
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 09 January 2018
Sec. Geriatric Medicine
Volume 4 - 2017 | https://doi.org/10.3389/fmed.2017.00244
This article is part of the Research Topic Active Aging and Disease Management View all 15 articles
Over the last decades, the world elderly population has increased exponentially and this tendency will continue during the coming years; from 2000 to 2050, people over 60 will double and those over 80 will quadruple. Loss of independence occurs as people age due to mobility restrictions, frailty, and decreased functional fitness and cognitive abilities. Evidence has shown that appropriate programs and policies contribute to keep older adults healthy and independent over time. The purpose of this chapter is to report the results of our 3-year follow-up study designed to characterize functional physical fitness in a sample of Portuguese community-dwelling older adults to propose a set of functional parameters that decline the most. We studied a group of 43 elderly people, aged 60 and over. Variables assessed on the participants were anthropometric measurements, functional capacity with the Senior Fitness Test battery (muscle strength, aerobic endurance, flexibility, agility, and dynamic balance), handgrip strength, levels of physical activity, and balance. Three years after the first assessment, a second assessment of the same variables was conducted. We analyzed what were the variables that, for this group, were related with a healthier aging and the relation with different physical activity levels. Our study showed that the distance covered in 6-min walk test and handgrip strength seem to explain a great amount of variability on functional variables that have changed on this period (68% of balance, lower and upper functional strength, respectively) and the active participants showed less decrements with aging in anthropometric and functional variables than those inactive or insufficiently active (p < 0.05). Greater importance should be given to prescription of exercise targeting older adults and, specifically, walking and manual activities should be given more attention as components of a community exercise program.
Aging is a gradual, life-long process and highly variable characterized by a progressive and cumulative generalized impairment of physiological functions (1), which may be explained at least by genetic factors, multiple morbidities, and non-genetic factors (specially nutrition, lifestyle, and physical activity) (1).
Nowadays, the increase in human life expectancy and the reduction in death rates has made the number of older adults to grow. Portugal is not an exception and, the rate of older people has risen until 148.7% in 2016 (2), which makes authorities and health care professionals be concerned with the retirement impact on levels of functional limitations (3).
According to Chen and colleagues, it is important to study disability as a process over time since it is very informative on the disability process of an aging population (4). So, a comprehensive follow-up of functional impairment rates and its relationship with disability over time may be the basic strategy to find out which factors contribute to a greater or lesser risk of disability and, thus, to promote strategies to a healthier aging process.
Body composition and cardiorespiratory fitness are the most studied health-related variables of physical fitness and function. Changes in body composition with a loss of muscle mass, bone mass, water content along with musculoskeletal and neuromotor function may predispose older adults to a functional decline with risk of disability increasingly high (5). In addition, changes in cardiorespiratory function with a decrement resulting as much as 50% by the age of 70 contribute also to a higher risk of disability (6). These previous findings have been partially confirmed in longitudinal studies focused on aging and disability, where independent associations of aging were found between lower mobility and mortality (7), and survival (8), dynapenia and abdominal obesity with disability worsening (9), cardiorespiratory fitness and muscle function (10), or cognitive/mental state or/and comorbidities and chronic diseases (11–13).
Although older adults are generally less active, physical activity and exercise training have beneficial effects on neuromuscular adaptations (muscle and myofiber hypertrophy with gains in strength and power (14)) in healthy older adults, depending on clinical status and the training modality exercise training, specially endurance training improves different aspects of muscle oxygenation (15). In fact endurance and resistance training programs have proved to be effective to the positive increment in aerobic capacity and thus also in functional capacity of participants as so in cognitive function and in the reduction of the risk for chronic diseases (16, 17). However, a great variability exists in functional responses to exercise and in levels of adherence and preferences (18). Particularly, changes in body composition with a loss of muscle mass, bone mass, and water content along with musculoskeletal and neuromotor function predisposed older adults to a functional decline with risk of disability increasingly high (5).
Despite this increment in research, it remains the need to identify the best predictors for functional capacity and what is the contribution of physical activity to maintain this capacity with aging.
It was our purpose to characterize longitudinally functional physical fitness in a sample of Portuguese community-dwelling older adults and find plausible associations between functional, and anthropometric variables, and differences across physical activity levels and cardiometabolic comorbidities in this population over a 3-year period.
Participants were recruited for this longitudinal study in day care centers and senior universities and were eligible if they were older than 60 years and independent in activities of daily living (ADL). Participants were excluded if they were unable to ambulate without assistance. Body composition, functional fitness, and physical activity assessments were carried out in all participations who met the inclusion criteria at beginning of the study (M1) and 3 years later (M2).
After an explanation of the study and after a signed informed consent, in accordance with the Declaration of Helsinki, participants performed a battery of tests to assess functional physical fitness. All study procedures were approved by the institutional review boards of the participating institutions.
