- 1African Center of Excellence for the Prevention and Control of Communicable Diseases, Faculty of Health Sciences and Techniques, Gamal Abdel Nasser University of Conakry, Conakry, Guinea
- 2University Hospital of Clermont-Ferrand, Department of Medicine & Paramedical Professions, National Centre for Scientific Research (CNRS), Sigma Clermont, Pascal Institute, University Clermont Auvergne, Aubière, France
- 3Ministry of Health and Public Hygiene, Centre National de Recherche et de Formation en Santé Rurale (CNRFSR), Maferenyah, Guinea
- 4Department of Public Health, Gamal Abdel Nasser University of Conakry, Conakry, Guinea
- 5Ministry of Health and Public Hygiene, National Malaria Control Program, Conakry, Guinea
- 6Centre de Recherche et de Formation en Infectiologie de Guinée (CERFIG), Gamal Abdel Nasser University of Conakry, Conakry, Guinea
Background: Early identification and management of cases are key for controlling and eliminating malaria. This study aimed to assess the factors associated with the delay malaria treatment in Guinea.
Methods: Cross-sectional study was conducted at 60 health facilities in eight administrative regions from December 2022 to March 2023. Patients with a diagnosis of malaria through either microscopy or a rapid diagnostic test (RDT), were interviewed using a standardized questionnaire. Treatment delays were defined as seeking care 48 hours after the onset of symptoms. Logistic regression was performed to assess factors associated with treatment delay. Adjusted odds ratio (OR) and confidence interval (CI) were used to explain the associated factors.
Results: 3,300 malaria patients were included and the findings showed a median time of symptoms onset and access of malaria treatment was 3.04 days. Alarmingly, only 800 (24.24%) of all cases sought and received treatment within 48 hours of symptom onset. The multivariate logistic regression indicated that children under 5 years of age who attempted self-medication for fever were 4.32 times more likely to experience a delay in treatment than those who sought immediate medical care in health facilities (OR:4.32, 95% CI: 2.96–6.36). Children whose parents had no formal education were 3.05 times more likely to experience a delay in treatment (OR:3.05, 95% CI: 1.66–5.60). Moreover, when the disease was considered non-severe the first time by caregivers, OR = 1.71 (95% CI: 1.26–2.33). For those 5 years old and above, using university hospital OR = 4.01, (95% CI: 2.01–8.44), living in Forest Guinea OR = 3.14, (95% CI 1.93–5.10) and Middle Guinea OR = 1.46 (95% CI: 1.09–1.95) were more likely to experience delay treatment.
Conclusions: The proportion of malaria patients with treatment within 48 is low, significantly falling short of the national targets. This substantial delay in treatment was attributed to factors such the lack of formal education, self-medication practices, and failure to recognize the illness severity. These findings underscore the urgent need for NMCP to enhance awareness regarding the importance of early presentation at health facilities, with targeted interventions.
1 Introduction
Malaria is a major public health concern especially in tropical regions. It was responsible for 249 million new cases and 608,000 deaths globally in 2022 (World Health Organization, 2023; Venkatesan, 2024). Sub-Saharan African alone accounted for 94% of cases and 95% of deaths (World Health Organization, 2023; Venkatesan, 2024). A favorable environment for the development of the vector, lack of resources and persistent poverty are factors that perpetuate this trend. According to the World Health Organization guidelines, malaria should be promptly diagnosed and treated within 24 hours of symptom onset to reduce the risk of severe disease, mortality and transmission (Bastaki et al., 2018; World Health Organization, 2022). Patient factors such as level of education, socio-economic status and medical factors such as perceived severity of symptoms can lead to delays in diagnosis and treatment of malaria (Bastaki et al., 2018; Adeoti and Cavallaro, 2022; Kaboré et al., 2022a). Nevertheless, little is known about the duration associated with each stage in the care of malaria patients at health facilities in the high-burden countries like Guinea. Knowledge of these different delays, and of the factors associated with delayed care, can help structure training for healthcare providers and awareness-raising messages of the communities.
In Guinea, there has been a notable reduction in the prevalence of malaria at the national level. The proportion has dropped significantly from 44% in 2012 to 17% in 2021 (Institut National de la Statistique, 2013; INS Guinée et al., 2022; Programme National de Lutte contre le Paludisme, 2023). This reduction can be attributed to the implementation of primary prevention strategies such as free insecticide-treated nets, chemoprevention of seasonal malaria and improved case management activities (INS Guinée et al., 2022). Consequently, the national Malaria Control Program has set a target objective in their 2023–2027 plan to reduce both the morbidity and mortality associated with malaria by at least 80%. This concerted effort is of utmost importance in order to achieve the ambitious goal of eliminating malaria as a public health concern by the year 2030 (Programme National de Lutte contre le Paludisme, 2023). However, to meet these goals, early treatment-seeking behavior and easy access to health services are crucial (Sonkong et al., 2015; Workineh and Mekonnen, 2018). Some authors have been recognized that self-treatment may lead to delays in seeking treatment, who can favorized to develop severe complications (Sonkong et al., 2015). A study carried out in Tanzania reported that out of 87.2% patients who sought care, 44.6% within 24 hours (Kassile et al., 2014). In some studies, age group, farmer occupation, high health care prices, self-medication practice, types of health facilities, distance to the health facilities were discovered to be major drivers of treatment seeking delay (Mburu et al., 2021; Guntur et al., 2022; Goshu and Tafasa, 2023).
In Guinea, a previous study of malaria patients at the Coyah district hospital in 2019 revealed that only 23.8% had access to treatment within 48 hours of the onset of symptoms (Cisse et al., 2021). However, no previous studies have clarified timeframes according to the health facilities level and the factors that may influence this delay in the adults and children’s patients in the country. Therefore, a better understanding of the factors contributing to delayed treatment of malaria patients has the potential to guide the design of case management strategies adapted to the local context. The aim of this study was to assess the factors associated with delayed malaria treatment in Guinea.
2 Methods
2.1 Study setting
Guinea is a coastal country in West Africa, with a surface area of 245,857 km2 and an estimated population of more than 13 million in 2022 (Institut National de la Statistique, 2017). The country is divided into four natural regions, eight administrative regions and 38 prefectures corresponding to 38 health districts. The national health system is organized in a pyramidal style with the primary level, accounting in 2022 for over 2,000 health post and 423 health centers. At the secondary level, there are referral hospitals, including 26 districts, eight regional hospitals and eight communal medical centers. At the tertiary level, there are three national hospitals that make up the Conakry University Hospital. The private healthcare sector is found at all three levels of the health pyramid and is less regulated. There are more than 606 private structures, 110 of which who the data are integrated by the National Malaria Control Program (Programme National de Lutte contre le Paludisme, 2023). The Guinean national guidelines recommend testing all patients with fever or history of fever and treating confirmed cases early with antimalarial drugs. Malaria rapid diagnostic tests (RDTs) are the most common diagnostic device and are used at all levels of health facilities, as well as by community health workers. Oral artemisinin-based combination therapies and intravenous or muscular artemisinin derivatives are the drugs indicated for the management of uncomplicated and complicated cases respectively (Guinea National Malaria Control Program, 2018).
