- 1Department of Internal Medicine and Healthcare System Gangnam Center, Seoul National University Hospital, Seoul, South Korea
- 2Department of Public Health Sciences, Seoul National University, Seoul, South Korea
Backgrounds: Depression and anxiety disorder are frequently seen in patients with nonalcoholic fatty liver disease (NAFLD). However, the associations between mood disorders and NAFLD have not been fully evaluated. In this study, we investigated the relationship between NAFLD and depression or anxiety in a Korean population.
Methods: We conducted a retrospective cross-sectional study that included subjects who underwent abdominal ultrasonography and completed a symptom questionnaire for a routine health check-up. NAFLD was diagnosed and graded according to the ultrasonography findings. Depression and anxiety were assessed using the Beck Depression Inventory and State-Trait Anxiety Inventory, respectively.
Results: Among the total of 25,333 subjects, the mean age was 47 years (men, 56.2%), and the prevalence rate of NAFLD was 30.9%. In the multivariate analysis, NAFLD showed a significant association with depression [adjusted odds ratio (OR) 1.43 and 95% confidence interval (CI) 1.14–1.80, p = 0.002] in women. Severe NAFLD significantly correlated with state anxiety and trait anxiety (adjusted OR 1.84 and 95% CI 1.01–3.37, p = 0.047 and adjusted OR 2.45 and 95% CI 1.08–4.85, p = 0.018, respectively) in women.
Conclusions: There was a higher tendency of women with NAFLD to suffer from depression with increase in steatosis, and severe stage of steatosis was significantly associated with anxiety in the female compared to non-NAFLD. Understanding the association between NAFLD and mood disorders may have clinical implications for reducing the prevalence of comorbidities.
Key points
• Depression and anxiety disorder are frequently seen in patients with nonalcoholic fatty liver disease (NAFLD). However, the associations between mood disorders and NAFLD have not been fully evaluated.
• NAFLD was significantly associated with depression, and severe stage of steatosis was significantly associated with anxiety in women compared to non-NAFLD.
• These findings provide new insight in understanding the association between NAFLD and mood disorders.
Introduction
Nonalcoholic fatty liver disease (NAFLD) is the most common cause of chronic liver disease worldwide, with increasing prevalence of up to 20–30% (1). Although NAFLD is generally a benign condition, some may progress to nonalcoholic steatohepatitis (NASH), fibrosis, and cirrhosis (2). Hepatic steatosis is commonly associated with various metabolic conditions, including cardiovascular disease (3), diabetes (4), chronic kidney disease (5), and colorectal cancer (6). In addition, NAFLD has been associated with an increased prevalence of psychological conditions such as depression and anxiety. A previous study reported that the prevalence rates of lifetime major depressive disorder (MDD) and generalized anxiety disorder were more increased in patients with NASH with more advanced histological features compared to controls (7).
Major depression is a common, recurrent disease leading to decreased quality of life, disability (8), and mortality (9). The lifetime prevalence of major depressive episode is estimated from 3 to 29.9% (10). Depression has been associated with cardiovascular diseases (11) and metabolic syndrome (12), with increased predisposition for NAFLD, suggesting shared pathogenesis of insulin resistance (13). In particular, a recent study based on US claim data has shown that depression was independently associated with NAFLD (14). In addition, generalized anxiety disorder is one of the most common anxiety disorders (15), and anxiety disorder is associated with hyperglycemia in patients with diabetes (16). This result suggests that there is a close link between anxiety and metabolic disease.
Therefore, we hypothesized that depression and anxiety disorder would be related to NAFLD and investigated the relationship between NAFLD and anxiety or depression in Korean subjects who participated in health check-ups.
Methods
Study Population
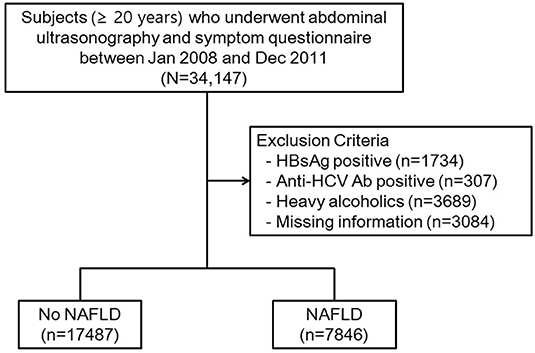
We performed a retrospective cross-sectional study that included subjects who underwent routine health check-up at the Seoul National University Hospital Healthcare System Gangnam Center between January 2008 and December 2011. Health examination has recently become popular in Korea because a thorough medical checkup can be performed in a few hours, and the majority of referred hospitals in Korea are now equipped with a Healthcare Center to provide such health check-ups. The subjects (age ≥ 20 years) voluntarily attended a general health check-up, while others were supported by their employers. They were mostly free of symptoms and voluntarily underwent examinations including abdominal ultrasonography and blood samplings and completed a symptom questionnaire on the same day. A schematic protocol of the study design is illustrated in Figure 1. Among the 34,147 subjects, 5,730 were excluded for potential cause of chronic liver disease, including hepatitis B virus positivity in 1,734 subjects, anti-hepatitis C virus antibody positivity in 307 subjects, and 3,689 subjects with significant alcohol consumption (>30 g/day for men and >20 g/day for women) (17). Additionally, 3,084 subjects were excluded because of missing data. The total number of eligible participants was 25,333.
