- 1School of Epidemiology and Public Health, Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada
- 2Bruyere Research Institute, Ottawa, ON, Canada
- 3K’Olo Vanona Association, Antananarivo, Madagascar
- 4National Institute of Public and Community Health, Ministry of Public Health, Antananarivo, Madagascar
- 5NTD Programme, Disease Control Unit, Public Health Division, Ghana Health Service, Accra, Ghana
- 6NTD Programme, Ministry of Public Health, Antananarivo, Madagascar
- 7Institute of Health Research, University of Health and Allied Sciences, Ho, Volta Region, Ghana
- 8Bridges to Development, Vashon, WA, United States
- 9Bridges to Development, Geneva, Switzerland
- 10Unlimit Health, London, United Kingdom
Women and girls who have been infected with the blood fluke Schistosoma haematobium can experience the chronic form of urogenital schistosomiasis, called female genital schistosomiasis (FGS). Some FGS symptoms resemble sexually transmitted infections. As a result, women and girls seeking treatment are often misdiagnosed and stigmatized. The FGS Accelerated Scale Together (FAST) Package project implemented a holistic approach to address FGS combining proven interventions in training, mass drug administration, diagnosis, and treatment as well as community awareness to address FGS in four selected districts in Ghana and Madagascar. The FAST Package was supported by an FGS National Committee who provided guidance on integration at the national level. Using an implementation research design, researchers worked closely with government counterparts in the programs for neglected tropical diseases in both countries. Baseline cross-sectional surveys and qualitative methodologies collected information on schistosomiasis and FGS awareness, experience with health seeking behaviors and knowledge of schistosomiasis prevention amongst community members and teachers. FAST Package interventions included healthcare provider training delivered in online and in person formats; development of an Educators’ booklet to support schistosomiasis/FGS awareness creation among teachers, healthcare providers and community members; suspected FGS case detection; and advocacy for the provision of praziquantel in the primary health care system. Endline results included a cross-sectional survey and qualitative methodologies amongst community members and teachers, including Photovoice for women of reproductive health age exposed to FGS. This paper presents a description of the FAST Package project, the value of its holistic approach, and selected results from both countries. It discusses the lessons learnt highlighting some of the challenges and opportunities for integration within the health system.
Introduction
Schistosomiasis is a parasitic disease caused by blood flukes that is prevalent in tropical and sub-tropical countries, particularly in areas with inadequate sanitation and poor access to safe drinking water. It has been reported in 78 countries worldwide, with the urogenital form of the disease found in Africa, the Middle East, and Corsica (1). The urogenital form is caused by infection with Schistosoma haematobium (1). Infection occurs when the larval forms of the parasite, released by freshwater snails, penetrate the skin of an individual who has contact with the snail-infested water. The larvae eventually mature into adult worms, which live in blood vessels where after mating, the female worm releases its eggs. Some eggs are released in urine or feces to continue the life cycle, while others get trapped in body tissues, causing immune reactions and progressive organ damage (1). Transmission continues when an infected person passes excreta containing parasite eggs into the freshwater sources, which later hatch in water and are taken up by the freshwater snails.
Evidence has shown that differences between males and females exist for schistosomiasis in terms of vulnerability, exposure, and access to treatment (2). The gender role of females as it relates to performing household chores such as fetching water for the family, washing clothes and dishes, and bathing children puts them at risk of infection with Schistosoma haematobium (1, 3) while for boys, activities like swimming, fishing and washing vehicles will influence their risk.
In many countries, urogenital schistosomiasis is widely regarded as a boy’s disease (4) due to the visible sign of hematuria which boys detect more easily than girls. This misconception prevents awareness about the chronic manifestations of untreated Schistosoma haematobium infection in women and girls (4, 5). In females, Schistosoma haematobium infection can cause a gynecological disease called Female Genital Schistosomiasis (FGS). FGS presents with vaginal bleeding, nodules in the vagina, genital lesions, vaginal discharge, and pain during sexual intercourse, and could result in ectopic pregnancy, miscarriage, sub-fertility, infertility, spontaneous abortion, and premature delivery (1, 6, 7). An estimated up to 56 million women and girls are affected by FGS (7) and it has been called the “sexual and reproductive health issue you’ve probably never heard of” (8). Despite its likely prevalence across Sub-Saharan Africa, awareness of FGS and its associated sequelae at the community level and health system is lacking; most medical textbooks do not mention FGS and global and national policymakers have largely overlooked the disease. Hence women and girls with FGS are often poorly diagnosed and misdiagnosed as having sexually transmitted infections by frontline healthcare providers, leading to stigma, discrimination, unnecessary investigations, and multiple health care visits (4, 6, 7, 9).
FGS is considered as a risk factor for HPV and HIV due to the immunological and pathological changes associated with the disease (6). Studies in sub-Saharan Africa have shown that women suffering from FGS are at a three-fold increased risk of HIV infection (7, 10, 11). African women carry a disproportionate global burden of cervical cancer and HIV infection (12, 13). There is increasing evidence that controlling one of these three infections (FGS, HIV, HPV) may decrease the risk of vulnerability and unwanted outcomes for the two others and improve women’s overall reproductive health (6, 7, 9). Each disease has a proven preventive intervention, from praziquantel treatment for FGS, pre-exposure prophylaxis, and anti-retroviral therapy for HIV and HPV vaccines for cervical cancer (9, 14).
As recommended by UNAIDS, national programs should address the gender inequalities that increase the vulnerability of women and girls in Sub-Saharan Africa to FGS, HIV, and cervical cancer, through a holistic, integrated, and multisectoral programming (7). For example, the health care providers responsible for prevention and screening programs should consider the higher rates of cervical cancer amongst people living with HIV and the risks of acquiring HIV associated with FGS (2, 6, 7). Age-appropriate management of schistosomiasis, cervical cancer screening programs, family planning, and other sexual and reproductive programs are not currently linked. Without breaking down the siloed approaches of sexual and reproductive health (SRH) programming, adapting and integrating diagnostic and treatment protocols for HIV, HPV, and STIs to include FGS and multifaceted approach at all levels, FGS cannot be effectively addressed (7, 15). Integrating FGS, HIV, and cervical cancer with existing sexual and reproductive health programs can improve the health outcomes of girls and women in Africa (14). The policy framework is already in place to integrate FGS into the primary health care system and sexual and reproductive health services. Sustainable Development Goal 3 seeks to ensure universal access to sexual and reproductive health, including “information and education, and integration of reproductive health into national strategies and programs by 2030” (7). The WHO 2030 NTD roadmap calls for mainstreaming and greater integration of NTD approaches into the national health system (1). FGS represents a unique global health challenge in terms of its scale, neglect, and positive impact if addressed. Global policymakers have increasingly advocated for FGS action as a gender, human rights, development, and reproductive health issue requiring urgent attention (2, 16, 17).
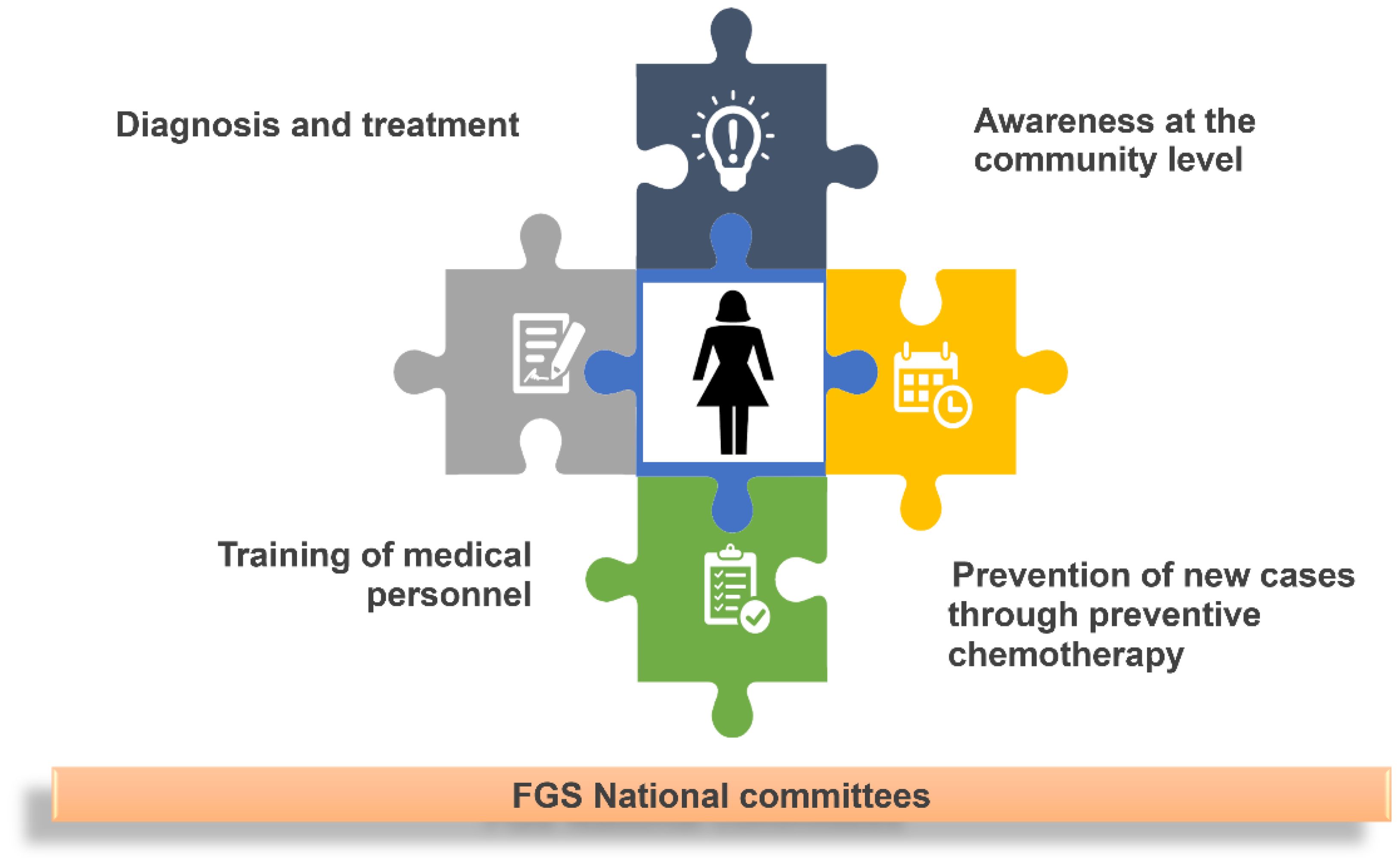
To address the burden of FGS in girls and women in Ghana and Madagascar, the FGS Accelerated Scale Together (FAST) Package or the FAST Package was launched in July 2020 to combine proven interventions that have been shown independently to improve detection and clinical outcomes while supporting the uptake and demand for preventive chemotherapy through mass drug administration (MDA) to prevent infection. These activities were supported by the establishment of a FGS National Advisory Committee to increase communication and collaboration about FGS with the longer-term goal of integrating FGS management into existing sexual and reproductive health, clinical training, and care. The FAST Package covers the life course of a woman, from prevention of new infections with schistosomiasis and new cases of FGS to the diagnosis and treatment for existing FGS cases and, finally, treatment for symptoms of complications due to FGS as a woman ages. The FAST Package addresses the issue of FGS at the individual, community, and health system levels (See https://fastpackage.org/). Each component of the FAST Package works together to provide a holistic response (See Figure 1).
