
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Med., 27 April 2021
Sec. Family Medicine and Primary Care
Volume 8 - 2021 | https://doi.org/10.3389/fmed.2021.585495
This paper argues that “functional,” “medically unexplained,” or “somatoform” symptoms and disorders necessarily require a patient-centered approach from the clinicians. In the first part, I address the multiple causes of the patients' suffering and I analyze the unease of the doctors faced with these disorders. I emphasize the iatrogenic role of medical investigations and the frequent failure in attempting to reassure the patients. I stress the difficulties in finding the right terms and concepts, despite overabundant nosological categories, to give a full account of psychosomatic complexity. Finally, I discuss the moral dimension attached to assigning a symptom, at times arbitrarily, to a psychogenic origin. The following part presents a brief reminder of the patient-centered approach (PCA) in medicine. In the last part, I aim to explain why and how patient-centered medicine should be applied in the context of functional disorders. First, because PCA focuses on the patients' experience of illness rather than the disease from the medical point of view, which is, indeed, absent. Second, because PCA is the only way to avoid sterile attribution conflicts. Last, because PCA allows doctors and patients to collaboratively create plausible and non-stigmatizing explanations for the symptoms, which paves the way toward effective management.
Symptoms and syndromes labeled as “functional,” “medically unexplained,” “psychosomatic,” “somatoform,” and so on are and will remain common, despite advances in medical science. Sometimes, they involve isolated symptoms, temporary or long-lasting; sometimes, they are relatively clearly defined (yet with labels that often change with a fragile nosology reflecting the controversy surrounding their causes and medical legitimacy) (1, 2); while at other times, they constitute idiosyncratic complaints that, at best, confuse doctors and, at worst, exasperate them. Though it is feasible to assume that their prevalence varies depending on how sophisticated the medical means used in explaining them, the fact that they are highly common and cause a considerable cost to health care systems cannot be denied (3, 4). Somatoform disorders [which are persistent medically unexplained symptoms (MUS) leading to impairment and distress] occur in ~6% of the population, 16% of primary care attenders, and up to 33% of patients in secondary care clinics (3). Specific functional somatic syndromes are also common, with prevalence estimates around 7% for irritable bowel syndrome, 2.5% for chronic fatigue syndrome, and 2–4% for fibromyalgia (3). Somatoform and functional disorders are associated with increased health care use and costs, and represent major reasons for sickness absence, disability benefits, and early retirement pensions in Europe and the US (3).
These functional conditions, symptoms, and syndromes pose many issues that may contribute to a frustrating and often iatrogenic doctor–patient relationship; among the issues are the following.
While telling a patient there is “nothing wrong” should be reassuring, in many cases, it is instead a cause of suffering for both patient and doctor. For the patient, the suffering due to symptoms (discomfort, pain, fatigue, and limits to daily life) is compounded by the uncertainty about their cause (and fear about their outcome), and the frustration induced by the lack of medical legitimacy. Doctors experience similar uncertainty regarding the nature of the patient's symptoms (and thus fear of misrecognizing a “medical” disorder), as well as difficulty of reassuring patients and powerlessness in front of refractory symptoms (4).
Symptoms are labeled as “medically unexplained” when there is no proven organic cause, yet physicians always fear to leave a “medical” cause undetected. Doctors always bitterly regret having missed a physical diagnosis, yet curiously never deplore having contributed, through extensive workup and uncoordinated referral to medical specialists, to the genesis of refractory somatization (5, 6). Uncertainty has become more and more intolerable for doctors (7), which have long been affected by the “futile search for certainty” that pushes them to order and perform more investigations (8). Diagnostic errors (labeling as functional symptoms explained thereafter by an organic disease) are nevertheless rare and do not always have harmful consequences (9, 10). Moreover, unlike common assumptions, patients that present with functional disorders do not always “push” their doctors to prescribe supplementary tests, or at least not to the extent they assume (6, 11, 12).
Most patients with functional disorders are worried, and doctors wish to reassure them. However, this crucial skill is far from simple and is not taught in medical schools (13). Besides, it is not always even appropriate, as the extent of disability and social consequences of some chronic functional disorders are sometimes much worse than those of organic diseases (4), as Michael Balint pointed out: “In some cases, a physical illness represents, in fact, a more serious threat to the patient's well-being, but in others, the functional illness is definitely the greater danger” (14).
Prescribing complementary tests expected to yield a negative result is generally used by doctors as a way of reassuring patients. However, this is a dangerous illusion (13, 15), since ordering test after test with the aim of “ruling out” an organic disease feeds the belief that “something has to be found,” reinforces anxiety while waiting for the results, and eventually increases the focus on symptoms while deceiving the patient's expectations for explanation when tests prove negative. In the worst-case scenario, complementary tests find abnormalities without significance (biological or radiological “incidentalomas” or false positives, especially common when the disease to be ruled out is unlikely), leading to more tests and consultations, further increasing uncertainty and anxiety, encouraging the patient to adopt a sick role, and eventually contributing to the chronicity of the condition (5, 6, 11, 12). Balint stated that “It is implied. that the patient is not changed or influenced by the process of ‘elimination' (but) the patient's attitude to his illness is usually considerably changed during and by the series of physical examination” (14).
