
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Med., 15 May 2020
Sec. Infectious Diseases – Surveillance, Prevention and Treatment
Volume 7 - 2020 | https://doi.org/10.3389/fmed.2020.00226
This article is part of the Research TopicCoronavirus Disease (COVID-19): Pathophysiology, Epidemiology, Clinical Management and Public Health ResponseView all 400 articles
The coronavirus, COVID-19, has infected hundreds of thousands and killed tens of thousands of individuals worldwide. This highly infectious condition continues to ravage the world population and has yet to reach it peak infective rate in some countries. Many conventional drugs including hydroxychloroquine/chloroquine, lopinavir, remdesivir, etc., have been repurposed as treatments for this often deadly disease, but there is no specifically-designed effective drug available; also, the drugs mentioned have significant side effects and their efficacy is unknown. New drugs and vaccines are being designed as COVID-19 treatment, but their development and testing will require months to years. Time is not a luxury that this crisis has. Thus, there is a serious unmet need for the identification of currently-available and safe molecules which can be used to slow or treat COVID-19 disease. Here, we suggest melatonin be given consideration for prophylactic use or treatment alone or in combination with other drugs. Melatonin's multiple actions as an anti-inflammatory, anti-oxidant, and anti-viral (against other viruses) make it a reasonable choice for use. Melatonin is readily available, can be easily synthesized in large quantities, is inexpensive, has a very high safety profile and can be easily self-administered. Melatonin is endogenously-produced molecule in small amounts with its production diminishing with increased age. Under the current critical conditions, large doses of melatonin alone or in combination with currently-recommended drugs, e.g., hydroxychloroquine/chloroquine, to resist COVID-19 infection would seem judicious.
In the past 20 years, two coronavirus epidemics that originated in China caused large-scale pandemics that involved over 20 countries leading to ~8,000 cases and 800 deaths. In 2002 the Middle East respiratory syndrome coronavirus produced 2,500 cases with infection and caused 800 deaths. The coronavirus disease 2019 (COVID-19) is highly contagious and has quickly spread globally (1). Using mathematical models, the attack rate of COVID-19 suggests an estimate of reproduction (R0) to be 2–3 indicating that 60% of the population will likely become infected (2). As of March 31, 2020 there have been 777,798 cases of COVID-19 reported worldwide, with 37,272 fatalities (3).
The cardinal symptoms of COVID-19 are cough, fever, and shortness of breath. These symptoms appear 2–14 days after infection (4, 5). The clinical picture varies from pausymptomatic to more serious clinical situations such as severe respiratory failure, sepsis, shock, and multiple organ dysfunction syndrome (6). Currently, there is no specific treatment for COVID-19, so drugs need to be developed or reused to end the pandemic. The World Health Organization has launched a clinical trial called SOLIDARITY to investigate 4 potential treatments: lopinavir and ritonavir plus interferon-beta, lopinavir and ritonavir, chloroquine/hydroxychloroquine, and remdesivir (7). The medical profession has quickly realized that there is no cure for this disease and vaccines will not be available for several months. This leaves a large unmet need for safe and effective treatments for COVID-19-infected patients. Obviously, there is a very urgent need for a cheap, viable, and readily available treatment such as melatonin (8).
Melatonin is synthesized from tryptophan in the pineal gland and by almost all the organs of the body, since its production is associated with mitochondria. It is noteworthy that high levels of melatonin play positive roles in health and aging. Melatonin, a well-known chronobiotic, is also a promising adjunctive drug for viral infections due to its anti-inflammatory, antiapoptotic, immunomodulatory, and powerful antioxidant properties (8). Herein, we review the current evidence for a role of melatonin as a COVID-19 treatment. Since the clinical data is very limited, we propose the use of melatonin in patients with COVID-19 to reduce morbidity and mortality.
Little is known about the crucial factors of disease severity and immune alteration produced by COVID-19 infection in humans (9). Cytokines and chemokines play important roles in immunity, demonstrating that an exaggerated immune response causes lung damage and a greater probability of death. In individuals infected with COVID-19, interleukin (IL)−10, 6 and tumour necrosis factor (TNF) -α are increased during the disease. The more severe patients have very high levels of IL-10, IL-6, and TNFα; and fewer CD8+ and CD4+ T cells (9). Previous animal studies have shown that the cytokine storm dampens adaptive immunity against COVID-19 infection (10).
