- 1Papua Agency of National Institute of Health Research Development, Jayapura, Indonesia
- 2Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia
- 3Indonesia Research Partnership on Infectious Disease, Jakarta, Indonesia
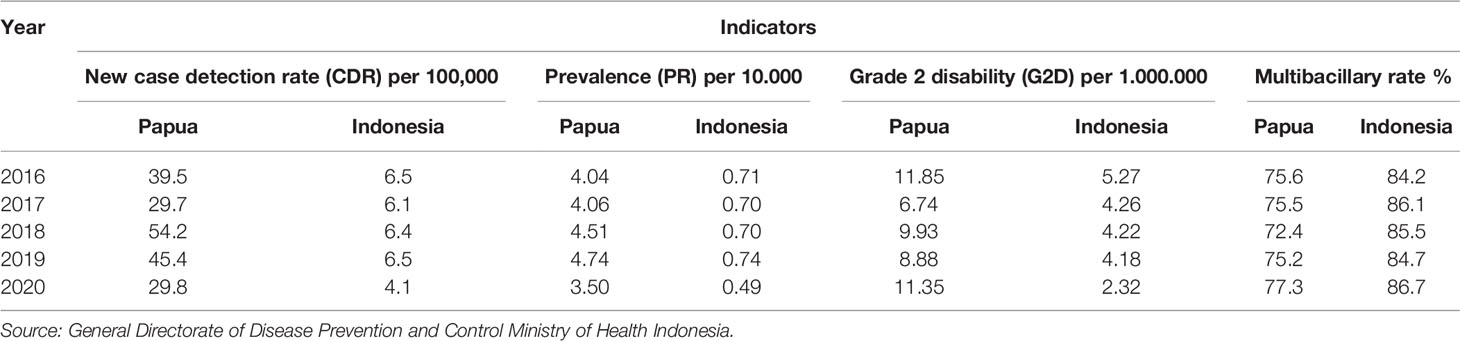
In 2020 we witnessed the global pandemic of COVID-19. Papua, Indonesia announced the first case of COVID-19 on 7 March 2020, and reached 41,137 positive cases with a total of 1,183 fatality cases in August 2021. In the midst of the effort to handle COVID-19, this area of hyper-endemic tropical diseases, including leprosy, has also had to cope with these established problems. Some leprosy indicators have shown decreased performance. The new case detection rate (NCDR) per 100,000 population in Papua Province decreased from 45.36 in 2019 to 29.75 in December 2020. Grade 2 disability (G2D) proportion amongst the new cases increased from 9.0% in 2019 to 11.4% in 2020. There was a 27% decrease of the proportion of child leprosy, following the decrease of elementary school surveys from 6.1% in 2019 to only 1.0% in 2020. Although precautions should be taken, it should be done to minimalize impacts not only for the current pandemic, but also the existing neglected tropical diseases (NTDs). The central government should optimize their functions as a control system to maintain standard services and to monitor the local health authority. The current guidelines regarding implementation of NTD programs during the COVID-19 pandemic should be evaluated and revised, and followed by adequate explanation and proper training to accommodate better services. Emphasis on prevention and early detection should be considered as the main way forward to strengthen the health system.
Introduction
Papua is Indonesia’s easternmost province, which encompasses the western half of New Guinea and several other islands. It is one of the big islands in Indonesia and the home of natural biodiversity with diverse ecosystem characteristics from the mountain, rainforest, and coastal area. The Papua population are dispersed throughout remote, rural, and urban areas. The geographic profile combined with less development of infrastructure, low knowledge, and less awareness exacerbate the health system problems in Papua Province, Indonesia (1).