Weight and height were measured using a digital balance with a stadiometer (SECA®). Body mass index (BMI) was calculated (BMI = kg/m2). An anthropometric tape was used for measuring waist (WC) and hip circumferences (HP) as markers of regional adiposity. Waist circumference was measured at the smallest circumference above the umbilicus and below the xiphoidal process (19) and hip circumference was measured at the highest circumference of the buttocks in a level horizontal plane. Ratio waist–hip was found by dividing the waist circumference (cm) by hip circumference (cm) (20, 21).
Body Composition was assessed using anthropometric measurements (height, weight, waist, and hip circumference) and BMI and waist to hip ratio (WHR) were calculated.
Whole-body skeletal muscle mass (SMM) was estimated using the following Al-Gindan et al. (22) equations:
and
where WC, waist circumference, HC, Hip circumference.
The Senior Fitness Test battery was used to assess functional capacity. This battery consists of six items to assess lower limbs strength and flexibility, upper body strength and flexibility, agility and dynamic balance, and aerobic endurance. All the tests were performed according to guidelines and protocols for administration (6). Briefly, lower limbs strength was measured with the 30 s chair stand test. An arm curl test was utilized for upper body strength assessment, which consists of carrying out as many forearm curls as possible within 30 s with 2.27 kg (5 lb) and 3.63 kg (8 lb) dumbbells for women and men, respectively. The chair sit-and-reach and the back scratch tests were used to assess lower and upper body flexibility, respectively. The 8-foot up and go tests were used to assess mobility. To measure aerobic endurance we used the 6-min walk test (6MWT) (23), and estimated distance walked was calculated with a validated equation (24).
where F = 0; M = 1; r2 = 0.66.
Isometric strength was assessed with a handgrip test using the American Society of Hand Therapists (ASHT) protocol. It was measured at both hands (in kg; JAMAR® dynamometer). ASHT recommends a sitting position with shoulder adducted, elbow flexed at 90° for arm and wrist in neutral position and wrist between 0° to 30° of dorsal flexion (25).
Balance was assessed with the Berg Balance Scale (BBS) (26) because it is easy to use, it takes ~15–20 min to complete and is appropriate for clinical and community settings. It consists on 14 items that the subject must complete safely. Each item is scored from 0 (unable to complete the task) to 4 (independent and safe performance). Maximum score is 56 points (26).
In addition, participants completed and ad hoc questionnaire about comorbidities or non-communicable diseases and musculoskeletal pain conditions.
Levels of physical activity (LPA) were assessed and subjects were classified in sedentary/inactive, insufficiently active or active according the classification of physical behavior (19). An active participant was considered who perform 30 min of moderate activity at least 5 days a week and/or 20 min of vigorous activity 3 days per week or a combination of both.
For all statistical analysis, the IBM SPSS 21.0 package for Macintosh was used (SPSS Inc., IBM Company, Chicago, IL, USA). The confidence level was established with a statistically significant p-value of less than 0.05. All variables were inspected and confirmed for a non-normal distribution prior to analysis (Kolmogorov–Smirnov normality test). Basic characteristics of the participants were obtained by analyzing frequencies (%), or calculating mean and SD (mean ± SD).
Differences of performance, body composition, and functional fitness between M1 and M2 were analyzed by Wilcoxon signed-rank test. In addition, differences by sex were carried out using a Mann–Whitney U test.
The association between comorbidities and functional variables at M1 and M2 were analyzed with Wilcoxon Signed Rank test or a Mann–Whitney U test, for comorbidities with significant impact on functional variables.
Linear regression models were performed for the clinical variables that had significant differences between two measures (differences in clinical variables were dependent variables and physical fitness and body composition as independent). Finally, a Kruskal–Wallis analysis was conducted to find differences in functional variables between physical inactive, insufficiently active and active.
Baseline (M1) and 3 years later (M2) characteristics of participants aged between 60 and 91 years, all Caucasian, are described in Table 1.
