- 1Department of Critical Care Medicine, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, China
- 2Department of Respiratory, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, China
- 3Department of Cardiology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, China
Purpose: This study aimed to describe the clinical and laboratory characteristics and the parameters of the respiratory mechanics of mechanically ventilated patients with confirmed COVID-19 pneumonia and to clarify the risk or protective factors for weaning failure.
Methods: Patients diagnosed with COVID-19 pneumonia were selected from the special intensive care unit (ICU) of the Sino-French New City Branch of Tong Ji Hospital, Wuhan, and treated by the National Medical Team Work. They were divided into successful weaning (SW) group (N = 15) and unsuccessful weaning (USW) group (N = 18) according to the prognosis. Information of these patients was analyzed.
Results: There were 33 patients included in this study. Patients in the USW group were associated with a poor outcome; the 28-day mortality rate was higher than in the SW group (86.7 vs. 16.7% p < 0.001). By comparison, we found that the initial plateau pressure (Pplat) and driving pressure (DP) of the USW group were higher and that compliance was lower than that of the SW group, but there was no difference between positive end-expiratory pressure (PEEP), partial pressure of carbon dioxide (PCO2), and the ratio of partial pressure arterial oxygen and fraction of inspired oxygen (P/F ratio). Comparing the worst respiratory mechanics parameters of the two groups, the results of the Pplat, DP, compliance, and PEEP were the same as the initial data. The PCO2 of the USW group was higher, while the P/F ratio was lower. A logistic regression analysis suggested that higher Pplat might be an independent risk factor and that higher compliance and lower DP might be protective factors for weaning failure of invasive mechanically ventilated patients with COVID-19 pneumonia.
Conclusions: Patients with USW were associated with a poor outcome, higher Pplat might be a risk factor, and a higher compliance and a lower DP might be protective factors for the weaning failure of ventilated COVID-19 patients. Mechanical ventilation settings will affect the patient's prognosis.
Introduction
The outbreak of COVID-19 disease caused by the novel coronavirus (SARS-CoV-2) has been a worldwide pandemic problem and resulted in thousands of death (1). Its morbidity and mortality are much higher than those of other viral pneumonia. About 15–20% of suspected and confirmed patients developed dyspnea and severe hypoxemia (2); since no specialized medication to treat SARS-CoV-2 infection has been identified at this time, mechanical ventilation is the main supportive treatment for critically ill patients, especially invasive mechanical ventilation. Whether the ventilated patients can wean successfully is a key factor related to the patient's outcome. The mortality of ventilated patients with COVID-19 pneumonia was high (86.3% 19/22) in an observational study from a single center, the Jinyintan Hospital (a temporarily designated center for critically ill patients with COVID-19), Wuhan, China (3). The parameters of the respiratory mechanics, especially plateau pressure (Pplat), transpulmonary pressure (Ptp), or driving pressure (DP), were the major risk factors for the acute respiratory distress syndrome (ARDS) patients (4). Recent studies showed that the DP was high, respiratory system compliance was low, and hypercapnia was common in the ventilated patients with COVID-19 while using low tidal volume ventilation (5, 6), but the sample size was small, and the risk factors for the weaning failure of the ventilated COVID-19 patients were not described.
We aim to describe the clinical and laboratory characteristics, and the parameters of the respiratory mechanics of mechanically ventilated patients with confirmed COVID-19 pneumonia, and to clarify the risk or protective factors for weaning failure. We hope our study findings will inform on the global fight against the COVID-19 disease.
Materials and Methods
Study Design and Patient Enrollment
This study was a retrospective clinical study at the special intensive care unit (ICU) of the Sino-French New City Branch of Tong Ji Hospital, Wuhan. All subjects were selected from the population of inpatients hospitalized between February 2020 and March 2020 in the departments mentioned above. This study was approved by the ethics review board of PUMCH (ZS-2332).
