
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Trop. Dis., 18 January 2022
Sec. Antimicrobial Resistance
Volume 2 - 2021 | https://doi.org/10.3389/fitd.2021.768842
This article is part of the Research TopicAntimicrobial Resistance in Developing Countries: Impact, Interventions and ImplicationsView all 5 articles
 Raphael Zozimus Sangeda1*
Raphael Zozimus Sangeda1* Mariki I. Urassa1
Mariki I. Urassa1 Deus Buma2
Deus Buma2 George Nyamanda Musiba2
George Nyamanda Musiba2 Faraja S. Chiwanga3
Faraja S. Chiwanga3 Mhina Chambuso4
Mhina Chambuso4 Pius Gerald Horumpende5,6,7
Pius Gerald Horumpende5,6,7Introduction: Antibacterial utilization studies can help identify areas of intervention of antimicrobial stewardship programs (ASP) to facilitate rational use and prevent the emergence of antimicrobial resistance (AMR). Assessment and comparison of antibacterial utilization depend on the Anatomical Therapeutic Chemical (ATC) classification system and Defined Daily Dose (DDD) recommended by the World Health Organization (WHO) collaborative center for international drug monitoring. This study aimed to determine the DDD of each prescribed antibacterial group and the proportions of wide-spectrum antibacterials used at Muhimbili National Hospital (MNH) in Tanzania to allow baseline data for hospital ASPs.
Methods: A retrospective analytical study using data collected from 1st January 2015 to 31st December 2015 was undertaken at MNH. Data on antibacterials prescribed and dispensed were obtained from the MNH database. The ATC/DDD system was used to classify and quantify the antibacterial utilization patterns.
Results: A total of 10,643.1 DDDs were used in thirteen ward units at the Kibasila, Mwaisela and Sewahaji blocks of the MNH. Eighteen different antibacterials were prescribed and dispensed to 1496 patients. Capsules were the most dispensed dosage form. The drug ciprofloxacin was the leading antibacterial prescribed, with a DDD of about 3780 (35.5%) per year. This was followed by metronidazole and amoxicillin. The proportion of wide-spectrum antibacterials was as high as 66%. Utilization peaks were noted in April, July and September. There was a significant monthly increase in antibacterials utilization between January and December 2015 (p-value = 0.002, R-square = 0.64). The trends forecasted increased through June 2016.
Conclusions: Utilization trends indicated a significant monthly increase in 2015 at MNH wards in Tanzania. The use of wide-spectrum antibacterials was widespread. This calls for continued antibacterial utilization surveillance and implementation of hospital-based ASP to mitigate the rapidly rising global threat of AMR.
Antimicrobial use (AMU) has been documented to be an important contributing factor for the development of antimicrobial resistance (AMR) (1–3). Excessive and inappropriate antimicrobial use relentlessly accelerates AMR (4). The World Health Organization (WHO) has recently declared AMR a global crisis (5, 6). In the modern era of medicine, the threat of AMR affects both low – and middle-income countries (LMICs) and high-income countries (HIC) (4). However, the burden of AMR is more of a concern in LMICs due to less stringent regulatory mechanisms over rational use of medicines (4, 7–9). Prescription and dispensing practices influence rational antibacterial use in hospitals and community settings (7, 10) (11). Inappropriate use of antibacterial may be appreciated in the form of inadequate dosage, use for viral infections, over-use of parenteral form in preference over oral dosage forms. It can also be practiced when prescriptions do not follow the available clinical guidelines. In addition, other forms of inappropriate antibacterial use include self-medication with antibacterials, pharmacists dispensing antibacterials without prescriptions, and non-adherence to prescribed regimens (8–10).
