- 1Department of Medicine, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, United States
- 2Divisions of Critical Care Medicine and Pulmonary Medicine, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, United States
- 3Division of Infectious Diseases, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, United States
- 4Division of Hospital Medicine, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, United States
- 5Division of Rheumatology, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, United States
- 6Division of General Internal Medicine, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, United States
- 7Division of Allergy and Immunology, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, United States
- 8Division of Endocrinology, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, United States
The first Covid-19 patient was admitted to Montefiore Medical Center (MMC) on March 10, 2020. Soon thereafter there was a rapid and exponential surge of Covid-19 admissions to MMC that could have resulted in catastrophic consequences if MMC had been overwhelmed, as happened in Europe. To adjust to this crisis our institution, under the inspiring leadership of Dr. Philip Ozuah, President and CEO of Montefiore Medicine, adopted an “all hands on deck” approach, mobilizing our entire workforce to expand our units to accommodate the growing number of patients being admitted. Given that the internal medicine (IM) and ICU units are part of the department of medicine (DOM), the DOM was at the center of this mobilization. The DOM is the largest department at MMC and mobilizing it required careful planning, seamless teamwork, and strong leadership. To achieve that goal, we applied a framework that we designate the “3C framework,” denoting Coordination, Communication, and Collaboration. In this report we describe the many initiatives the Montefiore Einstein DOM implemented during the Covid-19 pandemic using the 3C framework. These included establishing the Medicine Covid-19 Taskforce to lead our efforts, starting a daily newsletter for up-to-date communications, rapidly expanding the ICU and IM units, converting most specialty inpatient consults to eConsults, coordinating research studies, and more. The goal of this report is to serve as a guide on how the 3C framework helped us organize, mobilize, and energize the department of medicine effectively and efficiently during this unprecedented crisis.
Introduction
The first Covid-19 patient was admitted to the Montefiore Medical Center (MMC) intensive care unit (ICU) on March 10, 2020. Within 2 weeks, 345 Covid-19 patients were hospitalized at MMC (comprising 4 hospitals, Montefiore, Weiler, Children's Hospital, and Wakefield). As the rapid surge of Covid-19 admissions to MMC accelerated, predictive models were used to estimate the number of patients likely to be admitted in the coming days, and they all painted a grim picture. Three models (Montefiore Einstein Department of Epidemiology and Population Health model, New York City (NYC) Department of Health model, and Susceptible, Exposed, Infected, Resistant [SEIR] model) predicted that Montefiore would be overwhelmed with Covid-19 patients by early April, even after expanding bed capacity to its limits (Figure 1). This outcome could have resulted in catastrophic consequences, like the flooding of hospitals that was seen in Italy just a few weeks earlier (1, 2), where hospitals exhausted resources and personnel needed to care for the patients. To prevent this bioethical nightmare scenario (3) our institution, adopted an “all hands on deck” approach, mobilizing our entire workforce to expand our units to accommodate the growing number of patients being admitted. Given that the medical and ICU units are part of the department of medicine (DOM), the DOM was at the center of this mobilization.
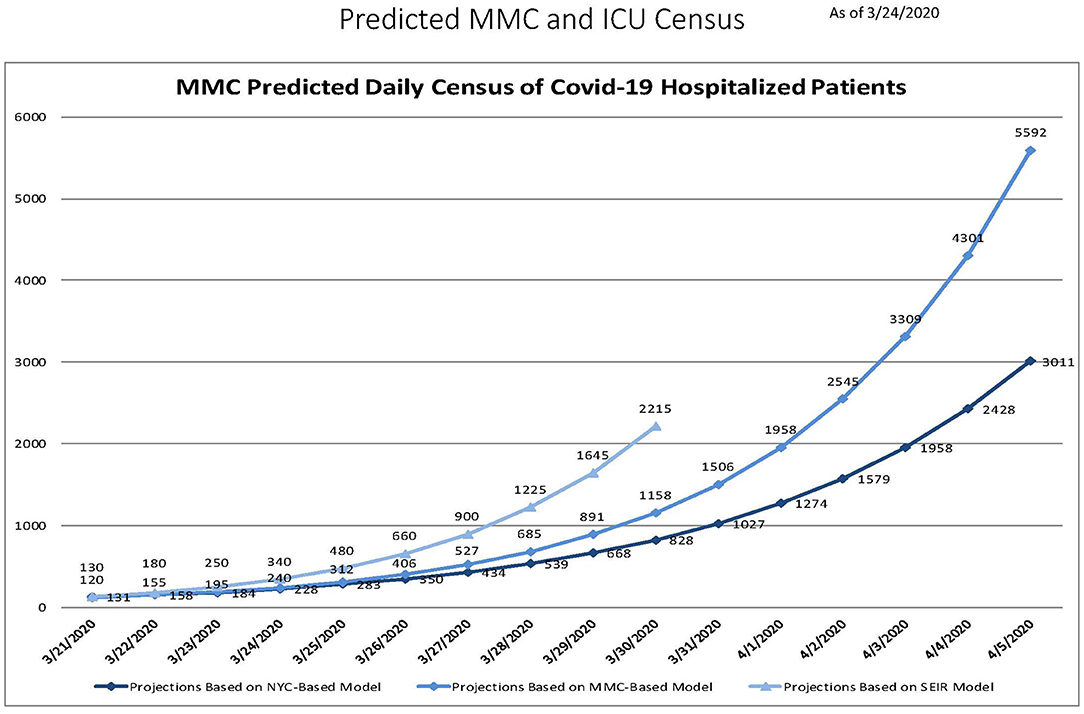
Figure 1. Three predictive models generated on March 24, 2020 showing the expected exponential increase in daily Montefiore Medical Center census over the following 2 weeks.
With 15 divisions the Montefiore Einstein DOM is the largest department in our institution and mobilizing such a large department required careful planning, seamless teamwork, and strong leadership. To achieve that goal, we applied a framework for our efforts and initiatives during the crisis that we designate the “3C framework”, an abbreviation for Coordination, Communication, and Collaboration (Figure 2). In this report we describe the many initiatives the Montefiore Einstein DOM implemented during the Covid-19 pandemic using the 3C framework. For a summary of our initiatives within the 3C framework see Table 1. The goal of our report is not to summarize the MMC Department of Medicine's experience during Covid-19 (such a summary would be beyond the scope of this manuscript), but to serve as a guide on how the 3C framework helped us organize, mobilize, and energize the department of medicine effectively and efficiently during this unprecedented crisis.
