
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Med., 22 November 2021
Sec. Intensive Care Medicine and Anesthesiology
Volume 8 - 2021 | https://doi.org/10.3389/fmed.2021.731196
This article is part of the Research TopicAcute Respiratory Distress Syndrome and Mechanical VentilationView all 15 articles
Background: Spontaneous breathing trial (SBT) has been used to predict the optimal time of weaning from ventilator. However, it remains controversial which trial should be preferentially selected. We aimed to compare and rank four common SBT modes including automatic tube compensation (ATC), pressure support ventilation (PSV), continuous positive airway pressure (CPAP), and T-piece among critically ill patients receiving mechanical ventilation (MV).
Methods: We searched PubMed, EMBASE, and the Cochrane Central Register of Controlled Trials (CENTRAL) to identify studies that investigated the comparative efficacy and safety of at least two SBT strategies among critically ill patients up to May 17, 2020. We estimated the surface under the cumulative ranking curve (SUCRA) to rank SBT techniques, and determined the certainty of evidence using the Grading of Recommendations Assessment, Development and Evaluation method. Primary outcome was weaning success. Secondary outcomes were reintubation, SBT success, duration of acute care, and intensive care unit (ICU) mortality. Statistical analysis was conducted by using RevMan 5.4, Stata, and R software.
Results: We enrolled 24 trials finally. Extubation success rate was significantly higher in ATC than that in T-piece (OR, 0.28; 95% CI, 0.13–0.64) or PSV (OR, 0.53; 95% CI, 0.32–0.88). For SBT success, ATC was better than other SBT techniques, with a pooled OR ranging from 0.17 to 0.42. For reintubation rate, CPAP was worse than T-piece (OR, 2.76; 95% CI, 1.08 to 7.06). No significant difference was detected between SBT modes for the length of stay in ICU or long-term weaning unit (LWU). Similar result was also found for ICU mortality between PSV and T-piece. Majority direct results were confirmed by network meta-analysis. Besides, ATC ranks at the first, first, and fourth place with a SUCRA of 91.7, 99.7, and 39.9%, respectively in increasing weaning success and SBT success and in prolonging ICU or LWU length of stay among four SBT strategies. The confidences in evidences were rated as low for most comparisons.
Conclusion: ATC seems to be the optimal choice of predicting successful weaning from ventilator among critically ill patients. However, randomized controlled trials (RCTs) with high quality are needed to further establish these findings.
Successful weaning from mechanical ventilation (MV) refers to the gradual transition from total artificial ventilation support to spontaneous breathing. Delayed disconnection from ventilator can be associated with numerous complications, such as ventilator-associated pneumonia, airway trauma, and multiple-organ failure (MOF) (1–3). The risk of complications and mortality may accrue with increasing duration of MV (4). Therefore, it is essential to timely and safely liberate patients from mechanical ventilator when they have restored the ability of spontaneous breathing (5–8).
Spontaneous breathing trial (SBT) is one of the most common approaches to facilitate the disconnection from MV (9). Evidence-based guidelines have also recommended to conduct SBT immediately before extubation for the purpose of assessing whether a patient is able to restore the ability of spontaneous breath, and thus determine the optimal time for disconnecting from ventilator (10–14). At present, T-piece, continuous positive airway pressure (CPAP), pressure support ventilation (PSV), and automatic tube compensation (ATC) are the most common ventilation techniques (11, 12, 15–20). SBT strategies focused in this study can be categorized into three categories as follows: (a) providing constant or dynamic ventilatory support to counteract the resistance of the endotracheal tube such as PSV and ATC (21–23), (b) providing continuous positive pressure in both inspiration and expiration to enhance breathing mechanics and reduce the effort needed by mechanically ventilated patients with airflow obstruction such as CPAP (24–27), and (c) accelerating spontaneous breath of patients without positive pressure support such as T-piece, which is related to more frequent respiratory activity and consumption of more oxygen (28, 29).
Disconnection from mechanical ventilator should be conducted when patients do not experience any intolerable events after accomplishing SBT (5). However, it is still conflicting as to which SBT should be preferentially selected in route daily practice. Although many studies comparing the efficacy and safety of more than two SBT strategies have been published (21, 22, 30–40, 94), only one (32) investigated the comparative efficacy and safety of all available SBT modes simultaneously at one analysis and suggested that ATC might be superior to T-tube or CPAP for extubation success and tolerance. It must be noted that the reliability of these findings should be interpreted cautiously because these findings were generated from a single-center trial with a limited sample size. Moreover, standard ventilators were utilized in this study, which deeply compromised the accurate compensation of ATC, provided an for the workload imposed by the tube (32). Furthermore, a direct meta-analysis (41) evaluated the efficacy of common types of SBTs, and revealed that patients receiving PSV (vs. T-tube) were more likely to obtain successful extubation. However, this meta-analysis ignored the variations in populations (children and adult) and study design (randomized and quasi-randomized trials) and only provided fragmentary pairwise results, all of which limited the value of pooled results.
As an expansion of direct meta-analysis, network meta-analysis (NMA) can simultaneously combine multiple treatments (more than two) in an individual analysis at one time. Consequently, it can make comprehensive assessments of the differences between all available treatments and clearly display the hierarchies of available treatments (42, 43). We therefore conducted the present NMA of randomized controlled trials (RCTs) to comprehensively compare and rank four common SBT strategies among critically ill patients who required invasive MV for at least 24 h through evaluating weaning success, reintubation, SBT success, duration of acute care, and ICU mortality.
We conducted the present study and reported all pooled results according to the preferred reporting items for systematic review and meta-analysis for NMA (PRISMA-NMA) (44). The completed PRISMA-NMA checklist is available in Supplementary Table 1. No informed consent and institutional ethical approval if the patients were required because all analyses were completed based on published data.
We conducted a systematic literature search in PubMed, EMBASE, and CENTRAL from their inception until to May 17, 2020, and the latest search was updated on May 28, 2021. No restriction on language was imposed. The following terms were used to construct search strategy based on principle of combination of medical subject heading (MeSH) and text words: “ventilator weaning,” “spontaneous breathing trial,” “artificial respiration,” “random,” and various SBT techniques. Details of electronic search strategies and results identified are summarized in Supplementary Table 2. Any disagreements about study retrieval were solved based on consensus between two authors.
All identified potentially eligible records were firstly imported into EndNote to develop a literature database, and then duplicate records were automatically eliminated by software. In the next step, two authors (LJY and XT) independently evaluated eligibility of unique records through screening titles and abstracts. Finally, they retrieved full-texts of all potentially relevant studies for further checking eligibility. To avoid literature omissions, clinical trial registry (such as www.clinicaltrials.gov) was also searched for unpublished and undergoing trials. Moreover, reference lists of included studies and relevant reviews were also manually screened to identify additional studies. Any controversies were solved based on consensus or adjudication with a third author (MC).
For inclusion, a study should meet the following criteria: (a) enrolled adult patients suffering from respiratory failure who received invasive MV for at least 24 h regardless of gender; (b) compared at least two SBT techniques (T-piece, CPAP, ATC, or PSV); (c) reported at least one of the following outcomes including weaning success, reintubation, SBT success, duration of acute care, and ICU mortality; (d) used a RCT design with full-text. Moreover, abstract with sufficient information was also considered. A study was excluded if it covered at least one of the following criteria: (a) evaluated SBT methods in tracheostomized patients or in patients receiving noninvasive ventilation; (b) SBTs was only used as a part of the comprehensive weaning strategy; (c) with insufficient information and additional data cannot be added from authors; (d) used ineligible study design such as crossover design, quasi-randomized trials, observational studies, and commentary; and (e) duplicate study with poor methodology and insufficient data.
