
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Med., 21 August 2019
Sec. Dermatology
Volume 6 - 2019 | https://doi.org/10.3389/fmed.2019.00180
This article is part of the Research TopicRecent Developments in Therapies and Diagnostic Tools for Melanoma and Non-melanoma Skin CancerView all 15 articles
Dermoscopy is a widely used non-invasive technique for diagnosing skin tumors. In melanocytic tumors, e.g., melanoma and basal cell carcinoma (BCC), the effectiveness of dermoscopic examination has been fully established over the past two decades. Moreover, dermoscopy has been used to diagnose non-melanocytic tumors. Here, we review novel findings from recent reports concerning dermoscopy of melanoma and non-melanoma skin cancers including BCC, sebaceous carcinoma, actinic keratosis, Bowen's disease, squamous cell carcinoma (SCC), Merkel cell carcinoma (MCC), extramammary Paget's disease (EMPD), and angiosarcoma.
Dermoscopy is a non-invasive technique for diagnosing skin lesions, which aids in the differentiation between benign and malignant alterations. Dermoscopy has been used to diagnose non-melanocytic tumors. Recently, vascular morphology has been identified as an important criteria in dermoscopic diagnosis when assessing non-melanocytic tumors. Here, we review recent reports of novel findings related to dermoscopy of melanoma and non-melanoma skin cancers.
Dermoscopy has been shown to improve significantly the diagnosis of melanocytic lesions in the clinical practice. Following the Consensus Net Meeting on Dermoscopy in 2000, a two-step algorithm for a method of dermoscopic diagnostic was established, especially for pigmented skin lesions (1). Marghoob and Braun subsequently devised a revised two-step algorithm including polarized dermoscopy and blood vessel morphology (2). In the second step of the revised algorithm, pattern analysis, the ABCD rule, the Menzies method (3), and the seven-point checklist are employed to diagnose melanoma. The seven-point checklist is based on seven melanoma-specific criteria; each is classified as major or minor. Major criteria consist of atypical networks, blue-whitish veils, and atypical vascular patterns while minor criteria are irregular dots/globules, irregular streaks, irregular blotches, and regression structures. A score of 2 is given to each of the major criteria, whereas a score of 1 is given to each of the minor criteria. Results yielding 3 points or more should be considered suspicious enough to justify exclusion.
The differential diagnoses related to lentigo maligna (LM) and lentigo maligna melanoma (LMM) include a myriad of other pigmented skin lesions, including solar lentigo, seborrheic keratosis, and pigmented actinic keratosis. While the pigment network is the dermoscopic hallmark of superficial spreading melanoma (SSM) located on the trunk and extremities, a true pigment network is rarely found in LM. A pseudonetwork pattern refers to the common dermoscopic finding of melanocytic and non-melanocytic pigmented macules of the face; it is a structureless diffuse brown pigmentation interrupted by numerous, variably broad, and hypopigmented holes, which correspond to hair follicles and sweat gland openings. Based on a report by Schiffner et al., the four most important features are asymmetric pigmented follicular openings, dark rhomboidal structures, slate-gray globules, and slate-gray dots. This analysis yields a sensitivity of 89% and a specificity of 96% (4).
Considering that most dermoscopic features have been described in the context of SMM, the dermoscopic recognition of nodular melanoma (NM) is also challenging since the tumor often lacks the well-known melanoma-specific criteria. Therefore, several accepted dermoscopic criteria of melanoma are not detected in purely nodular tumors.
Argenziano et al. described a new predictor of NM, namely the presence of blue-black color within the lesion (5). The blue-black color is thought to reflect the combination of pigments localized in the mid-deep dermis (blue) and the epidermis (black). The authors reported that all lesion surfaces that were comprised of at least 10% blue and black areas were significantly associated with pigmented NM. Moreover, Pizzichetta et al. reported NM was related to features such as ulceration, homogeneous disorganized patterns, homogeneous blue-pigmented structureless areas, multiple (≥3) colors, the combination of polymorphous vessels and milky-red globules/areas, and symmetric shapes (6).
Saida et al. reported dermoscopic patterns of acral melanoma in the Japanese population (7). They found that the parallel ridge pattern (PRP) is the most specific dermoscopic finding for acral melanomas. PRP consists of a band-like pigmentation located on the ridges of the skin markings. In their report, the sensitivity and specificity of PRP for acral melanoma were 86.4 and 99%, respectively. In additional studies, Phan et al. and Ozdemir et al. reported that PRP was detectable in 53 and 60.8% of their cases (8, 9). Lallas et al. proposed the BRAAFF checklist, a score composed of four positive features, i.e., irregular blotches, PRP, asymmetry of structures, and asymmetry of colors, and two negative features such as the parallel furrow pattern (PFP) and fibrillar pattern. Based on the results of the BRAAFF checklist, they proposed a dermoscopic diagnostic algorithm that achieves 93.1% sensitivity and 86.7% specificity for acral melanoma diagnosis (10).
