
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 19 August 2021
Sec. Intensive Care Medicine and Anesthesiology
Volume 8 - 2021 | https://doi.org/10.3389/fmed.2021.713733
This article is part of the Research TopicLung Ultrasound and COVID-19 Interstitial Pneumonia in Different Medical Care SettingsView all 5 articles
 Yuan Zhang1,2†
Yuan Zhang1,2† Rong Chen1,2†
Rong Chen1,2† Chen Cao3†
Chen Cao3† Yuan Gong4†
Yuan Gong4† Qin Zhou1,2
Qin Zhou1,2 Min Wei5
Min Wei5 ZhongYuan Xia1,2
ZhongYuan Xia1,2 XiangDong Chen6‡
XiangDong Chen6‡ QingTao Meng1,2*‡
QingTao Meng1,2*‡Background: SARS-CoV-2 infection was referred to sympathetic hyperactivity, which might increase the susceptibility of neuraxial anesthesia-related hypotension resulted from sympathetic inhibition. We conducted a multicenter, retrospective, propensity score matched (PSM) cohort study to determine whether COVID-19 parturients have an increased risk of hypotension after neuraxial anesthesia for cesarean delivery.
Methods: Clinical data of COVID-19 parturients were collected from the electronic medical records from 1th January to 31th May, 2020 in three hospitals of Hubei Province, China. Information of Control parturients (without COVID-19) were obtained at the same institutions over a similar period in 2019. All American Society of Anaesthesiologists (ASA) Physical Status II full termed pregnant women who received cesarean delivery under neuraxial anesthesia were included. The primary objective was to obtain and compare the incidence of neuraxial anesthesia-related hypotension. Secondary objectives were the analysis of anesthetic implementation and administration, intraoperative maternal vital signs and adverse reactions, and neonatal Apgar scores at 1 and 5 min after delivery. The clinical characteristics of COVID-19 parturients were also analyzed. PSM was derived to balance the predictors for neuraxial anesthesia-related hypotension based on previous studies.
Results: In present study, 101 COVID-19 parturients and 186 Control parturients were derived from 1,403 cases referenced to propensity score matching. The incidence of neuraxial anesthesia-related hypotension was 57.4% in COVID-19 parturients and 41.9% in Control parturients with an incidence risk ratio (IRR) of 1.37 (95% CI 1.08–1.74; P = 0.012; post-hoc Cramér's V = 0.15) in the PSM cohort. The incidences of nausea, vomiting, dizziness, and shaking were significantly higher in the COVID-19 group than Control group (48.5 vs. 17.2%, P < 0.001; 10.9 vs. 4.3%, P = 0.03; 18.8 vs. 3.2%, P < 0.001; 51.5 vs. 18.3%, P < 0.001; respectively). The Apgar scores at 1 min was significantly lower in newborns from COVID-19 parturients than that in Control babies (P = 0.04).
Conclusions: An increased risk of neuraxial anesthesia-related hypotension in COVID-19 parturients undergoing cesarean delivery should be stressed.
A novel coronavirus (SARS-CoV-2) infection disease (COVID-19) has devastated the global community since the end of 2019 (1). More importantly, mutations in SARS-CoV-2 might (partly) escape the immune response which led to a large drop in efficacy of vaccine. Several studies have forecasted a second rebound of COVID-19 would be manifested in countries with outbreaks (2, 3). We have to pay more attention to the current COVID-19 pandemic to cope with the unexpected medical scenarios.
Although the clinical characteristics of COVID-19 in pregnant women are similar with non-pregnant women (4), COVID-19 results in additional challenges for obstetric anesthesia as reported in previous study (5, 6). The most preferred method for cesarean delivery is neuraxial anesthesia [epidural anesthesia (EA), spinal anesthesia (SA), and combined epidural–spinal anesthesia (CES)] which allows parturients to remain respiration and avoids the effects of general anesthetic on newborns. Meanwhile, sympathetic blockade induced by neuraxial anesthesia can provoke maternal hypotension which has a potential risk for transient tachypnea of newborns (7). Several studies have examined the incidence and associated factors of hypotension after neuraxial anesthesia in healthy parturients undergoing cesarean delivery (8–11). However, parturients with COVID-19 have not been included in those studies.
Angiotensin-converting enzyme 2 (ACE2) has recently been identified as the SARS-CoV-2 receptor. Binding by SARS-CoV-2 attenuated the cardiovascular protection of ACE2 system, which closely linked with sympathetic overactivation and renin-angiotensin system overflow (12, 13). Besides, both psychological stress after being diagnosed with COVID-19 and emotional components associated with clinical isolation may further hasten sympathetic excitation (13). Enhanced sympathetic activity combined with hypoxemia induced by pulmonary inflammation would add significant stress to cardiovascular system. A latest study found the incidence of autonomic dysfunction (sympathetic, parasympathetic, or both) was 78.0% in mild COVID-19 patients, which resulted in a higher risk of orthostatic hypotension when compared with un-COVID-19 patients (14). Cardiovascular system complications in COVID-19 patients increasingly become a concern (15). However, the effects of SARS-CoV-2 infection on hemodynamics of parturients who underwent neuraxial anesthesia for cesarean delivery are still unclear.
