
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Med., 17 March 2021
Sec. Family Medicine and Primary Care
Volume 8 - 2021 | https://doi.org/10.3389/fmed.2021.616355
This article is part of the Research TopicThe Relationship Between Cardiovascular Disease and Other Chronic ConditionsView all 39 articles
 Li Zou1,2†
Li Zou1,2† Qiao Zong3†
Qiao Zong3† Wenning Fu4,5
Wenning Fu4,5 Zeyu Zhang1
Zeyu Zhang1 Hongbin Xu3
Hongbin Xu3 Shijiao Yan2,6
Shijiao Yan2,6 Jin Mao4
Jin Mao4 Yan Zhang7*
Yan Zhang7* Shiyi Cao3*
Shiyi Cao3* Chuanzhu Lv5,8,9,10*
Chuanzhu Lv5,8,9,10*Background and Objective: An increasing number of epidemiological original studies suggested that long-term exposure to particulate matter (PM2.5 and PM10) could be associated with the risk of myocardial infarction (MI), but the results were inconsistent. We aimed to synthesized available cohort studies to identify the association between ambient air pollution (PM2.5 and PM10) and MI risk by a meta-analysis.
Methods: PubMed and Embase were searched through September 2019 to identify studies that met predetermined inclusion criteria. Reference lists from retrieved articles were also reviewed. A random-effects model was used to calculate the pooled relative risk (RR) and 95% confidence intervals (CI).
Results: Twenty-seven cohort studies involving 6,764,987 participants and 94,540 patients with MI were included in this systematic review. The pooled results showed that higher levels of ambient air pollution (PM2.5 and PM10) exposure were significantly associated with the risk of MI. The pooled relative risk (RR) for each 10-μg/m3 increment in PM2.5 and PM10 were 1.18 (95% CI: 1.11–1.26), and 1.03 (95% CI: 1.00–1.05), respectively. Exclusion of any single study did not materially alter the combined risk estimate.
Conclusions: Integrated evidence from cohort studies supports the hypothesis that long-term exposure to PM2.5 and PM10 is a risk factor for MI.
The incidence and prevalence of cardiovascular diseases have increased in recent decades, and cardiovascular disease has become one of the main causes of death among adults (1–3). Myocardial infarction (MI) is an acute and severe cardiovascular disease that generally can endanger the life of patients and has become a serious public health problem (4). The causes of MI are complex and are related to lifestyle, diet structure, genetic factors, and environmental factors, including air pollution (5–7). Studies have shown that reducing modifiable risk factors may contribute to the prevention and control of MI (8–10), which is of considerable public health importance.
Air pollution, especially particulate matter (PM), has been increasingly investigated as an environmental risk factor for MI morbidity and mortality recently. However, studies have had modest sample sizes and reported inconclusive results (11–13). These inconsistent and controversial results indicate the need to quantitatively synthesize and interpret the available evidence to provide more explicit information for policy decisions and clinical use. Meta-analysis is a statistical tool that can be used to integrate results of multiple independent studies considered to be combinable for a more precise estimation (14, 15). Although previous meta-analyses have examined associations between air pollution exposure and MI, their studies have mostly included cross-sectional literatures (13), and much new research has been recently published. Therefore, more meta-analyses with cohort studies are urgently needed.
Taking into consideration the inconsistent conclusions and the limitations of existing epidemiological studies and the flaws of previous meta-analyses, we therefore performed a systematic review and meta-analysis of cohort epidemiological studies to examine the potential associations between air pollution exposure and the risk of MI. Given the heavy economic and health burden of curing MI, the results of our study may provide additional practical and valuable clues for the prevention of MI.
Ethical approval is not required for this systematic review.
We conducted this meta-analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) (16) and the checklist of items in the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) (17). A systematic literature search of PubMed and Embase was conducted through September 2019 by using the following search terms with no restrictions: “air pollution” or “particulate matter” or “air pollutants” or “PM10”or “PM2.5” or “air quality” in combination with “myocardial infarction” or “heart attack” or “acute coronary syndrome” or “cardiovascular disease” or “heart disease.” The language was restricted to English. Additionally, reference lists of the retrieved original articles and relevant review articles were also scrutinized to identify further pertinent studies.
Studies meeting the following criteria were included in the meta-analysis: (1) the study design was cohort; (2) the exposure of interest was ambient air pollution; the endpoint of interest was the incidence of MI; and (3) the relative risk (RR) and the corresponding 95% confidence interval (CI) of MI relating to ambient air pollution were reported or could be calculated from the data provided. Animal studies, clinical trials, reviews, letters, and commentaries were excluded. Only studies with detailed information on both ambient air pollution and the incidence of MI was included.
Two investigators (WF and SC) extracted the following information from the studies: first author, publication year, country, study period, age, number of cases, size of cohort, and time windows of exposure. Discrepancies were resolved by discussion with a third investigator (SC).
The Newcastle-Ottawa Scale, used to evaluate the qualities of cohort studies (18), is a nine-point scale allocating points based on the selection of participants, comparability of groups, and exposure/outcome. This scale awards a maximum of nine points to each study: four for selection of participants and measurement of exposure, two for comparability of cohorts or cases and controls on the basis of the design or analysis, and three for assessment of outcomes and adequacy of follow-up. Studies scoring 0–3 points, 4–6 points, and 7–9 points were categorized as low, moderate, and high quality of studies, respectively. When studies had several adjustment models, we extracted those that reflected the maximum extent of adjustment for potentially confounding variables. Each study was rated independently by two authors (WF and JM). Discrepancies were resolved by discussion with a third investigator (SC).