Inclusion and Exclusion Criteria
The following inclusion criterion was used: patients with diagnosed COVID-19 by nucleic acid detection and imaging evidence based on the Novel Coronavirus Pneumonia Diagnosis and Treatment Program (Version 7) released by China Health Commission. Patients were excluded from the study if they met the following criteria: (i) under 18 years of age and (ii) died within 48 h of admittance to the ICU. Patients who satisfied the inclusion criteria were divided into a successful weaning (SW) group and an unsuccessful weaning (USW) group in accordance with the outcome during the treatment. USW is defined as either the failure of spontaneous breathing trial (SBT) or the need for invasive mechanical ventilation or reintubation within 48 h following weaning or extubation in our study (7). Failure of SBT is defined by objective indices of failure, such as tachypnea, tachycardia, hypertension, hypotension, hypoxemia or acidosis, and arrhythmia (8).
Treatment
Based on the respiratory mechanics features and current medical conditions, we performed a ventilation strategy. (1) Initial application of lung protection ventilation strategy: low tidal volume (VT) ventilation (VT 4–6 ml/kg of predicted body weight), the target Pplat was set at lower than 30 cmH2O, a higher positive end-expiratory pressure (PEEP) strategy ≥10 cmH2O, usage of sedative and analgesic drugs and neuromuscular blocking agents (NMBAs). (2) Prone position ventilation (PPV) was performed when the ratio of partial pressure arterial oxygen and fraction of inspired oxygen (P/F ratio) was <150 and was performed at the physicians' discretion. (3) If refractory hypercapnia exists, evaluate the recruitability; a higher level of PEEP and recruitment maneuvers may help to reduce hypercapnia and acidosis in patients who were recruited by reducing physiologic dead space and shunt. (4) In those who had no potential for recruitment, increase the respiratory rate (RR) to 30–35 bpm, lower the PEEP, increase VT to 8 ml/kg, and ensure that the Pplat <30 cmH2O and the DP <17 cmH2O. (5) Due to shortage of extracorporeal membrane oxygenation (ECMO), extracorporeal carbon dioxide removal (ECCO2R) may mitigate hypercapnia. Routine procedures for the hemodynamic therapy and a conservative fluid strategy were performed, and antibiotics were administered intravenously at the discretion of the attending clinician.
Measurements and Data Collection Involved in this Study
All the data of these involved patients were recorded, including general data, mechanical ventilation data, hemodynamic data, outcome, and other therapies. The general data included the age, gender, Sequential Organ Failure Assessment (SOFA) score, Acute Physiology and Chronic Health Evaluation II (APACHEII) score, Glasgow coma scale (GCS), white blood cells (WBCs), lymphocytes, platelets, total bilirubin (Tbil), creatinine, prothrombin time, fibrinogen (Fbg), D-dimer, procalcitonin (PCT), IL-6, high-sensitivity C-reactive protein (hs-CRP), and high-sensitivity cardiac troponin I (hs-CTNI). In addition, comorbidities (hypertension, diabetes, coronary heart disease, chronic renal insufficiency, chronic underlying lung disease, and cerebrovascular disease), the time from the symptom onset to intubation, and the duration of non-invasive ventilation (NIV)/high-flow oxygen therapy (HFOT) were recorded. The initial and worst mechanical ventilation data included the Pplat, DP, VT, RR, partial pressure of carbon dioxide (PCO2), (P/F), and minute ventilation (MV). The initial respiratory mechanics parameters were defined as the value of the first day of intubation or admittance to the ICU. The worst respiratory mechanics parameters were defined as the worst value in the treatment process after ICU admission, including the lowest value of P/F, lung compliance, and the highest values of Pplat, DP, PCO2, and PEEP. The hemodynamic data included heart rate (HR), mean arterial pressure (MAP), left ventricular ejection fraction (LVEF), and lactate (lac). The outcome included ventilation-free day (VFD) of 28 days, the length of stay in ICU, 28 days' mortality, and the complications [pneumothorax, ventilator-associated pneumonia (VAP), bloody infection, acute kidney injury (AKI), myocardial injury, coagulopathy, and liver injury]. Acute kidney injury was identified on the basis of serum creatinine. Cardiac injury was diagnosed if the serum concentration of hs-CTNI was above the upper limit of the reference range (>15.6 pg/ml), measured in the laboratory of Tong Ji Hospital. Other therapies included PPV, ECMO, ECCO2R, continuous renal replacement therapy (CRRT), and the use of vasoactive drugs.
