- Department of Orthopaedic Surgery, Honghui Hospital, Xi’an Jiaotong University, Xi’an, China
Background: Although open reduction internal fixation (ORIF) with periarticular locking plates, retrograde intramedullary nail (IMN) fixation, and distal femoral replacement (DFR) have been widely used for the treatment of periprosthetic distal femur fractures (PPDFF), it remains unclear which one may be an optimal surgical strategy.
Objective: This network meta-analysis aimed to determine the optimal surgical strategy for PPDFF from ORIF, IMN, and DFR by evaluating major complication rates and revision rates.
Patients and Methods: We identified eligible studies by performing an updated literature search in PubMed, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) and checking published meta-analyses. The methodological index for non-randomized studies (MINORS) was used to assess the methodological quality of eligible studies. Major complications and revision rates were defined as outcomes of interest. All statistical analyses were performed by ADDIS 1.4 software.
Results: We included 17 eligible studies in the final analysis. Statistical analyses did not reveal significant differences when ORIF was compared with IMN and ORIF compared with DFR, and IMN compared with DFR in terms of two clinical outcomes. However, DFR achieved a beneficial trend in major complications [odds ratio (OR) = 1.34; 95% CrI = 0.48–3.80] and revision (OR = 1.64; 95% CrI = 0.68–4.38) rates compared with IMN. Ranking probabilities indicate that DFR has the highest probability of being the optimal option, followed by ORIF and IMN.
Conclusion: There was no difference in major complications or reoperations between the three treatments. However, ORIF with periarticular locking plates may be a preferred alternative option because DFR is limited by the high cost. Moreover, our study highlights the need for future prospective trials evaluating the outcomes of these three surgical strategies.
Introduction
As the prevalence of total knee arthroplasty (TKA) increases among the aging population, periprosthetic distal femur fracture (PPDFF) is becoming increasingly common with an incidence ranging from 0.3–2.5% (Agarwal et al., 2014; Konan et al., 2016). Meanwhile, the literature also reported a higher incidence of revision arthroplasties, ranging from 1.6% to 38.0% (Gracia-Ochoa et al., 2016). Studies revealed that the 1-year mortality of this injury has been increasing up to 15%, and the overall incidence of postoperative complications was as high as 37% (Ebraheim et al., 2014; Myers et al., 2018). More importantly, the morbidity rate of PPDFF is as high as 25% in the geriatric population (Lotzien et al., 2019).
Therapeutic strategies for PPDFF include nonoperative and surgical management; however, previous studies have reported poor outcomes in patients treated with nonoperative management (Darrith et al., 2020). In contrast, surgical management was identified as the preferred therapeutic option (Su et al., 2004; Kinney and Engh, 2018). Although several surgical approaches have been widely used for treating PPDFF (Darrith et al., 2020), advancements in implant technology have greatly increased the focus on three primary surgical strategies, including open reduction internal fixation (ORIF) with periarticular locking plates, or intramedullary nail fixation (IMN), and distal femoral replacement (DFR) (Quinzi et al., 2021). Currently, several pairwise meta-analyses (Ebraheim et al., 2015; Shin et al., 2017; Liu et al., 2019; Shah et al., 2020) have compared the clinical efficacy and safety of these three surgical strategies; however, a definitive conclusion about which one should be preferentially selected for the treatment of PPDFF remains unclear.
It is noted that the most recent systematic review and meta-analysis (Quinzi et al., 2021) separately investigated the comparative efficacy and safety of ORIF, IMN, and DFR in patients with PPDFF. Unfortunately, the preferred therapeutic option was still not determined due to the shortage of pair-wise meta-analysis (Lu and Ades, 2004). Additionally, all previously published meta-analyses did not include all eligible studies in the final analysis, and additional studies have also been published recently. Therefore, we conducted this network meta-analysis to determine the optimal surgical strategy by providing an up-to-date synthesis of the early complication rates and revision rates of three options including ORIF with periarticular locking plates, retrograde IMN, and DFR for PPDFF.
Methods
Study Design
The current network meta-analysis was performed following the Cochrane handbook for reviewers of systematic reviews (Higgins and Green, 2011), and the pooled results were reported according to the preferred reporting items for systematic reviews and meta-analysis (PRISMA) for network meta-analysis (PRISMA-NMA) (Hutton et al., 2015; Page et al., 2021). This network meta-analysis was exempted from ethical approval and informed consent because it was undertaken with previously published data.
Eligibility Criteria
We defined inclusion criteria following previous meta-analyses (Shah et al., 2020; Quinzi et al., 2021; Wadhwa et al., 2021): 1) patients were confirmed with PPDFF based on recognized criteria, 2) comparison of at least two of ORIF with periarticular locked plates, retrograde IMN, and DFR was available, 3) reported at least one of the data on major complications and revision rate, 4) randomized controlled trials (RCTs), or retrospective or prospective study designs, and 5) full text published in English.
The following exclusion criteria were also defined: 1) adequate sample size (<5 patients), 2) did not report outcomes of interest, 3) duplicate studies with inadequate information or poor methodological quality, and 4) animal study, review, correspondence, letter to the editor, and conference abstract.
Information Sources
We obtained six meta-analyses (Ebraheim et al., 2015; Shin et al., 2017; Liu et al., 2019; Shah et al., 2020; Quinzi et al., 2021; Wadhwa et al., 2021) through searching PubMed by two reviewers using periprosthetic distal femoral fracture and synonyms, and two (Quinzi et al., 2021; Wadhwa et al., 2021) out of the six meta-analyses published in 2021. Then we conducted an updated literature search in PubMed, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) from January 2020 until July 2021 in order to identify additional potential studies. We also manually checked references of all published meta-analyses and included studies to identify additional studies. Details of the literature search strategies are documented in Supplementary Table S1. A third senior reviewer was invited to solve any disagreements during the literature retrieval.