Chen et al. (11) have recently demonstrated immunological differences between moderate vs. severe COVID-19 patients. They demonstrate that CD8+ and CD4+ T cell numbers decrease significantly in patients with severe COVID-19. In patients with moderate COVID-19 the concentrations of IL-10, IL-6, and TNFα are within normal limits, and in the most severe patients they are very high. These cytokines are produced by macrophages and are involved in the cytokine storm (12). The cytokine storm magnifies the danger signal of the virus invasion, but also leads to destructive inflammation and host cell damage (13). In turn, the components released from damaged cells, particularly from stressed mitochondria, including mitochondrial DNA, cardiolipin, cytochrome C and also segments of nuclear DNA are recognized as damage associated molecular patterns by intra and intercellular immune molecules including toll-like receptors 4,7, and 9. Cyclic GMP-AMP synthase triggers a further large-scale proinflammatory cytokine release known as the “secondary cytokine storm”. If this vicious cycle is not interrupted, it results in widespread apoptosis, pyroptosis, and necrosis even of non-infected cells (13).
COVID-19 infection may attack the melatonin synthetic pathway resulting in reduced melatonin levels at a time when melatonin is most needed (14). The uncontrolled innate immune response promotes a massive inflammatory reaction and causes irreversible tissue damage and mortality. Melatonin is a potent antioxidant and immune regulator that not only suppresses oxidative stress but also controls the innate immune response and promotes the adaptive immune response (15, 16). The pineal gland produces and maintains the concentration of melatonin in the blood. The melatonin synthesized in the pineal gland is <5% of the total melatonin produced. The melatonin produced in the mitochondria is not discharged into the circulation, but is used by the cells that produce it (15). If patients do not generate sufficient amounts of melatonin their health status is likely compromised (16).
Autophagy plays an important role both in the antiviral defense responses and in the promotion of the different stages of the viral life cycle. The fact that melatonin is a regulator of autophagy due to its properties as a potent antioxidant and suppressor of endoplasmic reticulum stress suggests a potential beneficial role for this molecule in the management of some viral infections (17). Viruses, including Ebola, dengue, encephalomyocarditis, Venezuelan equine encephalitis, rabbit hemorrhagic disease, human papilloma, and inter alia, have demonstrated the success of melatonin in protecting against viral infections. There is no evidence that melatonin is viricidal but rather it reduces the severity of these infections (18–21). Melatonin's beneficial effects derive from its anti-inflammatory properties, free radical scavenging activity, and immunomodulatory functions.
Pharmaceutical laboratories are competing to identify vaccines for COVID-19. According to Benjami Neuman, a virologist, “it is difficult to immunize against the coronavirus, since there has never been a successful human vaccine against any member of the coronavirus family” (22).
The cytokine storm leads to acute cardiac injury, acute respiratory distress syndrome, and infection, leading to generalized sepsis and multisystem failure, which may lead to death (11, 12). Thus, preventing the cytokine storm may be key for the treatment of COVID-19 infected patients. Since there is a lack of effective therapies and immunological treatments may be insufficient, melatonin, owing to its multiple actions as summarized by Zhang et al. (8), may have beneficial effects in preventing or attenuating the cytokine storm and reducing morbidity and mortality from this disease.
A relationship between melatonin and aging has been suggested, due to a decrease in the concentration of nocturnal melatonin levels in the elderly (23). It has been hypothesized that melatonin can prolong life (24). The relationship of melatonin with aging involves three potential mechanisms: first, melatonin is a key molecule in regular circadian rhythms (25); second, melatonin prevents cardiolipin peroxidation and regulates the synthesis of mitochondrial proteins (26); finally, melatonin secreted by leukocytes exerts a powerful immunomodulatory function (24).
Wu and colleagues have recently shown that advanced age is a poor prognostic factor in patients with COVID-19. This is due to the fact that in the elderly their immune response and physiological functions are decreased as a result of age; therefore, they are more likely to develop severe pneumonia due to COVID-19 (25). Recent studies have shown that high levels of melatonin in the blood play a positive role in health and aging (27). These findings support a rationale for melatonin use in elderly suffering with COVID-19.