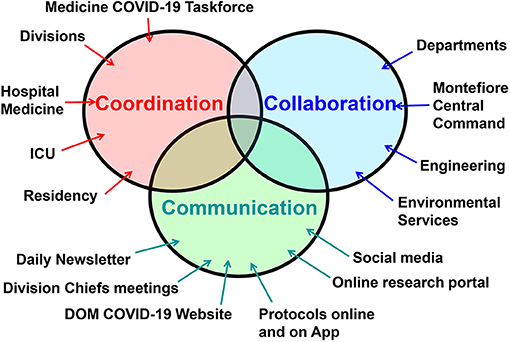
Figure 2. The 3C framework consists of three elements: coordination between the department of medicine (DOM) divisions, ICU, Covid-19 units, residency training program, as well as other arms of the DOM. This was led by the Medicine Covid-19 Taskforce; Communication between all arms of the DOM was achieved via a daily newsletter, division chiefs meetings, online resources, and even social media; Collaboration with all arms of the institution, especially with Montefiore Medical Center administration and central command, was essential to ensure synergy and uniformity of efforts within the entire institution.
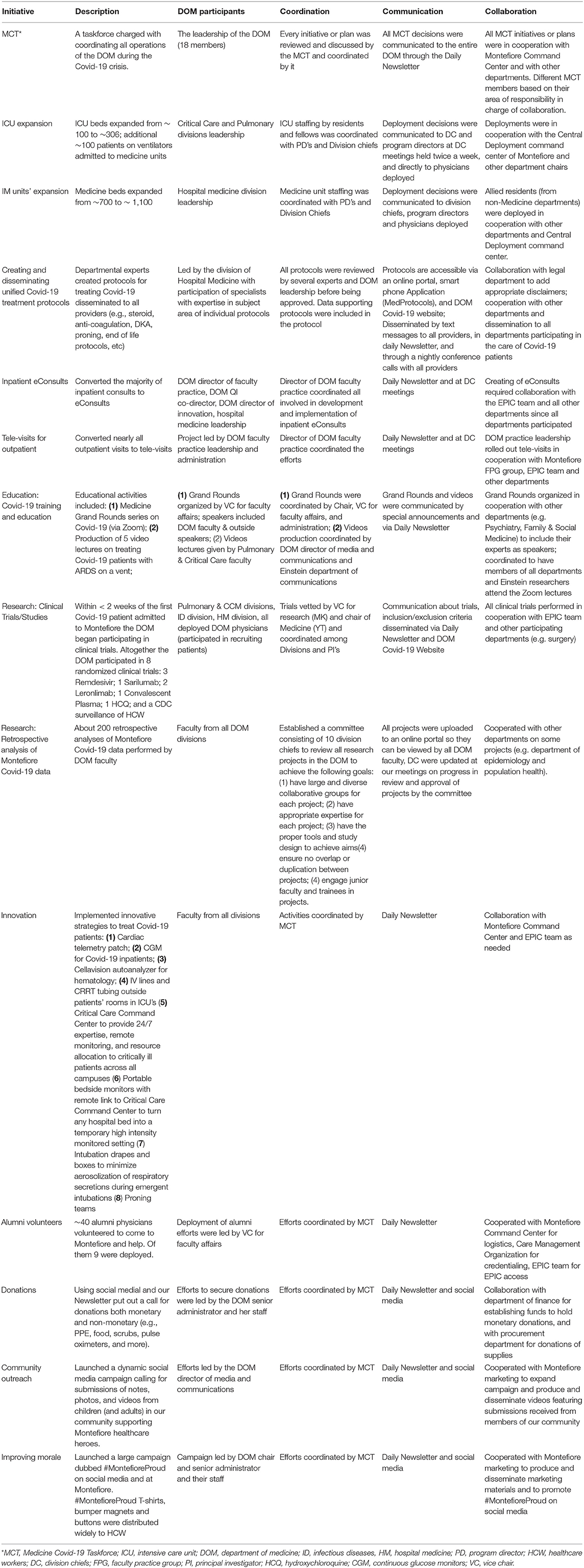
Table 1. List of Department of Medicine (DOM)-led initiatives in which the 3C framework was implemented.
Background: The Department of Medicine at Montefiore Medical Center
The MHS includes 11 hospitals located in the Bronx, Westchester County, and the Hudson Valley in New York State. MMC comprises four MHS hospitals located in the Bronx and includes the Montefiore Hospital, Weiler Hospital, Children's Hospital at Montefiore, and Wakefield Hospital, which together have approximately 1,500 beds including 108 intensive care unit (ICU) and 30 intermediate care unit beds, 93,000 annual admissions, and more than 200 outpatient care sites. The current manuscript focuses on the implementation of the 3C framework by the DOM at the MMC.
The DOM is the largest department at MMC and includes 25 inpatient units, 3 medical and cardiac ICUs, and 754 beds, with approximately 47,000 discharges per year. The DOM comprises 15 divisions and has 1,293 providers (of them > 800 full time faculty). The DOM trains 429 residents and fellows in 3 residencies (Moses-Weiler IM residency training 168 residents, Wakefield IM residency training 77 residents, and Dermatology residency training 19 residents) and 15 fellowships (training a total of 165 fellows). Of note the Critical Care Division includes all 7 ICU's and 2 step-down units including the surgical ICU's.
The DOM is also the largest research department at Einstein and Montefiore with approximately $96 million in total grant money received, 150 grants, and 140 ongoing clinical trials (pre-Covid-19) in 2019.