Amid the struggle combating many infectious diseases, in 2020, we witnessed the global pandemic of COVID-19 that was firstly reported in China (2) and spread around the world including almost all provinces in Indonesia (3). Indonesia’s government announced the first case on 7 March 2020, followed by the first COVID-19 case in Papua on 22 March 2020. By the end of August 2021, COVID-19 in Indonesia had reached more than 4 million confirmed cases, including 41,137 cases in Papua, with 1,183 (2.8%) fatality cases (4). On the other hand, Papua still has to cope with many infectious diseases such as HIV, TB, and malaria. Besides them, it also has to contend with neglected tropical diseases (NTDs) such as filariasis, yaws, soil-transmitted diseases, and leprosy (5).
According to the WHO list, leprosy is a neglected disease. Indonesia is the third ranked among leprosy cases after India and Brazil (6). Papua Province is among the highest endemicity provinces in Indonesia with a new case detection rate (NCDR) of 45.4 per 100,000, while the national NCDR was 6.5 in 2019. The World Health Organization (WHO) released the Global Leprosy Strategy 2016-2020 aimed at accelerating action towards a leprosy-free world. It contains three main strategies: strengthen government ownership, coordination, and partnership; stop discrimination and promote inclusion; and stop leprosy and its complications (7).
As typical of neglected diseases, the leprosy control program lacked resources and was less prioritized by health authorities (8). However, the Ministry of Health (MoH) Indonesia planned to target leprosy elimination in all districts by 2030 (9), in line with the WHO strategy (10). To reach this target, MoH mobilized intensive case finding (ICF) in all endemic provinces. Funding is provided for primary health care providers (PHCs) to perform active screening in villages and in elementary schools to increase the leprosy detection rate and treatment coverage (9).
Since 2017, following the national health development strategy, Papua has put a lot of effort into combating leprosy to reach the elimination target by 2030; these efforts consisted of the FKF (Filariasis, Kusta, and Frambusia) team, Cinta Sobat, Sobat Kusta, and Post-Exposure Chemoprophylaxis programs. The leprosy health care worker community initiated the FKF team; an integrated door-to-door active finding team with filariasis and yaws. Cinta Sobat is a social innovation to increase the case detection rate among school-aged children. Sobat Kusta is a self-care group for preventing permanent disability and promoting knowledge and awareness about leprosy. The Post-Exposure Chemoprophylaxis program was in planning and preparation and should have been launched in early 2020.
Unfortunately, the COVID-19 pandemic has reached Papua. The provincial government closed all access to Papua Province by closing the airport and port from 26 March to May 2020. It successfully reduced the community transmission during this period. Disease control programs and routine healthcare services were shifted to support national efforts to contain the COVID-19 morbidity and mortality in the community (11). COVID-19 has shifted the focus on management. The provincial government reallocated local resources to support COVID-19 testing, contact tracing, and treatment, developed crisis and emergency teams, limited service hours in public facilities, and tightened the health protocol in the community. A big question emerged: what will be the impact of COVID-19 on ongoing efforts to control infectious diseases, including leprosy?
We took examples of leprosy management in two districts in Papua to explore how COVID-19 has affected some interventions that were rolled out, such as the development of local policy for leprosy control, capacity building of health staff, and intensive case finding activities. Lessons learned from the current experiences should be used for enhancing health care delivery approaches to reach the goal of zero leprosy in 2030.
Subsections Relevant for the Subject
Current Policies for Preventing and Managing Leprosy During the COVID-19 Pandemic in Indonesia
Recommendations for leprosy services during the COVID-19 pandemic include suspending active case finding and distribution of chemoprophylaxis. Treatment should be continued by giving 2-3 months of multi drug therapy (MDT) supplies to reduce the frequency of visits to the health facilities (12). Examination of neural function should be done every 3 months to prevent disability and monitor adverse reactions to the MDT. The WHO issued interim guidance for implementing NTD programs (including leprosy) on 1 April 2020. It contains a recommendation to postpone NTD surveys, active surveillance, and community campaigns (13). On 27 July 27 2020, WHO published a new guideline recommending risk assessment and thorough planning to restart essential activities (14).