Study Selection
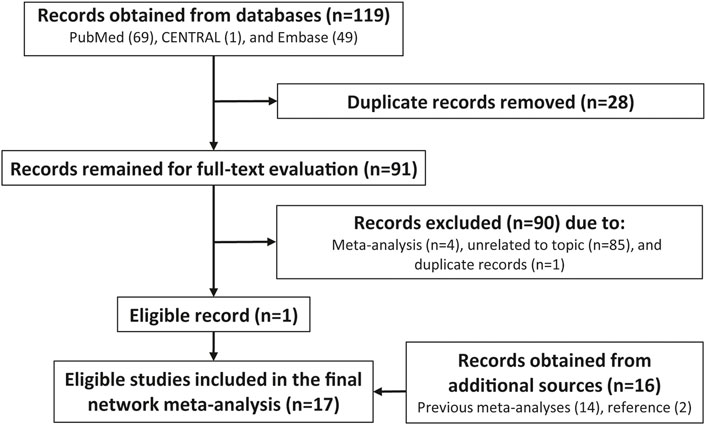
Two independent reviewers conducted the study selection. First, all identified potentially eligible records were imported into EndNote for literature database development. Second, all duplicate records were labeled and then removed into the trash file. Third, ineligible records were removed after screening titles and abstracts for eligibility. Fourth, full-text was checked for evaluating eligibility. Fifth, full-texts of all studies included in previous meta-analyses were downloaded and then verified for eligibility. A third senior reviewer was invited to solve any disagreements. The details of identifying and selecting eligible studies are displayed in Figure 1.
Outcomes of Interest
In this network meta-analysis, we evaluated two outcomes including major complication rates over the follow-up period and all-cause revision rates. Major complication rates were defined as the incidence of deep infection, nonunion, symptomatic malunion, hardware failure, aseptic loosening of arthroplasty, periprosthetic fracture, and extensor mechanism complications (Quinzi et al., 2021).
Data Extraction
Two independent reviewers utilized the standard data extraction sheet to extract the following information: basic characteristics of the study (the first author’s name, publication year, country of the first author, study design, comparison, and methodological information), essential characteristics of patients [sample size (%male), mean age (years), mean Charlson Comorbidity Index (CCI) score, mean American Society of Anesthesiologists (ASA) score, and mean time of follow-up], and outcomes. A third senior reviewer was asked to solve any disagreements.
Geometry of the Network
We used Stata 14.0 (Stata Corp LP, College Station, Texas, United States) to create an evidence structure of three surgical treatments on the basis of accumulated sample size and the number of eligible studies. The accumulated sample size was used to weigh the size of the circle representing treatment, and the accumulated numbers of eligible studies were used to weigh the width of the line representing the number of studies.
Methodological Quality Assessment
All included studies in this network meta-analysis were retrospective cohort or case series; we, therefore, utilized the non-randomized cohort studies using the methodological index for non-randomized studies (MINORS) (Slim et al., 2003) to assess the methodological quality of the evidence.
Statistical Analysis
We simultaneously performed direct and network meta-analysis, which was conducted with the aggregate data drug information system (ADDIS) software (Groningen, the Netherlands, www.drugis.org). For the direct meta-analysis, a random-effects model which considers the variations across studies in the real world was used. Estimates were reported in the odds ratio (OR) with a 95% confidence interval (CI) because two outcomes were categorical variables. Statistical heterogeneity was evaluated by using the chi-square test (Cochrane Q) (Bowden et al., 2011) and an I2 statistic (Higgins and Thompson, 2002). Substantial statistical heterogeneity was considered if the p-value was less than 0.1 and the I2 value was equal to or more than 50.0% (Higgins et al., 2003).
Network meta-analysis was performed using the Markov Chain Monte Carlo (MCMC) simulation which is graphically displayed in Supplementary Figure S1. Estimates were reported in OR with a 95% credible interval (CrI). For major complications rates, parameters including four chains, 20,000 tunings and 50,000 simulation iterations, the thinning interval of 10, 10,000 inference samples, and variance scaling factor of 2.5 (Cipriani et al., 2013) were defined to achieve a good convergence. However, for the revision rate, four chains, 20,000 tuning, and 100,000 simulation iterations, the thinning interval of 10, 20,000 inference samples, and variance scaling factor of 2.5 (Cipriani et al., 2013) were defined to achieve a good convergence. The convergence of data was evaluated using the Brooks Gelman-Rubin statistical method, and a good convergence was suggested when a potential proportional reduction factor (PRF) was close to 1 (Brooks and Gelman, 1998; Burger and Schall, 2015). Moreover, a PRF of 1.2 also indicated an acceptable convergence (Brooks and Gelman, 1998; Burger and Schall, 2015).
Inconsistency Test
In this network meta-analysis, a closed loop was available for three surgical treatments, and we, therefore, conducted the split node method to investigate whether the presence of inconsistency or not between direct and indirect effects (Dias et al., 2010; Albert and Makowski, 2019). This test was performed by using Stata 14.0 (Stata Corp LP, College Station, Texas, United States).
Ranking Probabilities
We estimated the ranking probabilities of being a certain rank for these three surgical treatments and utilized surface under the cumulative ranking curve (SUCRA) values to generate a ranking hierarchy of surgical treatments (Singh et al., 2015).
Publication Bias Test
We created the comparison-adjusted funnel plot to qualitatively examine the publication bias and small study effects because the accumulated number of eligible studies was more than 10 (Palma Perez and Delgado Rodriguez, 2006). The publication bias test was performed by using Stata 14.0 (Stata Corp LP, College Station, Texas, United States).
Results
Retrieval and Selection of Study
A total of 119 records were initially identified after conducting an updated search, and then 28 duplicate records were removed. A total of 90 ineligible studies were excluded after screening titles, abstracts, and full-texts for eligibility due to meta-analysis, unrelated to the topic, and duplicate records, so one study (Gausden et al., 2021) was considered to meet our selection criteria. Moreover, we obtained 16 eligible studies (Platzer et al., 2010; Hou et al., 2012; Aldrian et al., 2013; Horneff et al., 2013; Kiluçoğlu et al., 2013; Gondalia et al., 2014; Meneghini et al., 2014; Leino et al., 2015; Park and Lee, 2016; Matlovich et al., 2017; Ruder et al., 2017; Gan et al., 2018; Hoellwarth et al., 2018; Darrith et al., 2020; García Guirao et al., 2020; Jennison and Yarlagadda, 2020) from published meta-analyses and references. Finally, we included 17 studies (Platzer et al., 2010; Hou et al., 2012; Aldrian et al., 2013; Horneff et al., 2013; Kiluçoğlu et al., 2013; Gondalia et al., 2014; Meneghini et al., 2014; Leino et al., 2015; Park and Lee, 2016; Matlovich et al., 2017; Ruder et al., 2017; Gan et al., 2018; Hoellwarth et al., 2018; Darrith et al., 2020; García Guirao et al., 2020; Jennison and Yarlagadda, 2020; Gausden et al., 2021) in this network meta-analysis. Details of study retrieval and selection are shown in Figure 1.
