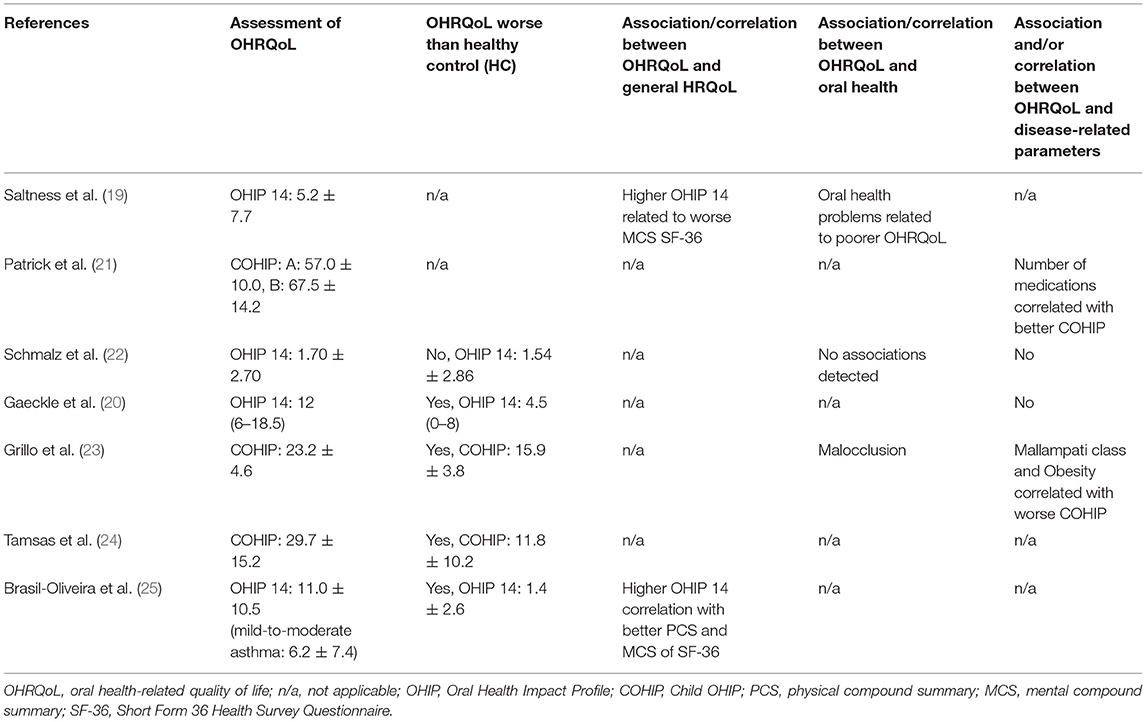
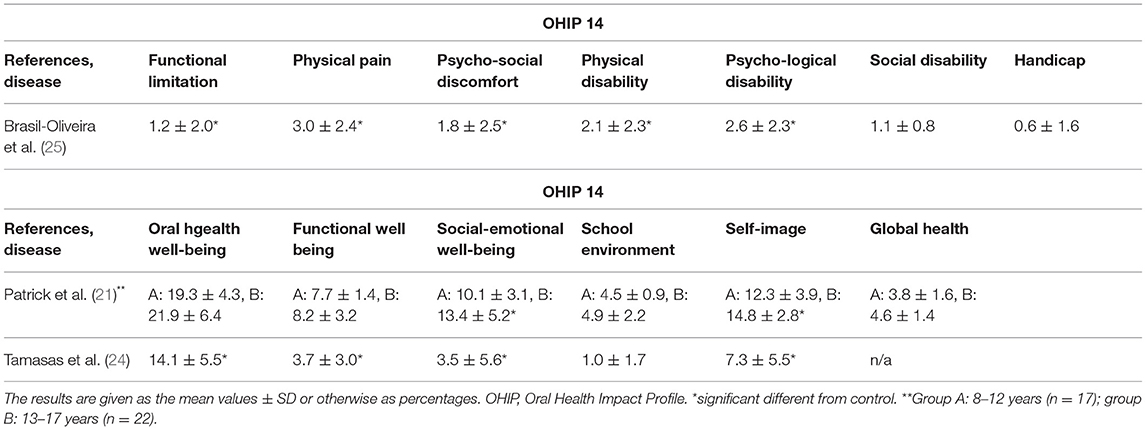
Oral Health-Related Quality of Life Measurements and Results
The four adult studies applied the Oral Health Impact Profile-14 (OHIP-14) for OHRQoL assessment, showing mean values between 1.7 and 12 points in sum scale (Figure 2) (19, 20, 22, 25). The three other studies applied the Child OHIP (COHIP), reporting average sum scores between 23.2 and 67.5 points (Figure 3) (21, 23, 24). Four studies (each two in children and adults) reported a worse OHRQoL in the respiratory disease compared to the healthy control group (20, 23–25), while only one study an adult lung transplant recipients did not show a difference against a healthy control (22). Associations between OHRQoL and HRQoL, disease-related parameters, or oral health conditions were rarely examined and reported, respectively (Table 4). Only one study examining adults (25) and two studies examining children (21, 24) reported on subscales of the OHIP-14 or the COHIP, respectively (Table 5).
