
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 16 November 2021
Sec. Geriatric Medicine
Volume 8 - 2021 | https://doi.org/10.3389/fmed.2021.713535
 Dung-Huan Liu1,2,3†
Dung-Huan Liu1,2,3† Chung-Yuan Hsu4†
Chung-Yuan Hsu4† Pei-Ching Wu2,5
Pei-Ching Wu2,5 Ying-Chou Chen4
Ying-Chou Chen4 You-Yin Chen6,7
You-Yin Chen6,7 Jia-Feng Chen4
Jia-Feng Chen4 Shan-Fu Yu4
Shan-Fu Yu4 Tien-Tsai Cheng4*
Tien-Tsai Cheng4*Background: Although the self-assessment tools for predicting osteoporosis are convenient for clinicians, they are not commonly used among men. We developed the Male Osteoporosis Self-Assessment Tool for Taiwan (MOSTAi) to identify the patients at risk of osteoporosis.
Methods: All the participants completed a questionnaire on the clinical risk factors for the fracture risk assessment tool. The risk index was calculated by the multivariate regression model through the item reduction method. The receiver operating characteristic (ROC) curve was used to analyze its sensitivity and specificity, and MOSTAi was developed and validated.
Results: A total of 2,290 men participated in the bone mineral density (BMD) survey. We chose a model that considered two variables (age and weight). The area under the curve (AUC) of the model was 0.700. The formula for the MOSTAi index is as follows: 0.3 × (weight in kilograms) – 0.1 × (years). We chose 11 as the appropriate cut-off value for the MOSTAi index to identify the subjects at the risk of osteoporosis.
Conclusions: The MOSTAi is a simple, intuitive, and country-specific tool that can predict the risk of osteoporosis in Taiwanese men. Due to different demographic characteristics, each region of the world can develop its own model to identify patients with osteoporosis more effectively.
Due to the aging population, osteoporosis in men is becoming a global health problem.
Aging men lose ~1% of their bone mineral density (BMD) each year while 20% of men over the age of 50 will develop osteoporosis-related fractures in their lifetime (1). In Taiwan, awareness and policy interventions have stabilized the epidemic trend of osteoporosis (2). The proportion of the population over 50 years of age is expected to increase from 32% (7.5 million) in 2013 to 57% (11.9 million) in 2050. The life expectancy of men will increase from 80 years in 2013 to 83 years in 2050 (3). The Taiwanese men have a higher annual hip fracture rate (4). Additionally, 20.67% of these men died within 1 year of injury (5). This percentage was much higher than the percentage of women diagnosed with hip fractures. Therefore, identifying these men is essential to prevent osteoporosis-related fractures.
According to the WHO classification criteria, dual-energy X-ray absorptiometry (DXA) is the gold standard diagnostic test for osteoporosis (T-score, −2.5). Due to the limited supply of DXA machines and restrictions on the reimbursement of medical expenses in some of the rural areas, the people living in these areas are not able to receive the routine DXA and BMD scans. To improve the relevance and effectiveness of these scans, several tools have been developed, such as Osteoporosis Self-Assessment Tool for Asians (OSTA) and the National Osteoporosis Foundation recommendations in 2013 (NOF 2013) (6, 7). Since 1993, several studies have associated osteoporosis with aging and low body weight (8, 9). In 2001, Koh et al. proposed OSTA as a convenient method to identify this risk due to weight and age (7). NOF 2013 determines the high-risk patients belonging to different age groups based on the number of clinical risk factors. In addition, this tool is used to identify the individuals who should be DXA tested. Currently, OSTA is validated in men of various races but is not directly evaluated in Taiwanese men yet. Additionally, the efficacy of OSTA is not directly compared with NOF 2013. Therefore, this study developed a risk index called Male Osteoporosis Self-Assessment Tool for Taiwan (MOSTAi) and validated it by using a separate cohort and comparing it with NOF 2013.
Between 2008 and 2011, the Taiwan Osteoporosis Association implemented a tour program for the entire island to evaluate BMD. This plan included a trained nurse, a DXA machine (Explorer; Hologic Inc., Waltham, MA, USA), a bus from the International Society for Clinical Densitometry, and a radiographer. The buses can be used in various locations on request and the DXA machines are used for measuring BMD. There is a total of 104 stations in Taiwan.
