
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Med. , 21 July 2020
Sec. Infectious Diseases: Pathogenesis and Therapy
Volume 7 - 2020 | https://doi.org/10.3389/fmed.2020.00328
Eosinophilic colitis is a rare inflammatory disorder of the digestive tract with chronic evolution and unknown pathophysiological mechanisms. The article describes the case of a 64-year old woman with a history of asthma and hypereosinophilia, who presented to a surgical department for persistent abdominal pain in the past 4 months, weight loss and malabsorption. She was diagnosed with eosinophilic colitis based on the colonoscopic result indicating extensive eosinophilic infiltration of the colonic mucosa correlated with the laboratory data and abdominal CT scan results. Following the colonoscopy, the patient developed fever, hypotension and diarrhea and was transferred to an Infectious Diseases Department with a presumptive diagnosis of abdominal sepsis. Treatment with ertapenem was immediately started. Metronidazole was also added due to a PCR positive stool test for Clostridioides difficile toxins encoding-genes. The patient displayed a rapid remission of the fever and of the intestinal complaints following antibiotic therapy and was discharged after 14 days. During a 3 months follow-up, the patient remained asymptomatic with normal values of laboratory parameters except for a persistent hypereosinophilia. The case outlines two distinguishing features: a histopathologic diagnosis of eosinophilic colitis, a rare diagnosis of a patient with chronic abdominal pain and an unexpected and rapid remission of the eosinophilic colitis following the antibiotic treatment and the restoration of the intestinal eubiosis.
Eosinophils are specialized granulocytes able to coordinate multiple pathogenic pathways involved in the allergic, inflammatory and antimicrobial response. Eosinophils arise in the bone marrow and travel to mucosal tissues, where they regulate the local immune response and tissue repair processes (1). In the gastrointestinal tract, most eosinophils reside in the lamina propria of the stomach and intestines (2). Under inflammatory conditions, eosinophils accumulate in gut-associated lymphoid tissue (3) where they promote immune homeostasis (4) and play an active role against helminths and pathogenic bacteria including Clostridioides difficile (C. difficile) intestinal invasion (5–9). On the other hand, significant eosinophilic infiltrates of the gastrointestinal mucosa were described in several conditions, including eosinophilic gastrointestinal diseases and to a lesser extend in patients with inflammatory bowel disease (10) or in those who gradually evolve toward inflammatory bowel diseases (11–13). Eosinophilic gastrointestinal diseases comprise a group of rare diseases with a controversial pathogenesis and therapeutic armamentarium. Depending on the location of the eosinophilic infiltrate, eosinophilic gastrointestinal diseases include esophageal, gastric and intestinal disorders. The number of documented eosinophilic gastrointestinal diseases cases is still low, with an estimated prevalence of around 3.3–5.1/100,000 persons (14, 15).
Hence, most data on eosinophilic gastrointestinal diseases derives from only a few hundred case reports (16–22). Of these, eosinophilic colitis appear to be a particularly rare entity with a challenging diagnosis (23, 24). Currently, only small case series or single case reports of eosinophilic colitis were reported in literature (14, 15, 17, 25–28).
We present the clinical course of a patient with symptomatic eosinophilic colitis who developed nosocomial C. difficile infection and sepsis following the diagnostic colonoscopic procedure. The patient displayed an unexpectedly rapid and favorable evolution of these severe infections but also a longstanding improvement of the eosinophilic colitis flare after prompt antibiotic therapy. The article further discusses current literature data on the immunomodulatory role of eosinophils and presents a viewpoint regarding its pathogenic significance in the intestinal inflammatory response in C. difficile infection and dysbiosis.
A 64-year old lady was hospitalized in a surgical department for abdominal pain lasting for more than 4 months and accompanied by vomiting, flatulence, fatigue and a 10 kg weight loss, without fever or chills. The patient had a history of asthma with recurrent exacerbations, and negative allergological assessments and had received inhalatory steroids for the past 3-years. The thoracic and abdominal CT examination disclosed diffuse intestinal wall thickening and dilated intestinal loops, sigmoid diverticulosis and a small pleural and pericardial effusion (Figure 1, Supplementary Figure 1). Superior endoscopy revealed a minimal erythematous gastritis and the colonoscopic evaluation confirmed sigmoid diverticulosis and segmental colitis. Five biopsy specimens were collected for examination during the colonoscopy. No specific yellow nodules, pseudomembranes or other lesions suggestive for C. difficile infection were observed during the colonoscopy. Following this procedure, the patient suddenly developed fever and vomiting. The abdominal pain gradually aggravated and the patient developed a severe diarrhea. Given the high probability of an abdominal sepsis, the patient was transferred to the Department of Infectious Diseases.
On admission the patient was febrile (39°C), pale, hypotensive (80/60 mmHg), tachycardic (heart rate 95/min) with a distended painful abdomen, peripheral edema and watery stools. Laboratory parameters displayed an intense inflammatory syndrome, increased liver enzymes, positive procalcitonin, hypoalbuminemia, and anemia secondary to the chronic malabsorption but also hypereosinophilia (twice the normal values) and increased IgE levels (three times higher than the normal values) (Table 1). C. difficile infection was suspected on the PCR stool assay for toxigenic genes of C. difficile (GeneXpert). Blood, stool and urine cultures remained negative. The result of the colonic biopsy was retrieved 48 h after admission and showed a significant eosinophilic infiltrate in the colonic mucosa and submucosa, as well as vasculitis, with numerous eosinophils in the vascular wall. The bioptic specimens did not show any signs of granulomas or malignancy and the histopathologic examination thus pleaded for eosinophilic colitis (Figures 2A,B). Considering the histopathological analysis along with the laboratory and imaging findings, the current presentation was considered as a case of eosinophilic colitis complicated with C. difficile infection and sepsis. The patient was initially treated as an abdominal sepsis with ertapenem 1 g/day, with the clinical remission of the fever and the improvement of the laboratory parameters, including the procalcitonin. After receiving the positive results of the PCR stool assay, the patient also received metronidazol 250 mg every 6 h and continued ertapanem for 14 days with a rapid favorable outcome. Upon discharge she was afebrile, asymptomatic, with decreasing IgE levels and normal values of the inflammatory markers. Corticoid treatment was not used during the hospitalization or on discharge. Three months after discharge the patient remained asymptomatic, with no digestive symptoms or asthma exacerbations and normal laboratory values except for persistent hypereosinophilia. The patient also exhibited increasing values of the eosinophils in the following 6 months, raising concerns of a malignant proliferation. She was then admitted to a hematology unit and later to a gastroenterology ward and was placed on corticosteroid treatment with favorable results. On follow-up the patient remained asymptomatic, with no relapse within the following 3-years. The eosinophil count gradually decreased, yet remained at the upper normal limit until now.