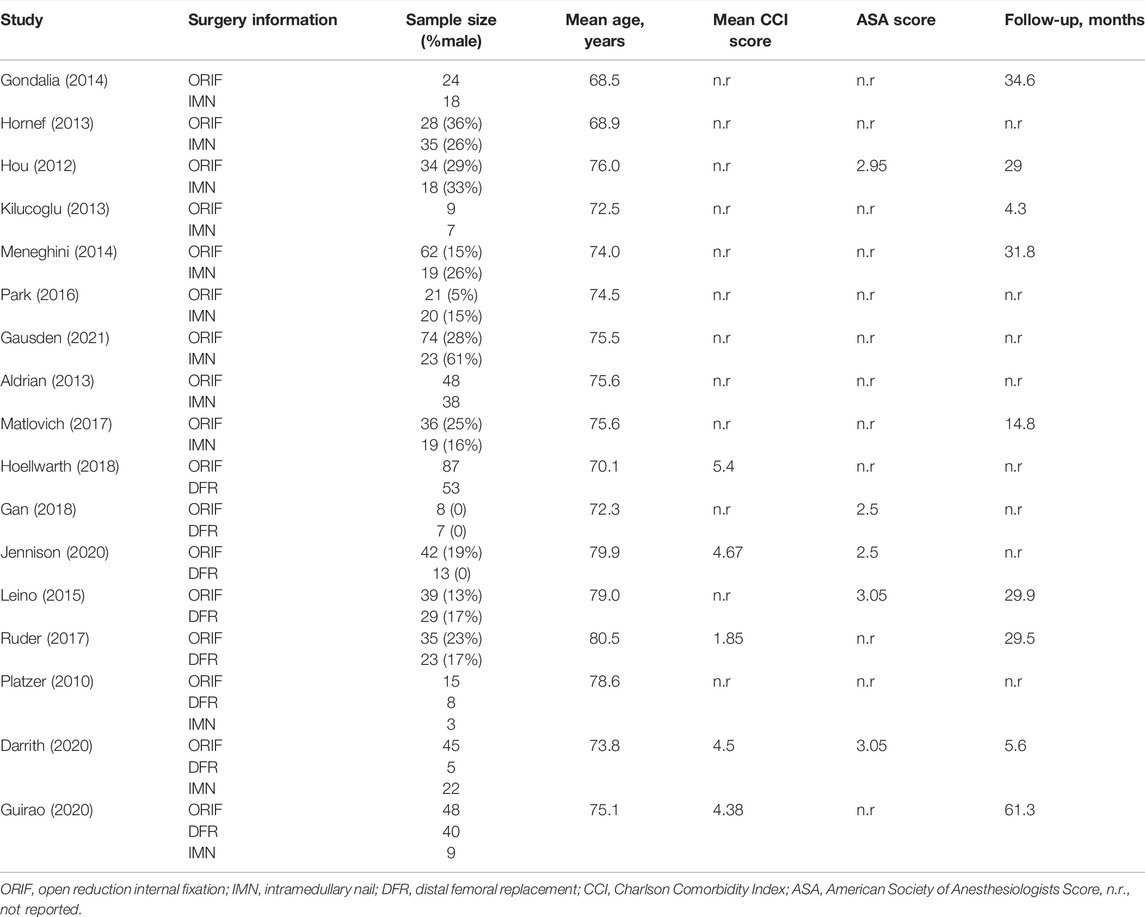
Basic Characteristics of Eligible Studies and Participants
A total of 14 retrospective cohort studies (Platzer et al., 2010; Hou et al., 2012; Horneff et al., 2013; Kiluçoğlu et al., 2013; Gondalia et al., 2014; Meneghini et al., 2014; Leino et al., 2015; Park and Lee, 2016; Matlovich et al., 2017; Ruder et al., 2017; Gan et al., 2018; Hoellwarth et al., 2018; Darrith et al., 2020; Gausden et al., 2021) and 3 case series (Aldrian et al., 2013; García Guirao et al., 2020; Jennison and Yarlagadda, 2020) were included. Three studies were 3-arm designs (Platzer et al., 2010; Darrith et al., 2020; García Guirao et al., 2020), and the remaining 14 studies were 2-arm designs (Hou et al., 2012; Aldrian et al., 2013; Horneff et al., 2013; Kiluçoğlu et al., 2013; Gondalia et al., 2014; Meneghini et al., 2014; Leino et al., 2015; Park and Lee, 2016; Matlovich et al., 2017; Ruder et al., 2017; Gan et al., 2018; Hoellwarth et al., 2018; Jennison and Yarlagadda, 2020; Gausden et al., 2021). The accumulated sample size was 655, 250, and 159 in ORIF, IMN, and DFR groups, respectively. Comparison of ORIF and IMN, ORIF, and DFR, as well as IMN and DFR was available in 12 (Platzer et al., 2010; Hou et al., 2012; Aldrian et al., 2013; Horneff et al., 2013; Kiluçoğlu et al., 2013; Gondalia et al., 2014; Meneghini et al., 2014; Park and Lee, 2016; Matlovich et al., 2017; Darrith et al., 2020; García Guirao et al., 2020; Gausden et al., 2021), 8 (Platzer et al., 2010; Leino et al., 2015; Ruder et al., 2017; Gan et al., 2018; Hoellwarth et al., 2018; Darrith et al., 2020; García Guirao et al., 2020; Jennison and Yarlagadda, 2020), and three studies (Platzer et al., 2010; Darrith et al., 2020; García Guirao et al., 2020), respectively. The evidence structure of the three surgical techniques is shown in Figure 2. The MINORS score of individual study ranged from 14 to 17, with a moderate level for overall methodological quality. The basic characteristics of included studies and patients are summarized in Tables 1, 2.