We used RR to measure the association between ambient air pollution and the risk of MI and the random effects model was used to calculate an overall pooled RR for the main analysis.
The Q statistic with a significance level at P < 0.10 and I2 statistic were used to test heterogeneity. The I2 statistic measures the percentage of total variation across studies due to heterogeneity rather than chance. It was calculated according to the formula by Higgins (19). We used I2 to quantify the heterogeneity, with 25%, 50%, and 75% indicating low, moderate and high degrees of heterogeneity, respectively.
In our meta-analysis the following formula was used to calculate the standardized risk estimates for each study:
Subgroup analyses were conducted to determine the possible influence of some factors such as state and publication years. We conducted a sensitivity analysis to explore potential sources of heterogeneity and to investigate the influence of various exclusion criteria on the pooled risk estimate. Begg's rank correlation and Egger's linear regression tests were used to assess the potential publication bias (20, 21). Using Duval and Tweedie's non-parametric trim-and-fill method to adjust potential publication bias (22). All analyses were performed using STATA statistical software (version 12.0; College Station, TX, USA), and all tests were two-sided with a significance level of 0.05.
Figure 1 shows the process of study identification and inclusion. Initially 3,097 and 3,243 citations were retrieved from PubMed database and Embase, respectively. After the exclusion of 282 duplicates, 6,058 potentially relevant studies from electronic databases were identified. Of these, we excluded 6,031 papers because they were experimental, biomechanics, reviews, or irrelevant studies. After full-text review of the remaining 213 articles, 46 articles were excluded because of insufficient data to calculate the risk estimates, and 167 were excluded because they were not a risk factor. Finally, 27 studies (23–49) were included.
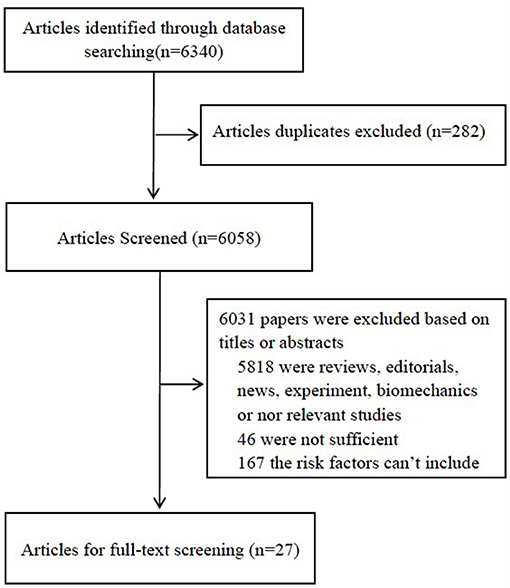
Figure 1. Flow diagram of identification of relevant observational studies of ambient air pollution in relation to the risk of MI.
The main characteristics of the 27 studies on MI and long-term PM exposure in our meta-analysis were summarized in Table 1. These studies were published between 2004 and 2019. Among them, eight studies were from Europe, two studies were from Asia, and twelve studies were from America. The size of the cohorts ranged from 1,120 to 4,404,046 for a total of 6,764,987 subjects. The exposure measure was PM2.5 in seventeen studies and PM10 in eleven studies; six publications investigated the association of MI with exposure to both PM2.5 and PM10.The end point was MI incidence (sixteen studies), MI mortality (twelve studies), and only one study MI hospital, and two studies included MI incidence and mortality. Twenty studies were published after 2010, and seven studies before 2010. The quality assessment scores ranged from 6 to 9, with an average score of seven points, representing satisfactory quality of the studies.