Leprosy Program Management Before COVID-19, Experiences From Papua
Following the decentralization of the health system in Indonesia, Papua Province has been provided with the authority to direct their health policies, priorities, and finances. The national health authority plays a role as a national standard pacesetter and undertakes monitoring and evaluation. Financially, the MoH allocates funds to support the execution of country health programs in every province and provides operational costs for every primary PHC, namely Biaya Operasional Kesehatan (BOK; operational health fund).
About 50% of districts in Papua Province have innovated their capacities to reach the national target. In addition to ICF funded by MoH, Biak and Keerom Districts have had a breakthrough in active case finding in villages by integrating the leprosy program in routine elderly and toddler mobile clinics provided by PHCs. Four districts planned and allocated the budget for chemoprophylaxis in 2019-2020. Many leprosy self-treatment communities were developed by the health authorities partnering with a research institute or non-government organization (NGO) to promote the treatment for disability and improve knowledge.
Leprosy Program Management During COVID-19, Experiences From Papua
We assessed the action of leprosy program management during COVID-19 and the impact of COVID-19 on the program indicators. We conducted an in-depth interview with leprosy program managers guided with semi-structured questionnaires in Keerom and Biak Districts, Papua, Indonesia. We also collected leprosy data from the district, provincial, and national central databases. We officially submitted a request to use national data of the General Directorate of Disease Prevention and Control, and provincial data of the Papua Provincial Health Office.
A new guideline for implementing leprosy services during the COVID-19 pandemic was shared through an online platform. As a result, the guideline was left unread. The local level has created its policies to survive during the COVID-19 pandemic, which has basically stopped active case finding and all community programs.