Our primary outcome was weaning success, which was defined as the absence of reintubation and/or resumption of ventilatory support for 48 h after extubation (45, 94). Secondary outcomes included reintubation rate (which was defined as the rate of reintubation within 48 h following extubation) (45, 94), successful SBT (if the patient showed no signs of intolerance when the SBT was performed, the SBT was considered successful) (45, 94), duration of ICU or long-term weaning unit (defined as the time from randomization to ICU or LWU) (46), and ICU mortality (defined as rate of the number of deaths during staying in ICU was divided by the number of all patients) (46).
Two authors independently extracted the following relevant information from eligible studies with a predesigned standard information extraction sheet:(a) details of the studies including the first author's name, publication year, country, publication type, study design, types of intervention and control;(b) population characteristics including ventilation time before SBT, age, and severity of the disease; (c) reported outcomes including primary and secondary outcomes. What's more, we also extracted the information about quality of included studies. Discrepancies were resolved through consulting a third author. Leading author was contacted via email if the information of interest is absent.
Two independent authors assessed the methodological quality by using the Cochrane risk of bias assessment tool from the following seven items (47, 48): random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective reporting, and other bias. Each item was labeled as low, unclear, or high risk of bias according to the evaluation criteria (47). Among these target outcomes, all except for two (ICU mortality and ICU duration) depended on subjective judgement, which means the existence of different detection bias; therefore we performed risk of bias assessment respectively. We usually assume that blinding of outcome assessment was generally low risk of bias for objective outcomes.
Network plots were produced to visualize the body of available evidence. In network geometry, each node represents a treatment and each line between the nodes represents a direct comparison. The size of the nodes and the thickness of the lines are proportional to total sample size and precision, respectively.
All analyses were done using RevMan 5.3 (used for pairwise meta-analysis) and R version 3.6.1 (used for conducting NMA with gemtc package, assessing global heterogeneity, and calculating the surface under the cumulative ranking curve [SUCRA]) and STATA version 15.0 (used for estimation of inconsistency and local heterogeneity, funnel plot, and contribution plot).
We conducted a pairwise meta-analysis for all comparisons by using the DerSimonian–Laird (DL) random-effects model. Odds ratio (OR) with 95% confidence interval (CI) was calculated for dichotomous outcome, whereas standardized mean difference with 95% CI was calculated for continuous outcome. We used Chi square and I2 statistic simultaneously to evaluate the heterogeneity across studies. I2 statistic measures the proportion of the overall variation that is attributable to between-study heterogeneity and I2 ≥ 50% was deemed as substantial heterogeneity (49, 50). For studies with multiple arms, outcome data were extracted from each group that meets the inclusion criteria, and then were created independent pairwise comparisons (43).
For each endpoint, a Bayesian random-effects NMA (51, 52) was conducted to combine direct and indirect results. We calculated the relative ranking probabilities of being the best, second best for each weaning method, and so on. What's more, we also employed the SUCRA to estimate the ranking probabilities for available weaning methods on various outcomes (53). When one weaning technique is regarded as the best one without uncertainty, SUCRA value equals 1. If not, we draw an opposite conclusion (53, 54).
To explore the inconsistency of the entire network, the design-by treatment interaction model was used (55, 56). By using the “ifplot” command, inconsistency factor (IF) was calculated in each closed loop (a loop is made up of three technologies) to estimate the local inconsistencies, with values near 1 denoting statistical consistency (57, 58). Besides, a node-splitting method was undertaken to assess the potential inconsistency between the direct and indirect evidence for each comparison, which is a node in a direct acyclic graph (59). A P of more than 0.05 was deemed as consistent, which implied that the information from both sources of evidence contains enough similarities to be combined (60). A global heterogeneity was quantified using the I2-statistic. The prediction intervals for the pooled ORs provided a limited range in which the relative effect of a future similar study is expected to be involved (61, 62). The predictive interval plot, considering the extent of heterogeneity, was used to assess the magnitude of uncertainty in the estimated effect size for the NMA (63). If uncertainty is affected by heterogeneity, discordances exist between the confidence intervals of relative treatment effects and their predictive intervals.
A contribution plot revealed the influence of each direct comparison to the estimation of the network summary effects, which helped to make an objective appraisal of the overall quality of evidence from NMA (58, 64). A comparison-adjusted funnel plot was constructed to inspect the small-study effects when sufficient number of eligible studies were analyzed in a single pair of comparison (<10) (65).
We evaluated the certainty of evidence contributing to all network estimates of the primary outcomes by using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) framework (66). Disagreements„ if any, were resolved by consulting a third researcher.
After assessment of 105 full-text articles, 24 publications involving 4,241 subjects were included to investigate the efficacy of T-piece, PSV, CPAP, and ATC in critically ill patients weaning from MV (21, 22, 30–40, 45, 67–75, 94). We designed Figure 1 to outline the details of capturing and selecting studies.
The baseline characteristics of included articles are summarized in Supplementary Table 3. The majority of the studies were designed double-arm trials (21/24, 87.5%) (21, 30, 31, 33–37, 39, 40, 45, 67–75, 94). Publication year was between 1991 and 2020, and the number of participants of individual study ranged from 14 to 578. To illustrate the head-to-head comparisons involved in the NMA, network plots for four outcomes were delineated in Figure 2. T-piece (20 studies) (21, 22, 31–33, 35, 37–40, 45, 67–73, 75, 94) and PSV (20 studies) (22, 31–33, 35–39, 45, 67, 69–75, 94) were the most frequently investigated SBT methods, whereas CPAP (six studies) (21, 22, 30, 32, 34, 38, 40, 68) and ATC(six studies) (32, 34, 36, 74) acquired fewer samples, thus suggesting a higher potential deviation in traditional meta-analysis.