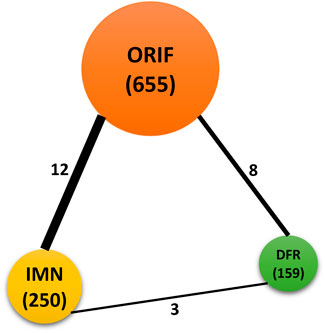
FIGURE 2. Evidence network of three surgical techniques including ORIF, IMN, and DFR. Circle size is positively corresponding to the accumulated sample size, and the width of the solid line is positively related to accumulated numbers of eligible studies.
Inconsistency Test
Node split generated an inconsistency factor (IF) of 1.01 with a p-value of 0.303 for the closed loop of major complications rates and an IF of 1.02 with a p-value of 0.264 for the closed loop of revision rates (Supplementary Figure S2), suggesting consistency between direct and indirect effects.
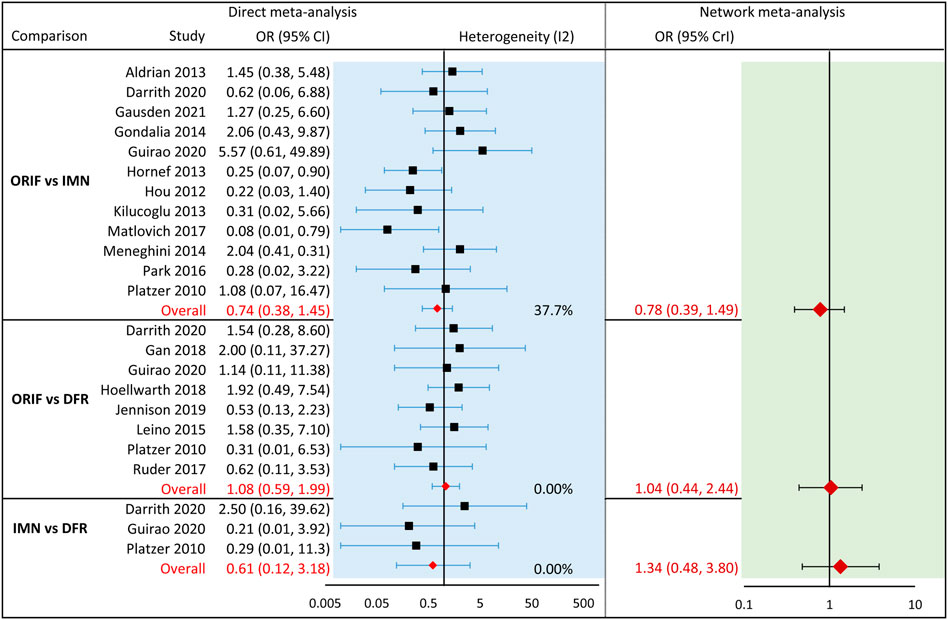
Meta-Analysis of Major Complication Rates
Direct meta-analyses did not reveal significant difference for comparison between ORIF and IMN (12 studies, OR = 0.74; 95% CI = 0.38 to 1.45; I2 = 37.7%), comparison between ORIF and DFR (eight studies, OR = 1.08; 95% CI = 0.59 to 1.99; I2 = 0.00%), and comparison between INM and DFR (three studies, OR = 0.61, 95% CI = 0.12 to 3.18, I2 = 0.00%). Meanwhile, these results were not significantly changed in the network meta-analysis of comparison between ORIF and INM (OR = 0.78; 95% CrI = 0.39–1.49), comparison between ORIF and DFR (OR = 1.04; 95%CrI = 0.44–2.44), and comparison between INM and DFR (OR = 1.34; 95% CrI = 0.48–3.80). However, the trend between INM and DFR was inversely benefitted to DFR because OR was changed from 0.61 to 1.37. All statistical results are shown in Figure 3.
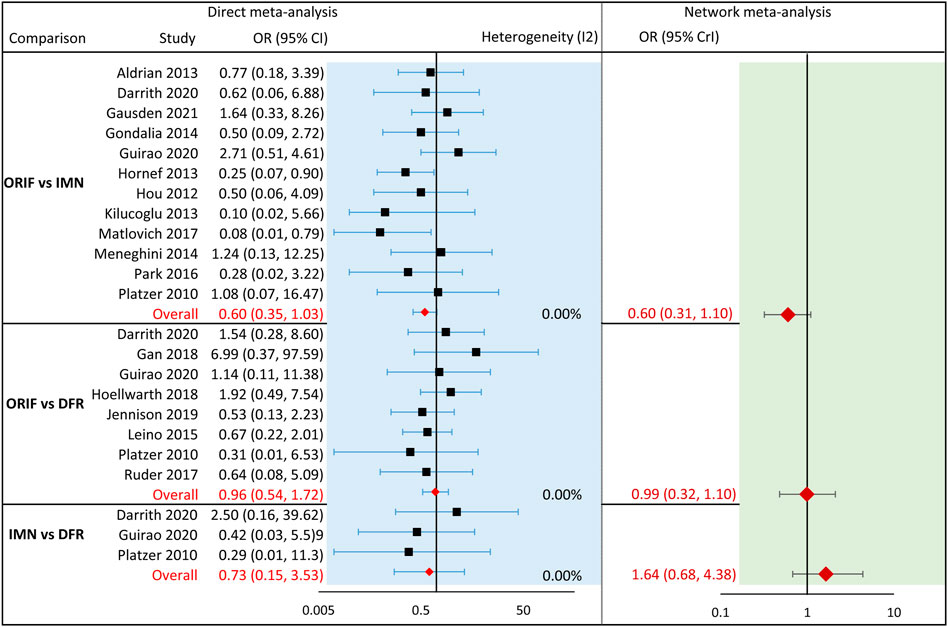
The Meta-Analysis of Revision Rates
Direct meta-analyses revealed a marginally favorable result in patients who received ORIF compared with IMN (12 studies, OR = 0.60; 95% CI = 0.35 to 1.03; I2 = 0.00%). However, this result received the support of network meta-analysis (OR = 0.60; 95% CrI = 0.31–1.10). For remaining comparisons including the comparison between ORIF and DFR (eight studies, OR = 0.96; 95% CI = 0.32 to 1.10; I2 = 0.00%) and comparison between IMN and DFR (three studies, OR = 0.73; 95% CI = 0.15 to 3.53; I2 = 0.00%) did not achieve statistically significant level in direct meta-analyses. Similarly, the network meta-analyses of these two comparisons did possess unchanged results. However, the trend between INM and DFR was inversely benefitted to DFR because OR was changed from 0.73 to 1.64 in network meta-analysis. All statistical results are shown in Figure 4.
