
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Mater. , 12 May 2022
Sec. Biomaterials
Volume 9 - 2022 | https://doi.org/10.3389/fmats.2022.889889
This article is part of the Research Topic Recent Advancements in the Dental Biomaterials Applied in Various Diagnostic, Restorative, Regenerative and Therapeutic Procedures View all 13 articles
 Adel S. Alagl
Adel S. Alagl Marwa Madi*
Marwa Madi*Background: Immediate implant placement in the area of multirooted molars includes many anatomical challenges, particularly with osteotomy preparation in the interradicular bone.
Methods: In this article, we are reporting ten cases in which implant beds were prepared before root extraction. After coronectomy, pre-extractive interradicular implant bed preparations were performed through the retained root complexes. A dimple in the roof of the furcation was created using a no. 8 round surgical bur. The osteotomies were then completed through the tooth’s initially retained root complex in the regular sequence of drilling. Before implant placement, the remaining root segments were removed. The retained root parts guided the osteotomy drills and allowed for precise positioning and angulation of the implant bed preparation with respect to the emergence profile of the tooth.
Results: Data from a 3-year follow-up of the crestal bone showed good bone levels in relation to the implant platform.
Conclusion: The technique described permitted accurate implant placement in the prepared osteotomy, thus enabling immediate implant positioning in multirooted extraction sites.
Since the introduction of the immediate implant placement technique, placing implants in fresh extraction sockets became an acceptable procedure for more than two decades (Barone et al., 2015). Frequently, immediate implants are used for single-rooted teeth. In the case of immediate molar placement into molar sites, there are challenges involving site anatomy, occlusion, and biomechanical issues (Schropp and Isidor, 2008).
Immediate implants offer several advantages compared to the more conventional placement technique that requires 4 months following tooth extraction before implant installment (Bhola et al., 2008). Thus, significant reduction of the surgical phase coupled with a much shorter overall treatment time is achieved (Bhola et al., 2008). Today, immediate implants achieve long-term survival rates comparable to those of delayed implants placed in healed sites with a two-stage surgical approach (Quirynen et al., 2007; Becker and Goldstein, 2008; Schropp and Isidor, 2008; Chen and Buser, 2009). These favorable outcomes are not only important for single-tooth replacement in the esthetic zone but also for implant placement in the molar regions (Atieh et al., 2010).
With respect to maxillary and mandibular molar regions, immediate implant placement entails a series of clinical challenges related to site-specific anatomical aspects, such as comparatively larger socket than implant size, root length, height of the root trunk, and divergence of roots (Valenzuela et al., 2018).
It is essential to evaluate the anatomy of each patient’s posterior mandible, including the variability in the position of the inferior alveolar canal and the submandibular fossa. This step is critical because of the potential high risk for inferior alveolar nerve injury and lingual plate perforation when attempting to achieve primary implant stability using native bone apical to the extraction socket (Greenstein and Tarnow, 2006).
In molar extraction sockets, achieving initial implant stability can be challenging due to the width of the alveolar socket, poor bone quality, and critical anatomical structures beyond the apices of molar roots, such as the inferior alveolar nerve. Consequently, consideration should be given to placing implants within the mandibular molar extraction socket itself (Cafiero et al., 2008).
The protocol of immediate implant placement offers several advantages, including a reduction in the number of the surgical procedures, favorable esthetics, preservation of bone height and width, improved quality of life, and increased patient comfort and satisfaction (Chen et al., 2004).
Placing implants in an ideal prosthetic position without compromising their primary stability remains a key goal. Thus, directing the initial osteotomy into the interradicular bone would be preferred. However, there are circumstances in which the drill may slip, resulting in implant placement within the confines of the residual extraction socket (Scarano, 2017). In this study, we present ten cases with three-year follow-up in which interradicular implant bed preparation was performed before root extraction; thus, the osteotomy drills would be stabilized and guided by the retained root aspects.
The study population consisted of ten patients, eight females and two males, all of whom were non-smokers, and none reported any history of any systemic diseases or conditions that would preclude surgical implant placement and subsequent restoration. The patients’ age ranged from 39 to 66 years.
All patients, after receiving a full description of the surgical procedure, signed informed consent in full accordance with the guidelines of the Helsinki World Medical Association Declaration and the revision of the 2013 Good Clinical Practice Guides, and ethical approval was obtained (IRB-2021-02-208).
Each patient had at least one molar tooth diagnosed as hopeless due to restorability or failed endodontic treatment (seven mandibular first molars, two mandibular second molars, and one maxillary first molar). These teeth were treatment-planned for extraction and immediate implant placement (Figure 2A, Figure 3A, Figure 4A,D). A Schematic presentation of the procedure is illustrated in Figure 1.