The FAST Package project aimed to:
1. Increase community members’ knowledge about FGS and its impact on women and girls.
2. Prevent new infections in children and young girls with schistosomiasis by promoting annual mass drug administration.
3. Increase the capacity of medical personnel to diagnose and treat FGS.
4. Improve diagnosis and treatment of FGS.
5. Support the National NTD program to integrate FGS into existing health programming at the Ministry of Health and partners.
The FAST Package combines a diverse partnership of global and national partners. The project was supported by Grand Challenges Canada from June 2020 to September 2022. Grand Challenges Canada is funded by the Government of Canada and is dedicated to supporting Bold Ideas with Big Impact®. Match funding for the FAST package was supported by the Coalition for Operational Research on NTDs, Merck Global Health Institute, WHO Expanded Special Project for the Elimination of Neglected Tropical Diseases, and Unlimit health (formerly the Schistosomiasis Control Initiative Foundation). This unique partnership allowed greater visibility for the FAST Package and allowed the learnings from the project to be transferred to a global level.
The paper describes some of the results and key learnings related to the project objectives, including a discussion of the challenges associated with implementation and lessons learned.
Materials and methods
Study design
The FAST Package is an implementation research study using mixed methods to improve the implementation and delivery of FGS interventions in selected sites. One of the foundational aspects of implementation research is to link research and practice through a close collaboration between researchers and program personnel. Through continuous feedback loops, data from the research is presented to the government program for input and adaptation (18). The FAST Package had three distinct phases: a baseline assessment, an interventional phase, and an endline assessment. At the baseline and endline phases, cross-sectional surveys were employed with community members and teachers. Using a concurrent mixed methods study design (19), in-depth interviews and focus group discussions were carried out at the same time as the cross sectional surveys. In the endline phase, photovoice was added to selected focus group discussions with women of reproductive health age.
Study setting
The FAST Package was carried out in Ghana and Madagascar. These two countries were selected based on schistosomiasis endemicity and on the willingness of the Neglected Tropical Diseases program managers to see FGS addressed in an integrated and sustained manner. Study sites included the Weija and North Tongu Districts in Ghana and the Morondava and Sakaraha Districts in Madagascar. All selected districts had a reported schistosomiasis prevalence rate of >50%.
In Ghana, more than 50% of the population is under 25 years, and about 24% are 25-54 years. Over 95% of Ghanaian children are enrolled in school. All regions in Ghana are endemic to schistosomiasis. However, there are specific regions that have a prevalence rate of over 50% (high-risk regions), and these include the Volta, Greater Accra, Eastern, and parts of the northern part of the country.
Weija district is one of the FAST Package districts in the Greater Accra Region, Ghana. It has a population of about 213,674 (City population, 2021) and is near the Weija Dam, which the Government of Ghana created to supply piped water and support fisheries and irrigation activities. The dam has provided an ideal situation for schistosomiasis transmission, with early prevalence ranging from 25 to 89.4% in 1991 - 1992 in areas around the dam (20). A 2019 study in 202 pupils found 135 were positive for schistosome eggs (including both S. mansoni and S. haematobium) in a peri-urban community along the Weija dam (21). North Tongu district, the second FAST Package site in Ghana, is in Volta Region. With a population of 110,891 (City Population, 2021), North Tongu is bounded by Lake Volta to the west, Akatsi south, and Ho Municipal District to the east. Lake Volta provides water transportation routes, generates electricity for the Volta River Authority and is a primary resource for fish farming and irrigation in the region.
Madagascar is an island country in the Indian Ocean off the coast of East Africa. Madagascar has 114 districts, and is predominantly populated by people belonging to the Malagasy ethnolinguistic group. Madagascar has an estimated population of about 25 million, with more than 60% below the age of 24 years and 32% within 25-54 years (49.3% males and 50.7% females) (22). About 64% of the Madagascar population are literate.
Morondava District located in the Menabe Region is one of the FAST Package districts in Madagascar. It is found in the delta of the Morondava Region with a population of about 150,531. It has a reported schistosomiasis prevalence rate of 79% and the highest incidence of HIV in Madagascar. Sakaraha District is in the Atsimo-Andrefana Region, Madagascar. It has a population of 150,356 and a schistosomiasis prevalence rate of 82% (22). Mining activities, including river mining are common in Sakaraha.
Questionnaire and qualitative topic guide development
The questionnaires and topic guides were designed to explore the existing sociocultural context, awareness, knowledge, perception and practices, health-seeking behaviors, and access to preventive chemotherapy (Praziquantel or PZQ) for schistosomiasis and FGS. Research instruments were developed based on known influences found in recent literature on FGS. The in-depth interview, FGD, and photovoice topic guides were developed based on experience from a previous FGS qualitative study in Ghana (4, 23). Questionnaires were modified slightly from the baseline at the end-line, to assess the change in awareness, knowledge, perception and practices, health-seeking behaviors, and access to preventive chemotherapy (PZQ) for schistosomiasis and FGS following the delivery of FGS interventions initiated by the FAST Package.
Research instruments were developed in English and translated into French and Malagasy by local and English language specialists. After that, the local language versions were given to another expert in the same local and English language to translate the instruments back into English. This back translation was done to ensure the accuracy of the translation. The translations were given to a panel of expert local language speakers of the study location for validation. The translation exercise ensured adequate comprehension of the instruments’ content and enabled the enumerators to ask the questions the same way without distorting their original meanings. To test the understandability of the research tools, the questionnaire was piloted to a small sample of individuals, and feedback was used to revise and ensure the final version was clear and language appropriate.
Data collection
The FAST Package adopted the modified EPI population proportion sampling frame (24) for the community survey for baseline and end-line assessments. For the community members’ survey, 30 (clusters) of 14 households per district per country (n=420 per district at baseline and n=420 at endline) were identified. The thirty (30) clusters within each district were selected with probability proportionate to the most recent census estimate of the community population size by systematic selection from a list of cumulative population sizes. At the village level, the enumerator team either selected 14 households (for one cluster) randomly from an available community list of households or the enumerator team went to the center of the village, threw a pen onto the ground, and walked in the direction the pen pointed to in selecting the first house. If one village has more than one cluster, the starting points for each random walk differ. Only one community member (18 years and above) per household was interviewed. Enumerators made a list of all eligible household members and randomly selected one person to participate in the survey. For the teachers’ survey, 5 teachers (18-60 years) were purposively sampled in each of the thirty clusters/communities selected for the community-based survey (n=150 teachers per district).
The in-depth interviews (IDI) occurred at the same time as the surveys in the same selected districts with 4 teachers and 1 district health director/medical officer per district per country during baseline and 4 teachers, 1 district health director/medical officer, 8 clinicians and 4 parents per district per country at endline. The study participants for these in-depth interviews were 18 years and above and selected using a purposive sampling frame. The focus group discussions (FGD) were conducted using a purposive sampling frame with three groups of women of reproductive age (18-49 years) and one group of men (18-60 years) per district, per country at baseline and endline. The aim of the qualitative research was to understand cultural beliefs and practices concerning schistosomiasis and FGS.
At the endline assessment, photovoice with a group of women of reproductive age using photography and group dialogue was used to deepen the understanding of the issues women face with FGS within their communities. The photovoice approach explored their feelings, views, and perspectives about schistosomiasis and FGS using pictures taken of objects or images near the meeting room/area where the discussion took place. Photos were shared with the group participants for discussion.
In all study districts, research partners selected and trained locally based enumerators on the methodology for the survey and qualitative guides. Quantitative data was collected using the Redcap platform (Version 10.5.1.).
Data management and analysis
Quantitative data generated through the community and teachers’ surveys were managed through the REDCap platform, exported to Excel spreadsheet, Statistical Package for Social Sciences (SPSS) version 26, and STATA 14 readable formats, and analyzed using descriptive statistics. The results obtained were expressed in simple percentages, tables, and charts. Chi-square was used to test for association between categorical variables at 0.05 alpha level. Item-by-item pre-post comparisons were done by running cross-tabulations variables pre-vs. post interventions. Multiple logistic regression was carried out. All analyses were done at a 5% level of significance and a 95% confidence interval.
For the qualitative data, recorded interviews were transcribed verbatim in the local language and then translated into English and French. The researchers read through each transcript, recording emergent themes in an Excel matrix. NVivo 12 software was used for coding and analysis of the interview transcripts. The coding process followed an integrated approach, making it deductive and inductive. All interviewees were assigned anonymous numbers so that no identifier could be used to identify respondents to maintain confidentiality.