Most of the available resources have been re-allocated for COVID-19, including trained cadres and health workers. Times spent in the PHC have also been limited (50% of human resources, with working hours from 09.00-12.00) due to the working from home mandate and mobility restriction. Several PHCs have to be closed for a while as some members tested positive for COVID-19. Implementation of training related to COVID-19 has been varied. According to the staff of Biak and Keerom Districts, training has been conducted for COVID-19 testing, tracing, and treatment. Officers or cadres received no training about COVID-19 and leprosy-related training to handle this situation. It was just business as usual.
There was a shortage of MDT for 1 month in Keerom District and 6 months in Biak District. The limited supply of MDT has caused a very high number of drop out, reaching 50% of all cases. In addition, the limitation of service hours in PHCs reduced the access to leprosy treatment. However, there was no problem in the availability of equipment recommended to follow the health protocol for preventing COVID-19 as some budgets were re-allocated for personal protective equipment (PPE) procurements. In the case of management, submission of the annual report was delayed mostly because some staff were infected with COVID-19 on top of disruption by additional tasks related to COVID-19.
Leprosy Program Indicators Before and After COVID-19
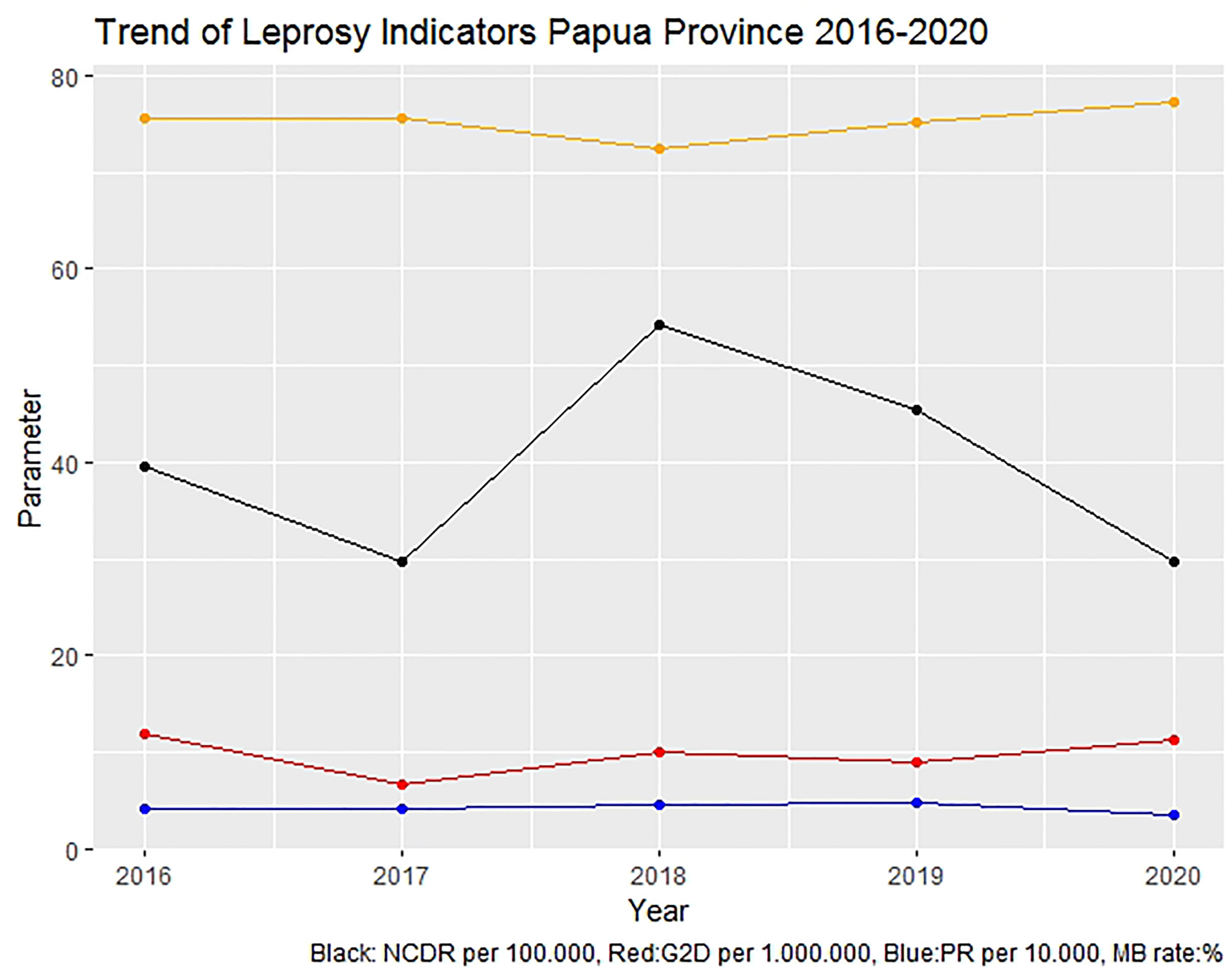
A significant increase of NCDR from 2016-2017 to 2018-2019 was caused by activating an active case-finding program organized by MoH, but it has significantly decreased during the pandemic (Table 1). The number of NCDR during the pandemic was worse than before the national program of active case finding was launched in 2017. Multibacillary cases were constantly increased in the past 3 years, even when the NCDR was highly decreased in 2020. Presumptively, national active case finding had a good impact on reducing the disability rate during 2018 - 2019, but the disability rate increased in 2020.
The NCDR per 100,000 population of Papua Province decreased from 45.36 in 2019 to 29.75 in December 2020 (Figure 1). The proportion of multibacillary (MB) leprosy among the new cases increased from 75.2% to 77.3%. Grade 2 disability (G2D) proportion amongst the new cases increased from 9.0% in 2019 to 11.4%. There was a 27% decrease in children’s leprosy, following the decrease of elementary school surveys (6.1% in 2019 to only 1.0% in 2020). Some districts in Papua, including Keerom District, totally discarded the elementary children survey during 2020.