The terms used in discussing functional disorders are numerous and the nosology in this field is unsatisfactory. The term functional qualifies the subjective nature of a symptom as opposed to one of organic origin (caused by a lesion or relating to an established physiopathology). It is a rather neutral term (not necessarily involving psychogenesis) and the most easily accepted by patients (16). The term medically unexplained brings up this pervasive belief that the primary task of doctors is to rule out an organic cause for the presented symptoms, giving the impression that without such a cause, they do not fall under the responsibility of medicine. At the very worst, it could be taken as a denial of the symptoms and suffering, or by default as the assertion of their psychogenic nature. Moreover, considering a given symptom as fully “explicable” does not take away the arbitrariness of the decision. The term somatization means, according to authors, a psychopathological process of “converting” distress or more or less conscious psychological conflicts into physical symptoms; a form of “illness behavior” characterized by the “tendency to experience and communicate somatic distress in response to psychosocial stress and to seek medical help for it” (17); or simply the persistent presence of debilitating functional somatic symptoms (18). The last two definitions differ from the first in that they are not predicated on the symptoms being (solely) psychogenic. Somatoform disorders are a group of mental disorders introduced in the third edition of the Diagnostic and Statistical Manual of Disorders (DSM-III) that all featured somatic symptoms are with no physical explanation and health care seeking. The categorization and even the very idea of somatoform disorders were severely criticized by many researchers of the field (19), leading to a complete overhaul creating the 5th edition (DSM-5), which identified a separate diagnostic group labeled somatic symptom disorders. The “medically unexplained” nature of the symptoms is no longer mandatory, while psychological distress and abnormal illness behavior associated with physical symptoms have become a major criterion, and the category has also been widened to include factitious disorders and “psychological factors affecting other medical conditions,” which were previously found in other sections of the DSM. Unlike somatic symptom disorders, which are categories developed by psychiatrists, functional somatic syndromes (FSS) are diagnostic labels coined by non-psychiatric physicians that refer to syndromes without an organic disease explanation, structural changes, or established pathophysiology, for which each medical specialty has at least one example, such as fibromyalgia for rheumatology, irritable bowel syndrome for gastroenterology, chronic fatigue syndrome for internal medicine and infectious diseases, hyperventilation syndrome and non-cardiac chest pain for respiratory medicine and cardiology, and so on. These syndromes, which display overlapping clinical features, frequently occur in association, and thus singling any of them out as a specific entity could simply just be the result of medical specialization (20). Indeed, there is supporting evidence for shared risk factors, triggers, and perpetuating factors across these disorders, as well as for the efficacy of similar treatment approaches (21). In line with this “lumping” view, a new category called bodily distress disorder has been constructed to capture most of the “somatoform” and “functional” disorders under a single diagnostic category (22), and this diagnostic term has been chosen to replace the somatoform disorders in ICD-11.
Due to this overabundant nosology, a patient suffering from functional symptoms may receive several different diagnostic labels, such as one or more among the functional somatic syndromes as well as one or more somatoform disorder, not to mention the anxiety and mood disorder diagnoses frequently associated with them which may sometimes explain all or some of the symptoms. Depending on the diagnostic term used, the psychogenic nature of the symptoms is either explicitly affirmed or implicitly assumed, and the associated psychological distress was viewed either as a causal factor or as mere comorbidity. This ambiguous and complex nosology makes communication between different health care professionals complicated, while it is of vital importance that they collaborate closely in order to manage and treat patients. Furthermore, doctor–patient communication is also hampered, with any attempt at offering the clear information that every patient deserves becoming near impossible.
Recently, the EURONET-SOMA group proposed “functional somatic disorder” as an umbrella diagnostic term for the various conditions characterized by persistent and troublesome symptoms, to be situated in a neutral space within disease classifications, favoring neither somatic disease etiology nor mental disorder (23). A wide adoption by the medical and psychological communities of this new classification would, in my opinion, be a great progress toward the resolution of the pervasive dualism that impedes communication with patients and between health care professionals, understanding, and proper management of “medically unexplained” symptoms and bodily distress.
The Cartesian dualism of mind and body are deeply ingrained across Western society and can be considered as an epistemic pillar of biomedicine. Not only is a symptom considered as more “real” if caused by an organic disorder than if “unexplained,” but there is a moral judgment of responsibility, if not of blame, imposed on symptoms suspected as being of psychological origin. This moral weight of dualism explains that the persons suffering from physical symptoms that they feel they have no control over tend to attribute them to a medical condition that they could in no way be considered as responsible. They understandably prefer to be seen as victims, legitimately requiring the help of medicine, rather than suspected culprits. Sociological studies of people suffering from functional disorders have extensively documented their painful experiences of misunderstanding and suspicion from the biomedical establishment, which underestimates their suffering and the pain of their symptoms, only grudgingly according them the status of patients that they believe is theirs by right (24). For some sufferers, the quest for medical legitimacy appears to take priority over looking for means to alleviate symptoms. This has deleterious consequences: as Nortin Hadler coined it, how can you get well if you have to prove you are ill? (25).
Questioning the validity of some of the “myths” that underlie our understanding of MUS, using the most recent research available (26), should help in avoiding some of these traps of dualism. MUS are not always associated with depression and anxiety, while “organic” disorders are often complicated by psychological distress or common psychiatric disorders. MUS are often associated with physical conditions, and the underlying mechanisms are not fundamentally different from those of organic diseases, with biological and psychological factors always at work: the pathophysiology of the major functional somatic syndromes is a good example of how complex their interactions can be (22).
The issues addressed in this chapter help pave the way toward a more constructive approach to managing functional disorders. Firstly, to address the multiple causes of a patient's suffering and to analyze the unease experienced by health care providers when faced with these disorders; secondly, to measure the iatrogenic role of medical investigations and to understand why most attempts to reassure the patient do not work; thirdly, to assess how difficult it is to find the right terms and concepts to give full account of psychosomatic complexity; and finally, to be conscious of the moral dimension attached to assigning a symptom, at times arbitrarily, to a psychogenic origin. This brought about an attempt of conceiving the problem from the patient's point of view, in order to help him/her get through it.