It is difficult to differentiate melanoma from melanocytic nevus if PRP or PFP is not observed. In melanoma on the volar skin without typical dermoscopic patterns, Mikoshiba et al. recently reported frequently observed features consisting of asymmetry, greater numbers of colors (≥3), irregular distribution of blue-white structures, dots and globules, vascular structures including milky red areas, ulcers, diffuse pigmentation, and irregular streaks (11).
Important dermoscopic features of nail apparatus (so-called subungual) melanoma include irregular lines on a brown background, micro-Hutchinson's sign triangular pigmentation on the nail plate, and a wide pigmented band (12). The width of pigmentation is an important risk factor. Ohn et al. reported the following factors to be associated with adult-onset in situ lesions: width of pigmentation ≥3 mm, width of pigmentation ≥6 mm (the minimum 6-mm width was more strongly associated with melanoma), multicolor pigmentation, asymmetry, border fading, and the Hutchinson sign (13). Moreover, Benati et al. reported that a width more than 2/3 of the nail plate suggested melanoma (14). They also reported that the second most important predictor of nail apparatus melanoma was the presence of gray to black color. This gray to black color was associated with 12.5% of nevus and 76% of nail apparatus melanoma.
Clinically, age is important to differentiate melanoma from melanocytic nevus. Most cases of nail apparatus melanoma are diagnosed in adults. Caution must be observed before diagnosing nail apparatus melanoma in children because irregular findings are frequently observed in the benign nevus of nails in children.
Amelanotic melanomas are a relatively rare subtype of melanomas with little or no pigment at visual inspection. Since the majority of melanoma-associated dermoscopic structures are pigmented, amelanotic melanomas remain a demanding diagnostic. The atypical vascular structures are frequently the only clue for its diagnosis (15, 16). Therefore, diagnosis and treatment are often delayed. Menzies et al. reported that the dermoscopically diagnostic accuracy of hypomelanotic or amelanotic melanomas was inferior to that of pigmented melanoma (15). In a recent study of amelanotic melanomas, Lin et al. reported polymorphous vessels as common features in 20 of 27 melanomas. However, in truly amelanotic melanomas, the vascular pattern of polymorphous vessels may not suffice as an only feature utilized to diagnose amelanotic melanoma since it is also found in other skin cancers (16).
The value of dermoscopy of basal cell carcinoma (BCC) has been extensively demonstrated over the past few decades. Menzies et al. reported the sensitivity of diagnostic criteria for pigmented BCC was 97% (17). The dermoscopic criteria associated with BCCs include the absence of a pigment network and the presence of specific features, e.g., arborizing vessels, large blue-gray ovoid nests, multiple blue-gray globules, leaf-like areas, spoke wheel areas, and ulceration. In reports from Menzies et al. and Altamura et al., arborizing vessels (52% in Menzies et al., 48.5% in Altamura et al.), large blue-gray ovoid nests (55%, 60.8%), multiple blue-gray globules (27%, 38.5%), leaf-like areas (17%, 22.7%), spoke wheel areas (10%, 13.1%), and ulceration (27%, 34.6%) were dermoscopically observed in pigmented BCCs (17, 18). Additional features have been reported recently, specifically multiple small erosions, shiny white streaks, and concentric structures (19–23). Altamura et al. reported that multiple small erosions were seen in 14.1% of non-pigmented BCCs (18), whereas shiny white streaks have been seen only in polarized dermoscopy (22, 24). Moreover, vascular patterns such as short fine telangiectasias (SFTs), arborizing microvessels, and milky-pink backgrounds have been reported, and these patterns may be useful particularly for non-pigmented BCCs. SFTs are small vessels without branches. Micantonio et al. (20) and Emiroglu et al. (25) reported that SFTs were the second most common vascular pattern found in BCCs. These telangiectasias were significantly more common in superficial BCCs than in nodular BCCs (20). Additionally, Pan et al. reported that arborizing microvessels, short, bright red, sharply focused, fine-caliber branching vessels, were seen in 62% of superficial BCCs (26). Reports on milky-pink backgrounds indicated that they were more common in superficial BCCs (21, 25–27).
Dermoscopic characteristics for each BCC subtype have been described. Some reports differentiated between superficial BCC and other subtypes by dermoscopy (19, 24, 25). In superficial BCC, maple leaf-like areas, spoke wheel areas, SFTs, multiple small erosions, and concentric structures were frequently observed (17–19, 23). Ahnlide et al. (23) summarized dermoscopic features in the common subtype of BCC, including superficial BCC (n = 202), nodular BCC (n = 76), and infiltrated BCC (n = 142) (Table 1). Based on their reports, both in nodular and infiltrated BCCs, arborizing vessels were the most common, while ulcerations were the second most common findings. Moreover, Lallas et al. reported that blue-gray ovoid nests may be predictors for non-superficial BCCs. According to their findings, both arborizing vessels and ulcerations would exclude superficial BCC (19).