Aging is a biological process that contributes to an increase in cardiovascular morbidity and mortality. In the HEIJO-KYO cohort (cohort of elderly Japanese patients), urinary excretion of melatonin was associated with reduced nocturnal systolic blood pressure, independent of other cardiovascular risk factors. More precisely, an increase in urinary melatonin excretion from 4.2 to 10.5 μg caused a 2 mmHg decrease in nocturnal systolic blood pressure. Patients who took melatonin at a dose of 2–5 mg/day for 7–90 days uniformly showed a reduction in night-time blood pressure (28, 29).
Obesity is a risk factor for cardiovascular disease. In different studies, melatonin has been shown to have anti-obesity effects (30, 31). Taking melatonin reduces intra-abdominal visceral fat deposition and body weight. Its antiobesogenic effects are believed to be due to two processes: regulation of energy reserves and a relationship with the physiological processes of wakefulness/sleep rhythm (32).
Diabetes is a risk factor for the development of cardiovascular diseases. Several studies have shown a functional interaction between insulin and melatonin, showing that diabetic subjects have a lower concentration of melatonin (33). Furthermore, decreased blood melatonin levels have been documented in patients with insulin resistance or glucose intolerance (34). The results of several studies suggest that low melatonin production is associated with an increased risk of cardiovascular disease (35–37).
Several studies have shown that 75% of COVID-19 patients have 1 or 2 medical comorbidities (38, 39). Other authors have reported that patients with hypertension, obesity, and diabetes are more likely to develop more severe COVID-19 infection, including death (40). The occurrence of heart failure and myocardial infarction is plausible in these patients. The immune system of these patients is altered, with a reduced immune response (40). Furthermore, obesity contributes to various chronic diseases; decreased immunity and subsequently an increased risk of infection (41). Therefore, medical comorbidities are a risk factor for a poor prognosis for patients with COVID-19. Published reports routinely show that melatonin reduces the consequences of the comorbidities in patients with COVID-19.
While physiological melatonin concentrations in biological fluids oscillate between 10−10 and 10−11 M range, a concentration of 10−5 M is required to elicit significant pharmacological effects (42). Melatonin protects against cellular damage induced by reactive oxidative species, thus justifying the need of a more generous supplementation of exogenous melatonin in life-threatening pathologies. Oral melatonin use by humans is generally considered safe, with minor side effects including headache, drowsiness, etc. (43). To date, the best dose of melatonin in older adults has not been determined, as its endogenous levels are subject to altered pharmacokinetics. This causes intra-individual variability (44). In a meta-analysis of 50 studies, some of which were not blinded, the efficacy of oral melatonin administration (1–20 mg) was evaluated caused only a few minor adverse side effects, commonly fatigue, and drowsiness (45).
In elderly patients with medical comorbidities, treatment with melatonin is beneficial, as it strengthens the immune response. We suggest a daily dose of ~3 mg to a maximum of 10 mg, 30–60 min before bedtime to better simulate the normal physiological circadian rhythm of melatonin (Figure 1). Furthermore, it may be beneficial in people who are at high risk of contracting COVID-19 infection, local health workers, where preventive treatment with melatonin would favor maximizing the immune response, along with anti-inflammatory and antioxidant effects. A daily dose of roughly 40 mg or higher would not seem an inappropriate amount (Figure 1).