In the present study, we conducted a retrospective analysis to obtain and compare the prevalence of neuraxial anesthesia-related hypotension during cesarean delivery in COVID-19 parturients and control parturients (without COVID-19).
Ethical approval for this study (No. WDRY2020-K077) was provided by the Institutional Review Board at Renmin Hospital of Wuhan University, Wuhan, China (Chairperson Prof. Hong Chen) on 29 February 2020. The study received exemption from informed consent. All personal information were removed from the database to protect patients' confidentiality.
A multicenter, retrospective, propensity score matched cohort study was designed to compare the incidence of neuraxial anesthesia-related hypotension in parturients with and without COVID-19 undergoing cesarean delivery. The methodology reported in this study was accordance with the recommendations of the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement (16).
Renmin Hospital of Wuhan University, Union Hospital Affiliated to Tongji Medical College of Huazhong University of Science and Technology, and Yichang Central People's Hospital were designated as the diagnosis and treatment center for COVID-19 patients (including pregnant women) in Hubei province during the pandemic. SARS-CoV-2 nucleic acid test was used to screen COVID-19 in all parturients. And the chest CT scan was performed on parturients after delivery. We planned to collect all of the available COVID-19 parturients undergoing cesarean delivery who met the inclusion/exclusion criteria in three hospitals from 1th January to 31th May, 2020. And, information of control parturients (without COVID-19) were obtained at the same institutions over a similar period in 2019. We identified patients with a primary International Classification of Diseases, Tenth Revision (ICD-10) diagnosis code of cesarean delivery from the electronic medical records to establish the study cohort. All ASA Physical Status II full termed pregnant women who received cesarean delivery (ICD-10 codes O82.0–O82.9, and O84.2 for cesarean delivery) under neuraxial anesthesia were eligible for inclusion in the study. Parturients who had a cesarean delivery after failed vaginal delivery were also included. The exclusion criteria included severe complicated births, significant bleeding (intraoperative bleeding over 1,000 ml), inadequate blockade (requiring addition of a general anesthetic administration) or incomplete data. The same inclusion and exclusion criteria were used for both two groups in present study.
A post-hoc estimated effect size (Cramér's V) for the study was assessed by comparing the incidence of neuraxial anesthesia-related hypotension between parturients with and without COVID-19 before and after propensity score matching (PSM). The clinical data including patient demographics, anesthesia management, and intraoperative records were independently collected using prefabricated forms and cross checked by two investigators in each institution in order to maintain the quality and consistency of data.
Neuraxial anesthesia protocols for cesarean delivery are similar in three institutions. Before initiation of anesthesia, an intravenous line, ECG, pulse oximetry, and non-invasive automatic blood pressure monitors (1- or 2-min interval) were placed. The puncture procedure was performed in the left lateral decubitus position. Block height was assessed bilaterally using loss of cold sensitivity to alcohol at an interval of 3–5 min. All patients were delivered oxygen by face masker and placed in the supine position with a right hip wedge after puncture procedure until the end of the surgical procedure. All BP recordings in this study were performed with the patient in the supine position.
The main objective of this study was to obtain and compare the prevalence of neuraxial anesthesia-related hypotension during cesarean delivery in COVID-19 parturients and control parturients (without COVID-19). Hypotension was defined as the systolic blood pressure (SBP) below 100 mmHg, or the mean arterial blood pressure (MAP) below 80% of the baseline value (the mean of repeated measurements before commencing anesthesia) (17, 18). Given the administration of vasopressors and fluid for prophylactic or treatment of hypotension depended heavily on anaesthesiologists, infusion volume over 1,000 ml or vasoconstrictor utilization were also considered as the presence of hypotension. Neuraxial anesthesia-related hypotension was based on a single episode of defined hypotension from the time of local anesthetic injection until 15 min after delivery of the newborn. The secondary objective was the analysis of anesthetic implementation and administration (full stomach, antiemetic utilization, infusion volume, site of puncture, approach of puncture, frequency of puncture, dose of local anesthetic, vasoconstrictor, and oxytocin utilization), intraoperative vital signs (SBP, MAP, heart rate, and SaPO2), intraoperative adverse reactions (hypoxia (SaPO2 <95%), arrhythmia, nausea, vomiting, dizziness, and shaking), and neonatal Apgar scores at 1 and 5 min after delivery. The clinical characteristics (COVID-19 diagnosis, signs and symptoms, and preoperative laboratory parameters) of COVID-19 parturients also be analyzed.
