- Department of Hepatobiliary and Pancreatic Surgery, Zhongnan Hospital of Wuhan University, Wuhan, China
Objective: This study aimed to determine the association between prognosis of COVID-19 patients with and without cancer. Moreover, we compared the prognosis of cancer patients subjected to anti-tumor therapy with those who have not undergone anti-tumor therapy in the past 6 months.
Methods and Results: A total of 7,926 adult patients with COVID-19 were retrospectively enrolled in Hubei Province,China between December 31, 2019 and February 20, 2020. Two hundred and seventy seven cancer patients (cancer group, median age 64 [IQR 56–70] years; 50.90% male) and 7,649 non-cancer patients were identified (non-cancer group, median age 55 [IQR 42–64] years; 48.19% male). The mortality rate was lower in the non-cancer group compared to the cancer group (4.50 vs. 9.03%; P < 0.001). The duration between onset and admission shorter in the cancer group (Days, 9 [IQR 5–18]) compared to the non-cancer group (Days, 10; [IQR 6–19]; P = 0.036). ICU occupancy was higher in the cancer group (n[%], 30[10.83%]) than in the non-cancer group (n[%], 314[4.11%]). In reviewing the anti-tumor therapy, data from 277 selected cancer patients were obtained out of which 74 patients had undergone anti-tumor therapy (mean age 65 [IQR 51–67] years; 45.95% male), 203 had not undergone anti-tumor therapy (non-anti-tumor therapy group, mean age 63 [IQR 53–75] years; 49.75% male) in the past 6 months. The mortality rate for the anti-tumor therapy group and the non-anti-tumor therapy group was similar (9.46 vs. 8.87%; P = 0.879).
Conclusion: The mortality rate was higher in COVID-19 patients with cancer compared to those without cancer. Moreover, anti-tumor therapy in the past 6 months did not worsen the prognosis of cancer patients with COVID-19.
Introduction
COVID-19 is currently a global pandemic. About 122,000 patients have been infected with COVID-19 in China with 4.63% death rate based on the data from the Chinese Center for Disease Control. There have been 207.17 million confirmed cases of COVID-19, including 4.36 million deaths on Aug 16th, 2021, reported to WHO (1). Previous studies focused on the general epidemiologic survey, clinical presentation, or prognosis of mild and severe pneumonia cases (2–7). However, limited studies exist on the epidemiology and prognosis in tumor patients infected with SARS-CoV-2 (8–11).
Herein, this study reports general epidemiologic survey, clinical presentation, and prognosis of a subgroup based on a multicentric observational outcome study from a large cohort of COVID-19 patients in Hubei province. A higher mortality rate was reported to be associated with cancer patients infected with SARS-CoV2. Of note, recent anti-tumor therapy does not jeopardize the prognosis of cancer patients with COVID-19. We hope that the findings from this study can provide insights to others (12) who are similarly confronted with the COVID-19 challenges that arise from cancer research.
Methods
Study Procedure and Patient Cohorts
This observational multicenter cohort study was performed in 19 tertiary hospitals in China. The admission of patients in the 19 hospitals were performed uniformly according to an executive order issued by the Chinese government (13). This study was approved by the Central Ethics Committees (Clinical Ethical Approval No. 2020010) and ratified by the Institutional Ethics Committees in each hospital without any alterations. Informed consent from patient was waived by the ethics committees from each hospital due to the emerging pandemics. COVID-19 diagnosis was determined through clinical manifestations, chest CT, or real-time RT-PCR according to WHO interim guidance and the New Coronavirus Pneumonia Prevention and Control Program (5th edition) published by the National Health Commission of China (14, 15). The inclusion criteria were patients diagnosed with COVID-19. The following exclusion criteria were used to determine the patient cohort: Age less than 18, incomplete medical records, without exact outcome (discharge or death). pregnancy, acute lethal organ injury (e.g., acute myocardial infarction, acute pulmonary embolism, or acute stroke), decompensated or end stage of chronic organ dysfunction (e.g., decompensated cirrhosis, decompensated chronic renal insufficiency, or severe congestive heart failure), acquired immune deficiency syndrome (AIDS), severe trauma (e.g., parenchymatous organ rupture, bleeding, fracture). Based on these criteria, a total of 7,926 COVID-19 patients admitted from December 31, 2019 to February 20, 2020 in 19 designated hospitals in Hubei Province, China were initially evaluated for inclusion. Exactly 277 patients having cancer or have a history of cancer were selected to represent the cancer group with COVID-19. The other 7,649 patients were enrolled in the non-cancer group.
