- 1Department of Mechanical Engineering, Faculty of Engineering, Diponegoro University, Semarang, Central Java, Indonesia
- 2Department of Mechanical Engineering, Faculty of Engineering, Wahid Hasyim University, Semarang, Central Java, Indonesia
- 3Department of Orthopaedic and Traumatology, Dr. Kariadi Hospital, Semarang, Central Java, Indonesia
- 4Department of Industrial Engineering, Faculty of Industrial Technology, University of Atma Jaya Yogyakarta, Yogyakarta, Indonesia
Total Knee Arthroplasty (TKA) proposed as an alternative treatment for damaged knee joints of humans is reviewed. The commercial application of TKA can help patients to improve their daily normal activities. Here the high-flex type total knee arthroplasty (High-Flex TKA) is typically designed for the patient’s convenience on which the greater range of motion can be adjusted for extreme activities such as Seiza and Muslim praying. However, the present High-Flex TKAs have not fulfilled the needs of Indonesians for religious activities with a flexion angle of 150°–165°. Therefore, this review aims to examine the flexion range of High-Flex TKAs proposed for the needs of Indonesians. This study is a narrative review, all studies published and reviewed are related to the range of flexion angles on the use of products from many manufacturers and various types that have been used by patients, as well as the development of a CAD-based TKA design. It was proposed in the present study that the flexion angle on High-Flex TKAs may be optimized by thickening the posterior femoral condyle, creating a medial pivot system, and applying a single radius system on the femoral component. Whereas, the tibial insert component could be designed by setting up the posterior tibial slope, and creating a post-cam stabilizer mechanism. Many knowledge gaps related to the population of research objects, lack of research on extreme angles, development of TKA components, are discussed. Further needs of extensive research on TKA in Mongoloid races are anticipated to be introduced for extreme angles and most comprehensive product development for optimization of the flexion angle.
Introduction
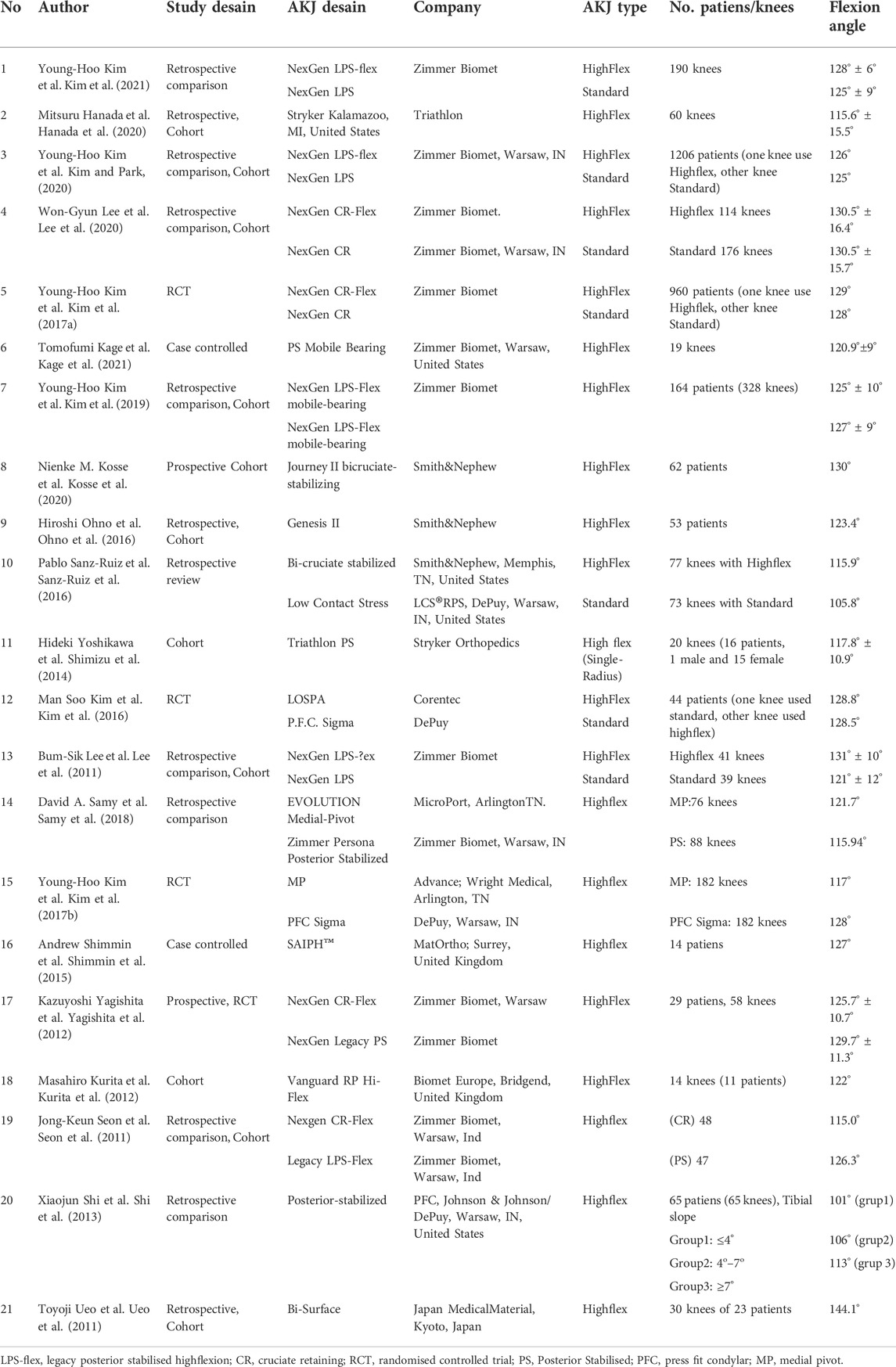
The knee joints are regarded as one of the complex parts of the human body, in which the thigh bone (femur) to the shin bone (tibia) is linked. In its place, the smaller bone in conjunction with the tibia (fibula) and the kneecap (patella) make the knee joint (Figure 1A). In daily life, the knees support body weights, especially when standing, walking, running, and jumping. Accordingly, the knee joint plays a significant role in mobilization or moving around. In this manner, muscles, bones, ligaments, cartilage, synovial tissue, synovial fluid, and other connective tissues strongly control the anatomical function and stability of the knee (Gupton et al., 2021). In general, the structure inside the knee joint can be categorized into three groups, namely stability structure (Ligament), load-carrying structure (Femoral, Tibial, and Patella), and other supporting structures (synovial fluid, capsules, and bursa) (Jawad and Michael, 2017). In particular, the knee joint commonly receives the most loading of body weight. The maximum load received by the knee joint can reach 3.9 times the bodyweight at the time of normal walking, and 8 times the bodyweight at the time of walking in heavy terrain conditions, while at the time of standing still receives a load equal to body weight (Kuster et al., 1997).