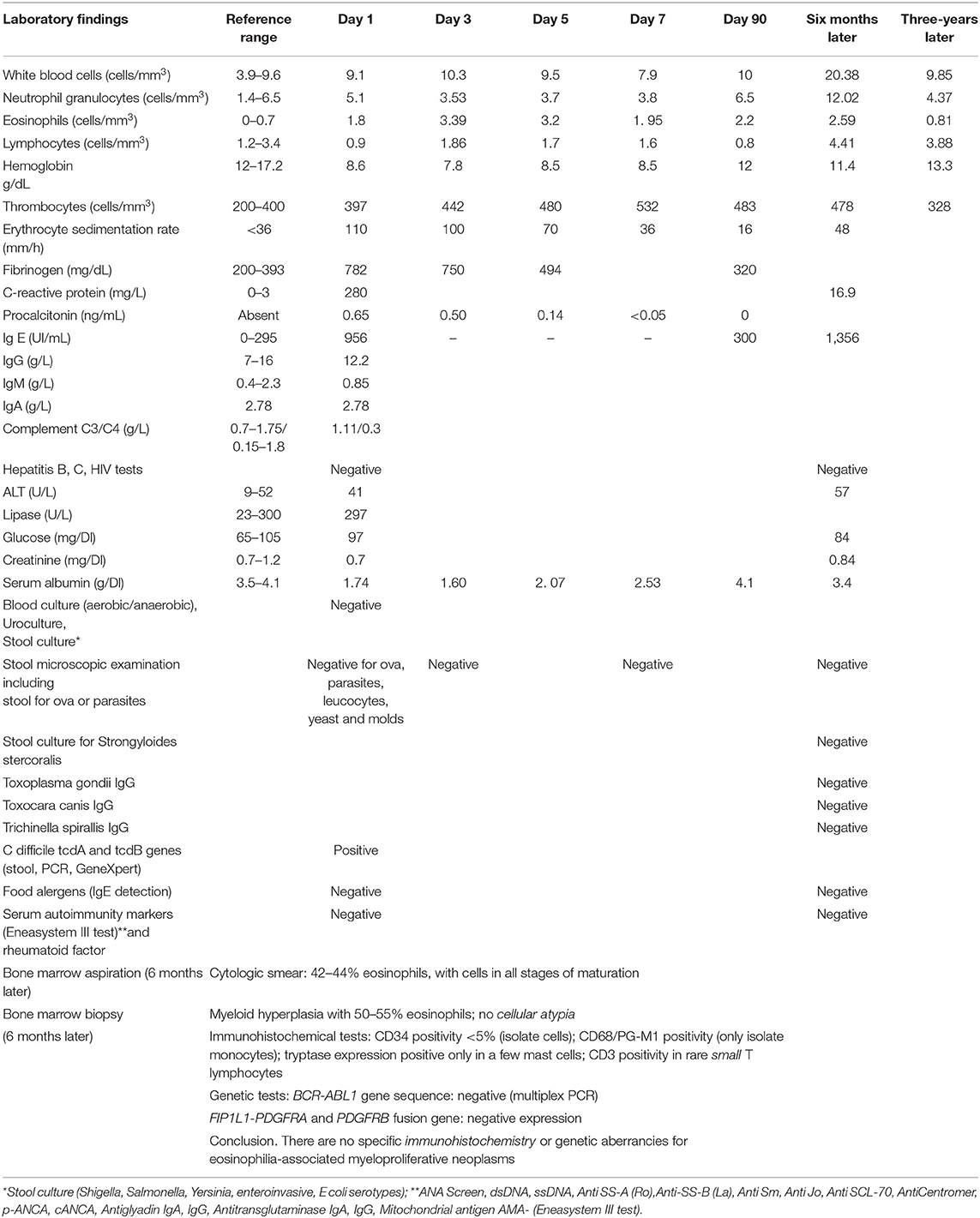
Table 1. Laboratory investigations in a case of eosinophilic colitis complicated with C. difficile infection and sepsis.
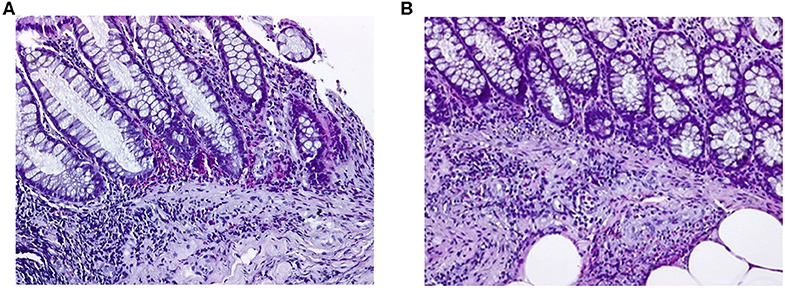
Figure 2. Eosinophilic colitis, histological section. Photography with objective at 200X. Biopsy was fixed in formalin, embedded in paraffin and stained with hematoxylin-eosin. (A) Colonic mucosa with numerous eosinophils infiltrating the lamina propria, of which some with an intraepithelial localization. Polymorphonuclear leukocytes and eosinophils are also seen infiltrating the muscularis mucosa. (B) Numerous eosinophils infiltrating the colonic submucosa.
Eosinophilic colitis is a rare and insufficiently characterized disease. The clinical presentation of eosinophilic colitis is highly unspecific and prompts a very wide differential diagnosis, which includes inflammatory bowel diseases, celiac diseases, neoplasia, vasculitis, the hypereosinophilic syndrome, drug induced colitis or various infectious etiologies (28). Currently, the only definitive criteria for eosinophilic colitis is the finding of an extensive eosinophilic infiltrate of the intestinal wall, containing at least 30 eosinophils per high-power field in at least five high-power fields associated with endoscopic abnormalities (29, 30). However, the histopathologic criteria are not standardized and differ between studies (22, 23, 31–33). Thus, in the absence of characteristic clinical and laboratory findings, many patients could remain undiagnosed (23). The underlying pathophysiologic mechanisms in eosinophilic colitis have not been fully elucidated and the therapeutic options are limited. Allergic mechanisms appear to play an important, albeit unknown role in a large number of patients and consequently the use of corticosteroids in severe cases is considered beneficial (16, 18, 30). An atopic state has been reported by various authors in 41.8% of patients with eosinophilic colitis (14). However, its presence is not mandatory (18, 34) and IgE–mediated mechanisms appear to be more common in young patients compared to adults (35). Peripheral eosinophilia was observed in 74–83.3% of cases with eosinophilic colitis and has been associated with a high rate of relapse (18, 20, 26). Still, serum eosinophilia was not recorded in all cases. Various authors have underlined the absence of a correlation between serum eosinophilia and the colitis outcome or the intestinal eosinophilic infiltrate, thus suggesting the secondary role of eosinophilia in the onset of colitis (36, 37).