The study protocol was approved by the Institutional Review Board of Seoul National University Hospital (1912–111–1089) and conformed to the ethical guidelines of the World Medical Association Declaration of Helsinki. The requirement for informed consent from individual subjects was waived because we used de-identified secondary data.
Clinical and Biochemical Evaluations
Study data consisted of medical information based on a self-administered questionnaire and anthropometric and laboratory measurements, as described previously (18). Briefly, height and body weight were measured using a digital scale. The body mass index (BMI) was calculated as weight (kg)/height2 (m2). Waist circumference (WC) was measured by a well-trained person, at the midpoint between the lower costal margin and the iliac crest. Based on smoking status, subjects were categorized as smoker (former or current smoker) or never-smoker. Based on alcohol consumption, subjects were categorized as alcohol user or nonuser (does not drink any alcohol). Diabetes was defined as fasting glucose levels ≥126 mg/dl and/or treatment with an oral hypoglycemic agent or insulin. Systolic blood pressure and diastolic blood pressure were each measured twice, and their mean values were reported. All subjects were fasted for at least 12 h prior to blood sampling; aspartate aminotransferase (AST), alanine aminotransferase (ALT), total cholesterol, triglyceride, and high-density lipoprotein (HDL) cholesterol were measured.
Evaluation of the State of Anxiety and Depression
The State-Trait Anxiety Inventory (STAI) scale was used to assess the level of anxiety in all subjects (19). The STAI is a well-known psychological instrument consisting of two self-report rating scales with 20 items each, for the measurement of two types of anxiety: state anxiety (how one feels at the moment, STAI-X1) and trait anxiety (how one generally feels, STAI-X2). Each item is rated between 1 and 4 depending on the frequency of target complaints (never, sometimes, often, and always), and overall scores are obtained by summing the ratings for the items (range, 20–80). We considered subjects showing moderate-to-severe state or trait anxiety by using a cut-off value of STAI-X1 ≥ 57 or STAI-X2 ≥ 59, respectively (18).
The depression status of subjects was evaluated using the Beck Depression Inventory (BDI) scale, which is one of the most commonly used self-report instruments designed to detect and measure the severity of depression in the general population (20). The BDI consists of 21 items describing symptoms of and attitudes regarding depression, and each item is rated from 0 (not at all) to 3 (extreme form of each symptom). The total score ranges from 0 to 63; the higher the score, the greater the degree of depression. By using the cutoff value of 15, subjects were classified as having no-to-mild depression (BDI < 15) or moderate-to-severe depression (BDI ≥ 15) (18).
Diagnosis of NAFLD
Hepatic ultrasonography (Acuson Sequoia 512; Siemens, Mountain View, CA) was performed to diagnose fatty liver by experienced radiologists who were unaware of the clinical information of the subjects (21). Fatty liver was diagnosed based on characteristic ultrasonographic findings consistent with a “bright liver” and evident contrast between hepatic and renal parenchyma, focal sparing, vessel blurring, and narrowing of the lumen of the hepatic veins (22). We graded the stage of steatosis based on ultrasonographic findings: mild fatty liver as a slight diffuse increase in bright homogeneous echoes in the hepatic parenchyma and normal visualization of the diaphragm and hepatic and portal borders; moderate fatty liver as a diffuse increase in bright echoes in the hepatic parenchyma with slightly impaired appearance of intrahepatic vessels and the diaphragm; and severe fatty liver as a marked increase in bright echoes with poor or no visualization of intrahepatic vessel borders, the diaphragm, and the posterior right lobe of the liver (22).
Statistical Analyses
Data are presented as the mean ± standard deviation for normally distributed continuous variables and as proportions for categorical variables. The Student t test and analysis of variance were used to analyze continuous variables, and the differences between nominal variables were compared with the chi-square test. Differences in anxiety or depression levels among the stages of steatosis were analyzed using one-way analysis of variance (ANOVA) with Tukey's honestly significant difference post hoc analysis. A logistic regression analysis was utilized to analyze the association of NAFLD and the stage of steatosis with depression or anxiety after adjusting for potential confounders. Among variables with a p value of <0.05 in univariate analyses, those with clinical importance were subjected to multivariate analyses. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA) and R version 3.2.3 (The R Foundation for Statistical Computing, Vienna, Austria, http://www.Rproject.org). p values of <0.05 were considered statistically significant.
