- 1Department of Critical Care Medicine, The First Affiliated Hospital, Guizhou University of Chinese Medicine, Guiyang, China
- 2Department of Critical Care Medicine and Infection Prevention and Control, The Second People‘s Hospital of Shenzhen & First Affiliated Hospital of Shenzhen University, Health Science Center, Shenzhen, China
- 3Department of Critical Care Medicine, General Hospital of Southern Theater Command of PLA, Guangzhou, China
- 4The First School of Clinical Medicine, Southern Medical University, Guangzhou, China
Background: Heatstroke is a common clinical symptom in summer with high mortality requiring identification of appropriate and rapid methods of assessment.
Method: This is a retrospective study that included the recent 10 years clinical data of heatstroke patients. A total of n = 186 patients were included in this study and grouped based on platelet (PLT) abnormality observed on admission.
Results: In the study group, n = 120 patients (64.5%) patients had normal PLT and n = 66 patients (35.5%) had abnormal PLT. Compared with PLT-normal group, PLT-abnormal group had higher Acute Physiology and Chronic Health Evaluation II (APACHE II) scores [median 15.0 (IQR 11.5–21.5) vs. 9.0 (IQR 7.0–12.5)] and SOFA scores [median 6.0 (IQR 4.0–10.0) vs. 2.0 (IQR 2.0–4.0)], lower Sequential Organ Failure Assessment (GCS)[median 8.0 (IQR 5.0–12.0) vs. 13.0 (IQR 9.0–14.0)]. The PLT-abnormal group had severe organ damage, including damage to the coagulation system, liver, and kidney (all p < 0.05). Significant differences were noted in 90-day survival between the two groups even after correction for Age, GCS, White blood cell count (WBC), Neutrophil, International normalized ratio (INR), Activated partial thromboplastin time (APTT), Procalcitonin (PCT), Alanine aminotransferase (ALT), Creatine (CR), D-Dime (D-D) (Before correction P < 0.001; After correction P = 0.009).The area under the ROC curve for the prediction of mortality based on PLT was 80.7% (95% CI 0.726–0.888, P < 0.001), the optimal cutoff value was 94, the sensitivity was 77.3%, and the specificity was 82.6%.
Conclusion: Patients with heatstroke with platelet abnormalities during admission have more severe organ impairment and a lower 90-day survival rate even when adjusted for other factors.
Introduction
Heatstroke is a common clinical symptom in any season especially in summer, manifesting as multi-system inflammation caused by central hyperthermia and eventually multi-organ dysfunction, mortality up to 40% (1, 2). Heatstroke can be clarified in exertional heatstroke or classic heatstroke. Classic heatstroke occurs mostly in older patients, especially those with chronic diseases, they have weak ability to regulate thermal stimulation and are easily affected by high temperature stimulation. Exertional heatstroke usually occurs in athletes, soldiers or worker engaged in outdoor physical labor and it usually occurs under the condition of continuous high temperature and high intensity exercise. The best way to diagnose heatstroke is with rapid body temperature assessment and evaluation of central nervous system status. Since much of the research on exertional heatstroke indicates cellular damage occurs when body temperature exceeds 40.5 C for 30 min. It is very important to find an effective indicator to quickly evaluate the severity and prognosis of the disease. Platelets stop bleeding and participate in thrombosis (3). Platelet abnormality is a risk factor for evaluating the prognosis of a variety of diseases (4–6). Hence this study, retrospectively analyzed the clinical data of patients admitted to hospital for severe heatstroke in the past 10 years, and evaluated early platelet changes on the prognosis of patients with heatstroke for timely and effective clinical treatment.
Methods
Study Design and Participants
This single-center retrospective case-control study collected all patients with heatstroke admitted to the ICU of the General Hospital of Southern Theater Command in China from October 2008 to May 2019.
The inclusion criteria were as follows: (1) age > = 18 years old; (2) met the diagnostic criteria of severe heatstroke described below; (3) The diagnostic criteria for heatstroke were as follows: classic or exertional heatstroke with a history of exposure to hot and humid weather or strenuous activity, concurrent hyperthermia (central temperature above 40°C), and neurological dysfunction, including delirium, cognitive disorders, and disturbed consciousness. The exclusion criteria were as follows: (1) existing irreversible underlying diseases affecting mortality and (2) pregnancy or breastfeeding.