Project intervention phase
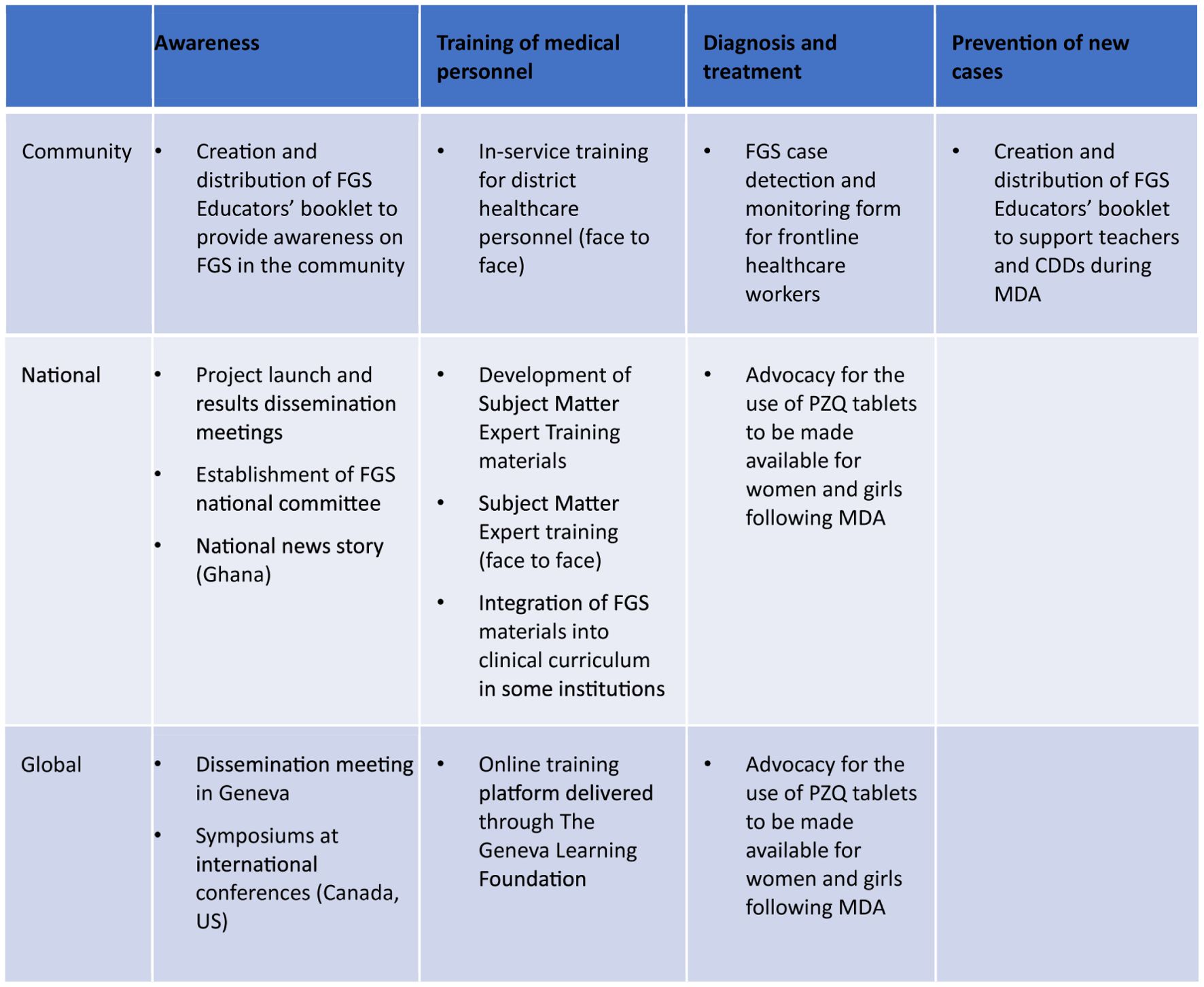
The FAST Package utilized the results and feedback from the baseline assessments to inform the interventional phase. The team engaged appropriate stakeholders at the global, national and district levels to design, test, implement, and monitor interventions. FAST Package interventions are described in Figure 2.
Ethics statement
All research activities were covered under the ethical approvals of Bruyère REB Approval (M16-20-061), University of Ottawa (H-08-21-7345), University of Health and Allied Sciences Ghana (UHAS-REC A.5[4] 20-21), Ghana Health Service (GHS-ERC 003/04/21), and Comité d’Evaluation Ethique pour la Recherche Biomédicale, INSPC Madagascar (013/2021-CEER/INSPC).
Results
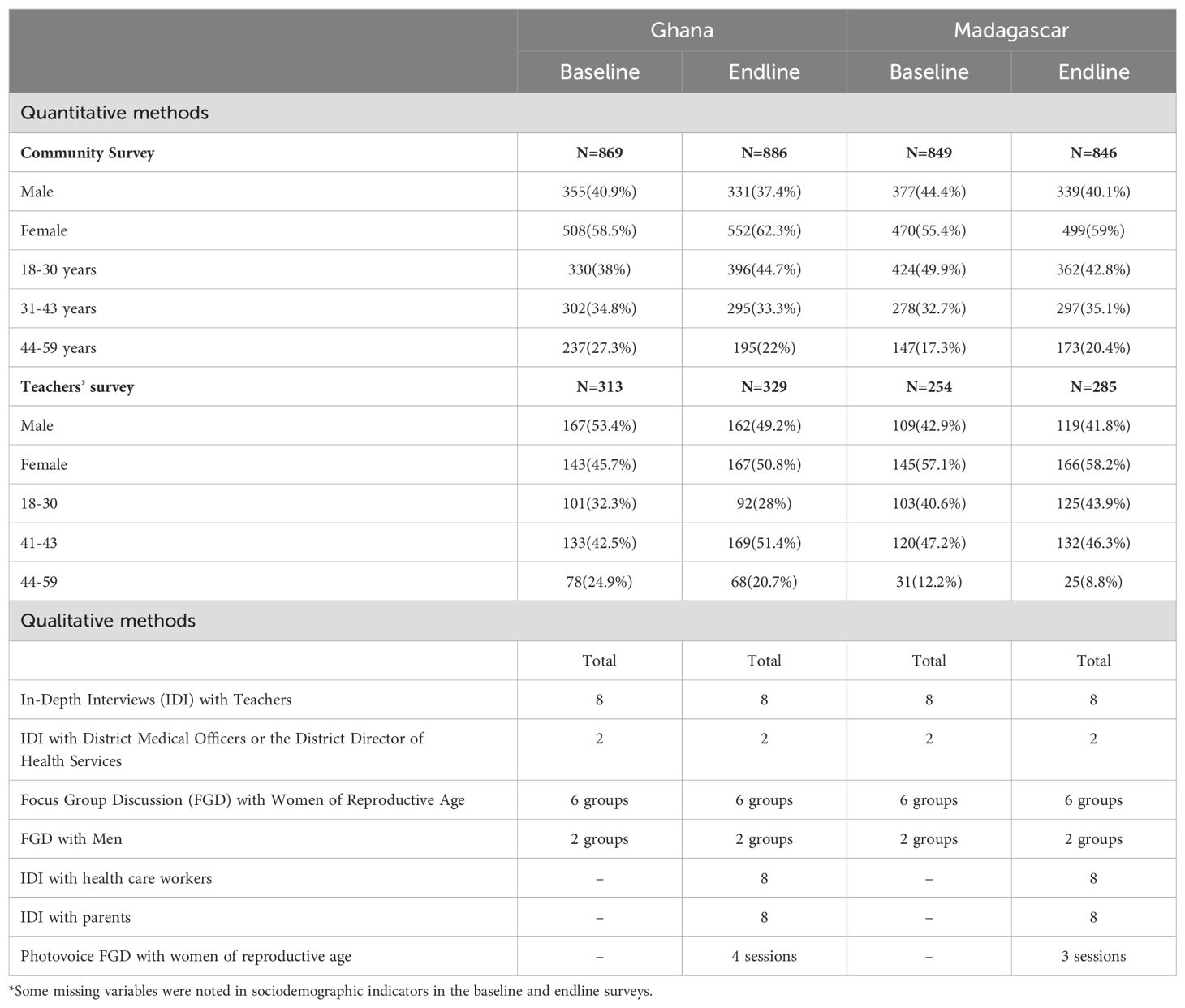
This section highlights the summary of data collected during the project and the high-level findings relating to the different components of the FAST package across the baseline assessments, interventional phase, monitoring, and endline assessments (Table 1).
Results are described along the four components of the FAST Package: awareness, prevention of new cases, training of medical personnel and diagnosis and treatment and the FGS national committee.
Awareness of schistosomiasis and FGS in the community
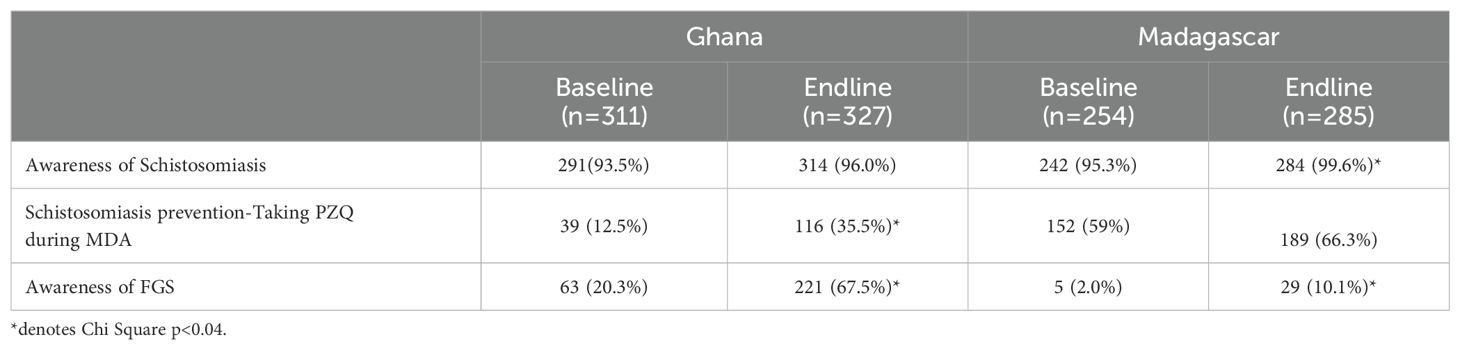
As illustrated in Table 2, there is higher awareness about schistosomiasis amongst community members in both sites, compared to awareness about FGS. This was consistent across all rounds of the surveys.
All communities included in the sample are located close to water sources where schistosomiasis transmission has been ongoing for many years. As such, participants noted the disease in their communities during the qualitative interviews, specifically mentioning the presence of urine in blood.
“We are all aware and have experienced Schisto in this community. It is because of the river that we use for our activities.” (FGD, Men, Vome, Ghana)
“Both boys and girls get it. But it is easy to see it in the boys than in the girls.” (FGD, Men, Tomefa, Ghana)
“My experience with it is that it is more prevalent in the boys than the girls. For obvious reasons, the boys go and swim more in the river than the girls, so it is more prevalent in the boys. I have seen some cases of schistosomiasis in boys in this school.” (IDI, Male teacher, North Tongu, Ghana)
“I know bilharzia by this very name, and what I know of its manifestations is that it causes pain in the lower abdomen, stomach aches and the end of the urine is blood.” (FGD, female 29-49 years, Morondava, Madagascar)
While awareness of schistosomiasis could be considered high, some people still were not aware about the disease, despite having heard about the mass drug administration through schools, as illustrated in the quote below.
“I have never heard of bilharzia. There has been some sensitization on the polio vaccine, for example, but I have not heard anything else except during the distribution of anti-bilharzia drugs to schools.” (FGD, Men, Morondava, Madagascar)
Compared to schistosomiasis awareness, levels of FGS awareness were lower in all study sites. In Ghana, levels of FGS awareness were higher than in Madagascar which may reflect previous research activities in the country prior to the start of the FAST Package (25). Some respondents knew of the symptoms of FGS, as illustrated here.