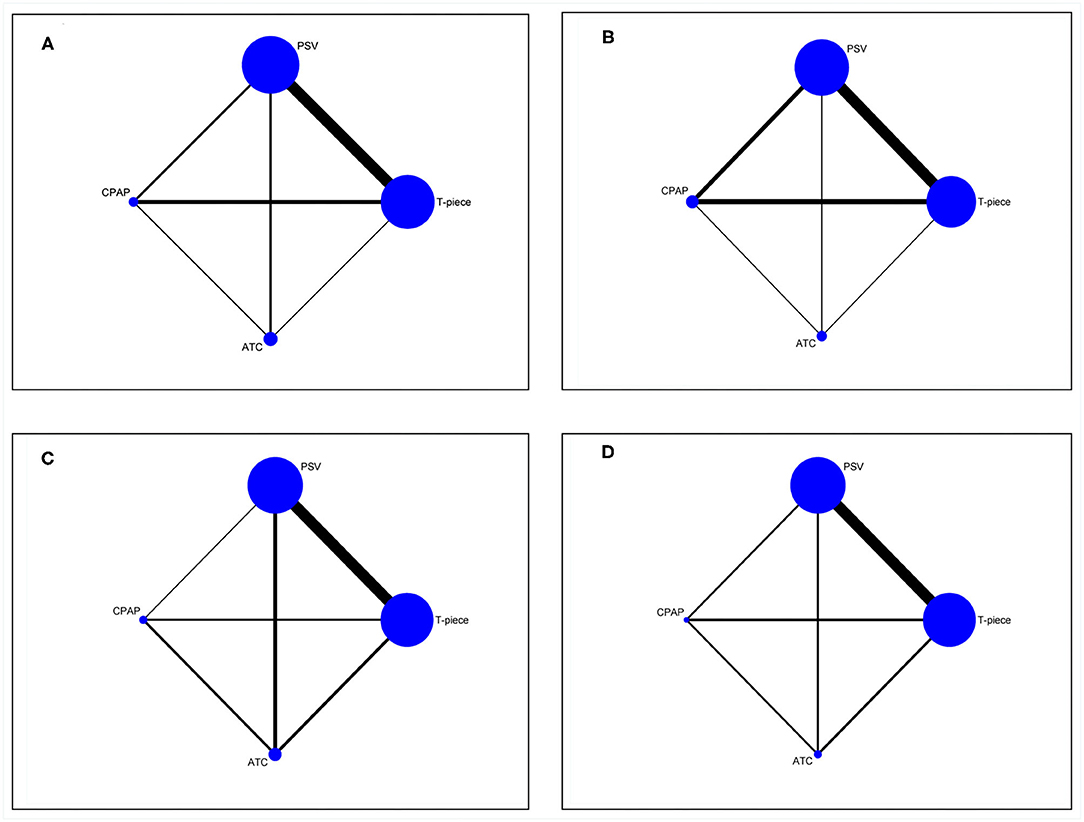
Figure 2. Evidence structure of eligible comparisons for network meta-analysis. (A) weaning success. (B). reintubation. (C) SBT success. (D) ICU or LWU length of stay. All SBT techniques are represented as blue solid circles, and existing head-to-head (direct) comparisons are drawn as black solid lines. The size of every node is proportion to the number of randomly assigned participants (sample size) and the width of the lines is proportion to the number of RCTs for each pairwise comparison. PSV, pressure support ventilation; CPAP, continuous positive airway pressure; ATC, automatic tube compensation.
Out of 24 RCTs, seven (29.1%) (32, 33, 35, 36, 45, 74, 75) did not describe the method of generating random sequence. Eight RCTs (33.3%) (33, 35, 36, 38, 39, 71, 74, 75) did not report the details of allocation concealment, which could cause potential selection bias. Besides, one study (34) stated that personnel supervising of the SBTs failed to conceal allocation, and was therefore considered to present a high risk of bias. For subjective outcomes (weaning success, reintubation, and SBT success), eight studies (21, 22, 30, 31, 34, 38, 68, 94) provided details on blinding of outcome assessors, and three articles (37, 67, 71) did not evaluate outcomes in a blinded manner. Since all studies stated a clear patient flow or used intention-to-treat analysis, there was no hint of attrition bias. What's more, no study selectively reported results. Risk of bias summary was documented in Supplementary Table 4.
The effects of four extubation strategies on weaning success from pairwise metaanalyses can be found in Figure 2A. Among six direct comparisons in direct random-effects meta-analysis, ATC was associated with increased weaning success rate compared with T-piece (OR, 0.28; 95% CI, 0.13 to 0.64) and PSV (OR, 0.53; 95% CI, 0.32 to 0.88), respectively. Remaining comparisons were not statistically significant (see Supplementary Figure 1).
In NMA, ATC was superior to the T-piece (OR, 0.34; 95% CI, 0.17 to 0.65) and PSV (OR, 0.5; 95% CI, 0.27 to 0.92) in terms of weaning success, respectively. Besides, an improvement effect of weaning success was detected for the comparison between PSV and T-piece (OR, 0.68; 95% CI, 0.45 to 0.98). Figure 3A reported all pooled results of the NMA.
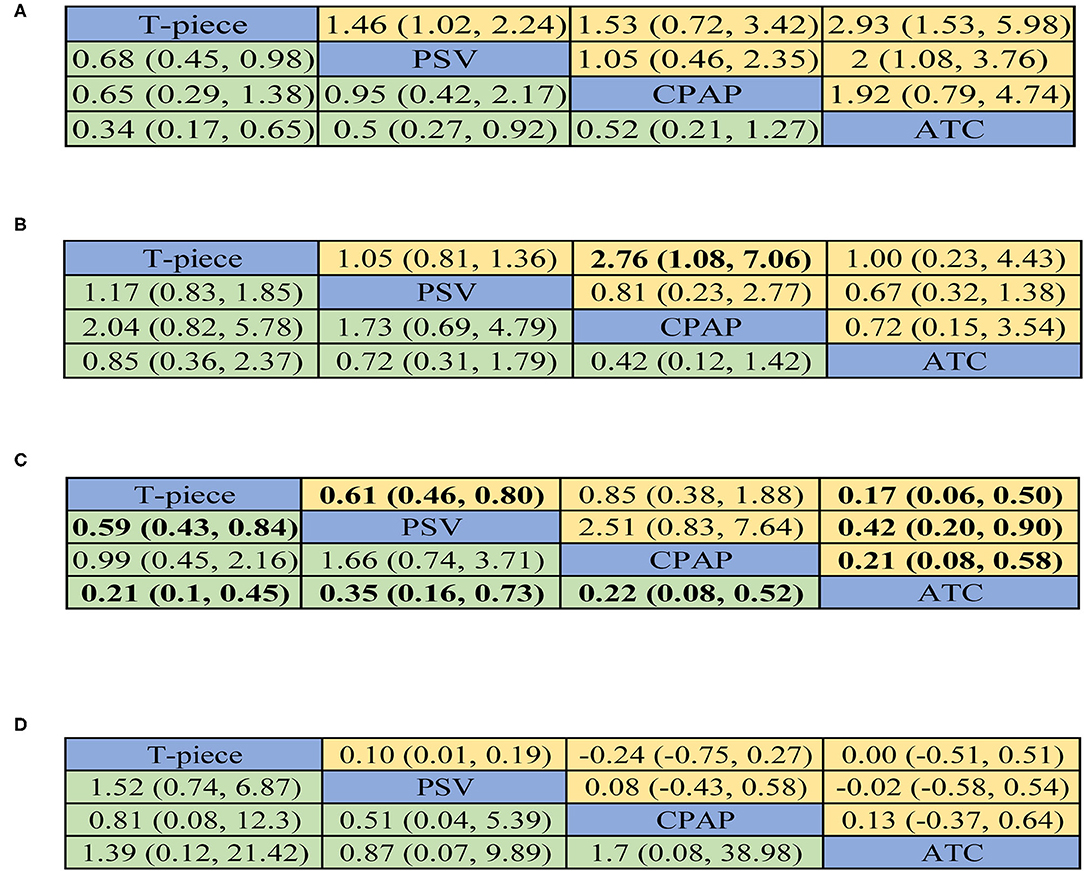
Figure 3. Summary for four outcomes of different SBT techniques. (A) weaning success. (B) reintubation. (C) SBT success. (D). ICU or LWU length of stay. If available, the upper right half presented results from pairwise meta-analysis and the left lower half showed the results from network meta-analysis. For direct comparison, odds ratios (ORs) below 1 favor the row-defining treatment. For indirect comparison, ORs below 1 favor the column-defining treatment. For numerical data, the number in each cell represented the effect size of the treatment in upper left area minus the treatment in bottom right area. Significant results are in bold print. PSV: pressure support ventilation, CPAP: continuous positive airway pressure, ATC: automatic tube compensation.
Of all 24 eligible RCTs, 17 (21, 22, 30–32, 37–40, 45, 67–69, 71–73, 94) reported the reintubation within 48 h following extubation, which included six direct comparisons (Figure 2B). CPAP could slightly decrease reintubation compared with T-piece (OR, 2.76; 95% CI, 1.08 to 7.06). All pooled results from traditional meta-analysis can be found in Supplementary Figure 2.