In order to be included as a part of this study, the patients had to meet the following inclusion criteria: men who had informed consent and were aged 50 years and older. The patients were excluded from the study if their hips were previously fractured or replaced. All the included men were randomly assigned a 1:1 development or validation cohort to form the MOSTAi index. The local Institutional Review Board of Chang Gung Memorial Hospital (102-1878B), Taoyuan City, Taiwan, approved the study. All the participants provided written informed consent for this study.
A trained nurse interviewed each participant and a questionnaire was filled out to be accessed by fracture risk assessment tool (FRAX). The clinical risk factors such as weight, height, use of glucocorticoids, previous fractures, rheumatoid arthritis (RA), secondary osteoporosis, gender, age, parental hip fracture, smoking, and drinking were assessed. The BMD measurements were performed in both the hips and the lumbar spine of all the patients using a DXA machine inside the bus. The least significant changes (LSCs) in each area were 3.93% (total hip), 4.19% (femoral neck), and 3.17% (lumbar spine) (10). The BMD value is based on the reference value of Asian young women aged 20–29 years (11).
The participants are divided into the non-osteoporosis or osteoporosis risk groups that require BMD testing based on whether they meet one of the following criteria in the NOF 2013 recommendation. The criteria include women of 65 years of age and older, or postmenopausal women younger than 65, who have one or more clinical risk factors for fractures, such as low weight, previous fractures, use of low bone mass, or high-risk medication use related to low bone mass, or a disease or condition related to bone loss. The criteria also evaluated the diagnostic performance of NOF 2013 in predicting osteoporosis in the population we studied.
The t and the chi-square tests analyzed the continuous and categorical variables, respectively. FRAX assessed the possible risk factors for the model development. A univariate analysis was included in the multiple variable logistic regression models after identifying the statistically significant risk factors (p < 0.05). The next step was to constitute the MOSTAi index through the multiple variable logistic regression analyses and item reduction methods that were based on the major risk factors.
The WHO criteria define osteoporosis with a T-score of ≤ −2.5 at any site (lumbar spine, femoral neck, or total hip) (12). A receiver operating characteristic (ROC) curve analysis was performed to assess the ability of MOSTAi to distinguish between the subjects diagnosed with and without osteoporosis. The sensitivity was defined as the proportion of men diagnosed with osteoporosis (T-scores ≤ −2.5) who had 1 tested positive (i.e., index values below the cut-off), and the specificity was defined as the proportion of men diagnosed without osteoporosis who tested normal (i.e., having index values above or equal to the cutoff). The area under the curve (AUC) compared the performance of MOSTAi with OSTA and NOF 2013. In order to test the statistical difference between the AUCs, Delong's test was performed; for the sensitivity and specificity, Mcnemar's test was performed. All the analyses were performed using the SPSS statistics. A P-value of <0.05 indicated a statistically significant difference.
The Taiwan OsteoPorosis Survey (TOPS) recruited a total of 18,992 participants, including 4,323 men (22.8%) and 14,669 women (77.2%). The analyses excluded the patients having inaccessible BMD data, incomplete or missing questionnaire data based on FRAX, and age group < 50. The distribution of these participants is shown in Figure 1. A total of 2,290 men were evaluated and randomly assigned a development (n = 1,145) or validation (n = 1,145) cohort.