The Challenges Faced by the MMC Department of Medicine
Challenges faced by the Department of Medicine included: the need to rapidly deploy physician staffing to care for a rapidly expanding inpatient census, provide support for physicians newly deployed to the inpatient setting as well as non-IM physicians who were deployed, stay abreast of the rapidly expanding body of research on Covid-19 to develop and continuously update standardized care protocols, develop processes for the triage and appropriate care of patients being placed in expanded ICUs and non-traditional care spaces, develop and rapidly initiate Covid-19-related research, maintain real-time communication with all providers, and offer emotional and logistical support to physicians and physician assistants (PAs) who were delivering care in extremely challenging and distressing conditions. Residents were the primary providers of inpatient care during the epidemic. In addition to postponing their usual educational activities, all residents were also exposed to the unpredictability and grief associated with caring for Covid-19 patients, during a formative period in their careers.
Coordination, Communication, and Collaboration
Medicine Covid-19 Taskforce: The Key to Coordinating the DOM Efforts
To coordinate the deployment and activities of such a large workforce we established a unique task force to centralize and synchronize all DOM activities during the Covid-19 crisis. This task force, the Medicine Covid-19 Taskforce (MCT), was charged with seamless coordination and implementation of all initiatives and operations of the DOM. The MCT included 18 members representing all arms of the DOM (Table 2), and it convened every morning through a conference call. During these structured conference calls, every DOM leader and member of the MCT gave a detailed report updating all members on activities, challenges, and plans within their domain. At the end of each presentation we discussed what coordination and synchronization of efforts and resources were needed to achieve our goals and implement our plans and how to communicate these to the entire department. The most important coordination of efforts involved deployment of faculty and trainees. The regular updates and discussions at the MCT ensured that all new ICU and medicine units that were being built and opened overnight were always properly staffed with attendings and trainees.
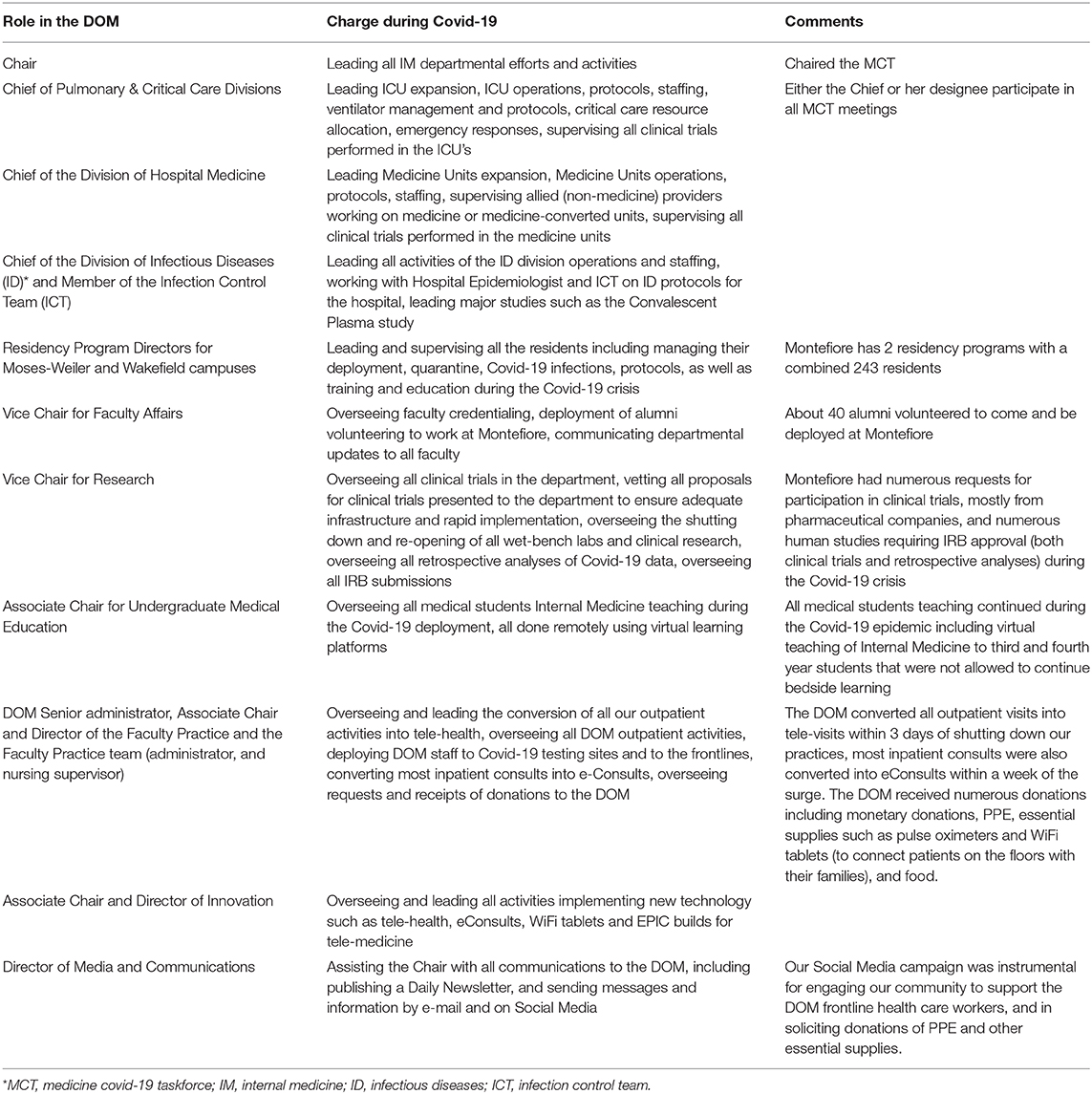
Table 2. Members of the medicine covid-19 taskforce and their roles in coordinating DOM efforts and initiatives.
Another example in which coordination was important was the development and dissemination of Covid-19 treatment protocols. We were able not only to ensure that all Covid-19 patients admitted to MMC were treated consistently, but also to implement new protocols very rapidly and in many cases much earlier than at other Medical Centers. Moreover, our uniform protocols allowed us to study in real time the impact of our treatment protocols on outcomes. As an example, analysis of Montefiore patient data showed that treatment with steroids was associated with reduced mortality only when the C-reactive protein (CRP) levels were >20 mg/dl, but when CRP was lower than 10 mg/dL steroid treatment was associated with increased mortality (4). This study that was performed in real time contributed to a modification of the protocol to incorporate these new data.