Risks associated with overuse of antibacterials include AMR, more severe disease, complication, increased duration of illness, increased healthcare cost, mortality and morbidity and recurrence of infection (3). Therefore, inappropriate use and overuse of antibacterials have medical, social, and economic ramifications (10, 12). Antimicrobial stewardship programs (ASP) serve as part of multifaceted interventions to reduce the over-use of antibacterials and counteract AMR (3, 13). Implementing ASP can exemplify the tendency of overdependence on newer expensive antibacterials for mild infections (3, 10) and the unnecessary use of reserved antibacterials. However, ASP and data to support it are scarce in LMICs (14, 15).
The Anatomical Therapeutic Chemical (ATC) classification system and Defined Daily Dose (DDD) are the internationally accepted classification methods approved by the WHO collaborative center for international drug monitoring in Europe. The classification system allows assessing and comparing medicines utilization at a national or facility level. DDD is a unit based on average daily use for primary consumption of a specific medication. DDD is a standardized methodology and allows the best comparison of antibacterial usage between different countries, regions and even health facilities (16, 17).
AMR and increased antibacterial procurement costs are significant challenges facing Tanzanian health facilities (18). Therefore, it is crucial to establish an effective dispensing and prescribing practice to reduce cost and the threat of AMR for the available antibacterials. Here we report the trends of utilization of antibacterials using the ATC/DDD system for each prescribed group of antibacterials and by spectrum antibacterials used in 2015 at the Muhimbili National Hospital (MNH) in Tanzania.
The research was conducted at Kibasila, Sewahaji and Mwaisela wards of the MNH, the Tanzanian National referral and a University teaching hospital. MNH is a National Referral Hospital, Research Center and a University Teaching Hospital with a 1,500-bed capacity and attending 2,000 outpatients per day (19), serving patients from all regions of Tanzania’s mainland and Zanzibar and Mafia Islands. It has a well-equipped clinical laboratory for patient care. Most patients are referrals from regional hospitals in Dar es Salaam, while others come directly for care in the emergency department.
There are six main inpatient blocks Kibasila, Sewahaji, Mwaisela, Maternity, Psychiatry ward, pediatric ward and emergence medicine.
A retrospective analytical cross-sectional study was performed on antibacterials dispensed between 1st January to 31st December 2015.
Data on antibacterials prescribed and dispensed were obtained from the MNH electronic prescription database. The information collected comprised of names of drug, strength, dosage form and route of administration, quantity dispensed and the package container used. Data were cleaned, re-grouped and analyzed using Microsoft Excel® software. The ATC/DDD system designed by the WHO collaborative center for international drug monitoring in Europe (16, 17) was used to re-classify the antibacterials and determine antibacterials use patterns.
The data were analyzed using Microsoft Excel 2013 software (Microsoft Corporation, Redmond, Washington, USA). Tables and charts are used to show the trends. We used Microsoft Excel 2013 to retrieve and store the combined utilization records. Products’ strength, pack size and the quantity of the antibacterial was converted into milligrams and grams. Generic names were retrieved from the dispensing data and the corresponding ATC codes were assigned to match the classes, DDD and antibacterial spectrum classification. The milligram and DDD of an antibacterial were calculated and aggregated for each generic name and class. Tables and graphs were plotted to reveal the utilization trends. Monthly utilization data were entered into the Statistical Package for the Social Sciences (SPSS) version 20 (IBM Corp., Armonk, NY, USA) for analysis. Time series and regression analyses were performed to detect seasonality in the data and verify the trend of antibacterials use. We used an autoregressive integrated moving average (ARIMA) model to predict the trends of antibacterial use. Statistical significance was attributed to a p-value of less than 0.05.
Ethical clearance was obtained from the Directorate of Research and Publications at Muhimbili University of Health and Allied Sciences (MUHAS) with numbers 2016-03-17/AEC/Vol. X/191. Permission to conduct the study was obtained from the MNH Training Research and Consultancy Unit.
