- 1Department of Critical Care Medicine, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Peking Union Medical College, Chinese Academy of Medical Science, Beijing, China
- 2Department of Critical Care Medicine, Beijing Jishuitan Hospital, Beijing, China
Objectives: This study aimed to investigate the effect of nurse-led, goal-directed lung physiotherapy (GDLPT) on the prognosis of older patients with sepsis caused by pneumonia in the intensive care unit.
Methods: We conducted a prospective, two-phase (before-and-after) study over 3 years called the GDLPT study. All patients received standard lung therapy for sepsis caused by pneumonia and patients in phase 2 also received GDLPT. In this study, 253 older patients (age ≥ 65 years) with sepsis and pneumonia were retrospectively analyzed. The main outcome was 28 day mortality.
Results: Among 742 patients with sepsis, 253 older patients with pneumonia were divided into the control group and the treatment group. Patients in the treatment group had a significantly shorter duration of mechanical ventilation [5 (4, 6) vs. 5 (4, 8) days; P = 0.045], and a lower risk of intensive care unit (ICU) mortality [14.5% (24/166) vs. 28.7% (25/87); P = 0.008] and 28 day mortality [15.1% (25/166) vs. 31% (27/87); P = 0.005] compared with those in the control group. GDLPT was an independent risk factor for 28 day mortality [odds ratio (OR), 0.379; 95% confidence interval (CI), 0.187–0.766; P = 0.007].
Conclusions: Nurse-led GDLPT shortens the duration of mechanical ventilation, decreases ICU and 28-day mortality, and improves the prognosis of older patients with sepsis and pneumonia in the ICU.
Introduction
Aging of the population is a critical worldwide trend. The proportion of individuals older than 60 years has tripled over the last 50 years and will triple again before 2050. This aging has major consequences on the health system, including the intensive care unit (ICU). In the USA, almost half (48.7%) of the patients admitted to an ICU are aged 65 years or older, and patients aged 85 years or older account for 7 to 25% of the admission rate (1, 2). The rate of pneumonia increases rapidly with age. Approximately 19% of adults hospitalized with pneumonia have an ICU admission, including 60.7% of patients aged 65 years or older (3). Pneumonia in older patients can lead to cardiopulmonary failure, sepsis, and even systemic multiple organ failure, and they have a high mortality rate (4). Older people with pneumonia are at risk for a longer hospital stay, extended antibiotic therapy, and higher healthcare costs (5, 6). Therefore, an appropriate treatment protocol for pneumonia in older patients needs to be determined.
Because of age-related changes in the body, comorbidity, and malnutrition, the onset of pneumonia is insidious, rapid, and critical, and clinical treatment is difficult in older patients (2, 7, 8). Lung physiotherapy plays an important role in treatment of older patients with pneumonia (2, 7, 8). Lung physiotherapy can help patients in reducing the accumulation of airway secretion, clearing the respiratory tract, preventing a collapsed lung, improving lung compliance, and reducing comorbidities (9, 10). Nurses are responsible for most respiratory treatment in China. However, there is little evidence for the effect of nurse-led GDLPT on the prognosis of pneumonia in older patients with sepsis. In a previous study, we found that nurse-led GDLPT improved the outcomes in patients with sepsis and pneumonia (11). In this study, we carried out a retrospective analysis of older patients (age ≥ 65 years) with sepsis and pneumonia to evaluate whether GDLPT affects the clinical outcome.
Materials and Methods
Study Design and Patients
The GDLPT study was a prospective, two-phase (before-and-after) study conducted in Peking Union Medical College Hospital of China from January 2017 to January 2020. Details of this study, including the inclusion and exclusion criteria, have been published previously (11). The study period was divided into two stages of phase 1 and phase 2. During phase 1 (January to December 2017), patients received standard physiotherapy for pneumonia, and patients in phase 2 (February 2018 to January 2020) also received GDLPT. The two study periods were separated by a 1 month washout period that was dedicated to teaching the GDLPT protocol to all nursing and medical staff. The study protocol was approved by the ethics committee of Peking Union Medical College Hospital (approval number: JS-1170). All family members agreed to participating in the study and signed an informed consent form, and the study was registered at chictr.org.cn (identifier: ChiCTR-ROC-17010750).
