
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Med. , 26 November 2021
Sec. Family Medicine and Primary Care
Volume 8 - 2021 | https://doi.org/10.3389/fmed.2021.681612
This article is part of the Research Topic Core Values and Tasks of Primary Care in Changing Communities and Health Care Systems View all 9 articles
Summary: Late in 2020, the Nordic Colleges of General Practice published a joint statement specifying what General Practitioners stand for and intend to act upon, our Core Values and Principles. In this article, the authors describe and analyze challenges and milestones encountered on our 50-year journey toward the creation of that document.
The shaping of Family Medicine/General Practice as an academic discipline began in the 1960's. During an initial, descriptive phase, the new specialty was defined, its educational curricula formulated, and the core competencies required to earn the title, Specialist in Family Medicine, were identified. Focus was not yet placed directly on the relationship between viable working principles and values, however.
Then, the 1978 WHO Alma Ata Declaration affirmed health to be a fundamental human right, with primary health care as the heart of sustainable health care systems, indirectly mandating that the field of Family Medicine deliver value-based health care. A major step in that process was taken in 2001: The Norwegian College of General Practice launched their statement identifying the seven theses, Sju teser, that characterize the principles, purposes—and core values—of General Practice. Later, the Nordic colleges worked together to formulate the 2020 joint statement.
We are confident that Family Medicine will continue to provide sustainable, relationship-based care, and to protect the human side of medicine. Sharing core values and principles can help us mobilize as effective advocates for our discipline and for our patients, the citizens whom we serve.
Late in 2020, the Nordic Colleges of General Practice/Family Medicine, referred to here as “Family Medicine,” published their Core Values and Principles (1, 2). These are explicit statements of what we as General Practitioners (GPs) stand for and intend to act upon—the professional values as postulated by our colleges, and the individual, personal values and principles that are embedded within them. The outline of these statements is shown in Table 1 (see Supplementary Text for the full version, including values definitions).
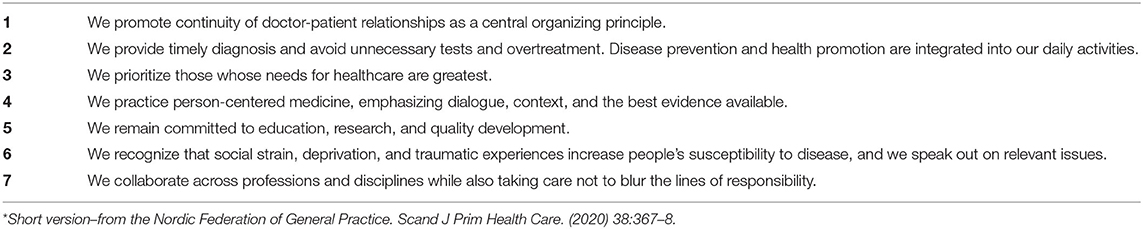
Table 1. Core Values and Principles of Nordic General Practice/Family Medicine*.
The focus of the pioneers developing Family Medicine in the mid-20th century was not primarily on the concept of values. Their extensive scholarly works explored: defining Family Medicine as a discipline; formulating educational curricula for these new generalists; debating which core competencies must be mastered to earn the title of “Specialist” in this new discipline; and envisioning the Family Medicine of the future. This was the crucial descriptive phase in the history of Family Medicine (further described in Supplementary Text).
During the 1990's, Family Medicine leaders from various countries began to examine ethical issues, questioning their aims, what to consider acceptable, what to deem worth fighting for, or against. Meantime, the profession had to adapt to changes within society and medicine, such as technological innovations and increasing commercialization. The fragmentation of care had also increased, leaving fewer stable communities, with more GPs working part-time while treating more patients, the emergence of “walk-in” centers and “screen doctoring” (3).
Inevitably, such developments challenged, perhaps even threatened, our profession, exposing an urgent need not merely to update it but to re-envision its very foundations. The European region's World Organization of Family Doctors, WONCA Europe, formulated a definition of Family Medicine (4) highlighting its essential concepts, its core professional competencies, and approaches to learning. This definition does not explicitly emphasize the relationship between viable working principles and values. Furthermore, while the terms vision, mission, and values were implicit within the earlier frameworks, they were not explored directly (2). Meantime, many terms that were assumed to be shared prove instead to have widely diverging definitions within the different languages, each carrying distinctive cultural implications and evoking unique—unshared—associations.