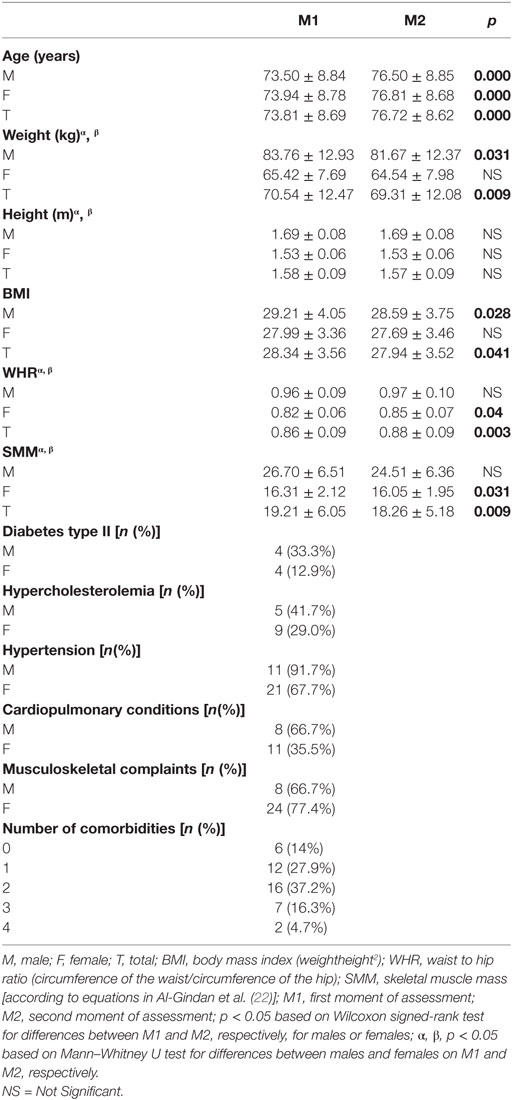
Table 1. Variables of characterization of participants (12 males; 31 females; total n = 43) (mean ± SD) or n (%) for characterization of comorbidities.
Fourteen percent had a normal BMI at M1 but this percentage was increased to 21% at M2. There were not underweight cases and the prevalence of obesity was 23.3% (BMI > 30.0).
Only six participants reported none disease or musculoskeletal issue. Eighty six percent reported one to four comorbidities and 58.1% present multibordity (2 or more chronic conditions): type II diabetes was present in 18.6% of all the participants, hypercholesterolemia in 32.6%, and hypertension in 74.4%. Musculoskeletal complaints were present in 74.4% of participants. Overall, 33.3% participants suffered one or more falls in the previous year (at M1). Almost all the anthropometrical and body composition characteristics changed over the 3-year follow-up period (Table 1). Males reduced their weight and BMI while females decreased SMM and had small although significant increment in WHR (Table 1).
Most our participants were sedentary or inactive (37.2%) or insufficiently active (39.5%) and only 23.3% were active at M1. These latter results were similar at M2: 39.5% were sedentary, 30.2% insufficiently active, and 30.2% were active.
Regarding physical fitness capacity, there were only a few components with significant alteration over time (Table 2). Males reduced flexibility with a small increase in upper limb strength (arm curl). Among females, we could observe a decrease in balance and muscle strength. No changes in functional aerobic capacity variables were verified in both sexes (Table 2). Although 58.3% of males and 48.4% of females presented values for the handgrip that were classified as poor (19) at M1, only 8.3% of males and 12.9% of females presented values on handgrip strength that could be classified as having sarcopenia at M2.
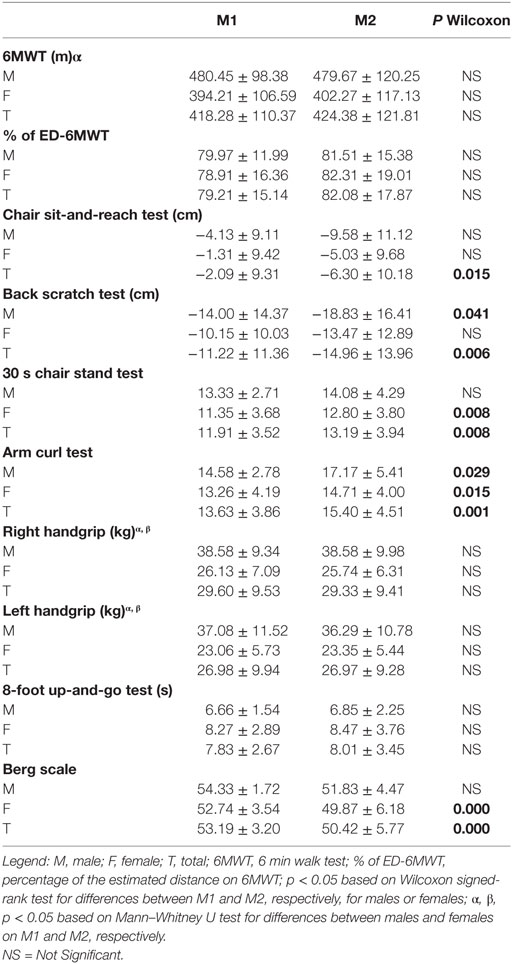
Table 2. Values for functional fitness variables by gender (12 males; 31 females; total n = 43) (mean ± SD).
Balance assessed by BBS was significantly reduced only in women. Nevertheless, a change of 6 points in BBS score indicated with 95% of confidence that a genuine change in function has occurred (27) and this occurred for 18.6% of our sample (three males and five females).
Women reduced lower limbs (30 s chair stand test) strength at M2 but not mobility, although they took longer to complete the test, the decrement in mobility was not significant (8-foot-up-and-go test). BBS results informed that our participants have an increased risk of 43% of falling, 16% risk for suffering multiple falls, and 24% risk for suffering an injurious fall.