Results
Baseline Characteristics of the Study Population
Among the total of 25,333 subjects, the mean age was 47 years, and men comprised 56.2%. The prevalence rate of NAFLD was 30.9%. The subjects with NAFLD were divided into three groups based on their ultrasonographic findings of steatosis. To rule out the effects of gender, we stratified the population according to gender. The baseline characteristics of the male participants are shown in Table 1. NAFLD was more frequently observed in people who were older and smokers. Prevalence of diabetes was significantly higher in subjects with NAFLD. In addition, most of the anthropometric and laboratory variables (including BMI, WC, systolic or diastolic blood pressure, AST, ALT, total cholesterol, triglyceride, and HDL-cholesterol) were less metabolically favorable in subjects with NAFLD (p < 0.001). The prevalence rates of depression and anxiety were not significantly different in the NAFLD and control groups.
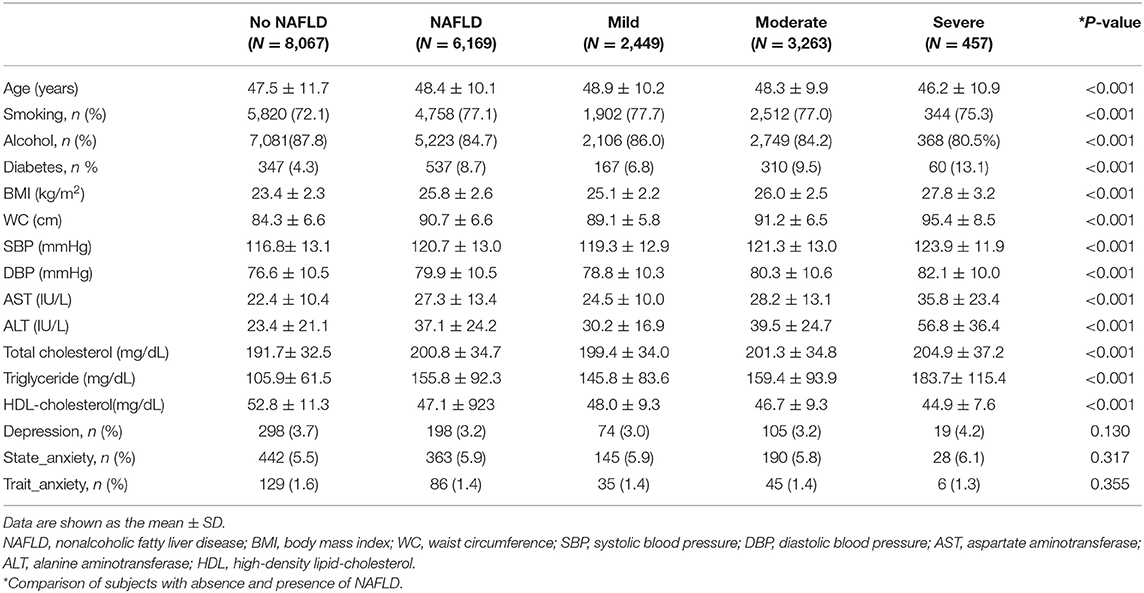
Table 1. Comparison of baseline characteristics according to nonalcoholic fatty liver disease in males.
In the female group, NAFLD was more frequently observed in people who were older and never-smokers. Other baseline characteristics were almost similar to those of men except for the prevalence rates of depression which was higher in the NAFLD group compared to the control group (Table 2). Figure 2 shows the scores of depression according to the stage of steatosis. The BDI score was significantly higher in the severe NAFLD group compared to the no-NAFLD group (7.2 ± 5.9 vs. 6.3 ± 5.5, p = 0.031). The effect sizes of the differences were provided in the Supplementary Table 1.