Research Procedures
The base data of patients were collected, including inflammatory and organ function parameters on admission. Patients were divided into the PLT-normal and PLT-abnormal group according to whether their PLT is normal or not. The main result was 90-day mortality. Survival curve analysis was also performed and ROC curve analysis of PLT to assess the 90-day mortality of heatstroke patients. The PLT-abnormal group was further divided into the Survivors subgroup and Non-survivors subgroup, and the characteristics of the subgroups were compared.
Definitions
Diagnostic criteria for platelet abnormalities: platelet count (PLT) <100(1 × 109/L) or platelet count >300(1 × 109/L).
Statistical Analysis
The categorical data are expressed as numbers and percentages, and intergroup comparisons were performed with the Mann-Whitney U test, χ2 test, or Fisher's exact test. Continuous variables are expressed as the medians and interquartile ranges. Continuous data with a Gaussian distribution were compared with Student's t-test or one-way ANOVA, and those with a non-Gaussian distribution were compared with the Wilcoxon rank-sum test. The patient endpoint event was death within 90 days after onset. The survival curve was drawn using the Kaplan-Meier method. Significant indicators were identified using single-factor analysis, ROC curves were used to predict the prognosis of patients according to PLT. Statistical analyses were performed using the SPSS Windows version 11.0 statistical package (SPSS Inc, Chicago, IL), and P values (two-tailed) <0.05 were considered statistically significant.
Results
Demographics and Baseline Characteristics
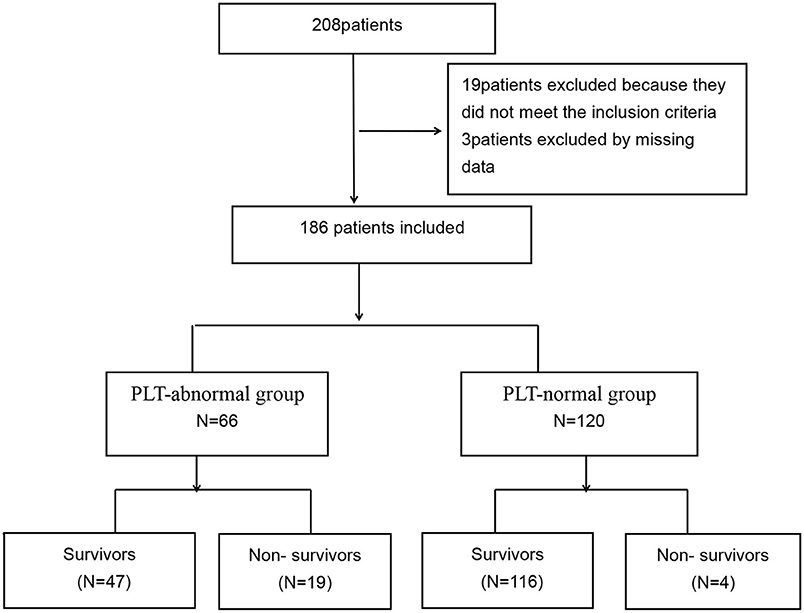
A total of 208 patients were included. After screening, 28 patients were excluded because they did not meet the inclusion criteria, 3 patients were excluded by missing data, 19 patients excluded because they did not meet the inclusion criteria, and 186 patients were finally included (Figure 1). All 186 patients were male, with a mean age of 21.0 years (IQR 19.0–27.0), Acute Physiology and Chronic Health Evaluation II (APACHE II) scores of 11.0 (IQR 8.0–16.0), Sequential Organ Failure Assessment (SOFA) scores of 3.0 (IQR 2.0–6.0), and GCS score of 12.0 (IQR 7.0–14.0). There were 120 patients (64.5%) patients with normal PLT and 66 patients (35.5%) with abnormal PLT.