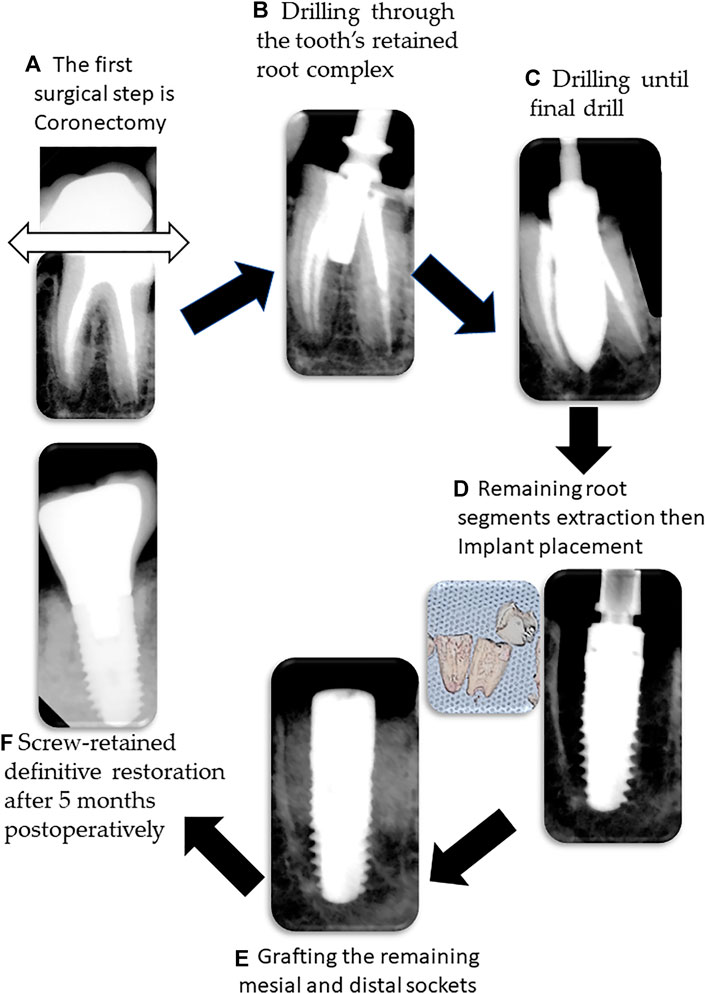
FIGURE 1. Illustration of the surgical procedure steps. (A) Initial surgical is coronectomy using a high speed tapered diamond bur coronectomy; (B) after forming a dimple in the roof of the furcation, drilling through the tooth’s retained root complex is performed; (C) final drilling is performed; (D) root separation is carried out and then the remaining root segments are extracted followed by implant placement; (E) bone graft is placed in the mesial and distal sockets; (F) after 5 months postoperatively, screw-retained definitive restoration is delivered.
All procedures were performed under local anesthesia using lidocaine 2% 1:100,000 epinephrine. Mucoperiosteal flap was made with minimal soft tissue reflection, and coronectomy was accomplished using a high-speed tapered diamond bur (Figures 1A and Figure 2B). Pre-extractive interradicular implant bed preparation was performed prior to root separation. A dimple in the roof of the furcation was created with a no. 8 round surgical bur to prevent skidding of the initial surgical drill (Figure 2C).
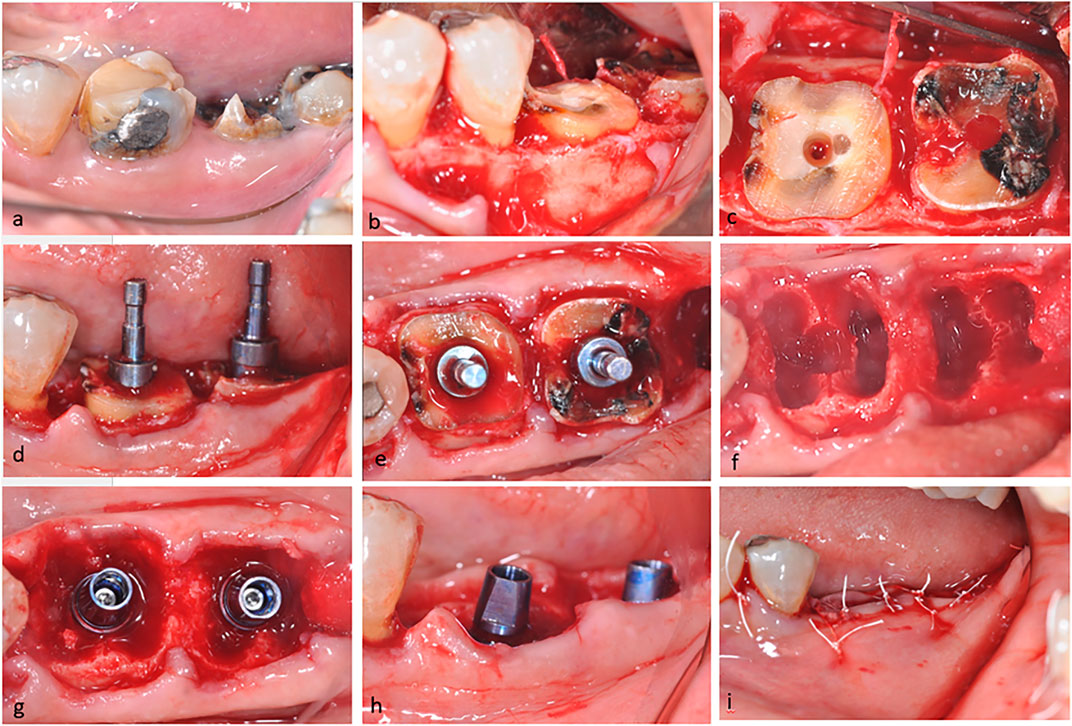
FIGURE 2. Clinical photographs of the steps in this surgical procedure. (A) Preoperative lateral view of the mandibular left first and second molars, which were unrestorable; (B) clinical view showing flap reflection and coronectomy; (C) occlusal view showing the dimple created with a #8 round bur; (D,E) lateral and occlusal views showing parallel pins; (F) occlusal view showing the final osteotomy in each molar tooth; (G,H) occlusal and lateral views showing implant placement in the pre-extractive drill; and (I) immediate postoperative lateral view of surgical sites with primary soft tissue closure.