The tensions between medicine focused on the disease/doctor and those centered on the patient/person are nothing new, and no explanation offered by biological sciences or advances in treatments of evidence-based medicine has changed anything. Take, for example, the aphorism variously attributed to Hippocrates, William Osler, and others, stating that it is “more important to know what sort of person has a disease than to know what sort of disease a person has” to be a good doctor. Some link this concept with the concern expressed by doctors throughout the ages about the risk of medicine becoming too scientific, turning doctors away from their humanist values. The idea of a doctor viewing and understanding a patient as a “whole” person is also central to the studies and life's work of Michaël and Enid Balint, the latter of whom is credited with being the first to use the term “patient-centered medicine” in the literature (27): “There is another way of medical thinking which we call ‘patient-centered medicine.' Here, in addition to trying to discover a localizable illness, the doctor has to examine the whole person [.]. This should include everything that the doctor knows and understands about his patient; the patient, in fact, has to be understood as a unique human being.” The patient-centered approach (PCA) is connected to the landmark “bio-psycho-social” theoretical model of George Engel (28, 29) and the operationalization of competing terms illness, disease, and sickness by Harvard psychiatrists and anthropologists (30) (to be discussed later), both of which appeared in the 70s. Yet, it was not until the 80s that the concept finally gained worldwide recognition, promoted by the family medicine department of Western University, Ontario (31). In its current form, the concept aligns with criticisms of the “paternalist” carer–patient relationship model and promoters of a “participatory” model that focuses on patient autonomy. It also echoes the distinction between cure and care. Finally, this approach has found its place in the “narrative medicine” movement (32) and modern conceptions of patient education and counseling. Whatever its form, it establishes that patients possess knowledge on their “illness,” that their psychological and behavioral reactions are impacted by their representations, and that they own resources that we must help them access and use to improve their health and decrease the suffering and social consequences of by their health condition.
PCA aims to combine traditional medical activities such as diagnosis and treatment (based, as far as is possible, on factual evidence) with the explicit understanding of what patients personally experience, including what they perceive and how they explain what is wrong, their emotions and feelings regarding their condition, especially their fears, the impact of their health issues on their day-to-day activities and functions, and their expectations of what should be done. According to its promoters (31), the implementation of PCA comprises six interactive components that are formulated as orders for doctors to follow (List 1). Recent reformulations of the basic elements of patient-centered care have been offered (List 2) (33). Many academic programs have been created to train doctors in PCA (34), especially in terms of interviewing and communication techniques (35). However, although health care organizations currently strive to improve health care system performance through the implementation of person-centered care, PCA is often “more preached than practiced,” and despite a large consensus on the values carried by the concept, actual implementation of PCA at the health care delivery level remains a challenge (36, 37).
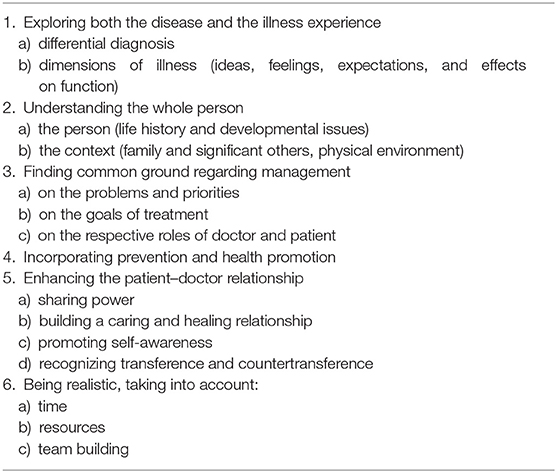
List 1. The six components of the patient-centered process (31).
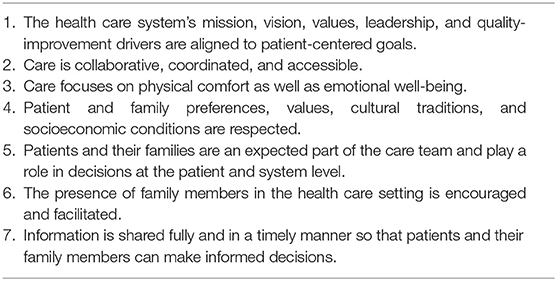
List 2. Elements of patient-centered care (33).
The benefits of PCA are potentially great, though the scientific evidence of these positive effects is weak (in part due to the difficulties in creating research contexts where the many ingredients of PCA can be operationalized, but also due to a lack of modeling of the mechanisms linking doctor–patient communication with patient health) (38–40). PCA has been shown to allow obtaining deeper and more pertinent information (including for establishing a biomedical diagnosis), to generate greater patient satisfaction, to achieve better compliance, to provide stronger reassurance, and to enable more effective therapeutic relationships (31, 40). Studies on patient perception have confirmed these expectations (41). Importantly, doctors who practice PCA report higher satisfaction themselves, and despite what many think, patient-centered consultations have been found to be no longer than traditional ones and could even save time (31, 35, 42). Patient-centered care has been associated with decreased use of diagnostic tests and referrals and decreased health care utilization (43, 44). Patient-centered care may thus improve resource allocation and reduce expenses throughout the continuum of care (33). Finally, it is likely that PCA helps to some extent to forewarn against lawsuits (45).
PCA has been criticized for the risk of diverting the physicians' attention from diagnostic issues, or for being difficult to implement due to time constraints in the consultation room. However, the main problems with PCA may well be practice gaps due to the widespread context of biomedically health care, the lack of emphasis on PCA in medical education, and the lack of supportive environment and financial incentives for practicing physicians (37).