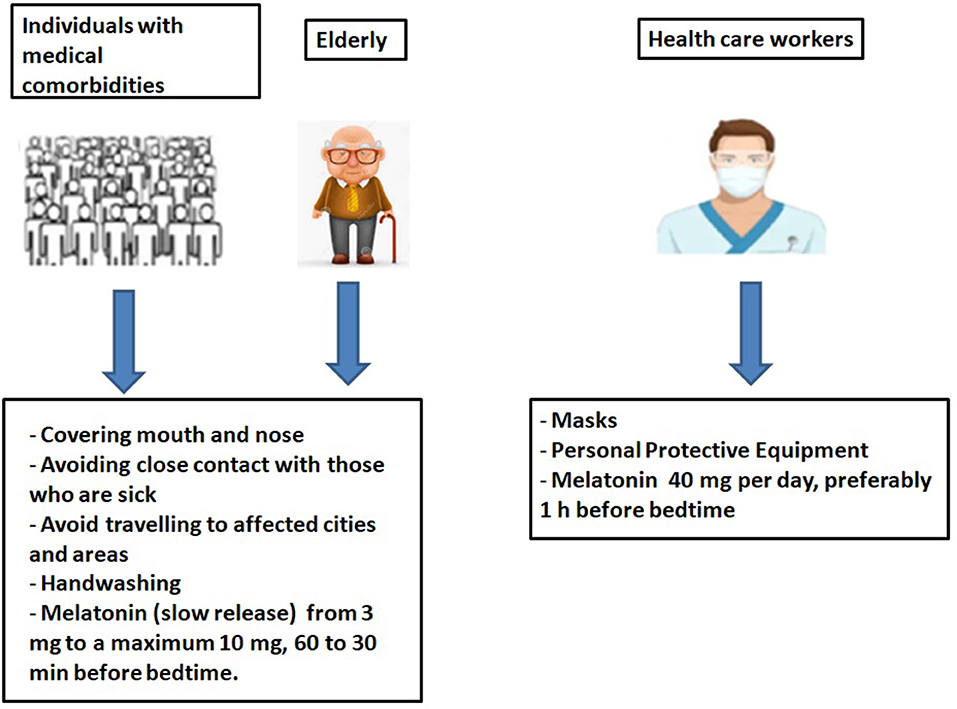
Figure 1. Prevention of COVID-19 infections in the elderly, in individuals with comorbidities and in health care workers.
The world is now facing a pandemic of COVID-19, for which no proven specific therapies are available, other than supportive care. In China, France, Spain, and Italy, a large number of patients have received compassionate use therapies. These therapies have been mostly given without controls, except for a few randomized trials initiated in China, and more recently in the US (46). In the 2014 Ebola outbreak, a randomized clinical trial was implemented and successfully launched during the outbreak; however, it was too late for the trials to be completed in time to be helpful to the currently or soon-to-be infective population (47). In our view, this tragedy cannot be repeated. The COVID-19 pandemic is catastrophic, even though different countries have implemented strict control measures.
Good medical practice requires the physician to use legally available medications according to knowledge-based evidence. If physicians use a product for an indication that is not currently approved, they must base its use on sound scientific reasons and sound medical evidence. Melatonin should be considered a treatment option for this deadly disease.
Melatonin has been shown to be clinically useful in sepsis (43), where the clinical features parallel those of COVID-19 viral infection; moreover, melatonin has been demonstrated to relieve many of the symptoms of other viral infections (17–21, 48). Given the current worldwide situation and in consideration of evidence-based medicine, the efficacy of melatonin and its high pharmacological safety profile supports its use in the treatment of infectious diseases, such as COVID-19. Melatonin can also be useful as a supplement with other treatment (hydroxychloroquine/chloroquine, lopinavir, remidisvir, etc).
Our research group has extensive experience in the use of melatonin in the context of cardiovascular physiology. Melatonin can be administered at a total dose of at least 120 to 1,000 μg/kg/subject weight and intravenously with a high safety profile (36, 37). An aggressive approach is required to prevent coronavirus disease progression and mechanical ventilation. Nordlund and Lerner (49) published a report years ago in which he gave humans one gram of melatonin daily for a month with no untoward effect. Melatonin has a large safety margin without serious adverse effects.
Our doses are based in an article recently published by Ramos et al. (50). The authors demonstrated that when we extrapolated effective animal doses to human for a 70 kg adult, the results ranged from 19 to 1,527 mg per day. As there is no time or clinical trials to test the efficacy of melatonin at different concentrations, we suggest the use of melatonin (100 or 400 mg per day) as an adjunct, especially if no efficient direct anti-viral treatment is available (Figure 2).