Table 3 shows the differences on functional variables between diabetic and non-diabetic groups, and participants with or without hypercholesterolemia at M1 and M2 (only for those variables with significant differences at least in one time point). In summary, only type II diabetes and cholesterolemia conditions seemed to influence the performance in endurance capacity, Berg scale and flexibility (type diabetes), and strength (hypercholesterolemia). Longitudinal changes in endurance capacity (6MWT) were reduced in diabetic participants but not in non-diabetic ones (Table 3).
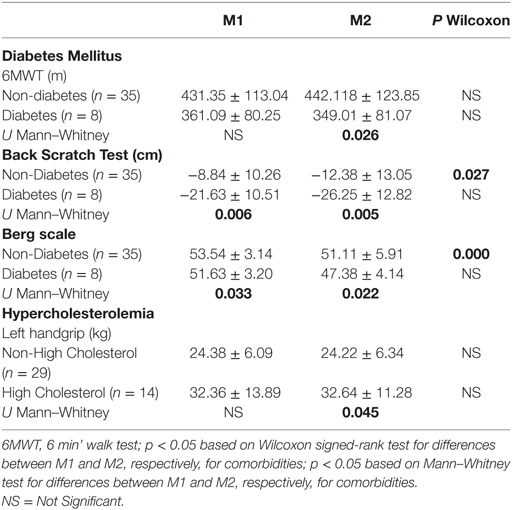
Table 3. Values for functional fitness variables related with comorbidities (12 males; 31 females; Total n = 43) (mean ± SD).
Anthropometrical and functional variables were statistically different across LPA and a better profile in functional capacity and anthropometry was showed for active when compared with inactive participants (Table 4). Distribution of comorbidities was similar among the physical activity level groups.
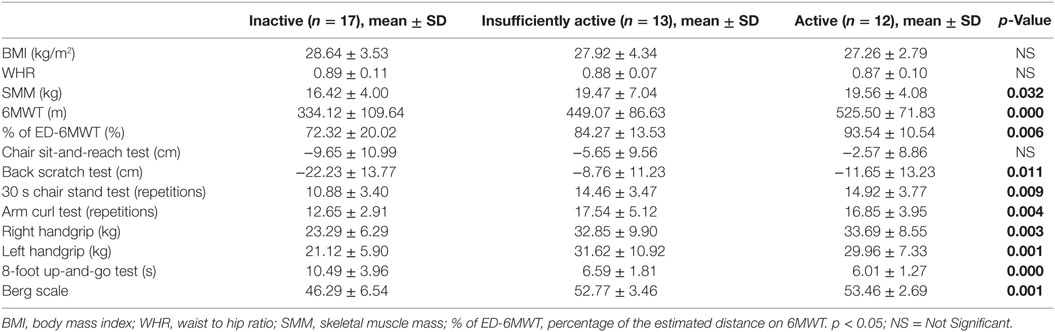
Table 4. Kruskal–Wallis analysis for differences in anthropometrical and functional variables between physical inactive, insufficiently active and active participants.
Finally, the linear regression models showed the best predictors of functional tests.
The first linear regression model to the dependent variable “Berg Balance Scale” was associated with 6MWT and “Right Handgrip” adjusted to weight was significant (F = 27.076; p = 0.000; R2 = 0.681, and SEE = 3.400). The contribution of each predictor to the model was significant with a standardized Beta coefficient of 0.635 (p = 0.000) and 0.313 (p = 0.039), respectively. The whole model explained 68% of the variance.
The second linear regression model to the dependent variable “30 s chair stand test” was associated with 6MWT adjusted to weight (F = 26.192; p = 0.000; R2 = 0.567, and SEE = 2.658). The contribution of the predictor to the model had standardized Beta coefficient of 0.779 (p = 0.000) with 57% of the variance explained by the model.
“Arm curl test” was correlated with 6MWT and “Left Handgrip” adjusted to weight (F = 12.190; p = 0.000; R2 = 0.484 and SEE = 3.362). The contribution of each predictor to the model was significant with a standardized Beta coefficient of 0.406 (p = 0.009) and 0.416 (p = 0.024), respectively (the model explained 48% of the variance).
Lower flexibility (“Chair Sit-and-Reach Test”) was associated with upper flexibility (“Back Scratch Test”) (F = 9.111; p = 0.001; R2 = 0.313, and SEE = 8.646). The contribution of the predictor to the model was significant with a standardized Beta coefficient of 0.529 (p = 0.000) and the model explained 31% of the variance. Regarding, upper flexibility (“Back Scratch Test”) was correlated with BBS (F = 6.894; p = 0.003; R2 = 0.256, and SEE = 12.34) The contribution of the predictor to the model was significant with a standardized Beta coefficient of 0.500 (p = 0.001) and the model explained 26% of the variance.
Summarizing, physical function predictors, 6MWT and handgrip strength were the best predictors.