Figure 1 shows a flow diagram of patient screening and selection for this study. In the nurse-led GDLPT study, 609 of 742 patients were diagnosed with sepsis caused by pneumonia, of whom 253 (41.5%) were older than 65 years. Demographics, comorbidities, clinical parameters, and laboratory data were analyzed.
Intervention and Comparisons
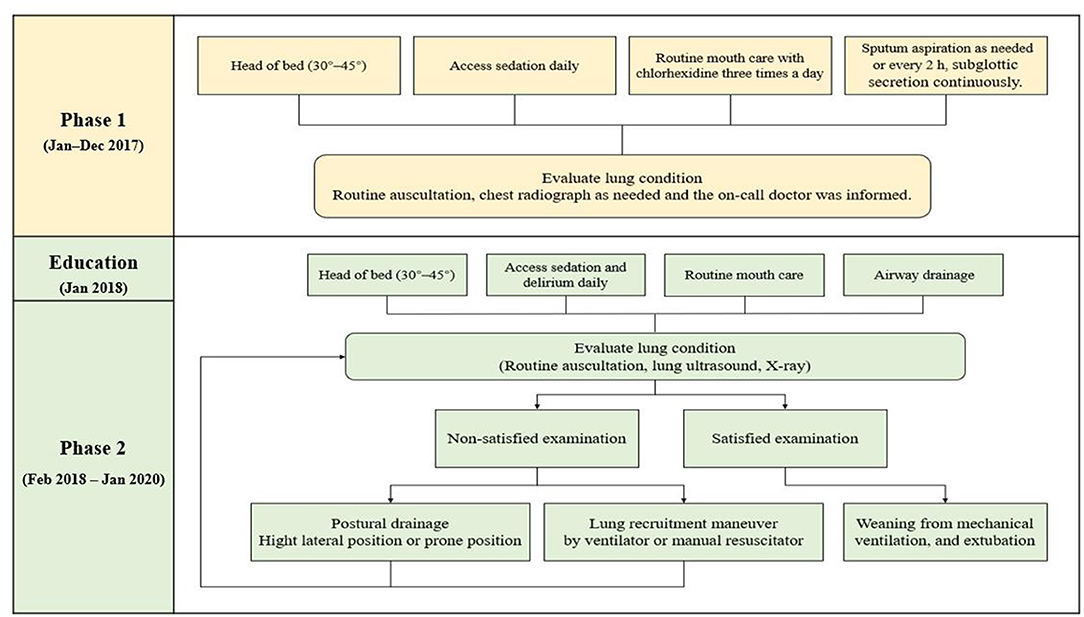
The protocols for pneumonia in the pre- and post-protocol groups are shown in Figure 2. Details of this study, including study details such as the intervention objective, methods, and intervention frequency, were the same as those in our previous study (11). The Supplementary File provides additional evidence relevant to the intervention and comparisons.
Data Collection
Baseline data of the patients, including sex, age, underlying diseases, the Sequential Organ Failure Assessment (SOFA) score, the Acute Physiology and Chronic Health Evaluation (APACHE) II score, and the Clinical Pulmonary Infection Score (CPIS), were analyzed. Vital signs, laboratory parameters, arterial blood gases, ventilatory parameters, life-sustaining treatments, and infection-related data during admission were also included. The data used in this study were the worst values in the first 24 h after ICU admission. The primary outcomes of this study were 28 day mortality. The secondary outcomes were the duration of ventilation, the length of the ICU stay, and the ICU mortality rate.
Statistical Analysis
Data were analyzed by IBM SPSS version 21.0 (IBM Corp., Armonk, NY, USA). The frequency and percentage and mean and standard deviation were calculated for descriptive statistics. Bivariate analysis was performed using the chi-square test for categorical variables and the t test or one-way analysis of variance for continuous variables. Logistic regression analysis was performed with 28 day mortality as the dependent factor, which was significant (p < 0.2) in univariate analysis.
