
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 22 November 2021
Sec. Ophthalmology
Volume 8 - 2021 | https://doi.org/10.3389/fmed.2021.732041
This article is part of the Research Topic Advances in the Pathophysiology, Diagnosis, And Treatment of Dry Eye Disease View all 41 articles
Purpose: This study aimed to investigate the effect of transcutaneous upper eyelid blepharoplasty on lipid layer thickness (LLT) and blink parameters in young women during the early postoperative period.
Methods: This prospective study included 110 eyes of 55 young female patients (age range, 19–31 years) who underwent transcutaneous upper eyelid blepharoplasty. The LLT and blink parameters measured using a LipiView interferometer were recorded before the surgery and 1 week and 1 month after the surgery. Ocular Surface Disease Index (OSDI) score, noninvasive tear film breakup time (NITBUT), and palpebral fissure height (PFH) measurements were also performed at each time point.
Results: The number of blinks significantly decreased (P < 0.001), and the number of partial blinks and partial blink rate (PBR) significantly increased 1 week after the surgery (P = 0.002 and P < 0.001); they all returned to baseline in 1 month. The LLT and OSDI score increased significantly 1 week and 1 month after the surgery (P < 0.001 and P < 0.001). A significant increase in the NITBUT and a significant decrease in the PFH were observed 1 week after the surgery (P < 0.001 and P < 0.001), and the values returned to baseline 1 month after the surgery. No clinical correlation was found between blink parameters and ocular surface parameters.
Conclusions: Transcutaneous upper eyelid blepharoplasty led to a change in blink parameters and ocular surface parameters during the early postoperative period. However, this influence was temporary, and the transitory change in blink parameters had no effects on the ocular surface environment.
Some Asians have a single upper eyelid or upper eyelid hypertrophy, which makes their eyes appear small and droopy, owing to the difference in fat distribution in the orbital septum and upper eyelid anatomical structures between Asians and the white race (1). Many Asians, especially young women, choose to undergo upper blepharoplasty to have a pair of attractive double eyelids. However, this surgical procedure is associated with many complications (2, 3), and dry eye disease (DED) is one of the most common complications (4). A retrospective study of 892 patients indicated that dry eye symptoms following blepharoplasty were reported in 26.5% of patients (4). Yan et al. measured subjective and objective parameters of dry eye in patients who underwent upper blepharoplasty and found that upper eyelid blepharoplasty might temporarily affect tear film dynamics and aggravate dry eye symptoms in young women. However, these changes generally disappear 3 months after the surgery (5). Zloto et al. (6) also confirmed no significant differences between the postoperative and preoperative objective and subjective dry eye tests in patients with blepharoplasty 3 months after the surgery.
However, DED is a multifactorial ocular surface disease characterized by a loss of homeostasis of the tear film (7), and a stable preocular tear film is a hallmark of ocular health (8). The tear film consists of a mucin layer, an aqueous layer, and a lipid layer. The lipid layer is important in preventing the loss of aqueous layer through overspill and evaporation (8–11). Upper blepharoplasty involved surgical removal of the skin, orbicularis oculi muscle, and (or) orbital fat, and might lead to the formation of scar and injury to the innervation, resulting in incomplete blink and decreased blink rate (3, 12). The fullness of the blink affects the stability of the tear film and its distribution in the inter-blink period (13). Moreover, the mechanical action of the lid muscles during the blink contributes to the delivery of meibomian oil (9). Jie et al. (14) indicated that partial blink would contribute to meibomian gland obstruction and subsequent loss of tear film homeostasis. Therefore, an abnormal eyeblink pattern was considered as a part of DED pathogenesis. Previously, few studies focused on the specific influence of upper blepharoplasty on eyeblink and lipid layer (15). Whether the postoperative dry eye symptoms have a correlation with the change in blink parameters and lipid layer is unclear. Thus, the lipid layer thickness (LLT) and blink parameters before and after the surgery need to be evaluated, and the specific influence of transcutaneous upper blepharoplasty on the LLT and blink parameters needs to be confirmed.