Statistical Analysis
Statistical analyses were performed using SPSS 16.0 (SPSS, Chicago, IL, USA), and a p < 0.05 was considered significant. Quantitative data with normal distributions are denoted as means ± standard deviation. Student's t-test was performed to compare means between the two groups. Quantitative data that were abnormally distributed are denoted as medians (interquartile ranges), and the rank-sum test was performed for these data. Data of unordered categories are denoted as rates, and differences between groups were examined using the chi-squared test or Fisher's exact test. The multi-factor logistic regression was used to estimate differences between the two groups and to explore the risk factors.
Results
The Demographic and Clinical Characteristics of the Patients Involved in this Study
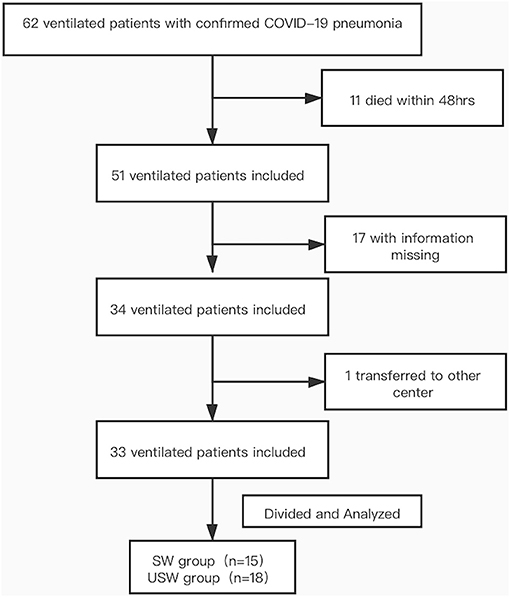
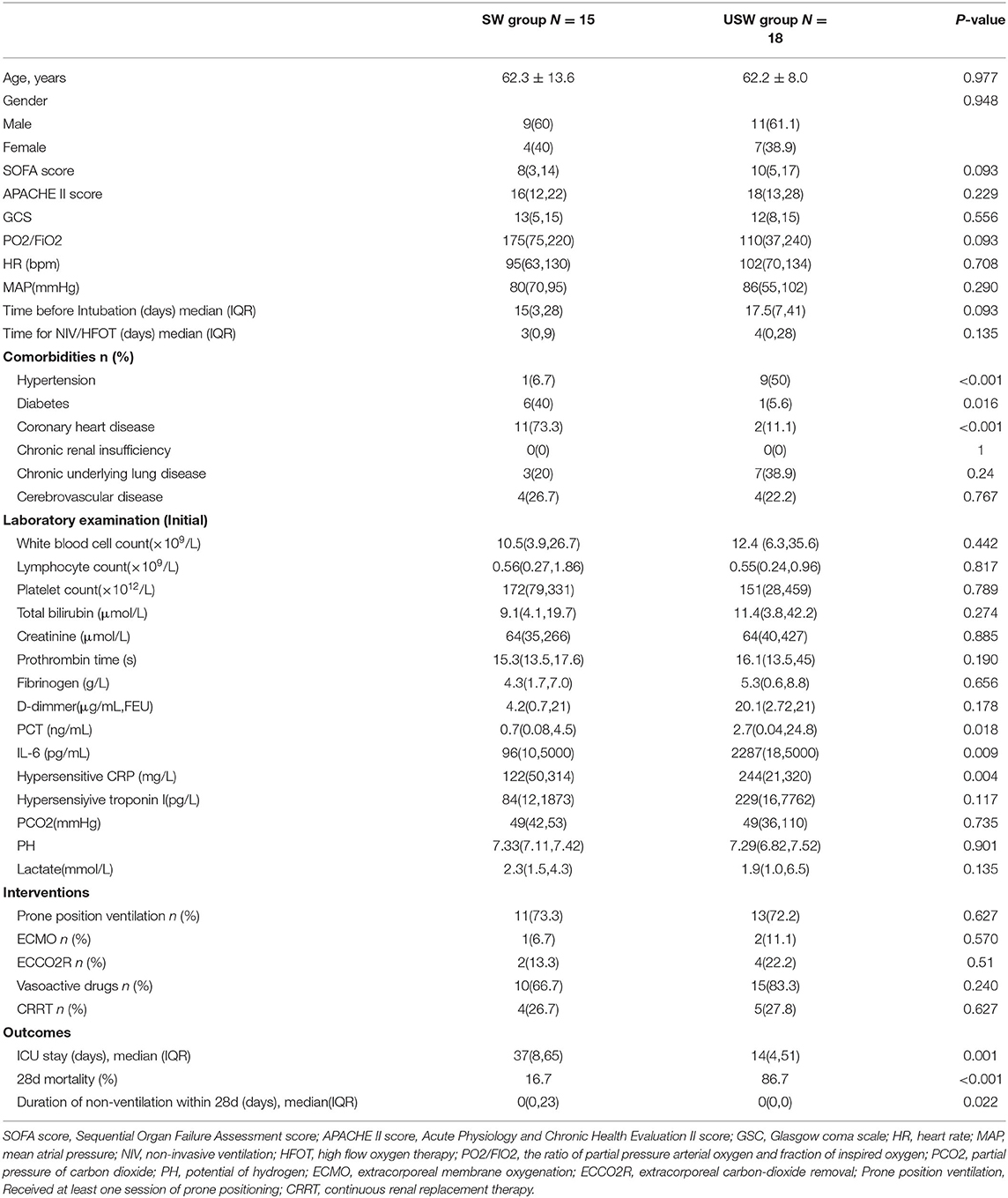
By March 2020, 62 ventilated patients with confirmed COVID-19 pneumonia had been admitted to the special ICU of the Sino-French New City Branch of Tong Ji Hospital, of whom 29 were excluded (11 died within 48 h of ICU admission, 17 with missed information, and one transferred to another center). There were 33 patients involved in this study, including 15 cases of SW group and 18 cases of USW group (as shown in Figure 1). The demographic and clinical characteristics of the included patients are summarized in Table 1. There was no