Chest computerized tomography (CT) or throat-swab specimens were obtained from all patients upon admission. A team of physicians evaluated the severity of COVID-19. The demographics, clinical characteristics, medical history, laboratory tests, radiological reports, therapeutic intervention, and outcome data were obtained from the electronic medical records of the patients. The final date of follow up for determining the outcome was April 16th, 2020.
Data Collection
The clinical end point was defined by death or recovery at the time of discharge from the hospital. Following data were collected including patient demographic information (age, gender), medical histories and underlying diseases [e.g., hypertension, diabetes mellitus, chronic obstructive pulmonary disease (COPD), chronic liver disease, chronic kidney disease], tumor type and location, prior treatment history (chemotherapy, radiation therapy, targeted therapy, surgery), physical examination findings and clinical manifestation (fever, cough, fatigue, dyspnea, and comorbidities), laboratory data [e.g., complete blood count, C-reactive protein (CRP), procalcitonin (PCT), hepatorenal function test, serum cardiac enzyme concentration], radiologic report data [unilateral or bilateral infiltrates was classified according to computed tomography (CT) scan of the chest], invasive or non-invasive therapeutic interventions [e.g., antibiotics, antivirals, Chinese patent medicine, vasoactive drugs, hormone therapy drugs, invasive or non-invasive ventilation, renal replacement therapy, extracorporeal membrane oxygenation (ECMO) therapy] and clinical outcomes [sepsis and septic shock, acute respiratory distress syndrome (ARDS), acute kidney injury (AKI), acute liver injury (ALI), acute myocardial injury (AMI), disseminated intravascular coagulation (DIC), ICU stay, clinical end point]. All identity information of patients was removed and recoded before data analysis. The database did not contain any patient identity or confidential information. Data were independently reviewed and confirmed by two experienced physicians to guarantee accuracy. When there was disagreement between the two examiners, a third physician was called in to give an opinion. Criteria definition is shown in Supplementary Table 4.
Statistics