We derived PSM to balance the predictors for neuraxial anesthesia-related hypotension based on previous studies (8–11, 19–25). Maternal age, body mass index (BMI), baseline heart rate, baseline MAP, baseline SBP, urgency of surgery, anesthetic technique (including EA, SA, and CES), sensory block height, the time interval between neuraxial anesthesia block and start of surgery (block-surgery time), newborns weight and experience of anaesthesiologists were included in the calculation of propensity scores with multivariate logistic regression in our study. Matching was performed without replacement with a 1: 2 matching protocol and a caliper width of 0.03. The quality of the PSM was assessed in two ways. First, we visually assessed propensity score histograms for two groups before and after PSM. Second, absolute standardized difference (ASD) <10% for a given covariate was considered well-balanced.
All statistical analyses were performed using Stata/SE 15.1 (Stata Corp, College Station, TX, USA). Continuous variables are expressed as Mean ± standard deviation (SD) or Median (inter-quartile range, IQR). Categorical variables are expressed as Number (proportion). The Mann-Whitney U-test, χ2 or Fisher's exact test were used on appropriate. A two-tailed P < 0.05 was considered as statistical significance.
The study flowchart was shown in Figure 1. Among 1,538 eligible subjects, we included 1,403 subjects [102 parturients infected with SARS-CoV-2 (COVID-19 group), and 1,301 parturients without (Control group)] for PSM after exclusion of individuals with inadequate blockade (84 cases) or incomplete data (51 cases). After PSM, 287 patients were created, with 101 cases in COVID-19 group and 186 cases in Control group. The characteristics of predictors for neuraxial anesthesia-related hypotension before and after PSM were shown in Table 1. There were statistically significant differences (P < 0.05) between COVID-19 and Control groups across several variables before PSM, including urgency of surgery (P < 0.01), anesthetic technique (P < 0.01), the time interval between EA initiation and surgery start (P = 0.02), and anaesthesiologist experience (P = 0.02). Parturients with preoperative comorbidities (such as chronic hypertension and hypertensive disorders of pregnancy) which were known to impact maternal blood pressure were not found in the PSM cohort. There were no significant differences between two groups for any of the measured variables after PSM. Meanwhile, ASD for all variables were <10%, indicating that the propensity scores were well-matched (Table 1).
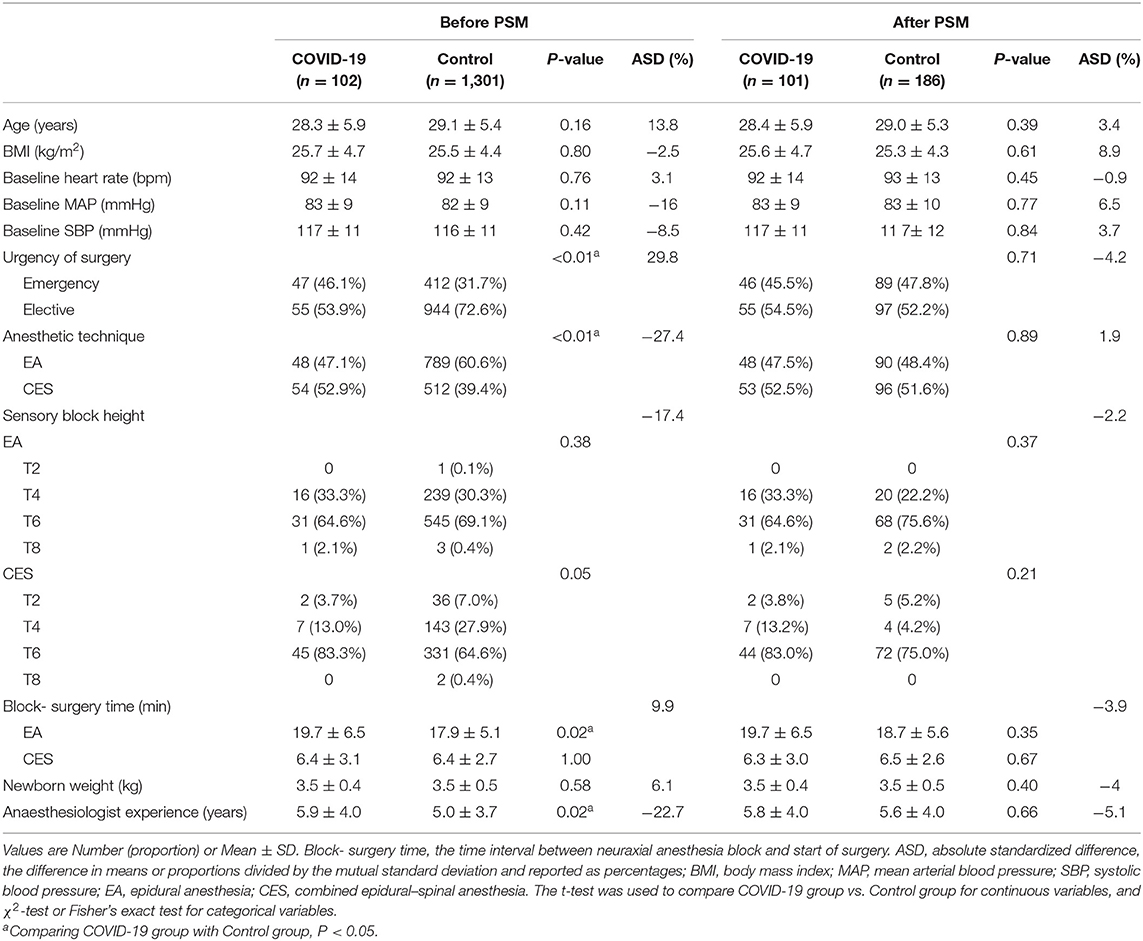
Table 1. The characteristics of predictors for neuraxial anesthesia-related hypotension in parturients before and after propensity score matching (PSM).