Ian McWhinney, considered the founding father of academic Family Medicine, described the principles of Family Medicine as early as 1981 as, “a distinctive worldview—a system of values and an approach to problems—that is identifiably different from that of other disciplines” (5). In 2002, Pendleton and King added, “If we are to release the potential motivating power of the vision and values in action, it may be time to articulate the values of our professions more explicitly” (6).
Words matter. Clearly, if the profession is to unify worldwide, GPs will need to agree on a vision and a set of values—based on a shared understanding of a common vocabulary. Carefully chosen words, slogans, and concepts have power when advocating for ideas and ideologies.
Thus, the aim of this paper is to chronicle the path that our community of GPs has taken during recent decades to investigate and shape our discipline, its fundamental mindset in general and its Nordic character in particular—with a special focus on values.
In the West, the rise of specialization combined with the increasing fragmentation of medical care that had begun by the 1950's to worsen the existing shortage of available GPs. In 1978, the declaration from the Alma Ata meeting emerged as a major milestone (7). At that meeting, international leaders declared that health is a fundamental human right with primary care being the key to the attainment of the goal of “Health for All”. The World Health Organization (WHO) soon adopted that view. This strengthened the GP's motivation to unite. Colleges of Family Medicine were established in the Nordic countries and elsewhere (Figure 1).
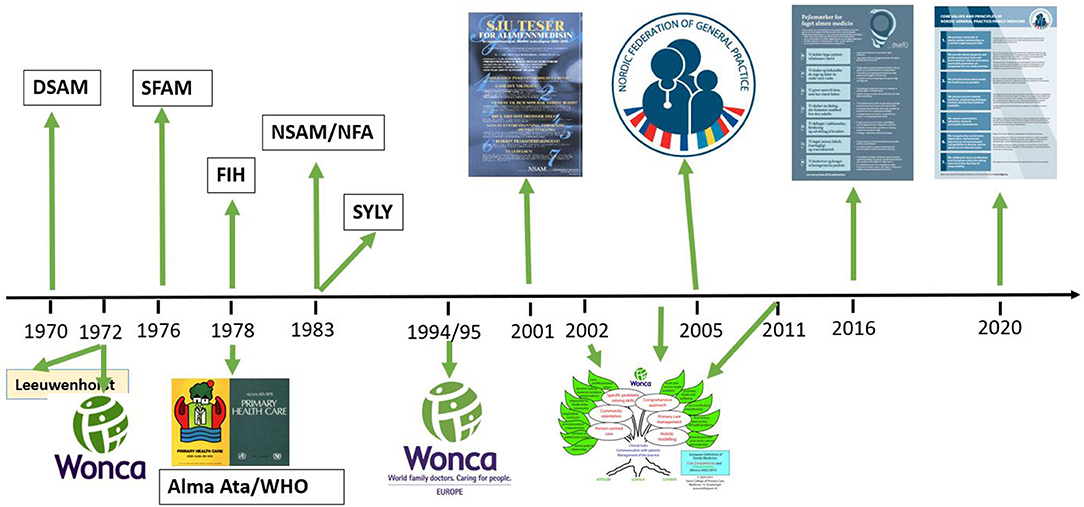
Figure 1. Milestones on our way toward the Nordic core values and principles of general practice (DSAM, Danish College of General Practice; Wonca, World Organization of Family Doctors; SFAM, Swedish College of General Practice; FIH, The Icelandic College of Family Physicians; NSAM/NFA, The Norwegian College of General Practice; SYLY, The Finnish Association of General Practice).
A new generation of pioneering doctors, mainly but not only in the United States and England, began emphasizing the need to teach Family Medicine in medical schools as a high-quality academic discipline. Modern Family Medicine, including the academic training of the “new generalists,” thus began to take shape (5). The Graduate Education of Physicians (8), known as the “Millis Report,” was among the first to specify curriculum requirements for this training, in a continuum extending through medical school, internship, and residency. It would take decades, however, to compress and clarify the vast contents and structure of the field of Family Medicine, as well as to develop appropriate vocational training programs (These historical processes are described in the Supplementary Text).
