- 1Department of Health Management and Organization, School of Preventive Medicine and Public Health, Hanoi Medical University, Hanoi, Vietnam
- 2Department of Medical Service Administration, Vietnam Ministry of Health, Hanoi, Vietnam
- 3Department of Otolaryngology, Hanoi Medical University, Hanoi, Vietnam
Introduction: The rapid spread of SARS-CoV-2, the varying vaccine coverage, and the appearance of new variants posed a significant threat during the pandemic, especially in LMIC countries. Hospitals in Vietnam at both central and local levels have had cross-infection of patients and healthcare workers. Therefore, providing a safe and secure environment for staff and patients was a major focus for all healthcare institutions.
Methods: We conducted a cross-sectional study, using both quantitative and qualitative methods, to answer the question of how hospital safety during the COVID-19 pandemic in Vietnamese hospitals was implemented and what the challenges were. Secondary data from a recent national survey of safety in 1,398 hospitals conducted by the Vietnam Ministry of Health (MOH) were extracted and analyzed. In-depth interviews of key health managers and health staff in four selected hospitals were performed to further explore challenges in implementing Decision 3088/QD-BYT.
Results: The proportion of hospitals classified as “safe hospital”, “safe hospital with moderate level”, and “unsafe hospital” was 91.7%, 7.3%, and 1.0%, respectively. The rate of “safe hospital” was highest in the central level hospitals (96.1%), followed by private hospitals (94.4%), provincial hospitals (94.2%), specialized hospitals (93.1%), regional hospitals (93.0%), and district hospitals (89.9%), while “safe hospital” rates were lowest in the ministerial level hospital group (82.2%). Challenges in ensuring hospital safety in public and private hospitals related to COVID-19 transmission, such as lack of preparedness before COVID-19 and other pandemics, limited hospital facility, limited space and equipment, shortage of human resources, inadequate training and knowledge transfer, poor patient compliance in declaring health conditions, and lack of patient understanding of infection prevention methods, were explored.
Conclusion: Most hospitals in Vietnam successfully met the classification of “safe hospitals” according to Decision 3088/QD-BYT, a key tool for hospitals to self-assess preparedness and responsiveness to the COVID-19 pandemic. The MOH should adapt the criteria in Decision 3088/QD-BYT to be more suitable for the new phase of the pandemic as we move towards “living with COVID”. Furthermore, we recommend that the MOH work to develop mechanisms or regulations that require hospitals to regularly report on disease preparation and responses for future pandemic preparedness.
Introduction
In Vietnam, the fourth wave of the COVID-19 pandemic, beginning from 27 April 2021, has been considered the most severe one. The number of new cases increased day by day; in particular, Ho Chi Minh City detected 667 new COVID-19 cases in 24 h (1). During this time in Vietnam, the infected people (F0) were treated in hospitals, which is different from several countries, where only moderate and severe COVID-19 patients are admitted to the hospital for treatment (2). This puts a strain on the Vietnamese health system, and since the peak of this fourth wave has not been reached, the work pressure on the health workforce would increase. Moreover, healthcare workers have a high probability of being infected since they have to take care of patients or perform procedures that pose a risk of SARS-CoV-2 infection. “Safe hospital” was first used to mention all healthcare institutions that could fully access and operate before, during, and after a natural disaster. Meanwhile, the World Health Organization (WHO) defined “safe hospital” as health facilities at all levels that are protected, which could provide health services with a continuous supply of water, electric power, and telecommunications (3). With the rapid spread of the COVID-19 pandemic, several vaccinations have been used and proved their safety and effectiveness in preventing COVID-19 (4). However, the vaccine imbalance and new variants of SARS-CoV-2 pose the greatest threat to the COVID-19 pandemic, especially in LMIC countries. The rate of health staff infected by COVID-19 varied, such as 33.3% in China and 53.5% in Iran. The level of risk of COVID-19 infection was high in several countries such as the US (73%) and Ethiopia (76%) (5, 6). This percentage was higher than that of Vietnam (6%), which was informed in 2020 (6). Therefore, proving a safe and secure environment for staff and patients during treatment is one of the main missions of healthcare institutions, especially during the COVID-19 pandemic.
Due to the rapid spread and the different virus variants of the COVID-19 pandemic, hospitals and long-term care facilities must have the necessary preparation measures in place; the WHO has issued the Rapid Hospital Readiness Checklist in 2020 to assist health institution administrators in optimizing their capacity to treat COVID-19 patients (7). It has been developed to be user-friendly while considering the human resources and time necessary to perform and complete it. However, the checklist provided by WHO considers various problems, including the necessity to continue to provide treatment to patients suffering from acute or chronic diseases; the laboratory tests required; the necessary blood supplies and services; the requirement for community health outreach initiatives such as vaccinations and prenatal care; the delivery, tracking, and safety of medications and medical supplies; hospital information management; the requirement to instruct employees and other individuals; security issues such as safeguarding healthcare workers, patients and residents of long-term care institutions, caregivers, and visitors; and the necessity of mental health and psychosocial programs for medical and nonmedical personnel working in medical institutions. It should be tailored to national and local settings by considering a country’s rules, guidelines, local hazards, needs, standards, and practices (7). Hospitals play an important role in the health system by providing crucial medical treatment to the population, identifying that the safety of health workers is the first concern for patient safety especially in the context of the COVID-19 pandemic. To deal with this situation, Decision No. 3088/QD-BYT was issued on 16 July 2020 by the MOH of Vietnam to promulgate the set of criteria for safe hospitals to prevent COVID-19 and other acute respiratory infections (8). The Decision applied to state and non-state hospitals. The set of criteria provides tools and self-assesses the current situation of the hospital to prevent COVID-19 and acute respiratory infections. Moreover, it orients the hospital to identify priority issues for safe medical examination and treatment, prevent infection of patients, and medical staff. Lines of evidence about the hospital safety of Vietnam during the COVID-19 pandemic contribute to improve the preparation of healthcare institutions to deal with the problems of natural and man-made pandemic, and hospital administrators must assure the implementation of appropriate general priority actions.