difference between the two groups in term of age (p = 0.977), gender (p = 0.948), SOFA score (p = 0.093), and APACHE II score (p = 0.229). Patients in the USW group were associated with a poor outcome, the 28-day mortality rate was higher than in the SW group (86.7 vs. 16.7% p < 0.001), and VFD of 28 days and ICU stays were lower than in the SW group (p = 0.022, 0.001). The PCT, IL-6, and hs-CRP were higher in the USW group; p-values were 0.018, 0.009, and 0.004, respectively. The comorbidities hypertension, diabetes, and coronary heart disease also had significant differences. In addition, there were no significant differences in terms of hemodynamic parameters, interventions, the time before intubation, and the time for NIV/HFOT between the two groups.
The Mechanical Ventilation Parameters at the Initial and Worst Stages
We compared the mechanical ventilation parameters (initial) of the first day of intubation or admittance to the ICU and those of the worst stage in the course of treatment. By comparison, we found that the initial Pplat and DP of the USW group were higher and that compliance was lower than that of the SW group, but there was no difference between PEEP, PCO2, and P/F ratio. Comparing the worst respiratory mechanics parameters of the two groups, the results of the Pplat, DP, compliance, and PEEP were same as the initial data. The PCO2 of the USW group was higher, while the P/F was lower (Figure 2).