Discussion
Lesson Learned From the Current Situation
The measures recommended to reduce transmission of COVID-19, such as isolation, social distancing, and restrictions on movement, create barriers for accessing health care in addition to those usually present. Thus, NTDs disproportionately affect the most socially and economically vulnerable individuals in low and middle-income countries (LMICs), who already experience considerable barriers to accessing health services. In addition, the fear of COVID-19 infection reduced availability of services due to restructured health care provision, and reduced staffing which limited access to the services. Thus, the COVID-19 pandemic will likely severely interrupt health systems worldwide, especially in LMICs, over the coming months and years.
The COVID-19 pandemic has highlighted the consequences of major disruptive events on population health and the immediate impact on the delivery of leprosy management. It has also exposed the fragility of health systems. The consequences of health service disruptions are likely to last for years, as the ability to recover is impaired by economic devastation related to the pandemic. The long-term impact of service interruptions on NTD control and disability is unknown; but most likely will be devastating. Beyond the effort from the central government to provide guidelines for providing leprosy services and management during the COVID-19 pandemic, local staff have learned almost nothing new due to lack of training.
Sustainable Funding; Both International and National
The fight against leprosy is being prolonged, and in some places, has been slowed down by several interconnected challenges. The first is the lack of robust, predictable, and sustained international and domestic financing, compounded by the difficulties in sustaining political commitment and ensuring regional collaboration at the highest level. The lack of resources across the health sector has compromised the delivery of good-quality services. Weak surveillance, monitoring, and evaluation systems fail to adequately identify gaps in program coverage and track changes in disease burden. Political commitment linked to resources and actions is required to ensure that all those in need have access to the appropriate mix of interventions for leprosy and other public health priorities without financial hardship.
Understanding the Urgency of Leprosy – It Should Not Only Be Measured by Fatality
The gap in priority between so-called priority diseases and neglected diseases has been caused mainly due to the paradigm of fatality. Leprosy is thought of as a disease with a low fatality since it could not affect mortality, except in cases with a complication during the treatment such as reaction or Dapsone Hypersensitivity Syndrome (DHS). However, leprosy is the only infectious disease that causes disability, even permanent disability. Disability is life-threatening since it decreases productivity and raises the stigma. In this view, COVID-19, known for its high fatality rate, worsens leprosy’s neglected status.
There are fewer published data about the clinical impact of COVID-19 in people with leprosy. However, limiting health service access in PHC and competing for priority of hospitalization due to COVID-19 may increase the challenge of leprosy complication management such as leprosy reaction (type 1, type 2, and ENL) and DHS. Leprosy reactions are immune-mediated episodes of inflammation that are often self-limiting but may also be severe and prolonged (15). Leprosy reactions are the underlying cause of most disabilities in leprosy and, thus, many of the psychosocial consequences that may follow (16). DHS is a severe idiosyncratic drug reaction characterized by the clinical triad of fever, rash, and systemic involvement (most commonly of the liver and the hematologic system), which can cause severe organ dysfunction and manifest 4 to 6 weeks after the initiation of therapy (17). It is a rare life-threatening reaction globally with a range of incidence of 2% to 12% with a fatality rate of 9.9% (18). Due to the dominant HLA-B*13:01 carrier in Papuan ethnic groups, the incidence rate of DHS is highly reported among leprosy patients (11%) treated by dapsone as the significant component in MDT (19). It is necessary to improve effective engagement between leprosy health workers or dermatologists and the undergoing treatment patients and release from treatment (RFT) patients. Adoption of telemedicine supported with active education about the possibility of leprosy complications to raise awareness among leprosy-related workers can be a good approach during this pandemic.