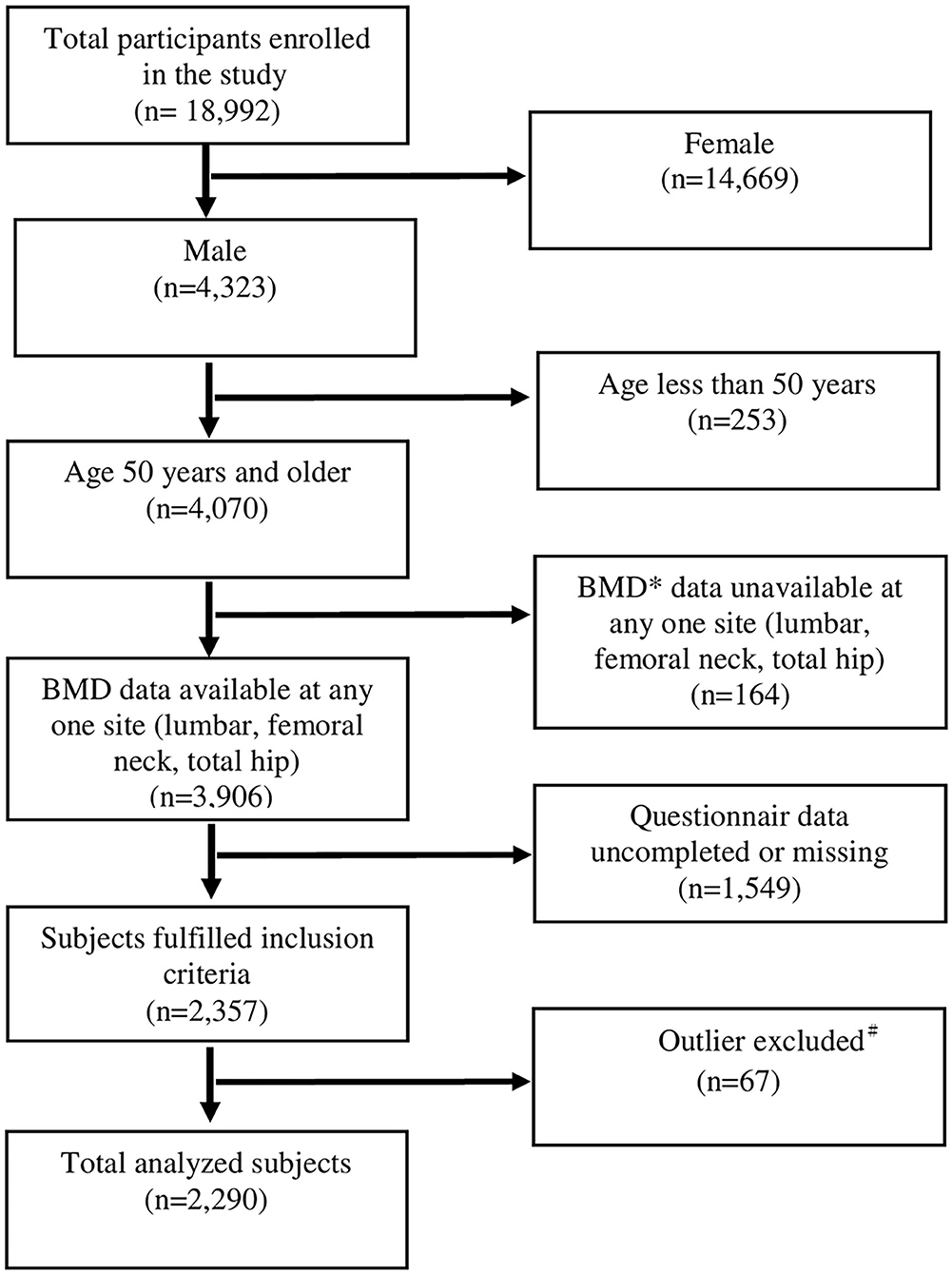
Figure 1. Inclusion of the participants in the study. *Participants whose BMD was missing at any one site for any reasons were excluded. #Participants with extreme values (deviating from the mean by more than three times the standard deviation), including demographics and BMD were excluded for data analysis.
Table 1 shows the characteristics of the development and validation cohorts. The average age is 69.6 ± 9.6 years. The average body weight and average body mass index (BMI) were 65.9 ± 9.8 kg and 24.1 ± 3.2 kg/m2, respectively. For all the characteristics and clinical risk factors, there were no significant differences between the development and validation cohorts (p > 0.05).
Univariate analysis showed that the four factors, namely, age, weight, previous fracture history, and height, were the main risk factors for osteoporosis. The index weights of these factors were determined by the multivariate regression and were finally used to score the MOSTAi for each subject. Table 2 shows the regression coefficients for the multivariate and univariate analyses in the development cohort. Finally, through multivariate analysis, only weight, age, and the previous fractures were significant factors in the developmental cohort.