The osteotomies were performed directly through each tooth’s retained root complex in the regular sequence of drilling starting with a point drill and finishing with the final drill before the roots were extracted and the implant was placed (Figures 1B,C).
The retained root components guided the osteotomy drills and aided precise positioning and angulation of the implant bed preparation with respect to the emergence profile of the tooth. The drilling depth was extended beyond the fundus of the socket in compliance with the preoperative radiographic assessment. After completion of the drilling protocol, according to the manufacturer’s instructions, the remaining root segments were separated. After root separation, periotomes were used to cut the periodontal ligament attachments to permit atraumatic extraction with the remaining root parts delicately removed using curved elevators (Figures 2D–H and Figure 3C–E).
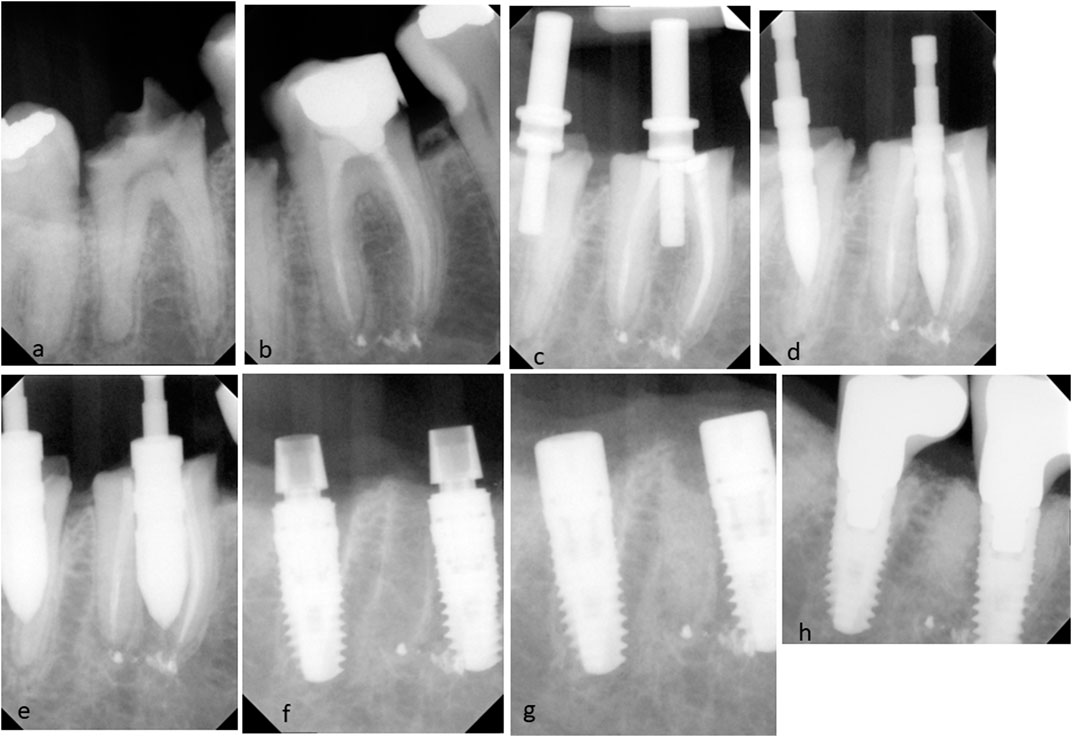
FIGURE 3. Radiographic images of the surgical procedure. (A,B) Preoperative radiographs of mandibular left first and second molars; (C) pre-extractive interradicular implant bed preparation. The parallel pins inserted in the initial osteotomy directly through each molar’s initially retained root complex of the left first and second molars; (D,E) other osteotomy drills drilled directly through the root complex; (F) insertion of cylindrical screw-type implants after removal of the remaining roots; (G) healing abutments were placed and bone graft material filled the extraction socket around each implant; and (H) a periapical radiograph taken 6 months after placement of the definitive restorations.