As shown in Table 2, the incidence of neuraxial anesthesia-related hypotension was higher in COVID-19 group than that in Control group before and after PSM [57.8 vs. 39.1% (P < 0.001); 57.4 vs. 41.9% (P = 0.01), respectively]. The incidence risk ratio for neuraxial anesthesia-related hypotension in parturients were 1.48 (95% CI 1.24–1.77) and 1.37 (95% CI 1.08–1.74) before and after PSM, respectively. At the 0.05 significance level, the un-PSM cohort had lower Cramér's V-value (0.10 vs. 0.15) than PSM cohort.
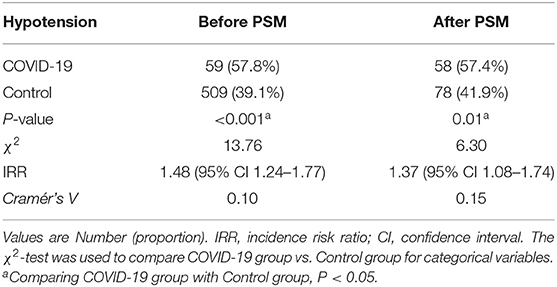
Table 2. The incidences of neuraxial anesthesia-related hypotension in COVID-19 group vs. Control group before and after propensity score matching (PSM).
In PSM cohort, COVID-19 parturients had more times of puncture (P < 0.001) and higher rate of vasoconstrictor utilization (P = 0.02) than Control parturients. However, there were no significant differences between two groups across those variables, including the rate of full stomach, antiemetic and oxytocin utilization, infusion volume and type of fluids, site and approach of puncture, and the dose of local anesthetic (Table 3). COVID-19 group showed significantly higher than Control group in MAP, but not in SBP, heart rate, and SaO2%. The incidences of nausea, vomiting, dizziness, and shaking were significantly higher in COVID-19 group than Control group (48.5 vs. 17.2%, P < 0.001; 10.9 vs. 4.3%, P = 0.03; 18.8 vs. 3.2%, P < 0.001; 51.5 vs. 18.3%, P < 0.001; respectively). There was no significant difference in the incidence of maternal tachycardia (P = 0.46) between two groups (No other arrhythmia was observed). And intraoperative hypoxia wasn't observed in two groups (Table 4). The Apgar score of newborns at 1 min (P = 0.04) after birth was significantly lower in COVID-19 group than that in Control group (Table 5), while no significant difference at 5 min (P = 0.36).