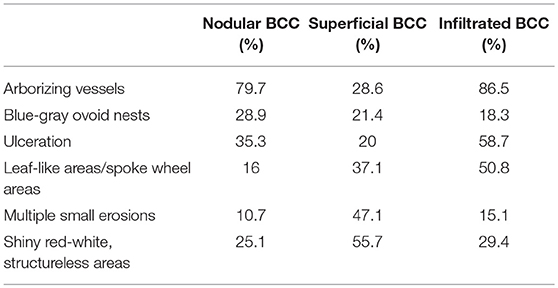
Table 1. Dermoscopic features in subtype of BCC in the report of Ahnlide et al. (23).
Although the common clinical presentation of sebaceous carcinoma (SC) is a yellow or red nodule, clinical diagnosis is challenging due to the absence of criteria for dermoscopic diagnosis (28, 29). The main dermoscopic features of SC are yellowish structures, polymorphous vessels, ulcerations, and whitish-pink areas (30–36) (Table 2). The most common findings are yellowish structures, i.e., background, globules and yellow/yellowish areas, which were described as the heterogeneously distributing yellowish objects with varying size, shape and number in the literatures. Polymorphous vessels and ulceration are the second most common appearances. Polymorphous vessels were reported as the combination of various types of vessels, i.e., linear irregular vessels, hairpin vessels, comma-like vessels, dotted vessels, arborizing vessels, and telangiectasias. Ulcerations or crusts on the surface of the tumor suggest the possibility of malignancy, which might help distinguish SC from the benign sebaceous tumors. Whitish-pink areas were described as the homogeneous white-to-pink background (35). Dermoscopically, benign sebaceous tumors should be differentiated from SC. Benign sebaceous tumors are classified as sebaceous hyperplasia, sebaceous adenoma, and sebaceoma (31). Sebaceous hyperplasia consists of a white-yellow, umbilicated, structureless center, radially arranged yellow globules, and peripheral telangiectasias (crown vessels). The absence of polymorphous vessels and ulcerations might be helpful to differentiate from SC.
A grading classification of actinic keratosis (AK) has been proposed based on clinical criteria (37). Grade I (mild) consists of slightly palpable AK, grade II (moderate) exhibits readily palpable and visible AK and grade III (severe) is characterized by very thick and hyperkeratotic AK. This clinical classification of AK corresponds to dermoscopic characteristics (38–42). In grade I, red pseudonetwork patterns and white scales are seen. In grade II, a strawberry pattern is typical. The strawberry pattern results from an erythematous background with white-to-yellow keratotic and dilated follicular openings. In addition, targetoid hair follicles are also seen in grade II (43). In grade III, either enlarged follicular plugs filled with keratotic plugs over a white to yellow background or marked hyperkeratosis are observed.
AKs cannot always be distinguished from SCC in situ or invasive SCC. Vascular patterns may be helpful concerning this. Casari et al. reported that the increasing atypia is usually associated with dotted vessels around follicles in severe AKs (44). Therefore, enlarging dotted vessels, forming glomerular vessels were seen in situ SCC. With the progression to invasive SCC, hairpin and/or linear-irregular vessels will appear.
In pigmented AK, the most typical dermoscopic structure is the superficial brown network consisting of brown, curved double lines that surround enlarged, partially confluent, keratotic follicles of various sizes. Pigmented AK may also reveal an annular-granular pattern and pseudonetwork and rhomboidal structures, which are also seen in lentigo maligna (45). The annular-granular pattern in pigmented AK tends to be more prominent and keratin may be observed in the follicular openings. Moreover, the strawberry sign, rosette pattern, and scale may help to distinguish AK from LM when making a diagnosis (43).
The dermoscopic characteristics of Bowen's disease (BD) were first described in 2004 (46).
Based on several studies, glomerular vessels (69–97%) and scaly white-to-yellow surfaces (64–96%) were commonly observed in non-pigmented BD (26, 46–50). Brown to gray globules/dots and structureless pigmentation were observed in 21–80% and 70–78% of pigmented BD, respectively (46, 48, 50, 51). These pigmented globules/dots are often distributed at the periphery, sometimes exhibiting a streak-like or leaf-like structure. However, these are not specific to pigmented BD. Chung et al. reported that streak-like structures did not converge toward the center of the lesion, nor did they connect to a common base and therefore may be distinguished from those seen in melanocytic lesions or in BCCs (52). Recently, Yang et al. found two new dermoscopic signs by analyzing 146 lesions of BD (49). One was parallel pigmented edges at the periphery of the lesion, named the double-edge sign. The other was several aggregated large pigmented massive structures, often distributed at the periphery of the lesion, named clusters of brown structureless areas. The former was observed in 44 of 146 lesions (30.1%), and the latter was in 56 (38.4%).