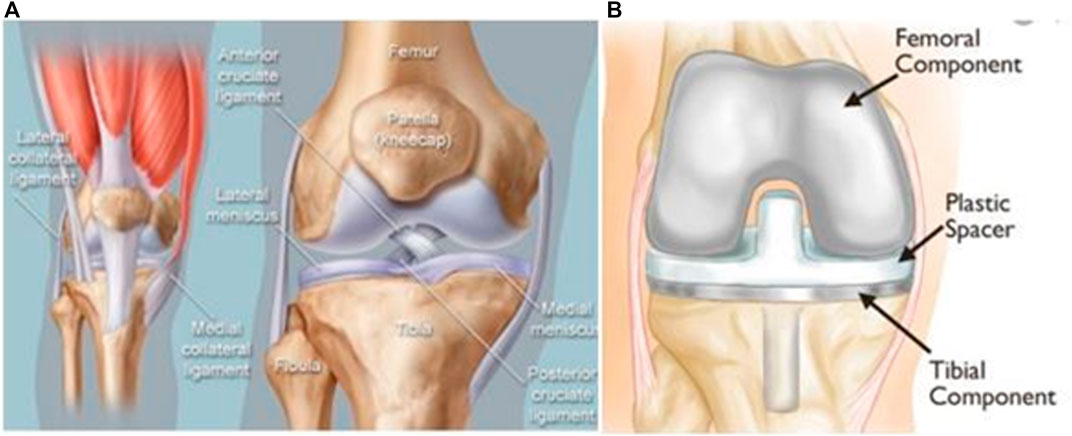
FIGURE 1. (A) Anatomy of human knee joints (Hoffman, 2019), (B) Total knee arthroplasty prostheses (Orthoinfo. Revision, 2021).
Further, the range of flexion in the knee joint relates to many physical activities, for instance, going up and down stairs requires 90°–120° flexion; getting in and out of the bathtub requires 130°–140° flexion; and kneeling, squatting, and sitting cross-legged require more than that 150° flexion (Rowe et al., 2000). In particular, physical activities such as cross-legged sitting, kneeling, and squatting are commonly performed in daily routine in social, cultural, and religious activities for many Asians (i.e., Japanese, Koreans, and Indonesians). Type of physical activities in Japanese tradition such as Seiza (sitting on both knees), agura (sitting cross-legged) and yokosuwari (sitting with legs bent to the side) require a large flexion angle (Park et al., 2007), (Ohno et al., 2016). Also, Seiza requires a deep flexion greater than 150° (Figure 2A) (Ueo et al., 2011). Additionally, a Muslim in performing praying requires a large flexion. Sitting tasyahud in praying requires the greatest range of flexion; this physical movement is the same as seiza requiring a degree flexion from 150° to 165° (Figure 2B) (Hefzy et al., 1998), (Lestari et al., 2015).
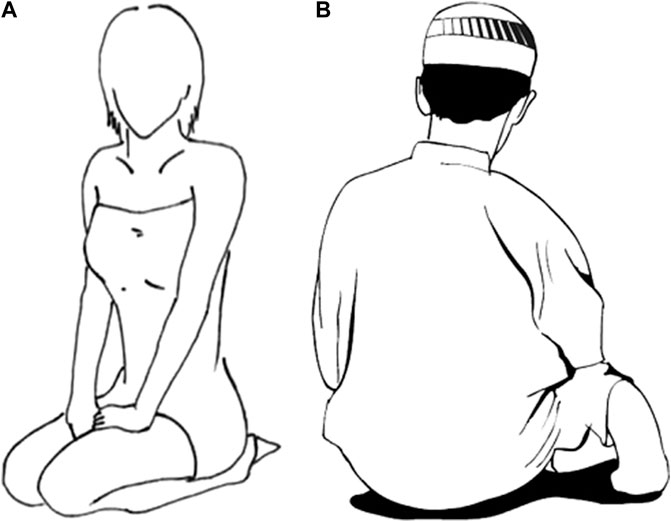
FIGURE 2. Sitting positions that require large flexion angles (A) Seiza (Ohno et al., 2016), (B) Tasyahud (Magee, 2008).
Because of health conditions such as knee joint disorders caused by accidents or diseases such as bone loss (osteoporosis), cartilage degeneration (osteoarthritis/OA), rheumatoid arthritis (RA), and birth defects, the flexion angles have become restricted in their movement. Among the most common disorders is osteoarthritis/OA (Mora et al., 2018). In this case, wear and tear can occur on the femoral bone and tibial bone that has sliding contacted with each other, resulting in a reduction in bone surface volume (osteolysis). This disease may be usually associated with the aging process resulting in degeneration of the cartilage (Hafez and Mohammed, 2014). Accordingly, an alternative to overcome knee joint disorders is total knee arthroplasty (TKA), which mainly consists of femoral components, plastic spacer/tibial insert, and tibial components (Figure 1B). Currently, TKA system has been widely used as an alternative treatment for damaging knee joints in humans.
An idea of the scientific and commercial importance of TKA come from a search on the works of literature. Kurtz et al. (2011) reported in 18 countries until 2011 that TKA cases reached 1,324,000 cases. The commercial application of TKAs may help many patients to carry out their physical activities. However, several studies have shown that patient’s TKA has still an obstacle in a movement when compared to normal joints (Li et al., 2007; Yagishita et al., 2012; Hanada et al., 2020; Kosse et al., 2020). Here patients have problems when doing deep flexion, this can be seen at the postoperative flexion smaller than preoperative. The range of flexion angles is limited in postoperative TKA patients as shown in Figure 3.
Furthermore, two types of commercial TKA prosthese product could be found in the world market, namely the standard/conventional type of TKA (the ability of flexion 125°) and the type of the TKA with the high flexion (the ability of flexion >125°) which is called high flexion (High-Flex) (Long and Scuderi, 2008). The range of flexion in the High-Flex TKAs can be set up to 15°–25° more than those of standard types (Jain et al., 2013). The use of this type of implant makes it easy for patients to carry out physical activities for a greater range of motion than the standard type (Long and Scuderi, 2008), (Murphy et al., 2009; Lee et al., 2011; Sanz-Ruiz et al., 2016; Kim et al., 2021).
A similar literature study on the most prolific companies indicated that De puy, Johnson, Warsaw, and Indiana, Inc., in the United States produce TKAs standard and High-Flex types with the criteria for application TKA types based on the patient’s activity needs. Further development of the High-Flex TKAs design based on the standard type was changed into the femoral part by increasing the radius of the posterior condyles, thickening the condyles offset, while the tibial insert was changed for the thickness, lengthening the contact groove, and the stabilizer design (Long and Scuderi, 2008). It is, therefore, important to discuss whether the range of flexion suggested to develop TKA could be optimized for the physical activities, before further advocating specific use of TKA in religious practice. Moreover, this review aims to examine the flexion range of High-Flex TKAs proposed for the needs of Indonesians. Accordingly, a comprehensive literature review of the flexion angle range of the High-Flex TKAs are presented along with their potential applications. Further research for next-generation TKA system is briefly proposed for the key innovations responsible for the recent technological advances in modern total knee arthroplasty.