In NMA, all comparisons did not show significant effects on reintubation. All pooled results can be found in Figure 3B.
Of all eligible RCTs, 13 (21, 22, 32, 34, 39, 45, 67, 68, 70–73, 94) reported SBT success, which included six direct comparisons (Figure 2C). In all direct comparisons, the comparative efficacy of T-piece vs. PSV (OR, 0.61; 95% CI, 0.46 to 0.80), T-piece vs. ATC (OR, 0.17; 95% CI, 0.06 to 0.50), PSV vs. ATC (OR, 0.42; 95% CI, 0.20 to 0.90), and CPAP vs. ATC (OR, 0.21; 95% CI, 0.08 to 0.58) reached statistical significance. All pooled results from direct comparisons can be obtained in Supplementary Figure 3.
The results of comparisons of SBT success in our NMA are presented in Figure 3C. ATC exerted a trend of high SBT success when compared with T-piece (OR, 0.21; 95% CI, 0.1–0.45), PSV (OR, 0.35; 95% CI, 0.16–0.73), and CPAP (OR, 0.22; 95% CI, 0.08–0.52), respectively. PSV had significant superiority over T-piece in SBT success (OR, 0.59; 95% CI, 0.43–0.84).
Of all included RCTs, seven (31, 32, 36, 39, 69–71) reported ICU or LWU length of stay, which included six direct-comparisons (Figure 2D). In all six direct-comparisons, no major differences between the four extubation technologies were observed (Supplementary Figure 4). In NMA, no significant difference was observed in any comparisons (Figure 3D).
Of all 24 eligible studies, 10 RCTs (31, 35, 39, 45, 67, 69–71, 73, 94) which focused exclusively on T-piece and PSV investigated the ICU mortality. Direct evidence supports that there was no significant difference in the effect of PSV and T-piece (OR, 1.19; 95% CI, 0.89 to 1.59) without heterogeneity (I2 = 0%) (Supplementary Figure 5).
The test of global inconsistency detected no significant difference between the consistency and inconsistency models for four outcomes (P = 0.690 for weaning success, P = 0.523 for reintubation, P = 0.951 for STB success, and P = 0.308 for ICU or LWU length of stay, respectively). For four outcomes, test for local inconsistency showed that all loops were consistent (Supplementary Figure 6). Predictive interval plot indicated 33.3%, 0.00%, 33.3%, and 0.00% of the comparisons for weaning success, reintubation, SBT success, and ICU or LWU length of stay respectively, and therefore no outcomes was substantially affected by the estimated heterogeneity in the network (Supplementary Figure 7). The common heterogeneity through the Bayesian meta-analysis was 0.224 for weaning success, 0.020 for reintubation, 0.036 for SBT success, and 0.000 for ICU or LWU length of stay.
We showed the mean values of SUCRA for providing the hierarchy ranking of different weaning technologies on weaning success, reintubation, SBT success, and ICU or LWU length of stay. According to SUCRA, T-piece ranked fourth, second, third, and second on increase of weaning success, reintubation, SBT success and ICU or LWU length of stay, among all strategies, with a probability of 85.2%, 51.7%, 49.8%, and 44.3%, respectively. Whereas ATC had a probability of 91.7%, 62.1%, 99.7% and 39.9% to rank first, first, first, and fourth for each corresponding outcome above (Supplementary Table 5). However, considering that the sample sizes of different interventions varied greatly, the results might be highly biased and should be interpreted with caution. The ranking of all SBT technologies is depicted in Supplementary Figure 8.
According to the contribution plots of the network (see Supplementary Figure 9), the comparison of T-piece (mode A) vs. PSV (mode B) or PSV (mode B) vs. ATC (mode D) in the four entire networks showed 26.4% and 24.3% for weaning success, 32.7% and 23.9% for reintubation, 31.0% and 18.5% for SBT success, 29.5% and 19.2% for ICU or LWU length of stay, respectively.
We performed comparison-adjusted funnel-plot analysis for four outcomes (Supplementary Figure 10). The funnel plots were relatively asymmetric, highlighting that there is a significant risk of publication bias in our study.
According to GRADE, the quality of evidence ranged from very low to high, but was rated as low and as very low for most comparisons. In terms of T-piece vs. PSV, the quality was low for ICU or LWU length of stay and weaning success, and was very low for SBT success and reintubation, whereas moderate for ICU mortality. Quality of evidence was low for the overall ranking of treatment for weaning success, reintubation, ICU or LWU length of stay, and SBT success (Supplementary Table 6).
This is the first NMA on this topic. After completing all analyses, we obtained several important findings: (a) Evidence from direct and NMA showed that ATC obtained superior weaning success compared to T-piece and PSV. Besides, the direct evidence demonstrated patients receiving PSV (vs. T-piece) appeared to be more likely to be extubated successfully; (b) Direct evidence suggested that T-piece had higher reintubation rate vs. CPAP, but these findings were not be supported by network evidence; (c) Direct evidence indicated that ATC was superior to others in SBT success, PSV was also better than T-piece in terms of this given outcome, and all statistically significant findings were detected in network meta-analyses; (d) In terms of prolonging ICU or LWU length of stay, no weaning technologies have been shown superior to another which were determined both directly and thorough NMA; (e) Compared with T-piece, PSV did not show different effects on the ICU mortality, whereas this conclusion was supported by direct evidence only; (f) The ranking of all weaning modes was ATC, CPAP, PSV, and T-piece in enhancing weaning success; (g) For increasing SBT success, the ranking of all weaning modes was ATC, PSV, T-piece, and CPAP; (h) The ranking of all weaning modes was ATC, T-piece, PSV, and CPAP in terms of reintubation rate; and (i) For prolonging ICU or LWU length of stay, the ranking of all weaning modes was CPAP, T-piece, PSV, and ATC.
Automatic tube compensation is a new mode of ventilatory assistance. It potentially simulates spontaneous breathing without the endotracheal tube, and so it has been called as “electronic extubation” (76, 77). There are several possible explanations for this clinical observation that ATC might be more efficacious than other investigated SBT techniques performed before extubation in critical patients. First and foremost, according to the actual flow that assists the spontaneously breathing intubated patient (78), ATC gives dynamic pressure support during the breathing cycle, which can automatically compensate for the non-linear resistance added by the artificial airway (21, 76, 79). This characteristic of ATC causes a reduction in the work of breathing (17, 80), and thus increases the probability of successful extubation (81). Secondly, ATC is able to maintain the natural and variable breathing pattern to the greatest extent (82, 83), which can more closely represent the postextubation scenario. This potential advantage of ATC can improve synchronization between patient and ventilator, and then promote respiratory comfort (82, 84, 85). Meanwhile, it can result in more significant predictive values for successful weaning and extubation (23). Last but not least, as a result of auto-positive end expiratory pressure (PEEP), ineffective ventilator-triggering is more likely to be less common with ATC than with PSV (77). Hence, ATC is ideally suitable for the weaning process (24).
Though direct evidence suggested that T-piece had higher reintubation rate when compared with CPAP, this finding was not supported by network evidence. Since network evidence combined the direct and indirect evidence in the same analytical model and more eligible RCTs were included, these results were more reliable and accurate.