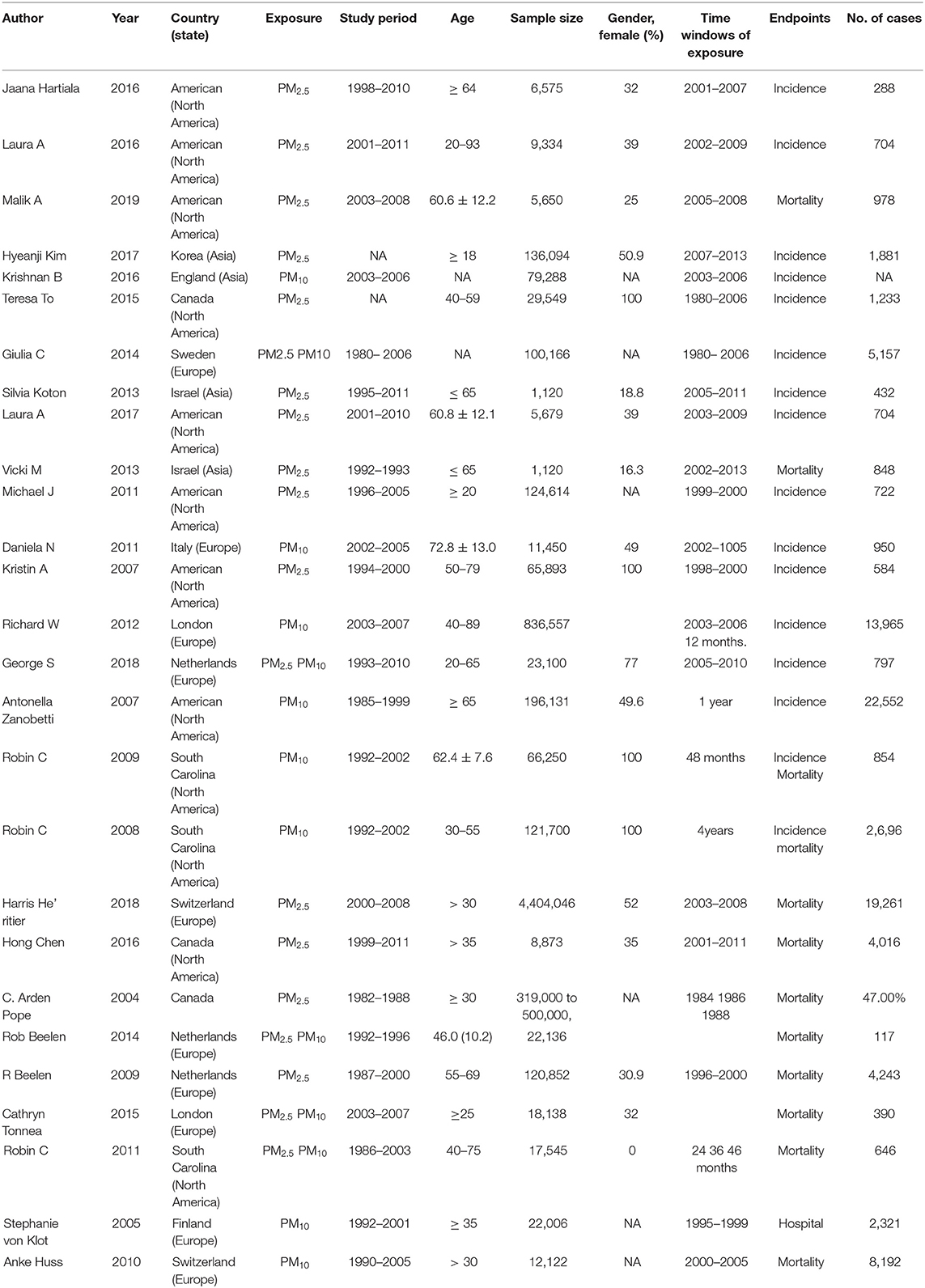
Table 1. Main characteristics of the studies included involving ambient air pollution and the risk of myocardial infarction.
We employed meta-analysis to assess the association of PM2.5 and PM10 with MI.
The results from random-effects meta-analysis of ambient air pollution (PM2.5 and PM10) and the risk of MI were shown in Figure 2. Twenty studies reported the effect of PM2.5 exposure on the risk of MI and the pooled estimates suggested a positive relationship. Results from standardized data showed that a 10 mg/m3 increase in PM2.5 exposure was positively associated with the risk of MI (RR = 1.18, 95% CI: 1.11 to 1.26), and there was a moderate heterogeneity (p = 0.002; I2 = 54.2%). Subgroup analyses by state, and publication year (before 2010 vs. after 2010) showed no statistically significant difference in results (Table 2). Every single pooled result of subgroup showed the positive and statistically significant relationship between exposure to PM2.5 and the risk of MI.
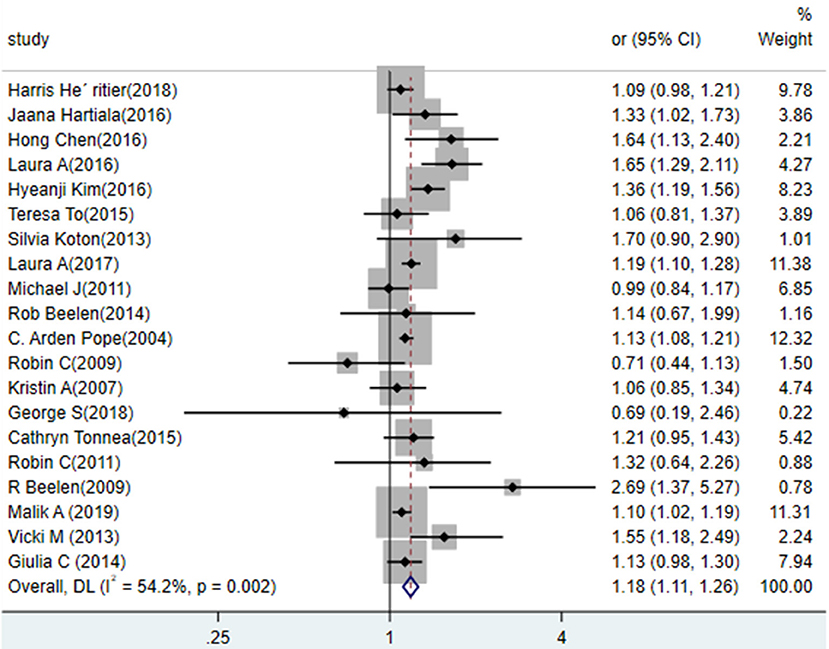
Figure 2. Association between exposure to PM2.5 and the risk of MI in a meta-analysis of cohort studies. Weights are from random- efforts model.