For all cases, proper debridement of each socket was performed using a bone curette and saline irrigation. Screw-type dental implants D 4.5x L11 mm (Xive S Plus, Dentsply Sirona, United States, Figure 1D) were inserted in the interradicular bone, and the implant shoulder of each implant was positioned at 1–2 mm apical to facial/buccal CEJ of adjacent teeth (Figures 2H and Figure 3F).
All 10 implants exhibited primary implant stability and were inserted under 35 NW torque. The gap around the implant and the mesial and distal sockets were completely packed with xenograft bone particles (Figure 1E) (NuOss cancellous bovine bone, 0.25–1 mm, ACE Surgical Supply Co., Massachusetts, United States) After inserting the bone graft material, the extraction socket was covered with a resorbable collagen membrane (BioMend Membrane, Zimmer Biomet, Indiana, United States). The collagen membrane was stabilized, and each extraction socket was covered using horizontal mattress sutures using 3-0 Cytoplast™ non-absorbable PTFE sutures (Osteogenics, Lubbock, Texas, United States) (Figure 1I). Periapical radiographs were taken during the implant bed preparation and again immediately postoperative after completion of the surgical treatment (Figure 3).
Healing was uneventful, and rinses were prescribed twice daily with 0.12% chlorhexidine digluconate (PerioAid®, Dentaid, Barcelona, Spain) for 2 weeks along with ibuprofen 600 mg (Abbott Laboratories, United States) to manage any postoperative inflammation and discomfort or pain. Postsurgical instructions and oral hygiene measures were explained to the patients. Sutures were removed 2 weeks after surgery.
Three months after implant placement, all patients were presented with healthy peri-implant tissues. A periapical radiograph was taken, and a second-stage surgery was performed by placing the healing abutment. The prosthetic treatment was initiated with provisional crown placement followed by placement of a screw-retained definitive restoration (Figure 1F). Annual radiographs were taken to evaluate the crestal bone level for each patient (Figure 4).
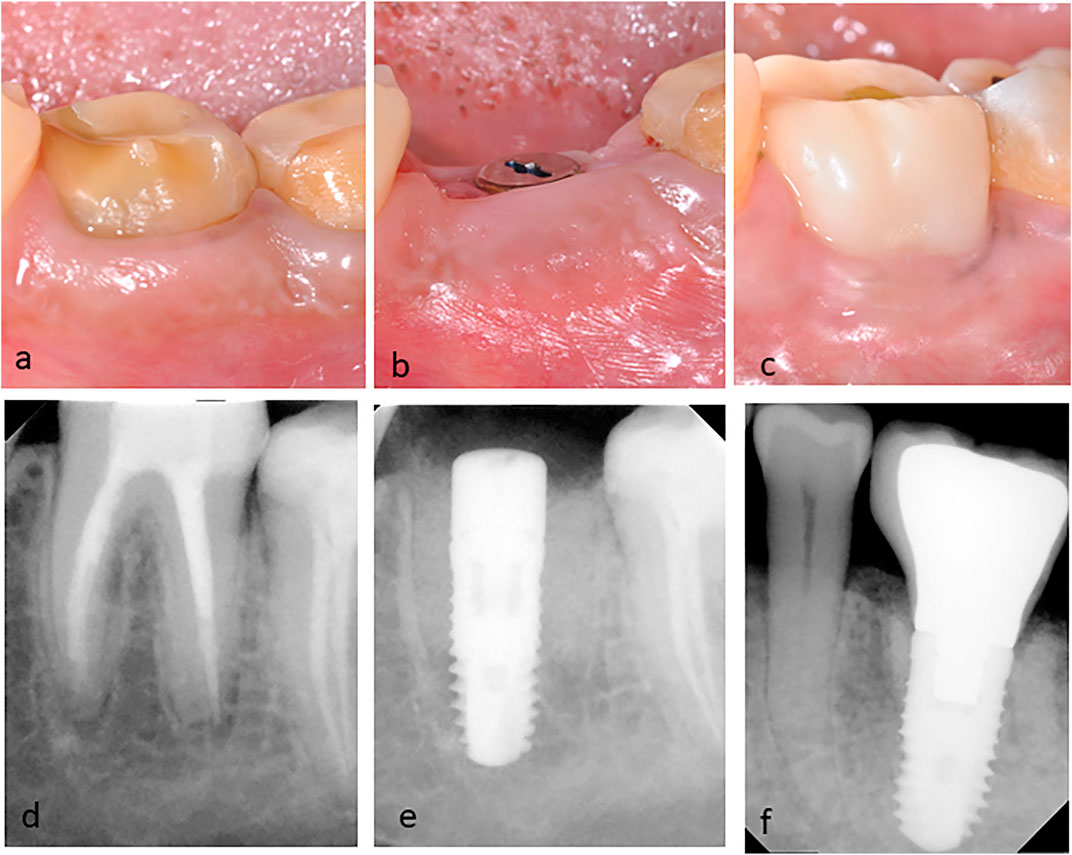
FIGURE 4. Clinical and radiographic images of the mandibular left first molar with failed endodontic treatment. (A) Preoperative clinical lateral view; (B) postoperative clinical lateral views after 3 months of implant placement; (C) clinical picture of definitive porcelain fused to the metal screw-retained implant crown at three-year follow-up; (D) Preoperative periapical radiograph; (E) periapical radiographs of the implant after 3 months; and (F) radiographic image at three-year follow-up showing the marginal bone level.
Healing was uneventful for all 10 patients with no complication during the follow-up period, thus giving a cumulative survival rate of 100% during the three-year follow-up period of this study. The change in the marginal bone level was 0.11 ± 0.08 mm in all patients at the 3-year examination.
ImageJ software version 1.47 (Wayne Rasband, National Institutes of Health, United States) was used to measure the crestal bone loss on both the mesial and distal aspects of the implants. To set the scale for the measurements, the known implant width was used to calibrate the measurements. Then, a straight line was delineated from the implant platform to the alveolar crest on the mesial as well as the distal side. The average of both mesial and distal measurements was used to represent the bone level of each implant. (Figure 4F).