Outcome of high flex total knee arthroplasty
The commercial application of High-flex TKAs are proposed for assisting patients in physical activities that require a large range of flexion, such as the habits of Asian and Middle Eastern people in social, cultural, and religious activities. According to research by Sumino et al. (SuminoRubash and Li, 2013), patient’s TKA from East Asia require a greater range of flexion compared to that of patients from western countries. It was reported that in the Middle East for patients using this type of implant required a mean flexion angle of 140.2° when squatting and 132.8° when praying (Acker et al., 2011), therefore these angles are almost the same as those for a normal knee. Middle Eastern people have a larger thigh circumference than Indonesians, so the flexion is less than 150° when praying. This report confirms that the angle of flexion may be related to the type of population.
Accordingly, the physical activity of praying in Indonesia with the majority of Muslims requires a typical TKA model. The review of the study about TKAs are presented in Table 1. Obviously, the High-Flex TKA has a greater range of flexion when compared to that of standard type, but the difference is not significant, while two reports provided the significant differences of results (Sanz-Ruiz et al., 2016), (Lee et al., 2011). Likewise, a systematic review with Meta-Analysis conducted by Jiang et al. (2015) also reported that the difference in flexion angle between High-Flex TKA type and standard was not significant.
Recently, several studies have reported that the use of High-Flex TKAs have a risk of aseptic loosening until the revision has been performed even though the percentage is relatively small (Kim et al., 2021), (Han et al., 2007; Bollars et al., 2011; Kim et al., 2017a; Kim and Park, 2020; Lee et al., 2020). The rate of revision after 20 years of use can be as high as 5.2% for the High-Flex type, and approximately 3.2% of the standard type (Kim et al., 2021). Another study reported revisions to the High-Flex TKA 1.6% and 1.3% occurred in the standard type for use up to 15 years (Kim and Park, 2020). However, the systematic review by Jiang et al. (2015) reported that there was no significant difference in the number of revision incidents in standard or High-Flex TKA, in which the High-flex TKA rate of survival is good enough to reach more than 10 years (Hafez and Mohammed, 2014), (Li et al., 2007; Yagishita et al., 2012; Kosse et al., 2020). According to Jeon et al. (2016) post-operatively after 6 years did not show symptoms of aseptic loosening in the use of this implant. This feature indicates that the High-Flex TKA type is safe to use and has the same service life as the standard type.
Further studies reported that the average flexion range of a patient’s TKA is below 150° (Table 1). However, in some cases, the postoperative flexion may be up to 150°, whereas, before surgery, it can reach 153° (Kosse et al., 2020). The patient’s High-Flex TKA with a Japanese lifestyle like sitting on the floor showed an increase in the flexion angle from 112°, prior to surgery, to 123° after surgery, but the level of comfort was reduced from 39% to 30% (Ohno et al., 2016). By comparing the TKA High-Flex Cruciate-Retaining model with Posterior Cruciate-Substituting, the flexion angle range is not significantly different (Yagishita et al., 2012). A similar study for comparing the TKA High-Flex Cruciate-Retaining model with Posterior Cruciate-Substituting, however, showed a significant difference in the flexion angle range (Seon et al., 2011). The different results of this study may relate to other factors, including the type of implant used, such as gender, age, weight, femoral size, ligament status, the range of motion before surgery, tibiofemoral angle, type of disease in the knee joint, surgical techniques by medical personnel, and postoperative therapy (Farahini et al., 2013), (Kotani et al., 2005).
Since 1989 in Japan, a typical bi-surface TKA, which has a unique shape, has been developed to meet the needs of their lifestyle of such Seiza, but it was only 3.2% of the cases suitable for foreign workers. Some patients have flexion angles above 150° (Ueo et al., 2011). The results of other studies have also shown that the lifetime of these implants could be reached above 10 years with good functionality and satisfaction (Nakamura et al., 2010).
Therefore, the criterion of success in TKA may include increasing the range of flexion angles and reducing the loss of pain in the knee joint (Farahini et al., 2013). Other researchers have reported that the criteria of success in TKA if the increase in flexion angle between pre and post-surgery is 15°–25° (Jain et al., 2013). Importantly, the TKA success factor may relate to the achievement of knee range of motion corresponding to postoperative physiotherapy (Kotani et al., 2005), (Nakamura et al., 2010). These factors may include proper ligament balancing, management of the PCL, and flexion of the knee at the time of the wound closure. Correspondingly, those complex factors affecting the success of TKA may be adopted for the achievement of flexible angles in the needs of Muslim prayer and Seiza.
Development of femoral components arthroplasty for the knee joint
The development of the femoral design on High-Flex TKA from the standard model may increase the thickness of the posterior femoral condyle (PFC) 2–4 mm (Lee et al., 2011), (Kim et al., 2016), (Yang et al., 2016). The posterior femoral condyle size in the standard model is 8 mm, whereas the High-Flex size is 10 mm (Kim et al., 2016). The addition of thickness replaced the cut part of the candle femur bone (Kim et al., 2016). This condition made the posterior femoral strength better, whereas the greater the angle of flexion contributes to an increased load. It was proposed previously that the increase in thickness by 2 mm may increase the flexion angle of 10°. This is because the contact area between the posterior femoral and the tibial insert increases in length as shown in Figure 4A (Lee et al., 2011). The development of the CAD-based TKA model by Darmanto et al. (2022a), showed that the addition of 1 mm PFC thickness caused an increase in the flexion angle of 3.2°.
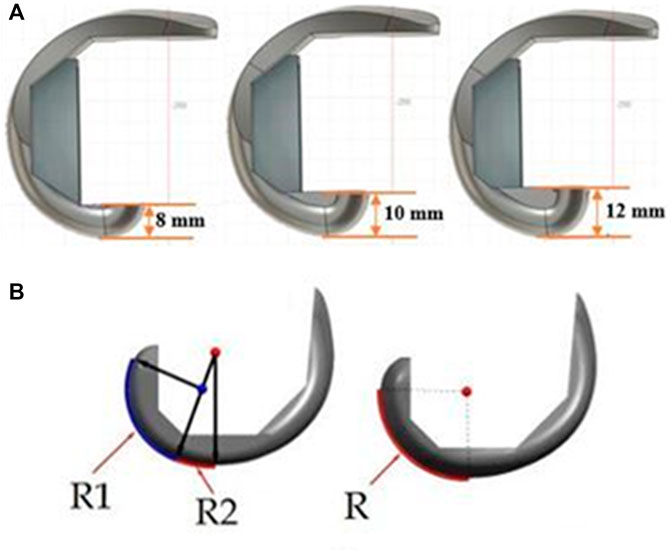
FIGURE 4. Development of femoral components AKJ, (A) Change of PFC (Darmanto et al., 2022a), (B) Change of radius system (Fekete, 2013).