Comparison of Groups
Compared with PLT-normal group, PLT-abnormal group had higher APACHE II scores [median 15.0 (IQR 11.5–21.5) vs. 9.0 (IQR 7.0–12.5)] and SOFA scores [median 6.0 (IQR 4.0–10.0) vs. 2.0 (IQR 2.0–4.0)], lower GCS [median 8.0 (IQR 5.0–12.0) vs. 13.0 (IQR 9.0–14.0)]. PLT-abnormal group had severe organ damage, including damage to the coagulation system, liver and kidney (all p < 0.05) (Table 1).
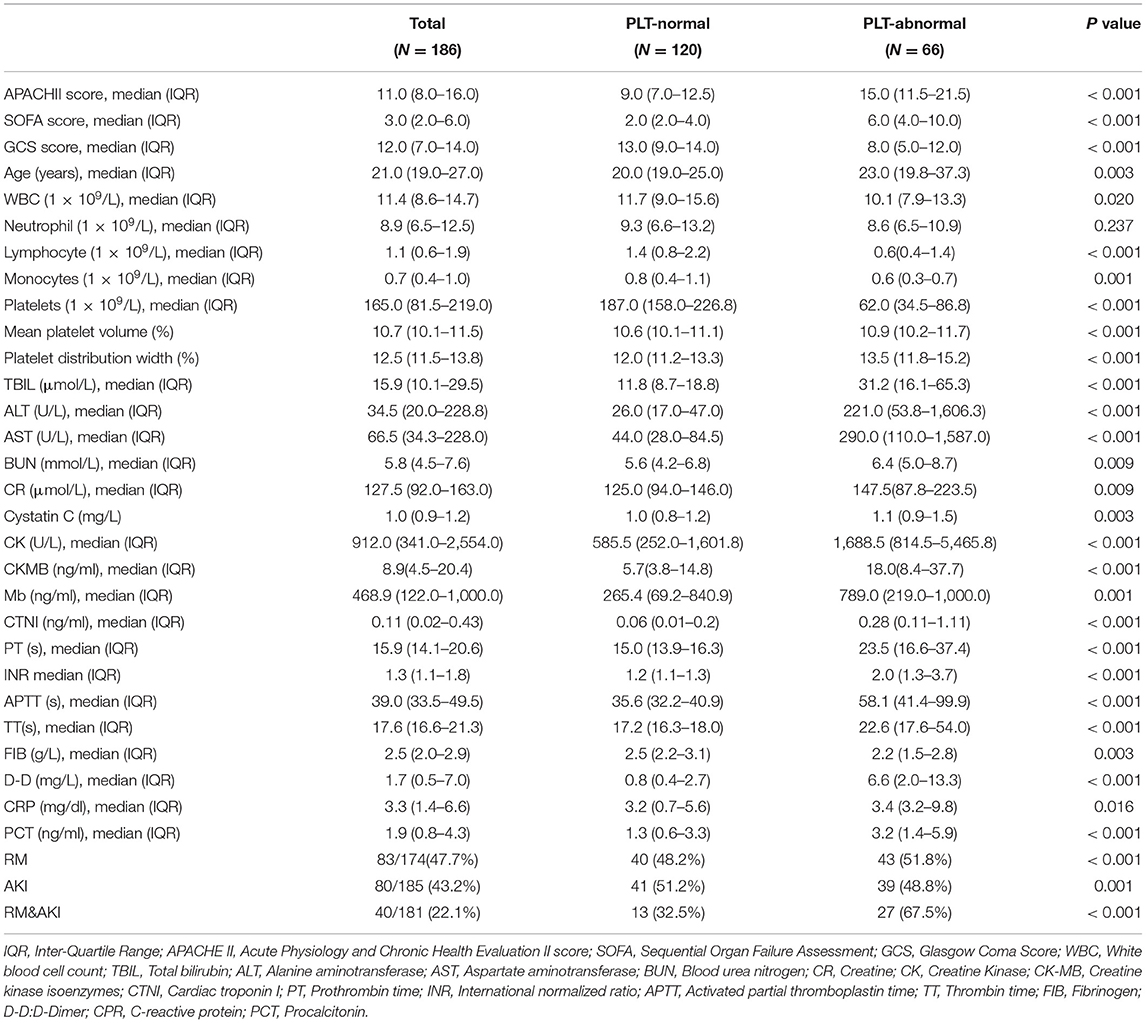
Table 1. Baseline characteristics of clinical and laboratory findings in PLT-normal group and PLT-abnormal group.