Ranking of Probabilities
We generated ranking probabilities of these three surgical treatments in terms of major complication rates and revision rates. According to the results of ranking probabilities, DFR had the highest probability of becoming the best option, ORIF had the probability of ranking at a second option, and IMN at the third option for two outcomes. The plot of rankings of three surgical treatments is shown in Figure 5.
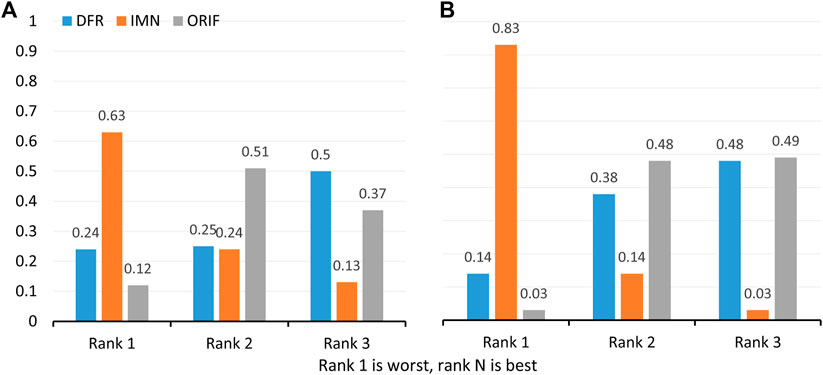
FIGURE 5. Ranking probabilities of all targeted interventions in terms of major complications (A) and reoperation rate (B).
Publication Bias
We generated a comparison-adjusted funnel plot for major complications and revision rates, and a symmetric outline indicates the absence of publication bias and small sample size effects (Supplementary Figure S3).
Discussion
Although the surgical strategy has been the preferred therapeutic option for PPDFF (Su et al., 2004; Kinney and Engh, 2018) and has been widely used in clinical practice (Darrith et al., 2020), it remains debatable regarding the optimal surgical procedure of choice (Quinzi et al., 2021) because several surgical regimes including ORIF, IMN, and DFR were available. In this network meta-analysis, we aimed to determine which regimes should be preferentially selected by evaluating major complication rates and revision rates following ORIF, IMN, and DFR. Pooled results suggest that these three surgical regimes have no statistical difference in the treatment of PPDFF. However, we still find that DFR should be preferentially selected to treat PPDFF, according to the rank probabilities of three regimes when objective resources are allowed.
Compared to conventional plating, ORIF with periarticular locking plates has the ability to improve rates of union and then decrease rates of revision because plating may facilitate a more anatomic reduction and allow for more predictable restoration of joint alignment (Christ et al., 2018). Meanwhile, IMN fixation has been proved to have the ability to avoid soft-tissue stripping and provide biomechanical advantages compared with ORIF with periarticular locking plates (Bong et al., 2002). Although several studies have investigated the comparative efficacy and safety of the two techniques (Horneff et al., 2013; Gondalia et al., 2014; Meneghini et al., 2014), there remains no consensus on the optimal treatment. Meanwhile, published meta-analyses (Shin et al., 2017; Liu et al., 2019; Shah et al., 2020) did not also reveal a significant difference between these two techniques in terms of clinical outcomes. More importantly, IMN fixation has significant dependence on the types of TKA prosthetic design, indirect reduction techniques, and previous hip implants (Shah et al., 2020). In this network meta-analysis, we also suggested that ORIF with periarticular locking plates should be preferentially selected according to the ranking probabilities compared with IMN fixation, although no difference is detected in major complications rates and revision rates between ORIF with periarticular locking plates and IMN fixation.
With the rapid improvements in prosthetic design, distal femoral replacement (DFR) has also been proposed to treat PPDFF in geriatric patients (Meluzio et al., 2020). Unfortunately, primary studies (Platzer et al., 2010; Darrith et al., 2020) and subsequent meta-analyses (Wadhwa et al., 2021) did not reveal the difference between the two techniques in a series of clinical outcomes. It is noted that deep infection is a major concern faced by the DFR technique (Mortazavi et al., 2010; Rahman et al., 2016); however, our network meta-analysis indicates beneficial trends for DFR related to ORIF with periarticular locking plates and IMN fixation although the statistical difference was not obtained. DFR is suggested as an optimal treatment option for PPDFF compared to other two surgical treatments; however, it should be rationally selected because this surgical technique is characterized by high cost (Quinzi et al., 2021).
Several meta-analyses have been published to compare two of these three surgical treatments; however, our study has more advantages. First and foremost, we utilized network meta-analysis to rank these three surgical treatments and, therefore, provide definitive evidence for making a decision in clinical practice. Second, more eligible studies appear in this network meta-analysis to generate more reliable and robust results. Third, both direct and indirect evidence were simultaneously incorporated to estimate the overall results, and thus the limitation resulting from an insufficient number of eligible studies directly comparing two out of three treatments is partially overcome.
Certainly, we must also recognize some limitations in this network meta-analysis. First, the accumulated sample size is relatively inadequate although 17 eligible studies are included, and thus, our findings should be cautiously interpreted, and future studies with a larger sample size should be designed. Second, some eligible studies did not report specific follow-up time; we cannot, therefore, calculate adjusted estimates according to follow-up time. Third, subgroup analysis cannot be conducted according to types of fractures, CCI score, and ASA score due to limited data.
Conclusion
Based on the best available evidence, ORIF with periarticular locking plates, IMN fixation, and DFR are comparable in major complication rates and revision rates. However, DFR should be preferentially selected under the full consideration of cost. Otherwise, ORIF with periarticular locking plates maybe a preferred alternative option. Moreover, our network meta-analysis emphasizes the need for future prospective randomized controlled trials evaluating the outcomes of these three surgical strategies.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding authors.