Results
Baseline Characteristics
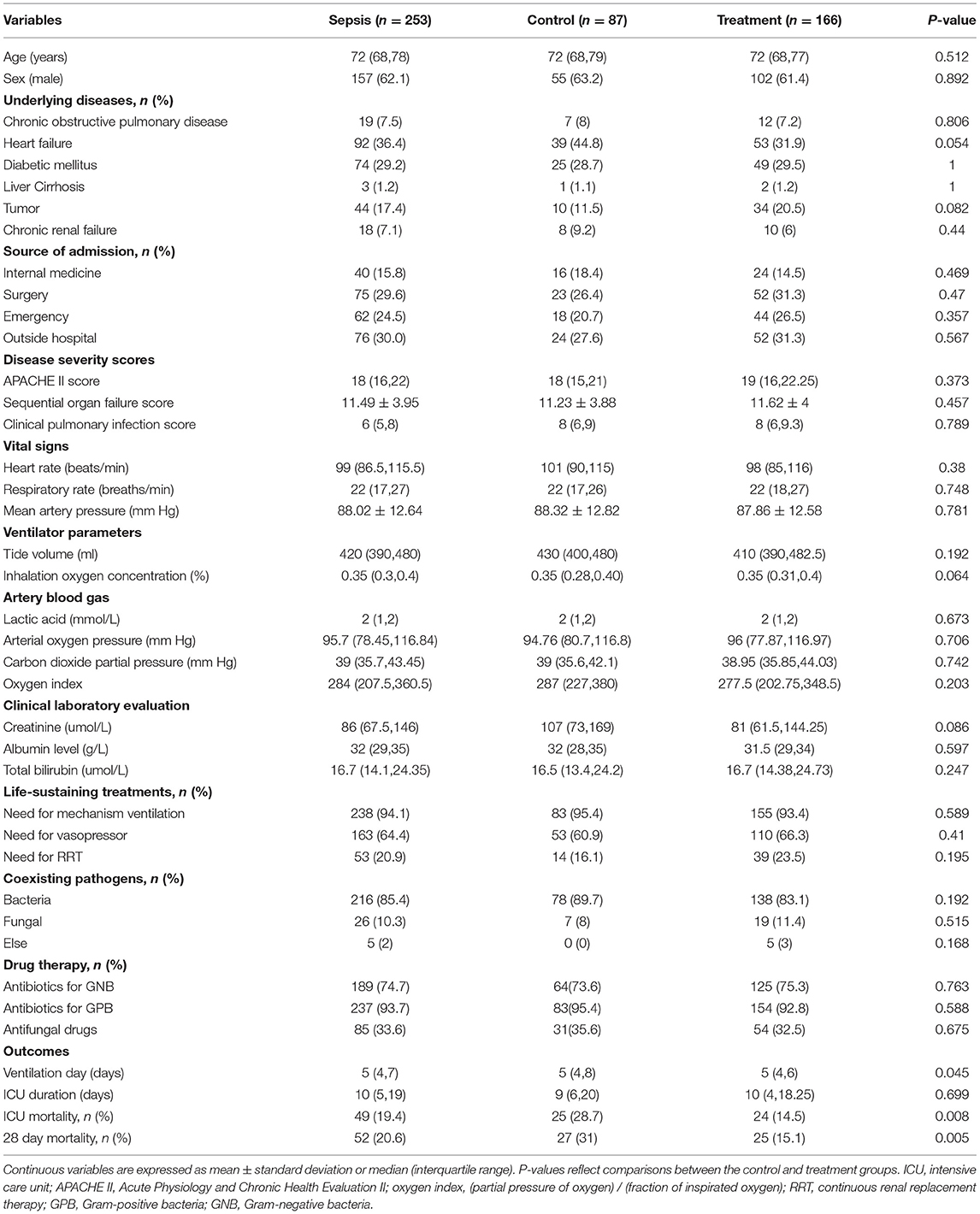
Among 742 patients with sepsis, 253 patients who were older than 65 years were included in this study. Table 1 shows the clinical characteristics of the patients who were enrolled in this study. The median age of the patients was 72 years (interquartile range: 68–78 years) and 62.1% (157/253) were men. At admission to the ICU, the mean SOFA score was 11.49 ± 3.95, the median APACHE II score was 18 (12–18), and the median CPIS score was 6 (5–8). Ninety-two (36.4%) patients had heart failure, 19 (7.5%) had chronic obstructive pulmonary disease, 74 (29.2%) had diabetes mellitus, 3 (1.2%) had liver cirrhosis, 44(17.4%) with tumors, and 18 (7.1%) had chronic renal failure. There were no significant differences in age, sex, underlying diseases, source of admission, disease severity scores (APACHE II, SOFA, and CPIS scores), vital signs (heart rate, respiratory rate, and mean arterial pressure), ventilatory parameters, arterial blood gases, clinical laboratory evaluation, life-sustaining treatments, coexisting pathogens, or drug therapy between the two groups after ICU admission.