Eyeblink is a fast eyelid movement that closes and opens the palpebral fissure (13, 16, 17); it is difficult to measure and analyze blink parameters. Recently, some new devices are being used to analyze eyeblink patterns. One of these is a LipiView interferometer (TearScience, NC, USA), which provides clinicians with the LLT of the tear film and partial blink rate (PBR) (14, 18, 19).
Therefore, this prospective study was designed to observe the effect of transcutaneous upper eyelid blepharoplasty on the LLT, blink parameters, and tear film stability, and also evaluate the relationship between blink parameters, LLT, and tear film stability using the LipiView interferometer.
This single-institution prospective, observational clinical study was approved by the ethics committee of the Shanghai Ninth People's Hospital. The study began on January 1, 2019, and lasted for 10 months. It was conducted in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Prior written informed consent was obtained from all patients after receiving a detailed explanation of the study protocols and possible consequences associated with participation.
A total of 55 female patients (110 eyes) referred to the Department of Ophthalmology of Shanghai Ninth People's Hospital, who underwent upper eyelid blepharoplasty, were included in the study.
Patients with a history of ophthalmic surgeries (intraocular surgeries, eyelid surgeries, etc.); previous dry eye disease; systemic diseases as thyroid eye disease, disorders of the eyelids, and other ophthalmic diseases that required priority treatment; glaucoma; incomplete medical patient records, and age <18 years or >35 years were excluded from the study.
The surgeries were performed by a single surgeon (Y.F.) using the same techniques. The incision line was marked about 6–10 mm above the upper lid. The orbicularis oculi muscle was removed inferior to the incision within 2–3 mm. Then, the septum was incised to expose and remove the fat tissue over the top of the tarsus. The incision was closed using a 6–0 silk suture through the skin and aponeurosis.
All patients were scheduled for examinations before the surgery and 1 week and 1 month after the surgery. At each scheduled time point, subjective symptoms were evaluated using the ocular surface disease index (OSDI) questionnaire, and then clinical examinations were performed in the following order: lipid layer thickness (LLT) measurement, blink parameter analysis, noninvasive tear breakup time (NITBUT), and palpebral fissure height (PFH). All the clinical examinations were performed by a single clinician (SZ) at the same room location at each visit.
The LLT and blink parameters were analyzed with the LipiView interferometer. The patients positioned their eyes in front of an illumination source and were asked to blink freely, and a 20-s video was captured and recorded. The interferometric color unit value reflected the local LLT with 1 color unit equivalent to 1 nm of lipid layer thickness. The number of blinks and partial blinks were recorded, and PBR was calculated as the rate between the two.
The NITBUT was recorded using the Keratograph 5M (Oculus, Optikgerate, Germany). The examination was carried out and repeated three times under the condition of natural eye opening, and the average value was recorded.
The PFH was measured using an imaging system designed based on a convolutional neural network. The images of the eyes were documented at each time point.
Statistical analysis was performed with SPSS for Windows version 25.0 (SPSS Inc., IL, USA). Descriptive statistics were expressed as mean ± standard error (SE). Data were examined for normality using the Shapiro–Wilk test. A generalized estimation equation (GEE) was used to compare the variables of interest among different visits. The working correlation for each GEE model was selected using the corrected quasi-likelihood under the independence model criterion. The Spearman correlation coefficient (r) was calculated to assess the relationship between blink parameters, LLT, NITBUT, and OSDI value. All tests were two-tailed, and a P < 0.05 was considered significant.
A total of 110 eyes of 55 female patients were identified. The mean age of the participants was 25.18 ± 2.99 (mean ± standard deviation) years (range, 19–31 years). The ocular findings based on routine ancillary tests performed in the cornea clinic are shown in Table 1.