“In my opinion, the manifestations are not the same, if it’s a little boy it’s as we mentioned earlier, pain in the lower abdomen and he urinates blood, but if it’s a girl I thought I already heard that her vagina was itchy, with sores, plus the presence of a liquid that runs, and when he was taken to a doctor, he said that it was bilharzia.” (FGD, female 29-49 years, Morondava, Madagascar)
Despite relatively low awareness about FGS across the community, women in the study sites were aware of the symptoms caused by schistosomiasis and FGS. In the FGDs with women of reproductive health age, photovoice was employed to explore the impact of suspected FGS felt by women. The findings from these sessions revealed that the impact of FGS symptoms on women and girls is stigmatizing and discriminatory.
For example, in Madagascar, study participants used dried leaves to explain the stress related to FGS. One of them stated that “dried leaves are withered and ugly.” Another woman mentioned that “dried leaves can be relatable to poor health, vulnerability as well as the shame of showing ourselves to others” (Photovoice, Women, 29-49 years, Morondava, Madagascar) (Figure 3).
In Ghana, one study participant used an abandoned building to explain social exclusion resulting from FGS. She stated explaining the image in Figure 4:
“As a woman, when you start urinating blood, and you do not treat it, it comes with a whole lot of complications. An example is infertility, and when you are infertile, there is a problem, you would be neglected like this building, and there wouldn’t be any hope for you.’’ (Photovoice, young women, 19–29 years, North Tongu, Ghana)
Awareness of schistosomiasis and FGS amongst teachers
Teachers had higher levels of awareness about schistosomiasis than community members (Table 3) with over 90% of the teachers surveyed in Ghana and Madagascar reporting that they were aware of schistosomiasis. This increased in the endline surveys carried out in both countries.
Regarding knowledge about schistosomiasis prevention, 12.5% (n=311) and 59% (n=254) in Ghana and Madagascar, respectively, knew that taking praziquantel during MDA could prevent schistosomiasis. This increased at endline to 35.7% in Ghana (n=327) and 66.3% in Madagascar (n=285).
“Schistosomiasis is contracted and transmitted through water; it enters through pores in the skin and reaches the blood vessel and ends up reaching the bladders where it lodges so that when the person urinates, they urinate blood.” (IDI- Male Teacher, Morondava, Madagascar)
In Ghana, the increased knowledge of FGS among teachers may be the result of the Schistosomiasis/FGS Educators booklet developed by the FAST package team in collaboration with NTD programs in Ghana and Madagascar. The primary target for distribution of the booklet was teachers who were involved in school-based MDA. The booklet was co-designed with the national NTD programs in both countries, the FGS national committee in Ghana and with the health promotion unit at the Ministry of Health in Madagascar. Over 3150 hard copies of the booklet were distributed within the study districts and at the national level. The impact of the booklet was detected in Ghana where the distribution and use of the booklets occurred prior to the endline surveys. In Madagascar, distribution was delayed due to various factors resulting in less time in between distribution and the endline assessment. In Ghana, teachers (n=327) who indicated the FGS booklet as a source of information about FGS awareness had 3.91 times (OR=3.91; p-value=0.003 and CI= 1.57-9.75) greater odds of sensitizing people about FGS than those who did not indicate the booklet. Furthermore, community members (n=882) who were aware of the FGS booklet were found to have 3.84 times (OR=3.84; p-value =0.000, CI=2.15-6.84) higher odds of being aware of FGS relative to those who were not aware of the FGS booklet. One teacher in Ghana noted:
“I have the FGS booklet. I show the images on it to the school children. I educate them that this book was brought from Ho and we are supposed to use it to teach them daily…’’ (IDI, Teacher, North Tongu, Ghana)
Prevention of new cases of FGS
The FAST Package did not provide preventive chemotherapy to communities in the study districts. Rather, by working closely with the national NTD programs, the project team supported awareness raising activities that promoted uptake of Praziquantel during the school-based MDA. Due to the constraints brought by the COVID-19 pandemic, the MDA schedules in both countries were disrupted during the project timeline (2020-2022). As a result, the intention of the FAST Package to roll out promotional materials prior to MDA was not easily realized.
Furthermore, the timing of the MDA in Madagascar occurred during a period of food insecurity and drought. As children must eat prior to taking PZQ, this reportedly affected uptake of treatment. The challenge of taking PZQ in a period of food insecurity is illustrated by the following quotes:
“The negative side of this medication is that the teacher will not provide bread. The parents are all in trouble. There is already the fact of giving tea to the child by the parents at home, so the children are hungry before taking the medicine, and they faint! The tea given to him is not enough, because he has not eaten before.” (FGD Morondava female 29-49 years)
“I have had students who have vomited, after taking the medicine, they have vomited and felt dizzy, but this is due to lack of food and not the medicine.” (FGD Morondava female 29-49 years)
Across all study sites in both rounds of surveys, more male members of the household were reported to have taken PZQ during the last MDA round than female members of the household (Figure 5). The largest difference in Ghana was in the Weija District endline survey where 90.39% of respondents reported male members in their household took the MDA within the last 12 months compared to 37.25% of respondents reporting female household members. In Madagascar, the difference was particularly notable in Morondava at baseline, 83.15% of participants reported male household members versus 64.04% of respondents noted female household members.
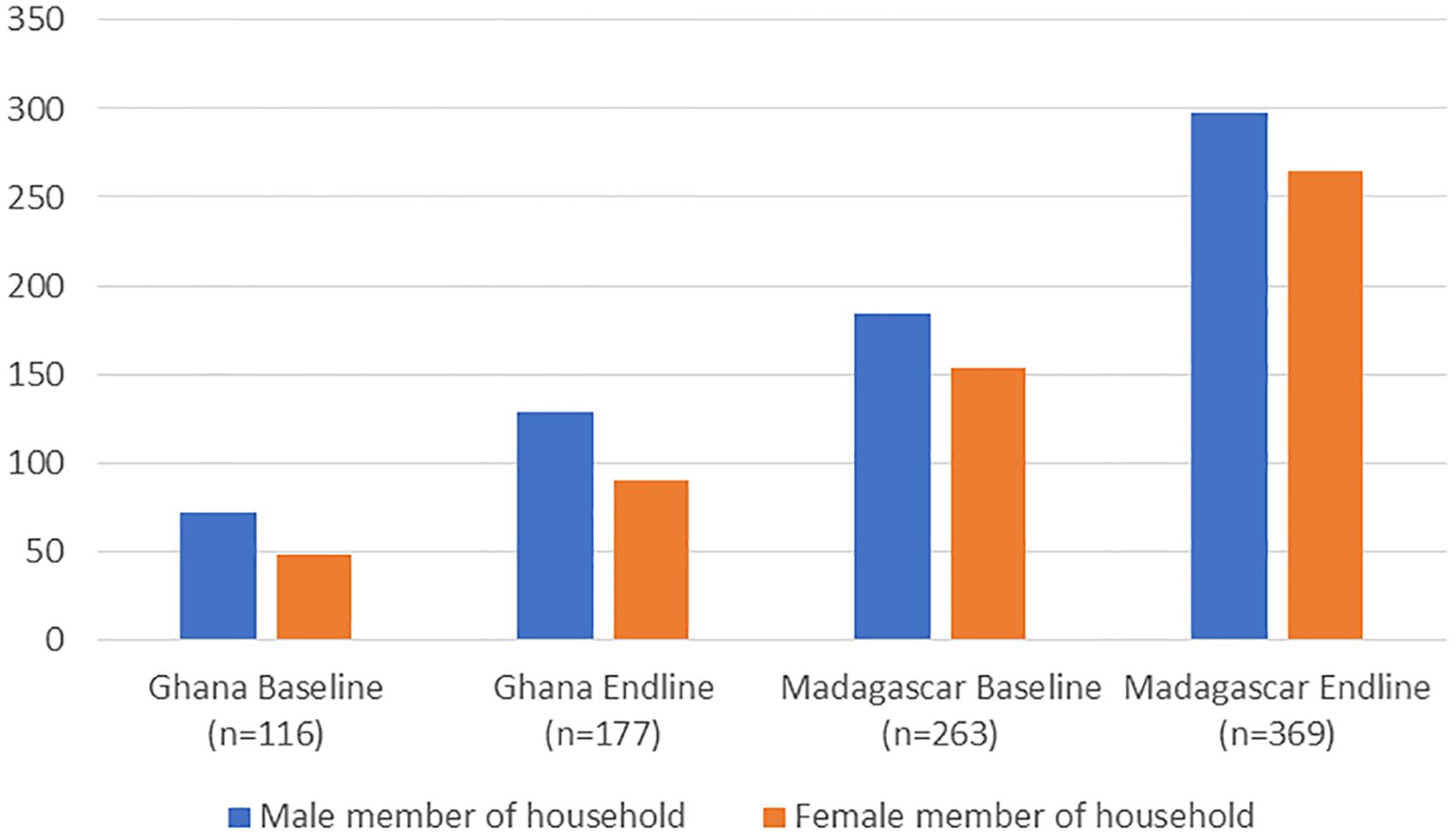
Figure 5. Household members reported to have taken schistosomiasis MDA within the last 12 months. Male member of household includes:son/brother/nephew/male cousin; female member of household includes: daughter/sister/niece/female cousin; multiple responses possible; n refers to the total number of participants responding to the question.