Clinical and experimental studies have showed that the trafficking of eosinophils to the gut and their activation is stimulated by intestinal signals released by the intestinal epithelia, as well as by type 2 innate lymphoid cells (ILC2) or by mucosal immune response (38–40). Hence, murine studies showed that eosinophils normally accumulate in the lamina propria of the gut and stomach and their presence is mainly regulated by eotaxin-1, a chemokine released by epithelial cells (38, 40). Eotaxin expressed throughout the gastrointestinal tract displays a synergism with IL-5 and IL-13, two ILC2- secreted cytokines (39, 40). Other potent regulators of tissue eosinophilia and ILC2 activity include the cytokines IL-25 (a member of the IL-17 family) and IL-33 (a member of the IL-1 family), two central mediators of the Th2 immunity and Foxp3(+) regulatory T (Treg) cells immunosuppressive activities of the gut barrier (41, 42). Thus, the intestinal trafficking of eosinophils is a result of the signals released by the intestinal barrier and of the immune mediators regulated by various physiologic or pathologic stimuli.
The ILC2-eosinophil axis plays a major role in the specific anti-inflammatory response to allergen exposure as well as in the protective immunity against pathogens and the remodeling and intestinal repair (43–45). Eosinophils constitutively express various toll like receptors which enable the recognition of numerous microbial antigens, sustain secretory IgA production, dendritic cells activation and Th1/Th17 pro-inflammatory response as well as the retention of immunosuppressive Treg cells in the lamina propria (4, 46, 47). Thus, eosinophils display both a pro-inflammatory and a cytotoxic potential against pathogenic germs, while also supporting a protective role in gut homeostasis. In studies on healthy mice, intestinal eosinophils preserve the integrity of the epithelial barrier and also regulate the innate host defense and tissue remodeling (4, 48–51).
Nevertheless, ILC2-Th2 secreted cytokines and intestinal eosinophils have been linked with significant histopathological changes during eosinophilic esophagitis or other intestinal disorders (2, 44, 52, 53). Still, there is insufficient data regarding the conditions which facilitate this phenotypical switch of eosinophils and which enable their extensive and chronic infiltration of the colonic wall. The changes of the intestinal environment and the pathologic transformation of tissue eosinophils have been associated with multiple factors such as a genetic predisposition, various intestinal allergens, as well as with persistent intestinal infections or severe and prolonged dysbiosis (54–57). Nevertheless, the pathologic role of intestinal eosinophils during dysbiosis or enteral infections such as C. difficile remains controversial (58–60).
The number of cases with C. difficile infection-associated eosinophilic colitis is extremely small. Kim et al. published a similar case (61). None of the existing prevalence studies have approached the impact of the intestinal eosinophilic infiltrate on the colonization with C. difficile strains. However, the role of intestinal eosinophils in the attenuation of the inflammatory immune response during C. difficile infection was underlined by Buonomo and other authors and was attributed to the mucosal eosinophilia (6, 62–64) and IL-25 induction. Additionally the previous studies also discussed the role of IL-33, in the recruitment of eosinophils (65) and ILC2 activation (45), in the maintenance of intestinal eubiosis (50) or in the reduction of C. difficile mortality (45). In this respect, most murine models highlighted the ability of IL-33 to orchestrate the inflammatory response and tissue remodeling, further leading to a subsequent decrease in the translocation of pathogenic bacteria (66–68) and to the preservation of the intestinal homeostasis (66, 68). Hence, the IL-25/IL-33/ILC2 axis activation and gut eosinophils regulate the local immune response during acute enteral infections and play a specific regulatory role in inflammatory response during C. difficile infections (45). At the same time, IL-33 remains a contradictory cytokine with a marked pro-inflammatory potential (69, 70). Hence, a high and persistent level of IL-33 could contribute to an excessive eosinophilic response and to the build- up of pathogenic lesions. Nevertheless, the previous hypotheses require further clinical validation and if proven could significantly change the current perspective on the role played by intestinal eosinophils in the pathogenesis of intestinal inflammatory diseases.
The microbiota plays a remarkable anti-infectious role, enabling the survival of commensal germs and the elimination of pathogens as a result of its connections with the intestinal immunity and the intestinal epithelia. The immune-microbiota homeostasis is closely linked to the eosinophilic immune response, explaining the rapid activation of the latter during dysbiosis (4). Regarding the underlying pathogenic mechanisms, both enteral infections and related dysbiosis increase the concentration of intestinal eosinophils through a Th17- pro-inflammatory response, as well as through the ILC2-eosinophil axis which ensues after the epithelial release of IL-25/IL-33 cytokines (71).
Once stimulated, the intestinal eosinophils exert an important immunomodulatory role, regulating the excessive inflammatory response (72). This regulatory role involves the suppression of the Th17 response elicited by IL-1 receptor antagonist IL-1 Ra, the activation of CD103+ dendritic cell activation, the differentiation of Treg cells and the synthesis of secretory antimicrobial IgA (47, 50, 73, 74). Eosinophils are thus involved in the preservation of the intestinal homeostasis and are correlated with the composition of the intestinal microbiota, as shown experimentally by Chu et al. (4) and Jung et al. (50).
Chu et al. (4) analyzed the microbiota of eosinophil-deficient mice and recorded various significant differences, most of which concerned segmented filamentous bacteria, a member of Clostridiales with an essential role in the Th17 induction of and T cell response (75, 76). At the same time, Jung et al. (50) showed that the lack of gastrointestinal eosinophils reduces the level of secretory IgAs and decreases the ensuing protection against microbial pathogens, leading to dysbiosis. These experiments support the Local Immunity And/or Remodeling/Repair (LIAR) hypothesis (51) formulated by Lee in 2010 according to which in a Th1/Th17 polarized microenvironment, the intestinal eosinophilic infiltrate is a regulatory and not a destructive event, an effect, rather than a cause of the intestinal inflammation. Hence, its presence in a severe illness (10) could be an adaptation mechanism to antigenic exposure meant to attenuate the Th17 immune response and to favor tissue regeneration.
The case discussed above displayed several notable features regarding its diagnosis and evolution.
For one thing, the patient reported a non-specific onset which initially suggested an abdominal tumor, given the diffuse abdominal pain and the accompanying weight loss in the past 4 months However, the subsequent histopathological exam disclosed numerous eosinophils located in the lamina propria of colonic mucosa and muscularis mucosa, accompanied by hypereosinophilia and an increased IgE serum level, which supported the final diagnosis of eosinophilic colitis. Furthermore, the disease was considered severe based on the extension of the eosinophilic infiltrates, the prolonged diseases course and hypoalbuminemia and anemia secondary to the colonic malabsorption (36).
Secondly, the diarrheal syndrome was interpreted in the context of a C. difficile infection, according to the case definitions elaborated by the Infectious Diseases Society of America (IDSA) and European Society of Clinical Microbiology and Infectious Diseases (ESCMID). The diagnosis of C. difficile infection was based on the following arguments: (a) the sudden debut of a diarrheal syndrome following colonoscopy; (b) the positive PCR assay indicating C. difficile toxin genes tcdA and tcdB; (c) the absence of other causes explaining the diarrheal syndrome (Table 1); (d) the therapeutic response to oral vancomycin.