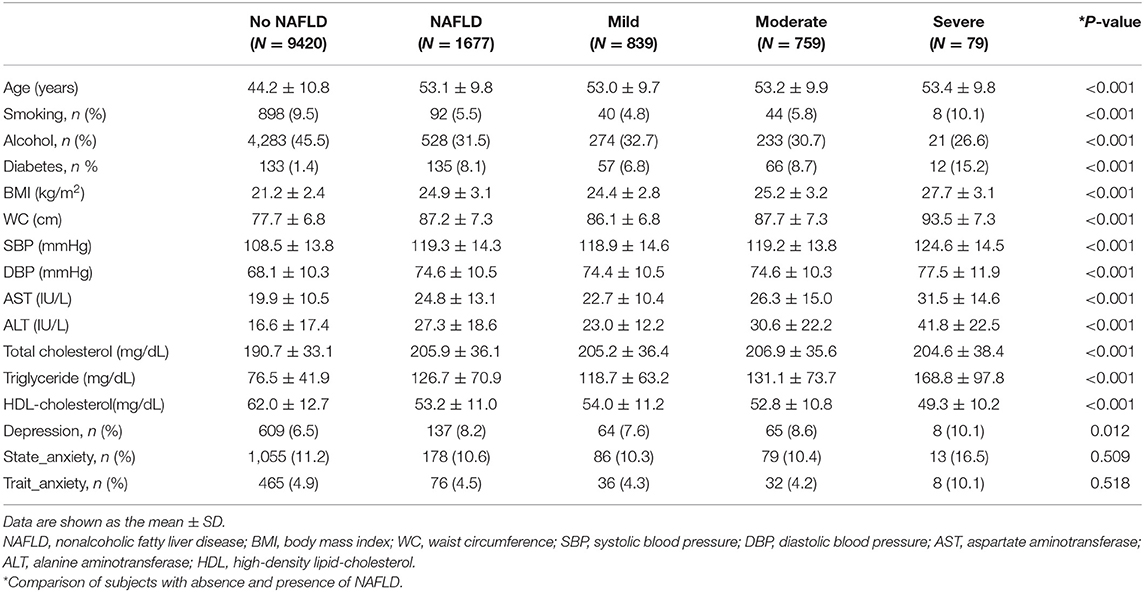
Table 2. Comparison of baseline characteristics according to nonalcoholic fatty liver disease in females.
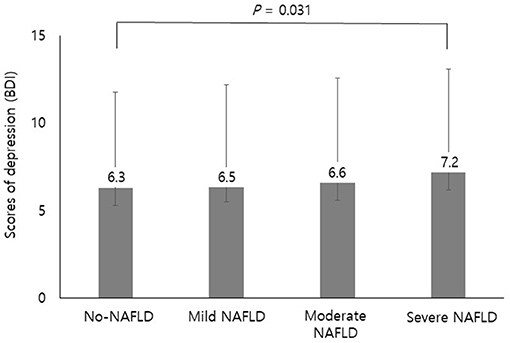
Figure 2. Scores of depression according to the stage of steatosis. The BDI score was significantly higher in the severe NAFLD group compared to the no-NAFLD group (7.2 ± 5.9 vs. 6.3 ± 5.5). Differences in depression levels among the stages of steatosis were analyzed using one-way ANOVA with Tukey's honestly significant difference post hoc analysis. BDI, Beck Depression Inventory; NAFLD, nonalcoholic fatty liver disease.
Risk of Depression and Anxiety With NAFLD
We investigated the relationship between depression or anxiety and NAFLD. In the univariate analysis, the presence of NAFLD had no association with depression. Regarding anxiety, the presence of NAFLD showed a significant association with state anxiety. NAFLD was associated with a 12% increase in the risk of state anxiety [odds ratio (OR) 1.12, 95% confidence interval (CI) 1.00–1.25]. When we adjusted for age, sex, diabetes, systolic and diastolic pressure, and smoking, the statistical significance has disappeared. In addition, the presence of NAFLD had no significant association with trait anxiety (Table 3).
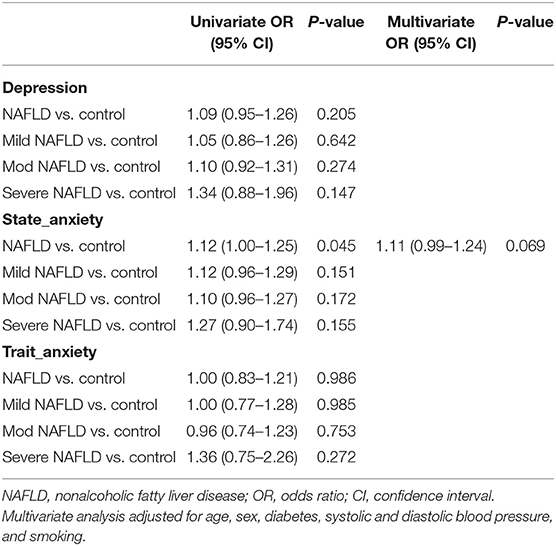
Table 3. Univariate and multivariate analyses of the risk for depression or anxiety with vs. without NAFLD.