Hence, the study was conducted with the following objectives: (i) to describe the implementation of hospital safety criteria during the COVID-19 pandemic according to Decision 3088/QD-BYT of public and private hospitals in Vietnam in 2020, and (ii) to analyze challenges in ensuring hospital safety in public and private hospitals related to COVID-19 transmission.
Methods
Research design
Study context
Vietnam’s medical system is divided into four administrative levels of health services: central, provincial, district, and commune (Figure 1). At present, the public healthcare sector extends from the top to the bottom of the pyramid. The central level includes the MOH of Vietnam, which is the governmental agency that leads all the activities of other medical organizations (9). They are responsible for protecting and improving the health of the Vietnamese population, particularly by adopting laws and other legal instruments.
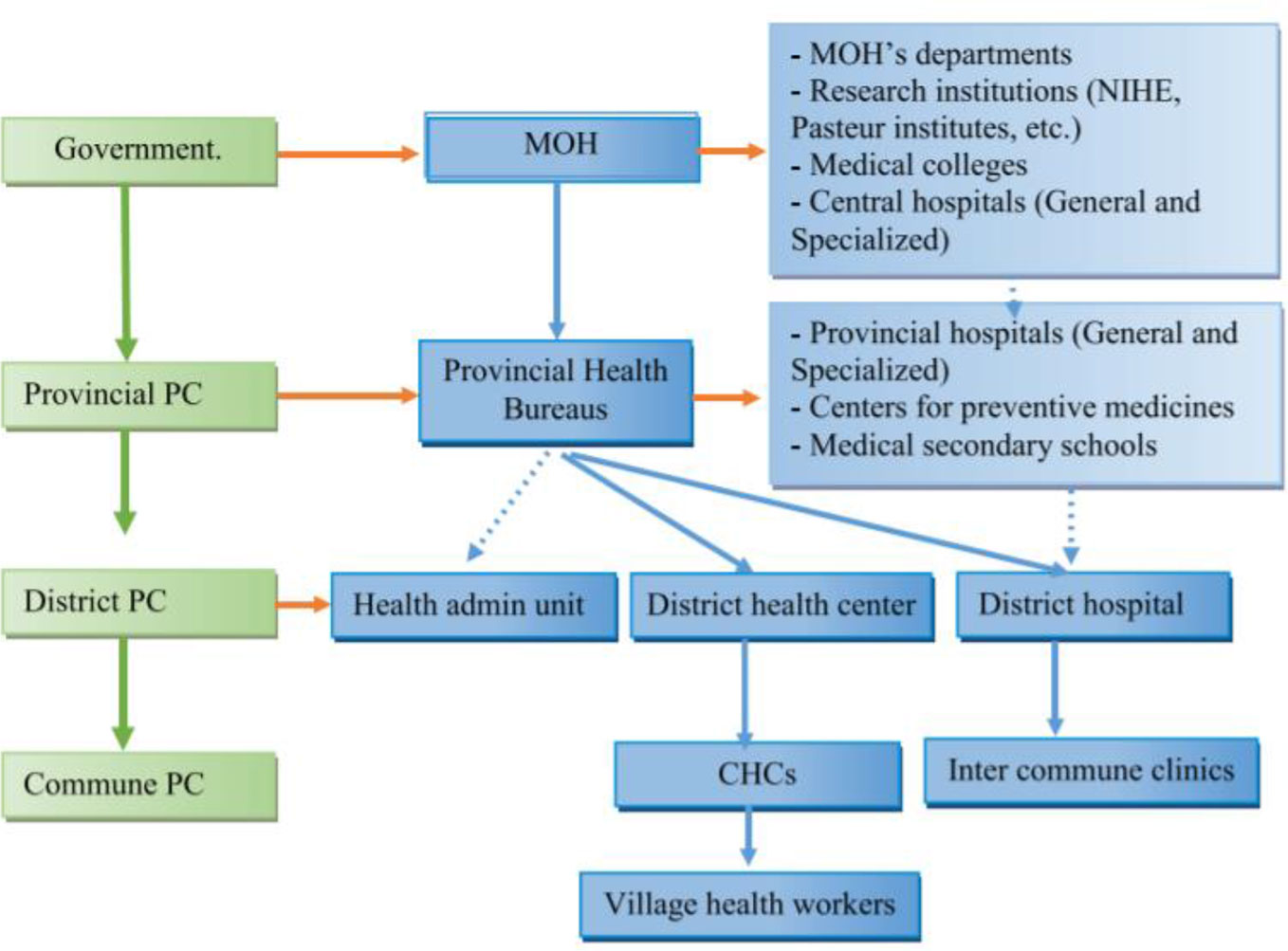
Figure 1 Vietnam Health System (10) (PC, people committee; CHC, commune health centers).
The study was conducted between February and August 2021. This cross-sectional study applied both quantitative and qualitative approaches. Quantitative research was based on recent national surveys of hospital safety conducted by the MOH (nationwide scale of public and private hospitals that participated in hospital safety assessment in the COVID-19 online reporting system of Quality Management Division, Ministry of Health). Qualitative research employed in-depth interviews of key health managers and staff in four selected hospitals.