The concept of patient-centered care extends for some authors to the customization of treatment based on individual biological characteristics, known as “personalized medicine,” broadly conceived as the use of genomics, proteomics, and other recent technologies to provide decisions with regard to prediction, diagnosis, and treatment of disease (33). Such an approach may be relevant to the treatment of functional disorders in the tradition of Engel's biopsychosocial model. Notably, systems thinking (46) is propelling research on persistent somatic symptoms, whether “medically unexplained” or not, beyond mind–body dualism and toward the integration of psychological, biological, and social contextual factors, using modern technology to link the subjective experience of somatic symptoms with objective measures of biological processes such as autonomic imbalance (47). However, some authors have argued that systems medicine remains insufficient in bridging the gap with humanistic medicine built on the concept of “patient as a person.” They consider that, being at least for the moment unable to account for meaning, value, and symbolic interaction, systems medicine cannot be fully integrative, holistic, and patient-centered in a humanistic sense (48). The question of whether PCA and personalized medicine are irreconcilable concepts or may be combined at theoretical and pragmatic levels is a subject of philosophical inquiry (49).
To begin with, we need to go back to the dichotomy between disease and illness, set into motion by medical anthropologists in the 70s and 80s (30, 50) building on René Leriche's concept of the “doctor's illness” as opposed to the “patient's illness.” The term disease represents the illness as an objectifiable biological reality. In this approach, the focus is on what is objective and, where possible, quantifiable; the disease is a “thing on its own” (ontological perspective) and medical inquiry aims to sort through the patient's experiences retaining as pertinent only their symptoms (which thus become signs) and complaints that can be linked to an anatomical or biochemical abnormality, or a well-defined pathological entity in the case of psychiatry. For the doctor, the ultimate “reality” is that of the disease: the social and cultural context of the sick persons, their emotions and personality, and the meaning ascribed to their ailments are contingent. The term illness, on the other hand, refers to the experience of disease, a fundamentally subjective and idiosyncratic reality that is also impacted by the cultural and social context, communicated to other people, covering the perception of trouble, the emotions that accompany it, and the lay interpretation of symptoms. This experience is most often created through interaction with friends or family, and more or less explicitly involves the patient's pervasive questioning about the meaning of the disease as a personal misfortune, along the lines of “do I deserve this?” or, in other cultural contexts, “who wishes harm to me?” (51). Finally, the term sickness aims to more comprehensively cover the multiple social dimensions of what is already suggested in the term illness: how the definitions of health and sickness vary from person to person, culture to culture, and even across different social classes; the existence of culturally recognizable and socially acceptable forms of being sick (idioms of distress); and the status of sickness requires a social legitimation that is obtained through conforming to standards governing illness behavior. In many societies, and particularly our own, the sick role can actually be seen as a deviant yet not sanctioned behavior, instead prompting help and compassion, as long as the disease can be blamed on an agent located out of the person's control (52).
These concepts show us just how far the disease-centered approach becomes untenable as soon as functional or “medically unexplained” symptoms are in play, since this means treating illnesses without disease. Then, the only pragmatic response to these symptoms is to address the illness experience of a specific person. On the other hand, doctors cannot overlook that they play a key role in our Western societies in the social legitimization of an ill person's status by establishing a diagnosis and prescribing sick leave, among other responsibilities. When faced with someone presenting functional symptoms, experienced doctors often quickly realize that an actual disease will not be found, but they can still choose to focus on the disease rather than on the patient, because there lies their field of expertise and skill, but also for fear of hastily taking the risk of delegitimizing the patient's complaint. Balint coined that “diseases are arranged in a kind of ranking order roughly corresponding to the seriousness of the anatomical changes which can be demonstrated or assumed in them. Unfortunately, not only are the diseases given this kind of rank, but also the patients, so to speak, are attached to them. Patients whose complaints may be traced back to demonstrable or assumable anatomical or physiological changes are rank higher, and neurotics are in a way the dregs left over after everything else has been drawn off. Thus, it is understandable that every doctor, when confronted with a new patient, tries to give a good rank and will relegate the patient to the class of neurotics only if he cannot find any justification to give a respectable status.” (14). This game of trickery helps to construct somatization, especially when a doctor proves incapable of seizing on the clues a patient offers him (6). Somatization can actually be fundamentally conceived as a dispute over attribution (“it's in my body” vs. “it's in his head”), yet empirical studies have shown that in a way this conflict may be overplayed by both parties (53), with patients often offering an opening for a psychosocial explanation for their symptoms (as long as that is not meant as their exclusive cause), and above all wishing for the doctor to be interested in their symptoms and not to immediately normalize them (6, 53).
Combining the benefits of PCA contribution with a bio-psycho-social approach for functional disorders (54) requires certain useful assertions to be retained (List 3). It is not about abandoning the biomedical approach focused on research of identifiable organic diseases and evidence-based treatment, but rather to explore concurrently and simultaneously the “patient's agenda,” meaning their background and life context, their representations, fears, expectations, and emotions. There would be less stigmatization of functional disorders if the exploration of the psychosocial aspects of suffering was not reserved solely for patients whose symptoms resist medical explanation (54).
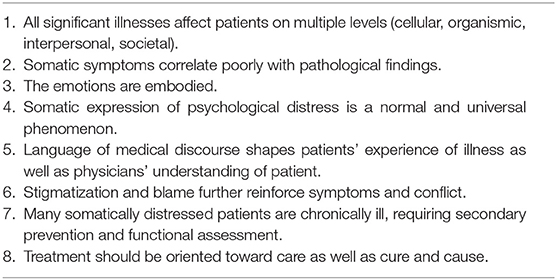
List 3. Principles of a biopsychosocial approach to unexplained somatic symptoms and functional disorders (54).