In rare occasions, BD develops in the nail, periungually, in the fingers and palm, often displaying the type of pigmented BD (53–55). Nakayama et al. reported four cases of periungual pigmented BD (53). Histologically, dilated vessels in the papillary dermis corresponding to a dermoscopic finding of glomerular vessels were observed, but none of the four cases presented glomerular vessels upon dermoscopic examination. They speculated that acral skin has a thicker stratum corneum than other skin, so papillary vessels might not be detectable by dermoscopy. In addition, the PFP was found in two of four cases, while the PRP was not found in any case. Similarly, Cavicchini et al. reported a case of pigmented BD developing in the palm that showed a PFP (54). The presence of the scaly surface and the lack of the PRP may distinguish acral BD from acral melanoma. Regarding BD developed in the fingernails, several case reports described subungual BD presented longitudinal melanonychia (55–57). Additionally, Hutchinson's sign was also observed in some reports (53, 58, 59).
Dermoscopic criteria for squamous cell carcinoma (SCC) include the presence of keratin/scales, blood spots, white circles, white structureless areas, hairpin vessels, linear-irregular vessels perivascular white halos, and ulceration (39, 60, 61). Keratin and scales are homogeneous opaque yellow to brown structures, corresponding to hyperkeratosis and parakeratosis (60, 62). Blood spots are the multiple red to black dots in the keratin mass, corresponding to small crusts or hemangiomas (60). White circles are the bright white circles surrounding a dilated infundibulum corresponding to acanthosis and hypergranulosis of the infundibular epidermis (62). White structureless areas are the whitish areas covering large areas of tumors, corresponding to large targetoid hair follicles (39, 63). Among the criteria discussed above, keratin and white circles reached the sensitivity and specificity for SCC diagnostic at a rate of 79 and 87%, respectively (60). The presence of vessels in more than half of the tumor's surface with a diffuse distribution of vessels and bleeding significantly increased the possibility of poorly differentiated SCC. Conversely, keratin/scales are a potent predictor of well- and moderately differentiated SCC (64). However, Pyne et al. reported that moderately and poorly differentiated SCC displayed more branched and serpentine vessels than well-differentiated SCC and that moderately and poorly differentiated SCC displayed larger numbers of vessel types than well-differentiated SCC (61). Regarding lip SCC, Benati et al. recently reported that scales, white structureless areas, and white halos were observed in the majority of the cases (100, 91, and 86%, respectively) (65).
Several recent studies have defined useful significant dermoscopic features for Merkel cell carcinoma (MCC). The most common dermoscopic finding is the milky-red areas that are usually associated with linear irregular vessels. Jalilian et al. reported dermoscopic features of 12 MCC cases (66). All cases presented polymorphous, linear irregular vessels, and structureless areas. Milky-pink areas were observed in 11 cases. Furthermore, Harting et al. reported that milky-red areas or linear irregular vessels were most commonly observed in 10 MCC cases studies (67). Additionally, Dalle et al. observed milky-red areas in 80% of their patients. While these patterns may be observed in amelanotic melanoma, the lack of findings of pigmentation or blue-gray veils could direct diagnosis against MCC (68).
Dermoscopic features of extramammary Paget's disease (EMPD) have not yet been established due to its rarity. Recently, Mun et al. compared the dermoscopic appearance of 35 EMPD cases and EMPD-mimicking lesions, e.g., eczematous dermatitis (ED), fungal infections (FI), and Bowen's disease (BD). In EMDP, they observed milky-red areas (32/35), dotted vessels (18/35), glomerular vessels (7/35), polymorphous vessels (6/35), surface scales (7/35), linear irregular vessels (1/35), ulcers/erosions (15/35), pigmented structures (11/35), shiny white lines (4/35), and white structureless areas (3/35) (69). Milky red areas were significantly more prevalent in EMPD than in ED, FI, or BD. Moreover, invasive EMPD correlated statistically with polymorphous vessels.
Dermoscopic features of angiosarcoma (AS) have not yet been established due to its rarity. De Giorgi et al. described steam-like areas with a white or skin-colored central area as a characteristic dermoscopic feature of AS (70). Furthermore, Oiso et al. reported that a gradation of various colors within the lesion may be an important dermoscopic feature of AS since it is not present in common purpura or ecchymosis (71). Minagawa et al. reported that AS is characterized by the absence of well-defined vascular structures, e.g., lacunae/lagoons that are commonly found in other vascular lesions such as angioma and pyogenic granuloma. Those features might be useful toward differential diagnosis with amelanotic melanomas (72).
We summarized recent reports of novel findings related to dermoscopy of melanoma and non-melanoma skin cancers. Dermoscopy is presently thought to be effective and helpful for diagnosing melanoma and non-melanoma skin cancers. However, it is important to consider that dermoscopy is just one of several means, others being clinical history, age and gross appearance, that can be utilized in cancer diagnosis. Therefore, we should not hesitate to do a biopsy in cases in which a diagnosis cannot be reached clearly through dermoscopy.