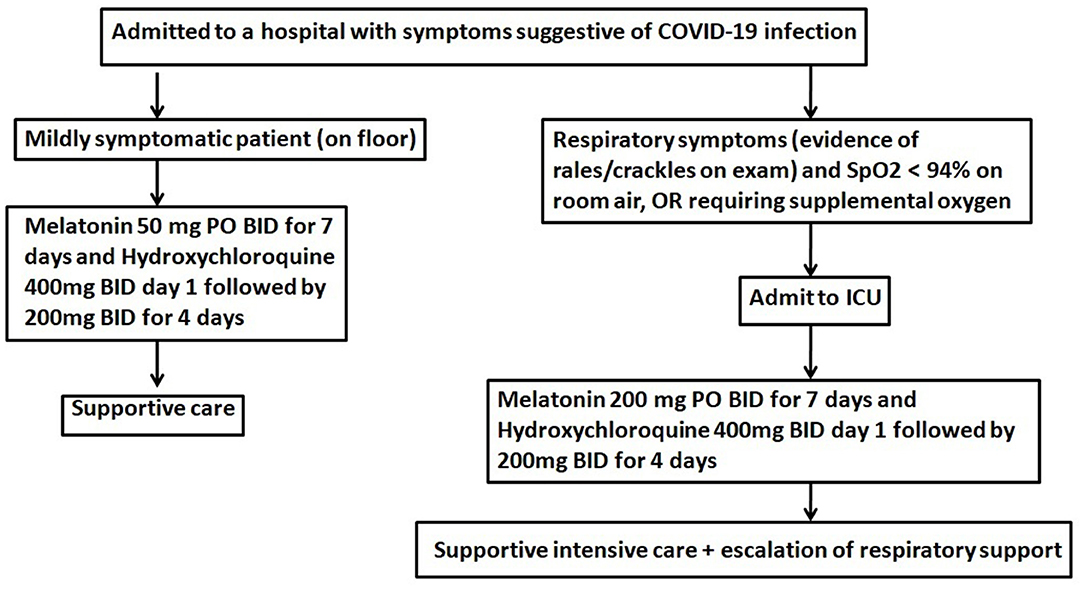
Figure 2. Therapeutic algorithm for use of melatonin in patients with COVID-19. Melatonin will likely reduce the toxicity of chloroquine and increase its efficacy. BID, twice daily; PO, per oral.
The COVID-19 pandemic has infected hundreds of thousands and killed tens of thousands of individuals worldwide. Time is not a luxury that this crisis has. The high mortality is caused by the uncontrolled innate immune response and destructive inflammation. Melatonin is a molecule that negatively regulates the overreaction of the innate immune response and excess inflammation, promoting adaptive immune activity. Moreover, the indole is an endogenous molecule, produced in small amounts, whose synthesis diminishes with increased age. These finding, together with those recently summarized by Anderson and Reiter (51) and Zhang et al. (8), support the use of melatonin in patients with COVID-19. We agree with the suggestion by those authors that melatonin should be given consideration for prophylactic use or treatment alone or in combination with other drugs, and propose a therapeutic algorithm for use in patients. Melatonin is readily available, can be easily synthesized in large quantities, is inexpensive, has a very high safety profile and can be easily self-administered.
RR: conceptualization, writing-review, and editing. PA-G and PM: writing-review and editing. AD-R: resources, writing original draft, review, and editing. All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
This research was funded by Fundación Canaria Instituto de Investigación Sanitaria de Canarias (FIISC) (PIFUN11/18).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Chafekar A, Fielding BC. MERS-CoV: understanding the latest human coronavirus threat. Viruses. (2018) 10:E93. doi: 10.3390/v10020093
2. Flahault A. Has China faced only a herald wave of SARS-CoV-2? Lancet. (2020) 395:947. doi: 10.1016/S0140-6736(20)30521-3
3. European Centre for Disease Prevention Control,. (2020). Available online at: https://www.ecdc.europa.eu/en/novel-coronavirus-china (accessed March 31, 2020).
4. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032
5. Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. (2020) 382:1177–9. doi: 10.1056/NEJMc2001737
6. Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med. (2020). doi: 10.1007/s00134-020-06022-5. [Epub ahead of print].