During the 1960's, cardiovascular epidemiological studies, such as the famous Framingham study, increased in number worldwide, and had a considerable impact on the development of Family Medicine and its values as described below. These studies documented high rates of cardiovascular diseases (CVD) associated with elevated blood pressure, high cholesterol, and smoking, which were then identified as disease risk factors (9, 10). Risk factors became equivalent to disease definitions. These important findings had a great impact on the curative as well as predictive-preventive medical interventions that were supported by governments and WHO.
Advanced statistics were also introduced during this period, with “Significant difference,” as illustrated in p-values, playing a major role. The best evidence, defined as p < 0.001, soon became a “golden goose,” marking the arrival of the Risk Factor Paradigm (9). CVD risk factor studies became quite popular during the late 20th century. Also during that period, a trend emerged to expand disease definitions, resulting in more and more people who had previously been considered healthy now being given a diagnosis, thus labeled as sick. When follow-up intervention studies failed to yield convincing results, larger studies were designed to ensure reaching the p < 0.001 level—that is, to demonstrate significant differences between those “at risk” vs. those “not at risk”. As the size of these studies increased, their results became less relevant to clinical settings. Nonetheless, healthy people continued to be promised even better health than they already enjoyed.
It also bears mentioning that most of the big intervention studies were designed and conducted to evaluate new types of drugs, and thus were initiated, and financed, by the pharmaceutical industry.
As the academic discipline and specialty of Family Medicine began taking shape in the 1960's, the interest in it grew. The new Icelandic Primary Health Care legislation of 1974 mandated the building of primary health care centers in every county, staffed by well-educated GPs, nurses, midwives, secretaries, and ancillary staff. Customarily, most Icelandic doctors completed their postgraduate education abroad. The advanced Family Medicine specialization programs in Canada had come farthest, offering training based on critical thinking, and practice conducting video-guided Family Medicine consultations (11). Our Icelandic pioneer, Olafur Mixa, GP, graduated from Calgary in 1971, becoming the first Nordic Specialist in Family Medicine to be educated according to the new curriculum of professional training; he was also an early advocate for these programs. A group of young, enthusiastic Icelandic doctors, fascinated by such ideas and opportunities, soon enrolled in the Canadian programs. Their teachers included Ian R. McWhinney (Western University) and David Sackett (McMaster). While not famous then, they would soon be recognized as the vanguard of examining, and thinking critically about, the ideology and principles of the medical establishment. The “bible” for our young doctors at that time was Ivan Illich's, Limits to Medicine (12), understood in retrospect as being filled with reflections on values. Furthermore, Sackett and his co-workers managed to popularize their course, Critical Appraisal of the Medical Literature, later entitled, Evidence Based Medicine.
The young Icelandic GPs returning to Iceland early in the 1980's after completing their specialty training in Canada, Sweden, and England, were full of fervor. They were (at least according to themselves) exceedingly well-versed not only in CVD epidemiology but also critical thinking and the ambitious ideology of Family Medicine—including its vision.
Fragmentation of care, however, had already re-shaped the Primary Care landscape in Iceland, with baby wellness care and school health care delegated to Pediatricians, maternity care placed within the domain of Gynecologists, etc. No wonder the new Family Medicine discipline, with all its principles and purposes, sparked both debate and conflict.
As did most Western countries, Iceland ran a comprehensive, national, epidemiological CVD study; they began in 1967, under the auspices of the Icelandic Heart Association. In addition to carrying out a study of CVD risk factors on carefully selected cohorts, the Heart Association offered all Icelandic citizens the opportunity to receive such “health checks” as funding came through the Social Security system, they could participate almost free of charge. These health checks were greatly appreciated and very popular (13). The notion that “More is Better” took hold, with ever more people being convinced that the strategy of “running all tests known to man—and as soon as possible” would improve their health.