According to several studies, the change in the thickness of the posterior femoral condyle is directly proportional to the change in the flexion gap (Matziolis et al., 2012; Yoon et al., 2013; Chia et al., 2018). The flexion gap is the distance between the tip of the femur and the tibia during flexion, and it is influenced by the system and the type of implant used (Kotani et al., 2005). This change in thickness causes the knee to be unstable when performing rollbacks on flexion movements. Flexion gap and extension gap in TKA is shown in Figure 5. Ideally between extension gap and flexion gap is the same, so that in the case of anterior-posterior (A-P) movement the knee remains stable. The thickening of the posterior femoral condyle will be a flexion gap greater than the extension gap.
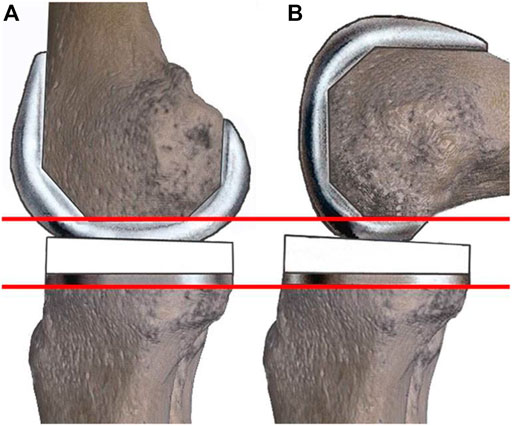
FIGURE 5. Extension gap (A) and flexion gap at (B) TKA (Nowakowski et al., 2014).
In view of femoral components in TKA, two radius systems could be developed, namely single radius, and multi-radius. Multi radius and single radius systems on TKA femoral components are shown in Figure 4B. A multi-radius femoral system could be formed with a variety of different radius, while the single radius system may form of one radius only. Knee joint instability due to flexion gap changes could be reduced by a single radius system in femoral components. According to Shimizu et al. (2014), a single radius system in femoral components provides knee stability to mid-angle flexion. Additionally, a single radius system in the femoral component does not affect the attainment of the flexion angle. Obviously, there is no difference in the result achieved against the flexion angle between the single radius and the multi-radius system (Jin et al., 2020). The results of the development of a CAD-based AKJ model by Darmanto et al. (2021) showed that a single radius system increases the range of flexion angles by 5.2°. Also, other studies have reported that a single radius system reduces A-P translation by 80% (Clary et al., 2013), so TKA became more stable.
Another improvement in the femoral component is through the Medial Pivot which is the center of contact between the femoral and tibial centers in the medial part. The medial becomes the center of movement of the knee for both flexion and rotation; this causes the contact displacement in the medial to be smaller than the lateral. The medial pivot was more satisfactory for the patient, while the range of motion of flexion did not change significantly (Samy et al., 2018), (Kim et al., 2017b), (French et al., 2020), (Carvalho Júnior et al., 2017). The study conducted by Liu et al. reported that the difference in thickness between lateral posterior and medial posterior 2.7 mm gave the most optimal effect of internal rotation (Liu et al., 2012). It was proposed that the medial pivot TKA contact type is similar to the anatomy of the original knee joint. When the flexion angle is large, the internal rotation of the femoral movement can occur (Bae et al., 2016). The medial pivot system affected the A-P translation on the medial and lateral sides, the low femoral condylar height difference will cause a small A-P translation difference between medial and lateral (Darmanto et al., 2022b). Modification of the femoral component by changing the posterior femoral condyle provides an additional range of flexion but has the side effect of aseptic loosening which can lead to revision. The improvement of the medial pivot system does not provide additional flexion angle, but rather provides stability and comfort to the patient.
Development of tibial components arthroplasty for knee joint
The tibial component has been extensively developed to support TKA to obtain a large range of flexion angles. Currently, the developed designs of the component have been focused on the post-cam stabilizer mechanism, tibial slope, and mobile bearing. In particular, the design of the post-cam stabilizer mechanism consists of two parts, such as the tibial post on the tibial insert component and the femoral cam on the femoral component, and the two are paired with each other. Post-cam mechanisms have been widely developed recently, and the results showed that a significant degree of flexion angle range could be obtained as compared to cruciate-retaining (Kosse et al., 2020), (Yagishita et al., 2012), (Sanz-Ruiz et al., 2016), (Seon et al., 2011). Principally, the post-cam mechanism can prevent the femoral from sliding out of the tibial insert area when the flexion angle is large. In this case, the Japanese people with this type of implant feel a satisfaction rate of up to 30% when doing activities on the floor (Ohno et al., 2016).
Further development of the post-cam stabilizer design has made various models such as a curve on a curve and a plate on a plate model. The post-cam stabilizer mechanism for TKA system is shown in Figure 6A. The curve on curve model has the advantage of internal rotational motion when the angle of flexion is large. This reason is that the curve on curve model has a larger free-angle than a plate on a plate model (Lin et al., 2011). In dynamic testing with a treadmill at a speed of 1 m/s, the curve on curve model showed a greater A-P translation distance than that of a plate-on-plate model (Tamaki et al., 2013). Of these two post-cam models, the curve on curve model has a closer characteristic to the natural properties of the knee joint. The limitation of the TKA high-flex design is that the flexion conditions cause contact on the center of the post-cam stabilizer (Ingrassia et al., 2013), (Watanabe et al., 2017), so the contact stress becomes higher, these causes wear on the CAM part. This condition needs further research to consider the use of a better type of material.
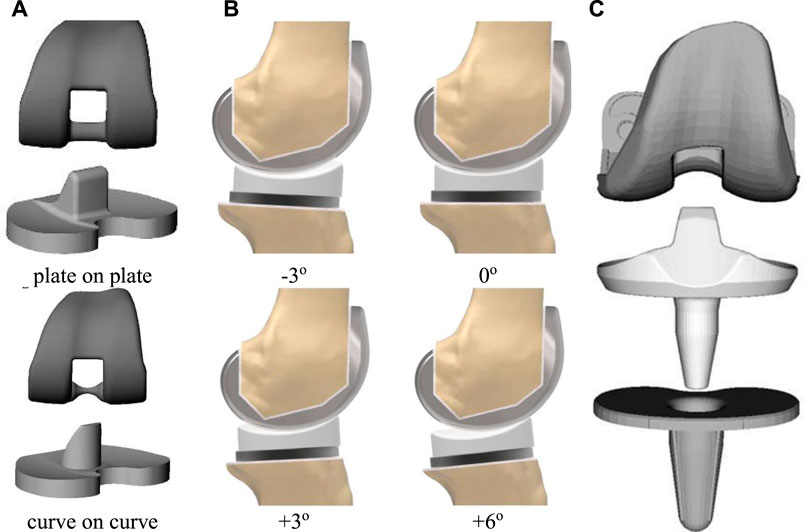
FIGURE 6. Development of tibial insert TKA components, (A) The post-cam stabilizer mechanism (Shimmin et al., 2015), (B) Change of PTS (Kang et al., 2018a), (C) The mobile bearing System (Kurita et al., 2012).