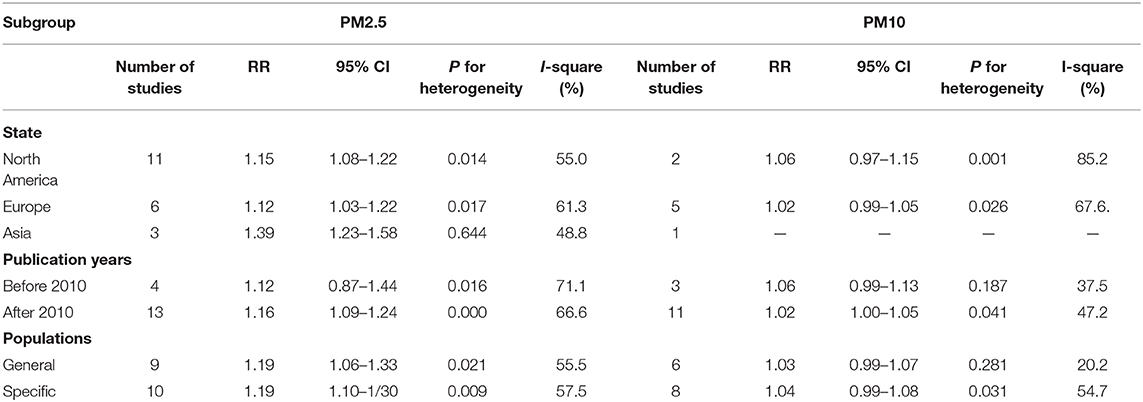
Table 2. Results of subgroup analyses about ambient air pollution and the risk of myocardial infarction.
Fourteen studies investigated the association of PM10 exposure with the risk of MI (Figure 3). The pooled estimates of these studies indicated that a 10 mg/m3 increase in PM10 was associated with a higher risk of MI (RR = 1.03, 95% CI: 1.00 to 1.05), and the heterogeneity is (p = 0.052, I2 = 41.5%). We conducted subgroup analyses by state, and publication year (before 2010 vs. after 2010). In general, these subgroup analyses showed no statistically significant difference in results.
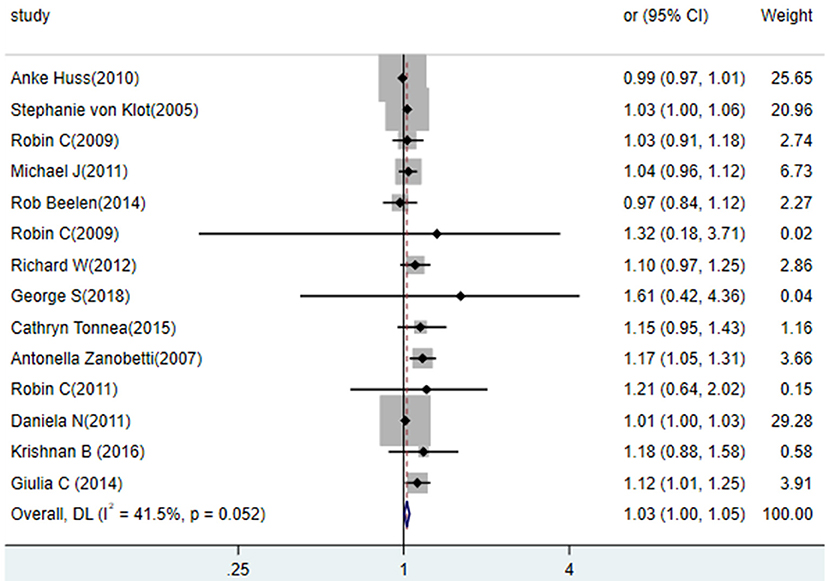
Figure 3. Association between exposure to PM10 and the risk of MI in a meta-analysis of cohort studies. Weights are from random- efforts model.
Sensitivity analyses was conducted to find potential sources of heterogeneity in the association between air pollution (PM2.5 and PM10) and MI risk, to examine the influence of various exclusions on the combined RR and assess the robustness of all results. The pooled RR did not materially change, for PM2.5 and PM10, the both overall combined RR did not materially change, with a range from 1.17 (95% CI: 1.10–1.24) to 1.19 (95% CI: 1.11–1.26), and 1.02 (95% CI: 1.00–1.04) to 1.03 (95% CI: 1.01–1.05), respectively.
Visual inspection of the funnel plot showed significant asymmetry (PM2.5: Figures 4, 5; PM10: Figures 6, 7). For PM2.5 and PM10, the Egger test indicated publication bias, but the Begg test did not (PM2.5: Egger, Z = 5.385, p = 0.000, Begg, t = 1.44: p = 0.168; PM10: Egger, Z = 2.283 p = 0.022, Begg, t = 1.22 p = 0.830). We used the trim-and-fill method to evaluate the impact of any potential publication bias, and the results showed that one and five potentially missing studies would be needed to obtain funnel plot symmetry for the association of MI and air pollution (PM2.5, PM10), respectively. After using the trim-and-fill method, both the corrected RR for PM 2.5 was 1.18 (95% CI: 1.10 to 1.26; random-effects model, p = 0.000), for PM10 was 1.03 (95% CI: 1.00 to 1.06; random-effects model, p = 0.027), which suggested the both pooled RRs were not substantially changed by the correction for potential publication bias.