A significant decrease was observed in number of blinks and PFH 1 week after the surgery; these values returned to baseline 1 month after the surgery (number of blinks: before the surgery, 7.40 ± 0.18; 1 week after the surgery, 6.36 ± 0.17, P < 0.001; 1 month after the surgery, 7.43 ± 0.20, P = 0.73; PFH: before the surgery, 9.45 ± 0.12; 1 week after the surgery, 8.52 ± 0.13, P < 0.001; 1 month after the surgery, 9.31 ± 0.11, P = 0.08). A significant increase in the number of partial blinks and PBR was observed 1 week after the surgery, and the values 1 month after the surgery had no significant differences compared with preoperative values (number of partial blinks: before the surgery, 4.22 ± 0.34; 1 week after the surgery, 5.12 ± 0.24, P = 0.002; 1 month after the surgery, 4.29 ± 0.38, P = 0.57; PBR: before the surgery, 0.58 ± 0.05; 1 week after the surgery, 0.81 ± 0.03, P < 0.001; 1 month after the surgery, 0.58 ± 0.04, P = 0.80). The OSDI value and LLT significantly increased 1 week after the surgery and increased further 1 month after the surgery (OSDI: before the surgery, 6.48 ± 0.36; 1 week after the surgery, 8.82 ± 0.41, P < 0.001; 1 month after the surgery, 11.93 ± 0.55, P < 0.001; LLT: before the surgery, 76.74 ± 2.51; 1 week after the surgery, 89.44 ± 1.75, P < 0.001; 1 month after the surgery, 90.85 ± 1.72, P < 0.001). The mean NITBUT increased significantly and returned to preoperative levels 1 week after the surgery (before the surgery, 8.91 ± 0.40; 1 week after the surgery, 11.66 ± 0.36, P < 0.001; 1 month after the surgery, 8.72 ± 0.35, P = 0.17; Figure 1).
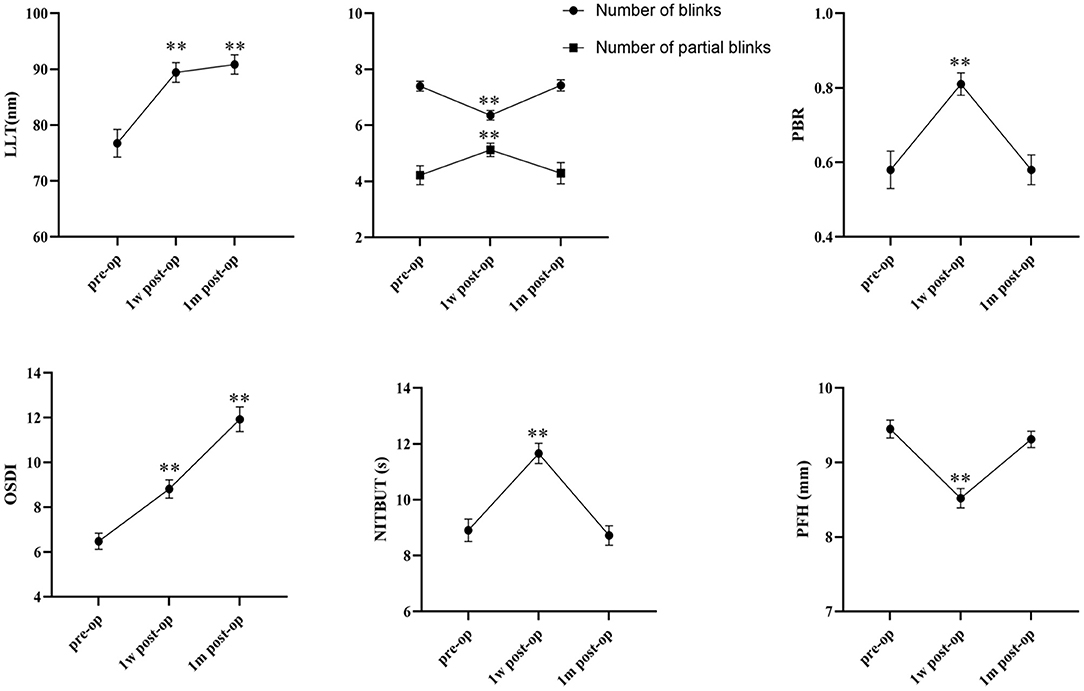
Figure 1. Graph depicting mean and standard error (SE) for OSDI, LLT, NITBUT, PFH, number of blinks, number of partial blinks, and PBR before and after upper blepharoplasty (**P < 0.001) (pre-op, preoperative; post-op, postoperative; 1w, 1 week; 1m, 1 month).