In view of the tibial slope, a development of the tibial component is made by adjusting the slope towards the femoral (posterior tibial slope). This method is intended to further optimize the flexion angle. Here, the inclination can be adjusted in two ways, first by thinning one part of the tibial insert A-P, second by tilting the cut on the surface of the tibial bone. According to Hofmann et al. (Kang et al., 2018a), the tibial slope ranges from 0° to 20° are suitable for the type of human population. Moreover, the tibial slope significantly affects the flexion angle range in that the angle of inclination is directly proportional to the flexion range (Shi et al., 2013), (Darmanto et al., 2021), (Fujito et al., 2018), (Massin and Gournay, 2006). In another study based on CAD models, every 1° slope increased the flexion angle by 1.03° (Darmanto et al., 2022a). In contrast, the tibial slope did not significantly affect the A-P translation distance (Darmanto et al., 2022b), (Fujito et al., 2018). The illustration of tibial slope changes in TKA is shown in Figure 6B. Another study reported that the larger the tibial slope provided the less contact stress (Koh et al., 2021), (Kang et al., 2018b). Obviously, the tibial slope affects the flexion gap and the slope of the tibial insert is directly proportional to the flexion gap (Nowakowski et al., 2014), (Okazaki et al., 2014). Accordingly, the flexion gap could be reduced by using a single radius system of the femoral component, as in the above femoral development. The development of the high-flex TKAs design by increasing the tibial slope of tibial insert is limited to a minimum thickness of 6 mm (Lingaraj et al., 2011), if the tibial slope is too large, the posterior thickness will be less than this requirement. Meanwhile, if the posterior part is at least 6 mm, then the anterior part becomes too thick (Darmanto et al., 2022a), so it is not suitable to be applied to non-revised patients.
Additionally, supporting the rotational movement of the TKA system requires the development of the tibial component of the mobile bearing model. The mobile bearing system with a post-cam stabilizer is shown in Figure 6C. In a mobile bearing, the tibial base metal and the tibial insert can move relative to one another, while the fixed bearing is in a permanent position. The range of flexion between mobile and fixed bearing types has no difference in angle (Chaudhry and Goyal, 2018), however, mobile bearings make a greater contribution to the rotation angle (Kurita et al., 2012), (Tamaki et al., 2009). Correspondingly, the development of the tibial component of the TKA system by modifying the post-cam mechanism and adjusting the posterior tibial slope provides a significant change in the range of flexion. Meanwhile, the development of the mobile bearing model has a great impact on the angle of rotation. The mobile bearing model has the same function as the medial pivot, but the medial pivot is functionally more like the original.
Research gap and future research
The current research on the range of flexible angles in TKA has been intensively carried out for clinical cases from the American and European populations belonging to the Caucasoid race. This population has an active lifestyle of physical activity that requires low flexion angles, therefore the standard TKA is suitable for their need. However, future research works need to be done for the needs of Asians with Mongoloid race, in which this race has a habit of physical activities on the floor that require a high flexion angle.
Table 1 above presents the average flexion angle that could be reached still below 150°. In spite of using High-flex TKAs, only two researchers, (Ueo et al., 2011; Kosse et al., 2020) demonstrated their research results of being able to reach flexion angle above 150°, but the percentage of success of TKA is very low. Moreover, their works were not discussed in detail about the success of the range of flexible angles to above 150°. Accordingly, it is necessary to conduct a detailed study about the extreme angle on the TKA system.
There are also some reports indicating that the flexion angle could be optimized by the development of TKA components through thickening posterior femoral condyle (Lee et al., 2011; Kim et al., 2016; Yang et al., 2016; Darmanto et al., 2022a), creating a single radius system (Shimizu et al., 2014; Jin et al., 2020; Darmanto et al., 2021; Clary et al., 2013), creating a medial pivot system (Samy et al., 2018; Kim et al., 2017b; French et al., 2020; Carvalho Júnior et al., 2017; Darmanto et al., 2022b), setting up posterior tibial slope (Shi et al., 2013; Darmanto et al., 2022a; Hohmann and Bryant, 2007; Fujito et al., 2018; Massin and Gournay, 2006), and creating a post-cam stabilizer mechanism (Ohno et al., 2016; Kosse et al., 2020; Yagishita et al., 2012), (Sanz-Ruiz et al., 2016; Seon et al., 2011; Tamaki et al., 2013). In the market, each prolific company has its characteristic in the development of TKA components. However, further research is needed to accumulate these developments in one type of product, so that TKA prosthesis products could be obtained at the most optimal angle flexibility.
Conclusion
Based on the analysis of the current study on the application of TKAs, it can be concluded: 1) High-Flex TKAs on the market has not fulfilled the needs of Indonesians for religious activities which require a flexion range of 150°–165°, 2) the flexion angle on High-Flex TKA could be optimized by thickening the posterior condyles offset, using a single radius and medial pivot on the femoral component, while on the tibial insert component by setting up a posterior tibial slope and use a post-cam stabilizer mechanism.
Author contributions
PA conceived and designed the analysis; wrote the paper; correspondent authors DD: collected the data; contributed data; wrote the paper RN: contributed data and analysis tools RI: Performed the analysis JJ: wrote the paper; conceived and designed the analysis AB: wrote the paper; funding recipient; performed the analysis.