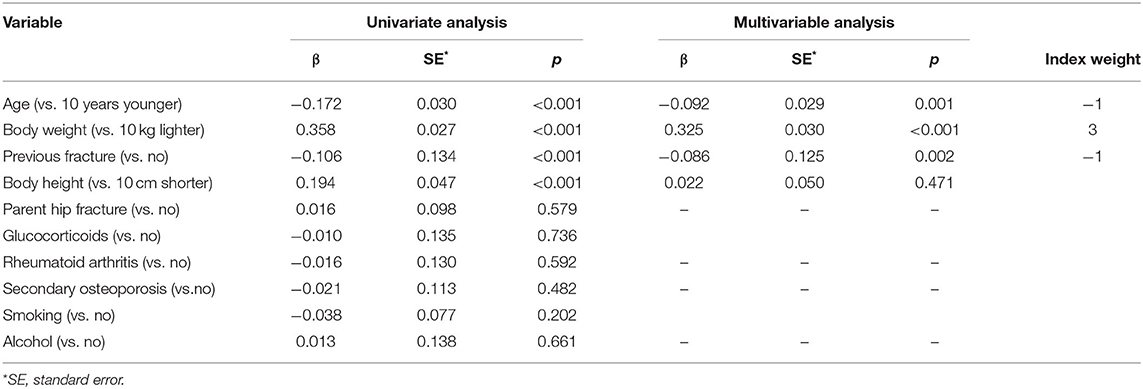
Table 2. Regression coefficients for the univariate and multivariable analysis in the developmental cohort.
The ROC curve for the developmental 1 cohort is shown in Figure 2 (left). The last variables were age, weight, and the previous fractures. A ROC curve analysis was performed to assess the ability of a model to distinguish between the subjects diagnosed with and without osteoporosis. The AUC for weight, weight + age, and weight + age + previous fractures were 0.690 (p < 0.001, 95% CI, 0.646–0.734), 0.700 (p < 0.001, 95% CI 0.656–0.742), and 0.701 (p < 0.001, 95% CI, 0.658–0.744), respectively. The AUC (of the diagnostic tool) <0.7 is considered unacceptable (13). Therefore, the models based solely on the weights were excluded. Besides, the model based only on age and weight behaves almost the same as the model using the three variables. Therefore, for simplicity, we only select age and weight to design the final model. According to the beta coefficient in Table 2, the index weight can be calculated. We converted the regression coefficients of age and weight into units of 10 years and 10 kg, respectively, to simplify the subsequent calculations. Therefore, MOSTAi value could be determined by adding +3 units per 10 kg increase in weight and −1 unit per 10 years increase in age with a reference age of 50 years and weight of 50 kg. The formula for the MOSTAi index is as follows: 0.3 × (weight in kilograms) - 0.1 × (age in years). The MOSTAi index of 1,145 participants in the development cohort was calculated. The average, median, SD, and range of the MOSTAi index were 12.8, 13, 3.4, and 4–23, respectively.
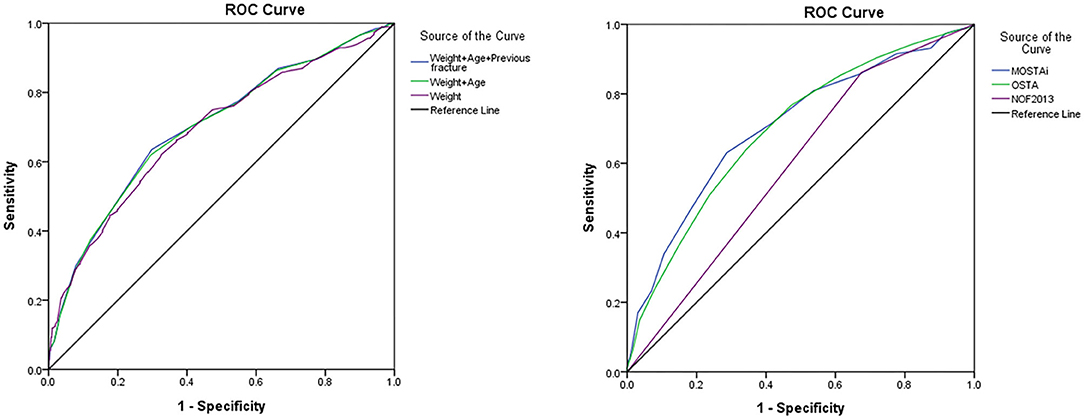
Figure 2. The receiver operating characteristic (ROC) curve of the developmental cohort (left side). The ROC curves for predicting osteoporosis by MOSTAi, OSTA, and NOF 2013 (right side). OSTA, osteoporosis self-assessment tool; NOF 2013, National osteoporosis foundation recommendations in 2013; MOSTAi, modified male osteoporosis self-assessment tool for Taiwan.