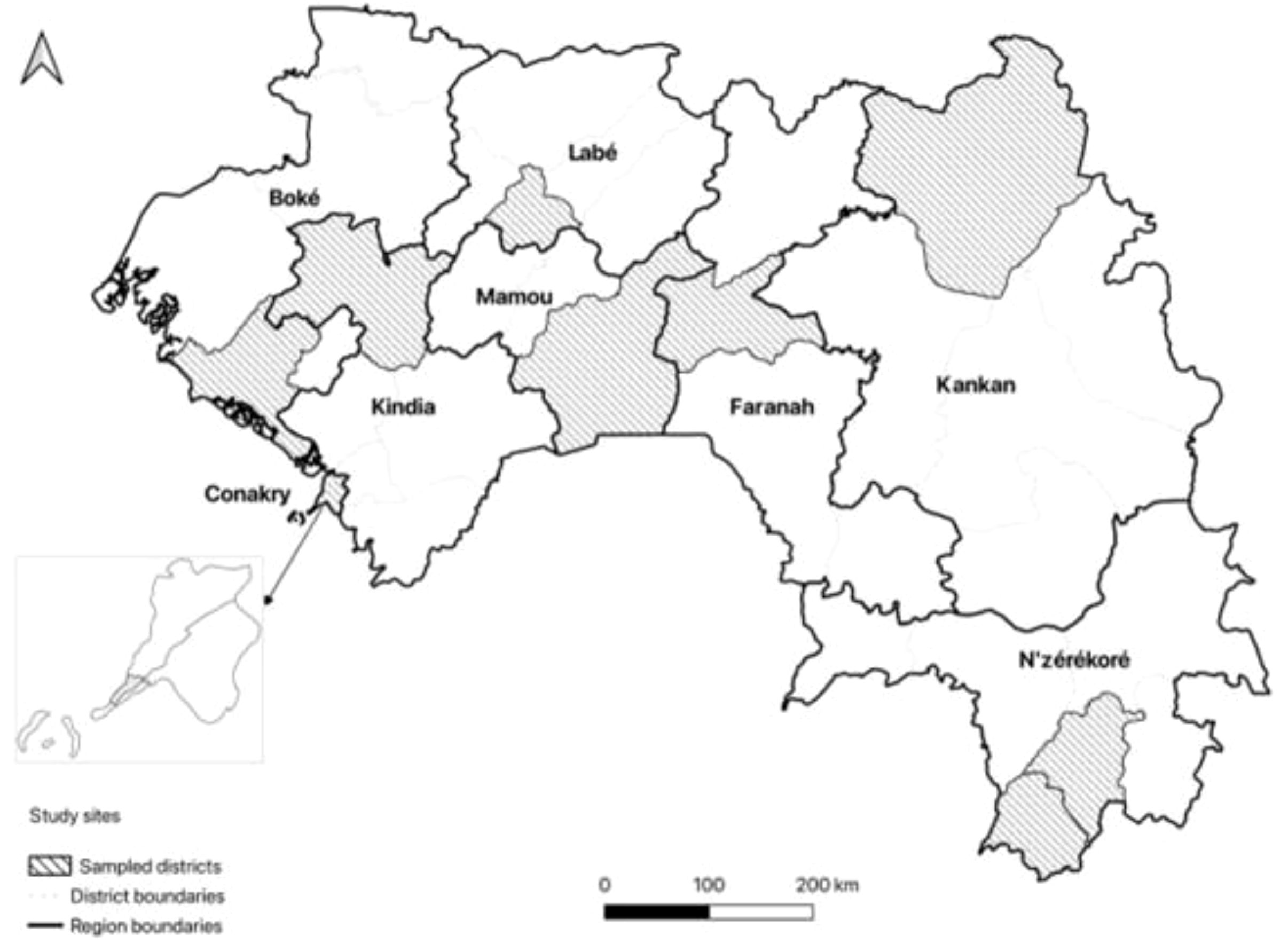
2.2 Site selection, sample size and study participants
Due to the regional prevalence of malaria (<1–30%), one health district was randomly sampled in each of the nine administrative regions, except for N’Zérékoré where two districts were selected due to the high prevalence of malaria (30%) and the size of the region (six districts) (INS Guinée et al., 2022; Hammer et al., 2024). Nine of Guinea’s 38 health districts were selected at random. In each health district, one hospital, one private facility integrated by the NMCP, one urban health center, two rural health centers, two health posts and four community health workers were selected randomly for inclusion in the study. The Figure 1 shows the map of Guinea with the selected districts by administrative region and natural region.
In this study, for each health district a minimal size calculated was 334 patients. For the nine districts chosen, the sample size minimum estimation was 3,006 malaria patients. This number was obtained after considering the proportion of 32% in Guinea for seeking advice in the first two days following the onset of fever (INS Guinée et al., 2022). The patients were divided into two age groups: children under 5, considered a vulnerable group for whom a range of activities are currently deployed (seasonal malaria chemoprevention, routine insecticide-impregnated nets (LLINs), perennial chemoprevention), and the 5+ age group benefiting from a general prevention strategy with a specific focus on pregnant women. The recruitment at each health facility took place until the required number of respondents agreed to participate.
2.3 Study design and period
This study was conducted in a cross-sectional from December 2022 to March 2023. The participants were patients who had received laboratory-confirmed diagnoses of malaria had been treated at health facilities in selected sites. These patients were recruited from hospitals, health centers, health posts and private clinics.
2.4 Study data collection
Data were collected from patients and caregivers using a tested and validated structured interview questionnaire. Eleven trained final-year medical and master students interviewed participants in French or local language. These investigators were trained in to carry out the interview face-to-face before the start of data collection. Data on socio-demographic characteristics collected included age, gender, residence area (rural or urban), marital status (married or unmarried), education (no education, less than university, university and professional), previous occupation (craftsman/farmer/trader, government worker, Not working), administrative region, religion (Muslim or Others), number of under-5 children in household (≤2 or >2)
The treatment seeking behavior included the access of health services included the type of health facilities of recruitment (Private health facility, Prefectural hospital, health centers, health posts and university hospital), travel time to nearest health facilities (≤2 hours, >2 hours), first actions taken in response to illness (Public health facility, private health facility, Self-treatment) and number of recourses before treatment (1 recourse, 2 recourses, ≥3 recourses).
The medical records informed the type of malaria (Uncomplicated, or Complicated) and type of laboratory confirmation (RTD, Microscopy and RTD associate to microscopy).