Continuous variables were presented as the mean±SD for normally distributed continuous variables while median and interquartile range (IQR) for non-normally distributed continuous variables. For all categorical variables, binary dummy variables and percentage (%) were introduced to represent the categorical values. Continuous variables were studied using the T-Test or Mann-Whitney U-test. Associations between categorical dependent variables and independent categorical variables were evaluated using Pearson's chi squared test or Yates's correction for continuity analysis. A difference was considered significant if the two-side p-value was less than 0.05. Statistical analyses were carried out using SPSS Statistics v23.0 (IBM, Armonk, NY, USA) and the statistical analysis package R-3.6.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
The Association Between Prognosis of COVID-19 Patients With and Without Cancer
To determine the prognosis difference between COVID-19 patients with and without cancer, the study cohort included 7,926 COVID-19 patients admitted to 19 hospitals in Hubei, China. Of the 7,926 patients, 277 participants with cancer were defined as cancer group [median age 64 (IQR 56–70) years; 50.90% male] and the leaving 7,649 were defined as the non-cancer group [median age 55 (IQR 42–64) years; 48.19% male]. Patient characteristics and comorbidities at admission are shown in Table 1.
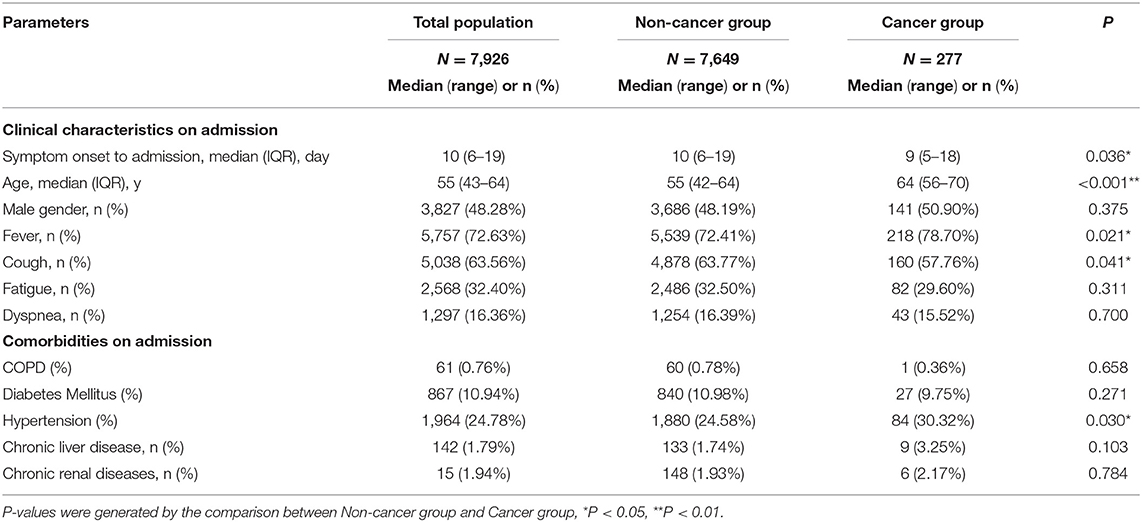
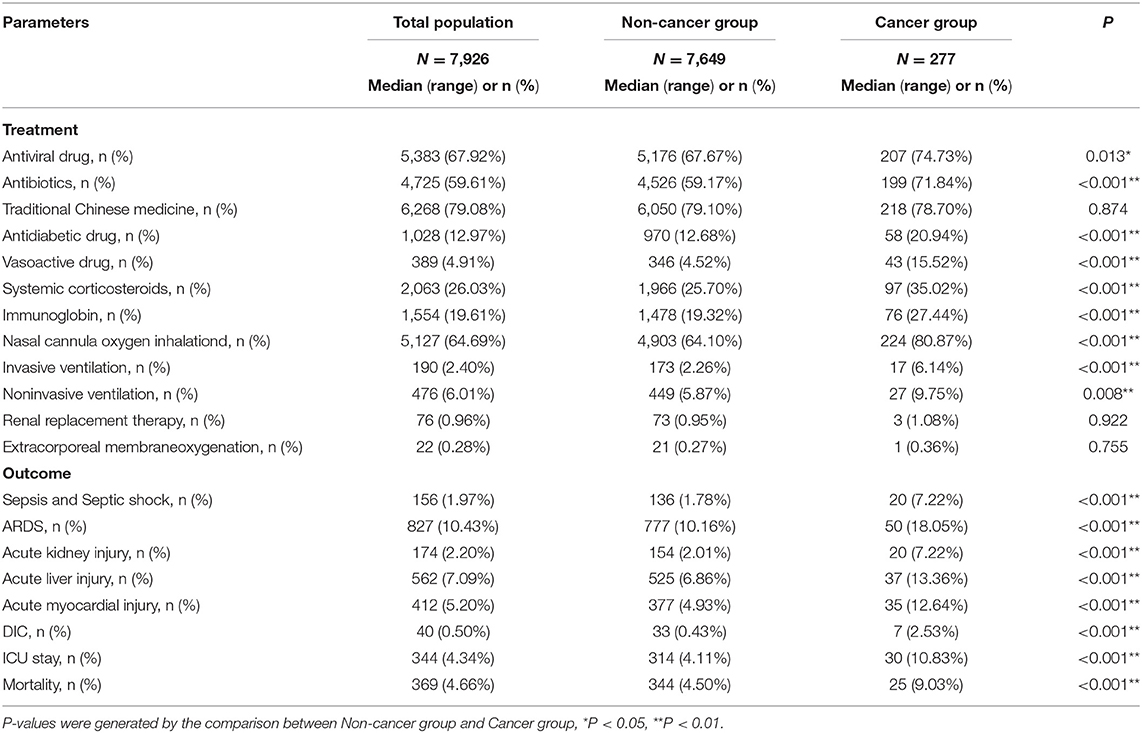
Table 1. Clinical characteristics and Comorbidities of patients with COVID-19 in Non-cancer group and cancer group on admission.
The cancer group was characterized by older age, lower prevalence of cough and higher prevalence of fever at presentation compared to the non-cancer group. Besides, the duration between onset and admission was shorter in the cancer group than in the non-cancer group [days, 9 (IQR 5–18) vs. 10(IQR 6–19); p = 0.036] (Table 1). The thoracic CT findings revealed higher prevalence of pulmonary infection lesions in cancer group compared to the non-cancer group (Supplementary Table 1). Laboratory examination on admission indicated increased liver enzymes (AST increase 22.02 vs. 14.77%, p < 0.001), kidney function abnormalities (CREA increase 10.83 vs. 5.43%, p < 0.001) and increased C-reactive protein (38.27 vs. 29.45%, p = 0.002) and procalcitonin level (27.80 vs. 16.16% p < 0.001) in the cancer group compared to the non-cancer group (Supplementary Table 1).
