- 1IHU Méditerranée Infection, Marseille, France
- 2Aix-Marseille University, Institut de Recherche pour le Développement (IRD), Assistance Publique - Hôpitaux de Marseille (AP-HM), MEPHI, Marseille, France
- 3Laboratoire de Diagnostic, Centre de Soins 1, Caisse Nationale de Sécurité Sociale (CNSS), Djibouti, Djibouti
- 4Centre National de la Recherche Scientifique, Marseille, France
Since the start of COVID-19 pandemic the Republic of Djibouti, in the horn of Africa, has experienced two epidemic waves of the virus between April and August 2020 and between February and May 2021. By May 2021, COVID-19 had affected 1.18% of the Djiboutian population and caused 152 deaths. Djibouti hosts several foreign military bases which makes it a potential hot-spot for the introduction of different SARS-CoV-2 strains. We genotyped fifty three viruses that have spread during the two epidemic waves. Next, using spike sequencing of twenty-eight strains and whole genome sequencing of thirteen strains, we found that Nexstrain clades 20A and 20B with a typically European D614G substitution in the spike and a frequent P2633L substitution in nsp16 were the dominant viruses during the first epidemic wave, while the clade 20H South African variants spread during the second wave characterized by an increase in the number of severe forms of COVID-19.
Introduction
Since the identification of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in China in late 2019 as the causative agent of COVID-19 (1–3), the virus has spread worldwide causing a global pandemic. Over the course of 17 months, the COVID-19 pandemic caused more than 3.69 million deaths and 171.74 million confirmed cases worldwide (4). SARS-CoV-2 genomic epidemiology has led to the detection of several mutations of the original Wuhan-Hu-1 strain of SARS-CoV-2. During the spring of 2020, a non-synonymous mutation leading to a spike protein substitution D614G became dominant in the reported sequences of SARS-CoV-2 and was found to enhance viral replication as a result of higher affinity for the ACE2 receptor (5, 6). Since the summer of 2020, the emergence of major viral variants has been observed (7–10). These variants have been found to be responsible for juxtaposed or successive epidemics in various geographic areas. Cases of re-infection with SARS-CoV-2 genotypes different from those which first infected patients, have also been documented (11). In order to track the evolution of the virus over time, many laboratories have performed virus genotyping. Laboratories equipped with whole genome sequencing capabilities have reported a large number of mutations which has increased over time. However, there are considerable disparities between countries and in some cases there is no database on circulating viruses (12).
The Republic of Djibouti is a country in East Africa with a population of 921,804 inhabitants in 2020 composed of 60% Somalis, 35% Afars, and 5% Arabs (Figure 1). To date no SARS-CoV-2 sequence has been characterized in the Djiboutian population although cases of COVID-19 have been declared by health authorities in March 2020 (13). In response to the WHO alert on the COVID-19 pandemic, the Republic of Djibouti has rapidly established a prevention strategy based on testing, isolation, treatment and tracing of contacts of each positive case (14). Being prepared for the prevention of the epidemic risk was perhaps more essential here than elsewhere due to regional specificities. Djibouti's geopolitical situation is interesting because it hosts the military bases of many countries such as China and the USA, as well as European countries including the largest French military base in Africa. This has led to a mixing of populations which is conducive to the circulation of pathogens, including SARS-CoV-2. The first COVID-19 case in Djibouti was confirmed on 18 March 2020 in a member of the Spanish special forces (15, 16). This patient was isolated and had no interaction with the local population (17). A second COVID-19 case was reported in the same month in a member of United States Department of Defense who was working in the US military base in Djibouti (18). The first epidemic period began on 8 April and lasted until 15 August 2020 with a peak in late May early June. A second epidemic wave period began on 21 February and lasted until 18 May 2021 with a peak in late March-early April. According to the most recent (23 June 2021) information available through the Johns Hopkins Resource Center, 11,595 total confirmed cases of SARS-CoV-2 infections and 155 deaths from severe forms of COVID-19 had been reported in Djibouti, (https://coronavirus.jhu.edu/).
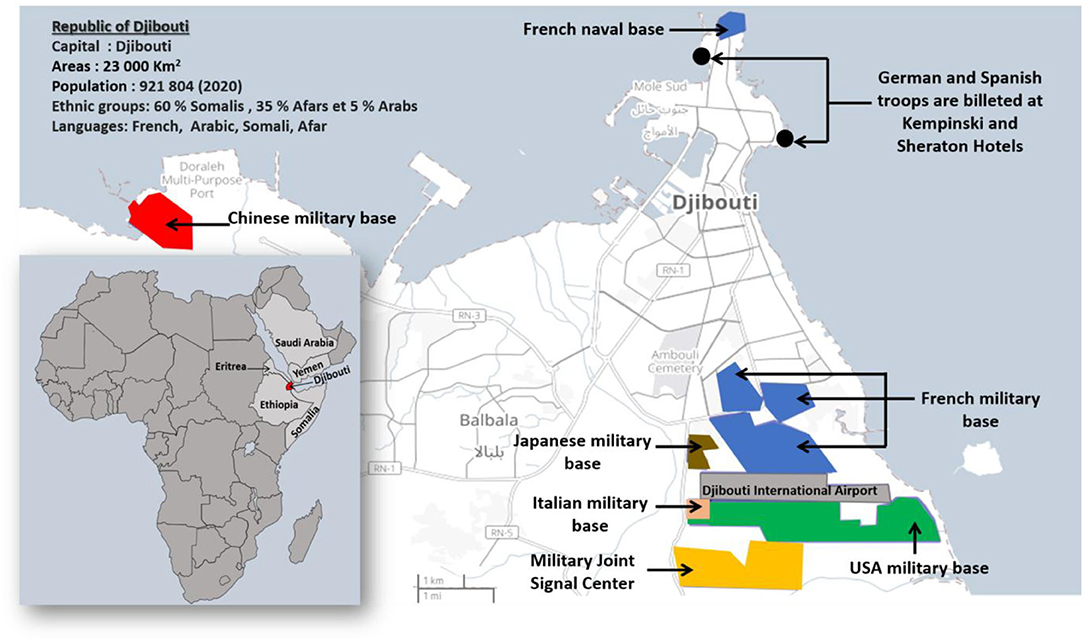
Figure 1. Map of Djibouti. The Republic of Djibouti is located in the horn of East Africa. In 2020, the population of the Republic of Djibouti consisted of 60% Somalis, 35% Afars, and 5% Arabs with a total of 921,804 inhabitants. The map of Dijbouti was adapted from the Open Street Map (http://umap.openstreetmap.fr/). The geographical and geopolitical situation of Djibouti is interesting because it hosts several military bases and forces from different countries including France, Italy, Germany, Spain, China, the USA, and Japan.
Our main objective was to reduce the large data gaps regarding the genomic characterization of SARS-CoV-2 circulating in Djiboutian population. Here we used mini-spike sequencing to type strains and whole genome sequencing to evaluate the diversity of SARS-CoV-2 strains that had spread in the Djiboutian population. In addition, we compared these sequences to the fifty-two SARS-CoV-2 sequences which were very recently released by the GISAID database and which corresponded to viruses that had infected foreigners working for the US Department of Defense in Djibouti.