Author Contributions
Substantially contributed to conception or design: YL, YZ, and TM. Contributed to the acquisition, analysis, or interpretation of data: QW, LS, CZ, and QH. Drafted the manuscript for important content: YX and CR. Critically revised the manuscript for important intellectual content: HX, ZL, and KZ. Gave final approval: all authors.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that maybe evaluated in this article, or claim that maybe made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to deeply appreciate all authors who performed all eligible studies which have been included in the present network meta-analysis.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmats.2022.862698/full#supplementary-material
Supplementary Figure S1 | Schematic figure for Monte Carlo simulation.
Supplementary Figure S2 | Node split plot of major complications and revision rates.
Supplementary Figure S3 | Comparison-adjusted funnel plot of major complications (A) and revision (B) rates.
References
Agarwal, S., Sharma, R. K., and Jain, J. K. (2014). Periprosthetic Fractures after Total Knee Arthroplasty. J. Orthop. Surg. Hong. Kong) 22 (1), 24–29. doi:10.1177/230949901402200108
Albert, I., and Makowski, D. (2019). Ranking Crop Species Using Mixed Treatment Comparisons. Res. Syn. Meth 10 (3), 343–359. doi:10.1002/jrsm.1328
Aldrian, S., Schuster, R., Haas, N., Erhart, J., Strickner, M., Blutsch, B., et al. (2013). Fixation of Supracondylar Femoral Fractures Following Total Knee Arthroplasty: Is There Any Difference Comparing Angular Stable Plate Fixation versus Rigid Interlocking Nail Fixation? Arch. Orthop. Trauma Surg. 133 (7), 921–927. doi:10.1007/s00402-013-1730-9
Bong, M. R., Egol, K. A., Koval, K. J., Kummer, F. J., Su, E. T., Iesaka, K., et al. (2002). Comparison of the LISS and a Retrograde-Inserted Supracondylar Intramedullary Nail for Fixation of a Periprosthetic Distal Femur Fracture Proximal to a Total Knee Arthroplasty. J. Arthroplasty 17 (7), 876–881. doi:10.1054/arth.2002.34817
Bowden, J., Tierney, J. F., Copas, A. J., and Burdett, S. (2011). Quantifying, Displaying and Accounting for Heterogeneity in the Meta-Analysis of RCTs Using Standard and Generalised Qstatistics. BMC Med. Res. Methodol. 11, 41. doi:10.1186/1471-2288-11-41
Brooks, S. P., and Gelman, A. (1998). General Methods for Monitoring Convergence of Iterative Simulations. J. Comput. Graph. Statistics 7, 434–455. doi:10.1080/10618600.1998.10474787
Burger, D. A., and Schall, R. (2015). A Bayesian Nonlinear Mixed-Effects Regression Model for the Characterization of Early Bactericidal Activity of Tuberculosis Drugs. J. Biopharm. Statistics 25 (6), 1247–1271. doi:10.1080/10543406.2014.971170
Christ, A. B., Chawla, H., Gausden, E. B., Villa, J. C., Wellman, D. S., Lorich, D. G., et al. (2018). Radiographic and Clinical Outcomes of Periprosthetic Distal Femur Fractures Treated with Open Reduction Internal Fixation. J. Orthop. Trauma 32 (10), 515–520. doi:10.1097/bot.0000000000001265
Cipriani, A., Higgins, J. P. T., Geddes, J. R., and Salanti, G. (2013). Conceptual and Technical Challenges in Network Meta-Analysis. Ann. Intern Med. 159 (2), 130–137. doi:10.7326/0003-4819-159-2-201307160-00008
Darrith, B., Bohl, D. D., Karadsheh, M. S., Sporer, S. M., Berger, R. A., and Levine, B. R. (2020). Periprosthetic Fractures of the Distal Femur: Is Open Reduction and Internal Fixation or Distal Femoral Replacement Superior? J. Arthroplasty 35 (5), 1402–1406. doi:10.1016/j.arth.2019.12.033
Dias, S., Welton, N. J., Caldwell, D. M., and Ades, A. E. (2010). Checking Consistency in Mixed Treatment Comparison Meta-Analysis. Stat. Med. 29 (7-8), 932–944. doi:10.1002/sim.3767
Ebraheim, N. A., Carroll, T., Bonaventura, B., Moral, M. Z., Jabaly, Y. G., and Liu, J. (2014). Challenge of Managing Distal Femur Fractures with Long-Stemmed Total Knee Implants. Orthop. Surg. 6 (3), 217–222. doi:10.1111/os.12117
Ebraheim, N. A., Kelley, L. H., Liu, X., Thomas, I. S., Steiner, R. B., and Liu, J. (2015). Periprosthetic Distal Femur Fracture after Total Knee Arthroplasty: A Systematic Review. Orthop. Surg. 7 (4), 297–305. doi:10.1111/os.12199
Gan, G., Teo, Y. H., and Kwek, E. B. K. (2018). Comparing Outcomes of Tumor Prosthesis Revision and Locking Plate Fixation in Supracondylar Femoral Periprosthetic Fractures. Clin. Orthop. Surg. 10 (2), 174–180. doi:10.4055/cios.2018.10.2.174
García Guirao, A. J., Andrés Cano, P., Moreno Domínguez, R., Giráldez Sánchez, M., and Cano Luís, P. (2020). Análisis de la mortalidad tras el tratamiento quirúrgico de las fracturas periprotésicas de fémur distal. Rev. Española Cirugía Ortopédica Traumatol. 64 (2), 92–98. doi:10.1016/j.recot.2019.11.002
Gausden, E. B., Lim, P. K., Rabonivich, A., Shaath, M. K., Mitchell, P. M., Hartline, B., et al. (2021). Outcomes of Periprosthetic Distal Femur Fractures Following Total Knee Arthroplasty: Intramedullary Nailing versus Plating. Injury 52 (7), 1875–1879. doi:10.1016/j.injury.2021.05.007