Regarding the inpatients medical treatment, compared to the non-cancer group, we found that patients in the cancer group suffered more from sepsis and septic shock (7.22 vs. 1.78%; p < 0.001), ARDS (18.05 vs. 10.16%; p < 0.001), AKI (7.22 vs. 2.01%; p < 0.001), ALI (13.36 vs. 6.86%; p < 0.001), AMI (12.64 vs. 4.93%, p < 0.001), DIC (2.53 vs. 0.43%, p < 0.001; Table 2). Moreover, the cancer group experienced more antiviral drugs (74.73 vs. 67.67%; p = 0.013), antibiotics (71.84 vs. 59.17%; p < 0.001), vasoactive drugs (15.52 vs. 4.52%; p < 0.001), hormone therapy drugs (35.02 vs. 25.70%, p < 0.001), ICU treatment (10.83 vs. 4.11%, p < 0.001), non-invasive ventilation (9.75 vs. 5.87%, p = 0.008) and invasive ventilation (6.14 vs. 2.26%, p < 0.001) compared to the non-cancer group (Table 2). Clinical end point showed a higher mortality rate in the cancer group than the non-cancer group (9.03 vs. 4.50%, p < 0.001; Table 2).
Prognosis of Cancer Patients Subjected and Not Subjected to Anti-Tumor Therapy in the Past 6 Months
A total of 277 COVID-19 cancer patients were enrolled in this subgroup study cohort. The cancer types of patients and num. of patients underwent anti-tumor treatment are displayed in Supplementary Table 3. We analyzed cancers of different sites, anti-tumor treatment in the past 6 months did not increase the mortality rate Supplementary Table 3. Of note, 74 patients underwent anti-tumor therapy in the past 6 months and were defined as anti-tumor therapy group [median age 65 (IQR 51–67) years; 45.95% male] whereas, the other 203 patients were classified as the non-anti-tumor therapy group [median age 63 (IQR 53–75) years; 49.75% male]. Patient characteristics at admission are highlighted in Table 3. Comparison of the general data (age, sex, onset to admission time, medical histories and underlying diseases, physical exam findings and clinical manifestation, radiologic report data) showed no statistical difference between the non-antitumor therapy group and antitumor therapy (p > 0.05; Table 3 and Supplementary Table 2).
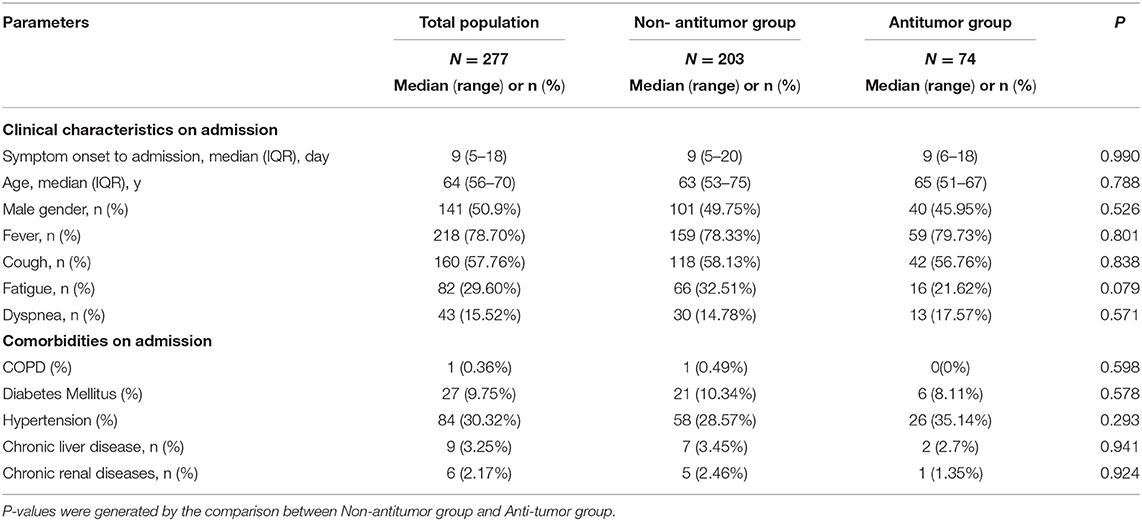
Table 3. Clinical characteristics and Comorbidities of cancer patients with COVID-19 in Non-antitumor group and Antitumor group on admission.
Regarding treatment, patients in the anti-tumor therapy group experienced a higher accuracy rate of ALI (21.62 vs. 10.34%; p = 0.015) compared to the non-anti-tumor therapy group. The accuracy rate of sepsis and septic shock, ARDS, AKI, AMI, and DIC were similar between the two groups. Treatments (antibiotics, antiviral drugs, Chinese patent medicine, vasoactive drugs, hormone therapy drugs, ICU treatment, non-invasive ventilation, invasive ventilation) had no statistical difference between the two groups (Table 4). Clinical end point showed no statistical difference in the mortality rate for the two groups (anti-tumor therapy group, 9.46% vs. non-anti-tumor therapy group, 8.87%, p = 0.879; Table 4).