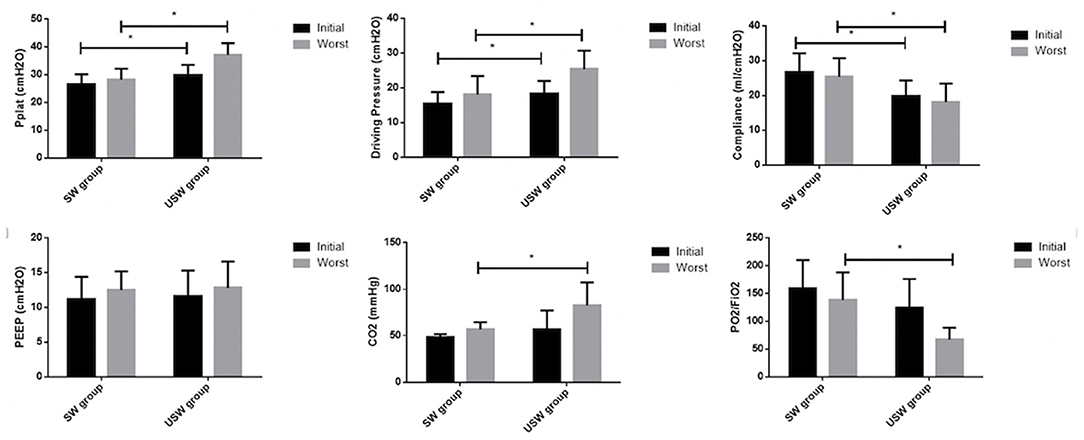
Figure 2. The mechanical ventilation parameter comparison between successful weaning (SW) and unsuccessful weaning (USW). Initial, the first day of intubation or admittance to the intensive care unit (ICU); Worst, the worst in the observation days; PEEP, positive end-expiratory pressure; Pplat, plateau pressure; PCO2, partial pressure of carbon dioxide; PaO2/FiO2, the ratio of partial pressure arterial oxygen and fraction of inspired oxygen. *means the p-value <0.05 between two groups.
Complication Comparison for Successful Weaning Vs. Unsuccessful Weaning
The USW group had more myocardial injury, coagulopathy, and liver injury than the SW group as shown in Table 2 (p-values were 0.001, 0.002, and 0.008 respectively); there was no difference in the incidence of other complications (p > 0.05).
Risk Factors for Weaning Failure of Mechanically Ventilated Patient
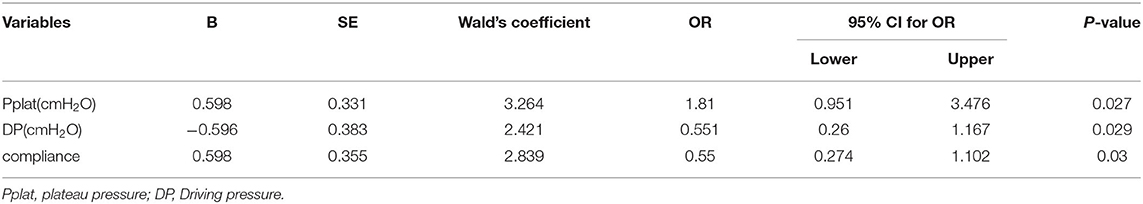
The Table 3 showed that the Pplat was a risk factor for unsuccessful weaning (OR = 1.81, 95% CI 0.951–3.476), Low driving pressure and high compliance were protective factors, The OR of low driving pressure and high compliance were 0.551 (95% CI, 0.26–1.1 67) and 0.55 (95% CI, 0.274–1.1 02), respectively.
Discussion
This retrospective study provided a detailed analysis of invasive mechanical ventilation of COVID-19 patients and explored the risk factors for the weaning failure in one tertiary center of Wuhan, China. Our results indicated that patients in the USW group were associated with a poor outcome and more complications. Furthermore, we found that high Pplat was a risk factor for USW and that low DP and high compliance were protective factors.