Regarding the risk of colonization with toxigenic strains of C. difficile, while this alternative is possible in asymptomatic patients, we argue that this is less likely given the sudden development of a diarrheic syndrome in our patient in the absence of other causes (Table 1) or of known risk factors for C. difficile colonization (77, 78).
Data regarding the risk of colonization with toxigenic strains of C. difficile remains controversial. While no data are available on C. difficile colonization in patients with eosinophilic colitis, Cowardin et al. showed in a mouse model of C. difficile colitis that toxigenic strains inhibit the protective eosinophilic response through a TLR2 mediated mechanism and favor the inflammatory response and the development of diarrhea (62). Nevertheless, the hypothesis of a toxigenic colonization before colonoscopy cannot be disproved. Given the preexistent inflammatory lesions it is probable that such a colonization would have induced a previous episode of C. difficile infection (78) which did not occur.
The colonoscopy also exposed the patient to supplementary complications. The risk of C. difficile infection after colonoscopy has been previously suggested (79, 80) and it is considered a rare occurrence. Nosocomial C. difficile strains exhibit high cytotoxicity and higher rates of recurrence and bloodstream infections (81). The occurrence of C. difficile infection in cases of inflammatory bowel disease leads to the activation of pro-inflammatory cytokines, including the IL-1β/Th17 axis (78) which aggravates the course of diseases (82–85), increases the risk of C. difficile recurrences (84) and raises the mortality by four times (86). Similarly the risk of sepsis in C. difficile infection is a severe event due to the altered intestinal barrier and the subsequent bacterial translocation (87, 88).
Nevertheless, in our case the patient displayed a favorable and unexpectedly rapid evolution, along with the significant improvement of the symptoms of eosinophilic colitis following antibiotic treatment.
The evolution of our case is compatible with a protective role of eosinophils toward C. difficile-associated infection as suggested by Buonomo et al. (6) and Cowardin et al. (62) as well as a beneficial role of eosinophils in gut homeostasis discussed by Jung et al. (50) and Chu et al. (4).
Our case also underlines the role of dysbiosis and the impact of its treatment on the flare of eosinophilic colitis. The clinical outcome of the patient suggested that the intestinal dysbiosis remitted; had the dysbiosis persisted it would have aggravated under ertapenem and the infection with C. difficile would have recurred. The rapid improvement without a recurrence was particularly intriguing: an antibiotic treatment in a patient with eosinophilic colitis resolved both the C. difficile infection and alleviated the manifestations of eosinophilic colitis. In other words, if the gut equilibrium between pathogens and commensals is re-established, the clinical course of intestinal inflammatory diseases should also improve, as has been shown by Khan et al. (89). Hence, it is possible that this finding could also apply to eosinophilic colitis, an intestinal inflammatory disease.
It is probable that the chronic inflammatory response in the eosinophilic colitis is maintained through either occult intestinal infections and related dysbiosis or through an abberant immune response to the intestinal microbiota, two key events which could favor the intestinal acummulation of eosinophils. Should this be the case, it is probable that the administration of synbiotics, fecal transplantation or other regulatory therapeutic agents of microbiota could address both the inflammatory response and dysbiosis. Hence, Dai and colleagues reported a severe case of eosinophilic gastroenteritis, with a rapid remission following fecal microbiota transplantation and glucocorticoid treatment (90). However, the role of dysbiosis in the exacerbation of the intestinal immune response and in the pathogenesis of intestinal inflammation has already been shown in experimental studies (91), in patients with inflammatory bowel disease (92, 93) and in various murine experiments (94, 95). This finding has led to an increased interest for therapeutic fecal transplantation in inflammatory bowel disease (96–98), although its indication has not been formally studied in eosinophilic colitis (99). Additional research is needed to establish the impact of therapeutic strategies against dysbiosis on the clinical outcome of eosinophilic colitis.
The study of gut dysbiosis in eosinophilic colitis was not previously approached although similar correlations have been observed in other intestinal inflammatory syndromes (100, 101). The importance of this case lies in a clinical hypothesis to be proven by future studies, regarding the correlation between eosinophilic colitis and intestinal dysbiosis. At the same time, we wanted to highlight that current results from experimental data support the physiopathological hypothesis of eosinophils as defense cell-lines attracted to the intestinal mucosa in order to maintain intestinal homeostasis. Hence, the presence of eosinophils in the gut indicates a previous intestinal “conflict,” potentially due to a shift of the harbored intestinal flora. If proven, this concept could enable a more simple, less expensive and less aggressive treatment which could potentially be implemented in eosinophilic colitis as well as in other intestinal inflammatory diseases. The publication of other cases could be useful for the understanding of other physio-pathological aspects in eosinophilic syndromes.
The current case describes an uncommon gastrointestinal disorder- eosinophilic colitis—complicated by nosocomial C. difficile infection and severe sepsis following a diagnostic colonoscopy. Moreover, the rapid and intriguing improvement of colitis after antibiotic treatment underlines the relevance of restoring the intestinal eubiosis in order to achieve the remission of both the infectious complications and the flare of eosinophilic colitis.
The case additionally highlights the role of eosinophils in the protection of the intestinal barrier and intestinal immune response during C. difficile infection and reveals how the reestablishment of the microbiota homeostasis leads to a favorable evolution of eosinophilic colitis.
All datasets generated for this study are included in the article/Supplementary Material.
Written informed consent was obtained from the patient's representative for the publication of this case report.
SI wrote the manuscript. DI collected the patient's clinical data, searched literature data, and critically reviewed the manuscript. MO collected the imagistic data and critically reviewed the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors thank the patient and the patient's representative, Ms. Andreea Lupescu for the provision of the written consent for publication and for the medical information that was kindly provided. We are also grateful to Dr. Valentin Enache from the Department of Anatomopathology, Floreasca Emergency Hospital, Bucharest, for performing the histological sections and the photographs.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2020.00328/full#supplementary-material
Supplementary Figure 1. Computed tomography of the abdomen and pelvis. Mild circumferential and diffuse intestinal wall thickening with parietal enhancement (arrows).