After estimating the ROC curve, the number 11 was selected as the appropriate cut-off value of the MOSTAi index to identify the high-risk subjects diagnosed with osteoporosis in the developmental cohort, with the highest sensitivity (61.96%) and the highest specificity (70.45%). Besides, the positive predictive value (PPV) and negative predictive value (NPV) of MOSTAi in the developmental samples (n = 1,145) were 28.64 and 90.63%, respectively. Table 3 shows the comparison between the MOSTAi index, OSTA index, and NOF 2013 in the validation cohort.
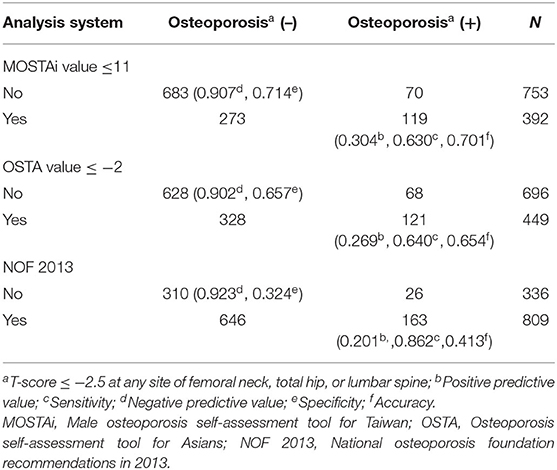
Table 3. The comparison between modified male osteoporosis self-assessment tool for Taiwan (MOSTAi) index, osteoporosis self-assessment tool (OSTA) index, and National osteoporosis foundation recommendations in 2013 (NOF 2013) in the validation cohort.
Using the optimal cutoff value (−2) for 1 OSTA, sensitivity, specificity, PPV, and NPV in the validation cohort were 64.0, 65.7, 26.9, and 90.2%, respectively. Figure 2 (right) shows the ROC curves of NOF 2013, MOSTAi, and OSTA for predicting osteoporosis. The different AUCs of MOSTAi, OSTA, and NOF 2013 were 0.706 (p < 0.001, 95% CI: 0.664–0.748), 0.697 (p < 0.001, 95% CI: 0.657–0.738), and 0.593 (p < 0.001, 95% CI: 0.552–0.634). We conducted a Delong's test between these models. The p-value between MOSTAi and OSTA is 0.82, which is not statistically significant. The p-value between MOSTAi and NOF 2013 is 0.004, which is statistically significant. In addition, we performed Mcnemar's test for sensitivity and specificity analysis. The P-value between MOSTAi and OSTA is <0.0001. In addition, the P-value between MOSTAi and NOF 2013 is also <0.0001. Both have reached statistical significance, showing that the sensitivity and specificity of MOSTAi are better.
Based on the osteoporosis risk categories used in the Koh study (7), we arbitrarily created three osteoporosis risk categories based on the index. The lowest T-scores at any site and the MOSTAi values for the development sample are showed in Figure 3. The high-risk, medium-risk, and low-risk groups included those with MOSTAi index values ≤5, between 5 and 11 (≤11 and >5), and >11.
In the developmental cohort, 65.2, 33.5, and 1.2% of the patients were classified as the low-risk, intermediate-risk, and high-risk groups, respectively. The prevalence of osteoporosis in these groups was 9.4% (70/747), 26.8% (103/384), and 78.6% (11/14). Similarly, in the validation cohort, the patients belonging to the low-risk, medium-risk, and high-risk categories accounted for 65.8, 33.1, and 1.1%, respectively. The prevalence of osteoporosis in these groups was 9.3% (70/753), 29.6% (112/379), and 53.8% (7/13).
Osteoporosis Self-Assessment Tool for Asians was originally developed for the Asian population and later validated in the Caucasian population (14). It has effectively identified postmenopausal women having a risk for osteoporosis. The differences in the accuracy of OSTA are reported in identifying osteoporosis in men as compared 1 with women (15, 16). Lynn et al. observed that the OST index was useful in the population of Caucasian American men when the threshold was ≤ 2 and Hong Kong Chinese men when the threshold was ≤-1 (16). Therefore, the optimal cut-off value for OSTA for predicting osteoporosis in men may vary among the different races. In addition, the different performances of OSTA may be related to how BMD is measured between the surveys (17).