JK and HU have full responsibility of this article. JK, KH, SS, TM, and HU confirmed the manuscript for submission.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Argenziano G, Soyer HP, Chimenti S, Talamin R, Corona R, Sera F, et al. Dermoscopy of pigmented skin lesions: results of a consensus meeting via the Internet. J Am Acad Dermatol. (2003) 48:679–93. doi: 10.1067/mjd.2003.281
2. Marghoob AA, Braun R. Proposal for a revised 2-step algorithm for the classification of lesions of the skin using dermoscopy. Arch Dermatol. (2010) 146:426–28. doi: 10.1001/archdermatol.2010.41
3. Menzies SW, Ingvar C, Crotty KA, McCarthy WH. Frequency and morphologic characteristics of invasive melanomas lacking specific surface microscopic features. Arch Dermatol. (1996) 132:1178–82. doi: 10.1001/archderm.1996.03890340038007
4. Schiffner R, Schiffner-Rohe J, Vogt T, Landthaler M, Wlotzke U, Cognetta AB, et al. Improvement of early recognition of lentigo maligna using dermatoscopy. J Am Acad Dermatol. (2000) 42:25–32. doi: 10.1016/S0190-9622(00)90005-7
5. Argenziano G, Longo C, Cameron A, Cavicchini S, Gourhant JY, Lallas, et al. Blue-black rule: a simple dermoscopic clue to recognize pigmented nodular melanoma. Br J Dermatol. (2011) 165:1251–5. doi: 10.1111/j.1365-2133.2011.10621.x
6. Pizzichetta MA, Kittler H, Stanganelli I, Bono R, Cavicchini S, De Giorgi V, et al. Pigmented nodular melanoma: the predictive value of dermoscopic features using multivariate analysis. Br J Dermatol. (2015) 173:106–14. doi: 10.1111/bjd.13861
7. Saida T, Miyazaki A, Oguchi S, Ishihara Y, Yamazaki Y, Murase S, et al. Significance of dermoscopic patterns in detecting malignant melanoma on acral volar skin: results of a multicenter study in Japan. Arch Dermatol. (2004) 140:1233–8. doi: 10.1001/archderm.140.10.1233
8. Phan A, Dalle S, Touzet S, Ronger-Savlé S, Balme B, Thomas L. Dermoscopic features of acral lentiginous melanoma in a large series of 110 cases in a white population. Br J Dermatol. (2010) 162:765–71. doi: 10.1111/j.1365-2133.2009.09594.x
9. Ozdemir F, Errico MA, Yaman B, Karaarslan I. Acral lentiginous melanoma in the Turkish population and a new dermoscopic clue for the diagnosis. Dermatol Pract Concept. (2018) 8:140–8. doi: 10.5826/dpc.0802a14
10. Lallas A, Kyrgidis A, Koga H, Moscarella E, Tschandl P, Apalla Z, et al. The BRAAFF checklist: a new dermoscopic algorithm for diagnosing acral melanoma. Br J Dermatol. (2015) 173:1041–9. doi: 10.1111/bjd.14045
11. Mikoshiba Y, Minagawa A, Koga H, Yokokawa Y, Uhara H, Okuyama R. Clinical and histopathologic characteristics of melanocytic lesions on the volar skin without typical dermoscopic patterns. JAMA Dermatol. (2019) 155:578–84. doi: 10.1001/jamadermatol.2018.5926
12. Koga H, Saida T, Uhara H. Key point in dermoscopic differentiation between early nail apparatus melanoma and benign longitudinal melanonychia. J Dermatol. (2011) 38:45–52. doi: 10.1111/j.1346-8138.2010.01175.x
13. Ohn J, Jo G, Cho Y, Sheu SL, Cho KH, Mun JH. Assessment of a predictive scoring model for dermoscopy of subungual melanoma in situ. JAMA Dermatol. (2018) 154:890–96. doi: 10.1001/jamadermatol.2018.1372
14. Benati E, Ribero S, Longo C, Piana S, Puig S, Carrera C, et al. Clinical and dermoscopic clues to differentiate pigmented nail bands: an International Dermoscopy Society study. J Eur Acad Dermatol Venereol. (2017) 31:732–6. doi: 10.1111/jdv.13991
15. Menzies SW, Kreusch J, Byth K, Pizzichetta MA, Marghoob A, Braun R, et al. Dermoscopic evaluation of amelanotic and hypomelanotic melanoma. Arch Dermatol. (2008) 144:1120–7. doi: 10.1001/archderm.144.9.1120