Problems with the Disappearance of Active Case Finding for Leprosy Patients and Delayed Treatment
MDT is a complex antibiotic that has been supplied by WHO since the 1990s. Multibacillary patients are treated using MDT for 12 months, while paucibacillary patients are treated for 6 months. These drugs effectively enhance leprosy elimination in many countries. Administering MDT treatment in the early stages prevents disability (damage to the skin, nerves, limbs, and eyes) among leprosy-affected people and interrupts the active transmission of Mycobacterium leprae from leprosy patients to their contacts (20). This makes early diagnosis of leprosy an efficient method of treatment, not only to prevent irreversible damages but also to contain transmission. The disappearance of active case finding has potentially decreased early diagnosis and treatment, further increasing the risk of disability and active transmission. Furthermore, delayed MDT treatment due to limited access to PHC during the COVID-19 pandemic for leprosy patients has increased the possibility of unexpected drop out from treatment, further expanding the possibilities of drug resistance. The COVID-19 pandemic is also a considerable challenge for implementing chemoprophylaxis prevention because of logistic shortage, and home visit screening required as a part of chemoprophylaxis distribution has been banned.
For leprosy-affected people, COVID-19 has a massive impact, especially in places with fragile health systems like Indonesia, because all the non-urgent hospital consultations and admissions are being discouraged because of increasing concern about COVID-19 cases. This has shifted the hospital priority toward COVID-19 responses, putting other health conditions at a lower priority at the moment. This situation has created a gap in health service needs for leprosy patients. Active case finding has been suspended in the context of COVID-19, and following WHO recommendation in May 2020 (21), the significant decrease of NCDR is alarming. The same experiences have been reported in Northeast Brazil (22) and India (23).
The observed decrease in the number of new leprosy cases registered in Northeast Brazil may indicate a major setback in the fight against leprosy, both because of the decrease in the number of diagnoses made and because of the operational losses that the pandemic caused in leprosy surveillance programs. The potential result is an increase in the hidden prevalence of leprosy and maintenance of the transmission chain in the community (22). In India, estimates suggest that 6 in 10 leprosy cases may go undetected if quality ACF activities are not implemented. G2D rates will increase further, and an important proportion of women, children, and marginalized communities will go undiagnosed (23).
Recommendations to Improve the Current Policies
Since the local authority faces a new situation and extreme transition due to the COVID-19 pandemic, leadership and central government control are critically important. In light of leprosy, new guideline distribution and training should be performed in an effective communication forum at a national level instead of distributing the guideline through a focal person. Furthermore, advanced monitoring and evaluation to ensure the implementation in the field should be implemented. Thus, the provincial health authority may locally initiate a breakthrough for combating leprosy during the pandemic era. However, the central government is supposed to be an eager initiator of developing new leprosy strategies at the national level (Box 1).
Box 1. Policy recommendations
Central government:
● Planning a new strategy, chasing the setback of leprosy elimination during the COVID-19 pandemic.
● Approaching and advocating for the local government to improve their support and commitment in the leprosy program.
● Renewing, distributing, training, and mobilizing a guideline to reactivate active case finding, contact survey, school survey, and chemoprophylaxis treatment.
Provincial/district health authority:
● Mandating leprosy program managers from all districts for organizing the budget allocation in every PHC for leprosy activities.
● Activating leprosy active case finding by integrating with other activities, such as elderly and toddler mobile clinics.
● Activating school surveys in a new format, such as integrating it into the student vaccination program.
A decrease in NCDR with an increase in disability at the provincial level exposes the persistent leprosy burden. After living with the pandemic for almost 2 years, a new strategic plan for chasing the setback in the leprosy elimination target is a necessity. Activation of active case finding, contact tracing, and implementation of chemoprophylaxis with an adequate health protocol should be encouraged. Active case finding in elementary schools to improve children’s leprosy detection rate can be initiated in a new format, using an integrated activity following the COVID-19 vaccination program among students. Politically, MoH plays an urgent role in approaching and advocating for the local government to improve their support and commitment to the leprosy program, especially in hyper-endemic areas like Papua Province. Financially, a lesson learnt from Biak District can be implemented at the provincial level. Since the source of sustainable funding is available in PHC through the BOK program, a provincial health authority has to mandate all districts’ leprosy program managers for organizing the budget allocation in every PHC for leprosy activities. The central government should optimize their functions as a control system to maintain standard services and monitor the local health authority. The current guidelines regarding the implementation of the NTD program during the COVID-19 pandemic should be evaluated and revised, followed by an adequate explanation and proper training to accommodate better services. Emphasis on prevention and early detection should be considered as the primary way forward to strengthen the health system.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements.