In this study, 373 participants were diagnosed with osteoporosis based on the T-score of the femoral neck, lumbar spine, or total hip. Actually, BMD of the femoral neck was used as a measure to define osteoporosis (18). However, the number of patients would have been underestimated if the T-score would be measured only on the lumbar spine (n = 127), or the femoral neck (n = 117), or the total hip (n = 7). In addition, it was known that osteoporosis diagnosed at any site could predict the risk of future fracture at other sites (19). According to the previous study, we developed MOSTAi to identify the T-score ≤ −2.5 at any site other than just on the femoral neck (20). It does not matter that the tool may be overestimated because the patient still needs DXA to confirm whether he has osteoporosis.
In a previous study of the author, some modifications were made to the original OSTA model by including risk factors from FRAX (21). This led to the development of the Osteoporosis Self-Assessment Tool for Taiwan postmenopausal women (OSTAi). It is a friendly tool for postmenopausal women to self-assess osteoporosis and is commonly used in Taiwan. However, for men, there are currently no self-assessment tools in Taiwan. In this study, the algorithm used to calculate MOSTAi was similar to the original OSTA except that different index weights were considered. In the OSTAi model, the weighted indices of age and weight were −0.2 and +0.2, respectively, and the cut-off value –f −1. In the MOSTAi model, the weighted 1 indices of age and weight were −0.1 and +0.3, respectively. In the MOSTAi formula, the importance of body weight is greater than age, which is different from OSTAi. The reason why lower body weight played a greater role in the development of osteoporosis in the elderly male Taiwanese population is still unclear.
In the validated sample of 1,145 Taiwanese men, the performance of MOSTAi was further compared with OSTA and NOF 2013 (Table 3). The optimal cut-off value of −2 for OSTA resulted in a sensitivity and specificity of 64.0 and 65.7%, respectively, with an AUC of 0.697. An AUC value (of OSTA) <0.7 was considered to be insufficient. MOSTAi showed acceptable sensitivity/specificity (63.0/71.4%) and a high NPV (90.7%). In addition, an AUC (0.706) of MOSTAi in the Taiwanese men was higher than that of OSTA. Therefore, compared with OSTA, the MOSTAi may be a more suitable tool for identifying the Taiwanese men at risk for osteoporosis. Compared with NOF 2013, the accuracy of MOSTAi (70.1%) and AUC (0.706) was improved (41.3% and 0.593, respectively). Although the PPV (30.4) of MOSTAi is not high, it has improved a lot compared with the OSTA (26.9) and NOF 2013 (20.1). Therefore, considering the specificity, sensitivity, and AUC, a MOSTAi is an effective tool for searching men with osteoporosis. It may be due to the formula we designed using local data, so other countries can use the study as a template to set up their own tools to provide better medical services for their population.
The Taiwan OsteoPorosis Survey is the first national survey of osteoporosis in Taiwan that can be used to launch more reliable diagnostic tools. The measurements performed by the same DXA machine and the same technician reduced the inter-modality and inter-operator variations. Although the clinical risk factors in FRAX have been included in MOSTAi, they have not been used to develop OSTA in men. In the near future, different variables can be analyzed for further prospective study design 1 to enhance the predictive power of this tool (22).
In recent years, with the aging of society, male osteoporosis has become an important problem. “The Osteoporotic Fractures in Men (MrOS) Study” focused on osteoporosis and fractures in men aged 65 years and over and published prospective data for more than 16 years (23). It tells us that in the first BMD test, elderly men with a BMD T score> −1.50 are highly unlikely to develop osteoporosis during the follow-up period and do not need to undergo another BMD test. The difference between the MOSTAi and MrOS is that MOSTAi provides a simple self-assessment tool that can decide whether to conduct a BMD survey on men without having to conduct a BMD first.