This study describes an alternative method of preparing osteotomy for immediate implant placement of multirooted molars. Drilling was performed prior to root separation, followed by root extraction and finally implant placement. Using this technique, surgeons are expected to receive better guidance during implant preparation. The osteotomy drills were stabilized and guided by the retained roots.
This form of osteotomy preparation can be less complicated and a useful modification of the standard surgical procedure to achieve more ideal implant positioning during immediate implant placement for a multirooted molar.
Immediate implant placement has become more popular among dentists providing implant dentistry treatment. However, still, primary implant stability and lack of micromovements are the two main factors necessary for achieving predictable high success of osseointegration (Albrektsson et al., 1981). Some advocate that the use of some specific implant surface treatment is able to reduce the healing time (Roccuzzo et al., 2001).
Optimal implant placement is more likely to be achieved using various technical approaches, such as radiographic templates or cone-beam computed tomography (CBCT) along with computer-assisted three-dimensional implant planning software programs.
In this study, sulcular incision was made around the mandibular molar to be extracted, and periosteal-releasing incisions were used for better flap adaptation following implant placement (Hamouda et al., 2015).
It is crucial to cover the surgical site and the peri-implant gap after immediate implant placement in order to achieve a successful grafting consolidation around the implant. Several recommendations have been published in the literature for the management of socket seals including the use of non-resorbable polytetrafluoroethylene (PTFE) membranes and resorbable collagen membranes for immediate implant placement (Hoffmann et al., 2008; Matarasso et al., 2009).
Hoffmann et al. (2008) used the non-resorbable polytetrafluoroethylene (PTFE) membranes to cover the socket with a significant regeneration of the volume of the socket, but the potential complications include exposure and dehiscence.
Urban et al. (2012) used the Ossix® cross-linked collagen membrane (Dentsply Sirona, York, Pennsylvania, United States), which is a resorbable collagen membrane, however, chemically treated in order to prolong the period without resorption. The current implant survival rate was 100% with no failures observed during the three-year follow-up period, which was greater than the 95% survival rate reported by Hamouda et al. (2015).
In this study, drilling was initiated through the root trunk, after coronectomy and before root separation. Rebele et al. (2013) suggested using a sharp new drill to drill through the dentin and cementum at the furcation region. They also suggested that drilling through the dentin and retained root aspects appeared to be similar to drilling through tissues; however, it is slightly harder than dense cortical bone (Rebele et al., 2013).
In contrast, Hamouda et al. (2015), Scarano (2017), and Smith and Tarnow (2013) recommended drilling after root separation in order to make the drilling process easier as well as preventing dulling of the surgical drills.