Our coordinated efforts through the MCT enabled us to coordinate many other initiatives. To name a few: (1) The production of critical educational video lectures to train physicians not usually working in the ICU setting; (2) Solicitation, receipt, and distribution of donated personal protective equipment (PPE), and other essential supplies such as pulse oximeters and electronic tablets; (3) Teaching of the medical students; (4) Continuation of essential procedures; (5) Conversion of most activities to telehealth and more.
The key to the 3C framework success was that it operated at all levels of the DOM, not only at the leadership level, that is, within the divisions, as well as at each Covid-19 unit. To facilitate the implementation of the 3C framework within the divisions, the MCT met with all division chiefs twice a week to update them on DOM deployment and other efforts. This ensured that all departmental and divisional efforts were coordinated, that there was no duplication of efforts, and, most importantly, that every issue was immediately addressed in real time. Division Chiefs then held conference calls with their faculty coordinating and communicating with them and receiving communication from their faculty and feedback that was then communicated back to the MCT. To ensure that the 3C framework reached the individual Covid-19 units the chiefs of the Critical Care (MNG) and Hospital Medicine (WS) divisions held regular virtual meetings with the attendings in the ICU's and Covid-19 IM units. Thus, the 3C framework was successful because it was delegated from the DOM leadership to Divisional leadership and to attending physicians at the Covid-19 unit level, and because it was bi-directional.
The chair of medicine (YT) and chiefs of Critical Care Medicine (MNG) and Hospital Medicine (WS) also held regular meetings with hospital administration, nursing leadership, and other departments to ensure seamless collaboration.
The DOM Covid-19 Daily Newsletter: The Key to our Communication
Transparency is essential for ensuring that members of the department have full trust in departmental leadership and are willing to do whatever is requested of them. This is especially true in times of crisis. Early on the decision was made that with very few exceptions everyone in the department would know what the leadership knew. Therefore, we created a DOM Covid-19 Daily Update, an electronic newsletter that was sent to all members of the department which updated them on everything that was happening—from our hospital Covid-19 statistics, to new protocols, to new relevant publications, and even to discounts by companies to healthcare workers. To ensure that the content was relevant we monitored the number of views of different items and focused on popular items. In addition, we gave the readers an e-mail address to offer suggestions, provide comments, or ask questions. The newsletter was highly successful; it was distributed to > 6,500 people with a daily open rate of up to 65%.
ICU Expansion
During the Covid-19 crisis our ICU beds at MMC expanded from about 100 ICU beds to 306. This rapid expansion necessitated coordination of deployment between the ICU leadership, residency directors, division chiefs, other departments, and the Montefiore Command Center (which oversaw all ICU deployments). Critical Care not only expanded its ICU bed capacity but also responded to cardiac arrests and rapid emergency calls that increased 5-fold (from an average of 7–8 per day pre-Covid-19 to 33 per day). The Chief of the Critical Care Division (MNG) led and supervised the ICU expansion. The expansion followed specific steps that included: (1) Identification of suitable space for an ICU that had enough room for patients in isolation, on ventilators, and with bedside monitoring (e.g., OR recovery unit); (2) Coordination with engineering to convert each unit into an ICU, including construction, terminal cleaning, and procuring equipment, especially ventilators; (3) Coordination with DOM leadership as well as other department leaders to organize deployment of faculty to the new units; (4) Coordination with the program directors and Montefiore Command Center to organize deployment of residents and fellows to the new units; (5) Coordination with nursing for the deployment of nurses to the new units; (6) Communication to the Emergency Department, Hospital Medicine division, and all providers about the establishment of a new ICU and which patients could be admitted or transferred to the new ICU; (7) Development of a Critical Care Command Center to provide 24/7 critical care expertise, remote monitoring of expanded ICU's, deployment of emergency personnel and equipment, point of care ultrasounds, and coordination of transfers of patients, resources and personnel between ICUs and between MMC campuses, and from outside hospitals; (8) Development of protocols and procedures for emergency responses like intubation and cardiopulmonary resuscitation to minimize aerosolization and infection risk during the pandemic; (9) Development of infection control measures in coordination with respiratory therapy and hospital epidemiology for high risk respiratory procedures in the hospital.
Expansion of Internal Medicine Units
At the same time as the ICU's were expanding the Internal Medicine (IM) general units were rapidly expanding, too, from approximately 700 beds to ~ 1,100 beds. To achieve this, space for the increased number of patients needed to be identified, and increased physician staffing needed to be mobilized. To provide the needed space, the Covid/Medicine service first expanded into virtually all inpatient spaces that do not traditionally accommodate Medicine patients including Neurology, Oncology and Surgical inpatient units. Next, many non-clinical spaces were rapidly renovated to accommodate inpatients including a large meeting space, unit day rooms, a cafeteria, and rehab gymnasiums. Finally, a large free-standing outpatient surgical center was converted into inpatient units. To provide physician staffing for the expanded service the DOM rapidly constructed novel 3-person inpatient care teams consisting of a Medicine attending, a Medicine resident and an “allied” (non-Medicine) resident. These teams could be constructed and deployed within 24 h of notification of a new staffing need. In addition, several non-Medicine services took over the care of Covid-19 patients including Neurology, Oncology and Pediatrics, and Family Medicine significantly increased their inpatient capacity.
In order to achieve this enormous expansion in a coordinated and organized way the Chief of the Division of Hospital Medicine (WS) implemented several key measures: (1) Leadership – with the exponential growth of the general medicine units a new divisional leadership structure was created appointing faculty to new leadership positions, such as director of the IM units at our outpatient facility; (2) Standards of care – Divisional leadership in consultation with specialists in different areas such as diabetes and coagulopathies, created uniform protocols for the treatment of Covid-19 patients, including an EPIC Covid-19 admission order set and note template; (3) Mentoring – several non-IM units (e.g., pediatrics, neurology) were converted into IM Covid-19 units that were staffed by the original department. Since the providers on these units did not have experience in adult hospital medicine and Covid-19 the Hospital Medicine division provided mentors that came daily and rounded with the providers on these units to help manage their service; (4) Triaging – the Division of Hospital Medicine developed criteria for transferring patients from acute Covid-19 units to post- acute areas (non-clinical areas converted into Covid-19 units). (5) Deployment of physician assistants (PAs) – PAs were essential on the IM Covid-19 units that did not have residents and the PA leadership at the Hospital Medicine division managed their deployment and training to take on new roles such as being on the code team.