Pressure support ventilation is widely used to overcome the additional work of breathing and pressure–time product exerted by the endotracheal tubes (18, 22, 86). Consequently, it can significantly decrease the endocrine stress response and relieve the clinical picture of intolerance (37, 38, 87). Furthermore, PSV allows patients to control the respiratory rate and the inspiratory flow during the spontaneous inspiration, thereby diminishing the oxygen consumption of respiratory muscles and preventing fatigue (88–90). These may be the primary reasons why PSV SBTs result in both higher SBT and extubation success rates compared with a T-piece SBT. This finding is broadly in line with previous work. A moderate-quality evidence (91) demonstrated that some intubated subjects who previously failed a weaning trial through the T-tube but continued a weaning trial with PSV were extubated successfully. A latest large-scale multicenter trial also compared PSV and T-piece ventilation in adults and noted that PSV SBT produced significantly higher rates of successful extubation, not adversely influencing reintubation rates (70).
It was worth mentioning that several studies have exclusively investigated the efficacy and safety of at least two modalities of ventilator weaning, but primary studies comparing all the approaches have but one and cannot identify subtle clinical differences due to small sample size. To date, three traditional pairwise metaanalyses with full-text have been performed to evaluate the comparative efficacy of PSV vs. T-piece (46, 92)and PSV vs. other alternative SBT techniques (41) in patients ready to be liberated from MV. However, no head-to-head meta-analysis comparing all SBTs with each other has been reported. Consequently, that in which SBT technique is superior remains to be elucidated.
The results of Ladeira et al. (46) indicated an improvement in PSV group for successful SBTs among patients with simple weaning, but no difference between these two strategies for weaning success, ICU mortality, reintubation, ICU and LWU length of stay was found. Li et al. (92) found no difference between PSV SBT mode and T-piece SBT mode in all outcomes reported in the above-mentioned trial. Burns et al. (41)verified that extubation only tended to be more successful during PSV as compared with T-piece, but there was no difference between PSV vs. CPAP and PSV vs. ATC. After excluding an outlier trial, authors observed that patients undergoing PSV are more likely to pass an SBT. In contrast to previous metaanalyses, we comprehensively evaluated four common SBT technologies and obtained more informative findings. Firstly, we found that PSVs were associated with higher weaning success and SBT success, which is in agreement with previous results, but only these findings were confirmed by network metaanalyses. In addition, our analysis supported that ATC is an important weaning alternative for critically ill patients. Without increasing the reintubation rate and ICU or LWU length of stay, ATC provides clinical benefits in improving weaning success and SBT success. We also firstly make hierarchies of four different SBT technologies including T-piece, PSV, CPAP, and TAC, all of which were not reported in previous studies.
Our NMA has certain important strengths including (a) We designed comprehensive search algorithms to obtain and identified eligible studies in critically ill patients, thereby minimizing information bias and enhancing generalizability; (b) NMA method allowed us to assess the results from both direct comparison and mixed-treatment comparisons, and thus optimally addressing the relative effectiveness of those SBT techniques; (c) We just included RCTs, which were the highest level of evidence; so we deemed that our pooled results can reflect closely the true effectiveness of the four most commonly performed SBT modes; and (d) We rated the certainty of evidence by the GRADE approach when explaining each unique comparison and across the network.
Nevertheless, some limitations in this study merited further discussion, including (a) Due to paucity of available data, we introduced criteria for pooling ventilation techniques. Many of the trials included varied in the level of pressure or did not specify whether PEEP was added; however, when implementing similar weaning strategies, we considered them to be in a clinically similar condition and combined them into a single group. This action may induce potential heterogeneity. (b) Since few publications existed, it is impossible to assess the impact of the mode of ventilation on other important indicators, such as hospital length of stay, hospital mortality, total duration of MV, and adverse events. Currently, most of the researchers monitored patients only during ICU stay, and very little data was available when they moved into the general ward. Further studies with a larger number of patients are warranted to consider these problems to gain full insight into the real effect of various extubation strategies. (c) No trials were designed to evaluate the impact of ATC and CPAP on ICU mortality in present. Also, we only captured 10 RCTs by directly comparing PSV and T-piece focusing on this parameter; thus larger studies with excellent designs are warranted to make up the gap. (d) It is important that neither patients nor personnel could be blinded after randomization as different SBT technologies had different requirements at the different preparation stages. We believe that this factor has potential influence on the results. However, the majority of weaning and extubation studies were not free from this limitation. (e) We did not specifically stratify all interventions in the current study, which may introduce a potential bias. However, the major aim of this NMA is to generally determine the comparative efficacy and safety of available macroscopic SBT techniques. Certainly, we suggest conducting future studies to further specifically differentiate the efficacy and safety of different regimes (e.g., low, middle, or high PSV) of each SBT technique.
Spontaneous breathing trials are an integrated component of the weaning assessment, so the “weaning condition” of a patient entering to SBT will influence the accuracy of different SBT methods. On the basis of the difficulty and duration of the weaning process, patients are divided into three categories: simple weaning, difficult weaning, and prolonged weaning (12, 93). In this review, the target patients in most of the studies included belonged to simple weaning, and our analysis supported the selection of ATC as an important alternative for this group. Hence, if one method to perform SBT has any superiority over the other, improvement in weaning outcome is more likely to be expected in selected populations at higher risk for prolonged weaning and difficult weaning. Further studies should be conducted to establish this classification and to confirm how related clinical outcomes are affected in each category of weaning, finalizing the optimal weaning strategy in specific weaning situations. Meanwhile, researchers should pay more attention to ATC weaning mode to clarify its role in weaning patients off mechanical ventilation.
It must be noted that, as an objective marker of identifying the severity, the MV duration before conducting SBT can reflect the demands for ventilation, the risk of suffering from infection, and refractory bronchospasm, all of which were positively associated with worse prognosis. A previous study (69) has revealed that the MV duration before conducting SBT may greatly increase the risk of weaning failure within 48 h. However, the role of this factor under the different SBT modes (PSV, T-piece, CPAP, and ATC) and among specific populations is unclear, which should be further clarified in future studies.