Research subjects
For quantitative research, the study subjects were public and private hospitals in Vietnam. Hospitals having sufficient data for analysis in the MOH’s Decision 3088/QD-BYT databases (https://covid19.chatluongbenhvien.vn/) were included into the study. The exclusion criteria included the following: (1) not having sufficient data for evaluation, and (2) not reporting in the databases.
For qualitative research, the study subjects were representatives of several public and private hospitals, including representatives of the board of directors, representatives of the department of planning, and representatives of healthcare workers in the hospitals. The inclusion criteria were as follows: (1) worked in hospitals at least 24 months (with hospital experience before the COVID-19 pandemic), and (2) agreed to participate and provide information.
Sample size and sampling technique
The quantitative research used reported data from all hospitals in the MOH’s Decision 3088 databases that met the inclusion and exclusion criteria. A total of 1,398 hospitals were included and analyzed.
The qualitative research conducted in-depth interviews in four hospitals including one central hospital, one regional hospital, one district hospital, and one private hospital. In each hospital, four people were invited: one representative of the board of directors, one representative of the department of planning or other departments with a similar function, and two representatives of healthcare workers in hospitals.
Research instrument and data collection
Researchers developed an outline according to research objectives, contacted the Quality Management Division, and collected information from necessary reports and data from the online reporting system on the implementation of Decision 3088/QD-BYT by the MOH on safety of the hospitals in Vietnam in 2020.
The outcome variable was “Hospital Safety”, and in accordance with Decision 3088, the set of hospital criteria had 37 items, divided into eight groups of criteria as below (8):TEST
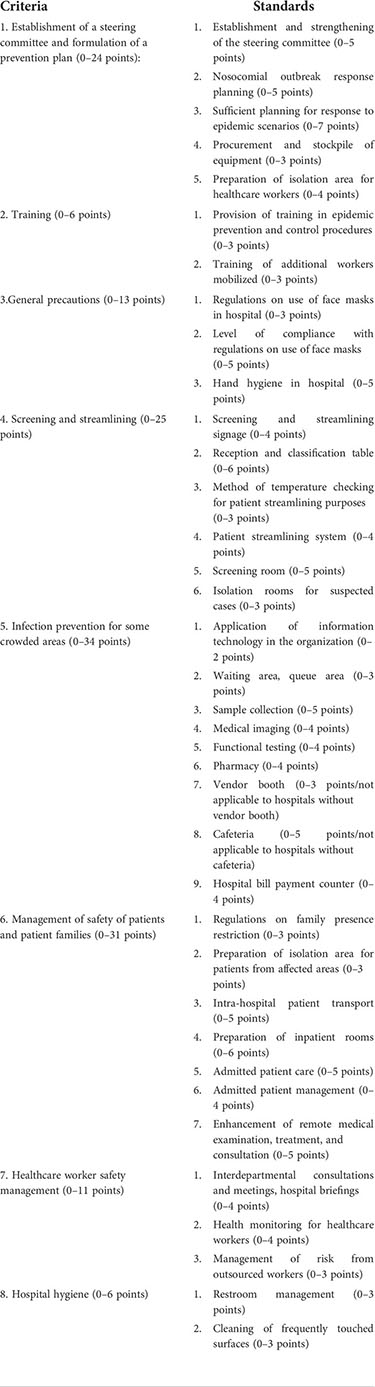
Maximum points: 150 points. Each subsection was scored as “pass” or “fail”. Each sub-category was given 1 point, two sub-categories were given 2 points. The score for each criterion was equal to the total score of the subsections. When no subsection was scored, the criterion score was 0. If the hospital did not have a criterion (e.g., the sales counter), the criteria could not be scored. Therefore, the outcome of this study, “Hospital Safety”, was classified by three categories: Safe hospital: total score was equal to or more than 75% maximum and there was no * criterion at 0 point; Hospitals with moderate safety: the total score ranged between 50% and <75% of the maximum score and there was no criterion * with 0 point; Unsafe hospital: overall score was equal to or less than 50% or any * criteria got 0 points (8).
The qualitative tool used in-depth interview guidelines, and each participant was verbally informed of the aims and requirements of the study and was assured of the confidentiality of the investigation. All questions in the questionnaire met the requirements of the study objectives.
Data management and analysis
For quantitative data, cleaned data were entered into standardized Excel worksheets, and analyzed using Stata 15.0 software. Mean, standard deviation, frequency, and percentage were presented. Chi-squared test and Kruskal–Wallis test were used to examine the difference of scores among different groups.
For qualitative information, all interviews were recorded, transcribed into word documents, and analyzed. To analyze the contents of the interviews, procedures from thematic analysis, developing and defining thematic codes to capture transcript segments related to health policies during the COVID-19 pandemic, and the implementation of hospital safety criteria in accordance with Decision 3088/QD-BYT by the MOH were carried out.
Ethical consideration
The study procedures were reviewed by the Internal Review Board of Institute for Preventive Medicine and Public Health, Hanoi Medical University.
Results
Decision-3088/QD-BYT by the MOH was promulgated to aim at improving hospital safety during the COVID-19 pandemic and was known by all hospitals. At hospitals, Decision-3088 had been disseminated through many information channels such as internal website, hospital announcement, and hospital board of directors. Some hospitals even conducted monthly inspection and evaluation teams to ensure that the hospital is safe for medical staff, patients, and caregivers.