The number of blinks had a statistically significant correlation with NITBUT and LLT (r = −0.13, P = 0.02; r = −0.13, P = 0.02). The PFH correlated significantly with the NITBUT (r = −0.12, P = 0.03); but the coefficients of correlation were less than 0.2 and had no clinical significance. No correlation was found between the other parameters (Table 2).
DED is caused by a variety of iatrogenic interventions, and one of the most emblematic situations is DED caused by surgical procedures (20). The increasing number of patients looking for cosmetic procedures has drawn more attention to DED caused or worsened by blepharoplasty (21). Studies indicated that the prevalence of DED after blepharoplasty ranged from 0 to 26.5% (3, 4, 22). Previous studies investigated the changes in tear film parameters after upper blepharoplasty (6, 23), but only a few of them paid attention to the changes in lipid layer and eyeblink parameters. Therefore, this study was performed to observe the specific influence of transcutaneous upper blepharoplasty on LLT, blink parameters, and tear film stability in young Asian women during the early postoperative period, using the LipiView interferometer and Keratograph 5M.
The results showed that blink patterns changed 1 week after the surgery and returned to baseline in 1 month. The number of blinks decreased while the number of partial blinks and PBR increased 1 week after the surgery. Eyeblink is a complex process influenced by many factors, such as ocular surface damage and exposure, corneal and lid margin sensitivity, muscular fatigue and tension, and so on (16). The active forces that produce the movement of the upper eyelid during a blink are generated only by the orbicularis oculi muscle and levator palpebral superior muscle. The transcutaneous upper blepharoplasty performed in the present study involved the removal of the orbicularis oculi muscle (2–3 mm) and periorbital fat. The surgical procedure caused tissue trauma, which led to inflammatory responses and postoperative periorbital swelling. During the early postoperative period, patients blinked less and incompletely due to the swelling and incision pain. However, this phenomenon was temporary. Patients were used to the condition, and the incision pain was greatly eased 1 month after the surgery. Hence, the blink patterns returned to baseline, indicating that the limited excision of the orbicularis oculi muscle did not affect blink patterns in young patients.
In this study, the postoperative LLT significantly increased compared with the preoperative value. The driving forces leading to meibum secretion onto the lid margin and tear film are responsible for the mechanical muscular action by muscle fibers of the pretarsal orbicularis muscle, located on the outside of the tarsus, and of the marginal muscle of Riolan, which encircles the terminal part of the meibomian gland (9). The transcutaneous blepharoplasty removed part of the orbicularis muscle, but did not involve the muscle of Riolan, thus retaining the maximum driving force on the meibomian glands. The meibum is secreted by the meibomian gland through the thickness of the lids due to pressure on the glands (10). The upper eyelid is thickened due to surgical damage, and the postoperative swollen eyelid contributes to the increased pressure on the meibomian glands. The PFH decreased during the early postoperative period, indicating a reduction in the ocular surface area. Therefore, the LLT increased 1 week and 1 month after the surgery due to increased meibum secretion and decreased ocular surface area.
Previous experiments have shown that tear film breakup occurs mainly as a result of evaporation from the tear film (8). The lipid layer is of great importance for the stabilization of the air/aqueous tear interface of the tear film (11). Thus, the NITBUT increased 1 week after the surgery and returned to baseline 1 month after the surgery, indicating that the effect of blepharoplasty on the tear film breakup time was temporary.
However, despite the increased LLT and NITBUT, the results showed that OSDI values increased 1 week and 1 month after the surgery, demonstrating the worsening of the subjective symptoms of the patients. Although the patients' objective signs improved, they still complained of suffering from more severe dry eye symptoms. The main complaints of the patient were the foreign body sensation and irritation. The decreased number of blinks and increased PBR would aggravate the foreign body sensation and irritation, and led to increase of OSDI values (16). And it was assumed that postoperative inflammation and incision pain might aggravate the subjective feeling.
In addition, no correlation was observed between blink parameters and ocular surface parameters. Previous studies showed that partial blink correlated with ocular surface parameters (14, 19). However, these studies were performed on middle-aged and elderly patients with DED, while the present study was conducted on normal young women. Young women had good muscle function with a small degree of partial blink. Therefore, the blink parameters had no correlation with ocular surface parameters. Moreover, the lack of correlation between LLT and other parameters was in accordance with previous findings, highlighting the difference between the thickness of the lipid layer and its quality.