Acknowledgments
The authors thank the Deputy for Strengthening Research and Development, the Ministry of Research and Technology, Higher Education, the Republic of Indonesia for research funding under Ph.D. research grants of number: 017/ES/PG.02.00.PT/2022 and 18752/UN7.6.1/PP/2022.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Acker, S. M., Cockburn, R. A., Krevolin, J., Li, R. M., Tarabichi, S., and Up, W. (2011). Knee kinematics of high-flexion activities of daily living performed by male Muslims in the Middle East. J. Arthroplasty 26, 319–327. doi:10.1016/j.arth.2010.08.003
Bae, D. K., Cho, S. D., Im, S. K., and Song, S. J. (2016). Comparison of midterm clinical and radiographic results between total knee arthroplasties using medial pivot and posterior-stabilized prosthesis—a matched pair analysis. J. Arthroplasty 31, 419–424. doi:10.1016/j.arth.2015.09.038
Bollars, P., Luyckx, J. P., Innocenti, B., Labey, L., Victor, J., and Bellemans, J. (2011). Femoral component loosening in high-flexion total knee replacement: An in Vitro comparison of high-flexion versus conventional designs. J. Bone Jt. Surg. Br. volume 93, 1355–1361. doi:10.1302/0301-620X.93B10.25436
Carvalho Júnior, L. H., Teixeira, B. P., Bernardes, C. O. S., Soares, L. F. M., Gonçalves, M. B. J., and Temponi, E. F. (2017). Range of motion predictability after total knee arthroplasty with medial pivot prosthesis. Rev. Bras. Ortop. 52, 197–202. doi:10.1016/j.rboe.2017.03.001
Chaudhry, A., and Goyal, V. K. (2018). Fixed-bearing versus high-flexion RP total knee arthroplasty (TKA): Midterm results of a randomized controlled trial. J. Orthop. Traumatol. 19, 2–4. doi:10.1186/s10195-018-0493-z
Chia, Z. Y., Pang, H. N., Tan, M. H., and Yeo, S. J. (2018). Gap difference in navigated TKA: A measure of the imbalanced flexion-extension gap. Sicot-J. 4, 30. doi:10.1051/sicotj/2018007
Clary, C. W., Fitzpatrick, C. K., Maletsky, L. P., and Rullkoetter, P. J. (2013). The influence of total knee arthroplasty geometry on mid-flexion stability: An experimental and finite element study. J. Biomech. 46, 1351–1357. doi:10.1016/j.jbiomech.2013.01.025
Darmanto, D., Novriansyah, R., Ismail, R., Jamari, J., Anggoro, P. W., and Bayuseno, A. P. (2022). Reconstruction of the artificial knee joint using a reverse engineering approach based on computer-aided design. J. Med. Eng. Technol. 46, 136–147. doi:10.1080/03091902.2022.2026502
Darmanto, D., Novriansyah, R., Ismail, R., Jamari, J., Bayuseno, A. P., and Anggoro, P. W. (2022). Computer-aided design for analyzing the influence of anteroposterior translation on artificial knee joint stability. Mater. Today Proc. 63, S159–S165. doi:10.1016/j.matpr.2022.02.120
Darmanto, D., Novriansyah, R., Ismail, R., Jamari, J., Bayuseno, A. P., and Anggoro, P. W. (2021). “Computer-Aided design for analyzing the influence of single radius on flexion angle of artificial knee joint,” in 2021 IEEE International Biomedical Instrumentation and Technology Conference (IBITeC), Yogyakarta, Indonesia, 20-21 October 2021, 114–118. doi:10.1109/ibitec53045.2021.9649381
Farahini, H., Moghtadaei, M., Bagheri, A., and Akbarian, E. (2013). Factors influencing range of motion after total knee arthroplasty. Iran. Red. Crescent Med. J. 15, 15–10. doi:10.5812/ircmj.1361
Fekete, G. (2013). Kinetics and kinematics of the human knee joint under standard and non-standard squat movement (Godollo: Szent István University). (Doctoral thesis).
French, S. R., Munir, S., and Brighton, R. (2020). A single surgeon series comparing the outcomes of a cruciate retaining and medially stabilized total knee arthroplasty using kinematic alignment principles. J. Arthroplasty 35, 422–428. doi:10.1016/j.arth.2019.09.021
Fujito, T., Tomita, T., Yamazaki, T., Oda, K., Yoshikawa, H., and Sugamoto, K. (2018). Influence of posterior tibial slope on kinematics after cruciate-retaining total knee arthroplasty. J. Arthroplasty 33, 3778–3782.e1. doi:10.1016/j.arth.2018.07.029
Gupton, M., Imonugo, O., and Terreberry, R. R. (2021). Anatomy, bony pelvis and lower limb, knee. Available at: https://ncbi.nlm.nih.gov/books/NBK500017/. [accessed 6 March 2021].
Hafez, A. R., and Mohammed, A. (2014). Knee osteoarthritis: A review of literature physical medicine and rehabilitation - knee osteoarthritis: A review of literature. Phys. Med. Rehabil. Int. 1, 8.
Han, H. S., Kang, S. B., and Yoon, K. S. (2007). High incidence of loosening of the femoral component in legacy posterior stabilised-flex total knee replacement. J. Bone Jt. Surg. Br. volume 89, 1457–1461. doi:10.1302/0301-620X.89B11.19840
Hanada, M., Hotta, K., Furuhashi, H., Koyama, H., and Matsuyama, Y. (2020). Association of knee flexion angle after posterior-stabilized total knee arthroplasty with postoperative tibial external position relative to the femur and the extent of tibial internal rotation from knee extension to flexion. Knee 27, 1467–1475. doi:10.1016/j.knee.2020.07.084
Hefzy, M. S., Kelly, B. P., and Cooke, T. D. (1998). Kinematics of the knee joint in deep flexion: A radiographic assessment. Med. Eng. Phys. 20, 302–307. doi:10.1016/S1350-4533(98)00024-1
Hoffman, M. (2019). Human anatomy. Available at: https://webmd.com/pain-management/knee-pain/picture-of-the-knee. [accessed 22 May 2021].
Hohmann, E., and Bryant, A. (2007). Closing or opening wedge high tibial osteotomy: Watch out for the slope. Oper. Tech. Orthop. 17, 38–45. doi:10.1053/j.oto.2006.09.010
Ingrassia, T., Nalbone, L., Nigrelli, V., Tumino, D., and Ricotta, V. (2013). Finite element analysis of two total knee joint prostheses. Int. J. Interact. Des. Manuf. 7, 91–101. doi:10.1007/s12008-012-0167-7
Jain, S., Pathak, A. C., Kanniyan, K., Kulkarni, S., Tawar, S., and Mane, P. (2013). High-flexion posterior-stabilized total knee prosthesis: Is it worth the hype? Knee Surg. Relat. Res. 25, 100–105. doi:10.5792/ksrr.2013.25.3.100
Jawad, F. A., and Michael, J. G. (2017). Anatomy and physiology of knee stability. J. Funct. Morphol. Kinesiol. 2, 34. doi:10.3390/jfmk2040034
Jeon, Y. S., Shin, J. S., Jung, J. H., and Kim, M. K. (2016). Total knee arthroplasty using NexGen LPS-flex® improves clinical outcomes without early loosening: Minimum 6-year follow-up results. J. Orthop. Surg. Res. 11, 83–84. doi:10.1186/s13018-016-0419-5
Jiang, Y., Yao, J. F., Xiong, Y. M., Ma, J. B., Kang, H., and Xu, P. (2015). No superiority of high-flexion vs standard total knee arthroplasty: An update meta-analysis of randomized controlled trials. J. Arthroplasty 30, 980–986. doi:10.1016/j.arth.2015.01.047
Jin, Q. H., Lee, W. G., Song, E. K., Kim, W. J., Jin, C., and Seon, J. K. (2020). No difference in the anteroposterior stability between the GRADIUS and multi-radius designs in total knee arthroplasty. Knee 27, 1197–1204. doi:10.1016/j.knee.2020.05.019
Kage, T., Inui, H., Tomita, T., Yamazaki, T., Taketomi, S., Yamagami, R., et al. (2021). In vivo kinematics of a newly updated posterior-stabilised mobile-bearing total knee arthroplasty in weight-bearing and non-weight-bearing high-flexion activities. Knee 29, 183–189. doi:10.1016/j.knee.2021.02.005