Training of healthcare providers/professionals
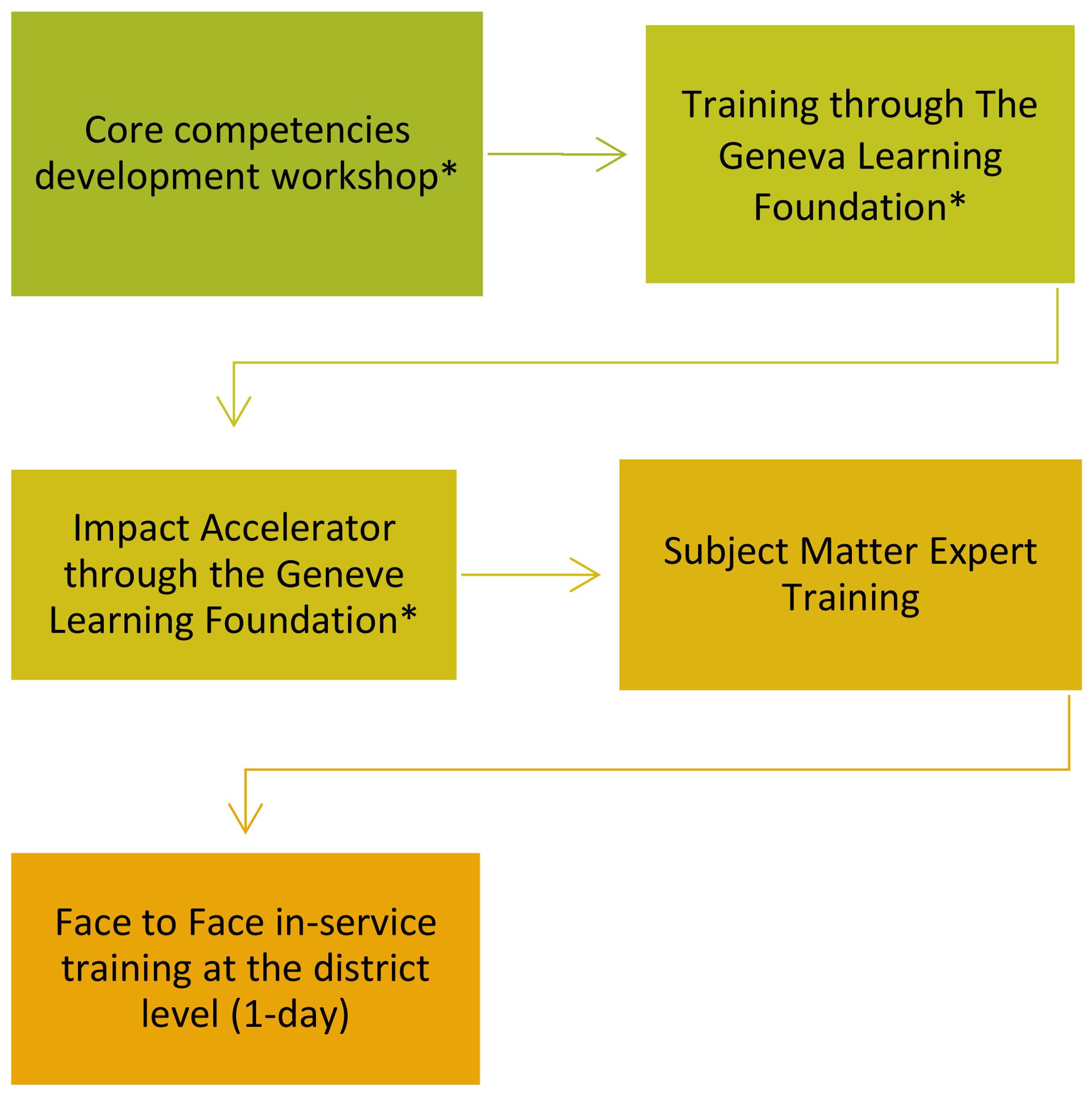
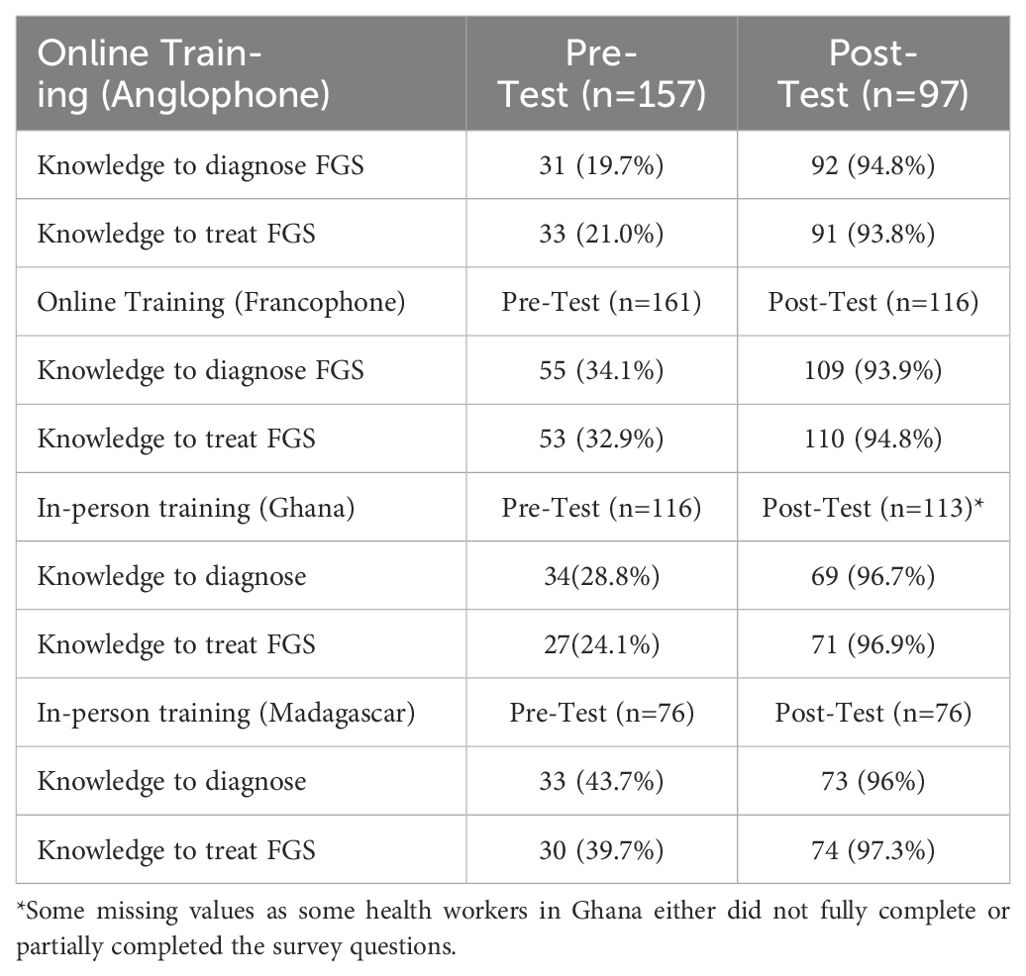
One of the objectives of the FAST package approach is to increase the capacity of healthcare personnel to prevent, diagnose, treat, refer suspected FGS cases, record, and integrate FGS into their clinical practice to improve women’s reproductive health (See Figure 6). To achieve this aim, the FAST package conducted an FGS online training for healthcare professional in Anglophone and Francophone countries in sub-Saharan Africa. The training was led by Bridges to Development in collaboration with the Geneva Learning Foundation (TGLF) and was aligned with the FGS core competencies (6). These core competencies were developed at the start of the FAST Package project through a virtual interactive workshop conducted by Bridges to Development and TGLF in close collaboration with the World Health Organization (WHO) Department of NTDs. The unique delivery of the FAST Package online training allowed for cross-border collaboration and peer-to-peer learning for learners. The training allowed for the participation of a wide variety of learners from OB/GYNs to community health workers due to the self-nomination to participate in the training. This variety demonstrated the range of healthcare professionals that have a role to play in the diagnosis, treatment, and prevention of FGS. Following the online training, an in-person training workshop was conducted at the national level in Ghana and Madagascar to create subject matter experts (SMEs). Where possible, individuals who had been involved with the online training were invited to further deepen their knowledge. In total the FAST Package virtually trained 504 multi-disciplinary healthcare professionals in more than 24 anglophone and francophone countries and 262 healthcare providers in a face-to-face format in both project sites. In addition, the FAST package created 26 FGS Subject Matter Experts in Ghana and 28 SMEs in Madagascar, comprising obstetricians/gynecologists, doctors, nurses, midwives, and health information officers.
The baseline and post-training survey analysis for the online and in-person trainings (Table 4) showed an increase in knowledge to diagnose and treat FGS cases among those who completed the course. Regardless of the delivery format of the training, healthcare workers expressed their appreciation to learn about FGS, many stating that they had never heard of the condition, despite having seen it clinically in their practices. One midwife in Ghana said, ““My experience of the workshop was wonderful. At the beginning of the workshop, I was just wondering how in my 29 years of nursing and midwifery practice, I never heard of FGS and perhaps could have been a victim without knowing, particularly being a rural dweller or failed to suspect a client of FGS.”
One key component of the training in both the online and in-person platforms was the creation of action plans. Participants created action plans outlining tangible and practical ways to address FGS within their existing budget and personnel capacity. These activities included community sensitization, training for colleagues on FGS among others. A total of 213 action plans were developed during the online training and 110 action plans during the in-person training workshops. Participants received feedback on the action plans from their peers, further refining their ideas. Following the training, learners were connected via social networking tools that facilitated continued learning and knowledge sharing across levels of the health system and national boundaries.
Diagnosis and treatment
In Ghana, the national health information platform had an indicator for FGS in its national health information system reporting forms. Despite the availability of an indicator, its introduction was relatively new and the FAST Package training activities were able to promote its use and definition. In Madagascar, the closest indicator within the health information system to indicate possible FGS was hematuria. However, recorded cases would not be specific on the presence of urogenital schistosomiasis as other diseases and infections can result in hematuria.
In both Ghana and Madagascar, frontline health personnel in the selected districts were provided with a project form to capture if they suspected an FGS case who they referred for treatment. Following the training activities, 351 cases of suspected FGS were reported in Ghana and 33 in Madagascar. Tracking the treatment of these cases was challenging as Praziquantel was not available through the primary health care centers in either country.
FGS national committee
The FAST Package was supported by the creation of FGS national committees, funded through support of WHO’s Expanded Special Program on NTDs (ESPEN). These committees brought together national level persons who could provide insight and create opportunities for integration of FGS into government health programs, like the HIV/AIDS program, family health, school health, cervical cancer, and national health training institutions. The committees provided a reach of FAST Package activities beyond the two study districts. The secretariat of the committee was situated within the NTD National Program.
The committee in Ghana was active in promoting training on FGS across other districts where S. haematobium was prevalent. The committee worked closely with the cervical cancer prevention program to sensitize FGS recognition. The membership of the Ghanian FGS committee included representatives from the clinical care division, public health division (including NTD Control Program), family health division, Ministry of Education, and Ministry of Health. About 103 healthcare professionals (including 26 district directors) across different cadres were trained by this committee. The committee also participated actively in developing and reviewing the Schistosomiasis/FGS educator’s booklet, which was adopted by the Ghana Health Service and included in the school deworming training material.
The committee in Madagascar secured high level support for its activities within the Ministry of Health, however due to many bureaucratic shifts within the government during the project period, the FGS committee was not able to be implemented.
Discussion
In the FAST Package study districts in Ghana and Madagascar, FGS was largely unknown amongst surveyed community members, healthcare professionals and teachers at baseline, despite good levels of knowledge regarding schistosomiasis. FGS is both a sexual and reproductive health issue as well as the result of a parasitic infection, as such, it is misunderstood by community members and often missed by healthcare professionals. The impact of this neglect is felt by women and girls who experience FGS symptoms and are unable to receive a timely diagnosis and appropriate treatment. Addressing these gaps and their impact on healthcare outcomes requires a holistic approach rooted in systemic changes at the demand (individual, community levels) and supply side (health systems level).
The FAST Package used implementation research to pilot a holistic approach to address FGS in four selected districts in Ghana and Madagascar. Baseline data informed the development of tailored interventions, the national FGS committee aided in scaling up parts of the FAST Package through its partnerships, and results at all stages of the research were presented to the NTD programme in the Ministries of Health in both countries. While the FAST Package was operational for two years (2000-2022) in Ghana and Madagascar, there were lessons learnt which can be applied to other countries considering how to address FGS.