1. Travers J, Rothenberg ME. Eosinophils in mucosal immune responses. Mucosal Immunol. (2015) 8:464–75. doi: 10.1038/mi.2015.2
2. Jung Y, Rothenberg ME. Roles and regulation of gastrointestinal eosinophils in immunity and disease. J Immunol. (2014) 193:999–1005. doi: 10.4049/jimmunol.1400413
3. Mishra A, Hogan SP, Brandt EB, Rothenberg ME. Peyer's patch eosinophils: identification, characterization, and regulation by mucosal allergen exposure, interleukin-5, and eotaxin. Blood. (2000) 96:1538–44. doi: 10.1182/blood.V96.4.1538
4. Chu VT, Beller A, Rausch S, Strandmark J, Zänker M, Arbach O, et al. Eosinophils promote generation and maintenance of immunoglobulin-a-expressing plasma cells and contribute to gut immune homeostasis. Immunity. (2014) 40:582–93. doi: 10.1016/j.immuni.2014.02.014
5. Hogan SP, Waddell A, Fulkerson PC. Eosinophils in infection and intestinal immunity. Curr Opin Gastroenterol. (2013) 29:7–14. doi: 10.1097/MOG.0b013e32835ab29a
6. Buonomo EL, Cowardin CA, Wilson MG, Saleh MM, Pramoonjago P, Petri WA, et al. Microbiota-regulated IL-25 increases eosinophil number to provide protection during Clostridium difficile infection. Cell Rep. (2016) 16:432–43. doi: 10.1016/j.celrep.2016.06.007
7. Yousefi S, Gold JA, Andina N, Lee JJ, Kelly AM, Kozlowski E, et al. Catapult-like release of mitochondrial DNA by eosinophils contributes to antibacterial defense. Nat Med. (2008) 14:949–53. doi: 10.1038/nm.1855
8. Svensson L, Wennerås C. Human eosinophils selectively recognize and become activated by bacteria belonging to different taxonomic groups. Microbes Infect. (2005) 7:720–8. doi: 10.1016/j.micinf.2005.01.010
9. Ramirez GA, Yacoub M-R, Ripa M, Mannina D, Cariddi A, Saporiti N, et al. Eosinophils from physiology to disease: a comprehensive review. Biomed Res Int. (2018) 2018:9095275. doi: 10.1155/2018/9095275
10. Bischoff SC, Mayer J, Nguyen Q-T, Stolte M, Manns MP. Immunohistological assessment of intestinal eosinophil activation in patients with eosinophilic gastroenteritis and inflammatory Bowel disease. Am J Gastroenterol. (1999) 94:3521–9. doi: 10.1111/j.1572-0241.1999.01641.x
11. Uzunismail H, Hatemi I, Dogusoy G, Akin O. Dense eosinophilic infiltration of the mucosa preceding ulcerative colitis and mimicking eosinophilic colitis: report of two cases. Turk J Gastroenterol. (2006) 17:53–7. Available online at: https://www.turkjgastroenterol.org/en/dense-eosinophilic-infiltration-of-the-mucosa-preceding-ulcerative-colitis-and-mimicking-eosinophilic-colitis-report-of-two-cases-1621539
12. Mutalib M, Blackstock S, Evans V, Huggett B, Chadokufa S, Kiparissi F, et al. Eosinophilic gastrointestinal disease and inflammatory bowel disease in children. Eur J Gastroenterol Hepatol. (2015) 27:20–3. doi: 10.1097/MEG.0000000000000230
13. Chetcuti Zammit S, Cachia M, Sapiano K, Gauci J, Montefort S, Ellul P. Eosinophilic gastrointestinal disorder: is it what it seems to be? Ann Gastroenterol. (2018) 31:475–9. doi: 10.20524/aog.2018.0263
14. Jensen ET, Martin CF, Kappelman MD, Dellon ES. Prevalence of eosinophilic gastritis, gastroenteritis, and colitis: estimates from a national administrative database. J Pediatr Gastroenterol Nutr. (2016) 62:36–42. doi: 10.1097/MPG.0000000000000865
15. Mansoor E, Saleh MA, Cooper GS. Prevalence of eosinophilic gastroenteritis and colitis in a population-based study, from 2012 to 2017. Clin Gastroenterol Hepatol. (2017) 15:1733–41. doi: 10.1016/j.cgh.2017.05.050
16. Reed C, Woosley JT, Dellon ES. Clinical characteristics, treatment outcomes, and resource utilization in children and adults with eosinophilic gastroenteritis. Dig Liver Dis. (2015) 47:197. doi: 10.1016/j.dld.2014.11.009
17. Díaz del Arco C, Taxonera C, Olivares D, Fernández Aceñero MJ. Eosinophilic colitis: case series and literature review. Pathol Res Pract. (2018) 214:100–4. doi: 10.1016/j.prp.2017.09.029
18. Zhang L, Duan L, Ding S, Lu J, Jin Z, Cui R, et al. Eosinophilic gastroenteritis: clinical manifestations and morphological characteristics, a retrospective study of 42 patients. Scand J Gastroenterol. (2011) 46:1074–80. doi: 10.3109/00365521.2011.579998
19. Vithayasai N, Jennuvat S, Lertsatit A. Eosinophilic gastrointestinal disease: analysis of sixteen cases from ten years experience in Thailand. J Med Assoc Thai. (2011) 94(Suppl. 3):S41–8.
20. Pineton de Chambrun G, Gonzalez F, Canva J-Y, Gonzalez S, Houssin L, Desreumaux P, et al. Natural history of eosinophilic gastroenteritis. Clin Gastroenterol Hepatol. (2011) 9:950–6.e1. doi: 10.1016/j.cgh.2011.07.017 Available online at: https://www.researchgate.net/publication/51761537_Eosinophilic_gastrointestinal_disease_analysis_of_sixteen_cases_from_ten_years_experience_in_Thailand
21. Lee CM Changchien CS Chen PC Lin DY Sheen IS Wang CS . Eosinophilic gastroenteritis: 10 years experience. Am J Gastroenterol. (1993) 88:70–4.
22. Abassa K-K, Lin X-Y, Xuan J-Y, Zhou H-X, Guo Y-W. Diagnosis of eosinophilic gastroenteritis is easily missed. World J Gastroenterol. (2017) 23:3556. doi: 10.3748/wjg.v23.i19.3556
23. Turner KO, Sinkre RA, Neumann WL, Genta RM. Primary colonic eosinophilia and eosinophilic colitis in adults. Am J Surg Pathol. (2017) 41:225–33. doi: 10.1097/PAS.0000000000000760
24. Hentschel F, Jansen AF, Günther M, Pauli R, Lüth S. Eosinophil counts in mucosal biopsies of the ileum and colon: interobserver variance affects diagnostic accuracy. Patholog Res Int. (2018) 2018:1–7. doi: 10.1155/2018/2638258
25. Pesek RD, Reed CC, Muir AB, Fulkerson PC, Menard-Katcher C, Falk GW, et al. Increasing rates of diagnosis, substantial co-occurrence, and variable treatment patterns of eosinophilic gastritis, gastroenteritis, and colitis based on 10-year data across a multicenter consortium. Am J Gastroenterol. (2019) 114:984–94. doi: 10.14309/ajg.0000000000000228
26. Alfadda AA, Shaffer EA, Urbanski SJ, Storr MA. Eosinophilic colitis is a sporadic self-limited disease of middle-aged people: a population-based study. Colorectal Dis. (2014) 16:123–9. doi: 10.1111/codi.12464
27. Alfadda AA, Storr MA, Shaffer EA. Eosinophilic colitis: an update on pathophysiology and treatment. Br Med Bull. (2011) 100:59–72. doi: 10.1093/bmb/ldr045
28. Egan M, Furuta GT. Eosinophilic gastrointestinal diseases beyond eosinophilic esophagitis. Ann Allergy Asthma Immunol. (2018) 121:162–7. doi: 10.1016/j.anai.2018.06.013
29. Lucendo AJ, Arias A. Eosinophilic gastroenteritis: an update. Expert Rev Gastroenterol Hepatol. (2012) 6:591–601. doi: 10.1586/egh.12.42
30. Sunkara T, Rawla P, Yarlagadda KS, Gaduputi V. Eosinophilic gastroenteritis: diagnosis and clinical perspectives. Clin Exp Gastroenterol. (2019) Volume 12:239–53. doi: 10.2147/CEG.S173130
31. Bates AWH. Diagnosing eosinophilic colitis: histopathological pattern or nosological entity? Scientifica. (2012) 2012:9. doi: 10.6064/2012/682576
32. Collins MH. Histopathologic features of eosinophilic esophagitis and eosinophilic gastrointestinal diseases. Gastroenterol Clin North Am. (2014) 43:257–68. doi: 10.1016/j.gtc.2014.02.007
33. Lowichik A, Weinberg AG. A quantitative evaluation of mucosal eosinophils in the pediatric gastrointestinal tract. Mod Pathol. (1996) 9:110–4.