In summary, the present NMA demonstrated that ATC is an alternative mode of ventilation for critically ill patients. Our finding should be interpreted with caution as it generates from RCT with small sample sizes. Further large scale and well-designed studies are needed to confirm this point.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
L-JY, XT, MC, and MJ-H: conception and design. XT and MJ-H: administrative support. L-JY, XT, and MC: provision of study materials or patients. L-JY, XT: collection and assembly of data. L-JY and XT: data analysis and interpretation. L-JY, XT, MC, J-ML, NX, and MJ-H: manuscript writing and final approval of manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
I would like to acknowledge my teammates for their wonderful collaboration. In addition, we would particularly like to express our appreciation to all authors listed in all the primary studies that were included in the current review.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.731196/full#supplementary-material
1. Esteban A, Anzueto A, Alía I, Gordo F, Apezteguía C, Pálizas F, et al. How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am J Respir Crit Care Med. (2000) 161:1450–8. doi: 10.1164/ajrccm.161.5.9902018
2. Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, Stewart TE, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. (2002) 287:345–55. doi: 10.1001/jama.287.3.345
3. Tomicic V, Espinoza M, Andresen M, Molina J, Calvo M, Ugarte H, et al. [Characteristics and factors associated with mortality in patients receiving mechanical ventilation: first Chilean multicenter study]. Rev Med Chil. (2008) 136:959–67. doi: 10.4067/S0034-98872008000800001
4. Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. (2005) 33:1266–71. doi: 10.1097/01.CCM.0000164543.14619.00
5. Epstein SK. Weaning from ventilatory support. Curr Opin Crit Care. (2009) 15:36–43. doi: 10.1097/MCC.0b013e3283220e07
6. Frutos-Vivar F, Ferguson ND, Esteban A, Epstein SK, Arabi Y, Apezteguía C, et al. Risk factors for extubation failure in patients following a successful spontaneous breathing trial. Chest. (2006) 130:1664–71. doi: 10.1378/chest.130.6.1664
7. Jindal SK, Aggarwal AN, Gupta D. Adult respiratory distress syndrome in the tropics. Clin Chest Med. (2002) 23:445–55. doi: 10.1016/S0272-5231(01)00009-0
8. Meade M, Guyatt G, Sinuff T, Griffith L, Hand L, Toprani G, et al. Trials comparing alternative weaning modes and discontinuation assessments. Chest. (2001) 120(Suppl. 6):425s−37s. doi: 10.1378/chest.120.6_suppl.425S
9. Pellegrini J, Moraes RB, Mac Ca Ri JG, Oliveira R, Teixeira C. Spontaneous breathing trials with t-piece or pressure support ventilation. Respir Care. (2016) 61:1693–703. doi: 10.4187/respcare.04816
10. Thille AW, Harrois A, Schortgen F, Brun-Buisson C, Brochard L. Outcomes of extubation failure in medical intensive care unit patients. Crit Care Med. (2011) 39:2612–8. doi: 10.1097/CCM.0b013e3182282a5a
11. MacIntyre NR, Cook DJ, Ely EW Jr, Epstein SK, Fink JB, Heffner JE, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest. (2001) 120(Suppl. 6):375s−95s. doi: 10.1378/chest.120.6_suppl.375S
12. Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. Eur Respir J. (2007) 29:1033–56. doi: 10.1183/09031936.00010206
13. Tobin MJ, Jubran A. Variable performance of weaning-predictor tests: role of Bayes' theorem and spectrum and test-referral bias. Intensive Care Med. (2006) 32:2002–12. doi: 10.1007/s00134-006-0439-4
14. Alía I, Esteban A. Weaning from mechanical ventilation. Crit Care. (2000) 4:72–80. doi: 10.1186/cc660
15. Bien MY, Hseu SS, Yien HW, Kuo BI, Lin YT, Wang JH, et al. Breathing pattern variability: a weaning predictor in postoperative patients recovering from systemic inflammatory response syndrome. Intensive Care Med. (2004) 30:241–7. doi: 10.1007/s00134-003-2073-8
16. El-Khatib M, Jamaleddine G, Soubra R, Muallem M. Pattern of spontaneous breathing: potential marker for weaning outcome. Spontaneous breathing pattern and weaning from mechanical ventilation Intensive Care Med. (2001) 27:52–8. doi: 10.1007/s001340000758
17. Fabry B, Haberthür C, Zappe D, Guttmann J, Kuhlen R, Stocker R. Breathing pattern and additional work of breathing in spontaneously breathing patients with different ventilatory demands during inspiratory pressure support and automatic tube compensation. Intensive Care Med. (1997) 23:545–52. doi: 10.1007/s001340050371
18. Kuhlen R, Max M, Dembinski R, Terbeck S, Jürgens E, Rossaint R. Breathing pattern and workload during automatic tube compensation, pressure support and T-piece trials in weaning patients. Eur J Anaesthesiol. (2003) 20:10–6. doi: 10.1097/00003643-200311000-00014
19. MacIntyre N. Discontinuing mechanical ventilatory support. Chest. (2007) 132:1049–56. doi: 10.1378/chest.06-2862
20. Wysocki M, Cracco C, Teixeira A, Mercat A, Diehl JL, Lefort Y, et al. Reduced breathing variability as a predictor of unsuccessful patient separation from mechanical ventilation. Crit Care Med. (2006) 34:2076–83. doi: 10.1097/01.CCM.0000227175.83575.E9
21. Cohen J, Shapiro M, Grozovski E, Fox B, Lev S, Singer P. Prediction of extubation outcome: a randomised, controlled trial with automatic tube compensation vs. pressure support ventilation. Crit Care (London, England). (2009) 13:R21. doi: 10.1186/cc7724
22. Haberthür C, Mols G, Elsasser S, Bingisser R, Stocker R, Guttmann J. Extubation after breathing trials with automatic tube compensation, T-tube, or pressure support ventilation. Acta Anaesthesiol Scand. (2002) 46:973–9. doi: 10.1034/j.1399-6576.2002.460808.x
23. G. Ferreyra S, Weber-Cartens V, Aquadrone. Comparison of automatic tube compensation (ATC) with pressure support ventilation (PSV) during spontaneous breathing trials. Int Care Med. (2007) 33:s57.
24. Cohen JD, Shapiro M, Grozovski E, Lev S, Fisher H, Singer P. Extubation outcome following a spontaneous breathing trial with automatic tube compensation versus continuous positive airway pressure. Crit Care Med. (2006) 34:682–6. doi: 10.1097/01.CCM.0000201888.32663.6A
25. Petrof BJ, Legaré M, Goldberg P, Milic-Emili J, Gottfried SB. Continuous positive airway pressure reduces work of breathing and dyspnea during weaning from mechanical ventilation in severe chronic obstructive pulmonary disease. Am Rev Respir Dis. (1990) 141:281–9. doi: 10.1164/ajrccm/141.2.281
26. Smith TC, Marini JJ. Impact of PEEP on lung mechanics and work of breathing in severe airflow obstruction. J Appl Physiol. (1988) 65:1488–99. doi: 10.1152/jappl.1988.65.4.1488
27. Lago AF, Goncalves EC, Silva EC, Menegueti MG, Nicolini EA, Auxiliadora-Martins M, et al. Comparison of energy expenditure and oxygen consumption of spontaneous breathing trial conducted with and without automatic tube compensation. J Clin Med Res. (2015) 7:700–5. doi: 10.14740/jocmr2250w
28. Pinsky MR. Breathing as exercise: the cardiovascular response to weaning from mechanical ventilation. Intensive Care Med. (2000) 26:1164–6. doi: 10.1007/s001340000619
29. Walsh TS. Recent advances in gas exchange measurement in intensive care patients. Br J Anaesth. (2003) 91:120–31. doi: 10.1093/bja/aeg128
30. Cekmen N, Erdemli O. The comparison of the effects of T-piece and CPAP on hemodynamic parameters, arterial blood gases and success of weaning. Bratisl Lek Listy. (2011) 112:512–6.
31. Chittawatanarat K, Orrapin S, Jitkaroon K, Mueakwan S, Sroison U. An open label randomized controlled trial to compare low level pressure support and T-piece as strategies for discontinuation of mechanical ventilation in a general surgical intensive care unit. Med Arch. (2018) 72:51–7. doi: 10.5455/medarh.2018.72.51-57
32. E. Zanfaly H. Automatic Tube Compensation versus Pressure Support Ventilation, Continuous Positive Airway Pressure and T-Tube during Spontaneous Breathing Trial. Res Opin Anesth Intensive Care. (2014) 2:35–42.
33. Faleh K, Fredj H, Maayouf H, Mokline A, Jami I, Saad MB, et al. Weaning from mechanical ventilation in burns: which weaning test in clinical practice? Ann Intensive Care. (2020) 10:105.
34. Figueroa-Casas JB, Ricardo M, Alejandro A, Connery SM. Comparison between automatic tube compensation and continuous positive airway pressure during spontaneous breathing trials. Respir Care. (2010) 55:549–54.