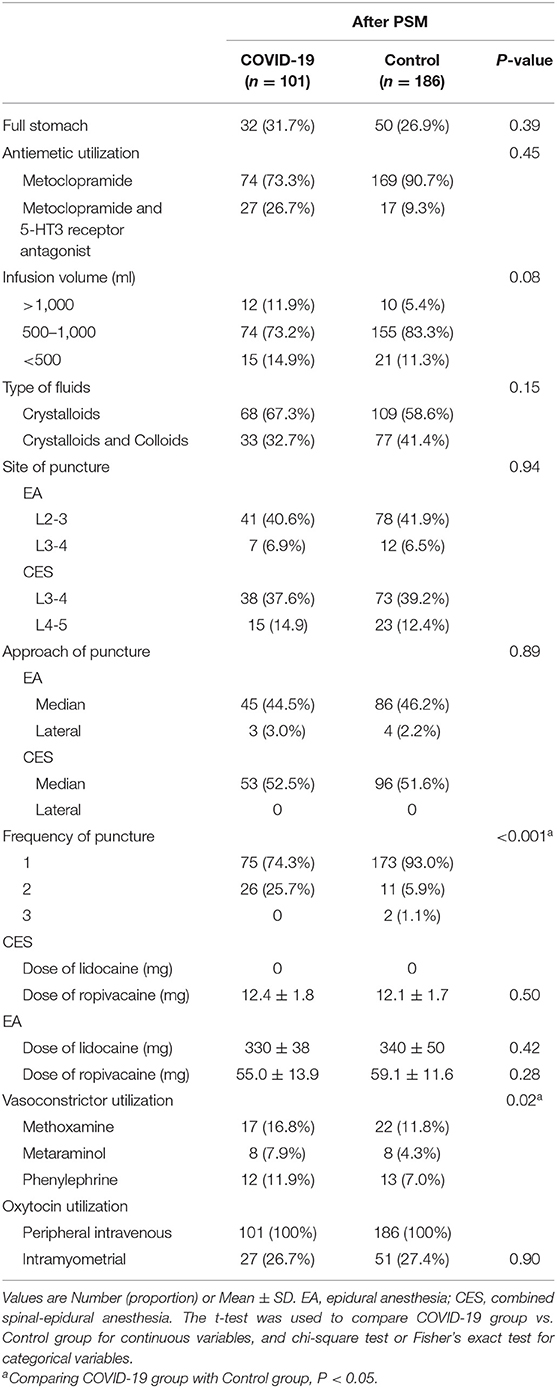
Table 3. Anesthetic implementation and administration in COVID-19 group vs. Control group after propensity score matching (PSM).
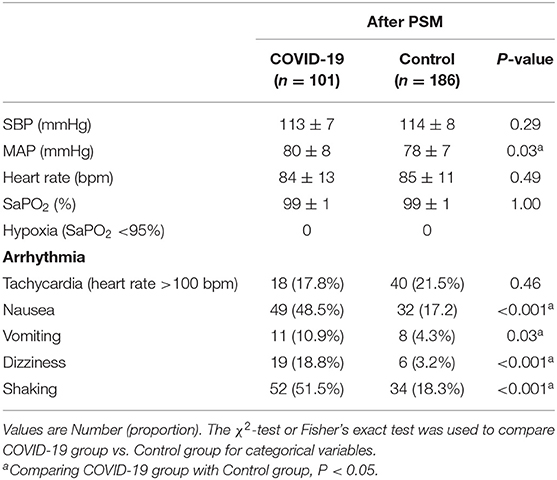
Table 4. Intraoperative maternal vital signs and adverse reactions in COVID-19 group vs. Control group after propensity score matching (PSM).

Table 5. Neonatal Apgar scores in COVID-19 group vs. Control group after propensity score matching (PSM).
Among COVID-19 parturients, there were no significant differences in the signs, symptoms, and preoperative laboratory parameters between parturients with neuraxial anesthesia-related hypotension and without (all P > 0.05, Supplementary Table 1). Body temperature over 37.4°C (38.6%) and cough (32.7%) were the main signs and symptoms, respectively. The other signs and symptoms included fatigue (9.9%), chest distress (14.6%), dyspnea (8.9%), and diarrhea (6.9%). Significant difference of neonatal Apgar scores at 1 min (P = 0.046), but not 5 min (P = 0.35), was observed in COVID-19 parturients with neuraxial anesthesia-related hypotension vs. without (Table 6).
In this study, we conducted a retrospective analysis of the incidence of neuraxial anesthesia-related hypotension in parturients with or without COVID-19 undergoing cesarean delivery. Our data suggested that parturients with COVID-19 might experience neuraxial anesthesia-related hypotension more frequently than without.
Previous studies showed that the incidences of hypotension in parturients who underwent a cesarean section were 32–52% after EA, 43–64% after SA, and 32–70% after CES (8–11, 20–22, 26). In present study, the incidences of hypotension after neuraxial anesthesia were ~58 and 40% in parturients with and without COVID-19, respectively. These different results might be attributed to several reasons, such as definition of hypotension, methods and interval time of measurement, and experience of anaesthesiologist (10, 11, 23, 24). Additionally, the short-lived hypotension might also be missed or rapidly recovered by vasoconstrictor pre-treatment. Given the underestimation of risk of hypotension in the retrospective study design, we adopted a loosen hypotension definition in present study.