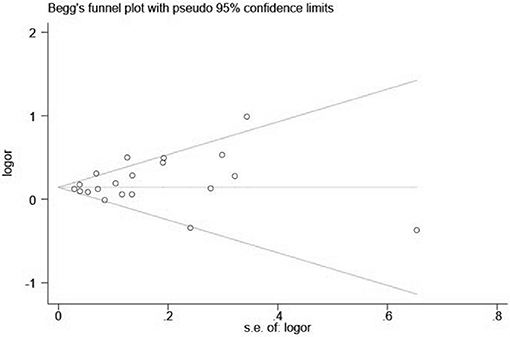
Figure 5. Filled funnel plot of RR from studies that investigated the association between PM2.5 and the risk of MI.
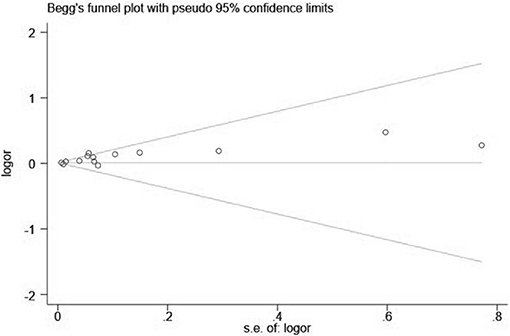
Figure 7. Filled funnel plot of RR from studies that investigated the association between PM10 and the risk of MI.
Myocardial infarction results in a high medical burden for families and society and remains a worldwide public health challenge (50). Ascertaining the risk factors of MI could provide significant information for the prevention of MI. Our meta-analysis has quantitatively examined the association between long-term exposure to ambient air pollution (PM2.5 and PM10) and MI. The pooled analysis, which included 27 cohort studies with more than 6.5 million people, showed an inverse association between exposures to air pollutants (PM2.5 and PM10) and the risk of MI, which was consistent with previous reviews and meta-analyses (13). However, previous meta-analyses included only studies published before 2014, while more recent studies were not included that might report lower estimates or negative results. Additionally, our meta-analysis included all cohorts from studies with reliable data, so that the effect of exposure can be fully and directly analyzed and conclusions are relatively stable.
The mechanisms by which air pollution exposure could contribute to the development of MI might include inflammation, induction of autophagy, and down-regulation of membrane repair protein MG53. Researchers found that inflammation plays an important role in the formation of coronary atherosclerosis and aggravation of plaque instability, and air pollutants can also promote MI by promoting inflammation (51). The second potential mechanism is the induction of autophagy. Several observational studies have shown that autophagy is a normal process for cells to achieve their own metabolism and organelle renewal. Autophagy can maintain the body's metabolism to reduce damage and protect the organism. However, excessive autophagy can lead to apoptosis of cardiomyocytes and aggravate the damage of ischemic-related sites (52). Studies have found that autophagic levels for exposure to air pollutants are significantly higher than in the control group, while the corresponding protein expression levels, MI size decreases, and myocardial cell damage decrease in Farnesoid X receptor (FXR) knock out SD rats. Therefore, it is speculated that exposure to air pollutants promotes the development of MI through FXR-induced autophagy (53). The third possible mechanism is down-regulation of membrane repair protein MG53. Exposure to air pollutants can affect membrane repair through down-regulation of the expression of MG53 protein and aggravation of the severity of ischemia and hypoxia in MI (54).
We also found that long-term exposure to PM2.5 has a more pronounced effect than PM10 on MI risk in each 10 μg/m3 increase, which is in line with previous related research (13). Compared with PM10, PM2.5 can remain suspended for a longer time in the air and be inhaled into the respiratory tract and directly into the pulmonary alveoli. In addition, PM2.5 has a larger superficial area and hence absorbs more chemical constituents than PM10. Therefore, PM2.5 is probably more harmful on human health than PM10 (55, 56).
Considering people's different diets and lifestyles and the prevalence of MI in different regions, we also conducted subgroup analysis by region, and statistically significant differences across subgroups were found except for PM10. In Asia, a 10 mg/m3 increase in PM2.5 exposure was positively associated with the risk of MI (RR = 1.38), which was inconsistent with previous studies. The possible reasons for the differences include inconsistency of study designs and potentially selective reporting of the results for pollutants. However, it is suggested that the Asia region should pay attention to the relationship between air pollution and MI, and more work on air pollution and epidemiology remains to be done. We conducted a subgroup analysis by publication year but found the pooled result of studies before 2010 was not significantly different from that after 2010.
There are several strengths in this meta-analysis. First, all the studies in our analysis were cohort studies, which is considered as stronger measure for demonstrating causation and identification of risk factors than other observational study designs (57). Second, in this comprehensive literature review, we pooled data from 22 cohort studies from several geographical regions in one meta-analysis, thus increasing the statistical power and allowing an investigation of regional patterns. Third, sensitivity analysis and consistent results from various subgroup analyses indicated that our findings were reliable and robust, although heterogeneity existed among the included studies. Furthermore, all the studies were published in the past decade, indicating that data on both the exposure and the outcome are recent and relevant.
Some limitations in the present meta-analysis should be of concern. First of all, the heterogeneity of the studies included was significant and existed through the whole analysis. But we explored the potential heterogeneity resources by subgroup analysis and sensitivity analysis. Second, there are relatively few studies on the mortality and hospitalization of MI, and there is a lack of data required for meta-analysis, so subgroup analysis is not conducted. Third, other air pollutants may have interaction with PM2.5 and PM10. A compounding effect of all these air pollutants should be examined and quantified on increasing the risk of MI.