What is most important is to come to an agreement on how to call the problem (2): a name that would make sense both to the doctors and patients, which should lead toward normalizing symptoms rather than psychologizing them, thus avoiding stigmatization, and which would communicate plausible, understandable, and personalized explanations of the mechanisms underpinning the disorder. The term chosen should also convey the complexity [distinguishing, for example, between predisposing, triggering, and maintaining/aggravating factors of the symptoms (21)], as well as being congruent with the experience of the patient, while allowing to alleviate some suffering. This, of course, is a difficult task. Patients tend to resist psychosomatic attributions unilaterally attributed by doctors (55). A diagnosis of “somatoform disorder” has no useful meaning for most patients, and diagnoses of functional somatic syndromes are no more easier to understand (56), except for functional disorders based on unorthodox or controversial attributions (multiple chemical sensitivity, electromagnetic hypersensitivity, chronic Lyme disease, and so on), which evidently offer a “cause” and sometimes a “meaning” to the symptoms, but also tend to isolate the “victims” and often determine hostile patient–doctor relationships (57). In no event does a diagnosis of fibromyalgia, for example, dispense the doctor from searching for physical or psychiatric differential diagnoses, from compiling the list of the multiple contributions to the disorder (somatic, psychological, behavioral, or other), or to carefully explore the representations of the “disease” (including the representations of the label chosen: does this name convey the meaning of an “imaginary illness?” of a mental illness? of a “cover-up” diagnosis to hide the doctor's ignorance? a prognosis of incurability or, conversely, of benignity?). Nevertheless, the doctor should also attempt to create, with the patient's participation, an explanatory model that is relatively coherent and includes personal details such as, for example, a background of childhood abuse as a vulnerability factor; an acute infection as a triggering factor; and the core mechanisms of central sensitization of pain, physical deconditioning due to prolonged rest, poor sleep quality, over-focusing on the symptoms induced by the fear of severe illness and complementary investigations, anger caused by a lack of recognition, and insulting attitudes of certain physicians as perpetuating factors, which create ever-worsening vicious circles. We can therefore say that one name is not enough; in fact, being simultaneously “precise and wrong,” it could even be dangerous (2). The causality of functional symptoms is, by necessity, made up of many factors and varies from person to person. By exploring the experience and representations of the patient, the doctor can in his turn put forward his own descriptive or mechanistic metaphors, engaged with the patients in creating an interpretation of their disorder that can itself have a therapeutic effect (4, 16, 53, 54, 56, 58, 59).
How could PCA might be a solution to the core issues posed by functional distress listed in the first part of this article? I argue that PCA offers the opportunity of explicitly discussing with the patient these problematic issues, taking account of his/her point of view. As examples, about the issues of doctors' and patients' discomfort with unexplained symptoms and management of uncertainty (points 1.1 and 1.2), the doctor may acknowledge that he/she is at unease with not having a simple explanation for the symptoms and that he/she shares with the patient (in part) the fear of missing a rare or atypical medical disorder. He/she can address explicitly the issue of the suffering experienced by the patient due to the lack of explication/medical legitimacy for his/her symptoms. Does the patient feel he/she has to “prove” that he/she is genuinely ill? Concerning the issue of reassurance and complementary medical workout (point 1.3), the doctor should explicitly enquire about the patient's experience and understanding of the process of “ruling out” organic causes for the symptoms. Does the patient feel actually reassured by negative findings, or does he/she feel that this was just not the right test or the right specialist? Has his/her anxiety been soothed or aggravated by the medical investigations? With regard to the traps of nosology (point 1.4), the problems with the words used to give account of the situation can also be explicitly addressed with the patient (see above). Are the diagnoses of “somatoform disorder,” “fibromyalgia,” “bodily distress disorder,” and so on, understandable? Which of these terms are felt as insulting? Does the patient feel that they mean that “it is all in the head?” Finally (point 1.5), the doctor should also address explicitly the issue of dualism and legitimacy of symptoms with the patient. How does the patient view mind–body relationships? Does accepting a “psychosomatic” explanation mean that the patient is “responsible” for his/her symptoms? Examples of wording that may prove useful can be found in the Appendix.
Although the scope of this paper is primarily a medical one, with emphasis on doctor–patient communication in primary and specialized (non-psychiatric) care, it must be stressed that evidence-based psychological treatments of functional disorders exist (21, 60, 61). However, in many countries such as France, functional somatic disorders remain under recognized and undertreated, the clinical reality being often characterized by unstructured use of specialized somatic care, resulting in high costs (62). Barriers to diagnosis and treatment of functional somatic syndromes and bodily distress in primary care are numerous (63), and we have stressed only some of them. Furthermore, in some countries, many psychiatrists and psychologists feel uncomfortable with somatic symptoms and syndromes, may be unwilling to take care of patients often considered as “difficult” and frustrating, or are unaware of published guidelines and specific psychotherapeutic techniques, while specialized treatment centers for patients with FFS are rare or inexistent. Then, one of the major challenges to improve the management of functional somatic syndromes is to get patients into treatment.
PCA can help overcome barriers to psychological treatment for functional somatic symptoms in several ways. PCA requires a deep enquiry on patients' attributions and expectations, which is the starting point for cognitive restructuring and “reattribution” techniques used in cognitive behavioral therapies (CBTs) for somatoform disorders. Practicing PCA means being aware of patients' beliefs and expectations and of their willingness to offer or accept psychosomatic explanation, based on their previous experiences with health care providers, for instance. PCA also allows the inclusion of patients' idioms in the discussion about illness explanations (63), and the crafting of shared metaphors may help to engage them in treatment. Beyond beliefs and attributions, PCA explicitly addresses the patients' emotional correlates of, and response to, physical symptoms, thus opening the door to emotion regulation training as an enrichment of CBT for MUS, whose efficacy remains overall moderate (64).