Implementation of Decision 3088/QD-BYT by the Minister of Health on safety of public and private hospitals in Vietnam in 2020
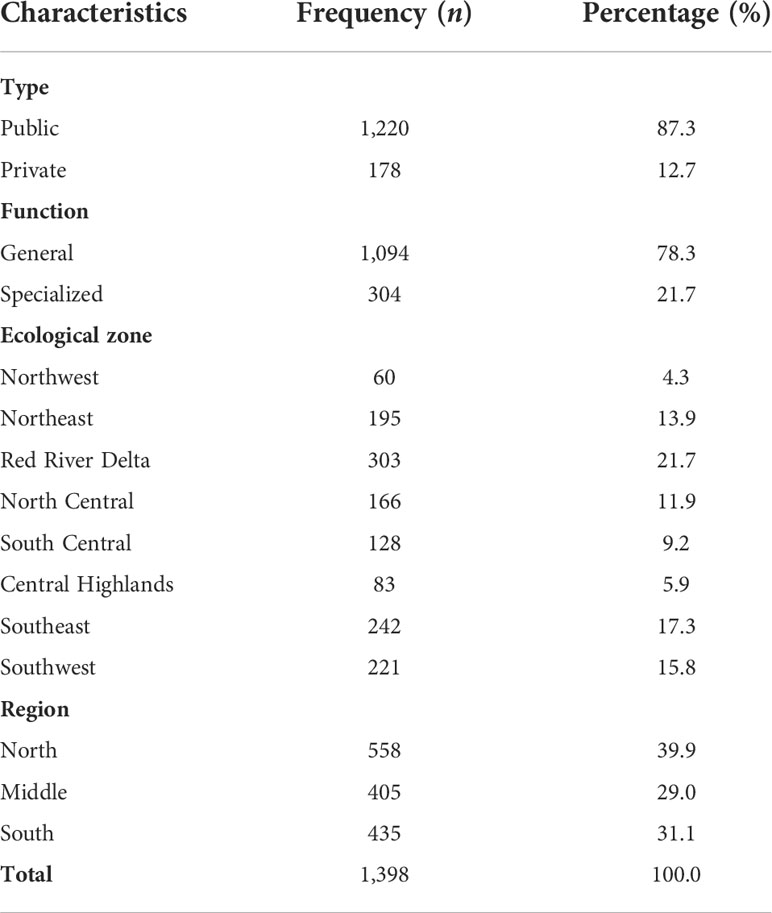
A total of 1,398 hospitals were selected in this study. Hospitals in the public sector were the majority with 87.3%, and only 12.7% of hospitals belonged to the private sector. The number of general hospitals accounts for 78.3%, while the rate of specialized hospitals is only 21.7%. The percentage of hospitals in the Red River Delta region was the highest at 21.7%, followed by the Southeast, Southwest, and Northeast regions with 17.3%, 15.8%, and 13.9%, respectively. The proportion of hospitals in the Northwest and Central Highland regions accounted for only 4.3% and 5.9%, respectively (Table 1).
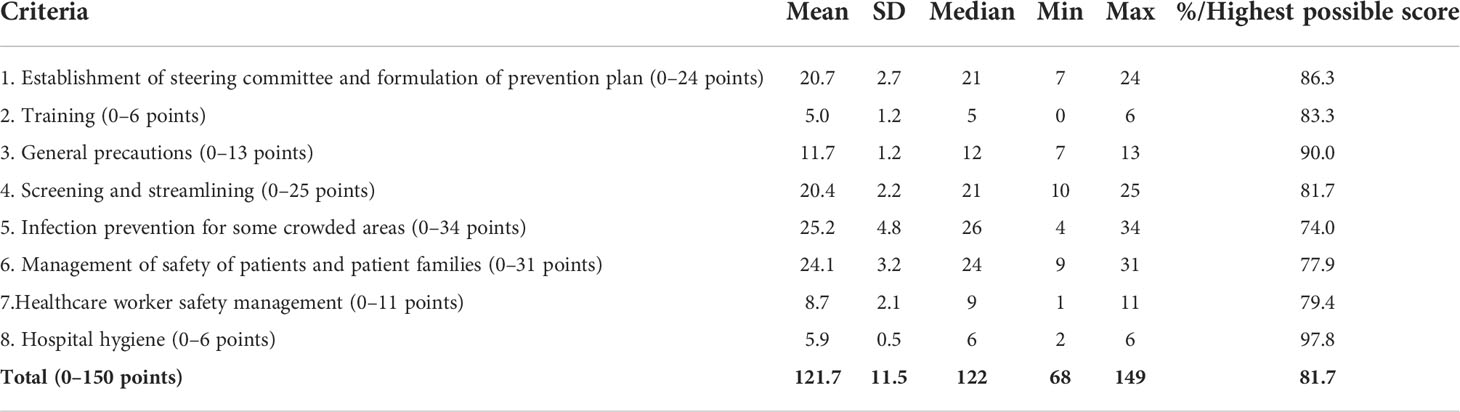
Table 2 shows the summed score of eight criteria for hospital safety according to Decision 3088/QD-BYT. Compared to the possible maximum score, the score of criterion 5 had the lowest percentage, followed by criteria 6 and 7. Meanwhile, criterion 8 had the highest percentage, followed by criteria 3 and 1. Overall, the total score of hospital safety was 121.7 (SD = 11.5), which equaled 81.7% of the possible maximum score.