Finally, we could not find associations between changes in functional capacity tests and Berg scale or improvement in comorbidities.
To better understand the complex nature of physical function decline among older adults, we pursued two directions. First, we evaluated and identified the progression of physical function decline over a 3-year follow-up in a sample of people older than 60 years. Our results showed differences between gender in the anthropometric and functional variables after follow-up period, and these differences could be associated with changes in body composition across the aging process which is not a new finding. The level of functional fitness decreased with age, and the decrease was more important in females. On the other hand, this prospective longitudinal study showed the association between functional variables related to the balance, risk of falls, strength, physical fitness tests, and comorbidities. Our data bring knowledge to understand the variables that suffer the worst decrease with aging and may contribute to create more efficient strategies focused in these functional variables. In this scenario, the most important finding in this study is the relevance of 6MWT as predictor of other functional capacities and the influence of type II diabetes in 6MTW performance and age-related impairment.
The specific sexual phenotype of change for body weight was not new (BMI was reduced for male participants, but not for females); this adaptation followed the sarcopenic obesity paradigm since women did not lose weight in 3 years, but they increased waist and hip circumference (regional adiposity markers), and decreased whole-body skeletal muscle mass (SMM), which may increase the risk of hip fractures in the presence of a loss of balance. Previous studies (28, 29) concluded that greater abdominal obesity measured by WHR increased the risk of hip fracture considerably. The mechanism for an increased fracture risk with increasing WHR after adjusting for BMI might be mechanical instability and impaired balance induced by an increased body size in the abdominal region, leading to a fall (30). It has been suggested that carrying excess weight on the torso rather than on the hips increases the risk of falls that result in hip fracture, perhaps due to a higher center of gravity (28). This paradigm that explains a relationship between the increasing in the WHR and increment in the risk of falls was partially confirmed with our results of differences in the BBS variables, which suffered biggest significant changes (see Table 2). Other previous studies have investigated the relationship between obese and the risk of falls and fear of falls in older women (31–33). In general, results from our study are aligned with previous studies (34–37) and also with the study of Bird et al. (38) were balance decreased without loss of strength.
The influence of physical activity in functional capacity was confirmed in our group of age with a dose–response effect, so LPA were positively associated with performance in functional tests showing better results for those who are more active. Although only 30% of the participants accomplish physical activity guidelines (physical activity at least three times a week) the deleterious effect of PA on physical function impairment may not be related with a fixed quantity of PA, which may indicate that even low amounts of PA must promote significant benefits for physical function.
Our data highlighted that balance seems to be greatly explained by aerobic functional capacity (6MWT) and strength (handgrip). These results are in accordance with a previous study, which has shown that higher lower-limb function, balance, and mobility are associated with better walking ability and distance covered in the 6MWT by healthy older adults (39). Our study revealed that 6MWT and ha handgrip strength are also related with the BBS. Handgrip strength has been used as an outcome to measure muscle strength because it has been identified as strongly related with lower extremity muscle power, knee extension torque, and calf cross-sectional muscle area (40, 41) and could predict functional decline (42, 43). These findings reveal not only major relevance of cardiorespiratory fitness but also strength for preserving a good functional capacity. The main result from functional capacity were those related with comorbidities, although functional capacity were barely affected by group of comorbidities, so type II diabetes seemed to affect functional capacity (lower distance on 6MWT, lower flexibility, and lower balance than participants without diabetes type II). Furthermore participants with diabetes present a higher decrement on distance walked on 6MWT, which can potentiate the functional decline and risk of disability associated with aging. This topic should be object of more studies since this association may be a determinant of a frailty phenotype (44–46). In addition, we noticed that 39.5% at M1 and 35.7% of participants at M2 walked less than 400 m on 6MWT, which is a cut-off point to classify sarcopenia with limited mobility; on average, diabetic participants walked way below of this cut-off latter, representing their high susceptibility to be classified as sarcopenic obese and higher risk of frailty (47, 48). Regarding handgrip data, values split by hypercholesterolemia group were paradoxical since hypercholesterolemia group had higher values of strength, nevertheless the proportion of males and body weight values in the group of hypercholesterolemia were higher than in the group without hypercholesterolemia (35.7 vs 24.9%)., which may explain our results. Although the fact of having or not having multimorbidity [the presence of 2 or more chronic conditions (49)] may put older people in higher risk of frailty our results did not confirm this hypothesis.
Physical decline, including muscle weakness, balance dysfunction and mobility problems are related to functional decline, contributing to limit functional capacity while performing ADL and increasing the risk of falling (50, 51). Individualized intervention programs should address fall risks previously identified and they should include balance training, aerobic endurance, muscle strengthening, and flexibility (50).