Younger GPs began to object, however. They argued that such comprehensive “screenings” were unethical, did not meet generally accepted screening criteria, fell outside the framework of research, and, in addition, jeopardized the value of offering a holistic approach, as well as the new plans that Primary Health Care would serve as the entry point for medical contact. The debate culminated in 1983. The Ethical Committee of the Icelandic Medical Association concluded that it had been the critique put forth by the younger GPs that had not only been unethical but had also exemplified unacceptable collegial behavior (13)!
Thus, the debate that emerged between GPs and the heads of the Icelandic Heart Association became a battle about the values embedded in Evidence Based Medicine.
In the mid-1980's, Jostein Holmen, GP, then the upcoming leader of the epidemiological HUNT study and later Professor of Community Medicine, began to critique the clinical guidelines for treating high blood pressure, in particular the cut-off levels recommended by CVD cardiologists (14, 15). He and his co-workers argued that “reductionist” organ specialists needed only to focus on one disease or condition (later referred to as “linear thinking”), independent of other levels of “risk.” GPs, on the other hand, and their colleagues within community medicine, had to respond not merely to patient's needs but also to such concerns as public funding and the equitable distribution of services (15). This aspect of the development of Family Medicine would be elaborated later, relating it to non-linear, complex, adaptive systems theories (16).
The Risk Project was formally established in 1994 by the Norwegian College of General Practice (NSAM, later NFA), under the leadership of Elisabeth Swensen, GP, and with the support of the Norwegian Ministry of Health. The topic of values within Family Medicine vs. those of other disciplines was explored in, Diagnose: Risiko (Diagnosis: At Risk), edited by Swensen (17), using events of 1989 as a case-in-point. In that year, all Norwegian citizens aged 40–42 residing in various counties were invited to participate in a comprehensive population study of cardiovascular risk factors (18). Arranged by The Norwegian Center for Health Research (Statens helseundersøkelser, SHUS), the study was promoted through an intensive information campaign in the mass media and elsewhere, presenting the benefits of such preventive measures as, “An offer you can't refuse” (17).
Soon, however, it became clear that the plan involved delegating much of the burden of carrying out years of follow-up work to the local GPs. Those with well-established practices grasped immediately that such added obligations would not glide smoothly into everyday General Practice clinical life. Some resistance—and anger—began to manifest within NSAM. In Norway, as in Iceland, the GP's clear, albeit unspoken, message was simple: “You are welcome to run your own shop—but not inside my shop.”
Questions arose: Who would define the problem? What sources of knowledge would be deemed valid, and by whose authority? What consequences would result? What actual benefits, if any, might this intervention yield?
Some GPs had raised such issues earlier, at the very start of the study, but without awakening much interest among health authorities and researchers (17). However, when the number of people posing this sort of question finally reached a critical mass, a common objective emerged: to examine evidence that sheds light on the discipline of Family Medicine in general, and on the role of the GP in particular.
Discussions and debates at the NSAM meetings in Norway, began to focus on what GPs stand for and want to prioritize. Based on this work, and under the leadership of Anna Stavdal, GP, NSAM drew up their Sju teser (Seven Principles of Good Medical Practice for General Practitioners). In 2001, this itemized, passionate, expression (in Norwegian) of GP's professional values and principles was published and distributed, formatted as an eye-catching poster (Figure 1) (1, 19–21). Here, the seven main principles are specified as imperatives, with clarifications of relevant principles and actions next to each. We have seen since then what an effective tool for advocating for our profession and our patients that this short, striking poster has proven to be.
The 2001 English translation draft of Principle 2. of the Sju teser reads: “Do what is most important,” further clarified by, “prioritizing patients with conditions in need of treatment, and sparing patients from wrongfully being treated as sick.” Today, we might have written, “avoid overmedicalization and overtreatment,” but those terms had not yet entered the medical discourse.
The ongoing debates in the Nordic countries, including those regarding Principle 2., convinced Irene Hetlevik, GP, later Professor of Family Medicine, and Stavdal, of the need to adapt the Norwegian Sju teser to suit the Nordic milieu. In 2004, they established the Nordic Risk Group (NRG), under Hetlevik's leadership (22). Inspired by such industrial companies as Toyota, the group began to refer to its tasks and actions in terms of vision and mission. As far as we know, this was the first time those concepts were applied in the context of Nordic Family Medicine. The NRG saw value as being implicit within the concept of vision. Medicalization, which had entered the discussions regarding good medical practice by then, was also seen as being incorporated within vision, as in, “… systematically aiming to minimize medicalization and risk-labeling” (22, 23). Later, the campaign against unnecessary health care interventions called “Choosing Wisely” came on the scene in the Nordic countries and elsewhere.