Although PCA is nothing new (the 60-year-old seminal work of Michael Balint having been quoted on purpose), this paper argues that its actual practice in clinical encounters with patients is a necessary condition for the management of functional symptoms and bodily distress. Its focus on illness, as the lived experience of symptoms of an individual patient and the idiosyncratic fears, expectations and feelings attached to them, allows the shift from the traditional disease perspective of biomedicine, which invariably leads to unhelpful conflicts of attribution, uncertainty-driven anxiety, distrust and frustration on both sides, as far as organic disorders have been reasonably ruled out or properly treated. PCA allows a therapeutic alliance to occur when the sociomoral issues of responsibility and blame are explicitly addressed and discussed with the patient (and at times with his/her family or significant others). When listened to carefully, most “somatizing” patients offer metaphors and sketches of explanations for their symptoms, on which doctors can help construct a shared model of psychosomatic entanglement contributing to the genesis of symptoms as predisposing, triggering, or perpetuating factors.
Functional symptoms and syndromes and “medically unexplained” or “psychosomatic” problems remain a blind spot of medicine. In a world of biomedically oriented medical education, a reminder of the person-centered approach seems at time mandatory. Of course, PCA should be learned as a set of clinical skill and not only as a theoretical framework. Much remains to be done within graduate and post-graduate medical education to effectively implement PCA in the management of bodily distress, an overlooked public health problem. However, this might not be enough. Since crucial moral issues are at stake with such conditions, medical education (especially within that field) should move, beyond competencies, to the development of a practical wisdom (phronesis), which link the knowledge and skills of biomedical and clinical science to moral orientations that addresses human interests in the practice of medicine (65).
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The author confirms being the sole contributor of this work and has approved it for publication.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.585495/full#supplementary-material
1. Cathébras P. La fibromyalgie doit-elle passer le siècle? [Should fibromyalgia survive the century?]. Rev Med Interne. (2000) 21:577–9. doi: 10.1016/S0248-8663(00)80001-6
2. Cathébras P. Qu'y a-t-il dans un nom? A propos des anciens et nouveaux noms de la fatigue chronique [What's in a name? New and older labels for chronic fatigue]. Rev Med Interne. (2016) 37:791–5. doi: 10.1016/j.revmed.2016.10.002
3. Creed F, Henningsen P, Fink P editors. Medically Unexplained Symptoms, Somatisation and Bodily Distress. Developing Better Clinical Services. Cambridge: Cambridge University Press (2011).
4. Ranque B, Nardon B. Prise en charge des symptômes médicalement inexpliqués en médecine interne: un paradigme de la relation médecin-malade en situation d'incertitude [Medically unexplained symptoms' care in internal medicine: a paradigm of doctor-patient relationship in situation of uncertainty]. Rev Med Interne. (2017) 38:458–66. doi: 10.1016/j.revmed.2016.12.005
5. Biderman A, Yeheskel A, Herman J. Somatic fixation: the harm of healing. Soc Sci Med. (2003) 56:1135–8. doi: 10.1016/S0277-9536(02)00108-9
6. Ring A, Dowrick CF, Humphris GM, Davies J, Salmon P. The somatizing effect of clinical consultation: what patients and doctors say and do not say when patients present medically unexplained symptoms. Soc Sci Med. (2005) 61:1505–15. doi: 10.1016/j.socscimed.2005.03.014
7. Simpkin AL, Schwartzstein RM. Tolerating uncertainty: the next medical revolution? New Engl J Med. (2016) 375:1713–5. doi: 10.1056/NEJMp1606402
8. Kassirer JP. Our stubborn quest for diagnostic certainty. A cause of excessive testing. N Engl J Med. (1989) 320:1489–91. doi: 10.1056/NEJM198906013202211
9. Stone J, Carson A, Duncan R, Coleman R, Roberts R, Warlow C, et al. Symptoms “unexplained by organic disease” in 1144 new neurology out- patients: how often does the diagnosis change at follow-up? Brain. (2009) 132:2878–88. doi: 10.1093/brain/awp220
10. Eikelboom EM, Tak LM, Roest AM, Rosmalen JGM. A systematic review and meta-analysis of the percentage of revised diagnoses in functional somatic symptoms. J Psychosom Res. (2016) 88:60–7. doi: 10.1016/j.jpsychores.2016.07.001
11. Ring A, Dowrick CF, Humphris GM, Salmon P. Do patients with unexplained physical symptoms pressurize general practitioners for somatic treatment? A qualitative study. BMJ. (2004) 328:1057–60. doi: 10.1136/bmj.38057.622639.EE
12. Salmon P, Humphris GM, Ring A, Davies JC, Dowrick CF. Why do primary care physicians propose medical care to patients with medically unexplained symptoms? A new method of sequence analysis to test theories of patient pressure. Psychosom Med. (2006) 68:570–7. doi: 10.1097/01.psy.0000227690.95757.64
13. Cathébras P. Rassurer: un acte médical essentiel mais plus difficile qu'il n'y parait, aux conséquences socio-économiques négligées [Reassurance: an essential but difficult medical task with neglected social and economic outcomes]. Rev Med Interne. (2004) 35:285–8. doi: 10.1016/j.revmed.2013.11.005