Next, we performed stratified analysis according to gender to exclude the influence of gender. In the univariate model, the presence of NAFLD showed a significant association with depression. NAFLD was associated with a 44% increase in the risk of depression (OR 1.44, 95% CI 1.17–1.76) in women. After adjusting for age, BMI, alcohol, diabetes, and smoking, the multivariate analysis revealed that the presence of NAFLD still showed a significant association with depression, suggesting that NAFLD has an independent association with the risk for depression (OR 1.43, 95% CI, 1.14–1.80). Although there was no statistical significance, there was a trend of increasing risk of depression according to the stage of steatosis in a dose-dependent manner (OR 1.35, 95% CI, 1.00–1.78; OR 1.52, 95% CI, 1.12–2.03; and OR 1.75, 95% CI, 0.76–3.56, mild, moderate, and severe, respectively; Table 4).
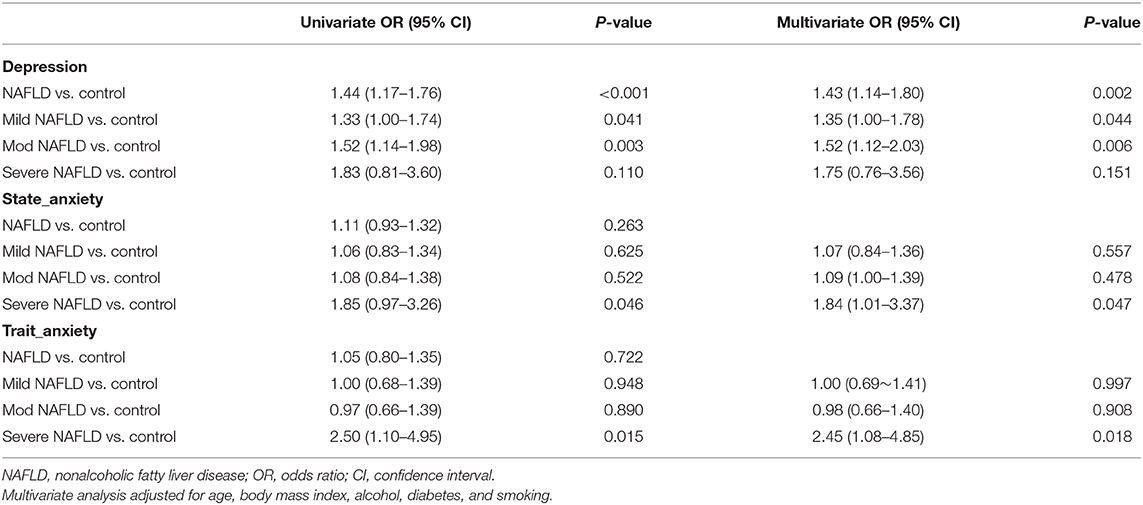
Table 4. Univariate and multivariate analyses of the risk for depression or anxiety in women with vs. without NAFLD.
Regarding anxiety, the presence of NAFLD had no significant association with anxiety. However, the stage of steatosis showed significant associations with both state anxiety and trait anxiety (severe NAFLD, both p < 0.05), and these associations remained significant after adjusting for age, BMI, smoking, alcohol, and diabetes (adjusted OR 1.84 and 95% CI 1.01–3.37, p = 0.047 and adjusted OR 2.45 and 95% CI 1.08–4.85, p = 0.018, respectively) in women. When we performed analysis in male subjects with NAFLD, the associations were not significant (data not shown).
Discussion
In the present study, there was a trend of increasing risk of depression according to the stage of steatosis in a dose-dependent manner in women compared with the non-NAFLD group, even after adjusting for confounding factors. In addition, severe stage of steatosis was significantly associated with state and trait anxiety in women.
These findings are in agreement with previous results showing the association between NAFLD and depression. A previous study with biopsy-proven NAFLD patients showed that more severe histological steatosis and higher NAFLD activity score were found in NAFLD patients with MDD than in those without MDD (23). Another study performed in Japan showed that depression was associated with more severe hepatocyte ballooning in pathology in patients with NAFLD (24). Although these findings were strengthened based on histological diagnosis, they are limited in their small sample size. In a study based on US claim data, those with depression were 1.6- to 2.2-fold more likely to have NAFLD compared to subjects without depression (14). A recent study based on a large Korean population showed the dose-dependent pattern of the relationship between the risk for depression and the ultrasonographically graded severity of NAFLD (25). Unlike our results, the significant association was found especially in men in the previous study, and these different results may be due to the heterogeneous study population, including the mean age of the subjects (40 vs. 47 years) and the prevalence of depression (10.6 vs. 4.7%), and the different definitions regarding depression, which were based on the Center for Epidemiological Studies-Depression scale. Regarding anxiety, few studies have evaluated the association with NAFLD. A previous study based on patients with biopsy-proven NAFLD showed that anxiety tended to be associated with less hepatocyte ballooning; however, there was no significant association between anxiety and portal fibrosis (24).