Materials and Methods
Patients' Samples
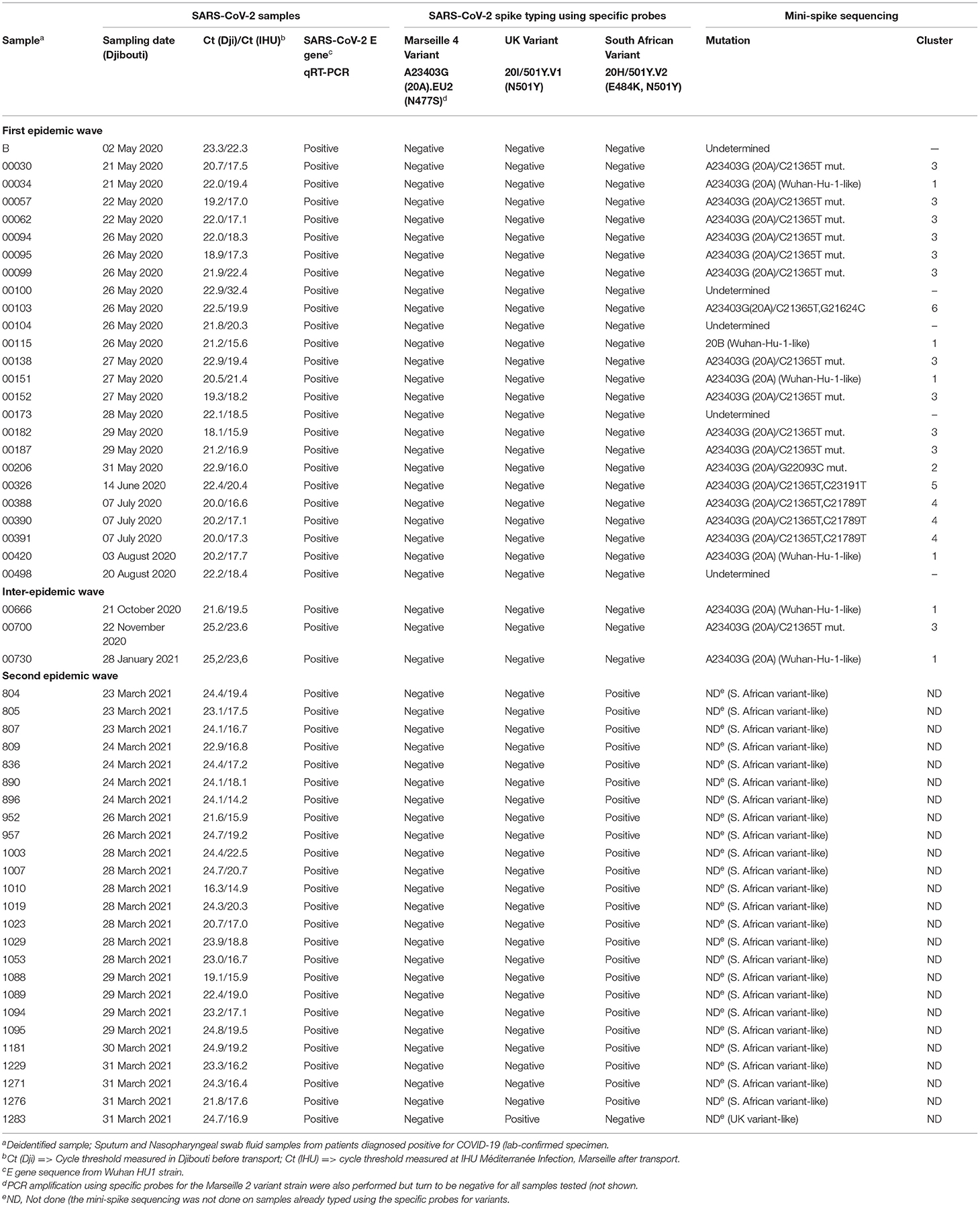
Sputum and nasopharyngeal swab fluid (5–10 mL) samples from patients who had been diagnosed as positive for COVID-19 (lab-confirmed specimen by a quantitative reverse transcriptase-polymerase chain reaction, qRT-PCR) were collected in Djibouti (“Centre de soins 1 de la Caisse Nationale de Sécurité Sociale,” Social Security Care center number 1 of the Republic of Djibouti). The bank of samples (1,861 samples collected, including 407 SARS-CoV-2 positive samples) was kept in Djibouti until use and only fifty three frozen samples from individual with a cycle threshold (Ct) value below 25 [see column “Ct(Dji)” in Table 1] corresponding to a high viral load, were transferred in biohazard containers (Aramex company) to the IHU Méditerranée Infection institute (Marseille, France). Among these fifty three samples representative of the epidemiological situation, twenty-five were collected during the period from May 2020 to August 2020; three were collected during the inter-waves period (October 2020 to January 2021); and twenty-five were collected during the second epidemic wave in March 2021. Before being processed, each transferred sample was retested using a qRT-PCR performed with specific primers for the E gene of SARS-CoV-2, to confirm the presence of virus in sample after transport [see column “Ct(IHU)” in Table 1]. All samples received at the IHU showed CT values below 25, with the exception of sample number 00100 found with a CT of 32.4. According to our diagnostic criteria, this sample remained positive since the qRT-PCR are considered positive when the Ct value is below 35, as previously reported (19). Only samples that meet a Ct < 25 were transferred to the IHU Marseille genomic sequencing platform for mini-spike sequencing and/or whole genome sequencing.
SARS-CoV-2 Variant Typing and Mini-Spike Sequencing
Several specific qRT-PCR systems with primers and fluorescent dye-tagged probes (see Supplementary Table 1) that can confirm the presence of SARS-CoV-2 in samples (a pan-genomic SARS-CoV-2 probe that hybridizes with the E gene; size of the amplification fragment: 113 bp), and probes which can discriminate between the Marseille 4 variant (primers in the ORF1; size of the amplification fragment: 114 bp), UK variant (Nextstrain clade 20I; primers in the N gene; size of the amplification fragment: 110 bp), and South African variant (Nextstrain clade 20H; primers in nsp2; size of the amplification fragment: 119 bp) strains, were used for the rapid identification of variants.
Regarding the samples which were found positive for the SARS-CoV-2 E gene and negative for the three variants, a mini-spike sequencing strategy was performed as follows. the sequences of the spike gene 5'-region (nucleotides 1-1,854 in reference to NC_045512.2), named mini-spike, were obtained by next-generation sequencing (NGS) following an in-house protocol that enables the PCR amplification of a fragment between position 21,296 (in the ORF1b) and position 23,424 (in the spike gene) of the viral genome (primers: 5′-GCAAACCACGCGAACAAATA-3′; 5′-GGGACTTCTGTGCAGTTAAC-3′; size of the amplification fragment: 2,128 bp). Sequences were analyzed using Nextclade (https://clades.nextstrain.org/) (20) and an in-house Python script.
SARS-CoV-2 Whole Genome Sequencing
A few samples were further characterized by next-generation sequencing (NGS) using the Nanopore sequencing (Oxford Nanopore Technologies, Cambridge, UK), as previously described (21). Regarding the eight samples from the first wave characterized by NGS, they were selected to be representative of the different SARS-CoV-2 clusters found using the mini-spike sequencing (e.g., the Djiboutian sample 103 from May 2020 in Table 1 corresponds to sample ID Djibouti CNSS00103-IHU1031243436/2020 in Table 2). Regarding the five samples from the second wave, we have chosen to better characterize four South African variants (e.g., the Djiboutian sample 1095 from March 2021 in Table 1 corresponds to sample ID Djibouti CNSS001095-IHU1031441326/2021 in Table 2) and the only UK variant discovered in this series of samples. The consensus sequences were generated with a minimum coverage of 100 reads. Genome consensus sequences were generated through mapping on the SARS-CoV-2 genome using the sequence from the Wuhan-Hu-1 reference strain (GenBank accession no. NC_045512.2) with the Minimap2 software using short genomic paired-end reads as pre-set (22). All the new SARS-CoV-2 sequences reported herein have been placed in the open access GISAID database (Accession ID: EPI_ISL_2820509; EPI_ISL_2820514; EPI_ISL_2820756; EPI_ISL_2820520; EPI_ISL_2820757; EPI_ISL_2820547; EPI_ISL_2820621; EPI_ISL_2820626; EPI_ISL_2820687; EPI_ISL_2820701; EPI_ISL_2820704; EPI_ISL_2820705; EPI_ISL_2820706).