This study was novel in focusing on the effect of transcutaneous upper blepharoplasty on LLT and blink parameters in young women, while previous studies were mostly carried out on elders and paid no attention to eyeblink parameters and LLT. However, the present study had certain limitations. In the present study, the blink parameters and NITBUT returned to baseline 1 month after the surgery, which was sufficient to observe the effect of upper blepharoplasty on blink parameters. However, the LLT did not return to baseline 1 month after the surgery, which might be related to eyelid edema. In the early stage, the eyelid edema had a dominant role. However, the effect of the removal of the orbicularis muscle on the LLT when edema was eliminated remains unknown. Long-term follow-up of postoperative patients is required to confirm the findings of this study.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Shanghai Ninth People's Hospital. The patients/participants provided their written informed consent to participate in this study.
SZ: acquisition of data, drafting the article, final approval of the version to be published, and agreement to be accountable for all aspects of the work. YY: analysis and interpretation of data, drafting the article, final approval of the version to be published, and agreement to be accountable for all aspects of the work. YL: acquisition of data, revising it critically for important intellectual content, final approval of the version to be published, and agreement to be accountable for all aspects of the work. YZ: analysis and interpretation of data, revising it critically for important intellectual content, final approval of the version to be published, and agreement to be accountable for all aspects of the work. YF: substantial contributions to conception and design, revising it critically for important intellectual content, final approval of the version to be published, and agreement to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
This research was supported by the National Natural Science Foundation of China (Grant no. 81770888), Shanghai Municipal Education Commission-Gaofeng Clinical Medicine Grant Support (no. 20161421), and Shanghai Ninth People's Hospital Clinical Research Promotion Project (Grant no. JYLJ201904).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Jeong S, Lemke BN, Dortzbach RK, Park YG, Kang HK. The Asian upper eyelid: an anatomical study with comparison to the Caucasian eyelid. Arch Ophthalmol. (1999) 117:907–12. doi: 10.1001/archopht.117.7.907
2. Pacella SJ, Codner MA. Minor complications after blepharoplasty: dry eyes, chemosis, granulomas, ptosis, scleral show. Plast Reconstr Surg. (2010) 125:709–18. doi: 10.1097/PRS.0b013e3181c830c7
3. Leatherbarrow B, Saha K. Complications of blepharoplasty. Facial Plast Surg. (2013) 29:281–8. doi: 10.1055/s-0033-1349362
4. Prischmann J, Sufyan A, Ting JY, Ruffin C, Perkins SW. Dry eye symptoms and chemosis following blepharoplasty: a 10-year retrospective review of 892 cases in a single-surgeon series. JAMA Facial Plast Surg. (2013) 15:39–46. doi: 10.1001/2013.jamafacial.1
5. Yan Y, Zhou Y, Zhang S, Cui C, Song X, Zhu X, et al. Impact of full-incision double-eyelid blepharoplasty on tear film dynamics and dry eye symptoms in young asian females. Aesthetic Plast Surg. (2020) 44:2109–116. doi: 10.1007/s00266-020-01874-0
6. Zloto O, Matani A, Prat D, Leshno A, Ben Simon G. The effect of a ptosis procedure compared to an upper blepharoplasty on dry eye syndrome. Am J Ophthalmol. (2020) 212:1–6. doi: 10.1016/j.ajo.2019.11.021
7. Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, et al. TFOS DEWS II definition and classification report. Ocular Surf. (2017) 15:276–83. doi: 10.1016/j.jtos.2017.05.008