Within the Nordic countries, the pace of implementing modern Family Medicine has varied, and that saga can not be told fully here. While some of our colleagues were fighting for Family Medicine to serve as an organizing concept, others formed groups to focus on specific topics. In Sweden, the ideology of Family Medicine was met with great resistance, primarily from representatives of various specialties. In the 1980's, two prominent colleagues, Göran Sjönell, GP, later President of WONCA, and Carl Edward Rudebeck, GP, later Professor of Family Medicine, initiated a heroic fight for modern Family Medicine (3, 24). In 1988, when Sjönell and colleagues cast doubts on the evidence used to justify routine, breast cancer screening using mammography, a heated and longstanding debate was ignited (25, 26). Our Swedish colleague's experiences contribute significant insight and support to the development of our common Nordic Core Values.
Most of the above processes were ongoing in other parts of the world as well, and were interconnected. In Denmark, in the late 1990's, Hanne Hollnagel, GP, Professor of Family Medicine and head researcher for the Glostrup Epidemiological Study, took the initiative to organize debates on the risk concept, similar to those in which our colleagues in Norway, Sweden, and Iceland were engaged (27, 28).
In 1998, Carl Erik Mabeck, GP, Professor of Family Medicine, led Danish GPs in arranging a workshop to explore the future of General Practice (Et fremtidsværksted). Implicit in the title of their published brochure, Discussion Paper on Core Functions of General Practice (29), is an acknowledgment that ongoing discussions regarding the core functions of General Practice are both important and necessary. It also indicates support for the type of self-awareness the Balint model includes, one which gradually leads to a “…limited but substantial change in the GP's personality” (30).
In 2014, the Organization of General Practitioners in Denmark (PLO) joined with the Danish College (DSAM), to launch an extensive vision process. They collected data from hundreds of Danish GPs participating in nation-wide focus group discussions, who had agreed to share their views on the core principles and purposes of General Practice. Although political concerns put a stop to their vision process, the organizers did not waste their collected data. In 2016, inspired by the structure of the Norwegian Sju teser of 2001, DSAM, headed by one of the authors here (AB), utilized analyses of that data to help them formulate Pejlemaerker for faget almen medicin (Guideposts for the Profession of General Practice Medicine), their own, updated version of their professional principles and values. Instead of phrasing these as seven imperatives, they expressed them as personal values by using first-person plural descriptions: “We do….” (2, 31).
Finland, Sweden, Norway, Denmark, and Iceland have been collaborating productively for decades (32–34). They share common history, culture, and ideology, as well as knowledge, skills, and attitudes, regarding Family Medicine, their Nordic colleagues, and their academic institutions (32). In 2005, this collaboration was formalized through the establishment of the Nordic Federation of General Practice (NFGP) (35).
In 2017, the Nordic Federation decided to reexamine our tasks and objectives, ultimately expressed as vision and mission statements. The first aim of this project was to merge the Norwegian Sju teser and the Danish Pejlemaerker for faget almen medicin into an English-language statement on which we could all agree. By 2020, we had our: Core Values and Principles of Nordic Family Medicine. The second project aim was to reach out digitally to our Nordic networks, associations, and congresses, to engage as many Nordic colleagues as possible in a shared awareness process. The third aim was to devise ways to adapt and extend our own consensus process to include colleagues and their associations in countries beyond our own region. These processes have been described more fully elsewhere (2).
The main strength of our analysis of this Saga-In-Progress lies in the fact that we, the authors, not only experienced the fifty years covered here as active GPs but were also opinion leaders in the Nordic evolution of modern Family Medicine. Those years of the new discipline's development were often turbulent, with hefty debates going on within the health care establishment. Consequently, the main limitation of this analysis may be that it is undeniably from our perspective.