There was no significant difference in the ICU duration between the groups. Patients in the treatment group had a significantly shorter duration of mechanical ventilation [5 (4, 6) vs. 5 (4, 8) days, P = 0.045], and a lower ICU mortality [14.5% (24/166) vs. 28.7% (25/87); P = 0.008] and 28 day mortality [15.1% (25/166) vs. 31% (27/87); P = 0.005] compared with those in the control group.
Clinical Differences Between Survivors and Non-survivors
The clinical characteristics of all patients and for survivors and non-survivors (28 day) are shown in Table 2. Non-survivors had a higher APACHE II score, higher CPIS score, faster respiratory rate, higher carbon dioxide partial pressure on ICU admission, and longer mechanical ventilation compared with survivors (all P < 0.05). The rates of heart failure and chronic renal failure were significantly higher in non-survivors than in survivors (both P < 0.05). The requirement for renal replacement therapy was significantly more frequent in the in non-survivors compared with survivors (32.7 vs. 17.9%, P = 0.034). Importantly, more patients received nurse-led GDLPT in survivors than in non-survivors (70.1 vs. 48.1%, P = 0.005).
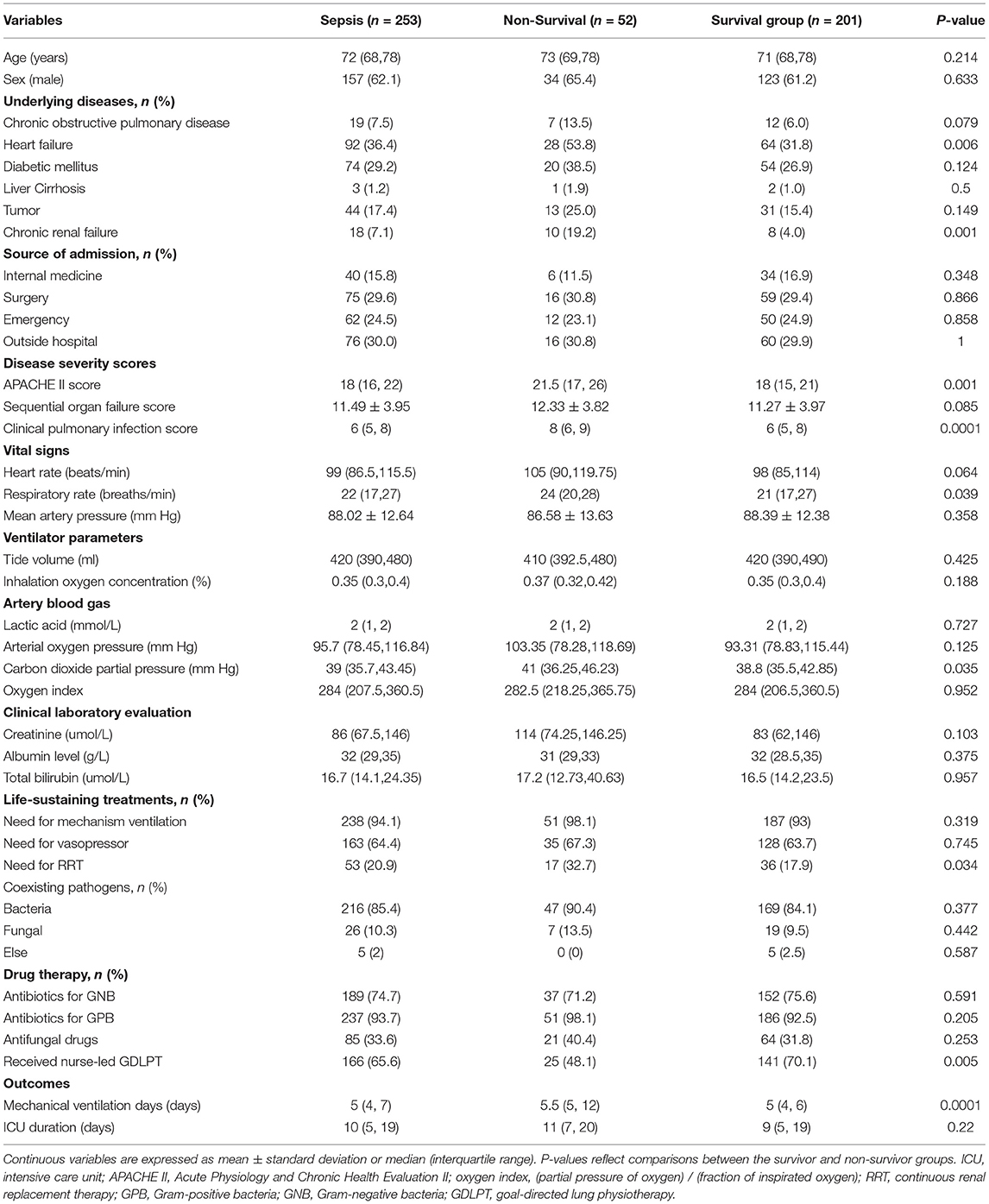
Table 2. Characteristics of the study population in survivors and non-survivors according to 28 day mortality.
Risk Factors for 28 Day Mortality in Older Patients With Sepsis Caused by Pneumonia
Multivariate logistic regression analysis identified five factors that independently predicted 28-day mortality in patients with sepsis who were diagnosed with pneumonia. These factors were nurse-led GDLPT [odds ratio (OR), 0.379; 95% confidence interval (CI), 0.187–0.766; P = 0.007], heart failure (OR, 2.779; 95% CI, 1.360–5.679; P = 0.005), tumor (OR, 2.825; 95% CI, 1.181–6.757; P = 0.02), need for renal replacement therapy (OR, 2.450; 95% CI, 1.122–5.351; P = 0.025), and mechanical ventilation days (OR, 1.147; 95% CI, 1.055–1.247; P = 0.001). GDLPT was a protective factor for 28 day mortality (Table 3).
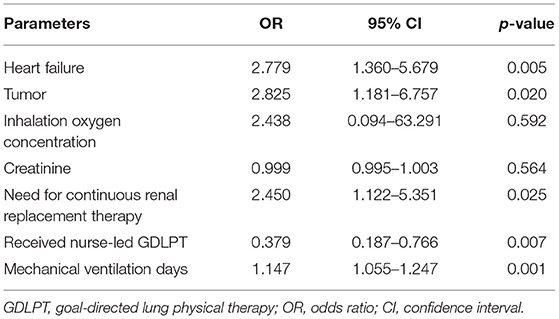
Table 3. Multivariate logistic regression analysis for predicting 28 day mortality in older patients with sepsis and pneumonia.