A recent study found that baby weight, baseline SBP, sensory block height, the time interval between spinal induction and skin incision, and experience of anaesthesiologists were associated with SA-related hypotension in obstetric surgery (11). Maternal age, BMI, weight gain, gravidity, history of hypotension, baseline heart rate, fluid preloading, and anesthetic adjuvant were also demonstrated to be predictive factors for SA-related hypotension in cesarean delivery (10). Chronic alcohol consumption, history of hypertension, ASA physical status, urgency of surgery, surgical department, amount of local anesthetic, and preload liquid were found to have a critical predictive value for the incidence of hypotension in SA and CES for non-obstetric surgery (23, 24). According to evidences above, maternal age, BMI, baseline heart rate, MAP, SBP, urgency of surgery, anesthetic technique, sensory block height, block- surgery time, newborn weight, and anaesthesiologist experience were employed to calculate the propensity scores in present study. However, significant differences were only found in urgency of surgery, anesthetic technique, block- surgery time of EA, and anaesthesiologist experience between COVID-19 group and Control group in un-PSM cohort of present study. The effects of COVID-19 epidemic on urgency of surgery and the choice of anesthetic technique should be taken into account during anesthesia and investigated in future studies.
There was a higher incidence of hypotension in obese parturients during neuraxial anesthesia due to vascular compression by hypertrophic uterus (27). A left-tilt position has been commonly used in parturients, particularly in obese parturients. Nevertheless, a recent study declared that the hemodynamic parameters derived from a non-invasive cardiac output monitoring system were not statistically different between the left-tilt and supine position (28). Pre-administration of vasoconstrictor and volume most likely concealed the appearance of hypotension (18, 29, 30).
Consistent with previous studies, our data also revealed anaesthesiologist experience in association with the risk of neuraxial anesthesia-related hypotension (11). An experienced anaesthesiologist can protect parturients with low baseline BP or high level of sensory blockade from high risk of hypotension. Intriguingly, there was a significantly higher incidence of hypotension in COVID-19 group than that in Control group before PSM, although those anaesthesiologists had more experience. In the PSM cohort, experience of anaesthesiologists was comparable in two groups, but COVID-19 parturients still had a higher incidence of neuraxial anesthesia-related hypotension and vasoconstrictor utilization. Those results supported COVID-19 parturients were at an increased risk for neuraxial anesthesia-related hypotension. Additionally, COVID-19 parturients suffered more times of puncture in present study. Part of this difference seems due to the personal protective equipment of anaesthesiologists.
ACE2 dysfunction induced by SARS-CoV-2 infection was referred to virus toxicity, hypoxia status, inflammation, and sympathetic hyperactivity (31), which might increase the susceptibility of neuraxial anesthesia-related hypotension resulted from sympathetic inhibition in COVID-19 parturients. Although clinical practices have demonstrated that neuraxial anesthesia is a safe technique for obstetric anesthesia in COVID-19 parturients (5, 6, 32, 33), higher incidences of hypotension and discomforts, and lower Apgar scores at 1 min were observed in COVID-19 parturients and their babies in present study. More evidences derived from a larger sample size and randomized controlled trails are also needed to determine the effects and mechanisms of COVID-19 on hemodynamics of parturients undergoing neuraxial anesthesia for cesarean delivery.
Clinical practice, such as anesthetic technique, local anesthetic concentration, vasopressor, and volume administration, were not sufficiently standardized in this multicenter retrospective study in order to draw conclusive conclusions. And, a post-hoc estimated power value 0.71 and effect size (Cramér's V-value) 0.15 after PSM would be another limitation. However, an increased risk of neuraxial anesthesia-related hypotension in COVID-19 parturients undergoing cesarean delivery should be stressed.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Institutional Review Board at Renmin Hospital of Wuhan University, Wuhan, China (Chairperson Prof. Hong Chen). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
QM and XC designed the study. YZ, RC, CC, YG, and QZ collected the data. CC and YG analyzed and interpreted the work. YZ and RC drafted the manuscript. ZX and MW revised it critically for important intellectual content. All authors contributed to the manuscript and approved the final version.
This work was supported by grants from the National Natural Science Foundation of China (81671948 and 81801085).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Assistance with the study: We would like to thank Prof. Daqing Ma, Ph.D., FRCA for his assistance with the study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.713733/full#supplementary-material
Supplementary Figure 1. Summaries of the balance of covariates before and after propensity score matching. Absolute standardized difference <10% for a given covariate was considered well balanced. Block- surgery time, the time interval between neuraxial anesthesia block and start of surgery; BMI, body mass index; SBP, systolic blood pressure; MAP, mean arterial blood pressure.
Supplementary Table 1. Clinical characteristics of COVID-19 parturients with or without hypotension. Values are Number (proportion) or Median (IQR).