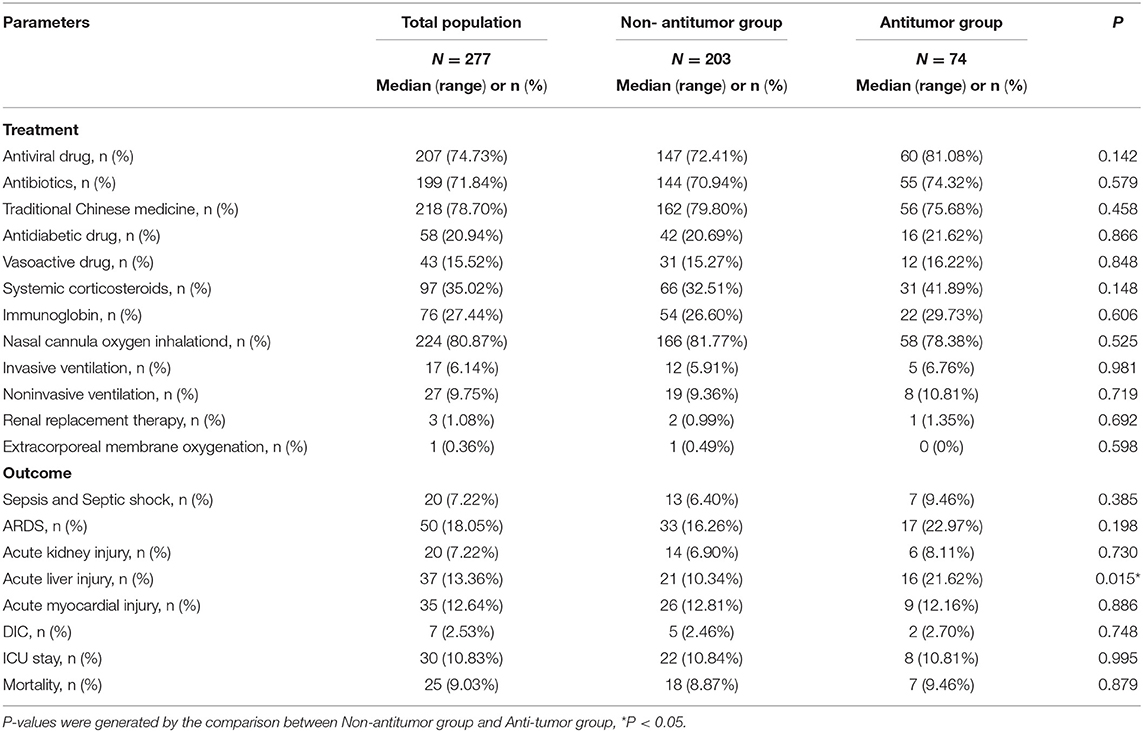
Table 4. Treatment and Outcome of patients with COVID-19 in Non-antitumor group and Antitumor group.
Discussion
In the present study, we reported a considerably high prevalence of COVID in tumor patients (277/7, 926, 3.49%). We speculate the reason is two-fold. First, tumor patients were highly exposed to the risk of virus infection, because they require more hospitalization or outpatient visits. Also, the immune homeostasis of the tumor patients was blunted (16, 17), especially those receiving chemotherapy, immunosuppressive therapy or molecular-targeted drug therapy, even those newly diagnosed patients have not been subjected to treatment or patients with best supportive care, their immune status were compromised (18).
Findings from this study indicated that cancer patients are characterized by older age, but lower prevalence of cough and higher prevalence of fever at onset stage. Of note, the duration between onset and admission was shorter in the cancer group than in the non-cancer group. This may be attributed to the blunted immune status in cancer patients. Previous studies have demonstrated that cancer patients have a higher risk of severe events (19). This study reported that the physiological severity of illness such as sepsis and septic shock, ARDS, AKI, ALI, AMI, and DIC occurred frequently in cancer patients. Besides, they also experienced more antiviral drugs, antibiotics, vasoactive drugs, hormone therapy drugs, ICU treatment, non-invasive ventilation and invasive ventilation. This indicates the health care providers more resources such as medications, medical supplies, modern equipments, employees were needed to allocate to the population. Even though, higher mortality occurred in the patients of cancer group. These findings remind us, to decrease the incidence of virus infection, phone communication or network consulting service must be considered by both physicians and patients as a way to improve care and follow-up and to reduce unnecessary visits to hospitals during the outbreak (20–22). Urgent and semi-urgent patients who require hospital treatment or check-up should do more protections to prevent nosocomial infection.