Previous studies have investigated the influence of mood disorder on the therapeutic effect of liver disease. Tomeno et al. suggested that NAFLD patients with depression had poor response to standard treatment for NAFLD (23). A meta-analysis showed that psychological distress such as depression and anxiety was associated with mortality in chronic liver disease (26). Taken together, NAFLD patients with depression may experience worse clinical outcomes than those without; thus, active screening and appropriate treatment of depression may prevent the development or progression of NAFLD.
It is well known that there is gender difference in the prevalence of NAFLD and depression. While NAFLD is more common in men (1), depression is more prevalent in women (27). In our study, women had a prevalence of depression (6.7%) up to twice that of men (3.5%), whereas men had a higher prevalence of NAFLD (43.3%) than women (15.1%). Thus, we stratified the population according to gender, and the rate of individuals having both depression and NAFLD increased after adjusting for gender, resulting in a significant association between NAFLD and mood disorder only in women.
The pathogenesis underlying the association between NAFLD and depression or anxiety has not been fully elucidated. There are possible explanations for the close link between hepatic steatosis with insulin resistance and poor glycemic control, both of which have been associated with depression (28) or anxiety (16). The involvement of insulin signaling on brain mechanisms related to depression indicates that insulin resistance may be one of the main pathogenic drivers for NAFLD (29). In addition, increased inflammation markers (30) and pro-inflammatory cytokines, such as tumor necrosis factor-alpha and interleukin-6, in patients with mood disorders may offer another plausible explanation for the association of these mood disorders with NAFLD (31). Another line of evidence suggests the involvement of the serotonin pathway. Experimental murine models of NAFLD showed that serotonin played an important role in the pathogenesis of NASH. Additionally, the expression of monoamine oxidase-A, one of the main enzymes catalyzing monoamines such as serotonin, increased in patients with NASH (32).
The strengths of this study include the large sample size, which ensured the robustness of results, and the STAI scale, which was able to assess both types of anxiety, including trait or chronic anxiety, which reflects a person's permanent characteristics, and state or acute anxiety, which reflects a recent state (33).
There are several limitations in this study. First, due to its observational study design, the results need to be interpreted cautiously. The association between NAFLD and mood disorder may not imply causality. Further research with longitudinal study design is needed to clarify the causal relationship. Second, since depression or anxiety was defined based on the self-reporting questionnaire, there is the potential for over- or underreporting-related symptoms. Because the recommended cutoff points of BDI or STAI is not consistent among specific disease or populations (34–38), we used the cutoff values referring to previous study based on Korean population (18). Third, although liver biopsy is considered to be a gold standard for the diagnosis of NAFLD, it was assessed only by ultrasonography in this study. Thus, there may be a limitation of lack in accurate diagnoses for mild steatosis. And although the fibrosis was found to be a critical factor in mental health of NAFLD patients (39), we could not evaluate the fibrosis stage. In clinical practice, liver biopsy is not typically used in healthy subjects due to its invasiveness. Thus, radiographic techniques such as ultrasonography or magnetic resonance imaging are used for the diagnosis of NAFLD. Fourth, we could not assess the influence of the history of anti-depressant medications. Fifth, as a result of this study using the previous cohort (18), there is a limitation that there is no information on the history of hypertension. However, systolic and diastolic blood pressure were adjusted as variables in the multivariate analysis. Finally, because we could not exclude all patients that have drinking habit, there might be bias in the results.
In conclusion, NAFLD was significantly associated with depression in women, and severe NAFLD was significantly associated with anxiety in the female group compared to non-NAFLD. Understanding the association between NAFLD and mood disorders may have clinical implications for reducing the prevalence of comorbidities, and appropriate screening and active referrals for early treatment of depression may be suggested for patients with NAFLD.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board of Seoul National University Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