1. Zhou P, Yang X-L, Wang X-G, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. (2020) 579:270–3. doi: 10.1038/s41586-020-2012-7
2. Malki Z, Atlam E-S, Ewis A, Dagnew G, Alzighaibi AR, ELmarhomy G, et al. ARIMA models for predicting the end of COVID-19 pandemic and the risk of second rebound. Neural Comput Appl. (2020) 18:833–41. doi: 10.1007/s00521-020-05434-0
3. Panovska-Griffiths J, Kerr CC, Stuart RM, Mistry D, Klein DJ, Viner RM, et al. Determining the optimal strategy for reopening schools, the impact of test and trace interventions, and the risk of occurrence of a second COVID-19 epidemic wave in the UK: a modelling study. Lancet Child Adolesc Health. (2020) 4:817–27. doi: 10.1016/S2352-4642(20)30250-9
4. Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. (2020) 370:m3320. doi: 10.1136/bmj.m3320
5. Chen R, Zhang Y, Huang L, Cheng B-H, Xia Z-Y, Meng Q-T. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing cesarean delivery: a case series of 17 patients. Can J Anaesth. (2020) 67:655–63. doi: 10.1007/s12630-020-01630-7
6. Ashokka B, Chakraborty A, Subramanian BJ, Karmakar MK, Chan V. Reconfiguring the scope and practice of regional anesthesia in a pandemic: the COVID-19 perspective. Reg Anesth Pain Med. (2020) 45:536–43. doi: 10.1136/rapm-2020-101541
7. Singh S, Lumbreras-Marquez MI, Farber MK, Xu X, Singh P, Gorman T, et al. Transient tachypnea of newborns is associated with maternal spinal hypotension during elective cesarean delivery: a retrospective cohort study. Anesth Analg. (2019) 129:162–7. doi: 10.1213/ANE.0000000000004064
8. Bishop DG, Cairns C, Grobbelaar M, Rodseth RN. Heart rate variability as a predictor of hypotension following spinal for elective caesarean section: a prospective observational study. Anaesthesia. (2017) 72:603–8. doi: 10.1111/anae.13813
9. Bishop DG, Cairns C, Grobbelaar M, Rodseth RN. Obstetric spinal hypotension: preoperative risk factors and the development of a preliminary risk score - the PRAM score. South Afr Med J. (2017) 107:1127–31. doi: 10.7196/SAMJ.2017.v107i12.12390
10. Fakherpour A, Ghaem H, Fattahi Z, Zaree S. Maternal and anaesthesia-related risk factors and incidence of spinal anaesthesia-induced hypotension in elective caesarean section: a multinomial logistic regression. Indian J Anaesth. (2018) 62:36–46. doi: 10.4103/ija.IJA_416_17
11. Shitemaw T, Jemal B, Mamo T, Akalu L. Incidence and associated factors for hypotension after spinal anesthesia during cesarean section at Gandhi Memorial Hospital Addis Ababa, Ethiopia. PLoS ONE. (2020) 15:e0236755. doi: 10.1371/journal.pone.0236755
12. Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong J-C, Turner AJ, et al. Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: celebrating the 20th anniversary of the discovery of ACE2. Circ Res. (2020) 126:1456–74. doi: 10.1161/CIRCRESAHA.120.317015
13. Del Rio R, Marcus NJ, Inestrosa NC. Potential role of autonomic dysfunction in covid-19 morbidity and mortality. Front Physiol. (2020) 11:561749. doi: 10.3389/fphys.2020.561749
14. Milovanovic B, Djajic V, Bajic D, Djokovic A, Krajnovic T, Jovanovic S, et al. Assessment of autonomic nervous system dysfunction in the early phase of infection with SARS-CoV-2 virus. Front Neurosci. (2021) 15:640835. doi: 10.3389/fnins.2021.640835
15. Zheng Y-Y, Ma Y-T, Zhang J-Y, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. (2020) 17:259–60. doi: 10.1038/s41569-020-0360-5
16. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology. (STROBE) statement: guidelines for reporting observational studies. Int J Surg. (2014) 12:1495–9. doi: 10.1016/j.ijsu.2014.07.013
17. Klöhr S, Roth R, Hofmann T, Rossaint R, Heesen M. Definitions of hypotension after spinal anaesthesia for caesarean section: literature search and application to parturients. Acta Anaesthesiol Scand. (2010) 54:909–21. doi: 10.1111/j.1399-6576.2010.02239.x
18. Singh PM, Singh NP, Reschke M, Ngan Kee WD, Palanisamy A, Monks DT. Vasopressor drugs for the prevention and treatment of hypotension during neuraxial anaesthesia for caesarean delivery: a Bayesian network meta-analysis of fetal and maternal outcomes. Br J Anaesth. (2020) 124:e95–107. doi: 10.1016/j.bja.2019.09.045