The journey toward formulating our core values that we have documented here may also be understood in terms of the WHO Alma Ata Declaration of 1978 mentioned above. Viewed from that perspective, the WHO did indeed mandate the field of Family Medicine to provide value-based health care. As stated in the Alma Ata Declaration:
…The Conference strongly reaffirms that health, which is a state of complete physical, mental and social well-being, and not merely the absence of disease or infirmity, is a fundamental human right and that the attainment of the highest possible level of health is a most important world-wide social goal whose realization requires the action of many other social and economic sectors in addition to the health sector.
GPs and stakeholders of Family Medicine have acted accordingly. A substantial body of research and literature described elsewhere confirms the relevance and validity of Family Medicine, associating it with better health, better health care, and lower costs (2, 36–39). Among the conclusions to be drawn from the history above is that, to understand General Practice, knowledge must be combined with a specific skill set and a particular attitude. In other words, implementing a holistic approach involves more than addressing the complexity of patient's problems; it also requires an understanding of the complexity of the role of Family Medicine within society.
Although our values will endure, standards of care do indeed vary, depending on the economy, organization, and/or political situation of each country. As the WHO Alma Ata Declaration acknowledges, standards of care must be tailored to what the community/country can afford. Consequently, the precise formulations of the Core Values and Principles that the Nordic Colleges have put forth can not, and should not, be assumed to be applicable everywhere; each culture/country must consider what adaptations are needed. Nonetheless, our Nordic Core Values and Principles statement, and our process of arriving at it, serve as useful resources.
In a recent paper published in this journal, Arvidsson et al. (40) recount the ongoing discussions about European core values and the challenges being faced. They note that the attention given to these concepts is increasing as processes to define core values emerge in various European countries.
In line with the WHO's declaration regarding primary health care (7, 41, 42), Family Medicine will continue to provide sustainable, responsible, relationship-based care, and to protect the human side of medicine. Meantime, as described earlier, our organizational principles and clinical priorities are challenged, repeatedly, by stakeholders outside our discipline. In such situations, awareness processes among our colleagues, colleges, and our WONCA family are of utmost importance. Sharing a common set of core values and principles can motivate and mobilize us as advocates both for our discipline and for our patients, the citizens whom we serve.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
JS and AS: conceived of the idea for this paper. JS, AB, and AS: contributed to its planning. JS: wrote the first draft. All authors: read and approved the final manuscript.
The Research Fund of the Icelandic College of Family Physicians and the Nordic Federation of General Practice contributed to this work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank Susan Schwartz Senstad, MA, MFA, editorial consultant, and novelist, for her language editing, semiotic skills, and contributions to the text.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.681612/full#supplementary-material
1. Nordic Federation of General Practice (NFGP). Core values and principles of Nordic general practice/family medicine. Scand J Prim Health Care. (2020) 38:367–8. doi: 10.1080/02813432.2020.1842674
2. Sigurdsson JA, Beich A, Stavdal A. Our core values will endure. Scand J Prim Health Care. (2020) 38:363–6. doi: 10.1080/02813432.2020.1842676
3. Rudebeck CE. Relationship based care - how General Practice developed and why it is undermined within contemporary healthcare systems. Scand J Prim Health Care. (2019) 37:335–44. doi: 10.1080/02813432.2019.1639909
4. WONCA Europe. The European definition of General Practice/Family Medicine. 2nd ed. (2011). Available online at: http://www.globalfamilydoctor.com/site/DefaultSite/filesystem/documents/regionDocs/European%20Definition%20of%20general%20practice%203rd%20ed%202011.pdf.
5. McWhinney I. Principles of family medicine. In: Ian McWhinney R. A Textbook of Family Medicine. 2nd ed. Oxford, Oxford University Press (1997). p. 13.