In this study, immediate implant placement was achieved using a new pre-extraction implant bed preparation technique in ten patients. Prior to root separation, implants’ osteotomies were prepared, then roots were separated, and implants were inserted. This allows for accurate implant placement in the drilled osteotomy, and also the remaining root segments would be partially luxated during the osteotomy drilling process.
The previous study (Valenzuela et al., 2018) mentioned that this alternative drilling method might result in a deficient implant insertion since it would modify the socket wall’s morphology during the extraction procedure. Therefore, careful extraction using desmotomes or ultrasonic appliances should be conducted.
In order to avoid destroying the prepared implant bed and affecting the initial implant stability during the extraction operation, in this study, after osteotomy preparation, root separation was performed. Then, periotomes were used to sever the periodontal ligament surrounding the remaining roots. This eliminates the negative pressure present around the remaining roots as well as facilitates deeper insertion of the desmotomes and elevators to elevate the roots. Thus, atraumatic extraction operation was carried out to avoid altering the prepared implant bed.
This alternative drilling protocol will modify the socket wall’s morphology during the extraction procedure, leading to a deficient implant insertion. Therefore, careful extraction using desmotomes or ultrasonic appliances is advised.
Similar to previous studies, Rebele et al. (2013), and Scarano (2017) recommended placing the implant after root extraction to minimize the complications encountered with extracting the remaining root segments.
In order to achieve initial implant stability, the implant should be placed in native apical and/or lateral bone to the extraction socket. Based on the anatomy of the tooth, the morphology of the extraction socket is determined. Accordingly, the tooth anatomy will have an influence on implant stability in the socket. Various parameters should be considered, including the width of the root at the cementoenamel junction (CEJ), the length of the root, the degree of root divergence, and any anatomical limitations beyond the apices of the molar roots, such as the inferior alveolar nerve.
In this technique, the osteotomy was planned to engage the interradicular bone of the socket (type A and type B sockets) (Smith and Tarnow, 2013). Therefore, the presence of a sufficient amount of septal bone that adequately supports circumferentially the implant facilitates achieving primary stability.
There is much debate in the literature as to the appropriate implant design to be used for immediate implantation in the mandibular molar region. Rebele et al. (2013) and Scarano (2017) used a cylindrical implant design, while Hamouda et al. (2015) and Rohra et al. (2017) preferred implants with a tapered design. In this study, the cylindrical body with a tapered end implant similar to that of Urban et al. (2012) was used. We observed a 100% implant success rate after 3 years as well as minimal marginal bone changes.
In the literature, there have been diverse approaches to combining immediate implant placement with regenerative procedures despite reports that regenerative treatments are not essential to achieve more successful healing or osseointegration for immediate implant (Botticelli et al., 2004; Lang et al., 2012).
Several grafting materials have been suggested in order to fill the mesial and distal bony sockets around immediate implants. Hayacibara et al. (2013), Tallarico et al. (2016), Scarano (2017) used bovine xenograft particles that showed marginal bone loss of approximately 1 mm compared to nongrafted implant sockets. According to Araújo et al. (2011,) the placement of deproteinized bovine bone mineral in a model of fresh extraction sockets enhanced hard tissue formation and improved marginal bone height.
Similar to the current study, a natural bovine porous bone mineral matrix was used with a 100% survival rate and no marginal bone loss after a three-year follow-up. The natural structure of this bone substitute is physically and chemically comparable to the mineralized matrix of human bone. The results of this study support the hypothesis that a low-resorption particulate graft should be used to the gap surrounding peri-implant in case of immediate implant placement to retain the surrounding bony walls and reduce the risk of marginal bone loss.
Immediate implant placement in the molar extraction site using the described technique would be indicated in extraction sites with sufficient root divergence in which primary stability can be achieved. Contraindications are tooth mobility, due to severed bone, presence of advanced furcation involvement, and unfavorable root position, such as fused roots and ankylosed roots (Tizcareño and Bravo-Flores, 2009; Rebele et al., 2013).
The strength of this technique is to provide guidance for the surgeon during immediate implant placement by using the tooth structure as a stent or guide. This technique may raise concerns regarding the possibility of a deleterious reaction caused by drill debris that has become lodged in the socket or within an osteotomy. Accordingly, it is highly recommended that the site be thoroughly curetted prior to implant insertion. The limitation of this study is that it is a multiple case series of one technique, so a comparative study or clinical trial study would be recommended to further investigate the advantages of this technique. Also, more clinical parameters could be assessed in future studies.
The use of a modified pre-extractive interradicular implant bed preparation technique resulted in adequate primary implant stability and optimum implant location. After 3 years, implants placed using the pre-extraction interradicular implant bed preparation demonstrated a 100% success rate and less than 1 mm marginal bone loss (Hayacibara et al., 2013).
