
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Med. , 04 November 2020
Sec. Rheumatology
Volume 7 - 2020 | https://doi.org/10.3389/fmed.2020.588527
This article is part of the Research Topic Sarcoidosis – the great mimicker View all 12 articles
 Michael Manansala1*
Michael Manansala1* Christian Ascoli1
Christian Ascoli1 Ana Goico Alburquerque1
Ana Goico Alburquerque1 David Perkins1
David Perkins1 Mehdi Mirsaedi2
Mehdi Mirsaedi2 Patricia Finn1
Patricia Finn1 Nadera J. Sweiss1
Nadera J. Sweiss1Data on the clinical presentation and outcomes of sarcoidosis patients with coronavirus disease 19 (COVID-19) are scarce. In this case series, we identified 5 out of 238 sarcoidosis patients who are enrolled in an ongoing longitudinal observational study who developed COVID-19 during the study period and follow their clinical course. Four patients recovered completely, whereas one patient expired during hospital admission. Our preliminary experience suggests that African American patients with chronic sarcoidosis treated with disease-modifying anti-rheumatic drugs (DMARDs) or anti-tumor necrosis factor (TNF) therapy do not seem to be at increased risk of respiratory or life-threatening complications from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) compared with the general population, although at the present time, we advocate for maintaining a high level of vigilance and strict follow-up in this patient population.
The recent outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) responsible for severe acute respiratory syndrome (SARS) represents a source of concern for the management of patients with sarcoidosis (1). Within the realm of sarcoidosis, it has been shown that African Americans have 12 times the rate of age-adjusted mortality compared with similar Caucasian patients (2). This is compounded by the observation that African American patients are at disproportionately increased risk of mortality and morbidity from coronavirus disease 19 (COVID-19) (3). Data on COVID-19 in patients with sarcoidosis are scarce. Additionally, there is a concern that immunocompromised patients are at increased risk of mortality from COVID-19. Here, we report a case series describing the clinical course of five African American patients with sarcoidosis after infection with SARS-CoV-2.
We assessed patients with sarcoidosis care established at the University of Illinois of Chicago Bernie Mac STAR Clinic who are enrolled in an ongoing longitudinal observational study for SARS-CoV-2 infection during the period of March 12 to April 30, 2020. We identified five out of 238 patients (2.1%) with confirmed SARS-CoV-2 infection by PCR and clinical symptoms consistent with COVID-19 disease. Demographic and clinical data were collected.
We identified 5 out of 238 sarcoidosis patients who were infected with SARS-Cov-2 during the study period. All patients were of African American descent. The most common presenting symptom was cough. One patient had an atypical presentation of gastrointestinal discomfort and diarrhea. Four patients recovered completely despite having comorbidities and being on chronic immunosuppression. Two of the five patients did not receive any additional treatment for COVID-19. Three of the five patients received hydroxychloroquine (HCQ) and azithromycin for treatment for COVID-19. No changes were made to the patients' current immunosuppressive regimen. They also did not experience significant relapses of sarcoidosis from the time of COVID-19 diagnosis to date. One patient died after developing a likely thromboembolic event during hospitalization in the intensive care unit (ICU). Additional clinical characteristics of these patients are summarized in Table 1. The clinical data, including symptoms, laboratory data, and outcomes, are included in Table 2.
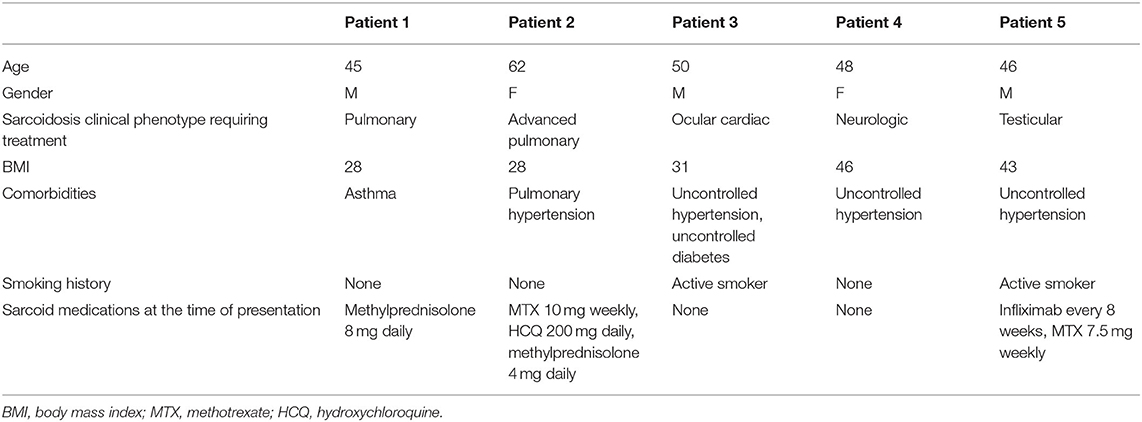
Table 1. Clinical characteristics of five African American sarcoidosis patients with confirmed COVID-19.