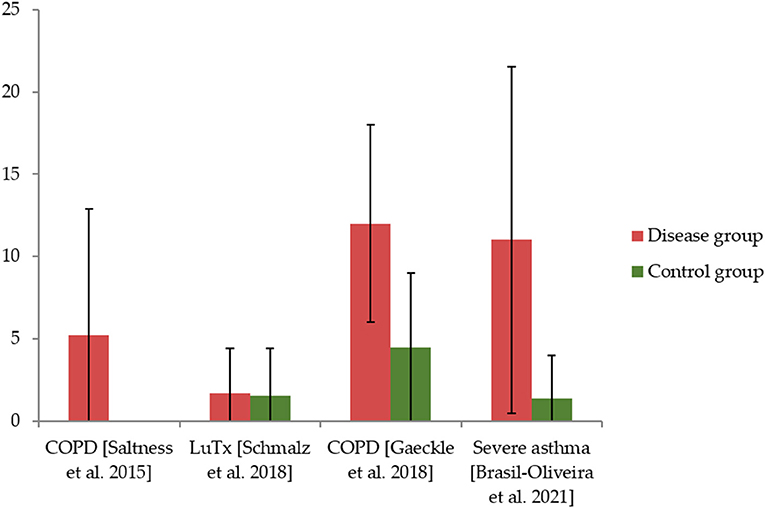
Figure 2. The Oral Health Impact Profile (OHIP) values of included studies on adults and values for healthy controls, if applicable.
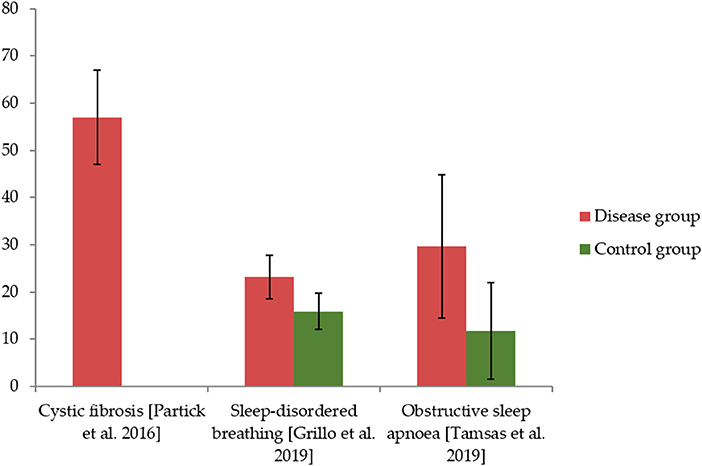
Figure 3. The Child OHIP (COHIP) values for children in included studies and of healthy controls, if applicable.