Discussion
Pneumonia is frequently encountered in older patients admitted to the ICU, with an incidence rate of >60% in those with sepsis (6). In numerous clinical studies, lung physiotherapy was analyzed in patients with various critical diseases (12, 13, 19). However, little is known about nurses providing lung physiotherapy to older patients with sepsis and pneumonia. Furthermore, the effect of lung physiotherapy on the prognosis of these patients is unclear. In this study, we found that nurse-led GLDPT was associated with shorter ventilation days, and reduced ICU mortality and 28 day mortality rates.
With aging, there are significant changes in the anatomical and physiological function of the lungs. Older people are more likely to develop pulmonary complications and underlying diseases, including COPD, aspiration, pneumonia, tumor, heart failure, chronic renal failure, and have a poor prognosis (14). The GDLPT protocol has several advantages over conventional physiotherapy. One advantage is that the frequency of oral care is determined by the Beck Oral Assessment Scale score and mucosal-plaque score. Another advantage is that enhancement of airway drainage is conducted every 4 h for 20 to 30 min each time, with a vibration frequency of 20 to 30 Hz. Additionally, the cough strength is evaluated every 6 h. Older people with a weak cough are more likely to have nosocomial pneumonia and aspiration pneumonia (15). In the USA, the incidence of aspiration pneumonia in older patients is 30.9 cases per 10,000 people, which is twice that in patients aged <65 years (16). A further advantage is that airway humidification is evaluated regularly to maintain humidification at degree II (17). For patients with specific pulmonary consolidation, goal-directed patient positioning is actively used. The frequency of turning over is adjusted, and a lung recruitment maneuver is also performed through mechanical ventilation or a manual resuscitator. Therefore, as a non-invasive intervention strategy, nurse-led GDLPT is useful for older patients with pneumonia.
In this nurse-led GDLPT study, pain assessment, delirium assessment, and active early activities were carried out every 6 h by nurses. Delirium varies from 11 to 42% in older patients and has adverse outcomes and high health care costs (18). Up to 60% of delirious patients were unrecognized unless actively screened, and sedative medications and deeper sedation are associated with the development of delirium (20). According to the patient's delirium status, early activities were carried out, such as sitting at the wheel and early walking. Frailty in older patients is also a risk of a longer ICU stay, prolonged ventilation duration, and increased mortality. Early exercise is the most effective intervention for debilitating syndrome and significantly improves muscle strength. In this nurse-led GDLPT study, old patients without delirium were able to get out of bed into a wheelchair early or walk early after therapy. Additionally, patients with intermittent delirium were able to perform bedside wheelchair activity, and patients with continuous delirium were able to receive passive movement in bed or sitting upon the bed. The nurse-led GDLPT protocol was formulated in the critical clinical setting and designed using more than 20 years of clinical experience, with specific items and strong operability. This therapy enabled good management of older patients.
In this study, nurse-led GDLPT significantly shortened the duration of ventilation. Prolonged mechanical ventilation might result in an increased incidence of ventilator-associated pneumonia, which is clinically meaningful, especially for older patients with pneumonia. A high frequency of antibiotic use and antibiotic resistance in patients is caused by ventilator-associated pneumonia. The prevalence of multidrug resistance is increasing, and ventilator-associated pneumonia caused by multidrug resistance is often fatal in the ICU (21). Several factors such as the CPIS score, and the APACHE II score contribute to a high percentage of multidrug resistance in the ICU and are important reasons for the poor prognosis of older patients with sepsis and pneumonia (22).
At present, older patients with a critical illness are frequently admitted in the ICU. However, data on older patients with pneumonia are relatively rare, and there have been few evidence-based medical reports (23). This study was a retrospective analysis based on data from a previous nurse-led GDLPT study. All collected data, including vital signs, ventilatory parameters, and laboratory indicators, were obtained from electronic information systems. Data were double checked to minimize the risk of data entry errors and there were missing data. Therefore, prospective, randomized, controlled trials are required to further investigate the role of nurse-led GDLPT on older patients with pneumonia. The nurse-led GDLPT study was a prospective, before-and-after study in a single center. Therefore, a multicenter study needs to be performed to further examine the details of GDLPT and validate its wide applicability in older patients with pneumonia.