A total of 17038 prescriptions were analyzed in 2015, of which 2542 (15%) constituted an antibacterial item. These were from the Kibasila, Mwaisela and Sewahaji blocks of the hospital. Thirteen wards were surveyed to estimate the total DDDs of antibacterial utilization (Supplementary Table 1). Eighteen different antibacterials were used in the study period (Table 1), totaling 10,643.1 DDDs. These were prescribed and dispensed to 1496 unique patients. We excluded 174 prescriptions, for which, although indicated to be prescribed, no amount of dispensed antibacterials units was indicated.
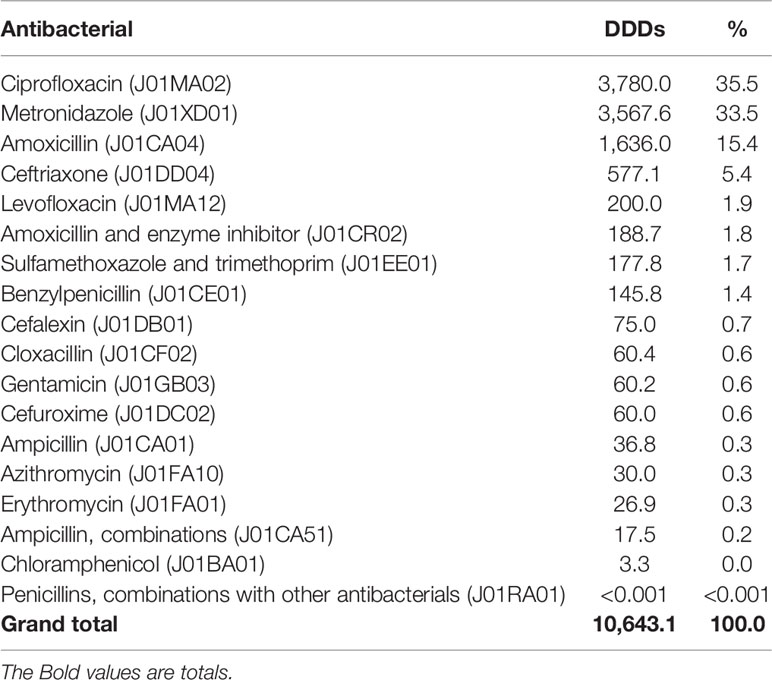
Table 1 Individual antibacterial utilization and proportion at Muhimbili National Hospital, Tanzania, for 12 months in 2015.
Capsules comprised 53.8% of all DDDs utilized in the study period, followed by injectables, tablets and syrup dosage forms (Table 2).
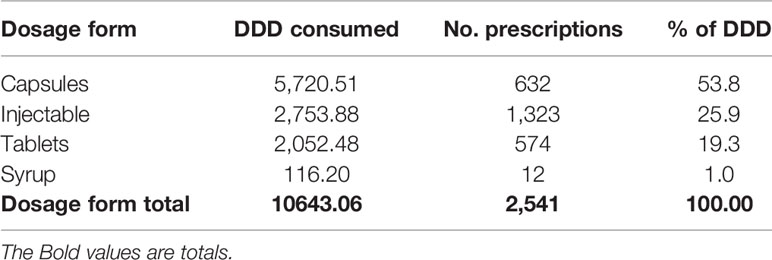
Table 2 Consumption of antibacterials per dosage form at Muhimbili National Hospital, Tanzania in the year 2015.
According to the spectrum of antibacterials consumed, the majority (66%) of all utilized antibacterials were broad-spectrum (Figure 1).