14. Balint M. The Doctor, his Patient and the Illness. 2nd ed. London: Churchill Livingstone (1963).
15. Rolfe A, Burton C. Reassurance after diagnostic testing with a low pretest probability of serious disease: systematic review and meta-analysis. JAMA Intern Med. (2013) 173:407–16. doi: 10.1001/jamainternmed.2013.2762
16. Stone J, Wojcik W, Durrance D, Carson A, Lewis S, MacKenzie L, et al. What should we say to patients with symptoms unexplained by disease? The “number needed to offend”. BMJ. (2002) 325:1449–50. doi: 10.1136/bmj.325.7378.1449
17. Lipowski ZJ. Somatization: the concept and its clinical application. Am J Psychiatry. (1988) 145:1358–68. doi: 10.1176/ajp.145.11.1358
19. Mayou R, Kirmayer LJ, Simon G, Kroenke K, Sharpe M. Somatoform disorders: time for a new approach in DSM-V. Am J Psychiatry. (2005) 162:847–55. doi: 10.1176/appi.ajp.162.5.847
20. Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: one or many? Lancet. (1999) 354:936–9. doi: 10.1016/S0140-6736(98)08320-2
21. Henningsen P, Zipfel S, Sattel H, Creed F. Management of functional somatic syndromes and bodily distress. Psychother Psychosom. (2018) 87:12–31. doi: 10.1159/000484413
22. Fink P, Schröder A. One single diagnosis, bodily distress disorder, succeeded to capture 10 diagnostic categories of functional somatic syndromes and somatoform disorders. J Psychosom Res. (2010) 68:415–26. doi: 10.1016/j.jpsychores.2010.02.004
23. Burton C, Fink P, Henningsen P, Löwe B, Rief W, on behalf of the EURONET-SOMA Group. Functional somatic disorders: discussion paper for a new common classification for research and clinical use. BMC Medicine. (2020) 18:34. doi: 10.1186/s12916-020-1505-4
24. Nettleton S. “I just want permission to be ill”: towards a sociology of medically unexplained symptoms. Soc Sci Med. (2006) 62:1167–78. doi: 10.1016/j.socscimed.2005.07.030
25. Hadler NM. If you have to prove you are ill, you can't get well. The object lesson of fibromyalgia. Spine. (1996) 21:2397–400. doi: 10.1097/00007632-199610150-00021
26. Creed F. Exploding myths about medically unexplained symptoms. J Psychosom Res. (2016) 85:91–3. doi: 10.1016/j.jpsychores.2016.02.007
27. Balint E. The possibilities of patient-centered medicine. J Roy Coll Gen Pract. (1969) 17:269–76.
28. Engel G. The need for a new medical model: a challenge for biomedicine. Science. (1977) 196:129–36. doi: 10.1126/science.847460
29. Berquin A. Le modèle biopsychosocial: beaucoup plus qu'un supplément d'empathie [The biopsychosocial model: much more than additional empathy]. Rev Med Suisse. (2010) 6:1511–3.
30. Kleinman AM, Eisenberg L, Good B. Culture, illness and care. Ann Intern Med. (1978) 88:251–8. doi: 10.7326/0003-4819-88-2-251
31. Stewart M, Brown JB, Weston WW, McWilliams CL, Freeman TR (editors). Patient-Centered Medicine: Transforming the Clinical Methods. Thousand Oaks, CA: Sage (1995).
32. Charon R. Narrative medicine. A model for empathy, reflection, profession, and trust. JAMA. (2001) 286:1897–902. doi: 10.1001/jama.286.15.1897
33. Anonymous. What is Patient-Centered Care? Available online at: https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0559 (accessed January 09, 2021).
34. Cushing AM. Learning patient-centred communication: the journey and the territory. Patient Educ Couns. (2015) 98:1236–42. doi: 10.1016/j.pec.2015.07.024
35. Platt FW, Gaspar DL, Coulehan JL, Fox L, Adler AJ, Weston WW, et al. “Tell me about yourself”: the patient-centered interview. Ann Intern Med. (2001) 134:1079–85. doi: 10.7326/0003-4819-134-11-200106050-00020
36. Nelson WA, Forcino RC, Elwyn G. Patient-centered organizational statements: merely rhetoric? A survey of health care leaders. Health Care Manag (Frederik). (2017) 4:342–6. doi: 10.1097/HCM.0000000000000186
37. Santana MJ, Manalili K, Jolley RJ, Zelinski S, Quan H, Lu M. How to practice person-centred care: a conceptual framework. Health Expect. (2018) 21:429–40. doi: 10.1111/hex.12640
38. Mead N, Bowers P. Patient-centred consultations and outcome in primary care: review of the literature. Patient Educ Couns. (2002) 48:51–61. doi: 10.1016/S0738-3991(02)00099-X
39. Street RL. How clinician-patient communication contributes to health improvement: modeling pathways from talk to outcome. Patient Educ Couns. (2013) 92:286–91. doi: 10.1016/j.pec.2013.05.004
40. McMillan SS, Kendall E, Sav A, King MA, Whitty JA, Kelly F, et al. Patient-centered approaches to health care: a systematic review of randomized controlled trials. Med Care Res Rev. (2013) 70:567–96. doi: 10.1177/1077558713496318
41. Jagosh J, Boudreau JD, Steinert Y, MacDonald ME, Ingram L. The importance of listening from the patient's perspective: enhancing diagnosis, healing, and the doctor-patient relationship. Patient Educ Couns. (2011) 85:369–74. doi: 10.1016/j.pec.2011.01.028
42. Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. (2000) 284:1021–7. doi: 10.1001/jama.284.8.1021
43. Stewart J, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, et al. The impact of patient-centered care on outcomes. Fam Pract. (2000) 49:796–804.
44. Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. (2011) 24:229–39. doi: 10.3122/jabfm.2011.03.100170
45. Forster HP, Schwartz J, DeRenzo E. Reducing legal risk by practicing patient- centered medicine. Arch Intern Med. (2002) 162:1217–9. doi: 10.1001/archinte.162.11.1217
46. Flores M, Glusman G, Brogaard K, Price ND, Hood L. P4 medicine: how systems medicine will transform the healthcare sector and society. Per Med. (2013) 10:565–76. doi: 10.2217/pme.13.57
47. Walker LS. Commentary: understanding somatic symptoms: from dualism to systems, diagnosis to dimensions, clinical judgment to clinical science. J Pediatr Psychol. (2019) 44:862–7. doi: 10.1093/jpepsy/jsz050
48. Vogt H, Ulvestad E, Eriksen TE, Getz L. Getting personal: can systems medicine integrate scientific and humanistic conceptions of the patient? J Eval Clin Pract. (2014) 20:942–52. doi: 10.1111/jep.12251
49. El-Alti L. Person centered care and personalized medicine: irreconcilable opposites or potential companions? Health Care Anal. (2019) 27:45–59. doi: 10.1007/s10728-017-0347-5
51. Zempleni A. La (maladie) et ses (causes). Introduction. [“Illness” and its “causes”. Introduction]. L'Ethnographie. (1985) 81:13–44.
52. Young A. Some implications of medical beliefs and practices for social anthropology. Am Anthropologist. (1976) 78:5–24. doi: 10.1525/aa.1976.78.1.02a00020
53. Salmon P. Conflict, collusion or collaboration in consultations about medically unexplained symptoms: the need for a curriculum of medical explanation. Patient Educ Couns. (2007) 67:246–54. doi: 10.1016/j.pec.2007.03.008
54. Epstein RM, Quill TE, McWhinney I. Somatization reconsidered: incorporating the patient's experience of illness. Arch Intern Med. (1999) 159:215–22. doi: 10.1001/archinte.159.3.215
55. Burbaum C, Stresing AM, Fritzsche K, Auer P, Wirsching M, Lucius-Hoen G. Medically unexplained symptoms as a threat to patients' identity? A conversation analysis of patients' reactions to psychosomatic attributions. Patient Educ Couns. (2010) 79:207–17. doi: 10.1016/j.pec.2009.09.043
56. Cournoyea M, Graham Kennedy A. Causal explanatory pluralism and medically unexplained physical symptoms. J Eval Clin Pract. (2014) 20:928–33. doi: 10.1111/jep.12238
57. Dumit J. Illnesses you have to fight to get: facts as forces in uncertain, emergent illnesses. Soc Sci Med. (2006) 62:577–90. doi: 10.1016/j.socscimed.2005.06.018
58. Kirmayer LJ, Groleau D, Looper KJ, Dao MD. Explaining medically unexplained symptoms. Can J Psychiatry. (2004) 49:663–72. doi: 10.1177/070674370404901003
59. Stone L. Explaining the unexplainable. Crafting explanatory frameworks for medically unexplained symptoms. Aust Fam Physician. (2011) 40:440–4.
60. Kleinstäuber M, Witthöft M, Hiller W. Efficacy of short-term psychotherapy for multiple medically unexplained physical symptoms: a meta-analysis. Clin Psychol Rev. (2011) 31:146–60. doi: 10.1016/j.cpr.2010.09.001
61. van Dessel N, den Boeft M, van der Wouden JC, Kleinstäuber M, Leone SS, Terluin B, et al. Non-pharmacological interventions for somatoform disorders and medically unexplained physical symptoms (MUPS) in adults. Cochrane Database Syst Rev. (2014) 11:CD011142. doi: 10.1002/14651858.CD011142
62. Kohlmann S, Löwe B, Shedden-Mora MC, on behalf of the EURONET-SOMA Group. Health care for persistent somatic symptoms across Europe: a qualitative evaluation of the EURONET-SOMA expert discussion. Front Psychiatry. (2018) 9:646. doi: 10.3389/fpsyt.2018.00646
63. Murray AM, Toussaint A, Althaus A, Löwe B. The challenge of diagnosing non-specific, functional, and somatoform disorders: a systematic review of barriers to diagnostic in primary care. J Psychosom Res. (2016) 80:1–10. doi: 10.1016/j.jpsychores.2015.11.002
64. Kleinstäuber M, Allwang C, Bailer J, Berking M, Brünahl C, Erkic M, et al. Cognitive behavioral therapy complemented with emotion regulation training for patients with persistent physical symptoms: a randomised clinical trial. Psychother Psychosom. (2018) 88:287–99. doi: 10.1159/000501621
Keywords: patient-centered medicine, functional somatic syndromes, bodily distress, psychosomatic, dualism, reassurance
Citation: Cathébras P (2021) Patient-Centered Medicine: A Necessary Condition for the Management of Functional Somatic Syndromes and Bodily Distress. Front. Med. 8:585495. doi: 10.3389/fmed.2021.585495
Received: 20 July 2020; Accepted: 10 March 2021;
Published: 27 April 2021.
Edited by:
Susanne Fischer, University of Zurich, SwitzerlandReviewed by:
Charlotte Markert, Justus Liebig University Giessen, GermanyCopyright © 2021 Cathébras. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pascal Cathébras, cGFzY2FsLmNhdGhlYnJhc0BjaHUtc3QtZXRpZW5uZS5mcg==; orcid.org/0000-0001-7570-3366
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.