Improvements in balance may rely in specific balance training programs (38) but also in other strategies. Our results may suggest that exercise prescription for older people should include also aerobic endurance and muscle training (50) as guidelines state, with recommendations to walk at least 30 min a day (52). Physical activity such as walking in different environments should be prescribed as an activity of daily living with benefits on physical capacity especially in balance and specially to those that do not meet the recommended 150 min per week of physical activity of moderate intensity and have or are at risk for chronic diseases (53), with special attention to groups of participants with comorbidities such as diabetes.
This was a longitudinal study that analyzed whether aging-related changes could be related with a lower decrement in functional variables such as muscle strength, flexibility, or mobility. However, the time interval was too short to found undeniable or high predictive value in variables of disability.
Although our study has a well-defined target population (day care centers and senior universities), participants were volunteers, and this could be a small bias which could be overcome by a larger sample. In addition, the small size of the sample is also a limitation that prevents a more accurate analysis of the results.
A higher time interval and a larger sample should be considered in future studies.
Results of this 3-year follow-up study confirmed the relevance of endurance and strength capacities, which may be improved across physical activity levels in combination with other body composition and physical function variables. The main relevance was the influence of type II diabetes 6MWT impairment in the second time point, which may confirm the deleterious consequences of the disease on cardiovascular capacity and sarcopenia; in addition, these results must provide construct validity of 6MWT. Finally, our results suggested that the loss of functional capacity must be more related with qualitative variables than morphological (for example, SMM) since we could not find any relationship between changes in body composition and physical function variables.
When prescribing exercise or programs for promoting health targeting this population greater attention should be given in walking activities and activities that use hands since these specific components seems to have a major impact in functional physical condition.
After an explanation of the study, participants signed an informed consent. All procedures were in accordance with the Declaration of Helsinki. All study procedures were approved by the institutional review boards of the participating institutions.
MTT, AG-M, EC, and BF have equally contributed to this manuscript, in designing the study. Data were collected by MTT, AG-M, and BF and were analyzed by all authors. Data interpretation and manuscript preparation were undertaken by MTT, AG-M, EC, and BF. All authors approved the final version of the paper.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors wish to thank to Loures Municipality all the logistical support for the assessment of participants on two the moments.
This work was developed upon European Innovation Partnership for Active and Healthy Ageing (EIP-AHA) commitment without any financial support. A specific grant for supporting the publishing of knowledge was obtained from the institution of Portuguese authors (IPL/2016/SFQ2017_ESTeSL).
1. Kirkwood TBL. Why and how are we living longer? Exp Physiol (2017) 102(9):1067–74. doi:10.1113/EP086205
2. PORDATA. Retrato de Portugal, PORDATA. 1a edição. Lisboa: Fundação Francisco Manuel dos Santos (2017).
3. van Zon SKR, Bültmann U, Reijneveld SA, de Leon CFM. Functional health decline before and after retirement: a longitudinal analysis of the health and retirement study. Soc Sci Med (2016) 170:26–34. doi:10.1016/j.socscimed.2016.10.002
4. Chen CM, Su YY, Mullan J, Huang MS, Chiu HC. Trajectories of disability and their relationship with health status and social service use. Exp Aging Res (2015) 41(3):240–58. doi:10.1080/0361073X.2015.1021641
5. Magyari P, Lite R, Kilpatrick MW, Schoffstall JE. ACSM’s Resources for the Exercise Physiologist – A Practical Guide for the Health Fitness Professional. 2nd ed. American College of Sports Medicine, editor. Philadelphia: Wolters Kluwer Health (2018).
6. Rikli R, Jones CJ. Senior Fitness Test Manual. 2nd ed. Rikli R, Jones CJ, editors. Champaign, IL: Human Kinetics (2013).