Integrating new activities within the health system takes time
To sustainably address FGS, there must be an integrated approach within different elements and existing programs across the health system. This approach is consistent with the pillars of the WHO NTD 2030 Roadmap and calls from the research community (9, 26–28). The NTD road map calls for integration among NTDs, mainstreaming into national health systems, coordination with relevant programs for other diseases such as HIV, child and maternal health, and strengthening delivery of interventions through country health systems (14). FGS is an excellent candidate for integration, as it is a sexual and reproductive health issue that can be addressed through HIV, HPV programs, family health, maternal and child health programs, among others and yet can be prevented through preventive chemotherapy with Praziquantel delivered through the NTD programme. To help integration of FGS activities into other programme areas within the Ministry of Health, the FAST Package leveraged the FGS National Committee particularly in Ghana. This resulted in integration of FGS into some HPV activities and health worker training as well as the provision of a platform to integrate FGS awareness and training into other scheduled activities.
Incorporating FGS into the health system across multiple levels requires a long-term, flexible approach which is tailored to the national context and system. The World Health Organization Framework for Action titled “Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes” acknowledged the persistence of health gaps due to health system inadequacies that impact the delivery of health services to those in greatest need despite advancements in interventions and technologies (29, 30). Understanding the strengths and weaknesses of the health system can help to guide integration. Varying factors that relate to FGS integration include financing, political will, health workforce, availability of commodities such as PZQ and education materials, data collection through the DHIMS, including FGS case definitions. During the implementation of the FAST Package, we learned that the process to integrate the Educator’s booklet into the health system in both countries was different for example, affecting project planning and timelines. Although the process took longer than planned, it resulted in a resource that was approved for continued use within the Ministry of Health’s NTD programme in both countries.
Integration within the health system can be affected by elections, changes to leadership at different levels and delays due to government bureaucracy. Anticipating these risks needs to be a part of program planning. Creating awareness about FGS at the national level and across multiple departments of the Ministry of Health can help to mitigate these risks. The FGS committee and senior level FGS champions can help to sustain and promote efforts to address FGS within the health system.
Reach endemic communities with FGS messaging during and beyond the annual NTD MDA campaigns
A low level of awareness of FGS amongst community members (‘users’ of the health system) and providers of FGS-related health services in highly endemic areas may lead to a lack of both supply and demand of health services related to FGS diagnosis and management (31). Mass drug administration (MDA) programs for schistosomiasis prevention in highly endemic areas, particularly Sub-Saharan Africa, have increased awareness of schistosomiasis among the populations at risk and healthcare providers (32, 33). However, awareness of FGS amongst community members remains low (31, 34, 35). These findings align with results from the FAST Package in Ghana and Madagascar, which demonstrated a high level of schistosomiasis awareness among community members and teachers in Ghana and Madagascar and a low level of FGS awareness amongst community members and teachers, particularly at baseline. Low FGS awareness levels in the community can worsen the social inequalities and gender gaps among the at-risk population (31). This is particularly important given the gendered variation of risk of schistosomiasis infection between males and females as a result of their exposure to snail-infested freshwater bodies.
At the endline assessment, there was no appreciable increase in awareness of FGS amongst community members in Ghana and Madagascar. However, findings from the project showed an increase in awareness of FGS amongst teachers in Ghana and Madagascar. The increase in awareness of FGS amongst teachers was likely due to the impact of the FAST Package Educators’ booklet. The dissemination of the FGS Educators’ booklet was intended to coincide with MDA campaigns and be an integral part of education and awareness at the school and community levels prior to distribution. However, due to COVID-19, the MDA schedules in both countries were seriously affected, resulting in discordance between the booklet’s publication and distribution and the MDA, affecting the reach of community members in both countries. The value of included FGS as part of MDA promotion is expected to increase coverage and uptake of preventive chemotherapy. As demonstrated in other PC-NTD programs, education and care for associated morbidities increased community uptake in preventive chemotherapy offered through MDA (36). As a manifestation of urogenital schistosomiasis, FGS should be considered as morbidity management for schistosomiasis, with equal importance to the administration of preventive chemotherapy in endemic communities.
Increasing community awareness around the risks and impact of FGS needs ongoing concerted efforts beyond the annual cycle of NTD MDA programs. Symptoms and chronic effects of FGS infection occur outside the MDA cycle and in women and adolescent girls who are no longer included in the school-based MDA programs. Exposure to snail-infested water will continue outside of the MDA cycle, especially if water and sanitation conditions are not improved. Empowering teachers to deliver education about schistosomiasis and FGS can help to increase overall awareness in the community throughout the year.
To ensure that awareness and education becomes institutional, at the health systems leadership and governance level, FGS awareness should be promoted across existing health programs (such as sexual and reproductive health and rights (SRHR), HIV, HPV, and sexually transmitted infections (STI)) and other government programs as an important gender, human rights, and sexual and reproductive health issue (2). This will ensure that activities continue beyond the annual MDA cycle timeline and involve other sectors in support of the NTD program.
Expand availability of praziquantel beyond MDA in school-aged children is needed
Preventive chemotherapy with praziquantel can kill the parasite causing schistosomiasis and prevent infected people from developing chronic diseases (male and female genital schistosomiasis). In most countries, MDA programs mainly target school-aged and are provided through manufacturer donations and international aid in collaboration with the health ministries in schistosomiasis endemic regions (37) leaving out a large proportion of the infected population who are not in school or who are beyond school age. Furthermore, given the inadequate water and sanitation facilities within schistosomiasis-endemic communities, re-infection with Schistosoma parasites can re-occur in between periods of MDA (38, 39). The updated WHO Guideline on control and elimination of human schistosomiasis suggests that there may be increased benefits towards elimination when community-wide distribution goes beyond school aged children to incorporate pre-school aged children, older adolescents, and adults (40).
The findings from Ghana and Madagascar revealed uneven uptake of MDA in schools between males and females at baseline and endline within the last 12 months. In addition, there is evidence that boys received MDA more than girls in all four study districts. These findings suggest that the prevalent belief that schistosomiasis is a boys’ disease may be impacting the uptake with treatment. High levels of coverage are required to reach the elimination goals for schistosomiasis and a more tailored approach to MDA is needed (4).
The timing of MDA needs to consider seasonal availability of food and water. Households in some communities may not be able to provide the food necessary prior to MDA with PZQ. If community members do not understand the importance of MDA uptake as a preventive measure against the chronic manifestations of schistosomiasis, they may not see the value in providing additional food in a period of intense basic need. This will be increasingly challenging in regions where climate change has resulted in droughts and periods of famine, in addition to the impact of climate change on schistosomiasis (41).
According to the proposed framework for assessing gender-related health systems obligation from an FGS perspective, the leadership and governance level of the health system should ensure the expansion of preventative treatment with PZQ beyond schools to reach adolescents and women. (2).
Innovative training helps to reach a diverse audience about FGS
There is limited awareness and knowledge of FGS among healthcare providers, leading to incorrect diagnosis and treatment (5, 6, 42). FGS is rarely covered as part of continuing medical education programs nor is it mentioned in current medical textbooks (6, 7). To reduce gaps in FGS prevention, diagnosis, and treatment knowledge, the FAST Package developed a training course that used case-based scenarios and techniques, peer-to-peer learning, action plan development and implementation. Some of the elements were based on the experience of and successful training workshops developed by The Geneva Learning Foundation and Bridges to Development. The FAST Package FGS training emphasized syndromic diagnosis of FGS given the resource constraints in both countries, however colposcope diagnosis was also included at appropriate levels of care as per FGS core competencies (6). A unique feature of the online training program was the method in which participants were identified. Rather than naming relevant individuals to attend a training or asking the healthcare system to nominate individuals, participants self-nominated for the training. As a result, the final cohort of learners were highly motivated and included representation from across all levels of the health system (frontline health providers, district, regional as well as national level personnel), across countries and across disciplines (general medicine, specialists, midwifery, nursing, health information officers). This resulted in a dynamic learning environment for both learners and trainers. For the in-person training, there was an intent to capitalize on the self-nominated approach, however it was more challenging given the need to coordinate travel and attendance in coordination with the health services. Future training activities would benefit from a paradigm shift in how learners are identified, away from top-down selection of participants to include elements of self-nomination. This approach will ensure that those individuals with the highest interest, relevant subject matter experience and motivation are recruited into the training cohort.
The impact of the FGS trainings organized by the FAST Package continue to be felt at the national and global levels as learners roll out their action plans in their own contexts. Unfortunately, it was beyond the remit of the project to capture these ripple effects; however, certain activities were made known to the FAST Package team, like the creation of the National FGS Society in Nigeria (https://fgssofnigeria.com.ng/) which was a direct result of the online training platform (43). Some FGS SMEs have continued training healthcare workers through the implementation of their action plans.
Strong demand for more knowledge and information on FGS, including integration of FGS training material into routine health personnel pre-service training
The FGS online training had a broader reach beyond the FAST Package implementation countries. The reach helped to increase the depth and experience of the training for the participants in both Ghana and Madagascar, providing them with feedback and lived experiences from professionals working in other countries. During the online FGS workshops, the FAST Package team observed a far higher level of interest than expected and a high intrinsic motivation to develop and implement local solutions. The in-person SME training workshops in both countries included individuals who work in national training institutions. The aim of including these individuals in the SME training was that they would return to their institutions and consider the inclusion of FGS into their existing curriculum. In Ghana this included a module on FGS for continuous professional development in the Ghana College of Medicine and Physicians, inclusion at the nursing school at the University of Health and Allied Sciences and at Heritage Christian University. In Madagascar, nine institutions have included information on FGS in their training of paramedical personnel and three (out of six) Faculties of Medicine in Madagascar now include information on FGS during hospital training in obstetrics and gynecology. Globally, a reference to aid national training institutions to develop their own FGS curriculum is needed.
Reporting of FGS through the District Health Management Information System is non-existent or newly introduced
Although the FAST Package detected nearly 400 cases of suspected FGS as a result of its healthcare personnel training, there was likely under-reporting of cases. In both countries, there is no FGS case definition currently in use. In addition, there is no indicator to report FGS or genital schistosomiasis within Madagascar’s District Health Management Information System (DHMIS). In Ghana, there is the genital schistosomiasis indicator on the Ghana DHMIS; however, the awareness of the genital schistosomiasis indicator is still gathering momentum among frontline health care providers who lack the awareness and knowledge on FGS. The framework for assessing gender-related health systems’ obligations to FGS recommends making available guidelines for diagnosis and treatment of FGS at the health facilities, the inclusion of an FGS indicator, and reporting into the Health Information System (2). To understand the burden of FGS in endemic areas, accurate and consistent reporting is needed. Collaboration in between Schistosoma haematobium endemic countries would help facilitate understanding on what indicators are in use within the DHMIS, how they are defined and reported. Regional bodies like WHO ESPEN and Kikundi community of practice for African program managers can help to transmit these experiences and learnings in between countries.