Gondalia, V., Choi, D. H., Lee, S. C., Nam, C. H., Hwang, B. H., Ahn, H. S., et al. (2014). Periprosthetic Supracondylar Femoral Fractures Following Total Knee Arthroplasty: Clinical Comparison and Related Complications of the Femur Plate System and Retrograde-Inserted Supracondylar Nail. J. Orthopaed Traumatol. 15 (3), 201–207. doi:10.1007/s10195-014-0287-x
Gracia-Ochoa, M., Miranda, I., Orenga, S., Hurtado-Oliver, V., Sendra, F., and Roselló-Añón, A. (2016). Fracturas Periprotésicas de Fémur Sobre Prótesis de cadera y rodilla. Análisis de una serie de 34 Casos y revisión de las series Españolas en los Ultimos 20 años. Rev. Española Cirugía Ortopédica Traumatol. 60 (5), 271–278. doi:10.1016/j.recot.2016.06.005
Higgins, J. P. T., and Green, S. (2011). Cochrane Handbook for Systematic Reviews of Interventions. [updated March 2011]. The Cochrane Collaboration. Available from: www.handbook.cochrane.org
Higgins, J. P. T., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring Inconsistency in Meta-Analyses. Bmj 327 (7414), 557–560. doi:10.1136/bmj.327.7414.557
Higgins, J. P. T., and Thompson, S. G. (2002). Quantifying Heterogeneity in a Meta-Analysis. Stat. Med. 21 (11), 1539–1558. doi:10.1002/sim.1186
Hoellwarth, J. S., Fourman, M. S., Crossett, L., Goodman, M., Siska, P., Moloney, G. B., et al. (2018). Equivalent Mortality and Complication Rates Following Periprosthetic Distal Femur Fractures Managed with Either Lateral Locked Plating or a Distal Femoral Replacement. Injury 49 (2), 392–397. doi:10.1016/j.injury.2017.11.040
Horneff, J. G., Scolaro, J. A., Jafari, S. M., Mirza, A., Parvizi, J., and Mehta, S. (2013). Intramedullary Nailing versus Locked Plate for Treating Supracondylar Periprosthetic Femur Fractures. Orthopedics 36 (5), e561–566. doi:10.3928/01477447-20130426-16
Hou, Z., Bowen, T. R., Irgit, K., Strohecker, K., Matzko, M. E., Widmaier, J., et al. (2012). Locked Plating of Periprosthetic Femur Fractures above Total Knee Arthroplasty. J. Orthop. Trauma 26 (7), 427–432. doi:10.1097/BOT.0b013e31822c050b
Hutton, B., Salanti, G., Caldwell, D. M., Chaimani, A., Schmid, C. H., Cameron, C., et al. (2015). The PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-Analyses of Health Care Interventions: Checklist and Explanations. Ann. Intern Med. 162 (11), 777–784. doi:10.7326/m14-2385
Jennison, T., and Yarlagadda, R. (2020). A Case Series of Mortality and Morbidity in Distal Femoral Periprosthetic Fractures. J. Orthop. 18, 244–247. doi:10.1016/j.jor.2019.09.007
Kiluçoğlu, O. I., Akgül, T., Sağlam, Y., and Yazicioğlu, O. (2013). Comparison of Locked Plating and Intramedullary Nailing for Periprosthetic Supracondylar Femur Fractures after Knee Arthroplasty. Acta Orthop. Belg 79 (4), 417
Kinney, M. C., and Engh, C. A. (2018). Periprosthetic Femur Fractures. Seminars Arthroplasty 29 (3), 166–171. doi:10.1053/j.sart.2019.02.010
Konan, S., Sandiford, N., Unno, F., Masri, B. S., Garbuz, D. S., and Duncan, C. P. (2016). Periprosthetic Fractures Associated with Total Knee Arthroplasty: an Apdate. Bone . Jt. J. 98-b (11), 1489–1496. doi:10.1302/0301-620x.98b11.Bjj-2016-0029.R1
Leino, O. K., Lempainen, L., Virolainen, P., Sarimo, J., Pölönen, T., and Mäkelä, K. T. (2015). Operative Results of Periprosthetic Fractures of the Distal Femur in A Single Academic Unit. Scand. J. Surg. 104 (3), 200–207. doi:10.1177/1457496914552343
Liu, W., Gao, Q., Li, Q., and Jing, J. (2019). Locked Compression Plate versus Retrograde Intramedullary Nail for Peripros-Thetic Femur Fractures Following Total Knee Arthroplasty: A Meta-Analysis. Acta Medica Mediterr. 35 (2), 1019–1023. doi:10.19193/0393-6384_2019_2_155
Lotzien, S., Hoberg, C., Hoffmann, M. F., and Schildhauer, T. A. (2019). Clinical Outcome and Quality of Life of Patients with Periprosthetic Distal Femur Fractures and Retained Total Knee Arthroplasty Treated with Polyaxial Locking Plates: a Single-Center Experience. Eur. J. Orthop. Surg. Traumatol. 29 (1), 189–196. doi:10.1007/s00590-018-2266-z
Lu, G., and Ades, A. E. (2004). Combination of Direct and Indirect Evidence in Mixed Treatment Comparisons. Stat. Med. 23 (20), 3105–3124. doi:10.1002/sim.1875
Matlovich, N. F., Lanting, B. A., Vasarhelyi, E. M., Naudie, D. D., McCalden, R. W., and Howard, J. L. (2017). Outcomes of Surgical Management of Supracondylar Periprosthetic Femur Fractures. J. Arthroplasty 32 (1), 189–192. doi:10.1016/j.arth.2016.06.056
Meluzio, M., Oliva, M., Minutillo, F., Ziranu, A., Saccomanno, M., and Maccauro, G. (2020). The Use of Knee Mega-Prosthesis for the Management of Distal Femoral Fractures: A Systematic Review. Injury 51 (Suppl. 3), S17–s22. doi:10.1016/j.injury.2019.08.011
Meneghini, R. M., Keyes, B. J., Reddy, K. K., and Maar, D. C. (2014). Modern Retrograde Intramedullary Nails versus Periarticular Locked Plates for Supracondylar Femur Fractures after Total Knee Arthroplasty. J. Arthroplasty 29 (7), 1478–1481. doi:10.1016/j.arth.2014.01.025