SARS-CoV-2 Phylogenetic Tree
Phylogenetic reconstruction was performed using the IQ-TREE software with the GTR Model and 1,000 ultrafast bootstrap repetitions after aligning genomes using MAFFT v.7 (23); the tree was visualized with the Interactive Tree Of Life (iTOL)-v6 software, as previously described (21).
Results
Typing of SARS-CoV-2 Strains Spreading in Djibouti
As summarized in Figure 2 (upper panel), the Republic of Djibouti has experienced two epidemic waves of COVID-19. The first wave occurred between April and August 2020, and the second occurred between February and May 2021. The cases fatality rate was lower during the first wave (number of cases: 5,414; number of deaths: 60; fatality rate: 1.10%) than during the second wave (number of cases: 5,560; number of deaths: 90; fatality rate: 1.61%), (Figure 2 middle panel), suggesting the circulation of more deadly viruses during the second wave. The cumulative number of confirmed severe COVID-19 cases leading to patients' deaths was 152 from March 2020 to May 2021 (Figure 2, lower panel). As shown in the chart (Figure 3), all samples were tested for SARS-CoV-2 using a PCR-detection of the viral E gene, followed by screening using specific probes that discriminate between different SARS-CoV-2 variants (routinely used at the IHU for the identification of SARS-CoV-2 variants). This fast screening strategy was successful for the typing of samples collected in March 2021 in Djibouti but failed for samples collected during the first epidemic wave and the inter-wave period because the strains circulating in 2020 had not yet accumulated the characteristic mutations of the variants. In order to successfully type these SARS-CoV-2, the samples were submitted for mini-spike sequencing. For twenty-three samples the mini-spike sequencing (fragment 21296–23424) was successful, but for the five remaining strains it was not interpretable due to poor data quality. We found (Table 1) that during the first epidemic wave, all viruses derived from the Wuhan-Hu-1 reference strain but carried the non-synonymous A23403G mutation, leading to the substitution D614G in the spike. Six viruses showed only this mutation in the mini-spike region, while most other viruses (16 strains) carried an additional non-synoymous mutation C21365T in the ORF1b, leading to a P2633L substitution in the pp1ab precursor of nsp16 methyltransferase. Additional non-synonymous mutations were found in the mini-spike of some viruses, including G21624C (leading to a substitution R21T), C21789T (leading to a substitution T76I), and G22093C (leading to a substitution M177I), all located in the spike N-terminal domain.
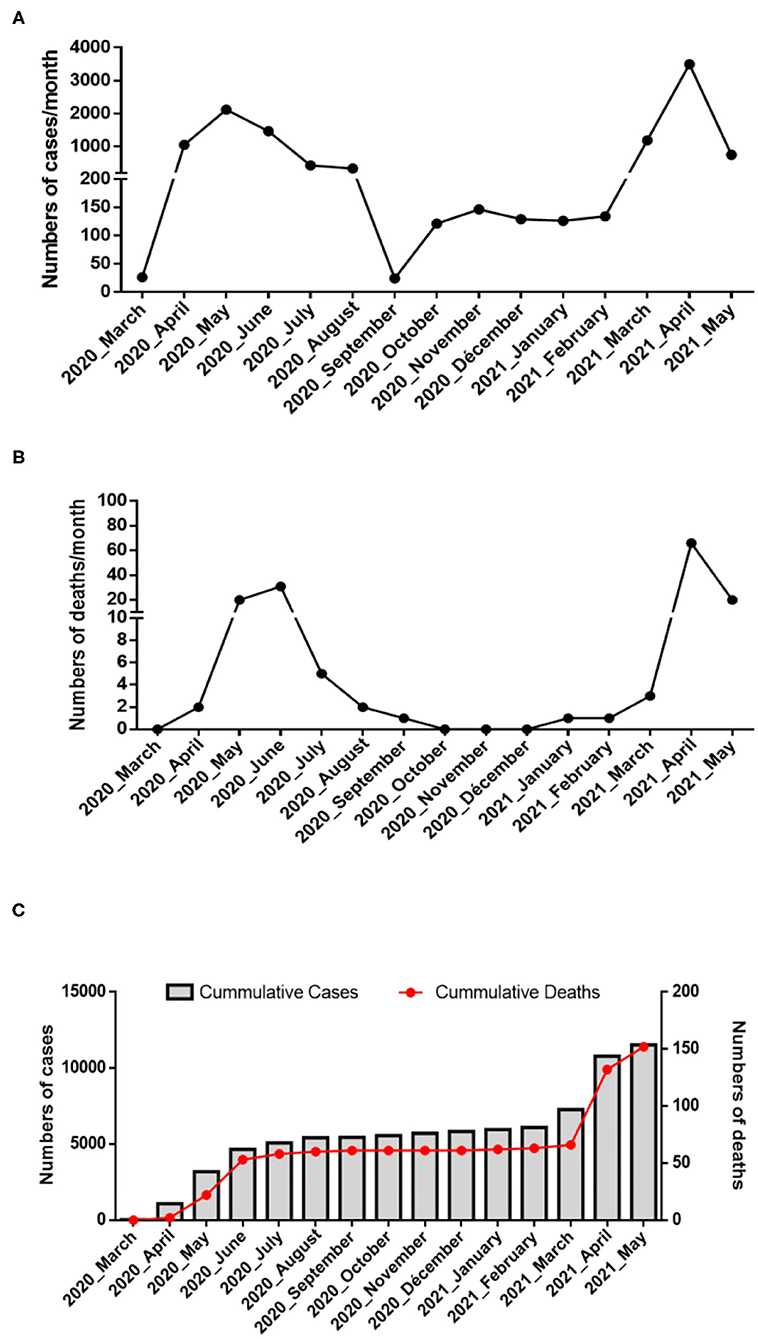
Figure 2. Epidemiology of COVID-19 in Djibouti. Summary of the COVID-19 outbreaks in the Republic of Djibouti. (A) Epidemiological data regarding the COVID-19 episodes compiled from information provided by the WHO from March 2020 to May 2021 (https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/). Three periods (first wave, inter-wave, second wave) were provisionally defined during which samples were collected for the genetic analysis of the SARS-CoV-2 strains. (B) Number of deaths over time. (C) Cumulative number of COVID-19 cases and SARS-CoV-2-associated deaths in Djibouti.