34. Gonsalves N. Food allergies and eosinophilic gastrointestinal illness. Gastroenterol Clin North Am. (2007) 36:75–91. doi: 10.1016/j.gtc.2007.01.003
35. Furuta GT, Forbes D, Boey C, Dupont C, Putnam P, Roy S, et al. Eosinophilic gastrointestinal diseases. J Pediatr Gastroenterol Nutr. (2008) 47:234–8. doi: 10.1097/MPG.0b013e318181b1c3
36. Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR. Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut. (1990) 31:54–8. doi: 10.1136/gut.31.1.54
37. Kamal MF, Shaker K, Jaser N, Leimoon BA. Eosinophilic gastroenteritis with no peripheral eosinophilia. Ann Chir Gynaecol. (1985) 74:98–100.
38. Matthews AN, Friend DS, Zimmermann N, Sarafi MN, Luster AD, Pearlman E, et al. Eotaxin is required for the baseline level of tissue eosinophils. Proc Natl Acad Sci USA. (1998) 95:6273. doi: 10.1073/pnas.95.11.6273
39. Nussbaum JC, Van Dyken SJ, von Moltke J, Cheng LE, Mohapatra A, Molofsky AB, et al. Type 2 innate lymphoid cells control eosinophil homeostasis. Nature. (2013) 502:245–8. doi: 10.1038/nature12526
40. Mishra A, Hogan SP, Lee JJ, Foster PS, Rothenberg ME. Fundamental signals that regulate eosinophil homing to the gastrointestinal tract. J Clin Invest. (1999) 103:1719–27. doi: 10.1172/JCI6560
41. Fort MM, Cheung J, Yen D, Li J, Zurawski SM, Lo S, et al. IL-25 induces IL-4, IL-5, and IL-13 and Th2-associated pathologies in vivo. Immunity. (2001) 15:985–95. doi: 10.1016/S1074-7613(01)00243-6
42. Schmitz J, Owyang A, Oldham E, Song Y, Murphy E, McClanahan TK, et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. (2005) 23:479–90. doi: 10.1016/j.immuni.2005.09.015
43. Klose CSN, Artis D. Innate lymphoid cells as regulators of immunity, inflammation and tissue homeostasis. Nat Immunol. (2016) 17:765–74. doi: 10.1038/ni.3489
44. Yazdani R, Sharifi M, Shirvan AS, Azizi G, Ganjalikhani-Hakemi M. Characteristics of innate lymphoid cells and their role in immunological disorders. Cell Immunol. (2015) 298:66–76. doi: 10.1016/j.cellimm.2015.09.006
45. Frisbee AL, Saleh MM, Young MK, Leslie JL, Simpson ME, Abhyankar MM, et al. IL-33 drives group 2 innate lymphoid cell-mediated protection during Clostridium difficile infection. Nat Commun. (2019) 10:2712. doi: 10.1038/s41467-019-10733-9
46. Loktionov A. Eosinophils in the gastrointestinal tract and their role in the pathogenesis of major colorectal disorders. World J Gastroenterol. (2019) 25:3503–26. doi: 10.3748/wjg.v25.i27.3503
47. Chu DK, Jimenez-Saiz R, Verschoor CP, Walker TD, Goncharova S, Llop-Guevara A, et al. Indigenous enteric eosinophils control DCs to initiate a primary Th2 immune response in vivo. J Exp Med. (2014) 211:1657–72. doi: 10.1084/jem.20131800
48. Lampinen M, Rönnblom A, Amin K, Kristjansson G, Rorsman F, Sangfelt P, et al. Eosinophil granulocytes are activated during the remission phase of ulcerative colitis. Gut. (2005) 54:1714–20. doi: 10.1136/gut.2005.066423
49. Furuta GT, Nieuwenhuis EES, Karhausen J, Gleich G, Blumberg RS, Lee JJ, et al. Eosinophils alter colonic epithelial barrier function: role for major basic protein. Am J Physiol Gastrointest Liver Physiol. (2005) 289:G890–7. doi: 10.1152/ajpgi.00015.2005
50. Jung Y, Wen T, Mingler MK, Caldwell JM, Wang YH, Chaplin DD, et al. IL-1β in eosinophil-mediated small intestinal homeostasis and IgA production. Mucosal Immunol. (2015) 8:930–42. doi: 10.1038/mi.2014.123
51. Lee JJ, Jacobsen EA, McGarry MP, Schleimer RP, Lee NA. Eosinophils in health and disease: the LIAR hypothesis. Clin Exp Allergy. (2010) 40:563–75. doi: 10.1111/j.1365-2222.2010.03484.x
52. Hogan SP, Mishra A, Brandt EB, Royalty MP, Pope SM, Zimmermann N, et al. A pathological function for eotaxin and eosinophils in eosinophilic gastrointestinal inflammation. Nat Immunol. (2001) 2:353–60. doi: 10.1038/86365
53. Doherty TA, Baum R, Newbury RO, Yang T, Dohil R, Aquino M, et al. Group 2 innate lymphocytes are enriched in active eosinophilic esophagitis. J Allergy Clin Immunol. (2015) 136:792–4.e3. doi: 10.1016/j.jaci.2015.05.048
54. Verma AK, Kandikattu HK, Manohar M, Shukla A, Upparahalli Venkateshaiah S, Zhu X, et al. Intestinal overexpression of IL−18 promotes eosinophils-mediated allergic disorders. Immunology. (2019) 157:110–21. doi: 10.1111/imm.13051
55. Keely S, Walker MM, Marks E, Talley NJ. Immune dysregulation in the functional gastrointestinal disorders. Eur J Clin Invest. (2015) 45:1350–9. doi: 10.1111/eci.12548
56. Walker MM. Inflammation, genetics, dysbiosis, and the environment. J Clin Gastroenterol. (2016) 50:S4–5. doi: 10.1097/MCG.0000000000000613
57. Walker MM, Potter M, Talley NJ. Eosinophilic gastroenteritis and other eosinophilic gut diseases distal to the oesophagus. Lancet Gastroenterol Hepatol. (2018) 3:271–80. doi: 10.1016/S2468-1253(18)30005-0
58. Zaiss MM, Maslowski KM, Mosconi I, Guenat N, Marsland BJ, Harris NL. IL-1β suppresses innate IL-25 and IL-33 production and maintains helminth chronicity. PLoS Pathog. (2013) 9:e1003531. doi: 10.1371/journal.ppat.1003531
59. Villani A-C, Lemire M, Fortin G, Louis E, Silverberg MS, Collette C, et al. Common variants in the NLRP3 region contribute to Crohn's disease susceptibility. Nat Genet. (2009) 41:71–6. doi: 10.1038/ng.285