In this single-center observational study, the mortality of ventilated COVID-19 patients was high compared with that of other reports at 25–50% (9–11); we assumed that the respiratory mechanics characteristics of our patients were not the same as those of the two phenotypes reported by Gattinoni et al. (12). Weaning from mechanical ventilation is an individualized process in which a gentle balance between respiratory system load and capacity must be achieved (13). Our result showed that patients with weaning failure had a poor outcome and more complications, which was similar to the previous study (14–16). A multicenter prospective study also found that the mortality rate of patients with successful liberation from MV of 28 days was lower than that of the unsuccessful group (0 vs. 62.4%) (14). Our findings indicate the importance of weaning failure in the management of COVID-19; whether the ventilated patients can be weaned successfully is a key factor related to the patient's mortality rate.
We observed that the USW group had higher Pplat, DP, and PCO2 and lower VT, P/F ratio, and compliance than the SW group (p < 0.05). Pplat was the risk factor for USW, and low DP and high compliance are protective factors in this study. Our findings were not consistent with those of other centers. Oadya found no statistically significant correlation between patients' characteristics and the weaning failure (15), and a study from Japan observed a decreasing trend in respiratory static compliance despite the higher PEEP setting after day 5 and a higher ventilatory ratio in patients with prolonged MV than in those with early liberation (16). In the landmark ARDS Network trial, long-term mortality improved when VT was limited to an average of 6 ml/kg of predicted body weight and Pplat to <30 cmH2O (17). Pplat is the sum of PEEP and DP. The mechanical effects of high PEEP depend on lung recruitability (18) and are harmful (hyperinflation of previously opened alveoli) for our patients with non-potential for recruitment. DP corresponds to the elastic pressure swing; excessive DP increases the risk of VT-induced strain and is associated with higher mortality (19, 20). In the PRoVENT-COVID study, the median of DP was 14 cmH2O (19). Actually, recent data (21) have demonstrated that there is no safe upper limit for DP; the slope of the relationship between DP and mortality appears to be positive even at DP below 14 cmH2O, suggesting that patient outcomes may be improved with the decreasing DP. The SATICOVID study also showed that DP was strongly associated with mortality (22). Regardless of whether it is due to the high peep or DP, a high Pplat (close to 30 cmH2O) is an important cause for alarm for clinicians. In prior studies, respiratory compliance has not been an independent factor for weaning failure when it was measured early in the ARDS (23, 24). Compliance <40 ml/cmH2O has been recently proposed to identify a more severe phenotype of COVID-19 (25). In Gamberini's study, the results showed that compliance <40 ml/cmH2O was independently associated with both prolonged mechanical ventilation and mortality (15). Our findings may be explained in part by using the worst compliance. The worst compliance of USW group patients was only 11.67 ± 4.51 ml/cmH2O, which were lower than that reported in other centers. PPV had been used to COVID-19 pneumonia in our patients (73.3% in the SW group and 72.2% in the USW group). There was no difference between the two groups. The reason may be that the pathophysiological phenotypes of the two groups were different; PPV has no obvious effectiveness in the USW group. These findings reminded us that in early implementation of lung protection strategies, lowering plateau pressure and DP is important to avoid lung injury in COVID-19 patients. As the sample size with extracorporeal support was too small due to shortage of resources, there was no difference between the two groups in our study. We still recommend that if conventional methods do not work, special respiratory therapy such as ECCO2R and ECMO should be performed as soon as possible.
This study has several limitations. First, this study was conducted at a single-center hospital with limited sample size. There may also be a selection bias when identifying factors that influence the clinical outcomes. A larger cohort study of ventilated patients with COVID-19 pneumonia would help to further define the clinical characteristics and risk factors of the disease. Second, some patients failed to enroll because specific information was missing. However, the 33 patients we enrolled had all the detailed results of complete respiratory mechanics monitoring and dynamic records. This is very precious. Third, this is a retrospective study; the data in this study permit a preliminary assessment of the outcomes of critically ill patients with SARS-CoV-2 pneumonia. Further studies are still needed.