6. Pendleton D, King J. Values and leadership. BMJ. (2002) 325:1352–55. doi: 10.1136/bmj.325.7376.1352
7. WHO. Declaration of Alma Ata. (1978). Available online at: https://www.euro.who.int/en/publications/policy-documents/declaration-of-alma-ata,-1978
8. Millis JS. The graduate education of physicians: report of the citizens committee on graduate medical education. Am Med Assoc. (1966). doi: 10.1001/jama.1966.03110120095022
9. Hajar R. Framingham contribution to cardiovascular disease. Heart Views. (2016) 17:78–81. doi: 10.4103/1995-705X.185130
10. Blackburn H. The origins and early evolution of epidemiologic research in cardiovascular diseases: a tabular record of cohort and case-control studies and preventive trials initiated from 1946 to 1976. Am J Epidemiol. (2019) 188:1–8. doi: 10.1093/aje/kwy175
11. Oddson OH, Brennan M. Framhaldsnám í heimilislækningum (from Icelandic: Graduate studies in Family Medicine). (University of Western Ontario, Canada). Laeknabladid. (1983) 69:146–9.
12. Illich I. Limits to Medicine. Medical Nemesis, The Expropriation of Health. London: Marion Boyars (1976). doi: 10.1097/00004010-197700000-00017
13. Icelandic Medical Association. Ársskýrsla Læknafélags Íslands, starfsárið* 1983–1984 (from Icelandic: Annual report from the Icelandic Medical Association years 1983–1984). Laeknabladid. (1984) 70:303–22.
14. Holmen J, Hetlevik I, Ellekjær E, Gjelsvik B, Kimsås A, Meland E. Kliniske retningslinjer for primærhelsetjenesten (from Norwegian: Clinical guidelines for primary health care). Tidsskr Nor Lægeforen. (1999) 119:1794–9.
15. Hetlevik I, Holmen J, Ellekjær H, Gjelsvik B, Kimsås A, Meland E. Kliniske retningslinjer for hypertensjon (from Norwegian: Clinical guidelines for hypertension). Tidsskr Nor Lægeforen. (1999) 119:3037–41.
16. Sturmberg JP, Martin CM, Katerndahl DA. Systems and complexity thinking in the general practice literature: an integrative, historical narrative review. Ann Fam Med. (2014) 12:66–74. doi: 10.1370/afm.1593
17. Swensen E. Diagnose: Risiko (From Norwegian: Diagnosis: At Risk). Oslo: Universitetsforlaget (2000). p 163.
18. Bjartveit K, Stensvold I, Lund-Larsen PG, Gjervig T, Krüger O, Urdal P. Hjerte-og karundersøkelser i norske fylker. Bakgrunn og gjennomføring. Status 1986–90 for risikomønster bland 40–42 åringer i 14 fylker (from Norwegian: Cardiovascular screenings in Norwegian counties. Background and implementation. Status of risk patterns during the period 1986–90 among persons aged 40–42 years in 14 counties). Tidsskr Nor Laegeforen. (1991) 111:2063–72.
19. Norsk Selskap for Allmennmedisin (NSAM). Sju teser for allmennmedisin (from Norwegian: Seven Principles of Good Medical Practice for General Practitioners). Utposten. (2001) 30:17–8.
20. Baerheim A, Rortveit G. Defining general practice: an open process gives challenging postulates. Scand J Prim Health Care. (2002) 20:129–31. doi: 10.1080/028134302760234546
21. Stavdal A. Fra projekt til syv teser for almen medisin (from Danish: From project to Seven Principles of good medical practice for General Practitioners). In: Kan sundhedsvæsenet skape usundhed? Refleksioner fra almen praksis Eds Lotte Hvas, John Brodersen and Birgitta Hovelius Aka-Print A/S, Tilst, Copenhagen. (2009).
22. The Nordic Risk Group. Available online at: http://nordicriskgroup.net/ (accessed May 2021).
23. Getz L. Sustainable and Responsible Preventive Medicine. Conceptualising Ethical Dilemmas Arising From Clinical Implementation of Advancing Medical Technology. Thesis, Trondheim: Norwegian University of Science and Technology (NTNU) (2006) p. 1–211. Available online at: https://core.ac.uk/download/pdf/52107523.pdf
24. Sjönell Göran (book) Husläkarfallet (from Swedish: The ‘Family Doctor’ Case). Stockholm Liber utbildning/Almqvist & Wiksell medicin (1994). p 158.