Conclusions
Managing pneumonia in critically ill older patients is a complex issue. Aging, comorbidities, frailty, and other factors in older patients significantly increase the management requirements and risks for those with critical illness. Nurse-led GDLPT significantly shortens the duration of ventilation and improves the 28 day mortality rate in older patients with sepsis and pneumonia. Nurse-led GDLPT is a new clinical intervention for the refined management of older patients with pneumonia, and it promotes the recovery of older patients with severe pneumonia.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of Peking Union Medical College Hospital (No. JS-1170). The study was registered at chictr.org.cn (identifier: ChiCTR1900025850). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
NC, QL, HW, and JS contributed to the conception of the study, data interpretation, and drafted the manuscript. WH, HL, and MZ contributed to the data collection and data analysis. WC and ZL contributed to data collection and interpretation and critically revised the manuscript for important intellectual content. All authors approved the final version of the manuscript.
Funding
The work was supported by National Natural Science Foundation of China (No. 82072226), Beijing Municipal Science and Technology Commission (No. Z201100005520049), Fundamental Research Funds for the Central Universities (No. 3332021018), Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (No. 2019XK320040), Tibet Natural Science Foundation (No. XZ2019ZR-ZY12(Z)), and Excellence Program of Key Clinical Specialty of Beijing in 2020 (No. ZK128001).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.753620/full#supplementary-material
References
1. Fuchs L, Chronaki CE, Park S, Novack V, Baumfeld Y, Scott D. S. ICU admission characteristics and mortality rates among elderly and very elderly patients. Intensive Care Med. (2012) 38:1654–61. doi: 10.1007/s00134-012-2629-6
2. Esme M, Topeli A, Yavuz BB, Akova M. Infections in the elderly critically-Ill patients. Front Med. (2019) 6:118. doi: 10.3389/fmed.2019.00118
3. Storms AD, Chen J, Jackson LA, Nordin JD, Naleway AL, Glanz JM, et al. Rates and risk factors associated with hospitalization for pneumonia with ICU admission among adults. BMC Pulm Med. (2017) 17:208. doi: 10.1186/s12890-017-0552-x
4. Corrales-Medina VF, Musher DM, Shachkina S, Chirinos JA. Acute pneumonia and the cardiovascular system. Lancet. (2013) 381:496–505. doi: 10.1016/S0140-6736(12)61266-5
5. Restrepo MI, Faverio P, Anzueto A. Long-term prognosis in community-acquired pneumonia. Curr Opin Infect Dis. (2013) 26:151–8. doi: 10.1097/QCO.0b013e32835ebc6d
6. Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA. (2009) 302:2323–9. doi: 10.1001/jama.2009.1754
7. Dyer C, Pugh L. Lung health in older adults. Age Ageing. (2019) 48:319–22. doi: 10.1093/ageing/afz008
8. Valley TS, Sjoding MW, Ryan AM, Iwashyna TJ, Cooke CR. Association of intensive care unit admission with mortality among older patients with pneumonia. JAMA. (2015) 314:1272–9. doi: 10.1001/jama.2015.11068
9. Belli S, Prince I, Savio G, Paracchini E, Cattaneo D, Bianchi M, et al. Airway clearance techniques: the right choice for the right patient. Frontiers in medicine. (2021) 8:544826–544826. doi: 10.3389/fmed.2021.544826
10. Wang TH, Wu CP, Wang LY. Chest physiotherapy with early mobilization may improve extubation outcome in critically ill patients in the intensive care units. Clin Respir J. (2018) 12:2613–21. doi: 10.1111/crj.12965
11. Sun J, Han W, Cui N, Li Q, Wang H, Li Z, et al. Effect of nurse-led goal-directed lung physical therapy on the prognosis of pneumonia in sepsis patients in the icu: a prospective cohort study. J Intensive Care Med. (2021). doi: 10.1177./0885066620987200. [Epub ahead of print].