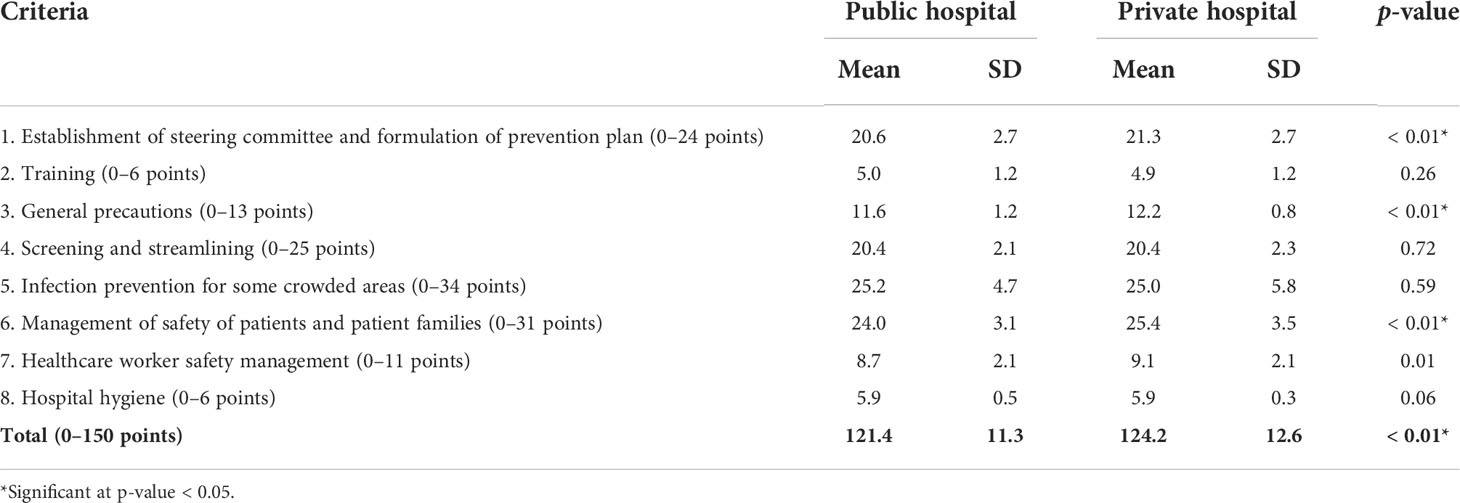
In general, private hospitals had a higher average score in criteria 1, 3, 6, and 7 and total score (p < 0.05). Meanwhile, no difference was found between public and private hospitals in criteria 2, 4, 5, and 8 (Table 3).
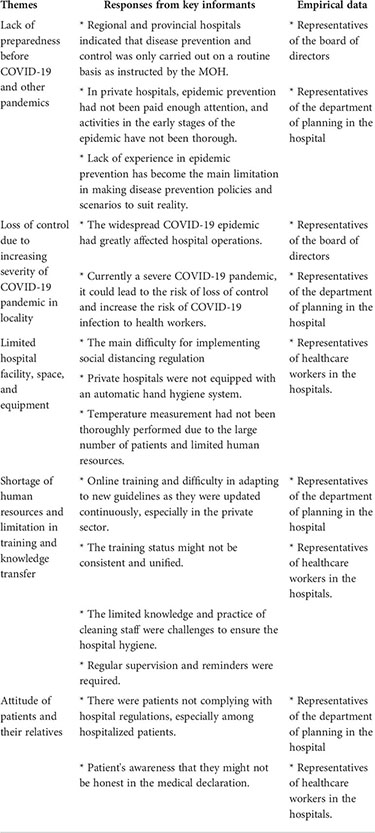
Challenges in ensuring hospital safety during COVID-19 pandemic in Vietnam
The difficulties and challenges in ensuring the safety of hospitals during the COVID-19 pandemic were assessed, in addition to the advantages and difficulties when implementing each content in Decision 3088 as mentioned above.
Lack of preparedness before COVID-19 and other pandemics
The experience of each hospital before an epidemic occurs was one of the important factors to assess the preparedness and ability of the hospital to respond to the epidemic. In big hospitals such as the Central Hospital, before 2020, the hospital had carried out epidemic prevention work such as establishing a Patient Safety Team to promote hospital infection control and monitoring and evaluation. Meanwhile, participants at regional and provincial hospitals indicated that disease prevention and control was only carried out on a routine basis as instructed by the MOH.
“The epidemic prevention and control before 2020 is not much different every day and every month, the hospital updates the circulars, decisions and guidelines issued by the Ministry of Health, prepares and plans in a timely manner. And train, guide, closely monitor and give specific procedures to implement epidemic prevention and control” (IDI-Province Hospital_Staff_2).
For private hospitals, epidemic prevention had not been paid enough attention; thus, activities in the early stages of the epidemic have not been thorough. As a result, there were hospital-acquired COVID-19 cases during the early part of 2020. The lack of experience in epidemic prevention had become the main limitation in making disease prevention policies and scenarios to suit reality.
“The members actively participate in the steering committee for epidemic prevention and control, but the experience in epidemic prevention is still limited, so the planning still faces many difficulties when giving a scenario that is not close to reality” (IDI-Private Hospital_Staff_2).
Loss of control due to increasing severity of COVID-19 pandemic in locality
The widespread COVID-19 epidemic had greatly affected hospital operations, especially hospital safety. For example, in the Southern region, where there was currently a severe COVID-19 pandemic, it could lead to the risk of loss of control and increase the risk of COVID-19 infection to health workers.
“Due to the complicated developments of the COVID-19 epidemic in Ho Chi Minh City, many cases appeared in the community. Therefore, in the hospital, there are also many cases of COVID-19 entering the community through outpatient examination and emergency. In addition, the hospital also has to receive severe COVID-19 cases transferred from other units. These are great challenges for the prevention and control of COVID-19 for hospitals today and in the near future” (IDI-Central Hospital_Staff_2).
Limited hospital facility, space, and equipment
Regarding facility, it became the main difficulty for implementing social distancing regulation. The space of the hospital was limited, so the distance was difficult to ensure.