Author Contributions
HK and AD conceived and prepared the first draft of the manuscript. MR and AO critically reviewed the draft. All the authors approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are grateful to the contributions of the leprosy program managers of Keerom and Biak District, Papua Province who trusted us with their stories. We thank the General Directorate of Disease Prevention and Control MoH Indonesia who supported us with the data. We thank Leprosy Research Initiative and The Netherland Leprosy Relief Indonesia for the publication grant. We also thank all respondents who participate in this study.
References
1. Tjandrarini DA, Dharmayanti I, Suparmi E, Nainggolan E. Indeks Pembangunan Kesehatan Masyarakat 2018. 1st. Trihono, et al, editors. Jakarata: Lembaga Penerbit Balitbangkes (2018).
2. Li Q, Guan X, Wu P, Wang X. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N Engl J Med (2020) 382(13):1199–207. doi: 10.1056/NEJMoa2001316
3. Aisyah DN, Mayadewi CA, Diva H, Kozlakidis Z, Siswanto, Adisasmito W. A Spatial-Temporal Description of the SARS-CoV-2 Infections in Indonesia During the First Six Months of Outbreak. PloS One (2020) 15(12 December):1–14. doi: 10.1371/journal.pone.0243703
4. Papua Provincial Health Office. PAPUA COVID 19 REPORT UPDATE 31 AUGUST 2021.Pdf. Jayapura: Papua Privincial Health Office (2021).
5. Pongtiku A, Kayame R, Sumolang IV, Wopari BIS, Rumainum A. Atlas of Neglected Tropical Diseases in Papua: The Illustrative Book for the Frontline Health Workers in Detection, Diagnostics and Treatment. 1st. Jayapura:Papua Province Health Office (2016).
6. World Health Organization. World Health Organization. Global Leprosy (Hansen Disease) Updat: Time to Step-Up Prevention Initiatives. Wkly Epidemiol Rec (2020) 95(36):417–40.
7. World Health Organization. Global Leprosy Strategy 2016–2020: Accelerating Towards a Leprosy-Free World. New Delhi: World Health Organization, Regional Office for South-East Asia (2016). Available at: https://apps.who.int/iris/bitstream/handle/10665/208824/9789290225096_en.pdf?sequence=14&isAllowed=y.
8. Wibawa T, Satoto TBT. Magnitude of Neglected Tropical Diseases in Indonesia at Postmillennium Development Goals Era. J Trop Med (2016) 2016:1–9. doi: 10.1155/2016/5716785
9. Kementerian Kesehatan Republik Indonesia. Peraturan Menteri Kesehatan Republik Indonesia Nomor 11 Tahun 2019 Tentang Penanggulangan Kusta (2019). Available at: http://hukor.kemkes.go.id/uploads/produk_hukum/PMK_No:11_Th_2019_ttg_Penanggulangan_Kusta.pdf.
10. World Health Organization. Towards Zero Leprosy. Global Leprosy (Hansen’s Disease) Strategy 2021–2030. New Delhi: World Health Organization, Regional O ce for South-East Asia (2017).
11. Kementerian Kesehatan Republik Indonesia. Keputusan Menteri Kesehatan Republik Indonesia Nomor HK.01.07/MenKes/413/2020 Tentang Pedoman Pencegahan Dan Pengendalian Corona Virus Disease 2019 (Covid-19), Covid-19 Control and Prevention. HK.01.07/MENKES/247/2020. Jakarta: Ministry of Health Republic of Indonesia (2020).
12. General Directorate of Disease Prevention and Control Ministry of Health Indonesia. SE Pelaksanaan Pencegahan Dan Pengendalian Penyakit Kusta Dan Frambusia Dalam Situasi Pandemi CoVid-19.Pdf. Jakarta: Ministry of Health Republic of Indonesia (2020).