Medicine Sub-specialty Inpatient Consults
The inpatient subspecialty consultation services had to resolve two main challenges: (1) Most consultants were deployed to ICU's or IM Covid-19 units and could not do inpatient consults; and (2) PPE was in short supply and consultants coming to do in-person consults would use a large amount of PPE. To resolve both issues the MCT initiated an eConsult service for all inpatient consultations except for a few that required procedures (Table 1).
Covid-19 Treatment Protocols and Education
One of the challenges our expansion created was that numerous providers with limited ICU or IM experience were deployed to ICU's and IM Covid-19 units. In order to ensure that they could perform their new roles well, we implemented two important initiatives: development and dissemination of detailed and uniform Covid-19 treatment protocols, and production and dissemination of educational Covid-19 video lectures. The Covid-19 treatment protocols were developed by experts in their fields together with the Hospital Medicine Division leadership and were based on the best available data. This approach resulted in very early adoption at Montefiore of life-saving Covid-19 protocols. To mention a few, the Montefiore steroid treatment protocol was rolled out and uniformly implemented on April 6 (4); our anti-coagulation protocol was rolled out on April 5; and the Montefiore subcutaneous (SQ) insulin diabetic ketoacidosis (DKA) protocol was rolled out on April 1. Some of these protocols were disseminated across the country (e.g., our DKA protocol was posted on the American Diabetes Association website and published in UpToDate) (5).
These protocols were easily accessible through an online portal and later through a free downloadable mobile application (MedProtocols, see below). In addition to making the protocols easily accessible from anywhere, any new protocols or modifications to existing protocols were communicated to every provider on the IM units through our daily newsletter, text messaging, and nightly briefs with the Chief of the division of Hospital Medicine. In addition, we converted our weekly Medicine Grand rounds to a virtual format, and held a special Covid-19 series that focused on Internal Medicine subspecialty manifestations of Covid-19.
Outpatient Deployment and Conversion to Telemedicine
Within 10 days of the first Covid-19 patient being admitted to MMC all but one outpatient practice were closed and many of their staff and providers deployed to Covid-19 units. However, MMC was able to continue most outpatient operations through a rapid conversion to telemedicine. The DOM implemented video visit platforms, and patients were called and instructed that their appointments would be done remotely. One of the challenges we faced in the Bronx was that many patients did not have the ability to do video visits (e.g., they did not have WiFi at home) and therefore only telephone visits were possible for them. The conversion of our outpatient practices to televisits required coordination and collaboration with the Faculty Practice Group, our call center, our Electronic Medical Record team, and our billing services in order to support billing for televisits. To ensure a smooth transition to televisits a DOM team trained and helped providers performing televisits.
Covid-19 Post-discharge Televisit Program
As large numbers of recovering Covid-19 patients began to be discharged home from Montefiore IM units, there was a need for follow-up care. Therefore, the DOM established a post-discharge follow-up program. Since most of our physicians were deployed we enlisted third year medical students to help with the program which included follow-up phone calls/video visits by physicians or medical students to address the following: (1) Ensure that patients were recovering; (2) For patients discharged home with pulse oximeters the oxygen saturation readings were evaluated; (3) If patients needed follow-up care with specialists, appointments were coordinated and scheduled; (4) Patients with financial and socio-economic challenges were assigned a care coordinator from the Montefiore Care Management Organization (the Montefiore accountable care organization) who contacted them to assist. These activities were coordinated with the Montefiore Primary Care group.
Infection Control and Prevention
Infection control procedures implemented at our institution included universal masking of patients and health care workers (6), appropriate PPE usage when caring for COVID-19 patients, conversion of in-person consults to telemedicine, universal PCR testing upon admission to the hospital, environmental disinfection, and education of staff via weekly lectures and the DOM newsletter. When we identified a suspected exposure, we activated an infection control team that performed the contact tracing and implemented isolation and quarantine measures (7). However, the DOM's infection control practices evolved over time in several ways: iterative approaches to PPE distribution were employed until all providers had easy access, and the infection control protocols were adjusted following changes in the CDC recommendations. To implement and disseminate these frequent protocol changes we used our 3C approach by coordinating the implementation of these changes through the MCT and communicating these changes to all providers through our various communication methods (see above). As a result of these efforts, resident sick calls returned to pre-COVID levels within weeks despite an ongoing rise in the number of COVID-19 patients hospitalized at our institution (8).
Mental Health Support
To address the stress and anxiety that the COVID-19 pandemic induced in healthcare workers the Psychiatry Department at Montefiore established several interventions. These included a support phone line, staff support centers, team support sessions, and more. For a review of these interventions see (9). An additional unique resource - the Montefiore Emotional Support Allies (MESA) – was also established, in which health care workers were individually assigned to a mental health professional (psychologist, psychiatrist, or social worker) who actively reached out to them and offered to help. The mental health professionals provided peer support and served as navigators to other emotional health resources. About 20% of those contacted opted for one or more peer support contacts; many finding them meaningfully helpful (Alpert, personal communication).”
Coordination of Research Studies
From the onset of the epidemic in NYC, clinical and laboratory investigator-initiated research studies aimed to better our understanding of Covid-19 and to improve the care of Covid-19 patients.