Information on the time between onset of symptoms and consultation at a health facility was sought and used to determine whether patients were delayed in seeking malaria care. Delay in case management was defined as a 48 hour between the onset of symptoms and care at the health facility.
2.5 Data analysis
Descriptive statistics were used to summarize sociodemographic, treatment-seeking behavior and delayed treatment-seeking. The time passed between the onset of symptom to the time of treatment was defined as early if care was sought within 48 hours after the onset of fever (coded as 0) and delayed if care was sought 48 hours after the onset of fever (coded as 1). Bivariate analyses and logistic regression were performed to estimate the effects of each explanatory variable on the dependent variable. The analysis of associated factors was carried out according to age groups (< 5 years and ≥ 5 years) due to the clinical classification of NMCP and to control for the effect of confounding variables. Logistic regression was performed to identify associations between independent variables and delay antimalarial treatment access. This analysis was performed separately between the group of under-5-year-olds who are currently benefiting of several prevention strategies, and those aged 5 and over.
Independent variables significantly related to delay in access to treatment (p-value ≤0.20) in the bivariate analysis were included in a multiple logistic regression analysis at the same time. Then, the Akaike Information Criterion (AIC) to optimize model performance with the STEPAIC function was used to obtain a final model. Statistical significance was defined as a p-value <0.05, while a final odds ratio (OR) with 95% confidence interval (95% CI) was used as an indicator of the magnitude of the association between independent variables and delay in access to antimalarial treatment. Checks were made for linearity, collinearity and interaction terms. The fit of the final model to the data was assessed by Hosmer and Lemeshow’s goodness of fit test. All analyses were performed using R 4.3.2 (RStudio 2023.12.0 + 369).
2.6 Ethical issues
The study was approved by the National Ethics Committee for Health Research of Guinea (registered as #151/CNERS, 2022). This study was conducted in accordance with the principles of the Declaration of Helsinki.
3 Results
3.1 Socio-demographic characteristics
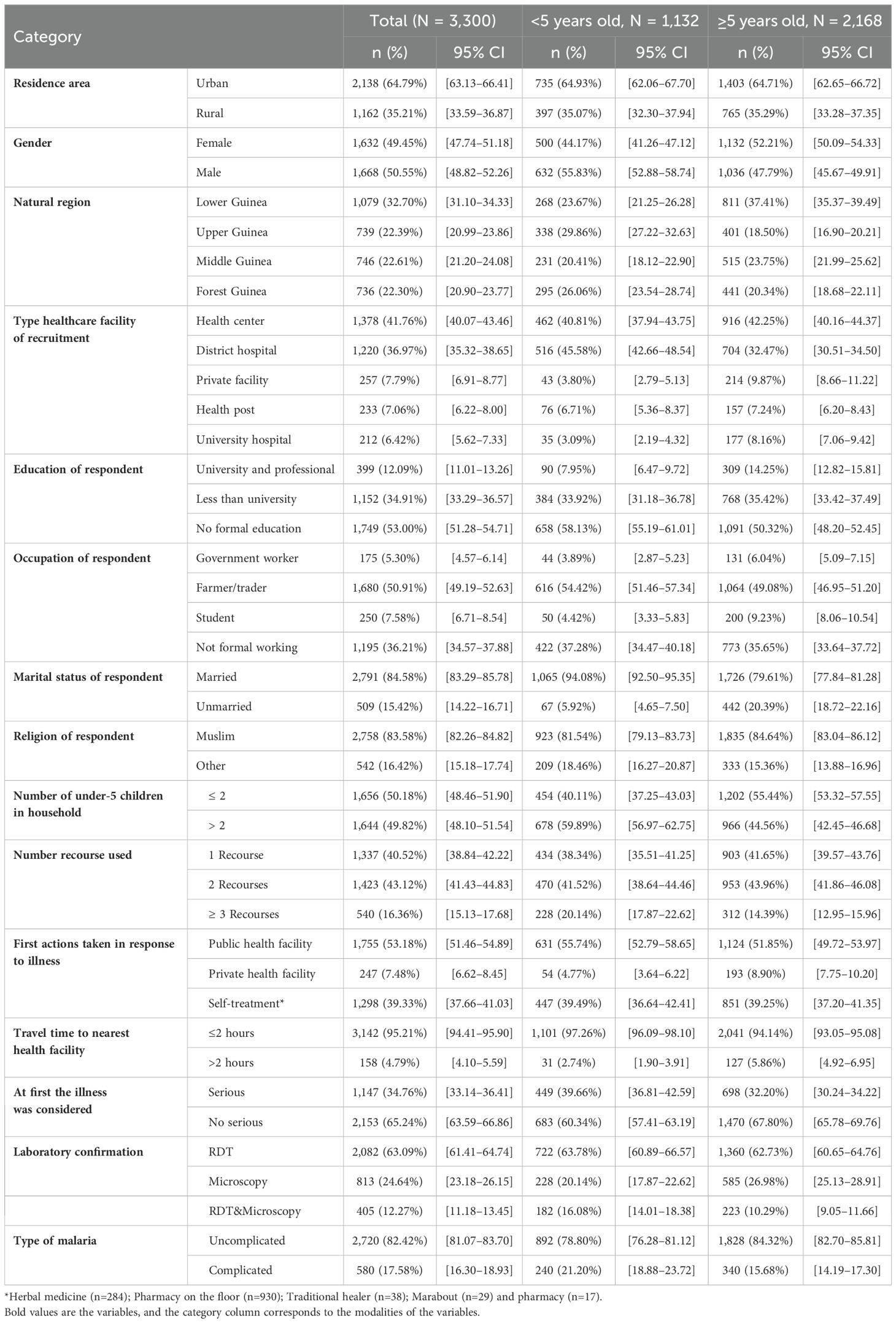
A total of 3,300 patients with confirmed malaria were surveyed. Children aged under 5 years old 1,132 (34.30%) and those aged 5–15 years old 682 (21.67%) were predominant. The age median of the patients aged under 5, was 24 months, the youngest was 6 months old and the oldest was 59 months. Most patients were recruited at the natural regions of Lower Guinea 1,079 (32.70%), from health centers 1,378 (41.76%), with a diagnosis of uncomplicated malaria 2,720 (82.42%), were urban residents 2,138 (64.79%). A total 1,632 (49.45%) were women and 1,668 (50,55%) were male. Respondents (patients or caregivers) were No formal education 1,749 (53.0%), currently married 2,791 (84.58%), farmers/traders 1,680 (50.91%), and Muslim faith 2,758 (83.58%). Basically, 1,656 (50.18%) respondents had fewer than two children under 5 years of age in their household, had a travel time to nearest health facility within 2 hours 3,142 (95.21%), and initially thought the illness was not serious 2,135 (65.24%). No conventional care was the first actions taken in response to illness for 1,298 (39.33%) of all malaria patients. The distribution of characteristics by age group of patients is summarized in Table 1.