25. Sjönell G. Ompröva mammografibesluten! (from Swedish: Re-think decisions regarding mammography screening!) Dagens Nyheter-arkivet. 21 oktober 1988
26. Sjönell G, Ståhle L. Hälsokontroller med mammografi minskar inte dödlighet i bröstcancer (from Swedish: Mammography screening does not reduce cancer mortality). Läkartidningen. (1999) 96:904–13.
27. Hollnagel H. Om risikosproget i den almenmedicinske konsultation. Fra gruppebaseret epidemiologisk viden til almenpraksis (from Danish: See ref no 29). Practicus. (1996) 106:237–9.
28. Hollnagel H. Explaining risk factors to patients during a General Practice consultation. Conveying group-based epidemiological knowledge to individual patients. Scand J Prim Health Care. (1999) 17:3–5. doi: 10.1080/028134399750002809
29. Mabeck CE, Moltke A, Schulsinger C, Gannik D, Maunsbach M, Foged L, et al. Debatoplæg om kernefunktionen i almen praksis (from Danish: Discussion Paper on the core functions of General Practice). Praktiserende Lægers Organization, Dansk Selskab for Almen Medisin Lægeforeningens forlag (2000).
30. Salinsky J. Balint groups and the Balint method. The Balint Society. (2003). Available online at: https://balint.co.uk/about/the-balint-method/ (accessed February 15, 2021).
31. Dansk Selskap for Almen Medicin (Danish College of General Practice). Available online at: https://www.dsam.dk/pejlemaerker/#baggrund (accessed August 14, 2020).
32. Sigurdsson JA, Stavdal A, Getz L. The nordic congresses of general practice - a gateway to a global treasure? Scand J Prim Health Care. (2006) 24:196–8. doi: 10.1080/02813430601016910
33. Reventlow S, Sångren H, Brodersen J, Christensen B, Grauengaard A, Jarbøl D, et al. Addressing the future role of general practice at the 16th Nordic congress in Copenhagen 2009: how can we ensure sustainable care in a complex world of evidence, context, organisation and personal care? Scand J Prim Health Care. (2008) 26:193–5. doi: 10.1080/02813430802542524
34. Sigurdsson JA. Milestones in the development of nordic general practice. Scand J Prim Health Care. (2013) 31:3–5. doi: 10.3109/02813432.2012.762163
35. Stavdal A. The Nordic federation of general practice. Scand J Prim Health Care. (2005) 23:129. doi: 10.1080/02813430500217106
37. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. (2005) 83:457–502. doi: 10.1111/j.1468-0009.2005.00409.x
38. van Royen P, Beyer M, Chevallier P, Eilat-Tsanani S, Lionis C, Peremans L, et al. The research agenda for general practice/family medicine and primary health care in Europe. Part 3 Results: person centred care, comprehensive and holistic approach. Eur J Gen Pract. (2010) 16:113–19. doi: 10.3109/13814788.2010.481018
39. Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors—a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open. (2018) 8:e021161. doi: 10.1136/bmjopen-2017-021161
40. Arvidsson E, Švab I, Klemenc-Ketiš Z. Core values of family medicine in Europe: current state and challenges. Frontiers in Medicine. (2021) 8:1–7. doi: 10.3389/fmed.2021.646353
41. WHO. Declaration of Astan. Available online at: https://www.who.int/teams/primary-health-care/conference/declaration (accessed March 2021).
Keywords: core values, sustainability, person-centered, continuity, history, family medicine
Citation: Sigurdsson JA, Beich A and Stavdal A (2021) A Saga-In-Progress: Challenges and Milestones on Our Way Toward the Nordic Core Values and Principles of Family Medicine/General Practice. Front. Med. 8:681612. doi: 10.3389/fmed.2021.681612
Received: 16 March 2021; Accepted: 04 November 2021;
Published: 26 November 2021.
Edited by:
Ryuki Kassai, Fukushima Medical University, JapanReviewed by:
Roger Peter Strasser, Northern Ontario School of Medicine, CanadaCopyright © 2021 Sigurdsson, Beich and Stavdal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Johann A. Sigurdsson, am9oYW5uLmEuc2lndXJkc3NvbkBudG51Lm5v
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.