Kang, K. T., Koh, Y. G., Son, J., Kwon, O. R., Lee, J. S., and Kwon, S. K. (2018). Influence of increased posterior tibial slope in total knee arthroplasty on knee joint biomechanics: A computational simulation study. J. Arthroplasty 33, 572–579. doi:10.1016/j.arth.2017.09.025
Kang, K. T., Kwon, S. K., Son, J., Kwon, O. R., Lee, J. S., and KohYG, (2018). Effects of posterior condylar offset and posterior tibial slope on mobile-bearing total knee arthroplasty using computational simulation. Knee 25, 903–914. doi:10.1016/j.knee.2018.06.011
Kim, M. S., Kim, J. H., Koh, I. J., Jang, S. W., and Jeong, D. H. (2016). Is high-flexion total knee arthroplasty a valid concept? Bilateral comparison with standard total knee arthroplasty. J. Arthroplasty 31, 802–808. doi:10.1016/j.arth.2015.09.001
Kim, Y. H., and Park, J. W. (2020). Comparison of modular conventional and high-flexion posterior-stabilized total knee arthroplasties in the same patients at a mean follow-up of 15 years. J. Arthroplasty 35, 1262–1267. doi:10.1016/j.arth.2019.12.022
Kim, Y. H., Park, J. W., and Jang, Y. S. (2021). 20-Year minimum outcomes and survival rate of high-flexion versus standard total knee arthroplasty. J. Arthroplasty 36, 560–565. doi:10.1016/j.arth.2020.07.084
Kim, Y. H., Park, J. W., and Kim, J. S. (2017). Clinical outcome of medial pivot compared with press-fit condylar sigma cruciate-retaining mobile-bearing total knee arthroplasty. J. Arthroplasty 32, 3016–3023. doi:10.1016/j.arth.2017.05.022
Kim, Y. H., Park, J. W., and Kim, J. S. (2017). Do high-flexion total knee designs increase the risk of femoral component loosening? J. Arthroplasty 32, 1862–1868. doi:10.1016/j.arth.2017.01.026
Kim, Y. H., Park, J. W., and Kim, J. S. (2019). The long-term results of simultaneous high-flexion mobile-bearing and fixed-bearing total knee arthroplasties performed in the same patients. J. Arthroplasty 34, 501–507. doi:10.1016/j.arth.2018.11.007
Koh, Y. G., Park, K. M., Kang, K. W., Kim, P. S., Lee, Y. H., Park, K. K., et al. (2021). Finite element analysis of the in?uence of the posterior tibial slope on mobile-bearing unicompartmental knee arthroplasty. Knee 29, 125–116. doi:10.1016/j.knee.2021.01.004
Kosse, N. M., Heesterbeek, P. J. C., Defoort, K. C., Wymenga, A. B., and van Hellemondt, G. G. (2020). Maximal flexion and patient outcomes after TKA, using a bicruciate-stabilizing design. Arch. Orthop. Trauma Surg. 140, 1495–1501. doi:10.1007/s00402-020-03491-7
Kotani, A., Yonekura, A., and Bourne, R. B. (2005). Factors influencing range of motion after contemporary total knee arthroplasty. J. Arthroplasty 20, 850–856. doi:10.1016/j.arth.2004.12.051
Kurita, M., Tomita, T., Yamazaki, T., Fujii, M., Futai, K., Shimizu, N., et al. (2012). In vivo kinematics of high-flex mobile-bearing total knee arthroplasty, with a new post-cam design, in deep knee bending motion. Int. Orthop. 36, 2465–2471. doi:10.1007/s00264-012-1673-8
Kurtz, S. M., Ong, K. L, Lau, E., Widmer, M., Maravic, M., Gómez-Barrena, E., et al. (2011). International survey of primary and revision total knee replacement. Int. Orthop. 35, 1783–1789. doi:10.1007/s00264-011-1235-5
Kuster, M. S., Wood, G. A., Stachowiak, G. W., Gächter, A., and Gachter, A. (1997). Joint load considerations in total knee replacement. J. Bone Jt. Surg. Br. 79, 109–113. doi:10.1302/0301-620X.79B1.6978
Lee, B. S., Kim, J. M., Lee, S. J., Jung, K. H., Lee, D. H., Cha, E. J., et al. (2011). High-flexion total knee arthroplasty improves flexion of stiff knees. Knee Surg. Sports Traumatol. Arthrosc. 19, 936–942. doi:10.1007/s00167-010-1272-4
Lee, W. G., Song, E. K., Choi, S. W., Jin, Q. H., and Seon, J. K. (2020). Comparison of posterior cruciate-retaining and high-flexion cruciate-retaining total knee arthroplasty design. J. Arthroplasty 35, 752–755. doi:10.1016/j.arth.2019.10.008
Lestari, H., Izzhati, D. N., Rachmat, N., Setyawan, D., Saputra, E., and Ismail, R. (2015). Measurement of the range of motion on the knees of Indonesians as preliminary data for the design of artificial upper knee legs, (Original in Indonesia). 64–69. Available at: https://unwahas.ac.id/publikasiilmiah/index.php/PROSIDING_SNST_FT/article/viewFile/1142/1248.
Li, P. H., Wong, Y. C., and Wai, Y. L. (2007). Knee flexion after total knee arthroplasty. J. Orthop. Surg. Hong. Kong) 15, 149–153. doi:10.1177/230949900701500204
Lin, K. J., Huang, C. H., Liu, Y. L., Chen, W. C., Chang, T. W., Yang, C. T., et al. (2011). Influence of post-cam design of posterior stabilized knee prosthesis on tibiofemoral motion during high knee flexion. Clin. Biomech. (Bristol, Avon. 6, 847–852. doi:10.1016/j.clinbiomech.2011.04.002
Lingaraj, K., Morris, H., and Bartlett, J. (2011). Polyethylene thickness in unicompartmental knee arthroplasty. Knee 18, 165–167. doi:10.1016/j.knee.2010.04.012
Liu, Y. L., Chen, W. C., Yeh, W. L., McClean, C. J., Huang, C. H., Lin, K. J., et al. (2012). Mimicking anatomical condylar configuration into knee prosthesis could improve knee kinematics after TKA - a computational simulation. Clin. Biomech. (Bristol, Avon. 27, 176–181. doi:10.1016/j.clinbiomech.2011.08.010
Long, W. J., and Scuderi, G. R. (2008). High-flexion total knee arthroplasty. J. Arthroplasty 23, 6–10. doi:10.1016/j.arth.2008.06.024
Massin, P., and Gournay, A. (2006). Optimization of the posterior condylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J. Arthroplasty 21, 889–896. doi:10.1016/j.arth.2005.10.019
Matziolis, G., Hube, R., Perka, C., and Matziolis, D. (2012). Increased flexion position of the femoral component reduces the flexion gap in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 20, 1092–1096. doi:10.1007/s00167-011-1704-9
Mora, J. C., Przkora, R., and Almeida, Y. C. (2018). Knee osteoarthritis: Pathophysiology and current treatment modalities. J. Pain Res. 11, 2189–2196. doi:10.2147/JPR.S154002
Murphy, M., Journeaux, S., and Russell, T. (2009). High-flexion total knee arthroplasty: A systematic review. Int. Orthop. 33, 887–893. doi:10.1007/s00264-009-0774-5
Nakamura, S., Kobayashi, M., Ito, H., Nakamura, K., Ueo, T., and Nakamura, T. (2010). The Bi-Surface total knee arthroplasty: Minimum 10-year follow-up study. Knee 4, 274–278. doi:10.1016/j.knee.2010.02.015
Nowakowski, A. M., Kamphausen, M., Pagenstert, G., Valderrabano, V., and Müller-Gerbl, M. (2014). Influence of tibial slope on extension and flexion gaps in total knee arthroplasty: Increasing the tibial slope affects both gaps. Int. Orthop. 38, 2071–2077. doi:10.1007/s00264-014-2373-3
Ohno, H., Murata, M., Ozu, S., Matsuoka, N., Kawamura, H., and Iida, H. (2016). Midterm outcomes of high-flexion total knee arthroplasty on Japanese lifestyle. Acta Orthop. Traumatol. Turc. 50, 527–532. doi:10.1016/j.aott.2016.08.005
Okazaki, K., Tashiro, Y., Mizu-uchi, H., Hamai, S., Doi, T., and Iwamoto, Y. (2014). Influence of the posterior tibial slope on the flexion gap in total knee arthroplasty. Knee 21, 806–809. doi:10.1016/j.knee.2014.02.019
Orthoinfo. Revision (2021). Total knee replacement. Available at: https://orthoinfo.aaos.org/en/treatment/revision-total-knee-replacement/. (accessed 22 May 2021).