Main Outcomes
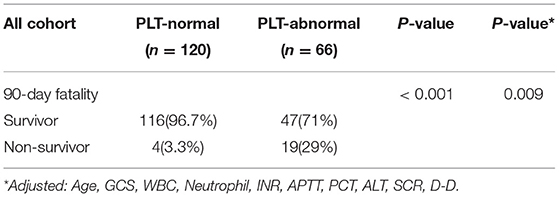
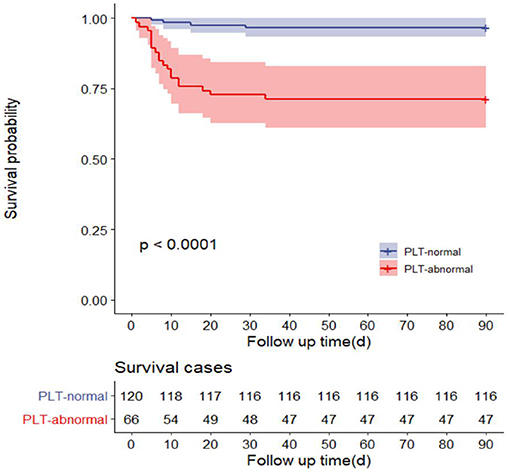
The 90-day mortality rate of the PLT-abnormal group was 29% (19/66), while that of the PLT-normal group was 3.3% (4/120). There were statistically significant differences in 90-day survival between the two groups even after correction for Age, GCS, White blood cell count (WBC), Neutrophil, International normalized ratio (INR), Activated partial thromboplastin time (APTT), Procalcitonin (PCT), Alanine aminotransferase (ALT), Creatine (CR), D-Dime (D-D) (Before correction P < 0.001; After correction P = 0.009) (Table 2). Survival analysis showed that the 90-day survival time of patients with PLT-abnormal group was shorter than that of the PLT-normal group (P < 0.001) (Figure 2).
Subgroup Analysis
In the subgroup analysis of the PLT-abnormal group, there were 47 survivors (71.2%) and 19 Non-survivors (28.8%).Compared with survivors, non-survivors had higher APACHE II scores [median 22.0 (IQR 17.8–23.5) vs. 14.0 (IQR 10.0–18.0)], higher SOFA scores [median 13.5 (IQR 8.8–15.0) vs. 6.0 (IQR 3.0–7.0)], lower GCS [median 4.0 (IQR 3.0–7.3) vs. 10.0 (IQR 6.0–14.0)]. In addition, kidney and blood coagulation system was more serious in the non-survivors (P < 0.05), (Table 3).
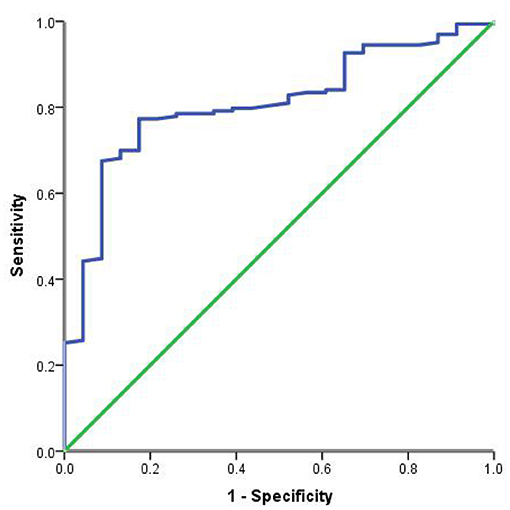
Risk Factor Analysis
The area under the ROC curve for the prediction of mortality based on PLT was 80.7% (95% CI 0.726–0.888, P < 0.001), the optimal cutoff value was 94 (1 × 109/L), the sensitivity was 77.3%, and the specificity was 82.6% (Figure 3).
Discussion
In this retrospective cohort study, patients with heat stroke and abnormal platelets at the time of admission had more serious organ function damage, mainly blood coagulation, liver, and kidney damage. Compared with patients without platelet abnormalities, patients with platelet abnormalities had a reduced 90-day survival rate. The cut-off value of PLT predicted by the ROC curve was 94(1 × 109/L), the sensitivity was 77.3%, and the specificity was 82.6%.