The case fatality rate of COVID-19 is estimated to be 1–6% in the general population (4). Currently, the Center for Disease Control and Prevention (CDC) lists several risk factors for severe COVID-19, including immunocompromised status (5). However, preliminary data from an observational study of 320 Italian patients on immunosuppressive therapy for rheumatoid arthritis did not show increased risk of respiratory or life-threatening complications from SARS-CoV-2 compared with the general population (6). Indeed, it has been postulated that the pathogenesis of severe COVID-19 disease is in large part due to virally driven hyperinflammation that is perpetuated by the host immune response (7–9). Analysis from a cohort of COVID-19 cases from Wuhan, China revealed that patients requiring ICU had increased levels of pro-inflammatory cytokines (10).
Our findings do not provide any conclusions on the incidence rate of SARS-CoV-2 infection in patients with sarcoidosis, nor on the severity or overall outcome of immunocompromised sarcoidosis patients affected by COVID-19 disease. However, our preliminary experience suggests that African American patients with chronic sarcoidosis treated with disease-modifying anti-rheumatic drugs (DMARDs) or anti-tumor necrosis factor (TNF) therapy do not seem to be at increased risk of respiratory or life-threatening complications from SARS-CoV-2 compared with the general population. Better understanding of the implications of COVID-19 in patients with sarcoidosis and the effects of immunosuppressive therapies on COVID-19 infection outcome is urgently needed to guide clinicians in patient care. At the present time, we advocate for maintaining a high level of vigilance and strict follow-up in this patient population, including the exclusion of superimposed infections.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
NS identified patients of interest within the cohort. MMa wrote the manuscript with assistance from CA, AA, DP, PF, and MMi. All authors contributed to the article and approved the submitted version.
Funding for publication of this article was provided by the Bernie Mac Foundation STAR Clinic.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Sweiss NJ, Korsten P, Syed HJ, Syed A, Baughman RP, Yee AMF, et al. When the game changes: Guidance to adjust sarcoidosis management during the COVID-19 pandemic. Chest. (2020) 158:892–5. doi: 10.1016/j.chest.2020.04.033
2. Mirsaeidi M, Machado RF, Schraufnagel D, Sweiss NJ, Baughman RP. Racial difference in sarcoidosis mortality in the United States. Chest. (2015) 147:438–49. doi: 10.1378/chest.14-1120
3. Chowkwanyun M, Reed AL. Racial health disparities and COVID-19 — caution and context. New Engl J Med. (2020) 383:201–20. doi: 10.1056/nejmp2012910
4. Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID-19 based on current evidence. J Med Virol. (2020) 92:548–51. doi: 10.1002/jmv.25722
5. CDC.People who are at Higher Risk for Severe Illness. (2020). Available online at: www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html (accessed May 5, 2020)
6. Monti S, Balduzzi S, Delvino P, Bellis E, Quadrelli VA, Montecucco C. Clinical course of COVID-19 in a series of patients with chronic arthritis treated with immunosuppressive targeted therapies. Ann Rheum Dis. (2020) 79:667–8. doi: 10.1136/annrheumdis-2020-217424
7. Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘Cytokine Storm' in COVID-19. J Infect. (2020) 80:607–13. doi: 10.1016/j.jinf.2020.03.037
8. Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, et al. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. (2020) 27:1451–4. doi: 10.1038/s41418-020-0530-3
9. Haberman R, Axelrad J, Chen A, Castillo R, Yan D, Izmirly P, et al. COVID-19 in Immune-Mediated Inflammatory Diseases — Case Series from New York. N Engl J Med. (2020) 383:85–8. doi: 10.1056/nejmc2009567
Keywords: sarcoidosis, COVID- 19, immunosuppression, DMARDs, African American (AA), SAR-CoV-2
Citation: Manansala M, Ascoli C, Alburquerque AG, Perkins D, Mirsaedi M, Finn P and Sweiss NJ (2020) Case Series: COVID-19 in African American Patients With Sarcoidosis. Front. Med. 7:588527. doi: 10.3389/fmed.2020.588527
Received: 29 July 2020; Accepted: 05 October 2020;
Published: 04 November 2020.
Edited by:
Xinhua Yu, Research Center Borstel (LG), GermanyReviewed by:
Jing Yuan, Children's Hospital of Capital Institute of Pediatrics, ChinaCopyright © 2020 Manansala, Ascoli, Alburquerque, Perkins, Mirsaedi, Finn and Sweiss. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael Manansala, bW1hbmFuM0B1aWMuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.