Several oncology societies have developed guidelines on cancer care during COVID-19 pandemic. However, there are some questions that remain open, including the risk of impairing the outcome when treatment stopped, continued, or modified for the patient's well-being and the “distraction effect” of the pandemic, which is represented by the risk of shifting total attention away from standard clinical care to COVID-19 only (23). ESMO, NICE and French guidelines suggested to use a tiered approach to categorize patients into different priority levels to receive active cancer therapy (24). This study reports that patients who underwent anti-tumor therapy in the past 6 month exhibited a higher accuracy rate of ALI. In the previse study, Yekedüz E reported chemotherapy increased the risk of death from COVID-19 in cancer patients, but there was no safety concern for immunotherapy, targeted therapies, surgery and radiotherapy (25). Song K demonstrated a possible association between recent receipt of oncologic treatment and a higher risk of death among patients with carcinoma who are hospitalized with COVID-19 (26). However, the findings of the current study do not support the previous research (19, 25). One unanticipated result was that the risk accuracy rate for severe events such as sepsis and septic shock, ARDS, AKI, AMI, and DIC were similar in the anti-tumor group compared with patients not subjected to anti-tumor therapy in the past 6 months. Interestingly, treatments of both populations experienced also had no statistical difference. Anti-tumor therapy (chemotherapy, radiotherapy, targeted therapy) in the past 6 months did not affect the mortality of cancer patients.
A note of caution is due here since a substantial proportion of patients who have longer disease courses may be clinically cured, or those new discovered patients incidentally during COVID-19 therapy may be mixed in the group not subjected to anti-tumor therapy. Even though, it is particularly encouraging to find that the patients who underwent antitumor treatments (chemotherapy, radiotherapy, targeted therapy) in the past 6-month still showed no worse outcome compared with the other group. The results of our study are similar to the results of the study conducted by Jee J et al. In their study, patients treated with cytotoxic chemotherapy did not have an increased risk of worse COVID-19 course (27). Interestingly, K Yang reported receiving chemotherapy within 4 weeks before symptom onset, and male sex were risk factors for death during admission to hospital (8). However, the effect of treatment on its postponement of cancer patients cannot be ignored (28, 29), the diagnostic or treatments' delays would result in life-years lost. We proposed that streamlined efficient anti-tumor treatment should not be affected or cancelled. Originally prescribed antitumor regimens are recommended when sufficient resources and standard precautions can be ensured.
However,there are still some limitations in our study and we have a lot of works to do in the future. First, patients enrolled were infected with early variants of the virus during the time frame of the first outbreak. The effect to cancer patients might change accompanied by viral mutations. Subsequent variants which might potentially result to a slightly different patient presentation. Second, our main aim was to check whether anti-tumor therapy in the past 6 months could worsen the prognosis of cancer patients with COVID-19. Treatment and outcome of different types of cancer with COVID-19 in non-antitumor group and antitumor group were illustrated. However, the older age for the cancer group might be biased by the types of cancer detected, especially as older patients might have a greater proportion of comorbidities. Limitations in sample size have hampered a more stratified analysis to reduce the effect of selection bias. In addition, we only conducted analysis and research in cohorts in Hubei, China. For patients in other regions, the conclusions we observed may be subject to geographic influences, including local medical conditions, economic levels, and government policies.
Although the current study enrolled limited patients, the findings confirmed the vulnerability of cancer patients with the SARS-CoV-2 (30). Moreover, we suggest that tumor patients should be considered as a special population because they are more susceptible to infection with SARS-CoV-2 due to immune change and social medical need, Antitumor treatments do not expose tumor patients to more risk of severe complications or higher mortality when they have SARS-CoV-2 infection. The antitumor treatments for tumor patients during pandemic should be recommended cautiously.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors. Meanwhile, the proposal with detailed aims, statistical plan, and other information/materials may be required and investigated by the 19 hospitals to guarantee the rationality of requirement and the security of the data.