Limited availability of PZQ for treating women and girls outside of the MDA cycle
The regular supply of praziquantel (PZQ) for treating women and girls with suspected cases of FGS within the community was challenging in Ghana and Madagascar. The PZQ donations were primarily for preventive treatment of school-aged children (5-14 years) through MDA, making it difficult for young women and girls with signs and symptoms of FGS to access treatment at the primary health care facility level outside of the MDA cycle. There were no PZQ tablets in health facilities, and the cost of procuring a single dose of PZQ can be expensive. The WHO policy brief recommends that adolescent girls and women of reproductive age be provided with deworming treatment with PZQ for schistosomiasis (40, 44). Advocacy for wider access to PZQ within the health system and the inclusion of a budget line for FGS as part of the SRHR programs to procure PZQ and train personnel on FGS prevention, diagnosis, and treatment is recommended as part of the governance and health financing health systems building block for FGS (2).
In-country FGS National Advisory Committee can be incredibly powerful and dynamic
Through the FAST Package, the NTD Program in Ghana established a multi and cross-sectoral FGS National Advisory Committee to increase communication and collaboration about FGS with the longer-term goal of integrating FGS management into existing clinical training and care. The FGS National Advisory Committee created awareness on FGS prevention, diagnosis, and treatment beyond the FAST Package implementation districts. When considering the importance of integration and sustainability of programs, national cross-sectoral committees provide a platform for discussion and innovative approaches. In the FAST Package, there were rich exchanges between the NTD program managers in Ghana and Madagascar as they shared ideas, challenges, and opportunities with each other. Some of the challenges of this type of national level committee include the potential for change in leadership within the NTD program, bureaucratic barriers and challenges that exist within the system and the importance of good professional relationships. Ideally, the FGS National Committee should be a pilot for other NTDs that require multi-sectoral action to ensure and sustain elimination.
Limitations
The FAST Package project was initiated during the COVID-19 pandemic, launching in July 2020. The associated intermittent lockdowns, in-country and cross-country restrictions of travel, and inability to hold face-to-face meetings affected the timeline of the project’s implementation, including project launch in Ghana and Madagascar, ethical approvals, baseline data collection, formation of the National FGS Advisory Committees, the distribution of the educator’s booklets as well as the delivery of mass drug administration. In addition to COVID-19, there were other contextual challenges that included insecurity, climatic events (drought) and other disease outbreaks during the project period. Given that the FAST Package project used an implementation research approach which is inherently grounded in the context in both countries, this allowed the team to understand some of the constraints that program personnel at all levels face in the implementation of schistosomiasis and FGS integration programs.
The aim of the FAST Package approach is a holistic approach to sustainably address FGS within the health system. It is contingent on the participation of the health system actors and dependent on their timelines. Changes at the system level are complex and take time. Ensuring that FGS is addressed within the health system at all levels will require patience and perseverance as it will take time. Furthermore, the engagement of global actors in these changes is essential as they can provide opportunities for integrated financing, reporting and action. The FAST Package in Ghana and Madagascar was limited to two years, as such, we were not able to realize all the systemic changes we hoped for within the project timeline. We planned for greater community engagement in the selected districts. However, at the start of the project, we noted the low levels of FGS awareness amongst healthcare personnel in all districts and so we focused more on training and awareness of these key individuals so that they could respond when demand for FGS services eventually came from the community.
The FGS national committee in Madagascar was not able to be fully implemented due to unexpected bureaucratic shifts and hurdles during the project period. Despite having high level support for the committee, it was not able to be implemented. This highlights the challenges and realities of implementing integrated national committees. Leveraging the present political will present, the FAST Package team continues to work to implement the committee.
Conclusion
At the time the grant was issued, the FAST Package in Ghana and Madagascar represented one of the largest single investments focused on addressing FGS within the health system. Since its inception, there has been an increase in global attention on FGS and new projects in Sub Saharan Africa. The FAST Package provides a learning opportunity on the integration of FGS into the health system. It demonstrates the value of innovative and diverse training platforms; the importance of local and national FGS champions to integrate FGS into the health system and pre-service training curriculum; the importance of consistent and regular awareness on FGS outside of the annual MDA cycle; the urgent need to ensure the availability of PZQ at the primary health care centers in endemic areas and; the need for a systems approach to ensure sustainable integration of FGS into the health system. The authors view the FAST Package is an approach. As such, the authors welcome other schistosomiasis endemic countries and research teams to adapt and implement the FAST Package as they seek to address FGS.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Bruyère Research Institute (M16-20-061), University of Ottawa (H-08-21-7345), University of Health and Allied Sciences Ghana (UHAS-REC A.5[4] 20-21), Ghana Health Service (GHS-ERC 003/04/21), and Ministère de la Sante Publique, Madagascar (013/2021-CEER/INSPC). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AK: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. KA: Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. MR: Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – review & editing. JO: Resources, Supervision, Validation, Writing – review & editing. CR: Resources, Supervision, Validation, Writing – review & editing. FR: Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. MD: Data curation, Formal analysis, Investigation, Writing – review & editing. MI: Data curation, Formal analysis, Investigation, Software, Writing – review & editing. IU-W: Data curation, Formal analysis, Investigation, Project administration, Writing – review & editing. CP: Supervision, Validation, Writing – review & editing, Resources. MS: Data curation, Formal analysis, Writing – review & editing. KP: Data curation, Formal analysis, Writing – review & editing. JJ: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – review & editing, Investigation. MG: Conceptualization, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Writing – review & editing, Investigation.
Funding
The author(s) declare financial support was received for the research, authorship and publication of this article. The FAST Package was supported by Grand Challenges Canada. Grand Challenges Canada is funded by the Government of Canada and is dedicated to supporting Bold Ideas with Big Impact ®. This work also received financial support from the Coalition for Operational Research on Neglected Tropical Diseases (COR-NTD), which is funded at The Task Force for Global Health primarily by the Bill & Melinda Gates Foundation (OPP1190754), by UK aid from the British government, and by the United States Agency for International Development through its Neglected Tropical Diseases Program. Under the grant conditions of the Foundation, a Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript version that might arise from this submission. Additional funding for the FAST Package was provided by Merck Global Health Institute, WHO Expanded Special Project for the Elimination of Neglected Tropical Diseases, with in kind support from Unlimit Health (formerly the Schistosomiasis Control Initiative Foundation). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
The authors wish to thank the communities of Morondava, Sakaraha, North Tongu and Weija districts and the healthcare professionals serving them for their participation in the FAST Package. We also acknowledge the members of the FGS National Committee in Ghana and thank them for their enthusiasm in supporting FGS integration. For the online training, we are grateful to the team at The Geneva Learning Foundation for their excellent support in the delivery of the first online training for FGS.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. Ending the neglect to attain the Sustainable Development Goals : A road map for neglected tropical diseases 2021–2030 (2023). Available online at: https://www.who.int/publications-detail-redirect/9789240010352. (Accessed: March 4, 2024)
2. Vlassoff C, Arogundade K, Patel K, Jacobson J, Gyapong M, Krentel A. Improving the response of health systems to female genital schistosomiasis in endemic countries through a gender-sensitive human rights-based framework. Diseases. (2022) 10:125. doi: 10.3390/diseases10040125
3. Ayabina DV, Clark J, Bayley H, Lamberton PHL, Toor J, Hollingsworth TD. Gender-related differences in prevalence, intensity and associated risk factors of Schistosoma infections in Africa: A systematic review and meta-analysis. PloS Negl Trop Dis. (2021) 15:e0009083. doi: 10.1371/journal.pntd.0009083
4. Kukula VA, MacPherson EE, Tsey IH, Stothard JR, Theobald S, Gyapong M. A major hurdle in the elimination of urogenital schistosomiasis revealed: Identifying key gaps in knowledge and understanding of female genital schistosomiasis within communities and local health workers. PloS Negl Trop Dis. (2019) 13:e0007207. doi: 10.1371/journal.pntd.0007207
5. Mazigo HD, Samson A, Lambert VJ, Kosia AL, Ngoma DD, Murphy R, et al. Female genital schistosomiasis is a sexually transmitted disease”: Gaps in healthcare workers’ knowledge about female genital schistosomiasis in Tanzania. PloS Global Public Health. (2022) 2:e0000059. doi: 10.1371/journal.pgph.0000059
6. Jacobson J, Pantelias A, Williamson M, Kjetland EF, Krentel A, Gyapong M, et al. Addressing a silent and neglected scourge in sexual and reproductive health in Sub-Saharan Africa by development of training competencies to improve prevention, diagnosis, and treatment of female genital schistosomiasis (FGS) for health workers. Reprod Health. (2022) 19:20. doi: 10.1186/s12978-021-01252-2
7. UNAIDS. No more neglect—Female genital schistosomiasis and HIV — Integrating sexual and reproductive health interventions to improve women’s lives | UNAIDS (2019). Available online at: https://www.unaids.org/en/resources/documents/2019/female_genital_schistosomiasis_and_hiv. (Accessed: March 4, 2024)
8. Gyapong M, Theobald S. The sexual and reproductive health issue you’ve probably never heard of…. openDemocracy (2015). Available online at: https://www.opendemocracy.net/en/5050/sexual-and-reproductive-health-issue-youve-probably-never-hear/. (Accessed: March 4, 2024)
9. Engels D, Hotez PJ, Ducker C, Gyapong M, Bustinduy AL, Secor WE, et al. Integration of prevention and control measures for female genital schistosomiasis, HIV and cervical cancer. Bull World Health Organ. (2020) 98:615−624. doi: 10.2471/BLT.20.252270
10. Brodish PH, Singh K. Association between schistosoma haematobium exposure and human immunodeficiency virus infection among females in Mozambique. Am J Trop Med Hyg. (2016) 94:1040−1044. doi: 10.4269/ajtmh.15-0652
11. Downs JA, Dupnik KM, Van Dam GJ, Urassa M, Lutonja P, Kornelis D, et al. Effects of schistosomiasis on susceptibility to HIV-1 infection and HIV-1 viral load at HIV-1 seroconversion: A nested case-control study. PloS Negl Trop Dis. (2017) 11:e0005968. doi: 10.1371/journal.pntd.0005968
12. De Vuyst H, Alemany L, Lacey C, Chibwesha CJ, Sahasrabuddhe V, Banura C, et al. The burden of human papillomavirus infections and related diseases in Sub-Saharan Africa. Vaccine. (2013) 31:F32−F46. doi: 10.1016/j.vaccine.2012.07.092
13. Kharsany ABM, Karim QA. HIV infection and AIDS in Sub-Saharan Africa: current status, challenges and opportunities. Open AIDS J. (2016) 10:34−48. doi: 10.2174/1874613601610010034
14. WHO. Deworming adolescent girls and women of reproductive age. Policy brief (2021). Available online at: https://www.who.int/publications-detail-redirect/9789240037670. (Accessed: March 4, 2024)
15. Krentel A, Steben M. A call to action : ending the neglect of female genital schistosomiasis. J Obstetrics Gynaecol Canada. (2021) 43:3−4. doi: 10.1016/j.jogc.2020.11.008
16. Hotez PJ, Harrison W, Fenwick A, Bustinduy AL, Ducker C, Sabina Mbabazi P, et al. Female genital schistosomiasis and HIV/AIDS: Reversing the neglect of girls and women. PloS Negl Trop Dis. (2019) 13:e0007025. doi: 10.1371/journal.pntd.0007025
17. Williams CR, Seunik M, Meier BM. Human rights as a framework for eliminating female genital schistosomiasis. PloS Negl Trop Dis. (2022) 16:e0010165. doi: 10.1371/journal.pntd.0010165
18. Special Programme for Tropical Diseases Research. TDR Implementation Research Toolkit (Second Edition). Access and Delivery Partnership. Consulté 1 mars 2024, à l’adresse. Available online at: https://adphealth.org/irtoolkit/. (Accessed: March 4, 2024)
19. Leech NL, Onwuegbuzie AJ. A typology of mixed methods research designs. Qual Quantity. (2009) 43:265−275. doi: 10.1007/s11135-007-9105-3
20. Ampofo JA, Zuta PC. Schistosomiasis in the Weija Lake: a case study of the public health importance of man-made lakes. Lakes & Reservoirs: Science, Policy and Management for Sustainable Use. (1995) 1:191–5. doi: 10.1111/j.1440-1770.1995.tb00023.x
21. Anyan WK, Abonie SD, Aboagye-Antwi F, Tettey MD, Nartey LK, Hanington PC, et al. Concurrent Schistosoma mansoni and Schistosoma haematobium infections in a peri-urban community along the Weija dam in Ghana: A wake up call for effective National Control Programme. Acta Tropica. (2019) 199:105116. doi: 10.1016/j.actatropica.2019.105116
22. Conseil national du recensement de la population et de l’habitation, Ministère de l’économie et des finances, institut national de la statistique, Cellule centrale d’execution du recensement. Résultats globaux du recensement général de la population et de l’habitation de 2018 de Madagascar (RGPH-3). Institut National de la Statistique. (2020).