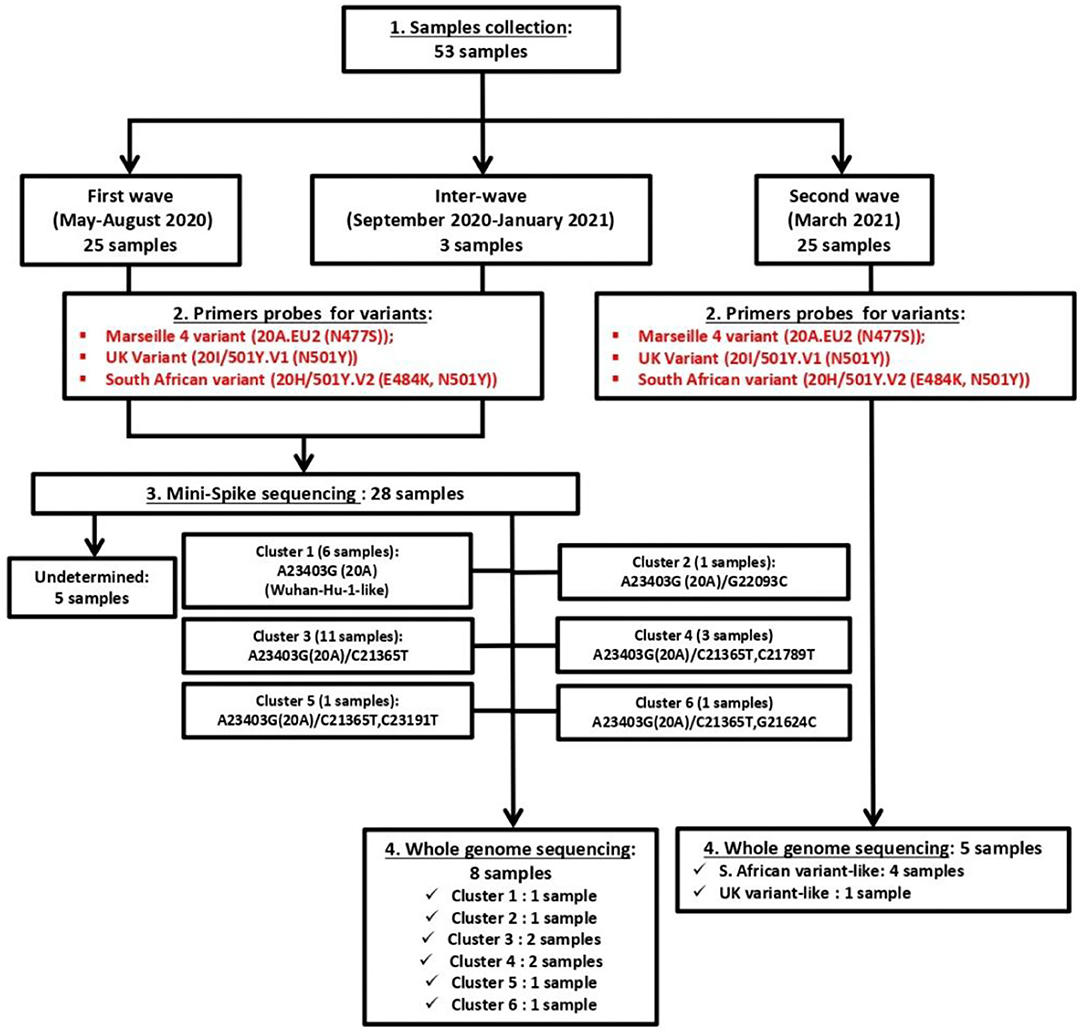
Figure 3. Chart of management of the fifty-three SARS-CoV-2 samples for typing and whole genome sequencing.
According to the mini-spike sequences, all SARS-CoV-2 circulating during the first epidemic wave derive from the 20A clade that evolves into two groups: one being clade 20B that comprises the ancestor viruses at the origin of the group 1 mutant virus carrying the non-synonymous mutation C18495T (leading to P1675L substitution in the ORF1b) and the synonymous mutation C19836T, and the other group comprising viruses carrying either the non-synonymous C21365T mutation compared to the 20A consensus sequence (cluster 6) or both mutations C21365T and C21789T (cluster 4). Regarding the viruses circulating during the inter-wave period, they belong to clade 20A with one virus which carried the non-synonymous mutation C21365T in the ORF1b. A completely different pattern was found for SARS-CoV-2 circulating during the second epidemic wave; one virus was identified as a UK variant (20I/501Y.V1) of SARS-CoV-2 while the large majority of the strains (24 of 25) were identified as South African variants (20H/501Y.V2).
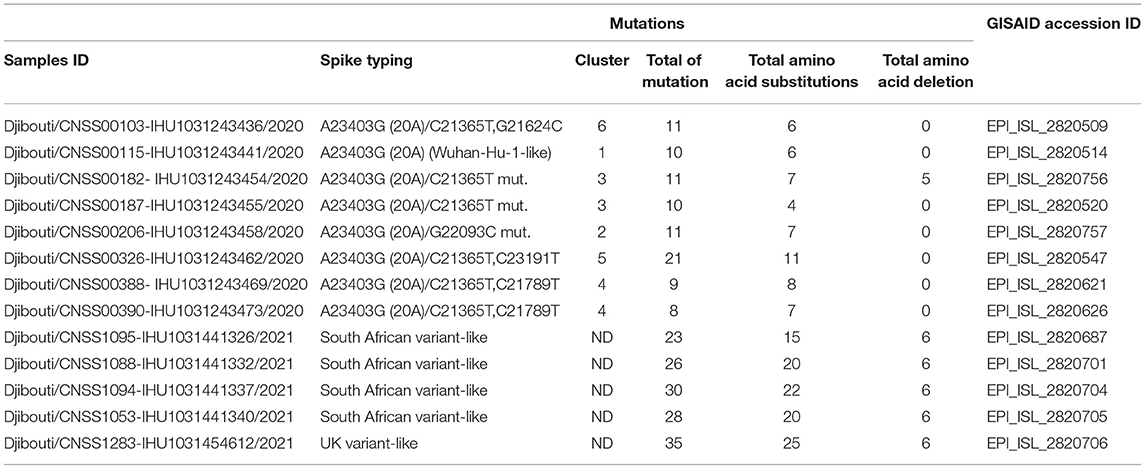
Whole Genome Sequencing of SARS-CoV-2 Spreading in Djibouti
Once the SARS-CoV-2 spike gene typing was performed, it became interesting to study the genetic polymorphism of these viruses using whole genome sequencing. To achieve this goal, eight SARS-CoV-2 circulating in Djibouti during the first epidemic wave (chosen on the basis of their polymorphism in the spike gene) and five SARS-CoV-2 circulating during the second epidemic wave (four South African variants and one UK variant) were submitted to whole genome sequencing (Table 2).
Regarding viruses from the first epidemic wave, the total number of mutations along the genomes compared to the Wuhan-Hu-1 reference genome varied from eight mutations (strain code Djibouti/CNSS00390-IHU1031243473/2020) up to 21 mutations (strain code Djibouti/CNSS00326-IHU1031243462/2020). These mutations lead to a number of amino acid substitutions varying from 4 to 11 (Table 2). In addition the deletion of 5 amino acids was observed for one virus. The distribution of these mutations on the genome of SARS-CoV-2 is illustrated in Figure 4. Four substitutions affect the spike while the others are distributed in the non-structural proteins (nsp2, nsp3, nsp5, nsp12, nsp13, nsp14, nsp16), M (membrane), ORF9b, and N (nucleocapsid) proteins. As shown in Figure 5, when compared to other sequences (the closest sequences selected via blast) available through the Global Initiative on Sharing Avian Influenza Data (GISAID), the 20A SARS-CoV-2 genomes of the first epidemic wave are genetically related to genomes obtained in Japan (GISAID ID: Japan/TC-0464/2020) and in the USA (GISAID ID: USA/MI-MDHHS-SC20548/2020) while the 20B genomes are related to genomes from Somalia (Somalia/CV1232/2020) and England (England/ALDP-95C3C7/2020) characterized during the same period.
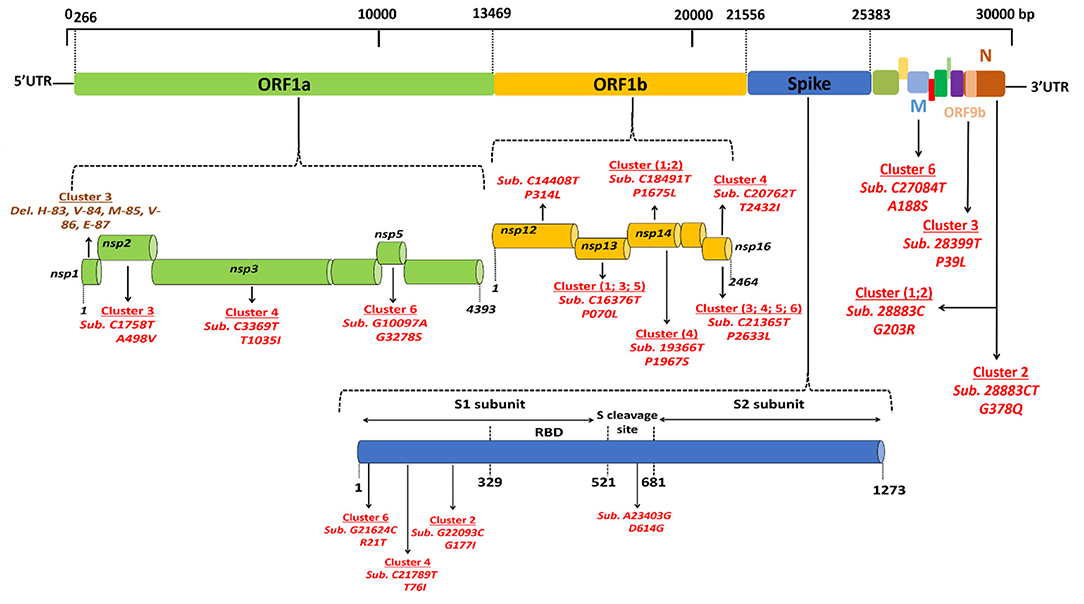
Figure 4. Location of genomic mutations and deletions on the complete nucleotide sequence from different isolates of SARS-CoV-2. Viruses circulating during the first epidemic wave derive from the 19A clade that evolves into two clades: 20A, including viruses from clusters 3, 4, 5, and 6, and 20B, including viruses from clusters 1 and 2. Del means deletion; Sub means substitution.