Discussion
This study hypothesized that patients with chronic respiratory diseases would show a reduced OHRQoL. Based on the findings of the literature search, this hypothesis can be confirmed, but several disease-specific and methodological issues need further discussion. Thereby, the following will provide: (I) an interpretation of the reduced OHRQoL in patients with chronic respiratory diseases in general and with respect to the different diseases, (II) a discussion of the applied methods alongside with (III) recommendations for further study in this field to strengthen the body of evidence and strive some clinical implications.
(I) Altogether, the OHRQoL of patients suffering from systemic diseases can be discussed controversially because several heterogeneous phenomena, depending on the form of the disease and/or therapy, exist. It is known that oral health can affect general HRQoL (26) and that reduced HRQoL can negatively affect OHRQoL (13, 27). Patients with severe chronic diseases or conditions, e.g., rheumatic diseases or hemodialysis show a reduced OHRQoL caused by their general disease burden including pain and impact on their daily life (15, 28). Thereby, the OHIP-14 values for patients with respiratory diseases in this study were similar as for rheumatic diseased patients or individuals undergoing renal replacement therapy (15, 28). Thus, the HRQoL impairment due to the general disease could be one reason for the reduced OHRQoL in this study; especially, severely diseased individuals with proceeded COPD, cystic fibrosis, and severe asthma are impaired in their everyday life and show affected HRQoL (29–31). Thereby, both severe symptoms, such as breathlessness, as well as mental health issues, such as anxiety or depression, can affect HRQoL outcomes (6, 31), potentially affecting OHRQoL of patients. A special position within this study is obstructive sleep apnea or sleep-disordered breathing, respectively. Although this is not an exclusive respiratory disease, it has been included in this study because it is a chronic condition affecting the respiratory system and is of high relevance for the dentist because oral health issues are common in these individuals (12). These sleep disorders lead to complex suffering of the patients, with an impairment of quality of life in both children and adults (12, 32). Furthermore, oral appliances for therapy or wearing an oxygen mask overnight could affect OHRQoL of respective individuals. Only one patient group, i.e., patients after lung transplantation, what rather represents a therapy than a respiratory disease, showed unaffected OHRQoL (22). It is known that patients after organ transplantation show a response shift, whereby oral health issues are pushed into the background because of the general disease burden (16, 33). While this is the reason for the unaffected OHRQoL of patients after lung transplantation, the other groups did not show this response shift phenomenon. A reasonable explanation for that appears the anatomic proximity between the airways and the oral cavity. Moreover, the association between oral diseases and the included respiratory conditions and/or the respective medication (7–12) could explain the affected OHRQoL. Altogether, the reduced OHRQoL of patients with chronic respiratory diseases appears expedient, but complex. However, the reporting of oral health conditions and HRQoL in the included studies was inconsistent. However, the association between COPD (19) and severe asthma (25) with HRQoL supports the upper mentioned interpretation. The affected OHRQoL of patients with chronic respiratory diseases appears of clinical significance because appropriate management of oral conditions of these systemically ill patients will be needed to positively affect their quality of life. Therefore, sufficient multidisciplinary dental care concepts might be needed, as already demanded for other groups of at-risk patients (15, 16, 28). Until now, there is no specific approach available for a respective dental care concept. It is known that a simple allocation to the dentist does not significantly decrease the dental treatment need of patients with severe general diseases (34). Moreover, respective patients need to receive psychosocial support and sensibilization within a multidisciplinary care concept (16). Therefore, it appears of high importance to apply an individualized, prevention-oriented, and patient-centered dental care concept, focusing on the risk and needs of respective patients (35).