3.2 Timeframes, treatment-seeking behavior for malaria
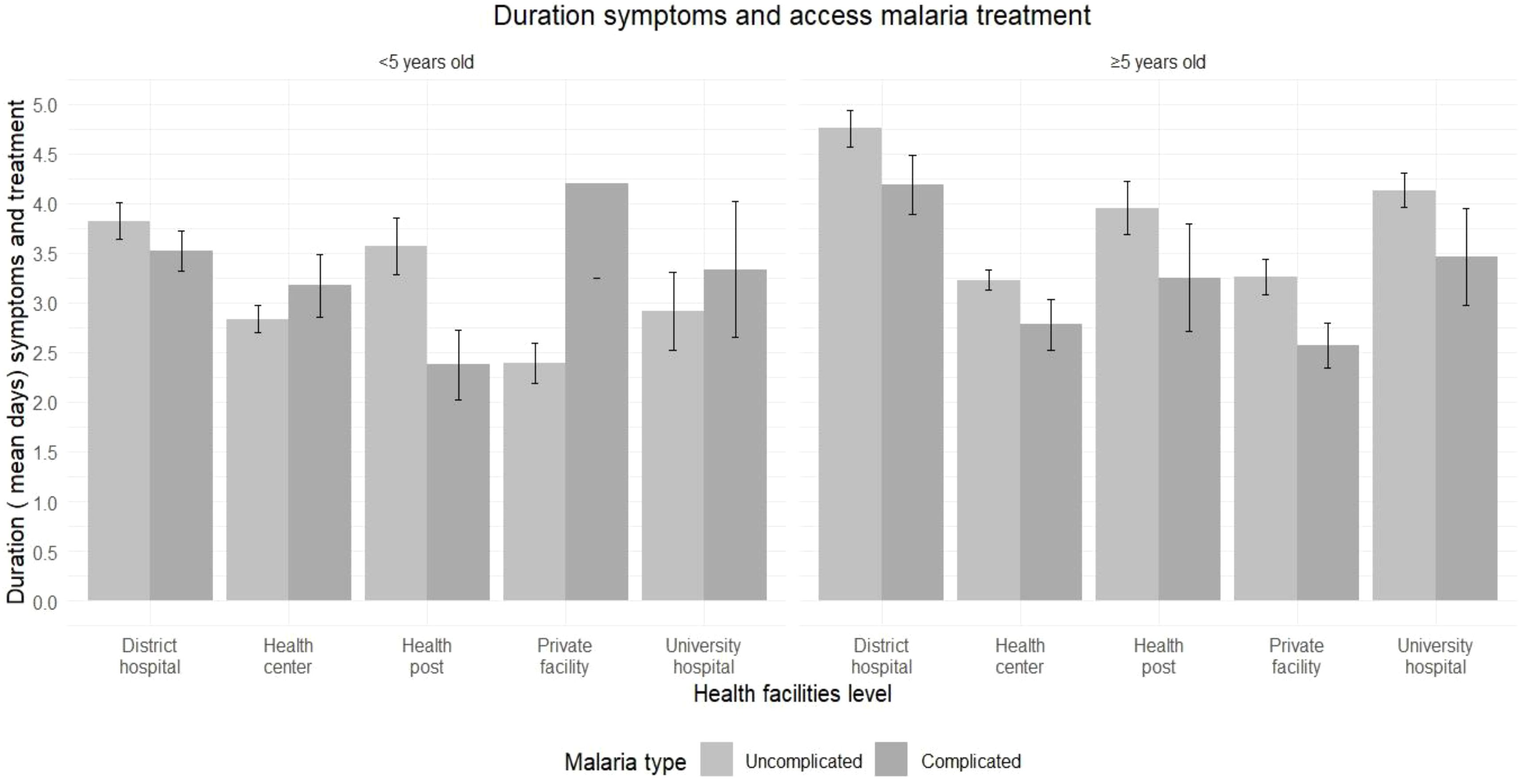
The median number of days until patients presented to the health facility was 3.0 days of symptoms onset, ranging from 1.0 day in 40 days. Once in the healthcare facilities, the median time between patient arrival and access to treatment was 1.5 hours, ranging from 1.50 hours for those under 5 to 1.75 hours for those 5 and over. In general, the median time for patients arriving and consultation at a health facility was 15 minutes, the time it took to perform a diagnostic test was 5 minutes, the time it took to receive test results was 30 minutes, and the duration between results to receive treatment was 15 minutes. Then according to the health facilities level, the median time from arrival to receiving treatment was 6 hours at university hospital, 2.9 hours at district hospitals, 2.25 hours at private health facilities, 1 hour at health post, and the health center. An illustration of the different ranges of patient treatment time according to health facilities level is shown in Figure 2. The median delay between first symptoms and access to malaria treatment was 3.04 days, with 3.03 days for under 5 years old to 3.06 days for 5 years old and over. According to age group and health facility level, the longest delays before access to treatment were observed for under-5 in private facilities for complicated cases (4.20 days), and in district hospitals for uncomplicated cases (3.80 days). For the 5 year and above group, the longest delays for complicated cases were observed in district hospitals and at the university hospital. The distribution of the number of days between symptoms and access to malaria treatment by age, type of malaria and level of health care facility is illustrated at Figure 3.