A problem was raised in a private hospital when hand hygiene could lead to cross-contamination because it was not equipped with an automatic hand hygiene system.
“The hospital has not equipped automatic hand sanitizer machines to limit contact, so there is still a potential risk of cross-infection” (IDI-Private Hospital_Staff_3).
An additional limitation was that temperature measurement had not been thoroughly performed due to the large number of patients and limited human resources. Another problem was that hot weather could greatly affect the health of medical staff if personal protective equipment was used regularly. Therefore, there was an urgent need to design equipment to help ensure the safety of medical staff, but also to be convenient and cool, suitable for the environment and climate.
Shortage of human resources and limitation in training and knowledge transfer
Difficulties were raised including online training and difficulty in adapting to new guidelines as they were updated continuously, especially in the private sector. In addition, the training status might not be consistent and unified because the implementation process was conducted according to each department.
“The training is not hand-held for each individual, but divided by group, by department, besides the staff is busy with professional work to take care of patients at the department, etc., so the participation is not consistent” (IDI-Central Hospital_Leader_1).
Along with these difficulties, the limited knowledge and practice of cleaning staff were also challenges to ensure hospital hygiene; thus, regular supervision and reminders were required.
Attitude of patients and their relatives
Health workers were assessed to comply 100% with regulations on wearing face masks. However, there were situations of patients not complying with this regulation, especially among hospitalized patients.
The participants also identified the difficulty in the implementation due to the patient’s awareness that they might not be honest in the medical declaration.
“… The patient’s ‘worry’ mentality when going to the doctor/re-examination but declaring the truth will be in trouble because they will be screened, streamed through areas for people at risk, and take a long time to go to the doctor, everyone thinks that they are 100% not at risk. This also contributes to difficulties for officials performing the medical declaration work” (IDI-Central Hospital_Staff_2).
Themes identified from the qualitative results
Discussion
The findings of this study showed that the proportion of hospitals classified as “safe hospital”, “safe hospital with moderate level”, and “unsafe hospital” was 91.7%, 7.3%, and 1.0%, respectively. Thus, basically, most hospitals in Vietnam have met the standards of safe hospitals according to Decision 3088/QD-BYT. The criterion 8 “Hospital hygiene” had the highest level of compliance, followed by criterion 3 “General precautions” and criterion 1 “Establishment of steering committee and formulation of prevention plan”. This could be partly explained by the habit of wearing masks by Vietnamese people when going out. In addition, the mandatory wearing of masks had been regulated by the government, so it could be seen that the compliance level of this standard was at a high level. However, compliance with “hand hygiene” standards was not as good as “wearing face mask” standards. In this study, although the level of compliance was still high, the score for this standard was lower than that of “wearing face mask” standards. A previous report in Vietnam on adults showed that only 26.3% practiced washing their hands correctly, and only 28.4% washed their hands for at least 20 s. Although 92.1% washed their hands after contacting surfaces at public places (e.g., lifts and knob doors), only 66.3% practiced handwashing after removing their masks (11). On the hospital side, a previous study reported that the overall compliance was 31%; physicians had the lowest rate of compliance at 15%, while nurses had the highest rate at 39%; internal medicine had the lowest rate at 16%, while the intensive care unit had the highest rate at 40% (12). Barriers to handwashing compliance among healthcare workers included limited resources, patient overcrowding, shortage of staff, allergic reactions to hand sanitizers, and lack of awareness (13). For criterion 1, one of the criteria to ensure that COVID-19 disease prevention and control at hospitals was unified and ran smoothly was the establishment of a steering committee on disease prevention that developed a plan and assigned work to each specific group of medical staff. This criterion was also emphasized in the international guidelines (10, 14).
However, despite good compliance in several criteria, there are still significant gaps in implementation in hospitals. Criterion 5 “Infection prevention for some crowded areas” had the lowest level of compliance, followed by criteria 6 and 7. For criterion 5 “Infection prevention for some crowded areas”, social distancing within hospitals was vital in reducing nosocomial spread, especially in hospitals where the majority of patients were nursed in multi-bedded cohort rooms, rather than in single-occupancy rooms. Preventing infections in healthcare facilities was uniquely difficult and important. Healthcare facilities were areas of mass gathering that cannot be closed during a lockdown. This was understandable since these were the areas where many groups were gathered including (1) patients, (2) caregivers, (3) medical staff, and (4) service staff. Given the limited space of these areas, implementing person-to-person distancing in these areas presents a major challenge for hospitals. Other countries faced a similar situation based on their experience (13, 15, 16). For criterion 6 “Management of safety of patients and patient families”, the average score in all hospitals was low. This could be explained by the fact that there were shortages of personal protective equipment and medical consumables. Frontline health professionals had a distinctly higher risk of infection, especially those who re-use personal protective equipment (PPE) or did not have adequate PPE (17). This was one of the major challenges in ensuring the safety of both patients and the medical staff. This result was similar to previous studies in Vietnam and other countries (18–20). Moreover, the lack of space in hospitals, especially at the grassroots level, limits the ability of hospitals to provide separate spaces for patients with respiratory diseases and those suffering from other diseases. For criterion 7 “Healthcare worker safety management”, the greatest problem in this criterion was “Management of risk from outsourced workers”. Non-hospital staff had many potential uncontrollable risks. However, it could be seen that, at present, hospitals, especially ministerial hospitals and private hospitals, did not have clear mechanisms and regulations on the management of this group of staff. If not well controlled, although the hospital might have other satisfactory conditions, the hospital might still be at high risk of experiencing a COVID-19 outbreak with an external source. Notably, this was related to criterion 2 “Training”. Sufficient knowledge and on-premises work experience might improve the ability of healthcare professionals to better handle COVID-19, since incorrect attitudes and practices directly increase the risk of infection (21).