19. Garrido MM. Covariate adjustment and propensity score. JAMA. (2016) 315:1521–2. doi: 10.1001/jama.2015.19081
20. Klimek M, Rossaint R, van de Velde M, Heesen M. Combined spinal-epidural vs. spinal anaesthesia for caesarean section: meta-analysis and trial-sequential analysis. Anaesthesia. (2018) 73:875–88. doi: 10.1111/anae.14210
21. McDonnell NJ, Paech MJ, Muchatuta NA, Hillyard S, Nathan EA. A randomised double-blind trial of phenylephrine and metaraminol infusions for prevention of hypotension during spinal and combined spinal-epidural anaesthesia for elective caesarean section. Anaesthesia. (2017) 72:609–17. doi: 10.1111/anae.13836
22. Wei C, Qian J, Zhang Y, Chang X, Hu H, Xiao F. Norepinephrine for the prevention of spinal-induced hypotension during caesarean delivery under combined spinal-epidural anaesthesia: randomised, double-blind, dose-finding study. Eur J Anaesthesiol. (2020) 37:309–15. doi: 10.1097/EJA.0000000000001152
23. Hartmann B, Junger A, Klasen J, Benson M, Jost A, Banzhaf A, et al. The incidence and risk factors for hypotension after spinal anesthesia induction: an analysis with automated data collection. Anesth Analg. (2002) 94:1521–9. doi: 10.1097/00000539-200206000-00027
24. Klasen J, Junger A, Hartmann B, Benson M, Jost A, Banzhaf A, et al. Differing incidences of relevant hypotension with combined spinal-epidural anesthesia and spinal anesthesia. Anesth Analg. (2003) 96:1491–5. doi: 10.1213/01.ane.0000057601.90930.18
25. Patorno E, Glynn RJ, Hernández-Díaz S, Liu J, Schneeweiss S. Studies with many covariates and few outcomes: selecting covariates and implementing propensity-score-based confounding adjustments. Epidemiology. (2014) 25:268–78. doi: 10.1097/EDE.0000000000000069
26. Reschke MM, Monks DT, Varaday SS, Ginosar Y, Palanisamy A, Singh PM. Choice of local anaesthetic for epidural caesarean section: a Bayesian network meta-analysis. Anaesthesia. (2020) 75:674–82. doi: 10.1111/anae.14966
27. Nani FS, Torres MLA. Correlation between the body mass index (BMI) of pregnant women and the development of hypotension after spinal anesthesia for cesarean section. Rev Bras Anestesiol. (2011) 61:21–30. doi: 10.1016/S0034-7094(11)70003-4
28. Tsai S-E, Yeh PH, Hsu PK, Tsao SL, Chang Y-J, Hsieh YJ. Continuous haemodynamic effects of left tilting and supine positions during caesarean section under spinal anaesthesia with a noninvasive cardiac output monitor system. Eur J Anaesthesiol. (2019) 36:72–5. doi: 10.1097/EJA.0000000000000895
29. Pereira IDF, Grando MM, Vianna PTG, Braz JRC, Castiglia YMM, Vane LA, et al. Retrospective analysis of risk factors and predictors of intraoperative complications in neuraxial blocks at Faculdade de Medicina de Botucatu-UNESP. Rev Bras Anestesiol. (2011) 61:568–81:311–8. doi: 10.1016/S0034-7094(11)70068-X
30. Chooi C, Cox JJ, Lumb RS, Middleton P, Chemali M, Emmett RS, et al. Techniques for preventing hypotension during spinal anaesthesia for caesarean section. Cochrane Database Syst Rev. (2020) 7:CD002251. doi: 10.1002/14651858.CD002251.pub4
31. Porzionato A, Emmi A, Barbon S, Boscolo-Berto R, Stecco C, Stocco E, et al. Sympathetic activation: a potential link between comorbidities and COVID-19. FEBS J. (2020) 287:3681–8. doi: 10.1111/febs.15481
32. Sun X, Liu Y, Mei W. Safety considerations for neuraxial anaesthesia in parturients with COVID-19. Br J Anaesth. (2020) 125:e313–4. doi: 10.1016/j.bja.2020.05.005
Keywords: neuraxial anesthesia, hypotension, COVID-19, cesarean delivery, propensity score matching
Citation: Zhang Y, Chen R, Cao C, Gong Y, Zhou Q, Wei M, Xia Z, Chen X and Meng Q (2021) The Risk of Neuraxial Anesthesia-Related Hypotension in COVID-19 Parturients Undergoing Cesarean Delivery: A Multicenter, Retrospective, Propensity Score Matched Cohort Study. Front. Med. 8:713733. doi: 10.3389/fmed.2021.713733
Received: 24 May 2021; Accepted: 19 July 2021;
Published: 19 August 2021.
Edited by:
Luigi Vetrugno, University of Udine, ItalyReviewed by:
Cristian Deana, Azienda Sanitaria Universitaria Integrata di Udine, ItalyCopyright © 2021 Zhang, Chen, Cao, Gong, Zhou, Wei, Xia, Chen and Meng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: QingTao Meng, bWVuZ3Fpbmd0YW8yMDE4QDEyNi5jb20=
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.