In conclusion, our meta-analysis identified long-term exposure to PM2.5 and PM10 as a significant risk factors of MI. In light of the heavy economic burden of MI, the results of our study provide additional valuable clues for the prevention of MI. For future studies, more high-quality longitudinal and interventional studies are needed to explore the underlying mechanisms of the relationships between ambient air pollution and MI, especially in Asia and other middle- and low-income countries. Besides, it is recommended that relevant departments must adopt a comprehensive particulate matter control policy to promote health and reduce the burden of MI.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
LZ, QZ, YZ, SC, and CL conceived and designed the study. LZ, QZ, WF, ZZ, HX, SY, JM, YZ, SC, and CL participated in the acquisition of data. LZ and QZ analyzed the data. YZ, CL, and SC gave advice on methodology. LZ drafted the manuscript. LZ, QZ, WF, ZZ, HX, SY, JM, YZ, SC, and CL revised the manuscript. All authors read and approved the final manuscript.
This study was funded by the China Postdoctoral Science Foundation (2020M672366) and Key Laboratory of Emergency and Trauma, Ministry of Education, College of Emergency and Trauma (KLET-202002).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank all the authors of the studies included in our meta-analysis.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.616355/full#supplementary-material
1. Brunekreef B, Holgate ST. Air pollution and health. Lancet. (2002) 360:1233–42. doi: 10.1016/S0140-6736(02)11274-8
2. Li J, Li X, Wang Q, Hu S, Wang Y, Masoudi FA, et al. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet. (2015) 385:441–51. doi: 10.1016/S0140-6736(14)60921-1
3. Pope CA, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA. (2002) 287:1132–41. doi: 10.1001/jama.287.9.1132
4. Cendon S, Pereira LAA, Braga ALF, Conceição GMS, Junior AC, Romaldini H, et al. Air pollution effects on myocardial infarction. Rev Saude Publica. (2006) 40:414–9. doi: 10.1590/S0034-89102006000300008
5. Anand SS, Islam S, Rosengren A, Franzosi MG, Steyn K, Yusufali AH, et al. Risk factors for myocardial infarction in women and men: insights from the INTERHEART study. Eur Heart J. (2008) 29:932–40. doi: 10.1093/eurheartj/ehn018
6. Dahabreh IJ, Paulus JK Association of episodic physical and sexual activity with triggering of acute cardiac events: systematic review and meta-analysis. JAMA. (2011) 305:1225–33. doi: 10.1001/jama.2011.336
7. Finegold JA, Asaria P, Francis DP. Mortality from ischaemic heart disease by country, region, and age: statistics from World Health Organisation and United Nations. Int J Cardiol. (2013) 168:934–45. doi: 10.1016/j.ijcard.2012.10.046
8. Smyth A, O'Donnell M, Lamelas P, Teo K, Rangarajan S, Yusuf S, et al. Physical activity and anger or emotional upset as triggers of acute myocardial infarction: the INTERHEART study. Circulation. (2016) 134:1059–67. doi: 10.1161/CIRCULATIONAHA.116.023142
9. Teo KK, Liu L, Chow CK, Wang X, Islam S, Jiang L, et al. Potentially modifiable risk factors associated with myocardial infarction in China: the INTERHEART China study. Heart. (2009) 95:1857–64. doi: 10.1136/hrt.2008.155796
10. Colombo A, Proietti R, Culic V, Lipovetzky N, Viecca M, Danna P. Triggers of acute myocardial infarction: a neglected piece of the puzzle. J Cardiovasc Med. (2014) 15:1–7. doi: 10.2459/JCM.0b013e3283641351
11. Bhaskaran K, Hajat S, Haines A, Herrett E, Wilkinson P, Smeeth L. Effects of ambient temperature on the incidence of myocardial infarction. Heart. (2009) 95:1760–9. doi: 10.1136/hrt.2009.175000
12. Madrigano J, Kloog I, Goldberg R, Coull BA, Mittleman MA, Schwartz J. Long-term exposure to PM2.5 and incidence of acute myocardial infarction. Environ Health Perspect. (2013) 121:192–6. doi: 10.1289/ehp.1205284
13. Mustafic H, Jabre P, Caussin C, Murad MH, Escolano S, Tafflet M, et al. Main air pollutants and myocardial infarction: a systematic review and meta-analysis. JAMA. (2012) 307:713–21. doi: 10.1001/jama.2012.126
14. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
15. Zeng X, Zhang Y, Kwong JSW, Zhang C, Li S, Sun F, et al. The methodological quality assessment tools for preclinicaland clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evidence Based Med. (2015) 8:2–10. doi: 10.1111/jebm.12141
16. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
17. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
18. Wells G, Shea B, O'Connell J (2014). Available online at: https://www.researchgate.net/publication/288802810_The_Newcastle-Ottawa_Scale_NOS_for_Assessing_The_Quality_of_Nonrandomised_Studies_in_Meta-analyses
19. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
20. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. Biometrics. (1994) 50:1088–101. doi: 10.2307/2533446
21. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
22. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. (2000) 56:455–63. doi: 10.1111/j.0006-341X.2000.00455.x
23. Hartiala J, Breton CV, Tang WH, Lurmann F, Hazen SL, Gilliland FD, et al. Ambient air pollution is associated with the severity of coronary atherosclerosis and incident myocardial infarction in patients undergoing elective cardiac evaluation. J Am Heart Assoc. (2016) 5:e003947. doi: 10.1161/JAHA.116.003947
24. Atkinson RW, Carey IM, Kent AJ, van Staa TP, Anderson HR, Cook DG Long-term exposure to outdoor air pollution and incidence of cardiovascular diseases. Epidemiology. (2013) 24:44–53. doi: 10.1097/EDE.0b013e318276ccb8
25. McGuinn LA, Ward-Caviness CK, Neas LM, Schneider A, Diaz-Sanchez D, Cascio WE, et al. Association between satellite-based estimates of long-term PM2.5 exposure and coronary artery disease. Environ Res. (2016) 145:9–17. doi: 10.1016/j.envres.2015.10.026
26. Kim H, Kim J, Kim S, Kang SH, Kim HJ, Kim H, et al. Cardiovascular effects of long-term exposure to air pollution: a population-based study with 900 845 person-years of follow-up. J Am Heart Assoc. (2017) 6:e007170. doi: 10.1161/JAHA.117.007170
27. To T, Zhu J, Villeneuve PJ, Simatovic J, Feldman L, Gao C, et al. Chronic disease prevalence in women and air pollution–A 30-year longitudinal cohort study. Environ Int. (2015) 80:26–32. doi: 10.1016/j.envint.2015.03.017
28. Koton S, Molshatzki N, Yuval, Myers V, Broday DM, Drory Y, et al. Cumulative exposure to particulate matter air pollution and long-term post-myocardial infarction outcomes. Prev Med. (2013) 57:339–44. doi: 10.1016/j.ypmed.2013.06.009
29. McGuinn LA, Ward-Caviness C, Neas LM, Schneider A, Di Q, Chudnovsky A, et al. Fine particulate matter and cardiovascular disease: comparison of assessment methods for long-term exposure. Environ Res. (2017) 159:16–23. doi: 10.1016/j.envres.2017.07.041
30. Lipsett MJ, Ostro BD, Reynolds P, Goldberg D, Hertz A, Jerrett M, et al. Long-term exposure to air pollution and cardiorespiratory disease in the California teachers study cohort. Am J Respir Crit Care Med. (2011) 184:828–35. doi: 10.1164/rccm.201012-2082OC
31. Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. (2007) 356:447–58. doi: 10.1056/NEJMoa054409
32. Downward GS, van Nunen E, Kerckhoffs J, Vineis P, Brunekreef B, Boer JMA, et al. Long-term exposure to ultrafine particles and incidence of cardiovascular and cerebrovascular disease in a prospective study of a Dutch Cohort. Environ Health Perspect. (2018) 126:127007. doi: 10.1289/EHP3047
33. Zanobetti A, Schwartz J. Particulate air pollution, progression, and survival after myocardial infarction. Environ Health Perspect. (2007) 115:769–75. doi: 10.1289/ehp.9201
34. Puett RC, Hart JE, Yanosky JD, Paciorek C, Schwartz J, Suh H, et al. Chronic fine and coarse particulate exposure, mortality, and coronary heart disease in the Nurses' Health Study. Environ Health Perspect. (2009) 117:1697–701. doi: 10.1289/ehp.0900572
35. Puett RC, Schwartz J, Hart JE, Yanosky JD, Speizer FE, Suh H, et al. Chronic particulate exposure, mortality, and coronary heart disease in the nurses' health study. Am J Epidemiol. (2008) 168:1161–8. doi: 10.1093/aje/kwn232
36. Heritier H, Vienneau D, Foraster M, Eze IC, Schaffner E, de Hoogh K, et al. A systematic analysis of mutual effects of transportation noise and air pollution exposure on myocardial infarction mortality: a nationwide cohort study in Switzerland. Eur Heart J. (2019) 40:598–603. doi: 10.1093/eurheartj/ehy650
37. Chen H, Burnett RT, Copes R, Kwong JC, Villeneuve PJ, Goldberg MS, et al. Ambient fine particulate matter and mortality among survivors of myocardial infarction: population-based cohort study. Environ Health Perspect. (2016) 124:1421–8. doi: 10.1289/EHP185
38. Pope CA 3rd, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, et al. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation. (2004) 109:71–7. doi: 10.1161/01.CIR.0000108927.80044.7F
39. Puett RC, Hart JE, Suh H, Mittleman M, Laden F. Particulate matter exposures, mortality, and cardiovascular disease in the health professionals follow-up study. Environ Health Perspect. (2011) 119:1130–5. doi: 10.1289/ehp.1002921
40. Beelen R, Hoek G, Houthuijs D, van den Brandt PA, Goldbohm RA, Fischer P, et al. The joint association of air pollution and noise from road traffic with cardiovascular mortality in a cohort study. Occup Environ Med. (2009) 66:243–50. doi: 10.1136/oem.2008.042358