(II) The included studies applied two different methods for OHRQoL assessment, according to the age of included participants. For adult patients, the short form of the OHIP-14 was chosen, which is a validated questionnaire-based tool (36, 37). This questionnaire allows assessing the OHRQoL by 14 different questions, which can be answered on a five-point scale between 0 and 4, where higher values indicate worse OHRQoL. As a patient-reported outcome, the OHRQoL is part of the evidence-based dentistry, and applying the OHIP-14 allows conclusions on the impairment of the domains, such as oral function, psychosocial impact, oral pain, and orofacial appearance (14, 38). Although the OHIP-14 is a validated and commonly used instrument, it is not specific for generally diseased individuals, what potentially limits this method in that case (15, 16, 28). The other measurement, which was applied for children, was the COHIP. This instrument is also validated and was found to present reliable results by the assessment of 34 items and five conceptually distinct subscales: oral health, functional well-being, social/emotional well-being, school environment, and self-image (39). Similar as for the OHIP-14, higher values represent a worse OHRQoL. Thereby, the assessment of the OHRQoL of children is difficult because children often have difficulties to express their concerns in clinical environments and they are largely influenced by socioenvironmental factors of their family and caregivers (40, 41). Although the COHIP findings perceived by the caregivers are sometimes reported, this was not considered in this study because it was aimed to exclusively display the perspective of patient. Within the included studies, the COHIP values between children and parents did not differ in a clinically relevant manner, so it seems reasonable to omit this issue in this study (23, 24). Accordingly, the applied OHRQoL measurement appears reasonable in the included studies, but the major flaw appears the rarely applied investigation on the relationship between OHRQoL and HRQoL, disease-related parameters, and, particularly, oral health.
(III) Some recommendations can be provided for future study in the field. The comprehensive assessment of oral health parameters and their consideration as an influential factor in patients with respiratory diseases would be helpful to evaluate this issue. Additionally, assessment of HRQoL alongside with disease-specific parameters as well as mental problems or conditions would help to gain a deeper understanding. Thereby, the different dimensions/subcategories of OHRQoL measurement should be addressed. Multicenter, prospective study designs, especially considering any dental or medical intervention, would also bring benefit to the understanding of OHRQoL and possibilities to its improvement in patients with respiratory diseases. Reference values and minimal important differences to interpret the clinical relevance of the data would also be of research interest in this study. Altogether, the body of evidence with respect to OHRQoL of patients with chronic respiratory diseases is quite weak, making more study in the field recommendable.
Strengths and Limitations
This is the first systematic study in this field. The methodology was sound, according to the PRISMA guidelines, and included a quality appraisal of the included studies. This quality appraisal revealed that the included studies were of moderate-to-high quality. The main points of criticism were missing blinding of examination and no consideration of any follow-up in most studies. Altogether, the included studies can be seen as of appropriate quality because the most relevant issues of quality appraisal were addressed by those investigations. The inclusion of such a heterogeneous combination of diseases and of children and adults together limits the comparability of findings. On one hand, the different diseases can cause different intra- and extraoral effects, potentially affecting OHRQoL of patients. For example, COPD and asthma are associated with periodontitis (7), while other included respiratory diseases are not associated with periodontitis. Periodontitis leads to reduced OHRQoL (42), what might be of relevance in the respective diseases, which are related to periodontal conditions. As this is just one potential example for the heterogeneity of the included diseases, the comparability of respective studies in this study is very limited. However, this study aimed to gain insight into the OHRQoL of patients with chronic respiratory diseases and not directly to compare the different diseases to each other. Similarly, the rationale for including children and adults together can be seen critically. Thereby, a direct comparison between the disease groups was not possible; but, due to the low number of studies on OHRQoL of the respective patient groups, it was decided to include studies on children, too. Of course, it is not possible to compare adults and children suffering from different respiratory diseases. To allow a comprehensive view on the OHRQoL of patients with chronic respiratory diseases, the inclusion appears reasonable, irrespective of the heterogeneity. Only seven studies were considered within this study, limiting the ability to draw meaningful conclusion. Moreover, the analysis was just qualitative. The low number of included studies is an important limitation, but is also an important result. The search terms were quite broad and a very comprehensive manual literature search was applied, checking the reference lists of all the included studies. Thereby, no additional findings could be detected. Therefore, this field of study appears understudied, yet, requiring an increased audience in the future. For this, this study provided several recommendations for future study in the field. More study will be necessary to gain insight into the OHRQoL of patients with respiratory diseases; this study can provide a basis for future study in the field.