13. World Health Organization. COVID-19: WHO Issues Interim Guidance for Implementation of NTD Programmes. Geneva: World Health Organization (2020). Available at: https://www.who.int/neglected_diseases/news/COVID19-WHO-interim-guidance-implementation-NTD-programmes/en/.
14. World Health Organization. Considerations for Implementing Mass Treatment, Active Case-Finding and Population-Based Surveys for Neglected Tropical Diseases in the Context of the COVID-19 Pandemic. Geneva: World Health Organization (2020).
15. Walker SL, Lebas E, Doni SN, Lockwood DNJ, Lambert SM. The Mortality Associated With Erythema Nodosum Leprosum in Ethiopia: A Retrospective Hospital-Based Study. PloS Negl Trop Dis (2014) 8(3):e2690. doi: 10.1371/journal.pntd.0002690
16. World Health Organization. Leprosy/Hansen Disease: Management of Reactions and Prevention of Disabilities. Technical Guidance. New Delhi: World Health Organization, Regional Office for South-East Asia (2017).
17. Zhang F-R, Liu H, Irwanto A, Fu X-A, Li Y, Yu G-O, et al. HLA-B*13:01 and the Dapsone Hypersensitivity Syndrome. N Engl J Med (2013) 369(17):1620–8. doi: 10.1056/NEJMoa1213096
18. Schmitt J, Lorenz M, Wozel G. Hypersensitivity Reactions to Dapsone: A Systematic Review. Acta Derm Venereol (2012) 92(2):194–9. doi: 10.2340/00015555-1268
19. Krismawati H, Irwanto A, Pongtiku A, Irwan ID, Maladan Y, Sitanggang YA, et al. Validation Study of HLA-B*13:01 as a Biomarker of Dapsone Hypersensitivity Syndrome in Leprosy Patients in Indonesia. PloS Negl Trop Dis (2020) 14(10):e0008746. doi: 10.1371/journal.pntd.0008746
20. Sansarricq H, Diseases, U.B.S.P. for R. and T. @ in T. Multidrug Therapy Against Leprosy: Development and Implementation Over the Past 25 Years. 1st. Sansarricq H, editor. Geneva:World Health Organization (2004).
21. World Health Organization. Community-Based Health Care, Including Outreach and Campaigns, in the Context of the COVID-19 Pandemic. Interim Guidance. May 2020 (No Date). Geneva & New York: World Health Organization, International Federation of Red Cross and Red Crescent Societies and the United Nations Children’s Fund (2020).
22. Matos TS, Nascimento VA, Carmo RF, Moreno de Oliveira Fernandes TR, Souza CDF, et al. Impact of the COVID-19 Pandemic on the Diagnosis of New Leprosy cases in Northeastern Brazil, 2020. Int J Dermat (2021) 60(8):1003–6.
Keywords: leprosy, COVID-19, Papua, Indonesia, neglected tropical diseases (NTD)
Citation: Krismawati H, Rochman MF, Oktavian A and Diana A (2022) Sustained Actions in Combating Neglected Tropical Diseases during the COVID-19 Pandemic: Lessons Learned From the Leprosy Program in the Hyper-Endemic Area in Papua Province, Indonesia. Front. Trop. Dis 2:782255. doi: 10.3389/fitd.2021.782255
Received: 24 September 2021; Accepted: 30 December 2021;
Published: 03 March 2022.
Edited by:
Katy Shaw-Saliba, National Institute of Allergy and Infectious Diseases (NIH), United StatesReviewed by:
Fekri Dureab, Akkon College of Human Sciences, GermanyCopyright © 2022 Krismawati, Rochman, Oktavian and Diana. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hana Krismawati, aGtyaXNtYXdhdGlAZ21haWwuY29t
 Hana Krismawati
Hana Krismawati Mohhamad Fadjri Rochman1
Mohhamad Fadjri Rochman1 Aly Diana
Aly Diana