In our study, it was found that 35.5% of heatstroke patients had abnormal platelets, of which thrombocytopenia was the majority. Those with platelet abnormalities will suffer more severe organ function damage, mainly blood clotting, liver, and kidney damage, which is consistent with previous studies (7). Platelet count and function play an important role in the coagulation lesions of heatstroke, and platelet activation is triggered by heat and/or endothelial injury (7). Heatstroke can lead to inflammation, coagulation, and direct cytotoxic effects, damage to endothelial cells, leading to microthrombosis, and eventually platelet depletion, which can lead to coagulation disorders and even DIC (8). Thrombocytopenia is an important finding in the development of HS-induced Acute kidney injury (AKI) (9, 10). AKI patients are combined with renal blood flow reduction, renal tissue ischemia, and hypoxia, fibrinolytic system disorders, causing abnormal coagulation, that are mainly manifested as platelet function loss (11). Heatstroke can lead to dysfunction of multiple organs, including liver damage. Serotonin from platelets are released and involved in pathophysiological processes such as liver injury response, regulation of liver function, and regeneration (12).
PLT has been evaluated in sepsis, diabetes, cardiovascular disease, and other diseases, and is correlated with disease severity and prognosis (13–16). PLT count is also part of the scoring for heatstroke patients (17). What makes our study different from other studies is that we investigated the effect of early platelet changes on 90-day prognosis in a population with exertional heat stroke, not limited to patients with AKI. In addition, we had a relatively long follow-up period, and prognostic parameters were adjusted for statistical analysis. The clinical characteristics of patients with platelet abnormality were analyzed in detail, which was not mentioned in other literatures. ROC curve analysis of platelets, and prediction of cut-off values, which further clarified the prognostic value of platelets for heatstroke patients. In our study, it was also found that compared with patients without platelet abnormality, the 90-day survival rate of patients with platelet abnormality was lower, and the sensitivity and specificity were 77.3% and 82.6% when the PLT of 94 (1 × 109/L) was taken as the critical point for predicting the 90-day death of patients with severe heatstroke. In the pathophysiological process of heatstroke, the relationship between heatstroke and platelets is very complex. Heatstroke damages platelets through heat stress and inflammation, and platelets aggravate the condition by activating coagulation response and further amplifying inflammation response (18). Therefore, platelets can assess the severity of heatstroke patients to a certain extent, contribute to the evaluation of the prognosis of heatstroke patients, and provide a reference for the selection of clinical treatment options.
This study has some limitations. First, it is a single-center cohort study with a relatively small number of cases. A multi-center study will be conducted in the later stage to increase the sample size and increase the statistical reliability. Second, exertional heatstroke is a special disease that occurs mainly in people who are engaged in heavy physical labor and exercise, often in a predominantly male group. In addition, due to estrogen protection and other factors, women under equal conditions rarely develop heatstroke. Therefore, our study subjects are also mainly male and may not fully reflect the changes of platelets in the overall population. Third, it is true that early recognition and treatment is crucial for heatstroke survivability, and the patients in our study usually received basic treatment before admission, including simple cooling and symptomatic support therapy. However, these information were pre hospital data. This study is a retrospective study, so we can not accurately obtain all these information, which is also one of the limitations of this study.
Conclusion
Patients with heatstroke who are admitted to hospital with platelet abnormalities have more severe organ impairment and a lower 90-day survival rate even when adjusted for other factors.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Medical Ethics Committee of the Southern Theater General Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
LZ and MW: data collection and analysis and manuscript preparation. JJ and CW: data collection and analysis. ZL: study designed, data collection and analysis, manuscript preparation, and review. All authors read and approved the final manuscript.
Funding
This work was supported by grants from the National Natural Science Foundation of China [NO. 82072143], grants from the Natural Science Foundation of Guangdong Province of China [NO. 2021A1515010170], and grants from the PLA Logistics Research Project of China [18CXZ030 and BLJ20J006].
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Morris A, Patel G. “Heat Stroke,” In: StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © (2020) StatPearls Publishing LLC., 2020.