23. Kukula VA, Gyapong M, Addei S, Tsey IH, MacPherson E, Theobald S. Experiences with female genital schistosomiasis: A neglected and misunderstood disease. Liverpool UK: Countdown Consortium (2019). Available at: https://countdown.lstmed.ac.uk/sites/default/files/centre/FGS%20in%20Ghana%20-%20FINAL.pdf. (Accessed: March 4, 2024)
24. Henderson RH, Sundaresan T. Cluster sampling to assess immunization coverage: A review of experience with a simplified sampling method. Bull World Health Organ. (1982) 60:253−260.
25. Dean L, Ozano K, Thomson R. Stronger together: Evidence for collaborative action on neglected tropical diseases. Int Health. (2023) 15:i1−i5. doi: 10.1093/inthealth/ihad004
26. Nemungadi TG, Furumele TE, Gugerty MK, Djirmay AG, Naidoo S, Kjetland EF. Establishing and integrating a female genital schistosomisis control programme into the existing health care system. Trop Med Infect Dis. (2022) 7:382. doi: 10.3390/tropicalmed7110382
27. Preston A, Vitolas CT, Kouamin AC, Nadri J, Lavry SL, Dhanani N, et al. Improved prevention of female genital schistosomiasis: piloting integration of services into the national health system in Côte d’Ivoire. Front Trop Dis. (2023) 4:1308660. doi: 10.3389/fitd.2023.1308660
28. Umbelino-Walker I, Wong F, Cassolato M, Pantelias A, Jacobson J, Kalume C. Integration of female genital schistosomiasis into HIV/sexual and reproductive health and rights and neglected tropical diseases programmes and services: A scoping review. Sexual Reprod Health Matters. (2023) 31:2262882. doi: 10.1080/26410397.2023.2262882
29. Stockton DA, Fowler C, Debono D, Travaglia J. World Health Organization building blocks in rural community health services: An integrative review. Health Sci Rep. (2021) 4:e254. doi: 10.1002/hsr2.254 (Accessed: March 4, 2024)
30. WHO. Everybody’s business—Strengthening health systems to improve health outcomes (2007). Available online at: https://www.who.int/publications-detail-redirect/everybody-s-business—strengthening-health-systems-to-improve-health-outcomes.
31. Rausche P, Rakotoarivelo RA, Rakotozandrindrainy R, Rakotomalala RS, Ratefiarisoa S, Rasamoelina T, et al. Awareness and knowledge of female genital schistosomiasis in a population with high endemicity: A cross-sectional study in Madagascar. Front Microbiol. (2023) 14:1278974. doi: 10.3389/fmicb.2023.1278974
32. Christinet V, Lazdins-Helds JK, Stothard JR, Reinhard-Rupp J. Female genital schistosomiasis (FGS): From case reports to a call for concerted action against this neglected gynaecological disease. Int J Parasitol. (2016) 46:395−404. doi: 10.1016/j.ijpara.2016.02.006
33. French MD, Evans D, Fleming FM, Secor WE, Biritwum N-K, Brooker SJ, et al. Schistosomiasis in Africa: Improving strategies for long-term and sustainable morbidity control. PloS Negl Trop Dis. (2018) 12:e0006484. doi: 10.1371/journal.pntd.0006484
34. Kutz J-M, Rausche P, Rasamoelina T, Ratefiarisoa S, Razafindrakoto R, Klein P, et al. Female genital schistosomiasis, human papilloma virus infection, and cervical cancer in rural Madagascar: A cross sectional study. Infect Dis Poverty. (2023) 12:89. doi: 10.1186/s40249-023-01139-3
35. Schuster A, Randrianasolo BS, Rabozakandraina OO, Ramarokoto CE, Brønnum D, Feldmeier H. Knowledge, experiences, and practices of women affected by female genital schistosomiasis in rural Madagascar: A qualitative study on disease perception, health impairment and social impact. PloS Negl Trop Dis. (2022) 16:e0010901. doi: 10.1371/journal.pntd.0010901
36. Cantey PT, Rout J, Rao G, Williamson J, Fox LM. Increasing compliance with mass drug administration programs for lymphatic filariasis in India through education and lymphedema management programs. PloS Negl Trop Dis. (2010) 4:e728. doi: 10.1371/journal.pntd.0000728
37. Secor WE. Early lessons from schistosomiasis mass drug administration programs. F1000Research. (2015) 4:1157. doi: 10.12688/f1000research.6826.1
38. Moses A, Adriko M, Kibwika B, Tukahebwa EM, Faust CL, Lamberton PHL. Residence time, water contact, and age-driven Schistosoma mansoni infection in hotspot communities in Uganda. Am J Trop Med Hygiene. (2021) 105:1772−1781. doi: 10.4269/ajtmh.21-0391
39. Zacharia A, Mushi V, Makene T. A systematic review and meta-analysis on the rate of human schistosomiasis reinfection. PloS One. (2020) 15:e0243224. doi: 10.1371/journal.pone.0243224
40. WHO. Schistosomiasis (2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/schistosomiasis.
41. Adekiya TA, Aruleba RT, Oyinloye BE, Okosun KO, Kappo AP. The effect of climate change and the snail-schistosome cycle in transmission and bio-control of schistosomiasis in Sub-Saharan Africa. Int J Environ Res Public Health. (2019) 17:181. doi: 10.3390/ijerph17010181
42. WHO. Female genital schistosomiasis: A pocket atlas for clinical health-care professionals (2015). Available online at: https://www.who.int/publications-detail-redirect/9789241509299. (Accessed: March 4, 2024)
43. Global Schistosomiasis Alliance. Female Genital Schistosomiasis Society of Nigeria : A model for local action. Consulté 1 mars 2024, à l’adresse. Available online at: https://www.eliminateschisto.org/sites/gsa/files/content/attachments/2022-04-27/Case%20Study%20FGS%20Network.pdf. (Accessed: March 4, 2024)
44. World Health Organization. Deworming adolescent girls and women of reproductive age. Policy brief. Consulté 29 février 2024, à l’adresse. Available online at: https://www.who.int/publications-detail-redirect/9789240037670. (Accessed: March 4, 2024)
Keywords: female genital schistosomiasis (FGS), Schistosoma haematobium, community awareness, healthcare training, Subsaharan Africa, Ghana, Madagasacar, online training
Citation: Krentel A, Arogundade K, Raharinivo M, Opare J, Rasoamanamihaja CF, Randrianasolo FH, Dalaba MA, Immurana M, Umbelino-Walker I, Pensotti C, Sangare M, Patel K, Jacobson J and Gyapong M (2024) A holistic approach to address female genital schistosomiasis in Ghana and Madagascar: the FGS Accelerated Scale Together Package. Front. Trop. Dis 5:1395467. doi: 10.3389/fitd.2024.1395467
Received: 04 March 2024; Accepted: 02 August 2024;
Published: 09 October 2024.
Edited by:
Roch Christian Johnson, CIFRED UAC, BeninReviewed by:
Humphrey Deogratias Mazigo, Catholic University of Health and Allied Sciences (CUHAS), TanzaniaVanessa Christinet, Centre Hospitalier Universitaire Vaudois (CHUV), Switzerland
Copyright © 2024 Krentel, Arogundade, Raharinivo, Opare, Rasoamanamihaja, Randrianasolo, Dalaba, Immurana, Umbelino-Walker, Pensotti, Sangare, Patel, Jacobson and Gyapong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alison Krentel, YWtyZW50ZWxAYnJ1eWVyZS5vcmc=
 Alison Krentel
Alison Krentel Kazeem Arogundade
Kazeem Arogundade Mbolatiana Raharinivo
Mbolatiana Raharinivo Joseph Opare
Joseph Opare Clara Fabienne Rasoamanamihaja
Clara Fabienne Rasoamanamihaja Faly Hariniaina Randrianasolo
Faly Hariniaina Randrianasolo Maxwell Ayindenaba Dalaba
Maxwell Ayindenaba Dalaba Mustapha Immurana7
Mustapha Immurana7 Kruti Patel
Kruti Patel Julie Jacobson
Julie Jacobson Margaret Gyapong
Margaret Gyapong