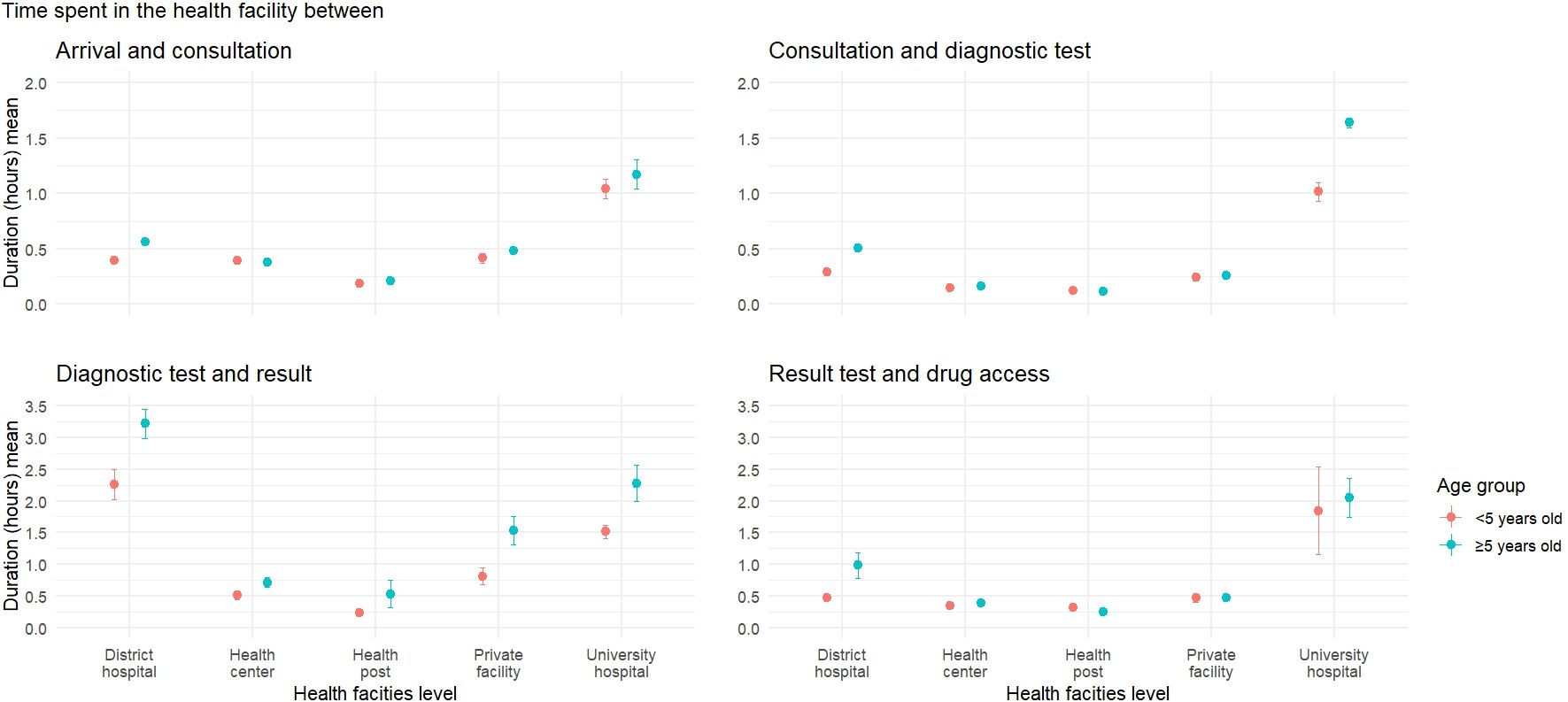
Figure 2. Time from arrival to malaria treatment in health facilities in the Republic of Guinea 2022–2023. Depending on the level of health facility, the longest stay was at the district hospital and the university hospital.
Out of a total of 3,300 patients, only 800 (24.24%) sought and received treatment within 48 hours of the onset of malaria symptoms. According to the age group, 29.15% of the under-5 of age and 21.68% of the 5 years old and above sought and received treatment within 48 hours of the onset of symptoms. The prevalence of delays in seeking care for patients who resorted to self-treatment for the first measures taken in response to the illness was 90.45%, with a proportion for the under-5s group of 85.46%, 95% CI: 81.77–88.5, and those aged 5 and over of 93.07% 95% CI: 91.09–94.64 (Additional files 1, 2).
3.3 Factors associated with delayed access to antimalarial treatment
The result of the multivariate logistic regression analysis showed in Table 2 the explanatory variables independently associated with delays antimalarial treatment access.
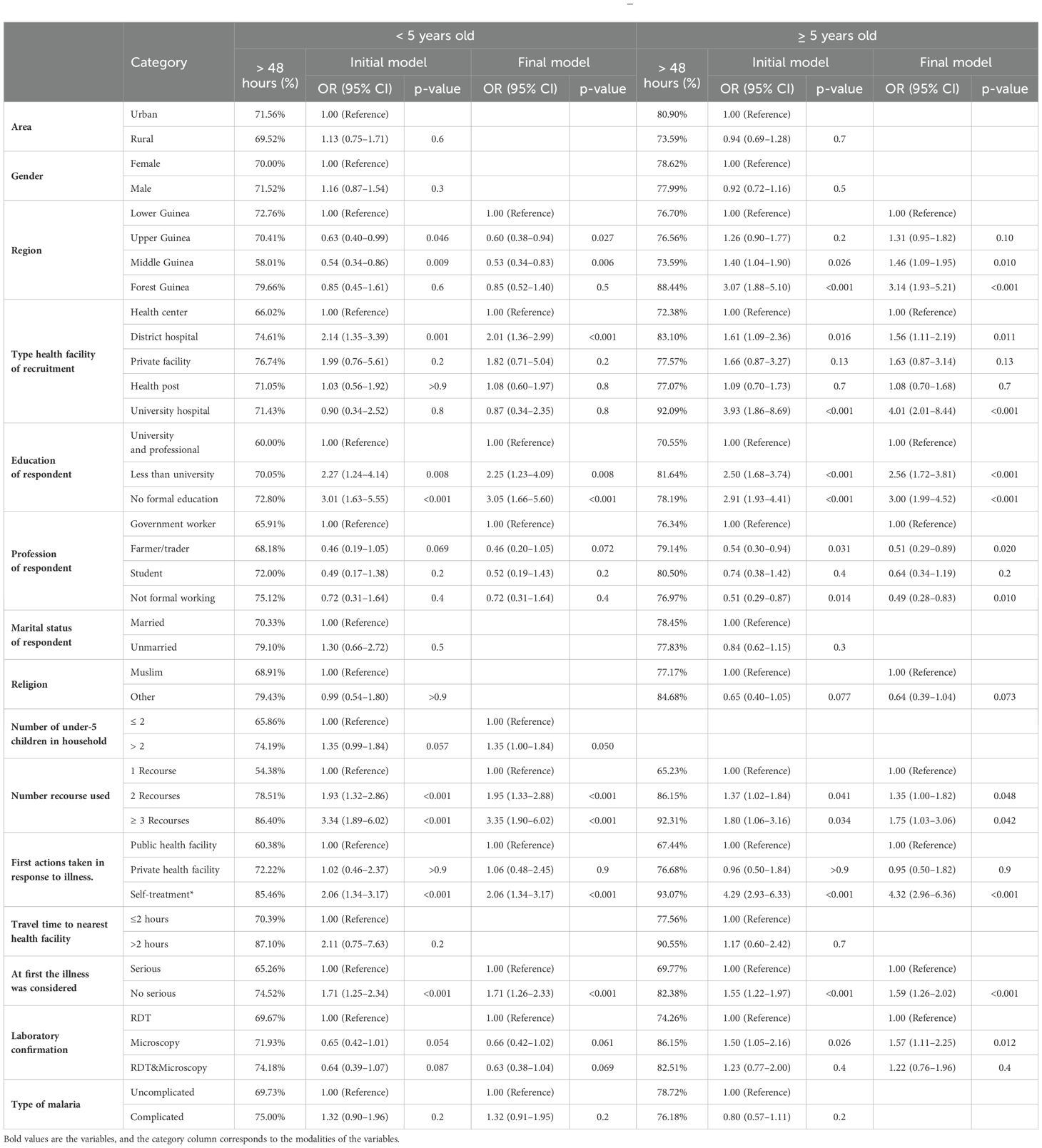
Table 2. Factors associated with delay in malaria treatment access at health facilities by age group of patients in Guinea, 2022–2023.