16. Lin MJ, Xie C, Pan Y, Jalilian C, Kelly JW. Dermoscopy improves diagnostic accuracy for clinically amelanotic nodules. Australas J Dermatol. (2019) 60:45–9. doi: 10.1111/ajd.12902
17. Menzies SW, Westerhoff K, Rabinovitz H, Kopf AW, McCarthy WH, Katz B. Surface microscopy of pigmented basal cell carcinoma. Arch Dermatol. (2000) 136:1012–6. doi: 10.1001/archderm.136.8.1012
18. Altamura D, Menzies SW, Argenziano G, Zalaudek I, Soyer HP, Sera F, et al. Dermatoscopy of basal cell carcinoma: morphologic variability of global and local features and accuracy of diagnosis. J Am Acad Dermatol. (2010) 62:67–75. doi: 10.1016/j.jaad.2009.05.035
19. Lallas A, Apalla Z, Argenziano G, Longo C, Moscarella E, Specchio F, et al. The dermatoscopic universe of basal cell carcinoma. Dermatol Pract Concept. (2014) 4:11–24. doi: 10.5826/dpc.0403a02
20. Micantonio T, Gulia A, Altobelli E, Di Cesare A, Fidanza R, Riitano A, et al. Vascular patterns in basal cell carcinoma. J Eur Acad Dermatol Venereol. (2011) 25:358–61. doi: 10.1111/j.1468-3083.2010.03734.x
21. Giacomel J, Zalaudek I. Dermoscopy of superficial basal cell carcinoma. Dermatol Surg. (2005) 31:1710–3. doi: 10.1097/00042728-200512000-00014
22. Marghoob AA, Cowell L, Kopf AW, Scope A. Observation of chrysalis structures with polarized dermoscopy. Arch Dermatol. (2009) 145:618. doi: 10.1001/archdermatol.2009.28
23. Ahnlide I, Zalaudek I, Nilsson F, Bjellerup M, Nielsen K. Preoperative prediction of histopathological outcome in basal cell carcinoma: flat surface and multiple small erosions predict superficial basal cell carcinoma in lighter skin types. Br J Dermatol. (2016) 175:751–61. doi: 10.1111/bjd.14499
24. Navarrete-Dechent C, Bajaj S, Marchetti MA, Rabinovitz H, Dusza SW, Marghoob AA. Association of shiny white blotches and strands with non-pigmented basal cell carcinoma: evaluation of an additional dermoscopic diagnostic criterion. JAMA Dermatol. (2016) 152:546–52. doi: 10.1001/jamadermatol.2015.5731
25. Emiroglu N, Cengiz FP, Kemeriz F. The relation between dermoscopy and histopathology of basal cell carcinoma. An Bras Dermatol. (2015) 90:351–6. doi: 10.1590/abd1806-4841.20153446
26. Pan Y, Chamberlain AJ, Bailey M, Chong AH, Haskett M, Kelly JW. Dermatoscopy aids in the diagnosis of the solitary red scaly patch or plaque-features distinguishing superficial basal cell carcinoma, intraepidermal carcinoma, and psoriasis. J Am Acad Dermatol. (2008) 59:268–74. doi: 10.1016/j.jaad.2008.05.013
27. Enache AO, Pătra?cu V, Simionescu CE, Ciurea RN, Văduva A, Stoica LE. Dermoscopy patterns and histopathological findings in nodular basal cell carcinoma-study on 68 cases. Curr Health Sci J. (2019) 45:116–22. doi: 10.12865/CHSJ.45.01.16
28. Nelson BR, Hamlet KR, Gillard M, Railan D, Johnson TM. Sebaceous carcinoma. J Am Acad Dermatol. (1995) 33:1–15. doi: 10.1016/0190-9622(95)90001-2
29. Buitrago W, Joseph AK. Sebaceous carcinoma: the great masquerader. Emerging concepts in diagnosis and treatment. Dermatol Ther. (2008) 21:459–66. doi: 10.1111/j.1529-8019.2008.00247.x
30. Coates D, Bowling J, Haskett M. Dermoscopic features of extraocular sebaceous carcinoma. Australas J Dermatol. (2011) 52:212–3. doi: 10.1111/j.1440-0960.2010.00699.x
31. Lallas A, Moscarella E, Argenziano G, Longo C, Apalla Z, Ferrara G, et al. Dermoscopy of uncommon skin tumours. Australas J Dermatol. (2014) 55:53–62. doi: 10.1111/ajd.12074
32. Manríquez J, Cataldo-Cerda K, Álvarez-Véliz S, Vera-Kellet C. Dermoscopy of sebaceous carcinoma: an unusual image. G Ital Dermatol Venereol. (2015) 150:626–8.