8. Willcox MDP, Argueso P, Georgiev GA, Holopainen JM, Laurie GW, Millar TJ, et al. TFOS DEWS II tear film report. Ocul Surf. (2017) 15:366–403. doi: 10.1016/j.jtos.2017.03.006
9. Knop E, Knop N, Millar T, Obata H, Sullivan DA. The international workshop on meibomian gland dysfunction: report of the subcommittee on anatomy, physiology, and pathophysiology of the meibomian gland. Invest Ophthalmol Vis Sci. (2011) 52:1938–78. doi: 10.1167/iovs.10-6997c
10. Foulks GN, Bron AJ. Meibomian gland dysfunction: a clinical scheme for description, diagnosis, classification, and grading. Ocular Surf. (2003) 1:107–26. doi: 10.1016/S1542-0124(12)70139-8
11. Georgiev GA, Eftimov P, Yokoi N. Structure-function relationship of tear film lipid layer: a contemporary perspective. Exp Eye Res. (2017) 163:17–28. doi: 10.1016/j.exer.2017.03.013
12. Hamawy AH, Farkas JP, Fagien S, Rohrich RJ. Preventing and managing dry eyes after periorbital surgery: a retrospective review. Plast Reconstr Surg. (2009) 123:353–9. doi: 10.1097/PRS.0b013e31819346ea
13. Braun RJ, King-Smith PE, Begley CG, Li L, Gewecke NR. Dynamics and function of the tear film in relation to the blink cycle. Prog Retin Eye Res. (2015) 45:132–64. doi: 10.1016/j.preteyeres.2014.11.001
14. Jie Y, Sella R, Feng J, Gomez ML, Afshari NA. Evaluation of incomplete blinking as a measurement of dry eye disease. Ocul Surf. (2019) 17:440–46. doi: 10.1016/j.jtos.2019.05.007
15. Abell KM, Cowen DE, Baker RS, Porter JD. Eyelid kinematics following blepharoplasty. Ophthalmic Plast Reconstr Surg. (1999) 15:236–42. doi: 10.1097/00002341-199907000-00003
16. Rodriguez JD, Lane KJ, Ousler GW III, Angjeli E, Smith LM, Abelson MB. Blink: characteristics, controls, and relation to dry eyes. Curr Eye Res. (2018) 43:52–66. doi: 10.1080/02713683.2017.1381270
17. Cruz AAV, Garcia DM, Pinto CT, Cechetti SP. Spontaneous Eyeblink activity. Ocular Surf. (2011) 9:29–41. doi: 10.1016/S1542-0124(11)70007-6
18. Jung JW, Park SY, Kim JS, Kim EK, Seo KY, Kim TI. Analysis of factors associated with the tear film lipid layer thickness in normal eyes and patients with dry eye syndrome. Invest Ophthalmol Vis Sci. (2016) 57:4076–83. doi: 10.1167/iovs.16-19251
19. Su Y, Liang Q, Su G, Wang N, Baudouin C, Labbe A. Spontaneous eye blink patterns in dry eye: clinical correlations. Invest Ophthalmol Vis Sci. (2018) 59:5149–56. doi: 10.1167/iovs.18-24690
20. Gomes JAP, Azar DT, Baudouin C, Efron N, Hirayama M, Horwath-Winter J, et al. TFOS DEWS II iatrogenic report. Ocul Surf. (2017) 15:511–38. doi: 10.1016/j.jtos.2017.05.004
21. Zhang SY, Yan Y, Fu Y. Cosmetic blepharoplasty and dry eye disease: a review of the incidence, clinical manifestations, mechanisms and prevention. Int J Ophthalmol. (2020) 13:488–92. doi: 10.18240/ijo.2020.03.18
22. Terella AM, Wang TD, Kim MM. Complications in periorbital surgery. Facial Plast Surg. (2013) 29:64–70. doi: 10.1055/s-0033-1333838
Keywords: upper blepharoplasty, blink, lipid layer thickness (LLT), dry eye, noninvasive tear film breakup time (NITBUT)
Citation: Zhang S, Yan Y, Lu Y, Zhou Y and Fu Y (2021) Effect of Transcutaneous Upper Eyelid Blepharoplasty on Blink Parameters and Lipid Layer Thickness. Front. Med. 8:732041. doi: 10.3389/fmed.2021.732041
Received: 28 June 2021; Accepted: 01 November 2021;
Published: 22 November 2021.
Edited by:
Xiuming Jin, Zhejiang University, ChinaReviewed by:
Lan Gong, Eye, Ear, Nose, and Throat Hospital of Fudan University, ChinaCopyright © 2021 Zhang, Yan, Lu, Zhou and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yixiong Zhou, MzUyNjcxMzBAcXEuY29t; Yao Fu, ZHJmdXlhb0AxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.