Conclusion
Patients with chronic respiratory diseases show a reduced OHRQoL. This could be caused by a higher prevalence of oral diseases and underlying disease burden that need further clarification in future studies. An interdisciplinary dental care to support oral health and OHRQoL could be recommendable in individuals with chronic respiratory diseases.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author Contributions
SL, WN, and WW conceptualized the research, conducted a systematic review, analyzed and interpreted the results, and wrote the manuscript. DZ and AA participated in data analysis and interpretation and revised the manuscript. GS, JZ, SH, and HX administrated and supervised the whole research project. All the authors have read and approved the final version of the manuscript.
Funding
This work was funded by Science Research Cultivation Program of Stomatological Hospital, Southern Medical University [No. PY2020004 for SL (c2ltaW4ubGkuZGVudGlzdEBnbWFpbC5jb20=) and No.PY2021002 for WN (d2FuY2hlbm5pbmcwNjI3QGdtYWlsLmNvbQ==)].
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.757739/full#supplementary-material
References
1. Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. (2007) 370:765–73. doi: 10.1016/S0140-6736(07)61380-4
2. Ratjen F, Bell SC, Rowe SM, Goss CH, Quittner AL, Bush A. Cystic fibrosis. Nat Rev Dis Primers. (2015) 1:15010. doi: 10.1038/nrdp.2015.10
3. Stern J, Pier J, Litonjua AA. Asthma epidemiology and risk factors. Semin Immunopathol. (2020) 42:5–15. doi: 10.1007/s00281-020-00785-1
4. Lin J, Suurna M. Sleep Apnea and Sleep-Disordered Breathing. Otolaryngol Clin North Am. (2018) 51:827–33. doi: 10.1016/j.otc.2018.03.009
5. Booth S, Johnson MJ. Improving the quality of life of people with advanced respiratory disease and severe breathlessness. Breathe. (2019) 15:198–215. doi: 10.1183/20734735.0200-2019
6. Fiorentino G, Esquinas AM, Annunziata A. Exercise and chronic obstructive pulmonary disease (COPD). Adv Exp Med Biol. (2020) 1228:355–68. doi: 10.1007/978-981-15-1792-1_24
7. Gomes-Filho IS, Cruz SSD, Trindade SC, Passos-Soares JS, Carvalho-Filho PC, Figueiredo ACMG, et al. Periodontitis and respiratory diseases: A systematic review with meta-analysis. Oral Dis. (2020) 26:439–46. doi: 10.1111/odi.13228
8. Thomas MS, Parolia A, Kundabala M, Vikram M. Asthma and oral health: a review. Aust Dent J. (2010) 55:128–33. doi: 10.1111/j.1834-7819.2010.01226.x
9. Gani F, Caminati M, Bellavia F, Baroso A, Faccioni P, Pancera P, et al. Oral health in asthmatic patients: a review: asthma and its therapy may impact on oral health. Clin Mol Allergy. (2020) 18:22. doi: 10.1186/s12948-020-00137-2
10. Coffey N. O' Leary F, Burke F, Roberts A, Hayes M. Periodontal and oral health status of people with Cystic Fibrosis: a systematic review. J Dent. (2020) 103:103509. doi: 10.1016/j.jdent.2020.103509
11. Bansal M, Khatri M, Taneja V. Potential role of periodontal infection in respiratory diseases—a review. J Med Life. (2013) 6:244–8
12. Huynh NT, Emami E, Helman JI, Chervin RD. Interactions between sleep disorders and oral diseases. Oral Dis. (2014) 20:236–45. doi: 10.1111/odi.12152
13. Reissmann DR, John MT, Schierz O, Kriston L, Hinz A. Association between perceived oral and general health. J Dent. (2013) 41:581–9. doi: 10.1016/j.jdent.2013.05.007
14. Reissmann DR. Methodological considerations when measuring oral health-related quality of life. J Oral Rehabil. (2021) 48:233–45. doi: 10.1111/joor.12983
15. Schmalz G, Patschan S, Patschan D, Ziebolz D. Oral-health-related quality of life in adult patients with rheumatic diseases—a systematic review. J Clin Med. (2020) 9:1172. doi: 10.3390/jcm9041172
16. Schmalz G, Garbade J, Kollmar O, Ziebolz D. Does oral health-related quality of life of patients after solid organ transplantation indicate a response shift? Results of a systematic review. BMC Oral Health. (2020) 20:356. doi: 10.1186/s12903-020-01350-w
17. Moher D, Liberati A, Tetzlaff J, Altman DG The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1136/bmj.b2535
18. Rostom A, Dubé C, Cranney A, Saloojee N, Sy R, Garritty C, et al. Celiac disease. Evidence Reports/Technology Assessments, No. 104. Agency for Healthcare Research Quality (US) (2004). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK35156/ (accessed September 2004).