7. Mahase E. Covid-19: what treatments are being investigated? BMJ. (2020) 368:m1252. doi: 10.1136/bmj.m1252
8. Zhang R, Wang X, Ni L, Di X, Ma B, Niu S, et al. COVID-19: Melatonin as a potential adjuvant treatment. Life Sci. (2020) 250:11758. doi: 10.1016/j.lfs.2020.117583
9. Diao B, Wang C, Tan Y, Chen X, Liu Y, Ning L, et al. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19). Front. Immunol. (2020) 11:827. doi: 10.3389/fimmu.2020.00827
10. Channappanavar R, Fehr AR, Vijay R, Mack M, Zhao J, Meyerholz DK, et al. Dysregulated type I interferon and inflammatory monocyte-macrophage responses cause lethal pneumonia in SARS-CoV-infected mice. Cell Host Microbe. (2016) 19:181–93. doi: 10.1016/j.chom.2016.01.007
11. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunologic features in severe and moderate coronavirus disease 2019. J Clin Invest. (2020) 130:2620–29. doi: 10.1172/JCI137244
12. Liao M, Yang L, Yuan J, Wen Y, Xu G, Zhao J, et al. The landscape of lung bronchoalveolar immune cells in COVID-19 revealed by single-cell RNA sequencing. medRxiv. (2020). doi: 10.1101/2020.02.23.20026690. [Epub ahead of print].
13. Huo C, Jin Y, Zou S, Qi P, Xiao J, Tian H, et al. Lethal influenza A virus preferentially activates TLR3 and triggers a severe inflammatory response. Virus Res. (2018) 257:102–12. doi: 10.1016/j.virusres.2018.09.012
14. Grunewald ME, Shaban MG, Mackin SR, Fehr AR, Perlman S. Murine coronavirus infection activates the aryl hydrocarbon receptor in an indoleamine 2,3-dioxygenase-independent manner, contributing to cytokine modulation and proviral TCDD-inducible-PARP expression. J Virol. (2020) 94:e01743–19. doi: 10.1128/JVI.01743-19
15. Huang H, Liu X, Chen D, Lu Y, Li J, Du F, et al. Melatonin prevents endothelial dysfunction in SLE by activating the nuclear receptor retinoic acid-related orphan receptor-α. Int Immunopharmacol. (2020) 83:106365. doi: 10.1016/j.intimp.2020.106365
16. Sedova KA, Bernikova OG, Cuprova JI, Ivanova AD, Kutaeva GA, Pliss MG, et al. Association between antiarrhythmic, electrophysiological, and antioxidative effects of melatonin in ischemia/reperfusion. Int J Mol Sci. (2019) 20:E6331. doi: 10.3390/ijms20246331
17. Boga JA, Caballero B, Potes Y, Perez-Martinez Z, Reiter RJ, Vega-Naredo I, et al. Therapeutic potential of melatonin related to its role as an autophagy regulator: a review. J Pineal Res. (2019) 66:e12534. doi: 10.1111/jpi.12534
18. Anderson G, Maes M, Markus RP, Rodriguez M. Ebola virus: melatonin as a readily available treatment option. J Med Virol. (2015) 87:537–43. doi: 10.1002/jmv.24130
19. Paemanee A, Hitakarun A, Roytrakul S, Smith DR. Screening of melatonin, α-tocopherol, folic acid, acetyl-L-carnitine and resveratrol for anti-dengue 2 virus activity. BMC Res Notes. (2018) 11:307. doi: 10.1186/s13104-018-3417-3
20. Crespo I, Miguel BS, Laliena A, Alvarez M, Culebras JM, González-Gallego J, et al. Melatonin prevents the decreased activity of antioxidant enzymes and activates nuclear erythroid 2-related factor 2 signaling in an animal model of fulminant hepatic failure of viral origin. J Pineal Res. (2010) 49:193–200. doi: 10.1111/j.1600-079X.2010.00787.x
21. Valero N, Mosquera J, Alcocer S, Bonilla E, Salazar J, Álvarez-Mon M. Melatonin, minocycline and ascorbic acid reduce oxidative stress and viral titers and increase survival rate in experimental Venezuelan equine encephalitis. Brain Res. (2015) 1622:368–76. doi: 10.1016/j.brainres.2015.06.034
22. MedicalXpress Breaking News and Events. Coronavirus Drugs: Who's. (2020). Available online at: www.mdlinx.com/painmanagement/top-medical-news/article/index.cfm/?publish_dt=03-17-2020&rowNum=7621393&_rw=true&utm_source=alert&utm_medium=email&utm_~campaign=ajm_49664& (accessed March 16, 2020).