This study has some limitations. First, the population was not randomly selected and the proportion of osteoporosis would have been higher than the general population (24). Some subjects do not participate in the study themselves, but the clinicians may refer certain high-risk patients for osteoporosis assessment, leading to selection bias. However, the prevalence of osteoporosis in Taiwanese men aged 50 years or older (16.3%) was similar to the elderly (17.2%) population (25). Second, although the lower body weight and aging can predict the risk of fractures in the future; further research is needed to check whether MOSTAi can predict this risk in Taiwanese men. On the other hand, although FRAX is most commonly used for predicting osteoporotic fractures, it is still not able to predict patients with the WHO defined osteoporosis. Therefore, we cannot compare MOSTAi with FRAX. Third, although secondary osteoporosis is a clinical risk factor for FRAX, our information about it comes from an item called “secondary osteoporosis” in the questionnaire. So, we do not know the proportion of individuals with these diseases. It is impossible to know their impact on this research.
A MOSTAi has been proven a simple tool with reasonable 1 sensitivity/specificity, PPV, and a high NPV. Compared with OSTA and NOF 2013, a MOSTAi may be more suitable for identifying the Taiwanese men who are at risk for osteoporosis and further recommending the risk groups for the DXA test.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
This study had been approved by Institutional Review Board of Chang Gung Memorial Hospital (102-1878B). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
D-HL, C-YH, and T-TC contributed to the conception and design of the study. P-CW, Y-CC, Y-YC, J-FC, and S-FY organized the database and performed the statistical analysis. T-TC wrote the first draft of the manuscript. D-HL, C-YH, and T-TC wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
This work was supported by a grant (CMRPG8K0441) from Chang Gung Memorial Hospital.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to thank the Taiwan osteoporosis association for authorizing access to the database, and Merck Sharp & Dohme pharmaceutical company (Taiwan) for providing the mobile DXA machine during the recruitment period. The authors would also like to thank Professor Chan SJ for their help with the statistical analysis.
1. Hannan MT, Felson DT, Dawson-Hughes B, Tucker KL, Cupples LA, Wilson PW, et al. Risk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res. (2000) 15:710–20. doi: 10.1359/jbmr.2000.15.4.710
2. Chen FP, Huang TS, Fu TS, Sun CC, Chao AS, Tsai TL. Secular trends in incidence of osteoporosis in Taiwan: a nationwide population-based study. Biomed J. (2018) 41:314–20. doi: 10.1016/j.bj.2018.08.001
3. Mithal A, Bansal B, Kyer CS, Ebeling P. The Asia-pacific regional audit-epidemiology, costs, and burden of osteoporosis in India 2013: a report of International Osteoporosis Foundation. Indian J Endocrinol Metab. (2014) 18:449–54. doi: 10.4103/2230-8210.137485
4. Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA, Cooper C, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. (2012) 23:2239–56. doi: 10.1007/s00198-012-1964-3
5. Wang C-B, Lin C-FJ, Liang W-M, Cheng C-F, Chang Y-J, Wu H-C, et al. Excess mortality after hip fracture among the elderly in Taiwan: a nationwide population-based cohort study. Bone. (2013) 56:147–53. doi: 10.1016/j.bone.2013.05.015
6. Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. (2014) 25:2359–81. doi: 10.1007/s00198-014-2794-2
7. Koh LK, Sedrine WB, Torralba TP, Kung A, Fujiwara S, Chan SP, et al. A simple tool to identify Asian women at increased risk of osteoporosis. Osteoporos Int. (2001) 12:699–705. doi: 10.1007/s001980170070
8. Margolis KL, Ensrud KE, Schreiner PJ, Tabor HK. Body size and risk for clinical fractures in older women. Study of Osteoporotic Fractures Research Group. Ann Internal Med. (2000) 133:123–7. doi: 10.7326/0003-4819-133-2-200007180-00011
9. Dargent-Molina P, Poitiers F, Breart G. In elderly women weight is the best predictor of a very low bone mineral density: evidence from the EPIDOS study. Osteoporos Int. (2000) 11:881–8. doi: 10.1007/s001980070048
10. Nazarian A, Chang Y-F, Chang C-S, Wang M-W, Wu C-F, Chen C-Y, et al. Effects of age and body mass index on thoracolumbar spine X-ray for diagnosing osteoporosis in elderly women: Tianliao Old People (TOP) Study 07. PLoS ONE. (2016) 11:e0161773. doi: 10.1371/journal.pone.0161773
11. Hwang JS, Chan DC, Chen JF, Cheng TT, Wu CH, Soong YK, et al. Clinical practice guidelines for the prevention and treatment of osteoporosis in Taiwan: summary. J Bone Mineral Metabol. (2014) 32:10–6. doi: 10.1007/s00774-013-0495-0
12. Kanis JA. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int. (1994) 4:368–81. doi: 10.1007/BF01622200
13. Zhu W, Zeng N, Wang N. Sensitivity, specificity, accuracy, associated confidence interval and ROC analysis with practical SAS implementations. NESUG Proc. (2010) 19:67.