19. Saltnes SS, Storhaug K, Borge CR, Enmarker I, Willumsen T. Oral health-related quality-of-life and mental health in individuals with chronic obstructive pulmonary disease (COPD). Acta Odontol Scand. (2015) 73:14–20. doi: 10.3109/00016357.2014.935952
20. Gaeckle NT, Heyman B, Criner AJ, Criner GJ. Markers of dental health correlate with daily respiratory symptoms in COPD. Chronic Obstr Pulm Dis. (2018) 5:97–105. doi: 10.15326/jcopdf.5.2.2017.0159
21. Patrick JR, da Fonseca MA, Kaste LM, Fadavi S, Shah N, Sroussi H. Oral Health-related quality of life in pediatric patients with cystic fibrosis. Spec Care Dentist. (2016) 36:187–93. doi: 10.1111/scd.12162
22. Schmalz G, Wendorff H, Marcinkowski A, Weinreich G, Teschler H, Haak R, et al. Oral health related quality of life depending on oral health and specific factors in patients after lung transplantation. Clin Respir J. (2018) 12:731–7. doi: 10.1111/crj.12625
23. Grillo C, La Mantia I, Zappala G, Cocuzza S, Ciprandi G, Andaloro C. Oral health in children with sleep-disordered breathing: a cross-sectional study. Acta Biomed. (2019) 90(7-S):52–9. doi: 10.23750/abm.v90i7-S.8661
24. Tamasas B, Nelson T, Chen M. Oral health and oral health-related quality of life in children with obstructive sleep apnea. J Clin Sleep Med. (2019) 15:445–52. doi: 10.5664/jcsm.7672
25. Brasil-Oliveira R, Cruz ÁA, Souza-Machado A, Pinheiro GP, Inácio DDS, Sarmento VA, et al. Oral health-related quality of life in individuals with severe asthma. J Bras Pneumol. (2020) 47:e20200117. doi: 10.36416/1806-3756/e20200117
26. Haag DG, Peres KG, Balasubramanian M, Brennan DS. Oral conditions and health-related quality of life: a systematic review. J Dent Res. (2017) 96:864–74. doi: 10.1177/0022034517709737
27. Sischo L, Broder HL. Oral health-related quality of life: what, why, how, and future implications. J Dent Res. (2011) 90:1264–70. doi: 10.1177/0022034511399918
28. Schmalz G, Patschan S, Patschan D, Ziebolz D. Oral health-related quality of life in adult patients with end-stage kidney diseases undergoing renal replacement therapy—a systematic review. BMC Nephrol. (2020) 21:154. doi: 10.1186/s12882-020-01824-7
29. Hodkinson A, Bower P, Grigoroglou C, Zghebi SS, Pinnock H, Kontopantelis E, et al. Self-management interventions to reduce healthcare use and improve quality of life among patients with asthma: systematic review and network meta-analysis. BMJ. (2020) 370:m2521. doi: 10.1136/bmj.m2521
30. Akinci B, Aslan GK, Kiyan E. Sleep quality and quality of life in patients with moderate to very severe chronic obstructive pulmonary disease. Clin Respir J. (2018) 12:1739–46. doi: 10.1111/crj.12738
31. Cronly JA, Duff AJ, Riekert KA, Fitzgerald AP, Perry IJ, Lehane EA, et al. Health-related quality of life in adolescents and adults with cystic fibrosis: physical and mental health predictors. Respir Care. (2019) 64:406–15. doi: 10.4187/respcare.06356
32. Pauletto P, Réus JC, Bolan M, Massignan C, Flores-Mir C, Maia I, et al. Association between obstructive sleep apnea and health-related quality of life in untreated adults: a systematic review. Sleep Breath. (2021) 11:1–7. doi: 10.1007/s11325-021-02323-1