Clinical Trials
Performing clinical trials during an epidemic when an institution is overwhelmed with patients is challenging. Nevertheless, we decided that it was imperative that we participate in clinical trials aimed at finding new therapies for Covid-19. Our leadership received numerous requests for participation in clinical trials examining new treatments for Covid-19, and those had to be vetted by experts in the field. All clinical trial efforts were centralized and coordinated by the vice chair for research (MJK). In addition, the Albert Einstein College of Medicine established a committee of experts in different relevant fields that evaluated proposed trials to select those that were suitable for our institution. The criteria used to select trials that our institution joined were: (1) Convincing premise and rationale for the proposed study; (2) Rigorous prior research and preliminary data showing potential efficacy; (3) Feasibility of performing the study at Montefiore; (4) Adequate infrastructure and staff for rapid implementation. To meet the sheer demands of the pandemic and the urgency of launching new studies quickly, experienced clinical trials coordinators were supplemented with coordinators who volunteered their time when their outpatient studies were suspended. Data collection and entry were assigned to coordinators and volunteers who were based outside of the hospital because of health or infection control restrictions to allow for hospital-based coordinators to concentrate on enrollment and study procedures. With these criteria and strategies, we participated in eight randomized clinical trials during the pandemic: three Adaptive Covid-19 Treatment Trials (ACTT) of remdesivir; sarilumab trial; two leronlimab trials; convalescent plasma trial; an NHLBI-funded hydroxychloroquine trial; and a CDC surveillance study of healthcare workers. These studies helped establish the efficacy of remdesivir, the safety of convalescent plasma, and the lack of efficacy of hydroxychloroquine and sarilumab. The leronlimab trials are ongoing.
Retrospective Analysis of Our Covid-19 Cohort
More than 8,000 Covid-19 patients were admitted to MMC and the data collected during their hospitalization was critical to learning about Covid-19. Therefore, investigators and clinicians in the DOM designed protocols and obtained IRB approval for analyzing data collected from all Covid-19 patients cared for at MMC. As these research efforts intensified, it became clear that there was a need for a centralized review and approval process. A large number of retrospective studies were being done simultaneously by various groups within the DOM and it was possible that many of them could overlap. Therefore, we established a Research Committee on Covid-19 (RCC) to coordinate all retrospective research efforts and to evaluate each study for premise, importance, feasibility, appropriate expertise, and overlap with other studies. The RCC evaluated approximately 200 projects. To assist the RCC in its work we built an online portal to which every new project was uploaded providing all the necessary information for the RCC to evaluate the project. At the time of the writing of this manuscript, 23 research studies from the DOM at Montefiore have been published. They include studies that had a huge impact on our understanding of Covid-19 (10–16) and on treatment protocols for Covid-19 (4).
Other Studies
Non-Covid-related clinical research continued remotely and transitioned to video visits when possible. Some projects used electronic consent (e-consent) to facilitate continued recruitment into studies. DOM investigators submitted 35 Covid-19-related applications for funding and 11 were awarded to implement high-impact trials, pursue multicenter observational studies, support underserved patients with diabetes, and implement artificial intelligence and machine learning to predict respiratory failure in patients with Covid-19.
New Technology and Innovation
The epidemic created many challenges that required innovative solutions. The DOM director of innovation (SPJ) led our efforts to use technology to overcome challenges the epidemic created. Some challenges that required innovative technological solutions included: (1) Converting most outpatient visits to video visits; this was achieved through several new platforms for video visits; (2) Connecting patients with their families as families were not allowed to visit; this was achieved by providing dozens of electronic tablets (donated to the department) to our inpatient floors and fitting them onto carts; (3) Rapid dissemination and updating of our treatment protocols; this was achieved by creating (with a developer) a free downloadable mobile App (MedProtocols, available on the iOS and Android App Stores) that stores all the Montefiore Covid-19 protocols.
Recruiting Alumni Volunteers and Outreach for Donations
We contacted physician alumni of Einstein and Montefiore asking for volunteers to work in our hospitals during the pandemic. These efforts were highly successful with many alumni volunteering to come to the Bronx and work in our hospitals (Table 1). We also solicited donations through an Amazon page where we listed items needed (e.g., pulse oximeters for patients, etc). Through our newsletter and social media outreach we received numerous donations that not only helped us cope with shortages of these items but also gave a strong morale boost to our providers.
Community Outreach and Efforts to Raise the Morale of Our Frontline Providers
Faced with a disease that had no treatment and caring for large numbers of patients decompensating and dying, the stress and heartbreak felt by our frontline providers cannot be overstated (17). We alleviated this stress through constant communication between leadership and the frontline providers (see above). We also collaborated with the Department of Psychiatry that established a strong mental health support program for the frontline providers at Montefiore. These measures were helpful, but we felt that we needed to do more. Therefore, we reached out to our Bronx, Westchester, and Hudson Valley communities through social media, and requested displays of support for the frontline providers at Montefiore. The response of the community was overwhelming and heartening. Hundreds of e-mails, letters, photos, videos, and artwork, mostly created by children, were sent to us and were shared with our frontline providers, energizing them and boosting their morale during these terrible times. We also launched a social media campaign under the hashtag #MontefioreProud. #MontefioreProud gear was distributed to DOM providers and staff and were highly popular and had a significant positive impact on morale and camaraderie at our institution.
The Department of Medicine Post-COVID
As of the writing of this manuscript the positive Covid-19 testing rate has declined significantly in New York City and the epidemic seems to be contained. However, our work is not finished as we have to address two main remaining challenges: (1) preparing for additional Covid-19 surges; (2) treating patients who recovered from Covid-19 and continue to suffer from its long-term consequences.
Preparing for Additional Surges
During the first Covid-19 wave at our institution we created an online database where we stored the information about all our deployed physicians. We have since updated this database with information about all physicians who may need to be deployed and where. Our approach is similar to military reserve preparedness where our central command can deploy physicians very quickly using this online database. Plans are in place for ICU expansion, IM units' expansion, and converting all our units into Covid-19 units, and rapid initiation of clinical trials.
Treating Patients With Chronic Consequences of Covid-19
It is becoming evident that a large number of patients who survived Covid-19, especially those that were admitted to the ICU, suffer from long-term consequences of Covid-19 including chronic fatigue, dyspnea, foggy thinking, chronic anosmia, memory loss, depression, as well as cardiac, renal, pulmonary, and brain complications from the disease (18, 19). To address these issues the Montefiore DOM established a Covid Recovery (CORE) clinic where a multi-disciplinary team of clinicians are following patients who recovered from Covid-19. The CORE clinic will also serve as a research platform to study the long-term consequences of Covid-19, their causes, and how they can be prevented and treated.