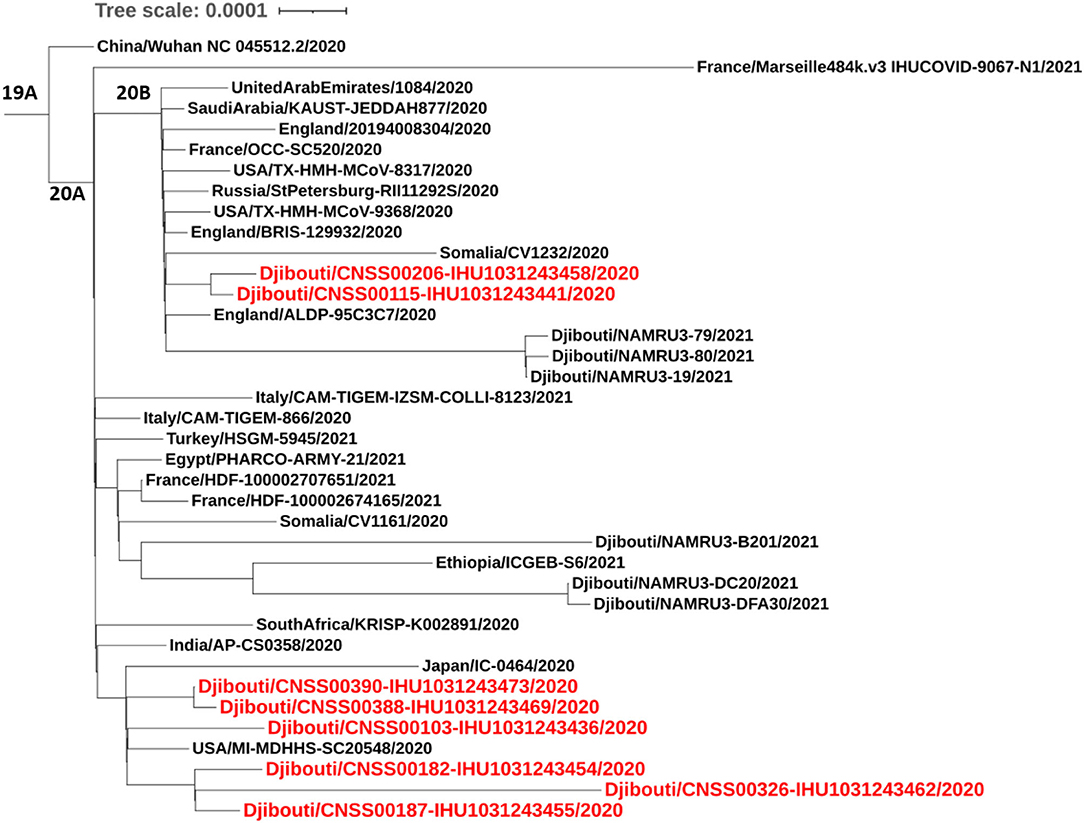
Figure 5. Phylogenetic tree (obtained using the IQ-TREE software with the GTR Model and 1,000 ultrafast bootstrap 84 repetitions), including height SARS-CoV-2 strains from the first COVID-19 wave in Djibouti compared to 23 SARS-CoV-2 sequences (clades 19B, 20A, 20B), available through GISAID.
Regarding the South African SARS-CoV-2 variant from the second epidemic wave, the four genomes obtained by NGS showed between 23 and 30 mutations compared to the Wuhan-Hu-1 genome. Most of these mutations were non-synonymous, leading to between 15 and up to 22 amino acid substitutions and five amino acid deletions (Table 2). These four viruses are genetically related to one another and belong to clade 20H. They were found to be closely related to viruses circulating in Spain (Spain/CT-HUB00604/2021) and Equatorial Guinea (Equatorial Guinea/85185/2021) circulating during the same period of 2021 (Figure 6). Regarding the only UK variant (Djibouti/CNSS1283-IHU1031454612/2021) found during the second epidemic wave, it shows 35 mutations compared to the Wuhan-Hu-1 strain, leading to 25 amino acid substitutions and six amino acid deletions (Figure 7). This genome belong to clade 20I and was genetically related to a genome circulating the previous year in South Korea (South Korea/KDCA830/2020).
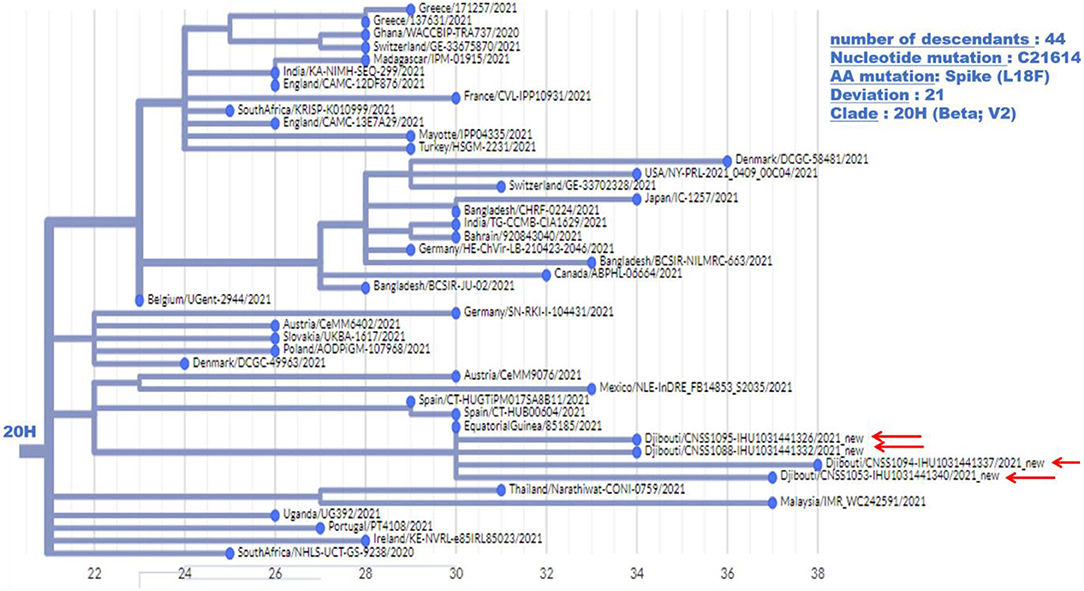
Figure 6. Phylogenetic tree (obtained using the Nexcladevv0.14.4 software (https://clades.nextstrain.org/), including four South African variants of SARS-CoV-2 strains from the second COVID-19 wave in Djibouti compared to forty SARS-CoV-2 sequences (clade 20H) available through GISAID and automatically selected using Nextclade. The scale at the bottom of the figure indicates the number of mutations (deviation) compared to the sequence of the reference strain (Wuhan-Hu-1 reference strain; GenBank accession no. NC_045512.2).