23. Duffy JF, Zitting KM, Chinoy ED. Aging and circadian rhythms. Sleep Med Clin. (2015) 10:423–34. doi: 10.1016/j.jsmc.2015.08.002
24. Pandi-Perumal SR, BaHammam AS, Brown GM, Spence DW, Bharti VK, Kaur C, et al. Melatonin antioxidative defense: therapeutical implications for aging and neurodegenerative processes. Neurotox Res. (2013) 23:267–300. doi: 10.1007/s12640-012-9337-4
25. Wu J, Li W, Shi X, Chen Z, Jiang B, Liu J, et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J Intern Med. (2020). doi: 10.1111/joim.13063. [Epub ahead of print].
26. Majidinia M, Reiter RJ, Shakouri SK, Mohebbi I, Rastegar M, Kaviani M, et al. The multiple functions of melatonin in regenerative medicine. Ageing Res Rev. (2018) 45:33–52. doi: 10.1016/j.arr.2018.04.003
27. Hardeland R. Melatonin and the theories of aging: a critical appraisal of melatonin's role in antiaging mechanisms. J Pineal Res. (2013) 55:325–56. doi: 10.1111/jpi.12090
28. Obayashi K, Saeki K, Tone N, Kurumatani N. Relationship between melatonin secretion and nighttime blood pressure in elderly individuals with and without antihypertensive treatment: a cross-sectional study of the HEIJO-KYO cohort. Hypertens Res. (2014) 37:908–13. doi: 10.1038/hr.2014.99
29. Borghi C, Cicero AF. Nutraceuticals with a clinically detectable blood pressure-lowering effect: a review of available randomized clinical trials and their meta-analyses. Br J Clin Pharmacol. (2017) 83:163–71. doi: 10.1111/bcp.12902
30. Gubin DG, Gubin GD, Gapon LI, Weinert D. Daily melatonin administration attenuates age-dependent disturbances of cardiovascular rhythms. Curr Aging Sci. (2016) 9:5–13. doi: 10.2174/1874609809666151130220011
31. Imenshahidi M, Karimi G, Hosseinzadeh H. Effects of melatonin on cardiovascular risk factors and metabolic syndrome: a comprehensive review. Naunyn Schmiedebergs Arch Pharmacol. (2020) 393:521–36. doi: 10.1007/s00210-020-01822-4
32. Prado NJ, Ferder L, Manucha W, Diez ER. Anti-inflammatory effects of melatonin in obesity and hypertension. Curr Hypertens Rep. (2018) 20:45. doi: 10.1007/s11906-018-0842-6
33. Cipolla-Neto J, Amaral FG, Afeche SC, Tan DX, Reiter RJ. Melatonin, energy metabolism, and obesity: a review. J Pineal Res. (2014) 56:371–81. doi: 10.1111/jpi.12137
34. Reutrakul S, Sumritsopak R, Saetung S, Chanprasertyothin S, Chailurkit LO, Anothaisintawee T. Lower nocturnal urinary 6-sulfatoxymelatonin is associated with more severe insulin resistance in patients with prediabetes. Neurobiol Sleep Circadian Rhythms. (2017) 4:10–6. doi: 10.1016/j.nbscr.2017.06.001
35. Dominguez-Rodriguez A, Abreu-Gonzalez P, Piccolo R, Galasso G, Reiter RJ. Melatonin is associated with reverse remodeling after cardiac resynchronization therapy in patients with heart failure and ventricular dyssynchrony. Int J Cardiol. (2016) 221:359–63. doi: 10.1016/j.ijcard.2016.07.056
36. Dominguez-Rodriguez A, Abreu-Gonzalez P, de la Torre-Hernandez JM, Consuegra-Sanchez L, Piccolo R, Gonzalez-Gonzalez J, et al. Usefulness of early treatment with melatonin to reduce infarct size in patients with ST-segment elevation myocardial infarction receiving percutaneous coronary intervention (from the melatonin adjunct in the acute myocardial infarction treated with angioplasty trial). Am J Cardiol. (2017) 120:522–6. doi: 10.1016/S0735-1097(17)34668-5
37. Dominguez-Rodriguez A, Abreu-Gonzalez P, de la Torre-Hernandez JM, Gonzalez-Gonzalez J, Garcia-Camarero T, Consuegra-Sanchez L, et al. Effect of intravenous and intracoronary melatonin as an adjunct to primary percutaneous coronary intervention for acute ST-elevation myocardial infarction: results of the melatonin adjunct in the acute myocardial infarction treated with angioplasty trial. J Pineal Res. (2017) 62. doi: 10.1111/jpi.12374
38. MacLaren G, Fisher D, Brodie D. Preparing for the most critically Ill patients with COVID-19: the potential role of extracorporeal membrane oxygenation. JAMA. (2020). doi: 10.1001/jama.2020.2342. [Epub ahead of print].