Park, K. K., Chang, C. B., Kang, Y. G., Seong, S. C., and Kim, T. K. (2007). Correlation of maximum flexion with clinical outcome after total knee replacement in Asian patients. J. Bone Jt. Surg. Br. volume 89, 604–608. doi:10.1302/0301-620X.89B5.18117
Rowe, P. J., Myles, C. M., Walker, C., and Nutton, R. (2000). Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: How much knee motion is sufficient for normal daily life? Gait Posture 12, 143–155. doi:10.1016/S0966-6362(00)00060-6
Samy, D. A., Wolfstadt, J. I., Vaidee, I., and Backstein, D. J. (2018). A retrospective comparison of a medial pivot and posterior-stabilized total knee arthroplasty with respect to patient-reported and radiographic outcomes. J. Arthroplasty 33, 1379–1383. doi:10.1016/j.arth.2017.11.049
Sanz-Ruiz, P., Carbo-Laso, E., Alonso-Polo, B., Matas-Diez, J. A., and Vaquero-Martín, J. (2016). Does a new implant design with more physiological kinematics provide better results after knee arthroplasty? Knee 23, 399–405. doi:10.1016/j.knee.2016.02.017
Seon, J. K., Park, J. K., Shin, Y. J., Seo, H. Y., Lee, K. B., and Song, E. K. (2011). Comparisons of kinematics and range of motion in high-flexion total knee arthroplasty: Cruciate retaining vs. substituting designs. Knee Surg. Sports Traumatol. Arthrosc. 19, 2016–2022. doi:10.1007/s00167-011-1434-z
Shi, X., Shen, B., Kang, P., Yang, J., Zhou, Z., and Pei, F. (2013). The effect of posterior tibial slope on knee flexion in posterior-stabilized total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 21, 2696–2703. doi:10.1007/s00167-012-2058-7
Shimizu, N., Tomita, T., Yamazaki, T., Yoshikawa, H., and Sugamoto, K. (2014). In vivo movement of femoral flexion axis of a single-radius total knee Arthroplasty. J. Arthroplasty 29, 2407–2411. doi:10.1016/j.arth.2013.12.001
Shimmin, A., Martinez-Martos, S., Owens, J., Iorgulescu, A. D., and Banks, S. (2015). Fluoroscopic motion study confirming the stability of a medial pivot design total knee arthroplasty. Knee 22, 522–526. doi:10.1016/j.knee.2014.11.011
SuminoRubash, T. H. E., and Li, G. (2013). Does cruciate-retaining total knee arthroplasty enhance knee flexion in western and East asian patient populations? A meta-analysis. Knee 20, 376–383. doi:10.1016/j.knee.2013.03.002
Tamaki, M., Tomita, T., Watanabe, T., Yamazaki, T., Yoshikawa, H., and Sugamoto, K. (2009). In vivo kinematic analysis of a high-flexion, posterior-stabilized, mobile-bearing knee prosthesis in deep knee bending motion. J. Arthroplasty 24, 972–978. doi:10.1016/j.arth.2008.06.012
Tamaki, M., Tomita, T., Yamazaki, T., Yoshikawa, H., and Sugamoto, K. (2013). Factors in high-flex posterior stabilized fixed-bearing total knee arthroplasty affecting in vivo kinematics and anterior tibial post impingement during gait. J. Arthroplasty 28, 1722–1727. doi:10.1016/j.arth.2012.09.006
Ueo, T., Kihara, Y., Ikeda, N., Kawai, J., Nakamura, K., and Hirokawa, S. (2011). Deep flexion-oriented bisurface-type knee joint and its tibial rotation that attributes its high performance of flexion. J. Arthroplasty 26, 476–482. doi:10.1016/j.arth.2010.02.011
Watanabe, T., Koga, H., Horie, M., Katagiri, H., Sekiya, I., and Muneta, T. (2017). Post-cam design and contact stress on tibial posts in posterior-stabilized total knee prostheses: Comparison between a rounded and a squared design. J. Arthroplasty 32, 3757–3762. doi:10.1016/j.arth.2017.07.010
Yagishita, K., Muneta, T., Ju, Y. J., Morito, T., Yamazaki, J., and Sekiya, I. (2012). High-flex posterior cruciate-retaining vs posterior cruciate-substituting designs in simultaneous bilateral total knee arthroplasty. J. Arthroplasty 27, 368–374. doi:10.1016/j.arth.2011.05.008
Yang, G., Chen, W., Sun, X., Zhou, D., Chen, S., Zhang, L., et al. (2016). Full-thickness cartilage-based posterior femoral condylar offset. Influence on knee flexion after posterior-stabilized total knee arthroplasty. Orthop. Traumatology Surg. Res. 102, 441–446. doi:10.1016/j.otsr.2016.02.011
Keywords: total knee arthroplasty, high-flex, femoral, tibial, knee joint
Citation: Darmanto D, Novriansyah R, Anggoro PW, Ismail R, Jamari J and Bayuseno AP (2022) A review on flexion angle in high-flexion total knee arthroplasty for indonesian’s need. Front. Mech. Eng 8:1049796. doi: 10.3389/fmech.2022.1049796
Received: 21 September 2022; Accepted: 18 October 2022;
Published: 01 November 2022.
Edited by:
Amit Bandyopadhyay, Washington State University, United StatesCopyright © 2022 Darmanto, Novriansyah, Anggoro, Ismail, Jamari and Bayuseno. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: P. W. Anggoro, cGF1bHVzd2lzbnVhbmdnb3JvQHltYWlsLmNvbQ==; A. P. Bayuseno, YXBiYXl1c2Vub0BnbWFpbC5jb20=
†These authors have contributed equally to this work
 D. Darmanto1,2
D. Darmanto1,2 P. W. Anggoro
P. W. Anggoro R. Ismail
R. Ismail J. Jamari
J. Jamari A. P. Bayuseno
A. P. Bayuseno