33. Schmalz G, Garbade J, Sommerwerck U, Kollmar O, Ziebolz D. Oral health-related quality of life of patients after solid organ transplantation is not affected by oral conditions: results of a multicentre cross-sectional study. Med Oral Patol Oral Cir Bucal. (2021) 26:e437–44. doi: 10.4317/medoral.24277
34. Ziebolz D, Friedrich S, Binner C, Rast J, Eisner M, Wagner J, et al. Lack in Periodontal Care of Patients Suffering from Severe Heart Diseases-Results after 12 Months Follow-Up. J Clin Med. (2020) 9:352. doi: 10.3390/jcm9020352
35. Schmalz G, Ziebolz D. Changing the Focus to the Whole Patient instead of One Oral Disease: The Concept of Individualized Prevention. Adv Prev Med. (2020) 2020:6752342. doi: 10.1155/2020/6752342
36. Slade GD, Spencer AJ. Development and evaluation of the oral health impact profile. Community Dent Health. (1994) 11:3–11.
37. Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. (1997) 25:284–90. doi: 10.1111/j.1600-0528.1997.tb00941.x
38. John MT, Rener-Sitar K, Baba K, Celebić A, Larsson P, Szabo G, et al. Patterns of impaired oral health-related quality of life dimensions. J Oral Rehabil. (2016) 43:519–27. doi: 10.1111/joor.12396
39. Broder HL, McGrath C, Cisneros GJ. Questionnaire development: face validity and item impact testing of the Child Oral Health Impact Profile. Community Dent Oral Epidemiol. (2007) 35 Suppl 1:8–19. doi: 10.1111/j.1600-0528.2007.00401.x
40. de Paula JS, Ambrosano GM, Mialhe FL. Oral Disorders, Socioenvironmental Factors and Subjective Perception Impact on Children's School Performance. Oral Health Prev Dent. (2015) 13:219–26. doi: 10.3290/j.ohpd.a32672
41. Scott JM, Gadbury-Amyot CC, Hoffman AM, Simmer-Beck ML. Associations of self-reported oral health quality of life with actual oral health status in children. J Dent Hyg. (2021) 95:57–66.
Keywords: oral health, oral health-related quality of life, respiratory disease, lung, COPD
Citation: Li S, Ning W, Wang W, Ziebolz D, Acharya A, Schmalz G, Zhao J, Huang S and Xiao H (2022) Oral Health-Related Quality of Life in Patients With Chronic Respiratory Diseases—Results of a Systematic Review. Front. Med. 8:757739. doi: 10.3389/fmed.2021.757739
Received: 12 August 2021; Accepted: 13 December 2021;
Published: 12 January 2022.
Edited by:
Kin-fai Ho, The Chinese University of Hong Kong, ChinaReviewed by:
Vinay Jain, University of Tennessee Health Science Center (UTHSC), United StatesJingjing Luo, Sichuan University, China
Copyright © 2022 Li, Ning, Wang, Ziebolz, Acharya, Schmalz, Zhao, Huang and Xiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shaohong Huang, aHNoLmNoaW5hQHRvbS5jb216; Jianjiang Zhao, empqMjUyMUBzaW5hLmNvbQ==; Hui Xiao, enptbXhoQDEyNi5jb20=
†These authors share first authorship
‡These authors share senior authorship
 Simin Li
Simin Li Wanchen Ning
Wanchen Ning Wei Wang1†
Wei Wang1† Dirk Ziebolz
Dirk Ziebolz Aneesha Acharya
Aneesha Acharya Gerhard Schmalz
Gerhard Schmalz Jianjiang Zhao
Jianjiang Zhao