39. Tong ZD, Tang A, Li KF, Li P, Wang HL, Yi JP, et al. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerg Infect Dis. (2020) 26:1052–4. doi: 10.3201/eid2605.200198
40. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. (2020). doi: 10.1001/jamacardio.2020.1286. [Epub ahead of print].
41. Huttunen R, Syrjänen J. Obesity and the risk and outcome of infection. Int J Obes. (2013) 37:333–40. doi: 10.1038/ijo.2012.62. [Epub ahead of print].
42. Nogueira LM, Sampson JN, Chu LW, Yu K, Andriole G, Church T, et al. Individual variations in serum melatonin levels through time: implications for epidemiologic studies. PLoS ONE. (2013) 8:e83208. doi: 10.1371/journal.pone.0083208
43. Colunga Biancatelli RML, Berrill M, Mohammed YH, Marik PE. Melatonin for the treatment of sepsis: the scientific rationale. J Thorac Dis. (2020) 12 (Suppl 1):S54–S65. doi: 10.21037/jtd.2019.12.85
44. Vural EM, van Munster BC, de Rooij SE. Optimal dosages for melatonin supplementation therapy in older adults: a systematic review of current literature. Drugs Aging. (2014) 31:441–51. doi: 10.1007/s40266-014-0178-0
45. Foley HM, Steel AE. Adverse events associated with oral administration of melatonin: a critical systematic review of clinical evidence. Complement Ther Med. (2019) 42:65–81. doi: 10.1016/j.ctim.2018.11.003
46. Adaptive COVID-19 Treatment Trial,. ClinicalTrials.gov identifier: NCT04280705 (2020). Available online at: https://clinicaltrials.gov/ct2/show/NCT04280705?term=remdesivir&cond=covid-19&draw=2&rank=5 (accessed April 02, 2020).
47. Davey RT Jr, Dodd L, Proschan MA, Neaton J, Neuhaus Nordwall J, Koopmeiners JS, et al. A randomized, controlled trial of ZMapp for Ebola Virus infection. N Engl J Med. (2016) 375:1448–56. doi: 10.1056/NEJMoa1604330
48. Zhou Y, Hou Y, Shen J, Huang Y, Martin W, Cheng F. Network-based drug repurposing for novel coronavirus 2019-nCov/SARS-CoV-2. Cell Discov. (2020) 6:14. doi: 10.1038/s41421-020-0153-3
49. Nordlund JJ, Lerner AB. The effects of oral melatonin on skin color and on the release of pituitary hormones. J Clin Endocrinol Metab. (1977) 45:768–74. doi: 10.1210/jcem-45-4-768
50. Ramos E, Farré-Alins V, Egea J, López-Muñoz F, Reiter RJ, Romero A. Melatonin's efficacy in stroke patients; a matter of dose? A systematic review. Toxicol Appl Pharmacol. (2020) 392:114933. doi: 10.1016/j.taap.2020.114933
Keywords: melatonin, COVID-19, SARS-CoV-2, treatment-drug, prevention & control
Citation: Reiter RJ, Abreu-Gonzalez P, Marik PE and Dominguez-Rodriguez A (2020) Therapeutic Algorithm for Use of Melatonin in Patients With COVID-19. Front. Med. 7:226. doi: 10.3389/fmed.2020.00226
Received: 06 April 2020; Accepted: 04 May 2020;
Published: 15 May 2020.
Edited by:
Zisis Kozlakidis, International Agency for Research on Cancer (IARC), FranceReviewed by:
Irene Crespo, University of León, SpainCopyright © 2020 Reiter, Abreu-Gonzalez, Marik and Dominguez-Rodriguez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Russel J. Reiter, cmVpdGVyQHV0aHNjc2EuZWR1; Alberto Dominguez-Rodriguez, YWRydmRnQGhvdG1haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.