35. Jamoussi A, Jarraya F, Ayed S, Merhabene T, Khelil JB, Besbes M. T-piece versus sub-therapeutic pressure support for weaning from invasive mechanical ventilation in patients with chronic obstructive pulmonary disease: a comparative prospective study. Ann Intensive Care. (2020) 10:58
36. Kashefi P, Abbasi S, Katiraei F, Alikiaii B. Comparison of the weaning rate in three mechanical ventilation methods, automatic tube compensation and pressure support ventilation with airway pressure of five and eight centimeters of water. J Isfahan Med Sch. (2017) 34:1297–303.
37. Koh Y, Hong SB, Lim CM, Lee SD, Kim WS, Kim DS, et al. Effect of an additional 1-hour T-piece trial on weaning outcome at minimal pressure support. J Crit Care. (2000) 15:41–5. doi: 10.1053/jcrc.2000.7898
38. Koksal GM, Sayilgan C, Sen O, Oz H. The effects of different weaning modes on the endocrine stress response. Crit Care. (2004) 8:R31–4. doi: 10.1186/cc2671
39. Lourenço IS, Franco AM, Bassetto S, Rodrigues AJ. Pressure support-ventilation versus spontaneous breathing with “T-tube” for interrupting the ventilation after cardiac operations. Braz J Cardiovasc Surg. (2013) 28:455–61. doi: 10.5935/1678-9741.20130075
40. Jones DP, Byrne P, Morgan C, Fraser I, Hyland R. Positive end-expiratory pressure vs T-piece: extubation after mechanical ventilation. Chest. (1991) 100:1655–9. doi: 10.1378/chest.100.6.1655
41. Burns KEA, Soliman I, Adhikari NKJ, Zwein A, Wong JTY, Gomez-Builes C, et al. Trials directly comparing alternative spontaneous breathing trial techniques: a systematic review and meta-analysis. Crit Care. (2017) 21:127. doi: 10.1186/s13054-017-1698-x
42. Mavridis D, Giannatsi M, Cipriani A, Salanti G. A primer on network meta-analysis with emphasis on mental health. Evid Based Ment Health. (2015) 18:40–6. doi: 10.1136/eb-2015-102088
43. Higgins JP, Green S. Cochrane Handbook for Systematic Review of Interventions Version 5.1.0. The Cochrane Collaboration. (2011). Available online at: http://handbook.cochrane.org
44. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/M14-2385
45. Matić I, Majerić-Kogler V. Comparison of pressure support and T-tube weaning from mechanical ventilation: randomized prospective study. Croat Med J. (2004) 45:162–6.
46. Ladeira M, Vital F, Andriolo R, Andriolo B, Atallah A, Peccin M. Pressure support versus T-tube for weaning from mechanical ventilation in adults. Cochrane Database Syst Rev. (2014) 2014:CD006056. doi: 10.1002/14651858.CD006056.pub2
47. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
48. Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. (2015) 8:2–10. doi: 10.1111/jebm.12141
49. Bowden J, Tierney JF, Copas AJ, Burdett S. Quantifying, displaying and accounting for heterogeneity in the meta-analysis of RCTs using standard and generalised Q statistics. BMC Med Res Methodol. (2011) 11:41. doi: 10.1186/1471-2288-11-41
50. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
51. Ades AE, Sculpher M, Sutton A, Abrams K, Cooper N, Welton N, et al. Bayesian methods for evidence synthesis in cost-effectiveness analysis. Pharmacoeconomics. (2006) 24:1–19. doi: 10.2165/00019053-200624010-00001
52. Lumley T. Network meta-analysis for indirect treatment comparisons. Stat Med. (2002) 21:2313–24. doi: 10.1002/sim.1201
53. Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. (2011) 64:163–71. doi: 10.1016/j.jclinepi.2010.03.016
54. Lu G, Ades AE. Assessing evidence inconsistency in mixed treatment comparisons. J. Am. Stat. Assoc. (2006) 101:447–59. doi: 10.1198/016214505000001302
55. Higgins JP, Jackson D, Barrett JK, Lu G, Ades AE, White IR. Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Res Synth Methods. (2012) 3:98–110. doi: 10.1002/jrsm.1044
56. Ansai JH, Aurichio TR, Gonçalves R, Rebelatto JR. Effects of two physical exercise protocols on physical performance related to falls in the oldest old: a randomized controlled trial. Geriatr Gerontol Int. (2016) 16:492–9. doi: 10.1111/ggi.12497
57. White IR, Barrett JK, Jackson D, Higgins JP. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Res Synth Methods. (2012) 3:111–25. doi: 10.1002/jrsm.1045
58. Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS ONE. (2013) 8:e76654. doi: 10.1371/journal.pone.0076654
59. Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. (2010) 29:932–44. doi: 10.1002/sim.3767
60. van Valkenhoef G, Dias S, Ades AE, Welton NJ. Automated generation of node-splitting models for assessment of inconsistency in network meta-analysis. Res Synth Methods. (2016) 7:80–93. doi: 10.1002/jrsm.1167
61. Dias S, Sutton AJ, Welton NJ, Ades AE. Evidence synthesis for decision making 3: heterogeneity–subgroups, meta-regression, bias, and bias-adjustment. Med Decis Making. (2013) 33:618–40. doi: 10.1177/0272989X13485157
62. Guddat C, Grouven U, Bender R, Skipka G, A. note on the graphical presentation of prediction intervals in random-effects meta-analyses. Syst Rev. (2012) 1:34. doi: 10.1186/2046-4053-1-34
63. Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. (2011) 342:d549. doi: 10.1136/bmj.d549
64. Chaimani ASG. Visualizing assumptions and results in network meta-analysis: the network graphs package. Stata J. (2015) 15:905–50. doi: 10.1177/1536867X1501500402
65. Chen LX, Zhou ZR Li YL, Ning GZ, Zhang TS, Zhang D, et al. Comparison of bone mineral density in lumbar spine and fracture rate among eight drugs in treatments of osteoporosis in men: a network meta-analysis. PLoS ONE. (2015) 10:e0128032. doi: 10.1371/journal.pone.0128032
66. Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JP. Evaluating the quality of evidence from a network meta-analysis. PLoS ONE. (2014) 9:e99682. doi: 10.1371/journal.pone.0099682
67. Matić I, Danić D, Majerić-Kogler V, Jurjević M, Mirković I, Vučinić NM. Chronic obstructive pulmonary disease and weaning of difficult-to-wean patients from mechanical ventilation: randomized prospective study. Croat Med J. (2007) 48:51–8.
68. Molina-Saldarriaga FJ, Fonseca-Ruiz NJ, Cuesta-Castro DP, Esteban A. Frutos-Vivar F. Spontaneous breathing trial in chronic obstructive pulmonary disease: continuous positive airway pressure (CPAP) versus T-piece. Med Intensiva. (2010) 34:453–8. doi: 10.1016/j.medin.2010.03.007
69. Pellegrini JAS, Boniatti MM, Boniatti VC, Zigiotto C, Viana MV, Nedel WL, et al. Pressure-support ventilation or T-piece spontaneous breathing trials for patients with chronic obstructive pulmonary disease - a randomized controlled trial. PLoS ONE. (2018) 13:e0202404. doi: 10.1371/journal.pone.0202404
70. Subirà C, Hernández G, Vázquez A, Rodríguez-Garciá R, González-Castro A, Garciá C, et al. Effect of pressure support vs T-piece ventilation strategies during spontaneous breathing trials on successful extubation among patients receiving mechanical ventilation: a randomized clinical trial. JAMA. (2019) 321:2175–82. doi: 10.1001/jama.2019.7234
71. Teixeira SN, Osaku EF, de Macedo Costa CRL, Toccolini BF, Costa NL, Cândia MF, et al. Comparison of proportional assist ventilation plus, T-tube ventilation, and pressure support ventilation as spontaneous breathing trials for extubation: a randomized study. Respir Care. (2015) 60:1527–35. doi: 10.4187/respcare.03915
72. Vats N, Khanna GL, Goyal R. Improved extubation outcome with breathing exercises during spontaneous breathing trials with t-tube/pressure support ventilation, decreased pulmonary complications in thoracic cancers: a clinical trial. Indian J Physiother Occup Ther. (2016) 10:46–51. doi: 10.5958/0973-5674.2016.00081.2
73. Vats N, Singh J, Kaira S. Extubation outcome after spontaneous breathing trials with T-tube or pressure support ventilation. Indian J Physiother Occup Ther. (2012) 6:86–9.