60. Alhallaf R, Agha Z, Miller CM, Robertson AAB, Sotillo J, Croese J, et al. The NLRP3 inflammasome suppresses protective immunity to gastrointestinal helminth infection. Cell Rep. (2018) 23:1085–98. doi: 10.1016/j.celrep.2018.03.097
61. Kim TG, Park J, Seo EH, Joo HR, Park SH, Kim TO, et al. Esosinophilic gastroenteritis with Clostridium difficile-associated colitis: a case report. Korean J Gastrointest Endosc. (2011) 43:64–8. Available online at: https://www.e-ce.org/upload/pdf/Kjge043-01-16.pdf
62. Cowardin CA, Buonomo EL, Saleh MM, Wilson MG, Burgess SL, Kuehne SA, et al. The binary toxin CDT enhances Clostridium difficile virulence by suppressing protective colonic eosinophilia. Nat Microbiol. (2016) 1:16108. doi: 10.1038/nmicrobiol.2016.108
63. Hosoki K, Nakamura A, Nagao M, Hiraguchi Y, Tokuda R, Wada H, et al. Differential activation of eosinophils by ‘probiotic' Bifidobacterium bifidum and ‘pathogenic' Clostridium difficile. Int Arch Allergy Immunol. (2010) 152:83–9. doi: 10.1159/000312131
64. Crook DW, Walker AS, Kean Y, Weiss K, Cornely OA, Miller MA, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection: meta-analysis of pivotal randomized controlled trials. Clin Infect Dis. (2012) 55(Suppl. 2):S93–103. doi: 10.1093/cid/cis499
65. Cherry WB, Yoon J, Bartemes KR, Iijima K, Kita H. A novel IL-1 family cytokine, IL-33, potently activates human eosinophils. J Allergy Clin Immunol. (2008) 121:1484–90. doi: 10.1016/j.jaci.2008.04.005
66. Williams MA, O'Callaghan A, Corr SC. IL-33 and IL-18 in inflammatory bowel disease etiology and microbial interactions. Front Immunol. (2019) 10:1091. doi: 10.3389/fimmu.2019.01091
67. Malik A, Sharma D, Zhu Q, Karki R, Guy CS, Vogel P, et al. IL-33 regulates the IgA-microbiota axis to restrain IL-1α-dependent colitis and tumorigenesis. J Clin Invest. (2016) 126:4469–81. doi: 10.1172/JCI88625
68. Gro P, Doser K, Falk W, Obermeier F, Hofmann C. IL-33 attenuates development and perpetuation of chronic intestinal inflammation. Inflamm Bowel Dis. (2012) 18:1900–9. doi: 10.1002/ibd.22900
69. McEntee CP, Finlay CM, Lavelle EC. Divergent roles for the IL-1 family in gastrointestinal homeostasis and inflammation. Front Immunol. (2019) 10:1266. doi: 10.3389/fimmu.2019.01266
70. Masterson JC, Capocelli KE, Hosford L, Biette K, McNamee EN, de Zoeten EF, et al. Eosinophils and IL-33 perpetuate chronic inflammation and fibrosis in a pediatric population with stricturing Crohn's ileitis. Inflamm Bowel Dis. (2015) 21:2429–40. doi: 10.1097/MIB.0000000000000512
71. Dias PM, Banerjee G. The role of Th17/IL-17 on eosinophilic inflammation. J Autoimmun. (2013) 40:9–20. doi: 10.1016/j.jaut.2012.07.004
72. Marichal T, Mesnil C, Bureau F. Homeostatic eosinophils: characteristics and functions. Front Med. (2017) 4:101. doi: 10.3389/fmed.2017.00101
73. Sugawara R, Lee E-J, Jang MS, Jeun E-J, Hong C-P, Kim J-H, et al. Small intestinal eosinophils regulate Th17 cells by producing IL-1 receptor antagonist. J Exp Med. (2016) 213:555–67. doi: 10.1084/jem.20141388
74. Chen H-H, Sun A-H, Ojcius DM, Hu W-L, Ge Y-M, Lin X, et al. Eosinophils from murine lamina propria induce differentiation of naïve T cells into regulatory T cells via TGF-β1 and retinoic acid. PLoS ONE. (2015) 10:e0142881. doi: 10.1371/journal.pone.0142881
75. Goto Y, Panea C, Nakato G, Cebula A, Lee C, Diez MG, et al. Segmented filamentous bacteria antigens presented by intestinal dendritic cells drive mucosal Th17 cell differentiation. Immunity. (2014) 40:594–607. doi: 10.1016/j.immuni.2014.03.005
76. Gaboriau-Routhiau V, Rakotobe S, Lécuyer E, Mulder I, Lan A, Bridonneau C, et al. The key role of segmented filamentous bacteria in the coordinated maturation of gut helper T cell responses. Immunity. (2009) 31:677–89. doi: 10.1016/j.immuni.2009.08.020
77. Hung Y-P, Tsai P-J, Hung K-H, Liu H-C, Lee C-I, Lin H-J, et al. Impact of toxigenic Clostridium difficile colonization and infection among hospitalized adults at a district hospital in southern Taiwan. PLoS ONE. (2012) 7:e42415. doi: 10.1371/journal.pone.0042415
78. Crobach MJT, Vernon JJ, Loo VG, Kong LY, Péchiné S, Wilcox MH, et al. Understanding Clostridium difficile colonization. Clin Microbiol Rev. (2018) 31: e00021–17. doi: 10.1128/CMR.00021-17
79. Rutala WA, Gergen MF, Weber DJ. Inactivation of Clostridium difficile spores by disinfectants. Infect Control Hosp Epidemiol. (1993) 14:36–9. doi: 10.1086/646628
80. Kovaleva J, Peters FTM, van der Mei HC, Degener JE. Transmission of infection by flexible gastrointestinal endoscopy and bronchoscopy. Clin Microbiol Rev. (2013) 26:231–54. doi: 10.1128/CMR.00085-12
81. Xu Q, Chen Y, Gu S, Lv T, Zheng B, Shen P, et al. Hospital-acquired Clostridium difficile infection in Mainland China: a seven-year (2009–2016) retrospective study in a large university hospital. Sci Rep. (2017) 7:9645. doi: 10.1038/s41598-017-09961-0
82. Saleh MM, Frisbee AL, Leslie JL, Buonomo EL, Cowardin CA, Ma JZ, et al. Colitis-induced Th17 cells increase the risk for severe subsequent Clostridium difficile infection. Cell Host Microbe. (2019) 25:756–65.e5. doi: 10.1016/j.chom.2019.03.003