Lessons Learned
During a crisis such as the Covid-19 pandemic effective leadership can be described by the abbreviation A,B,C,D,E:
Available – the leadership team should always be available and responsive to all communications and requests coming from the frontlines.
Back – the providers at the frontlines should know and be constantly reassured that the leadership team always has their back and will support them with all resources available.
Clear – communications coming from the leadership team should be clear and consistent.
Determined – the leadership team should show determination and decisiveness, and decisions have to be made promptly without delay.
Example – the leadership team should lead by example.
The DOM leadership team, comprising the Medicine Covid-19 Taskforce (MCT) and our division chiefs adhered to these five principles: Our leadership team was available all the time and communicated with frontline providers continuously; we supported our frontline providers with all our resources, and when resources were insufficient (e.g., PPE) we solicited donations to acquire them; communications were clear, consistent, and timely; decisions were made promptly and unambiguously; and all members of our leadership team who did not have medical/age exemptions worked at the frontline together with our providers.
The first important lesson is that the 3C framework was effective, but only when applied at all levels of the organization and in a bi-directional way, from leadership to frontlines but also from frontlines to leadership (Figure 2).
One of the key components of the 3C framework was the establishment of the Medicine Covid-19 Taskforce (MCT). An important lesson learned is that the MCT had to be large to encompass all arms of the department. The MCT had 18 members and while that lengthened our meetings it was critical for coordinating such a large department.
The 3C framework enabled us not only to coordinate all arms of the DOM but also to quickly implement creative, out of the box, solutions to the new challenges we were facing such as switching inpatients consults to eConsults, or making all our protocols available through a free downloadable mobile App.
Finally, one of the most important lessons learned is that while the main focus was on deployment and expansion of our ICU's and IM units to accommodate the rapid inflow of Covid-19 patients, our work did not end with deployment only. We had to devote time and effort to research, education, outpatient care, donations, community outreach and much more, while at the same time expanding our capacity to care for Covid-19 inpatients. Here again the 3C framework was very helpful.
Conclusions
The Covid-19 pandemic caused the most serious public health crisis of this century. No Medical Center in the US had experience with such a large-scale epidemic, and therefore hospitals had to adapt to the new situation and the many challenges it created overnight. Making things even worse, the lack of preparedness by government agencies for such a large-scale pandemic resulted in shortages of PPE, delayed testing for infection, and lack of clear and consistent treatment guidelines (20). Our medical center, located in the Bronx, was at the epicenter of the epidemic when it first hit the US during the months of March to May. In order to mobilize the DOM to handle the exponential increase in the number of patients with Covid-19 being admitted to our units we implemented a teamwork strategy that we dubbed the 3C framework. Using this framework, we were able to adapt quickly to the new situation in a coordinated and synergistic way, doubling our medicine units, deploying physicians, creating uniform and up-to-date treatment protocols, creating educational materials on treating Covid-19 for our frontline providers, converting inpatient consults and all outpatient activities into telemedicine, performing clinical trials, innovating and reaching out to our community through a large social media campaign. The main lesson from our experience is that the key to confronting such a challenging and stressful situation as the Covid-19 pandemic is to work in a cohesive leadership team that applies that 3C framework and functions in a coordinated and synergistic fashion. We believe that the same 3C framework can be effective not only within an individual Medical Center but when responding to a public health crisis at the regional and national level (3, 21, 22).
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Ethical review and approval were not required for the study since it did not involve human participants, in accordance with the local legislation and institutional requirements. Written informed consent was not required for the study since it did not involve human participants, in accordance with the national legislation and the institutional requirements.
Author Contributions
YT: performed the work described in the manuscript for the Chair of Medicine, conceived the idea of the manuscript, and wrote the manuscript. MN: performed the work described in the manuscript for the Chief of Critical Care Medicine and wrote certain sections of the manuscript. MK: performed the work described in the manuscript for the Vice Chair of Medicine for Research and wrote certain sections of the manuscript. WS: performed the work described in the manuscript for the Chief of Hospital Medicine and wrote certain sections of the manuscript. EK: performed the work described in the manuscript for the Vice Chair for Faculty Affairs and wrote certain sections of the manuscript. GK: performed the work described in the manuscript for the Residency Program Director (Wakefield campus) and wrote certain sections of the manuscript. LS: performed the work described in the manuscript for the Residency Program Director (Moses-Weiler campuses) and wrote certain sections of the manuscript. SJ: performed the work described in the manuscript for the Department of Medicine Director of Innovation and wrote certain sections of the manuscript. EE: performed the work described in the manuscript for the Director of Medicine Faculty Practice and wrote certain sections of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
YT was previously (1/2015 – 6/2017) the PI on a basic research project jointly funded by the Juvenile Diabetes Research Foundation and Pfizer that is unrelated to the current manuscript. YT has two patent applications. (PCT/US2016/067775 & US provisional No: 61/883,062) that are not related to the current manuscript.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We wish to express our utmost gratitude to the tens of thousands of Montefiore Health System's health care providers, who worked selflessly, day and night, for many weeks, risking their lives and the welfare of their families, to care for Covid-19 patients. They all deserve our profound thanks and gratitude. These brave men and women saved thousands of lives and are the reason that MHS responded to the epidemic so effectively. Special thanks to the Montefiore-Einstein leadership, Drs. Philip Ozuah, Andrew Racine and Dean Gordon Tomaselli for their unwavering stewardship, for inspiring us, and serving as role models for all of us. We also wish to thank Dr. Silvie Colman, PhD and Dr. Mimi Kim, ScD for producing Figure 1 of the manuscript.
References
1. Zangrillo A, Beretta L, Silvani P, Colombo S, Scandroglio AM, Dell'Acqua A, et al. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: facing the COVID-19 pandemic emergency. Crit Care Resusc. (2020) 22:91–4.