7. Bergland A, Jørgensen L, Emaus N, Strand BH. Mobility as a predictor of all-cause mortality in older men and women: 11.8 year follow-up in the Tromsø study. BMC Health Serv Res (2017) 17(1):22. doi:10.1186/s12913-016-1950-0
8. Franzon K, Byberg L, Sjögren P, Zethelius B, Cederholm T, Kilander L. Predictors of independent aging and survival: a 16-year follow-up report in octogenarian men. J Am Geriatr Soc (2017) 65(9):1953–60. doi:10.1111/jgs.14971
9. Rossi AP, Fantin F, Caliari C, Zoico E, Mazzali G, Zanardo M, et al. Dynapenic abdominal obesity as predictor of mortality and disability worsening in older adults: a 10-year prospective study. Clin Nutr (2016) 35(1):199–204. doi:10.1016/j.clnu.2015.02.005
10. Distefano G, Goodpaster BH. Effects of exercise and aging on skeletal muscle. Cold Spring Harb Perspect Med (2017):a029785. doi:10.1101/cshperspect.a029785
11. Nagarkar A, Kashikar Y. Predictors of functional disability with focus on activities of daily living: a community based follow-up study in older adults in India. Arch Gerontol Geriatr (2017) 69:151–5. doi:10.1016/j.archger.2016.11.015
12. Veronese N, Stubbs B, Trevisan C, Bolzetta F, De Rui M, Solmi M, et al. What physical performance measures predict incident cognitive decline among intact older adults? A 4.4 year follow up study. Exp Gerontol (2016) 81:110–8. doi:10.1016/j.exger.2016.05.008
13. Onoda K, Ishihara M, Yamaguchi S. Decreased functional connectivity by aging is associated with cognitive decline. J Cogn Neurosci (2012) 24(11):2186–98. doi:10.1162/jocn_a_00269
14. Cartee GD, Hepple RT, Bamman MM, Zierath JR. Exercise promotes healthy aging of skeletal muscle. Cell Metab (2016) 23(6):1034–47. doi:10.1016/j.cmet.2016.05.007
15. Fiogbé E, de Vassimon-Barroso V, de Medeiros Takahashi AC. Exercise training in older adults, what effects on muscle oxygenation? A systematic review. Arch Gerontol Geriatr (2017) 71:89–98. doi:10.1016/j.archger.2017.03.001
16. Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, et al. Exercise and physical activity for older adults. Med Sci Sports Exerc (2009) 41(7):1510–30. doi:10.1249/MSS.0b013e3181a0c95c
17. de Asteasu MLS, Martínez-Velilla N, Zambom-Ferraresi F, Casas-Herrero Á, Izquierdo M. Role of physical exercise on cognitive function in healthy older adults: a systematic review of randomized clinical trials. Ageing Res Rev (2017) 37:117–34. doi:10.1016/j.arr.2017.05.007
18. Chmelo EA, Crotts CI, Newman JC, Brinkley TE, Lyles MF, Leng X, et al. Heterogeneity of physical function responses to exercise training in older adults. J Am Geriatr Soc (2015) 63(3):462–9. doi:10.1111/jgs.13322
19. American College of Sports Medicine. ACSM’s Health-Related Physical Fitness Assessment Manual. 3rd ed. In: Kaminsky L, editor. Baltimore: Wolters Kluwer, Lippincott Williams & Wilkins (2010).
20. Heyward V. Advanced Fitness Assessment & Exercise Prescription. 3rd ed. Champaign: Human Kinetics (1997).
22. Al-Gindan YY, Hankey C, Govan L, Gallagher D, Heymsfield SB, Lean ME. Derivation and validation of simple equations to predict total muscle mass from simple anthropometric and demographic data. Am J Clin Nutr (2014) 100(4):1041–51. doi:10.3945/ajcn.113.070466
23. ATS. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med (2002) 166:111–7. doi:10.1164/ajrccm.166.1.at1102
24. Troosters T, Gosselink R, Decramer M. Six minute walking distance in healthy elderly subjects. Eur Respir J (1999) 14(2):270–4. doi:10.1034/j.1399-3003.1999.14b06.x
25. Rantanen T, Guralnik JM, Foley D, Masaki K, Leveille S, Curb JD, et al. Midlife hand grip strength as a predictor of old age disability. JAMA (1999) 281(6):558–60. doi:10.1001/jama.281.6.558
26. Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health (1992) 83(Suppl 2):S7–11.
27. Donoghue D; Physiotherapy Research and Older People (PROP) Group, Stokes EK. How much change is true change? The minimum detectable change of the Berg Balance Scale in elderly people. J Rehabil Med (2009) 41(5):343–6. doi:10.2340/16501977-0337
28. Parker ED, Pereira MA, Virnig B, Folsom AR. The association of hip circumference with incident hip fracture in a cohort of postmenopausal women: the Iowa Women’s Health Study. Ann Epidemiol (2008) 18(11):836–41. doi:10.1016/j.annepidem.2008.07.007
29. Søgaard AJ, Holvik K, Omsland TK, Tell GS, Dahl C, Schei B, et al. Abdominal obesity increases the risk of hip fracture. A population-based study of 43,000 women and men aged 60-79 years followed for 8 years. Cohort of Norway. J Intern Med (2015) 277(3):306–17. doi:10.1111/joim.12230
30. Corbeil P, Simoneau M, Rancourt D, Tremblay A, Teasdale N. Increased risk for falling associated with obesity: mathematical modeling of postural control. IEEE Trans Neural Syst Rehabil Eng (2001) 9(2):126–36. doi:10.1109/7333.928572
31. Rossi-Izquierdo M, Santos-Pérez S, Faraldo-García A, Vaamonde-Sánchez-Andrade I, Gayoso-Diz P, Del-Río-Valeiras M, et al. Impact of obesity in elderly patients with postural instability. Aging Clin Exp Res (2016) 28(3):423–8. doi:10.1007/s40520-015-0414-4
32. Dutil M, Handrigan GA, Corbeil P, Cantin V, Simoneau M, Teasdale N, et al. The impact of obesity on balance control in community-dwelling older women. Age (Omaha) (2013) 35(3):883–90. doi:10.1007/s11357-012-9386-x
33. Lim E. Sex differences in fear of falling among older adults with low grip strength. Iran J Public Health (2016) 45(5):569–77.