83. Li Y, Xu H, Xu T, Xiao M, Tang H, Wu D, et al. Case–control study of inflammatory bowel disease patients with and without Clostridium difficile infection and poor outcomes in patients coinfected with C. difficile and cytomegalovirus. Dig Dis Sci. (2018) 63:3074–83. doi: 10.1007/s10620-018-5230-1
84. Issa M, Vijayapal A, Graham MB, Beaulieu DB, Otterson MF, Lundeen S, et al. Impact of Clostridium difficile on inflammatory bowel disease. Clin Gastroenterol Hepatol. (2007) 5:345–51. doi: 10.1016/j.cgh.2006.12.028
85. Aletaha N, Dadvar Z, Salehi B, Ketabi Moghadam P, Niksirat A, Jowkar A, et al. Clinical and pathological features of ulcerative colitis in patients with and without Clostridium difficile infection; an observational study. Middle East J Dig Dis. (2018) 11:17–23. doi: 10.15171/mejdd.2018.123
86. Ananthakrishnan AN, McGinley EL, Binion DG. Excess hospitalisation burden associated with Clostridium difficile in patients with inflammatory bowel disease. Gut. (2008) 57:205–10. doi: 10.1136/gut.2007.128231
87. Lowenkron SE, Waxner J, Khullar P, Ilowite JS, Niederman MS, Fein AM. Clostridium difficile infection as a cause of severe sepsis. Intensive Care Med. (1996) 22:990–4. doi: 10.1007/BF02044130
88. Eckel F, Huber W, Weiss W, Lersch C. Recurrent pseudomembranous colitis as a cause of recurrent severe sepsis. Z Gastroenterol. (2002) 40:255–8. doi: 10.1055/s-2002-25147
89. Khan KJ, Ullman TA, Ford AC, Abreu MA, Abadir A, Marshall JK, et al. Antibiotic therapy in inflammatory bowel disease: a systematic review and meta-analysis. Am J Gastroenterol. (2011) 106:661–73. doi: 10.1038/ajg.2011.72
90. Dai Y-X, Shi C-B, Cui B-T, Wang M, Ji G-Z, Zhang F-M. Fecal microbiota transplantation and prednisone for severe eosinophilic gastroenteritis. World J Gastroenterol. (2014) 20:16368–71. doi: 10.3748/wjg.v20.i43.16368
91. Feng T, Wang L, Schoeb TR, Elson CO, Cong Y. Microbiota innate stimulation is a prerequisite for T cell spontaneous proliferation and induction of experimental colitis. J Exp Med. (2010) 207:1321–32. doi: 10.1084/jem.20092253
92. Stepankova R, Powrie F, Kofronova O, Kozakova H, Hudcovic T, Hrncir T, et al. Segmented filamentous bacteria in a defined bacterial cocktail induce intestinal inflammation in SCID mice reconstituted with CD45RBhigh CD4+ T cells. Inflamm Bowel Dis. (2007) 13:1202–11. doi: 10.1002/ibd.20221
93. Britton GJ, Contijoch EJ, Mogno I, Vennaro OH, Llewellyn SR, Ng R, et al. Microbiotas from humans with inflammatory bowel disease alter the balance of gut Th17 and RORγt+ regulatory T cells and exacerbate colitis in mice. Immunity. (2019) 50:212–24.e4. doi: 10.1016/j.immuni.2018.12.015
94. Ivanov II, Atarashi K, Manel N, Brodie EL, Shima T, Karaoz U, et al. Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell. (2009) 139:485–98. doi: 10.1016/j.cell.2009.09.033
95. Burrello C, Giuffrè MR, Macandog AD, Diaz-Basabe A, Cribiù FM, Lopez G, et al. Fecal microbiota transplantation controls murine chronic intestinal inflammation by modulating immune cell functions and gut microbiota composition. Cells. (2019) 8:517. doi: 10.3390/cells8060517
96. Moayyedi P, Surette MG, Kim PT, Libertucci J, Wolfe M, Onischi C, et al. Fecal microbiota transplantation induces remission in patients with active ulcerative colitis in a randomized controlled trial. Gastroenterology. (2015) 149:102–9.e6. doi: 10.1053/j.gastro.2015.04.001
97. Costello SP, Hughes PA, Waters O, Bryant R V., Vincent AD, Blatchford P, et al. Effect of fecal microbiota transplantation on 8-week remission in patients with ulcerative colitis. JAMA. (2019) 321:156. doi: 10.1001/jama.2018.20046
98. Imdad A, Nicholson MR, Tanner-Smith EE, Zackular JP, Gomez-Duarte OG, Beaulieu DB, et al. Fecal transplantation for treatment of inflammatory bowel disease. Cochrane Database Syst Rev. (2018) 11:CD012774. doi: 10.1002/14651858.CD012774.pub2
99. Cammarota G, Ianiro G, Tilg H, Rajilić-Stojanović M, Kump P, Satokari R, et al. European consensus conference on faecal microbiota transplantation in clinical practice. Gut. (2017) 66:569–80. doi: 10.1136/gutjnl-2016-313017
100. Kostic AD, Xavier RJ, Gevers D. The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology. (2014) 146:1489–99. doi: 10.1053/j.gastro.2014.02.009
Keywords: eosinophilic colitis, Clostridioides difficile, intestinal inflammation, dysbiosis, sepsis, pathogenesis, intestinal eosinophilic infiltrate, hypereosinophilia
Citation: Iacob SA, Olariu MC and Iacob DG (2020) Eosinophilic Colitis and Clostridioides difficile Sepsis With Rapid Remission After Antimicrobial Treatment; A Rare Coincidence and Its Pathogenic Implications. Front. Med. 7:328. doi: 10.3389/fmed.2020.00328
Received: 30 October 2019; Accepted: 03 June 2020;
Published: 21 July 2020.
Edited by:
Nicola Petrosillo, Istituto Nazionale per le Malattie Infettive Lazzaro Spallanzani (IRCCS), ItalyReviewed by:
Guangqiang Wang, University of Shanghai for Science and Technology, ChinaCopyright © 2020 Iacob, Olariu and Iacob. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Diana Gabriela Iacob, ZGlhbmFnaWFjb2JAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.