Mortazavi, S. M. J., Kurd, M. F., Bender, B., Post, Z., Parvizi, J., and Purtill, J. J. (2010). Distal Femoral Arthroplasty for the Treatment of Periprosthetic Fractures after Total Knee Arthroplasty. J. Arthroplasty 25 (5), 775–780. doi:10.1016/j.arth.2009.05.024
Myers, P., Laboe, P., Johnson, K. J., Fredericks, P. D., Crichlow, R. J., Maar, D. C., et al. (2018). Patient Mortality in Geriatric Distal Femur Fractures. J. Orthop. Trauma 32 (3), 111–115. doi:10.1097/bot.0000000000001078
Page, M. J., Moher, D., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. Bmj 372, n160. doi:10.1136/bmj.n160
Palma Pérez, S., and Delgado Rodríguez, M. (2006). Consideraciones prácticas acerca de la Detección del sesgo de Publicación. Gac. Sanit. 20 (Suppl. 3), 10–16. doi:10.1157/13101085
Park, J., and Lee, J. H. (2016). Comparison of Retrograde Nailing and Minimally Invasive Plating for Treatment of Periprosthetic Supracondylar Femur Fractures (OTA 33-A) above Total Knee Arthroplasty. Arch. Orthop. Trauma Surg. 136 (3), 331–338. doi:10.1007/s00402-015-2374-8
Platzer, P., Schuster, R., Aldrian, S., Prosquill, S., Krumboeck, A., Zehetgruber, I., et al. (2010). Management and Outcome of Periprosthetic Fractures after Total Knee Arthroplasty. J. Trauma 68 (6), 1464–1470. doi:10.1097/TA.0b013e3181d53f81
Quinzi, D. A., Ramirez, G., Kaplan, N. B., Myers, T. G., Thirukumaran, C. P., and Ricciardi, B. F. (2021). Early Complications and Reoperation Rates Are Similar Amongst Open Reduction Internal Fixation, Intramedullary Nail, and Distal Femoral Replacement for Periprosthetic Distal Femur Fractures: a Systematic Review and Meta-Analysis. Arch. Orthop. Trauma Surg. 141 (6), 997–1006. doi:10.1007/s00402-021-03866-4
Rahman, W. A., Vial, T. A., and Backstein, D. J. (2016). Distal Femoral Arthroplasty for Management of Periprosthetic Supracondylar Fractures of the Femur. J. Arthroplasty 31 (3), 676–679. doi:10.1016/j.arth.2015.09.042
Ruder, J. A., Hart, G. P., Kneisl, J. S., Springer, B. D., and Karunakar, M. A. (2017). Predictors of Functional Recovery Following Periprosthetic Distal Femur Fractures. J. Arthroplasty 32 (5), 1571–1575. doi:10.1016/j.arth.2016.12.013
Shah, J. K., Szukics, P., Gianakos, A. L., Liporace, F. A., and Yoon, R. S. (2020). Equivalent Union Rates between Intramedullary Nail and Locked Plate Fixation for Distal Femur Periprosthetic Fractures - a Systematic Review. Injury 51 (4), 1062–1068. doi:10.1016/j.injury.2020.02.043
Shin, Y.-S., Kim, H.-J., and Lee, D.-H. (2017). Similar Outcomes of Locking Compression Plating and Retrograde Intramedullary Nailing for Periprosthetic Supracondylar Femoral Fractures Following Total Knee Arthroplasty: a Meta-Analysis. Knee Surg. Sports Traumatol. Arthrosc. 25 (9), 2921–2928. doi:10.1007/s00167-016-4050-0
Singh, S., Murad, M. H., Chandar, A. K., Bongiorno, C. M., Singal, A. K., Atkinson, S. R., et al. (2015). Comparative Effectiveness of Pharmacological Interventions for Severe Alcoholic Hepatitis: A Systematic Review and Network Meta-Analysis. Gastroenterology 149 (4), 958–970. doi:10.1053/j.gastro.2015.06.006
Slim, K., Nini, E., Forestier, D., Kwiatkowski, F., Panis, Y., and Chipponi, J. (2003). Methodological Index for Non-randomized Studies (MINORS ): Development and Validation of a New Instrument. ANZ J. Surg. 73 (9), 712–716. doi:10.1046/j.1445-2197.2003.02748.x
Su, E. T., DeWal, H., and Di Cesare, P. E. (2004). Periprosthetic Femoral Fractures above Total Knee Replacements. J. Am. Acad. Orthop. Surg. 12 (1), 12–20. doi:10.5435/00124635-200401000-00003
Wadhwa, H., Salazar, B. P., Goodnough, L. H., Van Rysselberghe, N. L., DeBaun, M. R., Wong, H.-N., et al. (2022). Distal Femur Replacement versus Open Reduction and Internal Fixation for Treatment of Periprosthetic Distal Femur Fractures: A Systematic Review and Meta-Analysis. J. Orthop. Trauma 36, 1–6. doi:10.1097/bot.0000000000002141
Keywords: periprosthetic distal femur fracture, distal femoral replacement, periarticular locked plate, retrograde intramedullary nail, network meta-analysis
Citation: Lu Y, Xu Y, Ren C, Wang Q, Sun L, Zhang C, Huang Q, Xue H, Li Z, Zhang K, Zhao Y and Ma T (2022) Network Meta-Analysis of Open Reduction Internal Fixation, Intramedullary Nail Fixation, and Distal Femoral Replacement for Periprosthetic Distal Femur Fractures. Front. Mater. 9:862698. doi: 10.3389/fmats.2022.862698
Received: 24 February 2022; Accepted: 23 May 2022;
Published: 30 June 2022.
Edited by:
Masoud Mozafari, University of Toronto, CanadaReviewed by:
Fei Xing, Sichuan University, ChinaKrishna Ramajayam, Medical University of South Carolina, United States
Copyright © 2022 Lu, Xu, Ren, Wang, Sun, Zhang, Huang, Xue, Li, Zhang, Zhao and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yang Zhao, enk4ODEwMjdAMTI2LmNvbQ==; Teng Ma, Z3VrZW10QDE2My5jb20=
†These authors share first authorship
 Yao Lu
Yao Lu Yibo Xu†
Yibo Xu† Teng Ma
Teng Ma