41. Tonne C, Halonen JI, Beevers SD, Dajnak D, Gulliver J, Kelly FJ, et al. Long-term traffic air and noise pollution in relation to mortality and hospital readmission among myocardial infarction survivors. Int J Hyg Environ Health. (2016) 219:72–8. doi: 10.1016/j.ijheh.2015.09.003
42. von Klot S, Peters A, Aalto P, Bellander T, Berglind N, D'Ippoliti D, et al. Ambient air pollution is associated with increased risk of hospital cardiac readmissions of myocardial infarction survivors in five European cities. Circulation. (2005) 112:3073–9. doi: 10.1161/CIRCULATIONAHA.105.548743
43. Beelen R, Stafoggia M, Raaschou-Nielsen O, Andersen ZJ, Xun WW, Katsouyanni K, et al. Long-term exposure to air pollution and cardiovascular mortality: an analysis of 22 European cohorts. Epidemiology. (2014) 25:368–78. doi: 10.1097/EDE.0000000000000076
44. Huss A, Spoerri A, Egger M, Roosli M, Swiss National Cohort Study Group. Aircraft noise, air pollution, and mortality from myocardial infarction. Epidemiology. (2010) 21:829–36. doi: 10.1097/EDE.0b013e3181f4e634
45. Malik AO, Jones PG, Chan PS, Peri-Okonny PA, Hejjaji V, Spertus JA. Association of long-term exposure to particulate matter and ozone with health status and mortality in patients after myocardial infarction. Circ Cardiovasc Qual Outcomes. (2019) 12:e005598. doi: 10.1161/CIRCOUTCOMES.119.005598
46. Myers V, Broday DM, Steinberg DM, Yuval Drory Y, Gerber Y. Exposure to particulate air pollution and long-term incidence of frailty after myocardial infarction. Ann Epidemiol. (2013) 23:395–400. doi: 10.1016/j.annepidem.2013.05.001
47. Nuvolone D, Balzi D, Chini M, Scala D, Giovannini F, Barchielli A. Short-term association between ambient air pollution and risk of hospitalization for acute myocardial infarction: results of the cardiovascular risk and air pollution in Tuscany (RISCAT) study. Am J Epidemiol. (2011) 174:63–71. doi: 10.1093/aje/kwr046
48. Bhaskaran K, Hajat S, Armstrong B, Haines A, Herrett E, Wilkinson P, et al. The effects of hourly differences in air pollution on the risk of myocardial infarction: case crossover analysis of the MINAP databas. BMJ. (2011) 343:d5531. doi: 10.1136/bmj.d5531
49. Cesaroni G, Forastiere F, Stafoggia M, Andersen ZJ, Badaloni C, Beelen R, et al. Long term exposure to ambient air pollution and incidence of acute coronary events: prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ. (2014) 348:f7412. doi: 10.1136/bmj.f7412
50. Nielsen SH, Mouton AJ, DeLeon-Pennell KY, Genovese F, Karsdal M, Lindsey ML. Understanding cardiac extracellular matrix remodeling to develop biomarkers of myocardial infarction outcomes. Matrix Biol. (2019) 75–76:43–57. doi: 10.1016/j.matbio.2017.12.001
51. Frangogiannis NG. Cell biological mechanisms in regulation of the post-infarction inflammatory response. Curr Opin Physiol. (2018) 1:7–13. doi: 10.1016/j.cophys.2017.09.001
52. Hill SM, Wrobel L, Rubinsztein DC. Post-translational modifications of Beclin 1 provide multiple strategies for autophagy regulation. Cell Death Differ. (2019) 26:617–29. doi: 10.1038/s41418-018-0254-9
53. Tong F, Zhang H. Pulmonary Exposure to Particulate Matter (PM2.5) affects the sensitivity to myocardial ischemia/reperfusion injury through farnesoid-x-receptor-induced autophagy. Cell Physiol Biochem. (2018) 46:1493–507. doi: 10.1159/000489192
54. Miao Z, Chunren L, Xi L, Shuo C, Xinquan W, Lin Z, et al. Effect of fine particulate matter on myocardial infarction and MG53 expression in infracted heart of rats. Di San Jun Yi Da Xue Xue Bao. (2015) 37:404–8. doi: 10.16016/j.1000-5404.201409034
55. Guo Y, Tong S, Zhang Y, Barnett AG, Jia Y, Pan X. The relationship between particulate air pollution and emergency hospital visits for hypertension in Beijing, China. Sci Total Environ. (2010) 408:4446–50. doi: 10.1016/j.scitotenv.2010.06.042
56. Parker JD, Woodruff TJ, Basu R, Schoendorf eC. Air pollution and birth weight among term infants in California. Pediatrics. (2005) 115:121–8. doi: 10.1542/peds.2004-0889
Keywords: air pollution, particulate matter, myocardial infarction, meta-analysis, PM2.5 (AQI), PM10
Citation: Zou L, Zong Q, Fu W, Zhang Z, Xu H, Yan S, Mao J, Zhang Y, Cao S and Lv C (2021) Long-Term Exposure to Ambient Air Pollution and Myocardial Infarction: A Systematic Review and Meta-Analysis. Front. Med. 8:616355. doi: 10.3389/fmed.2021.616355
Received: 12 October 2020; Accepted: 04 February 2021;
Published: 17 March 2021.
Edited by:
Cristina Vassalle, Gabriele Monasterio Tuscany Foundation (CNR), ItalyReviewed by:
Francesca Gorini, National Research Council (CNR), ItalyCopyright © 2021 Zou, Zong, Fu, Zhang, Xu, Yan, Mao, Zhang, Cao and Lv. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chuanzhu Lv, bHZjaHVhbnpodTY3N0AxMjYuY29t; Yan Zhang, emhhbmd5YW4xNjA0QDE2My5jb20=; Shiyi Cao, Y2Fvc2hpeWlAaHVzdC5lZHUuY24=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.