The raw data supporting the conclusions of this article will be made available by the authors upon request.
The studies involving human participants were reviewed and approved by the Institutional Review Board of IAU (IRB-2021-02-208). The patients/participants provided their written informed consent to participate in this study.
AA and MM: study concepts and study design. AA and MM: investigation, manuscript preparation, manuscript review, and manuscript editing. All authors approved the final manuscript for submission.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Authors would like to acknowledge the assistance of W. Patrick Naylor, DDS, MPH, MS, for revising the manuscript and Rahaf Fahad Al Ghamdi for assisting in photography.
Albrektsson, T., Brånemark, P.-I., Hansson, H.-A., and Lindström, J. (1981). Osseointegrated Titanium Implants:Requirements for Ensuring a Long-Lasting, Direct Bone-To-Implant Anchorage in Man. Acta Orthopaedica Scand. 52 (2), 155–170. doi:10.3109/17453678108991776
Araújo, M. G., Linder, E., and Lindhe, J. (2011). Bio-Oss Collagen in the Buccal gap at Immediate Implants: A 6-month Study in the Dog. Clin. Oral Implants Res. 22, 1–8. doi:10.1111/j.1600-0501.2010.01920.x
Atieh, M. A., Payne, A. G., Duncan, W. J., de Silva, R. K., and Cullinan, M. P. (2010). Immediate Placement or Immediate Restoration/loading of Single Implants for Molar Tooth Replacement: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implants 25, 401–415.
Barone, A., Toti, P., Quaranta, A., Derchi, G., and Covani, U. (2015). The Clinical Outcomes of Immediate versus Delayed Restoration Procedures on Immediate Implants: A Comparative Cohort Study for Single-Tooth Replacement. Clin. Implant Dent Relat. Res. 17, 1114–1126. doi:10.1111/cid.12225
Becker, W., and Goldstein, M. (2008). Immediate Implant Placement: Treatment Planning and Surgical Steps for Successful Outcome. Periodontol. 2000 47, 79–89. doi:10.1111/j.1600-0757.2007.00242.x
Bhola, M., Neely, A. L., and Kolhatkar, S. (2008). Immediate Implant Placement: Clinical Decisions, Advantages, and Disadvantages. J. Prosthodont. 17 (7), 576–581. doi:10.1111/j.1532-849x.2008.00359.x
Botticelli, D., Berglundh, T., and Lindhe, J. (2004). Hard-tissue Alterations Following Immediate Implant Placement in Extraction Sites. J. Clin. Periodontol. 31, 820–828. doi:10.1111/j.1600-051x.2004.00565.x
Cafiero, C., Annibali, S., Gherlone, E., Grassi, F. R., Gualini, F., Magliano, A., et al. (2008). Immediate Transmucosal Implant Placement in Molar Extraction Sites: A 12-month Prospective Multicenter Cohort Study. Clin. Oral Implants Res. 19 (5), 476–482. doi:10.1111/j.1600-0501.2008.01541.x
Chen, S. T., and Buser, D. (2009). Clinical and Esthetic Outcomes of Implants Placed in Postextraction Sites. Int. J. Oral Maxillofac. Implants 24, 186–217.
Chen, S. T., Wilson, T. G., and Hämmerle, C. H. (2004). Immediate or Early Placement of Implants Following Tooth Extraction: Review of Biologic Basis, Clinical Procedures, and Outcomes. Int. J. Oral Maxillofac. Implants 19, 12–25.
Greenstein, G., and Tarnow, D. (2006). The Mental Foramen and Nerve: Clinical and Anatomical Factors Related to Dental Implant Placement: A Literature Review. J. Periodontol. 77 (12), 1933–1943. doi:10.1902/jop.2006.060197
Hamouda, N. I., Mourad, S. I., El-Kenawy, M. H., and Maria, O. M. (2015). Immediate Implant Placement into Fresh Extraction Socket in the Mandibular Molar Sites: A Preliminary Study of a Modified Insertion Technique. Clin. Implant Dentistry Relat. Res. 17, e107–e116. doi:10.1111/cid.12135
Hayacibara, R. M., Gonçalves, C. S., Garcez-Filho, J., Magro-Filho, O., Esper, H., and Hayacibara, M. F. (2013). The success Rate of Immediate Implant Placement of Mandibular Molars: A Clinical and Radiographic Retrospective Evaluation between 2 and 8 Years. Clin. Oral Impl. Res. 24 (7), 806–811. doi:10.1111/j.1600-0501.2012.02461.x
Hoffmann, O., Bartee, B. K., Beaumont, C., Kasaj, A., Deli, G., and Zafiropoulos, G.-G. (2008). Alveolar Bone Preservation in Extraction Sockets Using Non-resorbable dPTFE Membranes: A Retrospective Non-randomized Study. J. Periodontol. 79 (8), 1355–1369. doi:10.1902/jop.2008.070502
Lang, N. P., Pun, L., Lau, K. Y., Li, K. Y., and Wong, M. C. (2012). A Systematic Review on Survival and success Rates of Implants Placed Immediately into Fresh Extraction Sockets after at Least 1 Year. Clin. Oral Implants Res. 23 (5), 39–66. doi:10.1111/j.1600-0501.2011.02372.x
Matarasso, S., Salvi, G. E., Siciliano, V. I., Cafiero, C., Blasi, A., and Lang, N. P. (2009). Dimensional ridge Alterations Following Immediate Implant Placement in Molar Extraction Sites: A Six-Month Prospective Cohort Study with Surgical Re-entry. Clin. Oral Implants Res. 20 (10), 1092–1098. doi:10.1111/j.1600-0501.2009.01803.x
Quirynen, M., Van Assche, N., Botticelli, D., and Berglundh, T. (2007). How Does the Timing of Implant Placement to Extraction Affect Outcome? Int. J. Oral Maxillofac. Implants 22, 203–223.