74. Wafy S, El-Shahat H, Salama S, Bayoumi H. Automatic tube compensation versus pressure support ventilation as a weaning mode, does it make a difference? Chest. (2015) 148:312A. doi: 10.1378/chest.2250779
75. Zhang B, Qin YZ. Comparison of pressure support ventilation and T-piece in determining rapid shallow breathing index in spontaneous breathing trials. Am J Med Sci. (2014) 348:300–5. doi: 10.1097/MAJ.0000000000000286
76. Fabry B, Guttmann J, Eberhard L, Wolff G. Automatic compensation of endotracheal tube resistance in spontaneously breathing patients. Technol Health Care. (1994) 1:281–91. doi: 10.3233/THC-1994-1405
77. Stocker R, Fabry B, Haberthür C. New Modes of Ventilatory Support in Spontaneously Breathing Intubated Patients. Berlin, Heidelberg: Springer (1997). doi: 10.1007/978-3-662-13450-4_43
78. Kuhlen R, Rossaint R. Electronic extubation–is it worth trying? Intensive Care Med. (1997) 23:1105–7. doi: 10.1007/s001340050464
79. Kuhlen R, Guttmann J, Nibbe L, Max M, Reyle-Hahn S, Rossaint R, et al. Proportional pressure support and automatic tube compensation: new options for assisted spontaneous breathing. Acta Anaesthesiol Scand Suppl. (1997) 111:155–9.
80. Haberthür C, Elsasser S, Eberhard L, Stocker R, Guttmann J. Total versus tube-related additional work of breathing in ventilator-dependent patients. Acta Anaesthesiol Scand. (2000) 44:749–57. doi: 10.1034/j.1399-6576.2000.440615.x
81. Aggarwal AN, Agarwal R, Gupta D. Automatic tube compensation as an adjunct for weaning in patients with severe neuroparalytic snake envenomation requiring mechanical ventilation: a pilot randomized study. Respir Care. (2009) 54:1697–702.
82. Haberthür C, Fabry B, Zappe D, Guttmann J. Effects of mechanical unloading/loading on respiratory loop gain and periodic breathing in man. Respir Physiol. (1998) 112:23–36. doi: 10.1016/S0034-5687(98)00015-2
83. Haberthür C, Fabry B, Zappe D, Eberhard L, Trüeb K. Stulz P. Automatic tube compensation (ATC) und proportional assist V entilation (PA V) klinische erfahrungen mit einem neuen modus zur unterstützung von intubierten, spontanatmenden patienten. Intensivmed. (1996) 33:282–92.
84. Guttmann J, Bernhard H, Mols G, Benzing A, Hofmann P, Haberthür C, et al. Respiratory comfort of automatic tube compensation and inspiratory pressure support in conscious humans. Intensive Care Med. (1997) 23:1119–24. doi: 10.1007/s001340050467
85. Mols G, Rohr E, Benzing A, Haberthür C, Geiger K, Guttmann J. Breathing pattern associated with respiratory comfort during automatic tube compensation and pressure support ventilation in normal subjects. Acta Anaesthesiol Scand. (2000) 44:223–30. doi: 10.1034/j.1399-6576.2000.440302.x
86. Cabello B, Thille AW, Roche-Campo F, Brochard L, Gómez FJ, Mancebo J. Physiological comparison of three spontaneous breathing trials in difficult-to-wean patients. Intensive Care Med. (2010) 36:1171–9. doi: 10.1007/s00134-010-1870-0
87. Farias JA, Retta A, Alía I, Olazarri F, Esteban A, Golubicki A, et al. A comparison of two methods to perform a breathing trial before extubation in pediatric intensive care patients. Intensive Care Med. (2001) 27:1649–54. doi: 10.1007/s001340101035
88. Mancebo J, Amaro P, Mollo JL, Lorino H, Lemaire F, Brochard L. Comparison of the effects of pressure support ventilation delivered by three different ventilators during weaning from mechanical ventilation. Intensive Care Med. (1995) 21:913–9. doi: 10.1007/BF01712332
89. Brimacombe J, Keller C, Hörmann C. Pressure support ventilation versus continuous positive airway pressure with the laryngeal mask airway: a randomized crossover study of anesthetized adult patients. Anesthesiology. (2000) 92:1621–3. doi: 10.1097/00000542-200006000-00019
90. Brochard L, Harf A, Lorino H, Lemaire F. Inspiratory pressure support prevents diaphragmatic fatigue during weaning from mechanical ventilation. Am Rev Respir Dis. (1989) 139:513–21. doi: 10.1164/ajrccm/139.2.513
91. Ezingeard E, Diconne E, Guyomarc'h S, Venet C, Page D, Gery P, et al. Weaning from mechanical ventilation with pressure support in patients failing a T-tube trial of spontaneous breathing. Intensive Care Med. (2006) 32:165–9. doi: 10.1007/s00134-005-2852-5
92. Li Y, Li H, Zhang D. Comparison of T-piece and pressure support ventilation as spontaneous breathing trials in critically ill patients: a systematic review and meta-analysis. Crit Care. (2020) 24:67. doi: 10.1186/s13054-020-2764-3
93. Tonnelier A, Tonnelier JM, Nowak E, Gut-Gobert C, Prat G, Renault A, et al. Clinical relevance of classification according to weaning difficulty. Respir Care. (2011) 56:583–90. doi: 10.4187/respcare.00842
94. Esteban A, Alía I, Gordo F, Fernández R, Solsona JF, Vallverdú I, et al. Extubation outcome after spontaneous breathing trials with T-tube or pressure support ventilation. The Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med. (1997) 156:459–65. doi: 10.1164/ajrccm.156.2.9610109
Keywords: spontaneous breathing trials, weaning, mechanical ventilation, meta-analysis, systematic review
Citation: Yi L-J, Tian X, Chen M, Lei J-M, Xiao N and Jiménez-Herrera MF (2021) Comparative Efficacy and Safety of Four Different Spontaneous Breathing Trials for Weaning From Mechanical Ventilation: A Systematic Review and Network Meta-Analysis. Front. Med. 8:731196. doi: 10.3389/fmed.2021.731196
Received: 26 June 2021; Accepted: 19 October 2021;
Published: 22 November 2021.
Edited by:
Chunbo Chen, Maoming People's Hospital, ChinaReviewed by:
Denise Battaglini, Ospedale San Martino (IRCCS), ItalyCopyright © 2021 Yi, Tian, Chen, Lei, Xiao and Jiménez-Herrera. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria F. Jiménez-Herrera, bWFyaWEuamltZW5lekB1cnYuY2F0
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.