Ethics Statement
The studies involving human participants were reviewed and approved by Central Ethics Committees and Institutional Ethics Committees in Zhongnan Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
HW and YY: conception and design and acquisition of data (acquired and managed patients, provided facilities, etc.). DG and HW: development of methodology. DG, HW, and QZ: analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis), writing, review, and revision of the manuscript. DG and YY: administrative, technical, and material support (i.e., reporting or organizing data, constructing databases). YY: study supervision. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by a grant from the National Key Research and Development Program of China (2020YFC0845500 to YY), Zhongnan Hospital of Wuhan University Science, Technology and Innovation Seed Fund (CXPY2020015) and Cancer research and translational platform project of Zhongnan Hospital of Wuhan University (ZLYNXM202004).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
During the stage of data acquisition and ethical supervision in each center, we want to acknowledge the help from Juan-Juan Qin, MD (Institute of Model Animal of Wuhan University), Pengcheng Luo, MD (Wuhan Third Hospital & Tongren Hospital of Wuhan University), Shouzhi Fu, MD (Wuhan Third Hospital & Tongren Hospital of Wuhan University), Mingyu Liu, MD (Wuhan Ninth Hospital), Ping Ye, MD (The Central Hospital of Wuhan), Bing Xiao, MD (Xiantao First People's Hospital), Weiming Mao, MD (Huanggang Central Hospital), Liming Liu, MD (Ezhou Central Hospital), Youqin Yan, MD (Wuhan Seventh Hospital), Xiaofeng Liao, MD (Xiangyang Central Hospital), Guohua Chen, MD (Wuhan No.1 Hospital/Wuhan Hospital of Traditional Chinese and Western Medicine), Daihong Wang, MD (Xianning Central Hospital), Gang Peng, MD (Suizhou Central Hospital), Xigang Xia, MD (Jingzhou Central Hospital), Jun Hu, MD (Yichang Central Hospital), Junhai Wang, MD (Jingmen First People's Hospital), Haofeng Lu, MD (Jingzhou First People's Hospital), Zixiong Zhang, MD (Central Hospital of Enshi Tujia and Miao Autonomous Prefecture), Hongliang Li, MD, Ph.D. (Renmin Hospital of Wuhan University, Institute of Model Animal of Wuhan University). In the data analysis stage, we want to acknowledge the help from Juan-Juan Qin, MD (Institute of Model Animal of Wuhan University) and Hongliang Li, MD, Ph.D. (Renmin Hospital of Wuhan University, Institute of Model Animal of Wuhan University).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.614057/full#supplementary-material
Abbreviations
AIDS, acquired immune deficiency syndrome; AKI, acute kidney injury; ALI, acute liver injury; ALP, alkaline phosphatase; ALT, alanine aminotransferase; AMI, acute myocardial injury; ARDS, acute respiratory distress syndrome; AST, aspartate aminotransferase; CI, confidence interval; COPD, chronic obstructive pulmonary disease; CoV-2, coronavirus 2; COVID-19, coronavirus disease 2019; CRP, C-reactive protein; CT, computed tomography; DIC, disseminated intravascular coagulation; ECMO, extracorporeal membrane oxygenation; IQR, interquartile range; PCT, procalcitonin; SARS, severe acute respiratory syndrome; TBIL, total bilirubin; ULN, upper limit of normal.
References
1. WHO report on Coronavirus disease (COVID-19) Pandemic. Available online at: https://covid19.who.int/ (2021).
2. Tang W, Cao Z, Han M, Wang Z, Chen J, Sun W, et al. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial. BMJ. (2020) 369:m1849. doi: 10.1136/bmj.m1849
3. Knight SR, Ho A, Pius R, Buchan I, Carson G, Drake TM, et al. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ. (2020) 370:m3339. doi: 10.1136/bmj.m3339
4. Hao X, Cheng S, Wu D, Wu T, Lin X, Wang C. Reconstruction of the full transmission dynamics of COVID-19 in Wuhan. Nature. (2020) 584:420–4. doi: 10.1038/s41586-020-2554-8
5. Clift AK, Coupland CAC, Keogh RH, Diaz-Ordaz K, Williamson E, Harrison EM, et al. Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study. BMJ. (2020) 371:m3731. doi: 10.1136/bmj.m3731
6. Argenziano MG, Bruce SL, Slater CL, Tiao JR, Baldwin MR, Barr RG, et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ. (2020) 369:m1996. doi: 10.1136/bmj.m1996
7. Adam DC, Wu P, Wong JY, Lau EHY, Tsang TK, Cauchemez S, et al. Clustering and superspreading potential of SARS-CoV-2 infections in Hong Kong. Nat Med. (2020) 26:1714–9. doi: 10.1038/s41591-020-1092-0
8. Yang K, Sheng Y, Huang C, Jin Y, Xiong N, Jiang K, et al. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study. Lancet Oncol. (2020) 21:904–13. doi: 10.1016/S1470-2045(20)30310-7
9. Kuderer NM, Choueiri TK, Shah DP, Shyr Y, Rubinstein SM, Rivera DR, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. (2020) 395:1907–18.
10. Yu J, Ouyang W, Chua MLK, Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. (2020) 6:1108–10. doi: 10.1001/jamaoncol.2020.0980
11. Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R, et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. (2020) 31:894–901. doi: 10.1016/j.annonc.2020.03.296
12. The Lancet O. COVID-19: global consequences for oncology. Lancet Oncol. (2020) 21:467. doi: 10.1016/S1470-2045(20)30175-3
13. Announcement of New Coronavirus Pneumonia Prevention and Control Headquarters of Hubei. Available online at: http://www.gov.cn/xinwen/2020-01/24/content_5471995.htm (2020).