34. Milanovic Z, Jorgić B, Trajković N, Sporis G, Pantelić S, James N. Age-related decrease in physical activity and functional fitness among elderly men and women. Clin Interv Aging (2013) 8:549. doi:10.2147/CIA.S44112
35. Bassey EJ. Longitudinal changes in selected physical capabilities: muscle strength, flexibility and body size. Age Ageing (1998) 27(Suppl 3):12–6. doi:10.1093/ageing/27.suppl_3.12
36. Jenkins KR. Body-weight change and physical functioning among young old adults. J Aging Health (2004) 16(2):248–66. doi:10.1177/0898264303262626
37. Forrest KYZ, Zmuda JM, Cauley JA. Patterns and determinants of muscle strength change with aging in older men. Aging Male (2005) 8(3–4):151–6. doi:10.1080/13685530500137840
38. Bird M-L, Pittaway JK, Cuisick I, Rattray M, Ahuja KDK. Age-related changes in physical fall risk factors: results from a 3 year follow-up of community dwelling older adults in Tasmania, Australia. Int J Environ Res Public Health (2013) 10(11):5989–97. doi:10.3390/ijerph10115989
39. Caballer VB, Lisón JF, Rosado-Calatayud P, Amer-Cuenca JJ, Segura-Orti E. Factors associated with the 6-minute walk test in nursing home residents and community-dwelling older adults. J Phys Ther Sci (2015) 27(11):3571–8. doi:10.1589/jpts.27.3571
40. Lauretani F, Russo CR, Bandinelli S, Bartali B, Cavazzini C, Di Iorio A, et al. Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol (2003) 95(5):1851–60. doi:10.1152/japplphysiol.00246.2003
41. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing (2010) 39(4):412–23. doi:10.1093/ageing/afq034
42. Olguín T, Bunout D, de la Maza MP, Barrera G, Hirsch S. Admission handgrip strength predicts functional decline in hospitalized patients. Clin Nutr ESPEN (2017) 17:28–32. doi:10.1016/j.clnesp.2016.12.001
43. Owusu C, Margevicius S, Schluchter M, Koroukian SM, Berger NA. Short physical performance battery, usual gait speed, grip strength and vulnerable elders survey each predict functional decline among older women with breast cancer. J Geriatr Oncol (2017) 8(5):356–62. doi:10.1016/j.jgo.2017.07.004
44. Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev (2011) 10(4):430–9. doi:10.1016/j.arr.2011.03.003
45. Guaraldi G, Silva AR, Stentarelli C. Multimorbidity and functional status assessment. Curr Opin HIV AIDS (2014) 9(4):386–97. doi:10.1097/COH.0000000000000079
46. Portz JD, Kutner JS, Blatchford PJ, Ritchie CS. High symptom burden and low functional status in the setting of multimorbidity. J Am Geriatr Soc (2017) 65(10):2285–9. doi:10.1111/jgs.15045
47. Hubbard RE, Lang IA, Llewellyn DJ, Rockwood K. Frailty, body mass index, and abdominal obesity in older people. J Gerontol A Biol Sci Med Sci (2010) 65(4):377–81. doi:10.1093/gerona/glp186
48. Toosizadeh N, Wendel C, Hsu C-H, Zamrini E, Mohler J. Frailty assessment in older adults using upper-extremity function: index development. BMC Geriatr (2017) 17(1):117. doi:10.1186/s12877-017-0509-1
49. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet (2012) 380(9836):37–43. doi:10.1016/S0140-6736(12)60240-2
50. Rose DJ. Preventing falls among older adults: no “one size suits all” intervention strategy. J Rehabil Res Dev (2008) 45(8):1153–66. doi:10.1682/JRRD.2008.03.0041
51. Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med (2002) 18(2):141–58. doi:10.1016/S0749-0690(02)00002-2
52. WHO. Global Recommendations on Physical Activity for Health. Geneva: World Health Organization (2010). 60 p.
Keywords: predictors of disability, functional capacity, physical activity levels, aging, handgrip, 6 min walk test
Citation: Tomás MT, Galán-Mercant A, Carnero EA and Fernandes B (2018) Functional Capacity and Levels of Physical Activity in Aging: A 3-Year Follow-up. Front. Med. 4:244. doi: 10.3389/fmed.2017.00244
Received: 11 August 2017; Accepted: 15 December 2017;
Published: 09 January 2018
Edited by:
Giuseppe Liotta, Università degli Studi di Roma Tor Vergata, ItalyReviewed by:
Liang-Yu Chen, Taipei Veterans General Hospital, TaiwanCopyright: © 2018 Tomás, Galán-Mercant, Carnero and Fernandes. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Teresa Tomás, dGVyZXNhLnRvbWFzQGVzdGVzbC5pcGwucHQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.