Conclusion
Based upon an analysis of the data from mechanically ventilated COVID-19 patients, it can be observed that patients with weaning failure were associated with a poor outcome and more complications. A higher Pplat might be a risk factor; a higher compliance and a lower DP might be protective factors for the weaning failure of ventilated COVID-19 patients. Early implementation of lung protective strategies and lower plateau pressure and DP are important to avoid lung injury in COVID-19 patients.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics review board of PUMCH (ZS-2332). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
XZ and SZ: study conceptualization and writing—review and editing. HZ and LS: study design, formal analysis and investigation, and writing—original draft preparation. HZ, XD, HC, HZ, JW, and SZ: methodology. All authors commented on the previous version of the manuscript and have read and approved the final manuscript.
Funding
The National Key R&D Program of China (grant number 2020YFC0861000); The CAMS Innovation Fund for Medical Sciences (CIFMS) (No. 2020-I2M-CoV19-001); The China International Medical Exchange 2020 CMB Open Competition Program (No. 20-381); Chinese Medical Information and big data Association (CHMIA) Special Fund for Emergency Project, Beijing Municipal Natural Science Foundation (M21019).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. (2020) 46:846–8. doi: 10.1007/s00134-020-05991-x
2. Qiu H, Tong Z, Ma P, Hu M, Peng Z, Wu W, et al. China critical care clinical trials, intensive care during the coronavirus epidemic. Intensive Care Med. (2020) 46:576–8. doi: 10.1007/s00134-020-05966-y
3. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. (2020) 8:475–81. doi: 10.1016/S2213-2600(20)30079-5
4. Henderson WR, Chen L, Amato MBP, Brochard LJ. Fifty years of research in ARDS. Respiratory mechanics in acute respiratory distress syndrome. Am J Respir Crit Care Med. (2017) 196:822–33. doi: 10.1164/rccm.201612-2495CI
5. Liu X, Liu X, Xu Y, Xu Z, Huang Y, Chen S, et al. Ventilatory ratio in hypercapnic mechanically ventilated patients with COVID-19 associated ARDS. Am J Respir Crit Care Med. (2020) 201:1297–9. doi: 10.1164/rccm.202002-0373LE
6. Pan C, Chen L, Lu C, Zhang W, Xia JA, Sklar MC, et al. Lung recruitability in SARS-CoV-2 associated acute respiratory distress syndrome: a single-center, observational study. Am J Respir Crit Care Med. (2020) 201:1294–7. doi: 10.1164/rccm.202003-0527LE
7. Jubran A, Tobin MJ. Pathophysiologic basis of acute respiratory distress in patients who fail a trial of weaning from mechanical ventilation. Am J Respir Crit Care Med. (1997) 155:906–15. doi: 10.1164/ajrccm.155.3.9117025
8. Esteban A, Frutos F, Tobin MJ, Alia I, Solsona JF, Valverdu I, et al. A comparison of four methods of weaning patients from mechanical ventilation. Spanish Lung Failure Collaborative Group. N Engl J Med. (1995) 332:345–50. doi: 10.1056/NEJM199502093320601
9. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. doi: 10.1001/jama.2020.1585
10. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. (2020) 368:m1295. doi: 10.1136/bmj.m1295
11. Itelman E, Wasserstrum Y, Segev A, Avaky C, Negru L, Cohen D, et al. Clinical characterization of 162 COVID-19 patients in Israel: preliminary Report from a Large Tertiary Center. Isr Med Assoc J. (2020) 22:271–4.
12. Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. (2020) 46:1099–102. doi: 10.1007/s00134-020-06033-2
13. McConville JF, Kress JP. Weaning patients from the ventilator. N Engl J Med. (2012) 367:2233–9. doi: 10.1056/NEJMra1203367
14. Gamberini L, Tonetti T, Spadaro S, Zani G, Mazzoli CA, Capozzi C, et al. Factors influencing liberation from mechanical ventilation in coronavirus disease 2019: multicenter observational study in fifteen Italian ICUs. J Intensive Care. (2020) 8:80. doi: 10.1186/s40560-020-00499-4
15. Ovadya D, Bachar K, Peled M, Skudowitz M, Wollner A. Weaning of severe COVID-19 mechanically ventilated patients: experience within a dedicated unit in Israel. Isr Med Assoc J. (2020) 22:733–5.
16. Kasugai D, Ozaki M, Nishida K, Hiraiwa H, Jingushi N, Numaguchi A, et al. Usefulness of respiratory mechanics and laboratory parameter trends as markers of early treatment success in mechanically ventilated severe coronavirus disease: a single-center pilot study. J Clin Med. (2021) 10:2513. doi: 10.3390/jcm10112513
17. Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. (2000) 342:1301–8. doi: 10.1056/NEJM200005043421801
18. Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. (2006) 354:1775–86. doi: 10.1056/NEJMoa052052
19. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, Patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. (2016) 315:788–800. doi: 10.1001/jama.2016.0291
20. Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. (2015) 372:747–55. doi: 10.1056/NEJMsa1410639
21. Guerin C, Papazian L, Reignier J, Ayzac L, Loundou A, Forel JM, et al. Effect of driving pressure on mortality in ARDS patients during lung protective mechanical ventilation in two randomized controlled trials. Crit Care. (2016) 20:384. doi: 10.1186/s13054-016-1556-2
22. Estenssoro E, Loudet CI, Rios FG, Kanoore Edul VS, Plotnikow G, Andrian M, et al. Clinical characteristics and outcomes of invasively ventilated patients with COVID-19 in Argentina (SATICOVID): a prospective, multicentre cohort study. Lancet Respir Med. (2021). doi: 10.1016/S2213-2600(21)00229-0. [Epub ahead of print].
23. Monchi M, Bellenfant F, Cariou A, Joly LM, Thebert D, Laurent I, et al. Early predictive factors of survival in the acute respiratory distress syndrome. A multivariate analysis. Am J Respir Crit Care Med. (1998) 158:1076–81. doi: 10.1164/ajrccm.158.4.9802009
24. Zilberberg MD, Epstein SK. Acute lung injury in the medical ICU: comorbid conditions, age, etiology, hospital outcome. Am J Respir Crit Care Med. (1998) 157:1159–64. doi: 10.1164/ajrccm.157.4.9704088
Keywords: weaning failure, mechanical ventilation, COVID-19 pneumonia, risk factors, prognosis
Citation: Zhao H, Su L, Ding X, Chen H, Zhang H, Wang J, Long Y, Zhou X and Zhang S (2021) The Risk Factors for Weaning Failure of Mechanically Ventilated Patients With COVID-19: A Retrospective Study in National Medical Team Work. Front. Med. 8:678157. doi: 10.3389/fmed.2021.678157
Received: 09 March 2021; Accepted: 26 July 2021;
Published: 31 August 2021.
Edited by:
You Shang, Huazhong University of Science and Technology, ChinaReviewed by:
Jingen Xia, China-Japan Friendship Hospital, ChinaJiapeng Huang, University of Louisville, United States
Jianfeng Wu, The First Affiliated Hospital of Sun Yat-sen University, China
Copyright © 2021 Zhao, Su, Ding, Chen, Zhang, Wang, Long, Zhou and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiang Zhou, enhfcHVtY0AxNjMuY29t; Shuyang Zhang, c2h1eWFuZ3poYW5nMTAzQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Hua Zhao
Hua Zhao Longxiang Su
Longxiang Su Xin Ding
Xin Ding Huan Chen1
Huan Chen1 Yun Long
Yun Long Xiang Zhou
Xiang Zhou