12. Newman A, Gravesande J, Rotella S, Wu SS, Topp-Nguyen N, Kho ME, et al. Physiotherapy in the neurotrauma intensive care unit: a scoping review. J Crit Care. (2018) 48:390–406. doi: 10.1016/j.jcrc.09, 037.
13. Battaglini D, Robba C, Caiffa S, Ball L, Brunetti I, Loconte M, et al. Chest physiotherapy: an important adjuvant in critically ill mechanically ventilated patients with COVID-19. Respir Physiol Neurobiol. (2020) 282:103529. doi: 10.1016/j.resp.2020.103529
14. Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging. (2006) 1:253–60. doi: 10.2147/ciia.1, 3.253
15. Torres A, Gatell JM, Aznar E, El-Ebiary M, Puig DLBJ, González J, et al. Re-intubation increases the risk of nosocomial pneumonia in patients needing mechanical ventilation. Am J Respir Crit Care Med. (1995) 152:137–41. doi: 10.1164/ajrccm.152.1.7599812
16. Wu CP, Chen YW, Wang MJ, Pinelis E. National trends in admission for aspiration pneumonia in the United States, 2002-2012. Ann Am Thorac Soc. (2017) 14:874–9. doi: 10.1513/AnnalsATS.201611-867OC
17. Yang M, Song Y, Pan L, Xie X. Evaluation of the effect of two active warming and humidifying high-flow oxygen therapy systems in patients with tracheotomy. Biomed Rep. (2019) 11:31–7. doi: 10.3892/br.2019.1219
18. Li D, Zhang J, Bai G, Chen J, Cheng W, Cui N. Lymphocyte and NK cell counts can predict sepsis-associated delirium in elderly patients. Front Aging Neurosci. (2021) 12:621298–621298. doi: 10.3389/fnagi.2020.621298
19. Do ABM, Timenetsky K. Chest physiotherapy and outcomes in ICU. Intensive Care Med. (2007) 33:2232. doi: 10.1007/s00134-007-0893-7
20. Maxine D, Fan J, Yennu S, Tanco K, Shin SH, Wu J, et al. The frequency of missed delirium in patients referred to palliative care in a comprehensive cancer center. Support Care Cancer. (2015) 23:2427–33. doi: 10.1007/s00520-015-2610-3
21. Petty NK, Ben ZN, Stanton-Cook M, Skippington E, Totsika M, Forde BM, et al. Global dissemination of a multidrug resistant Escherichia coli clone. Proc Natl Acad Sci U S A. (2014) 111:5694–9. doi: 10.1073/pnas.1322678111
22. Paramythiotou E, Routsi C. Association between infections caused by multidrug-resistant gram-negative bacteria and mortality in critically ill patients. World J Crit Care Med. (2016) 5:111–20. doi: 10.5492/wjccm.v5.i2.111
Keywords: goal-directed lung physiotherapy, older patients, sepsis, pneumonia, intensive care unit
Citation: Sun J, Cui N, Han W, Li Q, Wang H, Li Z, Cheng W, Luo H and Zhao M (2021) Implementation of Nurse-Led, Goal-Directed Lung Physiotherapy for Older Patients With Sepsis and Pneumonia in the ICU. Front. Med. 8:753620. doi: 10.3389/fmed.2021.753620
Received: 05 August 2021; Accepted: 31 October 2021;
Published: 22 November 2021.
Edited by:
Claude E. Guérin, Hospices Civils de Lyon, FranceReviewed by:
Bo Hu, Zhongnan Hospital of Wuhan University, ChinaZeping Laing, Daping Hospital, China
Copyright © 2021 Sun, Cui, Han, Li, Wang, Li, Cheng, Luo and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Na Cui, cHVtY2hjbkAxNjMuY29t; Qi Li, MTg2MTI2NzEzOTRAMTYzLmNvbQ==; Hao Wang, bmV3d2FuZ2hhb0Bob3RtYWlsLmNvbQ==
†These authors have contributed equally to this work
 Jianhua Sun1†
Jianhua Sun1† Na Cui
Na Cui