For malaria patient aged under 5 years old, the most important and consistent predictive factors for delays treatment access at health facilities were no formal education of respondent (caregivers) with the final odds ratio of 3.05 (95% IC 1.66–5.60), using self-treatment at the first action OR = 2.06 (95% CI 1.34–3.17), using 3 recourses and over final OR = 3.35 (95% CI: 1.90–6.02), considering the illness was no serious at first by caregivers OR = 1.71 (95% CI: 1.26–2.33). According to the health facility level, the children recruited in district hospital OR = 2.01 (95% CI: 1.36–2.29) were at risk of delaying access antimalarial treatment. The factors such as gender, geographical region and marital status of the child’s caregiver were not associated with delayed access to antimalarial treatment in children under 5 years old group.
For the 5 years old and above group, absence of formal education among the patient or caregiver for the 5–15 years, final OR = 3.00, (95% CI: 1.99–4.52), use of self-treatment as first resort OR = 4.32 (95% CI: 2.96–6. 36), use of 3 or more treatments OR = 1.75 (95% CI: 1.03–3.06), the illness considered not serious at the start OR = 1.59 (95% CI: 1.26–2.02) were the factors associated with delays to antimalarial treatment. Then in this group, the logistic regression showed the regions of Middle Guinea OR = 1.46 (95% CI: 1.09–1.95) and Forest Guinea OR = 3.14 (95% CI 1.93–5.10) were predictive factors delaying treatment access but not statistical significance for the under-5 group. According to the level of health facility and biological examination to confirm malaria, the patients recruited at the university hospital OR = 4.01 (95% CI: 2.01–8.44) and having benefited the microscopy OR = 1.50 (95% CI: 1.05–2.16) in the 5 and over age group were at risk of delaying antimalarial treatment (Table 2 show the risk factors of delaying malaria treatment).
4 Discussion
This study used data of 3300 patients in all age from a nationally representative survey, to explore the extent and factors associated with delayed malaria treatment-seeking for the first time in Guinea.
This study shows that more than three quarter (75.76%) of the malaria patients of all ages received treatment after 48 hours of onset of symptom contrary to recommendations by the WHO target of treating malaria (World Health Organization, 2022). This finding is consistent with studies which reported respectively 79.4% in Thailand (Sonkong et al., 2015) and 73% Kenya (Guyatt and Snow, 2004) for delayed malaria treatment. The proportions of the patients who received treatment after 24 or 48 hours reported in Burkina Fasso was 66.5% and Ethiopia 52.4% (Workineh and Mekonnen, 2018; Kaboré et al., 2022b).
In this study, 70.85% the children under 5 years old experienced a delay to access treatment. The access to treatment after 48 hours for malaria patients and children under 5, similar results have been reported in Nigeria (77.9%) (Omale et al., 2021a), low proportion in Burkina Faso (68.5%) (Kaboré et al., 2022b), while high proportion was reported in Uganda (83.4%) (Humphreys et al., 2021a). The disparity observed may be due to the different level of malaria knowledge of communities in those settings. According to group 5 years old and over 8 out of 10 patients experienced a delay in access to treatment, and this is higher than in the under 5 years old group. This trend can be explained by the optimal care package available for children under 5 years of age, and the interest that households may have in the health of the very young.
In this study, the median days until patients presented to the health facility were 3.0 days of symptom onset and the duration between symptoms and treatment of malaria was 3.04 days. In non-endemic countries, a systematic review showed that in cases of P. falciparum malaria, the overall median time between symptoms and access to a health facility was 3 days, and to treatment was 3.25 days (Bastaki et al., 2018). The delay in treatment access is a serious risk factor for transmission of malaria and the increase of mortality and remains a problem for patients living in Guinea. The training of healthcare providers and the availability of diagnostic and therapeutic resources help to create an environment conducive to the use of healthcare services. Another study related improved access to timely treatment and better differential diagnostics by health professionals are essential to ensure correct and appropriate treatment and to reduce reliance of patients on unqualified persons (Mburu et al., 2021).
All participants with no formal education of respondent, considering the illness not serious at first, using self-treatment at the first action, having three recourses and more were more likely to delay treatment within 48 hours of symptoms onset in all age groups. These results support the assertion that care-seeking behavior and treatment access were an iterative process, influenced by individual, socio-cultural, ecological and policy factors (Mburu et al., 2021; Casella et al., 2024).
In this study, and others carried out in Africa (Omale et al., 2021b; Kaboré et al., 2022a; Kombate et al., 2022; Diallo et al., 2024), high education level was identified as determinants of prompt care-seeking. These findings reinforce the need to improve literacy rates in Guinea to improve care-seeking behavior, especially for the mothers or caregivers. Indeed, maternal education would contribute to improve understanding of the disease and the ability to seek formal advice or care early (Kombate et al., 2022).
This study indicates that whatever the form of malaria, the low perception of illness severity at first could be causing delay in seeking adequate treatment in Guinea. Similar observations were noted among caregivers in Equatorial Guinea (Romay-Barja et al., 2016) and Tanzania (Mburu et al., 2021).
Self-treatment was one of the most important factors associated with delay in antimalarial treatment access in Guinea. Some studies have indicated that self-treatment is common in most African areas when initial symptoms experienced are mild, or during the initial period of illness (Kassam et al., 2015; Sonkong et al., 2015). A better strategy to raise awareness among populations to go to health establishments early and an overall effectiveness of community health policy could be a solution. Indeed, management of illness by community health workers improves timely access to treatment and is associated with a reduction in malaria infections (Sunguya et al., 2017; Awasthi et al., 2024).
In this study we also noted, for 5 years old and over, natural region of residence, type of test used for diagnosis confirmation and for under 5 years of age group level, healthcare facility of recruitment and were associated with delay in malaria treatment. Similar findings of relation between natural region of residence and delay in seeking malaria treatment were documented in Burkina Faso (Negatou et al., 2021) and Togo (Kombate et al., 2022). This regional difference is probably related to cultural differences in the perception of health and illnessl (Sonkong et al., 2015; Mpimbaza et al., 2017; Kombate et al., 2022).
The high level of education in urban areas can improve the level of knowledge of malaria and have an impact on their willingness to use the health-center services can explain this state.
In multivariable analyses, the occupation, marital status, religion, number children in household, travel time to nearest health facilities were not significantly associated with delay in seeking treatment in this current study. This results contrasts findings from other studies where occupation, marital status, religion, number children in household, distance to nearest health facility were plays a major role (Oyekale, 2015; Nkoka et al., 2019; Humphreys et al., 2021b; Adeoti and Cavallaro, 2022). A possible reason for disparity would be the difference of sample sizes and study populations.
The next steps will be focus on analyzing the perception of malaria prevention services by communities and health practitioner, and to model the impact of different scenarios aimed at improving early access to treatment.