Challenges in ensuring hospital safety during the COVID-19 pandemic included the lack of preparedness before COVID-19 and other pandemics; having experience in responding to a pandemic and taking measures to prepare for a pandemic was one of the factors that help ensure a hospital’s rapid response in an emergency case. A previous study in health facilities in Hanoi showed that there were statistically significant differences in “Emergency preparedness” between health facilities in the area with and without positive cases, such that those with no positive cases had better performance. This result revealed the foresight of areas without positive cases, where the COVID-19 prevention and control work were implemented preemptively. In contrast, areas with existing positive cases were less able to be proactive in COVID-19 prevention and control (18).
Limited hospital facility, space, and equipment was another challenge in the field of hospital preparedness for biological events. Facilities, equipment, human resources, and ancillary spaces should be considered as capacity building in advance. The WHO 2020 stated that, due to the COVID-19 pandemic, protective equipment is a major challenge in hospitals (22).
Shortage of human resources and limitations in training and knowledge transfer were also major barriers. Hoang Van Minh et al. revealed that with the existing health workforce, it would be impossible to address the future burden of disease (18). The results revealed the importance of training and practical programs for healthcare providers, and they stated that different types of training programs are provided in hospitals. However, given the rapid change of the COVID-19 pandemic, the guideline was speedily updated, causing difficulties in medical staff to follow the guideline.
Another identified challenge was patient attitude and compliance. Participants refer to the non-cooperation of patients and caregivers in the implementation of COVID-19 prevention regulations at the hospital. This might be due to improper attitude of patients and caregivers about the epidemic. A study in Ho Chi Minh City showed that, although 93.7% had sufficient knowledge, only 76.3% had a supportive attitude and 57.7% had correct practice on COVID-19 prevention measures (23). One of the challenges they stated was that patients are not familiar with biological events and do not take them seriously. They also did not have a proper understanding of biological events and threats and do not properly understand the significance of these events. Health education communication strategies about COVID-19 should be promoted to improve the attitudes of patients and caregivers.
Study limitations: This study still had some limitations, such as using secondary data at one point in time; thus, it was not possible to assess the improvement in hospitals over time. Second, the study did not include all hospitals in Vietnam; the study results might not be applicable to unselected hospitals, such as some hospitals in the Ministry of Public Security. However, this study was selected in 1,398 hospitals nationwide with different characteristics (such as type, ownership, and regions). Third, the study used in-depth interviews to understand the hospital’s difficulties and challenges from the participants in different positions (from leader to staff) and in different hospitals (from central, regional, provincial, and private hospitals). The information might partly reflect the difficulties and challenges faced by hospitals at different levels of the health system. However, it was necessary to have large-scale quantitative surveys to help provide a complete picture of the current state of hospital safety and the challenges that hospitals are facing, thereby offering appropriate interventions and policies for hospitals to enhance the safety of the hospitals against the COVID-19 pandemic.
Conclusions
Overall, the hospitals well implemented the criteria according to Decision 3088/QD-BYT to ensure the safety of the hospital before the COVID-19 pandemic. The proportion of hospitals classified as “safe hospital”, “safe hospital with moderate level”, and “unsafe hospital” was 91.7%, 7.3%, and 1.0%, respectively. The rate of “safe hospital” was lowest in the ministerial hospital group and highest in the central level group. Hospitals in the private sector had a higher average score of “safe hospital” compared with public hospitals. Challenges in ensuring hospital safety in public and private hospitals related to COVID-19 transmission include lack of preparedness before COVID-19 and other pandemics; limited hospital facility, space, and equipment; shortage of human resources and limitations in training and knowledge transfer; and patient attitude and compliance in declaring health conditions or proper understanding of biological events and threats. Relying on the study results, it suggested that the hospitals should continue to complete the system of emergency response to epidemics and strengthen training and ensure the training and practice of non-hospital staff in COVID-19 prevention. The MOH of Vietnam should adapt the criteria in Decision 3088/QD-BYT to be more suitable to the new phase of the pandemic as we move towards “living with COVID”. Furthermore, we recommend that the MOH of Vietnam work to develop mechanisms or regulations that require hospitals to regularly report on disease preparation and responses as an ongoing situation for future pandemic preparedness.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
NT and LK conducted the study. NT and BA developed the structure and draft of the manuscript. All authors contributed to the study conception, design, and revising of the article, and approved the final version of the manuscript.
Acknowledgments
All authors would like to thank the MOH and all participants from hospitals in the public and private sectors who agreed to contribute to this research despite their busy schedule.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fitd.2022.940268/full#supplementary-material
References
1. Vietnam Ministry of Health. News 3/7: Ho chi minh city set a record for the number of COVID-19 cases in a day, Vietnam surpassed the milestone of 19,000 cases (2021). Available at: https://ncov.moh.gov.vn/vi/web/guest/-/6847426-5295 (Accessed 05 July 2021).
2. Vietnam Ministry of Health. Decision on the issuance of “Temporary guidance on supervision and prevention, against COVID-19. (2020) Hanoi, Vietnam.
3. World Health Organization. Safe hospitals (2021). PAHO/WHO | Pan American Health Organization. Available at: https://www.paho.org/en/health-emergencies/safe-hospitals (Accessed 05 July 2021).
4. Ledford H. Six months of COVID vaccines: what 1.7 billion doses have taught scientists. London: Nature Publishing Group (2021).
5. Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med (2021) 27(6):964–80. doi: 10.1038/s41591-021-01381-y
6. John Hopkins University and Medicine. Covid-19 dashbroad by the center for systems science and engineering (2021). John Hopskin University. Available at: https://coronavirus.jhu.edu/map.html (Accessed 05 July 2021).
7. World Health Organization. Rapid hospital readiness checklist: a module from the suite of health service capacity assessments in the context of the COVID-19 pandemic: interim guidance, 25 November 2020. (2020) Geneva. 144:2119–2132. doi: 10.2147/RMHP.S305959
8. Vietnam Ministry of Health. Decision 3088/QD-BYT issued on 16/07/2020 criteria for hospitals safe from COVID-19. (2020) Hanoi, Vietnam.
9. Takashima K, Wada K, Tra TT, Smith DR. A review of vietnam’s healthcare reform through the direction of healthcare activities Vol. 22. DOHA: Environmental health and preventive medicine (2017) 22(1):74. doi: 10.1186/s12199-017-0682-z
10. World Health Organization. Hospital preparedness for epidemics (2014). Available at: www.who.int/publications/i/item/hospital-preparedness-for-epidemics (Accessed 05 July 2021).
11. Huong LTT, Hoang LT, Tuyet-Hanh TT, Anh NQ, Huong NT, Cuong DM, Quyen BTT. Reported handwashing practices of Vietnamese people during the COVID-19 pandemic and associated factors: a 2020 online survey Vol. 7. AIMS Public Health (2020) 7(3):650–63. doi: 10.3934/publichealth.2020051
12. Le CD, Lehman EB, Nguyen TH, Craig TJ. Hand hygiene compliance study at a Large central hospital in Vietnam. Int J Environ Res Public Health (2019) 16(4):607. doi: 10.3390/ijerph16040607
13. Wilkinson LS, Moosa S, Cooke R, Muller AM, Boyles TH. Preparing healthcare facilities to operate safely and effectively during the COVID-19 pandemic: The missing piece in the puzzle. S Afr Med J (2020) 110(9):835–6. doi: 10.7196/SAMJ.2020.v110i9.150
14. World Health Organization. 2019 novel corornavirus ( 2019-nCoV): strategic preparedness and response plan. (2020) Geneva.
15. Ortega-García JA, R-Marín M, Cárceles-Álvarez A, Campillo I, López F, Claudio L. Social distancing at health care centers early in the pandemic helps to protect population from COVID-19. Environ Res (2020) 189:p.109957. doi: 10.1016/j.envres.2020.109957
16. Wee LE, Conceicao EP, Sim XYJ, Aung MK, Tan KY, Wonget HM. Minimizing intra-hospital transmission of COVID-19: the role of social distancing. J Hosp Infect (2020) 105(2):113–5. doi: 10.1016/j.jhin.2020.04.016
17. Iannone P, Castellini G, Coclite D, Napoletano A, Fauci AJ, Iacorossi L, D'Angelo D, Renzi C, La Torre G, Mastroianni CM, Gianola S. The need of health policy perspective to protect healthcare workers during COVID-19 pandemic. a grade rapid review on the N95 respirators effectiveness. PLoS One (2020) 15(6):e0234025. doi: 10.1371/journal.pone.0234025
18. Van Hoang M, Tuan Tran A, Thu Vu T, Duong TK. Covid-19 preparedness and response capability: A case study of the Hanoi primary healthcare system. (2021) 14:11786329211019224. doi: 10.1177/11786329211019224
19. Yoshioka-Maeda K, Iwasaki-Motegi R, Honda C. Preventing the dysfunction of public health centres responding to COVID-19 by focusing on public health nurses in Japan. J Adv Nurs (2020) 76(9):2215–6. doi: 10.1111/jan.14409
20. Zeenny RM, Ramia E, Akiki Y, Hallit S, Salameh P. Assessing knowledge, attitude, practice, and preparedness of hospital pharmacists in Lebanon towards COVID-19 pandemic: a cross-sectional study. J Pharm Policy Pract (2020) 13(1):54. doi: 10.1186/s40545-020-00266-8
21. Zhang M, Zhou M, Tang F, Wang Y, Nie H, Zhang L, et al. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in henan, China. J Hosp Infect (2020) 105(2):183–7. doi: 10.1016/j.jhin.2020.04.012
22. World Health Organization. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages. World Health Organization (2020) Geneva. interim guidance, 6 April 2020.
Keywords: Decision 3088/QD-BYT, safety hospital, COVID-19, health system preparedness, health system responsiveness, Vietnam
Citation: Thu NTH, Anh BTM, Khanh LB, Anh PT and Luong DH (2022) Hospital safety preparedness during the COVID-19 pandemic: Lessons learned from Vietnam. Front. Trop. Dis 3:940268. doi: 10.3389/fitd.2022.940268
Received: 10 May 2022; Accepted: 24 August 2022;
Published: 06 October 2022.
Edited by:
Harapan Harapan, Syiah Kuala University, IndonesiaReviewed by:
Olushayo Oluseun Olu, World Health Organization, South SudanAbhay Machindra Kudale, Savitribai Phule Pune University, India
Copyright © 2022 Thu, Anh, Khanh, Anh and Luong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bui Thi My Anh, YnVpdGhpbXlhbmhAaG11LmVkdS52bg==
†ORCID: Jakob Triebel, https://orcid.org/0000-0003-1678-6397
 Nguyen Thi Hoai Thu
Nguyen Thi Hoai Thu Bui Thi My Anh
Bui Thi My Anh Luong Bao Khanh
Luong Bao Khanh Pham Tran Anh3
Pham Tran Anh3