14. Richy F, Gourlay M, Ross PD, Sen SS, Radican L, De Ceulaer F, et al. Validation and comparative evaluation of the osteoporosis self-assessment tool (OST) in a Caucasian population from Belgium. QJM Monthly J Assoc Phys. (2004) 97:39–46. doi: 10.1093/qjmed/hch002
15. Steuart Richards J, Lazzari AA, Teves Qualler DA, Desale S, Howard R, Kerr GS. Validation of the osteoporosis self-assessment tool in US male veterans. J Clin Densitometry. (2014) 17:32–7. doi: 10.1016/j.jocd.2013.02.004
16. Lynn HS, Woo J, Leung PC, Barrett-Connor EL, Nevitt MC, Cauley JA, et al. An evaluation of osteoporosis screening tools for the osteoporotic fractures in men (MrOS) study. Osteoporos Int. (2008) 19:1087–92. doi: 10.1007/s00198-007-0553-3
17. Machado P, Coutinho M, da Silva JA. Selecting men for bone densitometry: performance of osteoporosis risk assessment tools in Portuguese men. Osteoporos Int. (2010) 21:977–83. doi: 10.1007/s00198-009-1036-5
18. Kanis JA, Adachi JD, Cooper C, Clark P, Cummings SR, Diaz-Curiel M, et al. Standardising the descriptive epidemiology of osteoporosis: recommendations from the Epidemiology and Quality of Life Working Group of IOF. Osteoporos Int. (2013) 24:2763–4. doi: 10.1007/s00198-013-2413-7
19. Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. (2000) 15:721–39. doi: 10.1359/jbmr.2000.15.4.721
20. Yang Y, Wang B, Fei Q, Meng Q, Li D, Tang H, et al. Validation of an osteoporosis self-assessment tool to identify primary osteoporosis and new osteoporotic vertebral fractures in postmenopausal Chinese women in Beijing. BMC Musculoskeletal Disord. (2013) 14:271. doi: 10.1186/1471-2474-14-271
21. Su FM, Liu DH, Chen JF, Yu SF, Chiu WC, Hsu CY, et al. Development and Validation of an Osteoporosis Self-Assessment Tool for Taiwan (OSTAi) Postmenopausal Women-A Sub-Study of the Taiwan OsteoPorosis Survey (TOPS). PLoS ONE. (2015) 10:e0130716. doi: 10.1371/journal.pone.0130716
22. Wang P, Abdin E, Shafie S, Chong SA, Vaingankar JA, Subramaniam M. Estimation of prevalence of osteoporosis using OSTA and its correlation with sociodemographic factors, disability and comorbidities. Int J Environ Res Public Health. (2019) 16:2338. doi: 10.3390/ijerph16132338
23. Gourlay ML, Overman RA, Fine JP, Filteau G, Cawthon PM, Schousboe JT, et al. Time to osteoporosis and major fracture in older men: the MrOS Study. Am J Prev Med. (2016) 50:727–36. doi: 10.1016/j.amepre.2015.11.015
Keywords: osteoporosis, self-assessment tool, men, Taiwan, fracture
Citation: Liu D-H, Hsu C-Y, Wu P-C, Chen Y-C, Chen Y-Y, Chen J-F, Yu S-F and Cheng T-T (2021) Simple Self-Assessment Tool to Predict Osteoporosis in Taiwanese Men. Front. Med. 8:713535. doi: 10.3389/fmed.2021.713535
Received: 23 May 2021; Accepted: 11 October 2021;
Published: 16 November 2021.
Edited by:
Kok Yong Chin, National University of Malaysia, MalaysiaReviewed by:
Thao Phuong Ho-Le, University of Technology Sydney, AustraliaCopyright © 2021 Liu, Hsu, Wu, Chen, Chen, Chen, Yu and Cheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tien-Tsai Cheng, dGlhbnRzYWlAbXMyLmhpbmV0Lm5ldA==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.