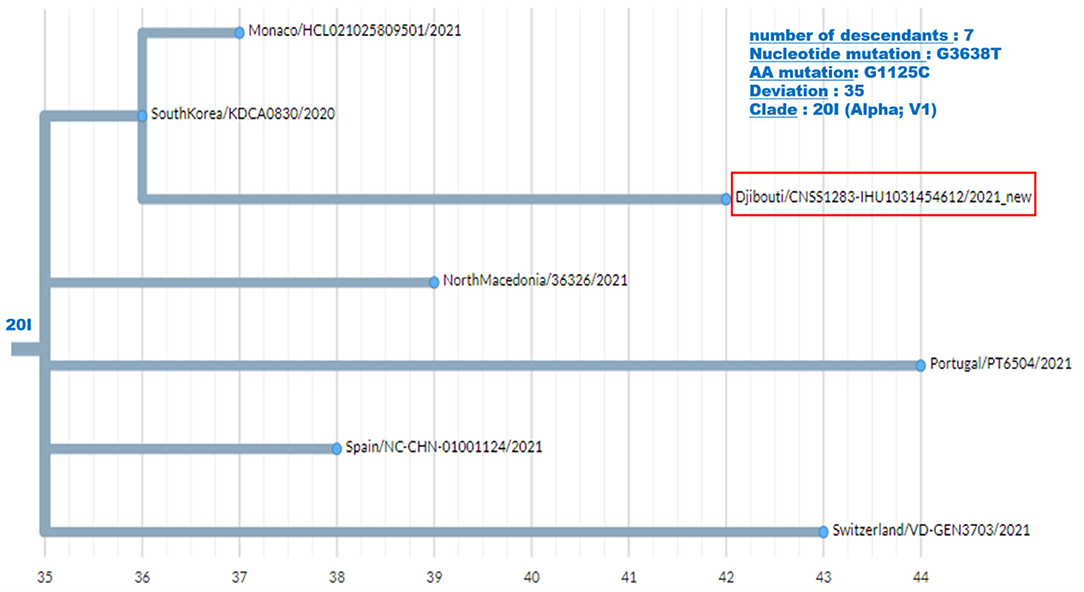
Figure 7. Phylogenetic tree (obtained using the Nexcladevv0.14.4 software (https://clades.nextstrain.org/), including the UK variant of SARS-CoV-2 strain from the second COVID-19 wave in Djibouti compared to six SARS-CoV-2 sequences (clade 20I) available through GISAID. The scale at the bottom of the figure indicates the number of mutations (deviation) compared to the sequence of the reference strain (Wuhan-Hu-1 reference strain; GenBank accession no. NC_045512.2).
Discussion
Like what has been observed in the rest of the world, the Republic of Djibouti was confronted in 2020 with an epidemic of SARS-CoV-2 dominated by Wuhan-HU-1-like viruses. This first epidemic wave was followed in 2021 by the emergence of SARS-CoV-2 variant viruses belonging mainly to the South African lineage known to cause more severe forms of COVID-19.
When SARS-CoV-2 started to spread worldwide, the viruses that circulated were closely related to the Wuhan-Hu-1 strain, with only a few mutations. However, a D614G substitution in the spike has emerged with an increasing prevalence of this variant during the COVID-19 pandemic (24). Patients infected with this virus shed more viral nucleic acid compared with those infected with the wild-type (D614) Wuhan-Hu-1 strain and showed significantly higher infectious titers in vitro as a consequence of higher affinity for ACE2 (6). During the summer of 2020, the dynamic tracking of the SARS-CoV-2 mutants in the global pandemic highlighted a rapid evolution of the virus with an increase in the frequency of mutations and an epidemic pattern characterized by the generation of new variants including the Marseille 4 variant Nextclade 20A.EU2 (7), the UK variant 20I/501Y.V1 (8), the South African variant 20H/501Y.V2 (9), the Brazilian variant 484K.V2 (25), and others (10). These variants can be associated with different clinical features of COVID-19 and increased frequency of death (26, 27).
Despite the restrictive measures on international transport and the lockdown measures applied in most countries, the variants continued to spread from one geographic region to another (28). Although Africa is considered as the most vulnerable continent, it was the last to be impacted by the pandemic (29, 30). The SARS-CoV-2 was reported to have spread to Africa in February 2020, with the earliest diagnosed cases being detected in Egypt and Nigeria. The virus introduction in Africa was considered to be mainly of American and European origins rather than China. In partnership with the WHO, the Africa Task Force established a strategy to fight COVID-19 and 43 African countries were able to test for SARS-CoV-2, although test kits were in short supply. On 11 March 2020, the WHO declared COVID-19 a global pandemic. By 31 March 2020, 5,389 cases of COVID-19 had been reported in Africa (31). By 18 April 2020, the African CDC had reported 19,895 confirmed cases, including 1,017 deaths from 52 African countries. Compared to the global 7,700 genome sequences of SARS-CoV-2 available, the African continent had reported only 90 genome sequences from five countries (29). By the end of April 2020, confirmed cases were found in most African countries, with Djibouti ranking in the top seven of the most affected countries (Egypt: n = 3,490; South Africa: n = 3,465; Morocco: n = 3,209; Algeria: n = 2,811; Cameroon: n = 1,163; Ghana: n = 1,042; Djibouti: n = 945) (32). Despite a weak health care system and a large immune-compromised population linked to the high prevalence of malaria, HIV/AIDS, tuberculosis, and malnutrition, the progression of COVID-19 in Africa remained well-below the predictions forecasting a disaster on the continent (30). However, the second wave of COVID-19 appeared to be more aggressive, with more cases and higher fatality rates. By 31 December 2020, African countries had reported 2,763,421 COVID-19 cases (e.g., 38.3% in South Africa; 15.9% in Morocco; 5.1% in Tunisia; 5.0% in Egypt; 4.5% in Ethiopia), and 65,602 deaths, accounting for 3.4% of global COVID-19 cases for a population that represents 15.8% of the world population (33). Phylogenetic analysis of SARS-CoV-2 performed using 69 sequences from Africa and 155 SARS-CoV-2 sequences from other origins available through GISAID (34), suggested that the SARS-CoV-2 transmitted to Africa were the mutated forms of the Wuhan-Hu-1 strain which first spread to Europe and America and had accumulated mutations. A major characteristic of the African isolates was the high frequency (84.2%) of the A23403G mutation leading to a D614G. Among the African isolates, only the South Africa-2 strain was found to be identical to the Wuhan-Hu-1 strain, while the Benin-3 and Mali-2 isolates were likely to be of Asian origin. More recently, a study (35) investigated 1,414 SARS-CoV-2 genomic sequences collected in the Eastern Mediterranean Region before 12 November 2020 and available through GISAID, including sequences from Saudi Arabia (n = 521), the United Arab Emirates (n = 186), Oman (n = 185), and Egypt (n = 150). The other sequences were from viruses isolated in Iran, Iraq, Jordan, Morocco, Palestine, Qatar, and Tunisia. About 65.6% of the viruses belong to clades 20A, 20B, and 20C and non-synonymous mutations leading to two amino acid substitutions, the D614G in the spike and P323L in nsp12, were predominant in most countries. Many country-specific substitutions were also detected. No sequences were available from Djibouti, Afghanistan, Libya, Somalia, Sudan, Syria, and Yemen.