33. Iikawa M, Namiki T, Arima Y, Kato K, Arai M, Ueno M, et al. Extraocular sebaceous carcinoma in association with a clonal seborrheic keratosis: dermoscopic features. J Dermatol. (2015) 42:1105–6. doi: 10.1111/1346-8138.13043
34. Satomura H, Ogata D, Arai E, Tsuchida T. Dermoscopic features of ocular and extraocular sebaceous carcinomas. J Dermatol. (2017) 44:1313–6. doi: 10.1111/1346-8138.13905
35. Horimoto K, Kato J, Sumikawa Y, Hida T, Kamiya T, Sato S, et al. Dermoscopic features distinctive for extraocular sebaceous carcinoma. J Dermatol. (2018) 45:487–90. doi: 10.1111/1346-8138.14170
36. Nair PA, Patel T, Gandhi S. The usefulness of dermoscopy in extraocular sebaceous carcinoma. Indian J Dermatol. (2018) 63:440–2. doi: 10.4103/ijd.IJD_315_17
37. Rower-Huber J, Patel MJ, Forschner T, Ulrich C, Eberle J, Kerl H, et al. Actinic keratosis is an early in situ squamous cell carcinoma: a proposal for reclassification. Br J Dermatol. (2007) 156:8–12. doi: 10.1111/j.1365-2133.2007.07860.x
38. Zalaudek I, Giacomel J, Argenziano G, Hofmann-Wellenhof R, Micantonio T, Di Stefani A, et al. Dermoscopy of facial nonpigmented actinic keratosis. Br J Dermatol. (2006) 155:951–6. doi: 10.1111/j.1365-2133.2006.07426.x
39. Zalaudek I, Giacomel J, Schmid K, Bondino S, Rosendahl C, Cavicchini S, et al. Dermatoscopy of facial actinic keratosis, intraepidermal carcinoma, and invasive squamous cell carcinoma: a progression model. J Am Acad Dermatol. (2012) 66:589–97. doi: 10.1016/j.jaad.2011.02.011
40. Lallas A, Argenziano G, Zendri E, Moscarella E, Longo C, Grenzi L, et al. Update on non-melanoma skin cancer and the value of dermoscopy in its diagnosis and treatment monitoring. Expert Rev Anticancer Ther. (2013) 13:541–58. doi: 10.1586/era.13.38
41. Russo T, Piccolo V, Lallas A, Giacomel J, Moscarella E, Alfano R, et al. Dermoscopy of malignant skin tumours: what's new? Dermatology. (2017) 233:64–73. doi: 10.1159/000472253
42. Deinlein T, Richtig G, Schwab C, Scarfi F, Arzberger E, Wolf I, et al. The use of dermatoscopy in diagnosis and therapy of nonmelanocytic skin cancer. J Dtsch Dermatol Ges. (2016) 14:144–51. doi: 10.1111/ddg.12903
43. Jaimes N, Marghoob AA. Squamous cell carcinoma, actinic keratosis and keratoacanthoma. In: Jaimes N, Marghoob AA, editors. Pocket Guide to Dermoscopy. Coimbatore: Jaypee Brothers Medical Publishers (P) Ltd (2017). p. 37–40.
44. Casari A, Chester J, Pellacani G. Actinic keratosis and non-invasive diagnostic techniques: an update. Biomedicines. (2018) 6:e8. doi: 10.3390/biomedicines6010008
45. Zalaudek I, Argenziano G. Dermoscopy of actinic keratosis, intraepidermal carcinoma and squamous cell carcinoma. Curr Probl Dermatol. (2015) 46:70–6. doi: 10.1159/000366539
46. Zalaudek I, Argenziano G, Leinweber B, Citarella L, Hofmann-Wellenhof R, Malvehy J, et al. Dermoscopy of Bowen's disease. Br J Dermatol. (2004) 150:1112–6. doi: 10.1111/j.1365-2133.2004.05924.x
47. Bugatti L, Filosa G, De Angelis R. Dermoscopic observation of Bowen's disease. J Eur Acad Dermatol Venereol. (2004) 18:572–4. doi: 10.1111/j.1468-3083.2004.01008.x
48. Mun JH, Kim SH, Jung DS, Ko HC, Kwon KS, Kim MB. Dermoscopic features of Bowen's disease in Asians. J Eur Acad Dermatol Venereol. (2010) 24:805–10. doi: 10.1111/j.1468-3083.2009.03529.x
49. Yang Y, Lin J, Fang S, Han S, Song Z. What's new in dermoscopy of Bowen's disease: two new dermoscopic signs and its differential diagnosis. Int J Dermatol. (2017) 56:1022–5. doi: 10.1111/ijd.13734
50. Payapvipapong K, Tanaka M. Dermoscopic classification of Bowen's disease. Australas J Dermatol. (2015) 56:32–5. doi: 10.1111/ajd.12200
51. Cameron A, Rosendahl C, Tschandl P, Riedl E, Kittler H. Dermatoscopy of pigmented Bowen's disease. J Am Acad Dermatol. (2010) 62:597–604. doi: 10.1016/j.jaad.2009.06.008
52. Chung E, Marchetti MA, Pulitzer MP, Marghoob AA. Streaks in pigmented squamous cell carcinoma in situ. J Am Acad Dermatol. (2015) 72:S64–5. doi: 10.1016/j.jaad.2014.08.044
53. Nakayama C, Hata H, Homma E, Fujita Y, Shimizu H. Dermoscopy of periungual pigmented Bowen's disease: its usefulness in differentiation from malignant melanoma. J Eur Acad Dermatol Venereol. (2016) 30:552–4. doi: 10.1111/jdv.12957