2. Ciceri F, Castagna A, Rovere-Querini P, De Cobelli F, Ruggeri A, Galli L, et al. Early predictors of clinical outcomes of COVID-19 outbreak in Milan, Italy. Clin Immunol. (2020) 217:108509. doi: 10.1016/j.clim.2020.108509
3. Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. Fair allocation of scarce medical resources in the time of covid-19. N Engl J Med. (2020) 382:2049–55. doi: 10.1056/NEJMsb2005114
4. Keller MJ, Kitsis EA, Arora S, Chen JT, Agarwal S, Ross MJ, et al. Effect of systemic glucocorticoids on mortality or mechanical ventilation in patients with covid-19. J Hosp Med. (2020) 15:489–93. doi: 10.12788/jhm.3497
5. Wexler DJ, Hirsch IB, Mulder JE. Coronavirus disease 2019 (COVID-19): issues related to diabetes mellitus in adults. UpToDate. (2020).
6. Richterman A, Meyerowitz EA, Cevik M. Hospital-acquired SARS-CoV-2 infection: lessons for public health. JAMA. (2020). doi: 10.1001/jama.2020.21399. [Epub ahead of print].
7. Spitzer Sverd S, Gardner LE, Cabassa JA, Schneider M, Noone RH, Jahdi MH, et al. A Bronx tale: exposure, containment and care on inpatient psychiatry units during COVID-19. Gen Hosp Psychiatry. (2020). doi: 10.1016/j.genhosppsych.2020.07.010. [Epub ahead of print].
8. Merken R, Kruger A, Bhardwaj G, Kajita GR, Shapiro LI. Internal medicine resident work absence during the COVID-19 pandemic at a large academic Medical Center in New York City. J Grad Med Educ. (2020) 12:682–5. doi: 10.4300/JGME-D-20-00657.1
9. Bernstein CA, Bhattacharyya S, Adler S, Alpert JE. Staff emotional support at montefiore Medical Center during the covid-19 pandemic. Jt Comm J Qual Patient Saf. (2020) 47:185–9. doi: 10.1016/j.jcjq.2020.11.009
10. Agarwal S, Schechter C, Southern W, Crandall JP, Tomer Y. Preadmission diabetes-specific risk factors for mortality in hospitalized patients with diabetes and coronavirus disease 2019. Diabetes Care. (2020) 43:2339–44. doi: 10.2337/dc20-1543
11. Reyes Gil M, Barouqa M, Szymanski J, Gonzalez-Lugo JD, Rahman S, Billett HH. Assessment of lupus anticoagulant positivity in patients with coronavirus disease 2019 (COVID-19). JAMA Netw Open. (2020) 3:e2017539. doi: 10.1001/jamanetworkopen.2020.17539
12. Palaiodimos L, Kokkinidis DG, Li W, Karamanis D, Ognibene J, Arora S, et al. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism. (2020) 108:154262. doi: 10.1016/j.metabol.2020.154262
13. Fisher M, Neugarten J, Bellin E, Yunes M, Stahl L, Johns TS, et al. AKI in hospitalized patients with and without covid-19: a comparison study. J Am Soc Nephrol. (2020) 31:2145–57. doi: 10.1681/ASN.2020040509
14. Nori P, Cowman K, Chen V, Bartash R, Szymczak W, Madaline T, et al. Bacterial and fungal coinfections in COVID-19 patients hospitalized during the New York City pandemic surge. Infect Control Hosp Epidemiol. (2020) 42:1–5. doi: 10.1017/ice.2020.368
15. Chand S, Kapoor S, Orsi D, Fazzari MJ, Tanner TG, Umeh GC, et al. COVID-19-associated critical illness-report of the first 300 patients admitted to intensive care units at a New York city Medical Center. J Intensive Care Med. (2020) 35:963–70. doi: 10.1177/0885066620946692
16. Sourial MY, Sourial MH, Dalsan R, Graham J, Ross M, Chen W, et al. Urgent peritoneal dialysis in patients with covid-19 and acute kidney injury: a single-center experience in a time of crisis in the United States. Am J Kidney Dis. (2020) 76:401–6. doi: 10.1053/j.ajkd.2020.06.001
17. Cunningham CO, Diaz C, Slawek DE. COVID-19: the worst days of our careers. Ann Intern Med. (2020) 172:764–5. doi: 10.7326/M20-1715
18. Carfi A, Bernabei R, Landi F, Gemelli against C-P-ACSG. Persistent symptoms in patients after acute COVID-19. JAMA. (2020) 324:603–5. doi: 10.1001/jama.2020.12603
19. Li Z, Zheng C, Duan C, Zhang Y, Li Q, Dou Z, et al. Rehabilitation needs of the first cohort of post-acute COVID-19 patients in Hubei, China. Eur J Phys Rehabil Med. (2020) 56:339–44. doi: 10.23736/S1973-9087.20.06298-X
20. Shapiro LI, Kajita GR, Arnsten JH, Tomer Y. Toward better preparedness for the next pandemic. J Clin Invest. (2020) 130:4543–45. doi: 10.1172/JCI140296
21. Schuchat A, Team CC-R. Public Health Response to the Initiation and Spread of Pandemic COVID-19 in the United States, February 24–April 21, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:551–6. doi: 10.15585/mmwr.mm6918e2
Keywords: COVID-19, department of medicine, pandemic, teamwork, leadership, telehealth, coordination, communication
Citation: Tomer Y, Ng Gong M, Keller MJ, Southern W, Kitsis EA, Kajita GR, Shapiro LI, Jariwala SP and Epstein EJ (2021) Teamwork and Leadership Under Fire at the Epicenter of the COVID-19 Epidemic in the Bronx. Front. Med. 8:610100. doi: 10.3389/fmed.2021.610100
Received: 25 September 2020; Accepted: 23 February 2021;
Published: 18 March 2021.
Edited by:
Ryuki Kassai, Fukushima Medical University, JapanReviewed by:
Shinn-Jang Hwang, Taipei Veterans General Hospital, TaiwanRobert Drury, ReThink Health, United States
Copyright © 2021 Tomer, Ng Gong, Keller, Southern, Kitsis, Kajita, Shapiro, Jariwala and Epstein. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yaron Tomer, eXRvbWVyQG1vbnRlZmlvcmUub3Jn
 Yaron Tomer
Yaron Tomer Michelle Ng Gong2
Michelle Ng Gong2 Marla J. Keller
Marla J. Keller Sunit P. Jariwala
Sunit P. Jariwala