5 Limitations
The limitations of this research include its cross-sectional design, which limits the ability to make causal inferences. The use of self-reported data from multiple questions rounds may be limited by recall or social desirability bias, which could create misclassification for late treatment-seeking. Another limitation of this study is the lack of quality control of malaria laboratory tests. Consequently, there could be a misclassification of malaria cases. In addition, the study deals only with data from patients having used a healthcare facility (public or integrated private) or the services of a community relay.
6 Conclusion
A low proportion of malaria patients sought and obtained treatment in a health facility within 48 hours of the onset of symptoms. This substantial delay in treatment was attributed to factors such the lack of formal education, self-medication practices, and failure to recognize the illness severity. These findings underscore the urgent need for NMCP to enhance awareness regarding the importance of early presentation at health facilities, while also implementing targeted interventions. Progress is still needed to reach the target set by the national malaria control strategy. The results show the need to strengthen malaria management at hospital and community level, with greater involvement of community health workers. These highlights show that the NMCP must also strengthen communication and stratify appropriate interventions according to groups and zones, to optimize prevention and early access to antimalarial treatment. Emphasis must be placed on raising community awareness of malaria prevention methods and early treatment-seeking behaviour.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
ED: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. KK: Formal analysis, Validation, Writing – review & editing. ND: Writing – review & editing. AD: Writing – review & editing. MB: Writing – review & editing. AT: Project administration, Resources, Validation, Writing – review & editing. LG: Supervision, Validation, Visualization, Writing – review & editing. AC: Funding acquisition, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the African Centre of Excellence for the Prevention and Control of Transmissible Diseases (CEA-PCMT) of the Faculty of Health Sciences and Techniques of the University of Conakry, the Centre de Recherche et de Formation en Infectiologie de Guinée (CERFIG) through the West Africa Mathematical Modelling Capacity Development (WAMCAD) project, and the France Embassy in the Republic of Guinea.
Acknowledgments
Our gratitude goes to the CEA-PCMT, as well as to the Public Health Department of the Clermont-Ferrand University Hospital. We would also like to express our appreciation to the Centre de Recherche et de Formation en Infectiologie de Guinée and the National Malaria Control Program in Guinea for their technical and financial support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmala.2024.1469790/full#supplementary-material
References
Adeoti I. G., Cavallaro F. L. (2022). Determinants of care-seeking behaviour for fever, acute respiratory infection and diarrhoea among children under five in Nigeria. PloS One 17, e0273901. doi: 10.1371/journal.pone.0273901
Awasthi K. R., Jancey J., Clements A. C. A., Rai R., Leavy J. E. (2024). Community engagement approaches for malaria prevention, control and elimination: a scoping review. BMJ Open 14, e081982. doi: 10.1136/bmjopen-2023-081982
Bastaki H., Carter J., Marston L., Cassell J., Rait G. (2018). Time delays in the diagnosis and treatment of malaria in non-endemic countries: A systematic review. Travel Med. Infect. Dis. 21, 21–27. doi: 10.1016/j.tmaid.2017.12.002
Casella A., Monroe A., Toso M., Hunter G., Underwood C., Pillai R., et al. (2024). Understanding psychosocial determinants of malaria behaviours in low-transmission settings: a scoping review. Malar J. 23, 15. doi: 10.1186/s12936-023-04831-9
Cisse M., Camara A., Fofana A., Lama E.. (2021). Parcours du malade pour la recherche des soins contre le paludisme au niveau d’un district sanitaire. Infectious Diseases Now 51, S109–S110. doi: 10.1016/j.idnow.2021.06.248
Diallo E. M., Traore F. B., Camara B. S., Langlet A., Delamou A., Diallo O. O., et al. (2024). Analysis of care-seeking pathways and factors influencing early and appropriate care-seeking for malaria patients in the Republic of Guinea: a cross-sectional study. Malar J. 23, 273. doi: 10.1186/s12936-024-05102-x
Goshu C. J., Tafasa S. M. (2023). Determinants of delay in treatment seeking among malaria patients in public health facilities of dambi dollo and sayyo district, western Ethiopia: A facility based case control study. Open Access J. Dis. Glob Health 1, 6–20. doi: 10.21203/rs.3.rs-2655663/v1
Guinea National Malaria Control Program. (2018). Training manual on the management of malaria in Guinea (Conakry, Guinea: Guinea Ministry of Health).
Guntur R. D., Kingsley J., Islam F. M. A. (2022). Malaria treatment-seeking behaviour and its associated factors: A cross-sectional study in rural East Nusa Tenggara Province, Indonesia. PloS One 17, e0263178. doi: 10.1371/journal.pone.0263178
Guyatt H. L., Snow R. W. (2004). The management of fevers in Kenyan children and adults in an area of seasonal malaria transmission. Trans. R Soc. Trop. Med. Hyg. 98, 111–115. doi: 10.1016/S0035-9203(03)00016-6
Hammer C. C., Diallo M. D., Kann B., Sanoh F., Leno T. N., Mansare O., et al. (2024). High prevalence of asymptomatic malaria in Forest Guinea: Results from a rapid community survey. Epidemiol. Infect. 152, e1. doi: 10.1017/S0950268823001929
Humphreys D., Kalyango J. N., Alfvén T. (2021a). The impact of equity factors on receipt of timely appropriate care for children with suspected malaria in eastern Uganda. BMC Public Health 21, 1870. doi: 10.1186/s12889-021-11908-0
Humphreys D., Kalyango J. N., Alfvén T. (2021b). The impact of equity factors on receipt of timely appropriate care for children with suspected malaria in eastern Uganda. BMC Public Health 21, 1–9. doi: 10.1186/s12889-021-11908-0
INS Guinée, NMCP, DHS Program. (2022). Enquête sur les Indicateurs du Paludisme et de l’Anémie en Guinée 2021 [Internet]. (Conakry, Guinée). Available at: https://www.stat-guinee.org/index.php/publications-ins/rapports-d-enquetes.
Institut National de la Statistique. (2013). Ministère du Plan, MEASURE DHS, ICF International. INS_Enquete EDS-MICS 2012 (Conakry, Guinée). Available at: https://www.stat-guinee.org/index.php/publications-ins/rapports-d-enquetes.
Institut National de la Statistique. (2017). Recensement Général de la Population et de l’Habitat (RGPH3). Available online at: https://www.stat-guinee.org/index.php/publications-ins/rapports-d-enquetes (Accessed October 14, 2021).