In this context, the situation of Djibouti, located in the horn of Africa with a strategic position at the southern entrance to the Red Sea, where 20,000 ships and 30% of the world's trade passes through (36), is interesting because it hosts the military bases of many countries, leading to a mixing of populations which might favor the circulation of SARS-CoV-2, including particular variants. As early as February 2020, the Republic of Djibouti had worked with the WHO to set up a response plan with rapid implementation to prevent and/or control SARS-CoV-2 spreading in the country (37). The first case of COVID-19 was detected in Djibouti on 17 March 2020, leading the health authorities to apply the strategy aimed at testing any person suspected of being infected with the virus or of being a contact case. Djibouti became the African country that has performed the most SARS-CoV-2 screening in Africa (the country increased its laboratory testing capacity from 100 samples tested by PCR per day up to 2,000 samples per day in April 2020) (14). Between 17 March 2020 and 16 May 2020, Djibouti reported 1,401 confirmed COVID-19 cases including four deaths (a case fatality rate of 0.3%) (13). SARS-CoV-2 continued to spread across the country over the following months. Since the start of the COVID-19 epidemic, the Republic of Djibouti has experienced two epidemic waves. On 18 May 2021, 11,468 confirmed cases of SARS-CoV-2 infection and 152 deaths from severe forms of COVID-19 had been reported in Djibouti (a case fatality rate of 1.32%), according to the Johns Hopkins Resource Center (https://coronavirus.jhu.edu/), with a case fatality rate of 1.10% during the first epidemic wave, 0.36% during the inter-wave period, and 1.61% during the second epidemic wave. This remains lower than the 2.27% fatality reported worldwide.
Although the COVID-19 epidemic has been well-managed with massive screening followed by treatment, the health authorities had no information on the type of strains circulating in the country. The first COVID-19 case in Djibouti was a member of the Spanish special-forces (15, 16). Our study sheds light on the history of COVID-19 in Djibouti. During the first wave of the epidemic, the strains that circulated derived from Wuhan-Hu-1-like strains (also named the “China” strain), namely clade 20A and 20B, but these viruses already carried the D614G found in Europe and USA. The 20A SARS-CoV-2 were genetically related to the Japan/TC-0464/2020 strain and USA/MI-MDHHS-SC20548/2020 strain while the 20B were related to the Somalia/CV1232/2020 and England/ALDP-95C3C7/2020 strain and can be organized in six clusters. It should be noted, the P323L substitution has been frequently observed in nsp12 in the strain spreading in Africa. During the inter-wave phase, the circulating viruses were of the same clade as those present during the first epidemic wave. In contrast, during the second epidemic wave the Wuhan-Hu-1-like viruses were no longer found giving way to variants previously described in Europe (UK variant) and South Africa (South African variant). The UK variant was found in 4% of samples, while the South African variant was found in 96% of samples. South African-like variants circulating in the Djiboutian population during the second epidemic wave belong to clade 20H and were related to viruses circulating in Spain (Spain/CT-HUB00604/2021) and Equatorial Guinea (Equatorial Guinea/85185/2021) Regarding the UK variant found in Djiboutian people, it was genetically related to a strain belonging to clade 20I that circulated the year before in South Korea (South Korea/KDCA830/2020). Very recently (13 June 2021), 52 sequences of SARS-CoV-2 spreading during the second epidemic wave among members of the US department of Defense in Djibouti were deposited in GISAID (GISAID ID Djibouti/NAMRU3-XXXX/2021 where XXXX corresponds to the number of the sequence and 2021 is the year for sample collection). We compared these sequences to the SARS-CoV-2 genomes from Djiboutian' COVID-19 patients (Supplementary Figure 1). Of these viruses sequenced by the US department of Defense in Djibouti, 28 genomes belong to clade 20I (UK variant) and 18 belong to clade 20H (South African variant); the others being 20A and 20B strains. This corroborates our results. However, the frequency of clade 20I was apparently much more widespread among foreigners (American troops) than Djiboutians, while clade 20I was spread in both populations.
In conclusion, the dynamics of SARS-CoV-2 spreading in Djibouti was not so different from that which was observed worldwide, with a first wave dominated by viruses belonging to clades 20A and 20B (Wuhan-Hu-1 -like viruses with viruses presenting several mutations), followed by a decay phase of the epidemic and then a second wave linked to the circulation of variant viruses with a very strong predominance of the South African variant strain of the virus belonging to clade 20H. This second wave turned out to be characterized by an increase in the number of severe forms of COVID-19, leading to more deaths.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
IO, MHA, DR, and CAD contributed to the design of the study. IAH, ISA, ZAW, and MHA took care of the COVID-19 patients in Djibouti and collected the samples. AL, LB, JD, MB, LH, P-EF, and PC generated and analyzed the virus sequences. IO and CAD prepared the first draft of the manuscript. CAD, MHA, and DR supervised the work. DR obtained the funding for this study. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the French Government under the Investments for the Future programme managed by the National Agency for Research (ANR), Méditerranée-Infection10-IAHU-03 to DR, funding from Region Provence-Alpes-Côte d'Azur, European funding FEDER, PRIMMI (European Regional Development Fund-Plateformes de Recherche et d'Innovation Mutualisées Mediterranée), and a grant from the Caisse Nationale de Sécurité Sociale (CNSS) Djibouti to IO.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Emilie Burel and Mamadou Beye for helpful technical discussions.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.737602/full#supplementary-material
Supplementary Figure 1. Phylogenetic tree (obtained using the IQ-TREE software with the GTR Model and 1,000 ultrafast bootstrap 84 repetitions), including SARS-CoV-2 genomes from the COVID-19 Djiboutian patients reported herein (Djibouti/CNSS00XXX-IHU103XXXXXXX/2020 for samples collected in 2020 and Djibouti/CNSS1XXX-IHU103XXXXXXX/2021 for samples collected in 2020; Djibouti/CNSS00XXX: the number XXX can be found in Table 2) compared to the 52 sequences of SARS-CoV-2 spread during the second epidemic wave among members of the US department of Defense in Djibouti (GISAID ID: Djibouti/NAMRU3-XXXX/2021) and several other strains chosen to strengthen the organization of the phylogenetic tree.
Supplementary Table 1. qRT-PCR primers and probes.
References
1. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. (2020) 579:270–73. doi: 10.1038/s41586-020-2012-7
2. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China 2019. N Engl J Med. (2020) 382:727–33. doi: 10.1056/NEJMoa2001017
3. Yang X, Yu Y, Xu J, Shu H, Xia JA, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Resp Med. (2020) 8:475–81. doi: 10.1016/S2213-2600(20)30079-5
4. Johns Hopkins Coronavirus Resource Center, JH University. Available online at: https://coronavirus.jhu.edu/map.html (accessed June 03, 2021).
5. Plante JA, Liu Y, Liu J, Xia H, Johnson BA, Lokugamage KG, et al. Spike mutation D614G alters SARS-CoV-2 fitness. Nature. (2021) 592:116–21. doi: 10.1038/s41586-020-2895-3
6. Korber B, Fischer WM, Gnanakaran S, Yoon H, Theiler J, Abfalterer W, et al. Tracking Changes in SARS-CoV-2 Spike: evidence that D614G increases infectivity of the COVID-19 Virus. Cell. (2020) 182:812–27.e19. doi: 10.1016/j.cell.2020.06.043
7. Fournier PE, Colson P, Levasseur A, Devaux CA, Gautret P, Bedotto M, et al. Emergence and outcomes of the SARS-CoV-2 ‘Marseille-4’ variant. Int J Infect Dis. (2021) 106:228–36. doi: 10.1016/j.ijid.2021.03.068
8. Tang JW, Tambyah PA, Hui DSC. Emergence of a new SARS-CoV-2 variant in the UK. J Infect. (2021) 82:e27–8. doi: 10.1016/j.jinf.2020.12.024
9. Tegally H, Wilkinson E, Giovanetti M, Iranzadeh A, Fonseca V, Giandhari J, et al. Detection of a SARS-CoV-2 variant of concern in South Africa. Nature. (2021) 592:438–43. doi: 10.1038/s41586-021-03402-9
10. Gonzalez-Candelas F, Shaw MA, Phan T, Kulkami-Kale U, Paraskevis D, Luciani F, et al. One year into the pandemic: short-term evolution of SARS-CoV-2 and emergence of new lineages. Infect Genet Evol. (2021) 92:104869. doi: 10.1016/j.meegid.2021.104869
11. Brouqui P, Colson P, Melenotte C, Houhamdi L, Bedotto M, Devaux C, et al. COVID-19 re-infection. Eur J Clin Invest. (2021) 51:e13537. doi: 10.1111/eci.13537
12. Colson P, Raoult D. Global discrepancies between numbers of available SARS-CoV-2 genomes and human development indexes at country scales. Viruses. (2021) 13:775. doi: 10.3390/v13050775
13. World Health Organization (WHO). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ (accessed June 10, 2021).
14. Elhakim M, Tourab SB, Zouiten A. COVID-19 pandemic in Djibouti: epidemiology and the response strategy followed to contain the virus during the first two months, 17 March to 16 May 2020. PLoS ONE. (2020) 15:e0243698. doi: 10.1371/journal.pone.0243698
16. Covid-19: Spain to Repatriate Command Team From Djibouti After Positive Coronavirus Test|Jane's 360. www.janes.com. (Retrieved March 22, 2020).