54. Cavicchini S, Tourlaki A, Ghislanzoni M, Alberizzi P, Alessi E. Pigmented Bowen disease of the palm: an atypical case diagnosed by dermoscopy. J Am Acad Dermatol. (2010) 62:356–7. doi: 10.1016/j.jaad.2009.01.035
55. Saito T, Uchi H, Moroi Y, Kiryu H, Furue M. Subungual Bowen disease revealed by longitudinal melanonychia. J Am Acad Dermatol. (2012) 67:e240–1. doi: 10.1016/j.jaad.2012.03.031
56. Park SW, Lee DY, Mun GH. Longitudinal melanonychia on the lateral side of the nail: a sign of Bowen disease associated with human papillomavirus. Ann Dermatol. (2013) 25:378–9. doi: 10.5021/ad.2013.25.3.378
57. Matsuya T, Nakamura Y, Teramoto Y, Shimizu A, Asami Y, Arai E, et al. Image gallery: Bowen's disease of a nail unit presenting with 'woodgrain appearance' - a new dermoscopic finding. Br J Dermatol. (2018) 178:e66. doi: 10.1111/bjd.16070
58. Baran R, Simon C. Longitudinal melanonychia: a symptom of Bowen's disease. J Am Acad Dermatol. (1988) 18:1359–60. doi: 10.1016/S0190-9622(88)80115-4
59. Saxena A, Kasper DA, Campanelli CD, Lee JB, Humphreys TR, Webster GF. Pigmented Bowen's disease clinically mimicking melanoma of the nail. Dermatol Surg. (2006) 32:1522–5. doi: 10.1111/j.1524-4725.2006.32367.x
60. Rosendahl C, Cameron A, Argenziano G, Zalaudek I, Tschandl P, Kittler H. Dermoscopy of squamous cell carcinoma and keratoacanthoma. Arch Dermatol. (2012) 148:1386–92. doi: 10.1001/archdermatol.2012.2974
61. Pyne J, Sapkota D, Wong JC. Squamous cell carcinoma: variation in dermatoscopic vascular features between well and non-well differentiated tumors. Dermatol Pract Concept. (2012) 2:204a5. doi: 10.5826/dpc.0204a05
62. Yélamos O, Braun RP, Liopyris K, Wolner ZJ, Kerl K, Gerami P, et al. Dermoscopy and dermatopathology correlates of cutaneous neoplasms. J Am Acad Dermatol. (2019) 80:341–63. doi: 10.1016/j.jaad.2018.07.073
63. Manfredini M, Longo C, Ferrari B, Piana S, Benati E, Casari A, et al. Dermoscopic and reflectance confocal microscopy features of cutaneous squamous cell carcinoma. J Eur Acad Dermatol Venereol. (2017) 31:1828–33. doi: 10.1111/jdv.14463
64. Lallas A, Pyne J, Kyrgidis A, Andreani S, Argenziano G, Cavaller A, et al. The clinical and dermoscopic features of invasive cutaneous squamous cell carcinoma depend on the histopathological grade of differentiation. Br J Dermatol. (2015) 172:1308–15. doi: 10.1111/bjd.13510
65. Benati E, Persechino F, Piana S, Argenziano G, Lallas A, Moscarella E, et al. Dermoscopic features of squamous cell carcinoma on the lips. Br J Dermatol. (2017) 177:e41–e43. doi: 10.1111/bjd.15274
66. Jalilian C, Chamberlain AJ, Haskett M, Rosendahl C, Goh M, Beck H, et al. Clinical and dermoscopic characteristics of Merkel cell carcinoma. Br J Dermatol. (2013) 169:294–7. doi: 10.1111/bjd.12376
67. Harting MS, Ludgate MW, Fullen DR, Johnson TM, Bichakjian CK. Dermatoscopic vascular patterns in cutaneous Merkel cell carcinoma. J Am Acad Dermatol. (2012) 66:923–7. doi: 10.1016/j.jaad.2011.06.020
68. Dalle S, Parmentier L, Moscarella E, Phan A, Argenziano G, Thomas L. Dermoscopy of Merkel cell carcinoma. Dermatology. (2012) 224:140–4. doi: 10.1159/000337411
69. Mun JH, Park SM, Kim GW, Song M, Kim HS, Ko HC, et al. Clinical and dermoscopic characteristics of extramammary Paget's disease: a study of 35 cases. Br J Dermatol. (2016) 174:1104–7. doi: 10.1111/bjd.14300
70. De Giorgi V, Grazzini M, Rossari S, Gori A, Verdelli A, Cervadoro E, et al. Dermoscopy pattern of cutaneous angiosarcoma. Eur J Dermatol. (2011) 21:113–4. doi: 10.1684/ejd.2010.1173
71. Oiso N, Matsuda H, Kawada A. Various color gradations as a dermatoscopic feature of cutaneous angiosarcoma of the scalp. Australas J Dermatol. (2013) 54:36–8. doi: 10.1111/j.1440-0960.2012.00885.x
Keywords: dermoscopy, melanoma, basal cell carcinoma, sebaceous carcinoma, actinic keratosis, Bowen's disease, squamous cell carcinoma, Merkel cell carcinoma
Citation: Kato J, Horimoto K, Sato S, Minowa T and Uhara H (2019) Dermoscopy of Melanoma and Non-melanoma Skin Cancers. Front. Med. 6:180. doi: 10.3389/fmed.2019.00180
Received: 27 June 2019; Accepted: 29 July 2019;
Published: 21 August 2019.
Edited by:
Taku Fujimura, Tohoku University, JapanCopyright © 2019 Kato, Horimoto, Sato, Minowa and Uhara. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hisashi Uhara, dWhhcmFoQHNhcG1lZC5hYy5qcA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.