GC conceived the idea, determined the study design, collected the data, drafted and revised the manuscript. JC and SK collected the data, performed the statistical analysis and revised the manuscript. MK, JYa, and JYi collected and reviewed the data, and revised the manuscript. BP performed the statistical analysis. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2020.585618/full#supplementary-material
References
1. Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. (2004) 40:1387–95. doi: 10.1002/hep.20466
2. Cohen JC, Horton JD, Hobbs HH. Human fatty liver disease: old questions and new insights. Science. (2011) 332:1519–23. doi: 10.1126/science.1204265
3. Wong VW, Wong GL, Yip GW, Lo AO, Limquiaco J, Chu WC, et al. Coronary artery disease and cardiovascular outcomes in patients with non-alcoholic fatty liver disease. Gut. (2011) 60:1721–7. doi: 10.1136/gut.2011.242016
4. Adams LA, Harmsen S, St Sauver JL, Charatcharoenwitthaya P, Enders FB, Therneau T, et al. Nonalcoholic fatty liver disease increases risk of death among patients with diabetes: a community-based cohort study. Am J Gastroenterol. (2010) 105:1567–73. doi: 10.1038/ajg.2010.18
5. Targher G, Bertolini L, Rodella S, Zoppini G, Lippi G, Day C, et al. Non-alcoholic fatty liver disease is independently associated with an increased prevalence of chronic kidney disease and proliferative/laser-treated retinopathy in type 2 diabetic patients. Diabetologia. (2008) 51:444–50. doi: 10.1007/s00125-007-0897-4
6. Wong VW, Wong GL, Tsang SW, Fan T, Chu WC, Woo J, et al. High prevalence of colorectal neoplasm in patients with non-alcoholic steatohepatitis. Gut. (2011) 60:829–36. doi: 10.1136/gut.2011.237974
7. Elwing JE, Lustman PJ, Wang HL, Clouse RE. Depression, anxiety, and nonalcoholic steatohepatitis. Psychosom Med. (2006) 68:563–9. doi: 10.1097/01.psy.0000221276.17823.df
8. Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. (2016) 388:1545–602. doi: 10.1016/S0140-6736(16)31678-6
9. Spijker J, Graaf R, Bijl RV, Beekman AT, Ormel J, Nolen WA. Functional disability and depression in the general population. Results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Acta Psychiatr Scand. (2004) 110:208–14. doi: 10.1111/j.1600-0447.2004.00335.x
10. Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. (2012) 21:169–84. doi: 10.1002/mpr.1359
11. Carney RM, Freedland KE. Depression and coronary heart disease. Nat Rev Cardiol. (2017) 14:145–55. doi: 10.1038/nrcardio.2016.181
12. Park SJ, Roh S, Hwang J, Kim HA, Kim S, Lee TK, et al. Association between depression and metabolic syndrome in korean women: results from the korean national health and nutrition examination survey (2007-2013). J Affect Disord. (2016) 205:393–9. doi: 10.1016/j.jad.2016.08.022
13. Winokur A, Maislin G, Phillips JL, Amsterdam JD. Insulin resistance after oral glucose tolerance testing in patients with major depression. Am J Psychiatry. (1988) 145:325–30. doi: 10.1176/ajp.145.3.325
14. Kim D, Yoo ER, Li AA, Tighe SP, Cholankeril G, Harrison SA, et al. Depression is associated with non-alcoholic fatty liver disease among adults in the United States. Aliment Pharmacol Ther. (2019) 50:590–8. doi: 10.1111/apt.15395
15. Grigsby AB, Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. Prevalence of anxiety in adults with diabetes: a systematic review. J Psychosom Res. (2002) 53:1053–60. doi: 10.1016/S0022-3999(02)00417-8
16. Anderson RJ, Grigsby AB, Freedland KE, de Groot M, McGill JB, Clouse RE, et al. Anxiety and poor glycemic control: a meta-analytic review of the literature. Int J Psychiatry Med. (2002) 32:235–47. doi: 10.2190/KLGD-4H8D-4RYL-TWQ8
17. Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. (2012) 142:1592–609. doi: 10.1053/j.gastro.2012.04.001
18. Choi JM, Yang JI, Kang SJ, Han YM, Lee J, Lee C, et al. Association between anxiety and depression and gastroesophageal reflux disease: results from a large cross-sectional study. J Neurogastroenterol Motil. (2018) 24:593–602. doi: 10.5056/jnm18069
19. Julian LJ. Measures of anxiety: state-trait anxiety inventory (STAI), Beck anxiety inventory (BAI), and hospital anxiety and depression scale-anxiety (HADS-A). Arthritis Care Res. (2011) 63 (Suppl. 11):S467–72. doi: 10.1002/acr.20561
20. Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck depression inventory-II (BDI-II), center for epidemiologic studies depression scale (CES-D), geriatric depression scale (GDS), hospital anxiety and depression scale (HADS), and patient health questionnaire-9 (PHQ-9). Arthritis Care Res. (2011) 63 (Suppl. 11):S454–66. doi: 10.1002/acr.20556
21. Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. (2002) 346:1221–31. doi: 10.1056/NEJMra011775
22. Saadeh S, Younossi ZM, Remer EM, Gramlich T, Ong JP, Hurley M, et al. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology. (2002) 123:745–50. doi: 10.1053/gast.2002.35354
23. Tomeno W, Kawashima K, Yoneda M, Saito S, Ogawa Y, Honda Y, et al. Non-alcoholic fatty liver disease comorbid with major depressive disorder: the pathological features and poor therapeutic efficacy. J Gastroenterol Hepatol. (2015) 30:1009–14. doi: 10.1111/jgh.12897
24. Youssef NA, Abdelmalek MF, Binks M, Guy CD, Omenetti A, Smith AD, et al. Associations of depression, anxiety and antidepressants with histological severity of nonalcoholic fatty liver disease. Liver Int. (2013) 33:1062–70. doi: 10.1111/liv.12165
25. Jung JY, Park SK, Oh CM, Chung PW, Ryoo JH. Non-alcoholic fatty liver disease and its association with depression in Korean general population. J Korean Med Sci. (2019) 34:e199. doi: 10.3346/jkms.2019.34.e199
26. Russ TC, Kivimaki M, Morling JR, Starr JM, Stamatakis E, Batty GD. Association between psychological distress and liver disease mortality: a meta-analysis of individual study participants. Gastroenterology. (2015) 148:958–66.e4. doi: 10.1053/j.gastro.2015.02.004
27. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. (2005) 62:593–602. doi: 10.1001/archpsyc.62.6.593
28. Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care. (2000) 23:934–42. doi: 10.2337/diacare.23.7.934
29. Lyra E, Silva NM, Lam MP, Soares CN, Munoz DP, Milev R, De Felice FG. Insulin resistance as a shared pathogenic mechanism between depression and type 2 diabetes. Front Psychiatry. (2019) 10:57. doi: 10.3389/fpsyt.2019.00057
30. Laake JP, Stahl D, Amiel SA, Petrak F, Sherwood RA, Pickup JC, et al. The association between depressive symptoms and systemic inflammation in people with type 2 diabetes: findings from the South London diabetes study. Diabetes Care. (2014) 37:2186–92. doi: 10.2337/dc13-2522
31. Maes M, Song C, Lin A, De Jongh R, Van Gastel A, Kenis G, et al. The effects of psychological stress on humans: increased production of pro-inflammatory cytokines and a Th1-like response in stress-induced anxiety. Cytokine. (1998) 10:313–8. doi: 10.1006/cyto.1997.0290
32. Nocito A, Dahm F, Jochum W, Jang JH, Georgiev P, Bader M, et al. Serotonin mediates oxidative stress and mitochondrial toxicity in a murine model of nonalcoholic steatohepatitis. Gastroenterology. (2007) 133:608–18. doi: 10.1053/j.gastro.2007.05.019
33. Shek DT. Reliability and factorial structure of the Chinese version of the general health questionnaire. J Clin Psychol. (1987) 43:683–91. doi: 10.1002/1097-4679(198711)43:6<683::AID-JCLP2270430606>3.0.CO;2-B
34. Jo SA, Park MH, Jo I, Ryu S-H, Han C. Usefulness of Beck depression inventory (BDI) in the Korean elderly population. Int J Geriatr Psychiatry. (2007) 22:218–23. doi: 10.1002/gps.1664
35. Huffman JC, Doughty CT, Januzzi JL, Pirl WF, Smith FA, Fricchione GL. Screening for major depression in post-myocardial infarction patients: operating characteristics of the Beck depression inventory-II. Int J Psychiatry Med. (2010) 40:187–97. doi: 10.2190/PM.40.2.e
36. Nuevo R, Lehtinen V, Reyna-Liberato PM, Ayuso-Mateos JL. Usefulness of the Beck depression inventory as a screening method for depression among the general population of Finland. Scand J Public Health. (2009) 37:28–34. doi: 10.1177/1403494808097169
37. Santangelo G, Sacco R, Siciliano M, Bisecco A, Muzzo G, Docimo R, et al. Anxiety in multiple sclerosis: psychometric properties of the state-trait anxiety inventory. Acta Neurol Scand. (2016) 134:458–66. doi: 10.1111/ane.12564
38. Kvaal K, Ulstein I, Nordhus IH, Engedal K. The Spielberger state-trait anxiety inventory (STAI): the state scale in detecting mental disorders in geriatric patients. Int J Geriatr Psychiatry. (2005) 20:629–34. doi: 10.1002/gps.1330
Keywords: hepatic steatosis, anxiety, depression, association, mood disorder
Citation: Choi JM, Chung GE, Kang SJ, Kwak M-S, Yang JI, Park B and Yim JY (2021) Association Between Anxiety and Depression and Nonalcoholic Fatty Liver Disease. Front. Med. 7:585618. doi: 10.3389/fmed.2020.585618
Received: 21 July 2020; Accepted: 10 December 2020;
Published: 18 January 2021.
Edited by:
Oscar Escribano, Complutense University of Madrid, SpainReviewed by:
Nazri Mustaffa, Universiti Sains Malaysia (USM), MalaysiaJesús Funuyet-Salas, Sevilla University, Spain
Copyright © 2021 Choi, Chung, Kang, Kwak, Yang, Park and Yim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Goh Eun Chung, Z29od29tQGRhdW0ubmV0
 Ji Min Choi1
Ji Min Choi1 Goh Eun Chung
Goh Eun Chung Min-Sun Kwak
Min-Sun Kwak