17. Djibouti Joins Global Action to Prevent COVID-19 as First Case Is Confirmed in the Country - Djibouti. ReliefWeb. (Retrieved March 22, 2020).
19. La Scola B, Le Bideau M, Andreani J, Hoang VT, Grimaldier C, Colson P, et al. Viral RNA load as determined by cell culture as a management tool for discharge of SARS-CoV-2 patients from infectious disease wards. Eur J Clin Microbiol Infect Dis. (2020) 39:1059–61. doi: 10.1007/s10096-020-03913-9
20. Hadfield J, Megill C, Bell SM, Huddleston J, Potter B, Callender C, et al. Nextstrain: 213 real-time tracking of pathogen evolution. Bioinformatics. (2018) 34:4121–3. doi: 10.1093/bioinformatics/bty407
21. Colson P, Levasseur A, Delerce J, Pinault L, Dudouet P, Devaux C, et al. Spreading of a new SARSCoV-2 N501Y spike variant in a new lineage. Clin Microbiol Infect. (2021) S1198-743X(21)00226-3. doi: 10.1016/j.cmi.2021.05.006
22. Li H. Minimap2: pairwise alignment for nucleotide sequences. Bioinformatics. (2018) 34:3094–100. doi: 10.1093/bioinformatics/bty191
23. Katoh K, Standley DM. MAFFT multiple sequence alignment software version 7: improvements in performance and usability. Mol Biol Evol. (2013) 30:772–80. doi: 10.1093/molbev/mst010
24. Zhou B, Thao TTN, Hoffmann D, Taddeo A, Ebert N, Labroussaa, et al. SARS-CoV-2 spike D614G change enhances replication and transmission. Nature. (2021) 592:122–7. doi: 10.1038/s41586-021-03361-1
25. Troovey OTR, Harvey KN, Bird PW, Wei-Tze Tang J. Introduction of Brazilian SARS-CoV-2 484K.V2 related variants into the UK. J Infect. (2021) 82:e23–4. doi: 10.1016/j.jinf.2021.01.025
26. Davies NG, Jarvis CI, CMMID COVID-19 Working Group, Edmunds WJ, Jewell NP, Diaz-Ordaz K, et al. Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7. Nature. (2021) 593:270–4. doi: 10.1038/s41586-021-03426-1
27. Challen R, Brooks-Pollock E, Read JM, Dyson L, Tsaneva-Atanasova K, Danon L. Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: matched cohort study. BMJ. (2021) 372:n579 doi: 10.1136/bmj.n579
28. Cella E, Benedetti F, Fabris S, Borsetti A, Pezzuto A, Ciotti M, et al. SARS-CoV-2 lineages and sub-lineages circulating worldwide: a dynamic overview. Chemotherapy. (2021) 66:3–7. doi: 10.1159/000515340
29. Lone SA, Ahmad A. COVID-19 pandemic—an African perspective. Emerg Microbes Infect. (2020) 9:1300–8. doi: 10.1080/22221751.2020.1775132
30. Lalaoui R, Bakour S, Raoult D, Verger P, Sokna C, Devaux C, et al. What could explain the late emergence of COVID-19 in Africa? New Microbes New Infect. (2020) 38:100760. doi: 10.1016/j.nmni.2020.100760
31. Paintsil E. COVID-19 threatens health systems in sub-Saharan Africa: the eye of the crocodile. J Clin Invest. (2020) 130:2741–4. doi: 10.1172/JCI138493
32. Acter T, Uddin N, Das J, Akhter A, Choudhury TR, Kim S. Evolution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as coronavirus disease 2019 (COVID-19) pandemic: a global health emergency. Sci Total Environ. (2020) 730:138996. doi: 10.1016/j.scitotenv.2020.138996
33. Salyer S, Maeda J, Sembuche S, Kebede Y, Tshangela A, Moussif M, et al. The first and second waves of the COVID-19 pandemic in Africa: a cross-sectional study. Lancet. (2021) 397:1265–75. doi: 10.1016/S0140-6736(21)00632-2
34. Lamptey J, Oyelami FO, Owusu M, Nkrumah B, Idowu PO, Adu-Gyamfi EA, et al. Genomic and epidemiological characteristics of SARS-CoV-2 in Africa. PLoS Negl Trop Dis. (2021) 15:e0009335. doi: 10.1371/journal.pntd.0009335
35. Omais S, Kharroubi S, Zaraket H. No association between the SARS-CoV-2 variants and mortality rates in the Eastern Mediterranean Region. medRxiv preprint (2021). doi: 10.1101/2021.01.06.21249332
36. Bereketeab R. Djibouti: strategic location, an asset or a curse? J Afr Foreign Aff. (2016) 3:5–18. doi: 10.10520/EJC199947
37. Ministry of Health of Djibouti. National Action Plan for preparedness and response to COVID-19 pandemic in Djibouti. Available online at: https://sante.gouv.dj/storage/publications/April2020/cMcQEVZc9fS4wLjvUSqA.pdf (accessed March, 2021).
Keywords: SARS-CoV-2, UK variant, South African variant, Marseille 4 variant, COVID-19, epidemics, Djibouti
Citation: Osman IO, Levasseur A, Brechard L, Abdillahi Hassan I, Salah Abdillahi I, Ali Waberi Z, Delerce J, Bedotto M, Houhamdi L, Fournier P-E, Colson P, Aboubaker MH, Raoult D and Devaux CA (2021) Whole Genome Sequencing of SARS-CoV-2 Strains in COVID-19 Patients From Djibouti Shows Novel Mutations and Clades Replacing Over Time. Front. Med. 8:737602. doi: 10.3389/fmed.2021.737602
Received: 07 July 2021; Accepted: 05 August 2021;
Published: 01 September 2021.
Edited by:
Sanjay Kumar, Armed Forces Medical College, IndiaReviewed by:
Adnan Mannan, University of Chittagong, BangladeshKais Ghedira, Pasteur Institute of Tunis, Tunisia
Copyright © 2021 Osman, Levasseur, Brechard, Abdillahi Hassan, Salah Abdillahi, Ali Waberi, Delerce, Bedotto, Houhamdi, Fournier, Colson, Aboubaker, Raoult and Devaux. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christian A. Devaux, Y2hyaXN0aWFuLmRldmF1eEBtZWRpdGVycmFuZWUtaW5mZWN0aW9uLmNvbQ==
†These authors have contributed equally to this work and share last authorship
 Ikram Omar Osman
Ikram Omar Osman Anthony Levasseur
Anthony Levasseur Ludivine Brechard1,2
Ludivine Brechard1,2 Pierre-Edouard Fournier
Pierre-Edouard Fournier Philippe Colson
Philippe Colson Didier Raoult
Didier Raoult Christian A. Devaux
Christian A. Devaux