Rebele, S. F., Zuhr, O., and Hürzeler, M. B. (2013). Pre-extractive Interradicular Implant Bed Preparation: Case Presentations of a Novel Approach to Immediate Implant Placement at Multirooted Molar Sites. Int. J. Periodontics Restorative Dent 33 (1), 88–95. doi:10.11607/prd.1444
Roccuzzo, M., Bunino, M., Prioglio, F., and Bianchi, S. D. (2001). Early Loading of Sandblasted and Acid-Etched (SLA) Implants: A Prospective Split-Mouth Comparative Study. Clin. Oral Implants Res. 12 (6), 572–578. doi:10.1034/j.1600-0501.2001.120604.x
Rohra, D. E., Mistry, D. G., Joshi, D. T., and Khanvilkar, D. U. (2017). Implant Bed Preparation for Immediate Implantation in Molar Region: An Alternative Approach. Iosr Jdms 16 (05), 48–50. doi:10.9790/0853-1605064850
Scarano, A. (2017). Traditional Postextractive Implant Site Preparation Compared with Pre-extractive Interradicular Implant Bed Preparation in the Mandibular Molar Region, Using an Ultrasonic Device: A Randomized Pilot Study. Int. J. Oral Maxillofac. Implants 32 (3), 655–660. doi:10.11607/jomi.5342
Schropp, L., and Isidor, F. (2008). Timing of Implant Placement Relative to Tooth Extraction. J. Oral Rehabil. 35, 33–43. doi:10.1111/j.1365-2842.2007.01827.x
Smith, R. B., and Tarnow, D. P. (2013). Classification of Molar Extraction Sites for Immediate Dental Implant Placement: Technical Note. Int. J. Oral Maxillofac. Implants 28 (3), 911–916. doi:10.11607/jomi.2627
Tallarico, M., Xhanari, E., Pisano, M., De Riu, G., Tullio, A., and Meloni, S. M. (2016). Single post-extractive Ultra-wide 7 mm-Diameter Implants versus Implants Placed in Molar Healed Sites after Socket Preservation for Molar Replacement: 6-month post-loading Results from A randomised Controlled Trial. Eur. J. Oral Implantol. 9 (3), 263–275.
Tizcareño, M. H., and Bravo-Flores, C. (2009). Anatomically Guided Implant Site Preparation Technique at Molar Sites. Implant Dentistry 18 (5), 393–401. doi:10.1097/ID.0b013e3181b4b205
Urban, T., Kostopoulos, L., and Wenzel, A. (2012). Immediate Implant Placement in Molar Regions: A 12-month Prospective, Randomized Follow-Up Study. Clin. Oral Impl. Res. 23 (12), 1389–1397. doi:10.1111/j.1600-0501.2011.02319.x
Keywords: pre-extractive drilling, immediate implant, interradicular implant bed, clinical case, interradicular osteotomy
Citation: Alagl AS and Madi M (2022) Case Report: Combining Molar Interradicular Osteotomy With Immediate Implant Placement: A Three-Year Case-Series Study. Front. Mater. 9:889889. doi: 10.3389/fmats.2022.889889
Received: 04 March 2022; Accepted: 11 April 2022;
Published: 12 May 2022.
Edited by:
Mohammad Khursheed Alam, Al Jouf University, Saudi ArabiaReviewed by:
Daniel Fernando Torassa, National University of Cordoba, ArgentinaCopyright © 2022 Alagl and Madi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marwa Madi, bWltYWRpQGlhdS5lZHUuc2E=
†ORCID: Adel Alagl, orcid.org/0000-0001-6274-7677; Marwa Madi, orcid.org/0000-0002-3014-0405
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.