14. China NHC. New Coronavirus Pneumonia Prevention and Control Program. Available online at: http://www.nhc.gov.cn: National Health Commission of China (2020).
15. World Health Organization. Laboratory Testing for 2019 Novel Coronavirus (2019-nCoV) in Suspected Human Cases Interim Guidance. World Health Organization (2020). Available online at: http://apps.who.int/iris/handle/10665/331329
16. Burugu S, Dancsok AR, Nielsen TO. Emerging targets in cancer immunotherapy. Semin Cancer Biol. (2018) 52(Pt 2):39–52. doi: 10.1016/j.semcancer.2017.10.001
17. Schreiber RD, Old LJ, Smyth MJ. Cancer immunoediting: integrating immunity's roles in cancer suppression and promotion. Science. (2011) 331:1565–70. doi: 10.1126/science.1203486
18. Merli M, Perricone G, Lauterio A, Prosperi M, Travi G, Roselli E, et al. Coronaviruses and immunosuppressed patients: the facts during the third epidemic. Liver Transpl. (2020) 26:1543–4. doi: 10.1002/lt.25806
19. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. (2020) 21:335–7. doi: 10.1016/S1470-2045(20)30096-6
20. Burki TK. Cancer guidelines during the COVID-19 pandemic. Lancet Oncol. (2020) 21:629–30. doi: 10.1016/S1470-2045(20)30217-5
21. Jazieh AR, Kozlakidis Z. Healthcare transformation in the post-coronavirus pandemic era. Front Med (Lausanne). (2020) 7:429. doi: 10.3389/fmed.2020.00429
22. Kronenfeld JP, Penedo FJ. Novel Coronavirus (COVID-19): telemedicine and remote care delivery in a time of medical crisis, implementation, and challenges. Transl Behav Med. (2021) 11:659–63. doi: 10.1093/tbm/ibaa105
23. Cortiula F, Pettke A, Bartoletti M, Puglisi F, Helleday T. Managing COVID-19 in the oncology clinic and avoiding the distraction effect. Ann Oncol. (2020) 31:553–5. doi: 10.1016/j.annonc.2020.03.286
24. Tartarone A, Lerose R. COVID-19 and cancer care: what do international guidelines say? Med Oncol. (2020) 37:80. doi: 10.1007/s12032-020-01406-5
25. Yekeduz E, Utkan G, Urun Y. A systematic review and meta-analysis: the effect of active cancer treatment on severity of COVID-19. Eur J Cancer. (2020) 141:92–104. doi: 10.1016/j.ejca.2020.09.028
26. Song K, Gong H, Xu B, Dong X, Li L, Hu W, et al. Association between recent oncologic treatment and mortality among patients with carcinoma who are hospitalized with COVID-19: a multicenter study. Cancer. (2020) 127:437–448. doi: 10.1002/cncr.33240
27. Jee J, Foote MB, Lumish M, Stonestrom AJ, Wills B, Narendra V, et al. Chemotherapy and COVID-19 outcomes in patients with cancer. J Clin Oncol. (2020) 38:3538–46. doi: 10.1200/JCO.20.01307
28. Sud A, Torr B, Jones ME, Broggio J, Scott S, Loveday C, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. (2020) 21:1035–44. doi: 10.1016/S1470-2045(20)30392-2
29. Hartman HE, Sun Y, Devasia TP, Chase EC, Jairath NK, Dess RT, et al. Integrated survival estimates for cancer treatment delay among adults with cancer during the COVID-19 pandemic. JAMA Oncol. (2020) 6:1881–9. doi: 10.1001/jamaoncol.2020.5403
Keywords: COVID-19, SARS-CoV-2, pneumonia, cancer, antitumor therapy
Citation: Guo D, Wang H, Zhu Q and Yuan Y (2021) Clinical Characteristics of Cancer Patients With COVID-19: A Retrospective Multicentric Study in 19 Hospitals Within Hubei, China. Front. Med. 8:614057. doi: 10.3389/fmed.2021.614057
Received: 05 October 2020; Accepted: 27 August 2021;
Published: 05 October 2021.
Edited by:
Zisis Kozlakidis, International Agency for Research on Cancer (IARC), FranceReviewed by:
Annalisa Trama, Istituto Nazionale dei Tumori (IRCCS), ItalyChar Leung, The University of Hong Kong, Hong Kong, SAR China
Copyright © 2021 Guo, Wang, Zhu and Yuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yufeng Yuan, eXVhbnlmMTk3MUB3aHUuZWR1LmNu
†These authors have contributed equally to this work
 Deliang Guo
Deliang Guo Haitao Wang†
Haitao Wang† Qian Zhu
Qian Zhu Yufeng Yuan
Yufeng Yuan