2. Gauer R, Meyers BK. Heat-related illnesses. Am Fam Physician. (2019) 99:482–9. doi: 10.13201/j.issn.1009-5918.2017.05.005
3. Krishnegowda M, Rajashekaraiah V. Platelet disorders: an overview. Blood Coagul Fibrinolysis. (2015) 26:479–91. doi: 10.1097/01.mbc.0000469521.23628.2d
4. Wang JJ, Wang YL, Ge XX, et al. Prognostic values of platelet-associated indicators in resectable lung cancers. Technol Cancer Res Treat. (2019) 18:1533033819837261. doi: 10.1177/1533033819837261
5. Yang WChen YY Bi C, et al. Predictive and prognostic values of preoperative platelet parameters in patients with gynecological tumors. J Clin Lab Anal. (2020) 34:e23295. doi: 10.1002/jcla.23295
6. Budak YU, Polat M, Huysal K. The use of platelet indices, plateletcrit, mean platelet volume and platelet distribution width in emergency non-traumatic abdominal surgery: a systematic review. Biochem Med. (2016) 26:178–93. doi: 10.11613/BM.2016.020
8. Al-Mashhadani SA, Gader AM, Al Harthi S. The role of platelets in the coagulopathy of heatstroke—a study of platelet aggregation in heatstroke patients during the Makkah pilgrimage (Haj) to Makkah. Platelets. (1997) 8:37–42. doi: 10.1080/09537109777528
9. Fan H, Zhao Y, Zhu JH, et al. Thrombocytopenia as a predictor of severe acute kidney injury in patients with heat stroke. Ren Fail. (2015) 37:877–81. doi: 10.3109/0886022X.2015.1022851
10. Xing L, Liu SY, Mao HD, Zhou KG, Song Q, Cao QM. The prognostic value of routine coagulation tests for patients with heat stroke. Am J Emerg Med. (2021) 44:366–72. doi: 10.1016/j.ajem.2020.04.062
11. Celep RB, Unlu BS. Retrospective platelet values measurement. Is it acceptable to discuss? Eur Rev Med Pharmacol Sci. (2014) 18:1108.
12. Nocito A, Georgiev P, Dahm F, et al. Platelets and platelet-derived serotonin promote tissue repair after normothermic hepatic ischemia in mice. Hepatology. (2007) 45:369–76. doi: 10.1002/hep.21516
13. Guclu E, Durmaz Y, Karabay O. Effect of severe sepsis on platelet count and their indices. Afr Health Sci. (2013) 13:333–8. doi: 10.4314/ahs.v13i2.19
14. Laursen MA, Larsen JB, Larsen KM, et al. Platelet function in patients with septic shock. Thromb Res. (2020) 185:33–42. doi: 10.1016/j.thromres.2019.11.011
15. Strauss R, Wehler M, Mehler K, et al. Thrombocytopenia in patients in the medical intensive care unit: bleeding prevalence, transfusion requirements, and outcome. Crit Care Med. (2002) 30:1765–71. doi: 10.1097/00003246-200208000-00015
16. Zeng Z, Xia L, Fan X, et al. Platelet-derived miR-223 promotes a phenotypic switch in arterial injury repair. J Clin Invest. (2019) 129:1372–86. doi: 10.1172/JCI124508
Keywords: heatstroke, platelets, APACHE II scores, SOFA scores, mortality
Citation: Zhong L, Wu M, Ji J, Wang C and Liu Z (2021) Association Between Platelet Levels on Admission and 90-day Mortality in Patients With Exertional Heatstroke, a 10 Years Cohort Study. Front. Med. 8:716058. doi: 10.3389/fmed.2021.716058
Received: 28 May 2021; Accepted: 20 October 2021;
Published: 11 November 2021.
Edited by:
Ata Murat Kaynar, University of Pittsburgh, United StatesReviewed by:
Seda Akinci, Hacettepe University, TurkeyKevin C. Miller, Central Michigan University, United States
Copyright © 2021 Zhong, Wu, Ji, Wang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhifeng Liu, WmhpZmVuZ2xpdTc3OTdAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Li Zhong
Li Zhong Ming Wu
Ming Wu Jingjing Ji
Jingjing Ji Conglin Wang
Conglin Wang Zhifeng Liu
Zhifeng Liu