Kaboré J. M. T., Siribié M., Hien D., Soulama I., Barry N., Nombré Y., et al. (2022a). Attitudes, practices, and determinants of community care-seeking behaviours for fever/malaria episodes in the context of the implementation of multiple first-line therapies for uncomplicated malaria in the health district of Kaya, Burkina Faso. Malar J. 21, 1–14. doi: 10.1186/s12936-022-04180-z
Kaboré J. M. T., Siribié M., Hien D., Soulama I., Barry N., Nombré Y., et al. (2022b). Attitudes, practices, and determinants of community care-seeking behaviours for fever/malaria episodes in the context of the implementation of multiple first-line therapies for uncomplicated malaria in the health district of Kaya, Burkina Faso. Malar J. 21, 155. doi: 10.1186/s12936-022-04180-z
Kassam R., Collins J. B., Liow E., Rasool N. (2015). Caregivers’ treatment-seeking behaviors and practices in Uganda-A systematic review (Part II). Acta Trop. 152, 269–281. doi: 10.1016/j.actatropica.2015.07.029
Kassile T., Lokina R., Mujinja P., Mmbando B. P. (2014). Determinants of delay in care seeking among children under five with fever in Dodoma region, central Tanzania: A cross-sectional study. Malar J. 13, 1–10. doi: 10.1186/1475-2875-13-348
Kombate G., Cakpo G. E., Azianu K. A., Labité M. A., van der Sande M. A. B. (2022). Care-seeking behaviour among febrile children under five in Togo. BMC Public Health 22, 2107. doi: 10.1186/s12889-022-14550-6
Mburu C. M., Bukachi S. A., Shilabukha K., Tokpa K. H., Ezekiel M., Fokou G., et al. (2021). Determinants of treatment-seeking behavior during self-reported febrile illness episodes using the socio-ecological model in Kilombero District, Tanzania. BMC Public Health 21, 1075. doi: 10.1186/s12889-021-11027-w
Mpimbaza A., Ndeezi G., Katahoire A., Rosenthal P. J., Karamagi C. (2017). Demographic, socioeconomic, and geographic factors leading to severe malaria and delayed care seeking in Ugandan children: A case-control study. Am. J. Trop. Med. Hyg. 97, 1513–1523. doi: 10.4269/ajtmh.17-0056
Negatou M., Ouedraogo M., Donnen P., Paul E., Samadoulougou S., Kirakoya-Samadoulougou F. (2021). Care-seeking for fever for children under the age of five before and after the free healthcare initiative in Burkina Faso: evidence from three population-based surveys. Risk Manag Healthc Policy. 14, 2065–2077. doi: 10.2147/RMHP.S297983
Nkoka O., Chuang T. W., Chen Y. H. (2019). Multilevel analysis of factors associated with treatment-seeking behaviors among caregivers with febrile children in Malawi. Am. J. Trop. Med. Hyg. 100, 1454–1465. doi: 10.4269/ajtmh.18-0900
Omale U. I., Oka O. U., Okeke I. M., Azuogu B. N., Alo C., Madubueze U. C., et al. (2021a). Demand for malaria rapid diagnostic test, health care-seeking behaviour, and drug use among rural community members with fever or malaria-like illness in Ebonyi state, Nigeria: a cross-sectional household survey. BMC Health Serv. Res. 21, 857. doi: 10.1186/s12913-021-06865-8
Omale U. I., Oka O. U., Okeke I. M., Azuogu B. N., Alo C., Madubueze U. C., et al. (2021b). Demand for malaria rapid diagnostic test, health care-seeking behaviour, and drug use among rural community members with fever or malaria-like illness in Ebonyi state, Nigeria: a cross-sectional household survey. BMC Health Serv. Res. 21, 1–15. doi: 10.1186/s12913-021-06865-8
Oyekale A. S. (2015). Assessment of Malawian mothers’ Malaria knowledge, healthcare preferences and timeliness of seeking fever treatments for children under five. Int. J. Environ. Res. Public Health 12, 521–540. doi: 10.3390/ijerph120100521
Programme National de Lutte contre le Paludisme. (2023). “Plan stratégique de lutte contre le paludisme 2023-2027,” (Ministère de la santé et de l’hygiène publique, Conakry, République de Guinée). Available at: https://pnlp-guinee.org/documentations/.
Romay-Barja M., Cano J., Ncogo P., Nseng G., Santana-Morales M. A., Valladares B., et al. (2016). Determinants of delay in malaria care-seeking behaviour for children 15 years and under in Bata district, Equatorial Guinea. Malar J. 15, 187. doi: 10.1186/s12936-016-1239-0
Sonkong K., Chaiklieng S., Neave P., Suggaravetsiri P. (2015). Factors affecting delay in seeking treatment among malaria patients along Thailand-Myanmar border in Tak Province, Thailand. Malar J. 14, 3. doi: 10.1186/1475-2875-14-3
Sunguya B. F., Mlunde L. B., Ayer R., Jimba M. (2017). Towards eliminating malaria in high endemic countries: the roles of community health workers and related cadres and their challenges in integrated community case management for malaria: a systematic review. Malar J. 16, 10. doi: 10.1186/s12936-016-1667-x
Venkatesan P. (2024). The 2023 WHO World malaria report. Lancet Microbe 5, e214. doi: 10.1016/S2666-5247(24)00016-8
Workineh B., Mekonnen F. A. (2018). Early treatment-seeking behaviour for malaria in febrile patients in northwest Ethiopia. Malar J. 17, 406. doi: 10.1186/s12936-018-2556-2
World Health Organization. (2022). WHO guidelines for malaria, 3 June 2022 (World Health Organization). Available at: https://apps.who.int/iris/bitstream/handle/10665/354781/WHO-UCN-GMP-2022.01-Rev.2-eng.pdf?sequence=1.
World Health Organization. (2023). World malaria report 2023 (Geneva: World Health Organization (WHO)). Available at: https://iris.who.int/bitstream/handle/10665/374472/9789240086173-eng.pdf?sequence=1.
Keywords: malaria, associated factors, treatment delays, health facilities, Guinea
Citation: Diallo EM, Kourouma K, Diakite N, Diallo A, Blanquet M, Toure A, Gerbaud L and Camara A (2024) Factors affecting treatment delays among malaria patients presenting at health facilities in Guinea, 2022–2023. Front. Malar. 2:1469790. doi: 10.3389/fmala.2024.1469790
Received: 24 July 2024; Accepted: 14 October 2024;
Published: 12 November 2024.
Edited by:
Andre Lin Ouedraogo, Bill and Melinda Gates Foundation, United StatesReviewed by:
Joris Losimba Likwela, University of Kisangani, Democratic Republic of CongoKassoum Kayentao, University of Bamako, Mali
Copyright © 2024 Diallo, Kourouma, Diakite, Diallo, Blanquet, Toure, Gerbaud and Camara. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elhadj Marouf Diallo, ZWxoYWRqbWFyb3VmZEB5YWhvby5mcg==
 Elhadj Marouf Diallo
Elhadj Marouf Diallo Karifa Kourouma
Karifa Kourouma Nouman Diakite5
Nouman Diakite5 Laurent Gerbaud
Laurent Gerbaud