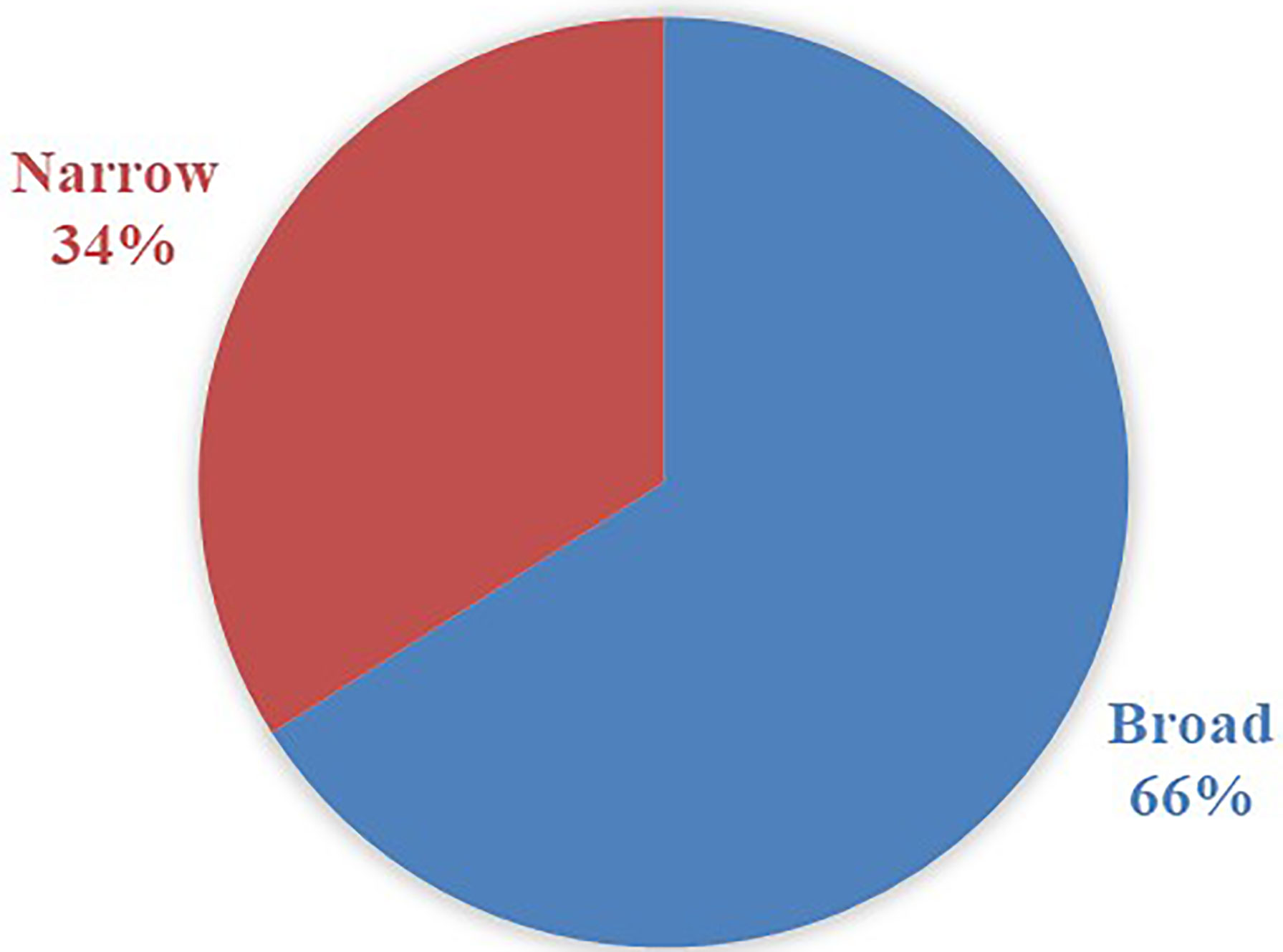
Figure 1 Contribution of antibacterials’ spectrum of activity in the volume of antibacterials per dosage form at Muhimbili National Hospital, Tanzania, in 2015.
These antibacterials were mainly used in the Mwaisela ward block, which serves two intensive care units (ICU) and internal medicine wards, including the infectious diseases unit (Table 2 and Supplementary Table 2. The highest proportion (83.8%) of these medicines was used in the two ICUs (Table 2).
At the level 3 class of ATC classification, quinolones were the most utilized antibacterials (Figure 2 and Supplementary Table 3), followed by other antibacterials and beta-lactam antibacterials.
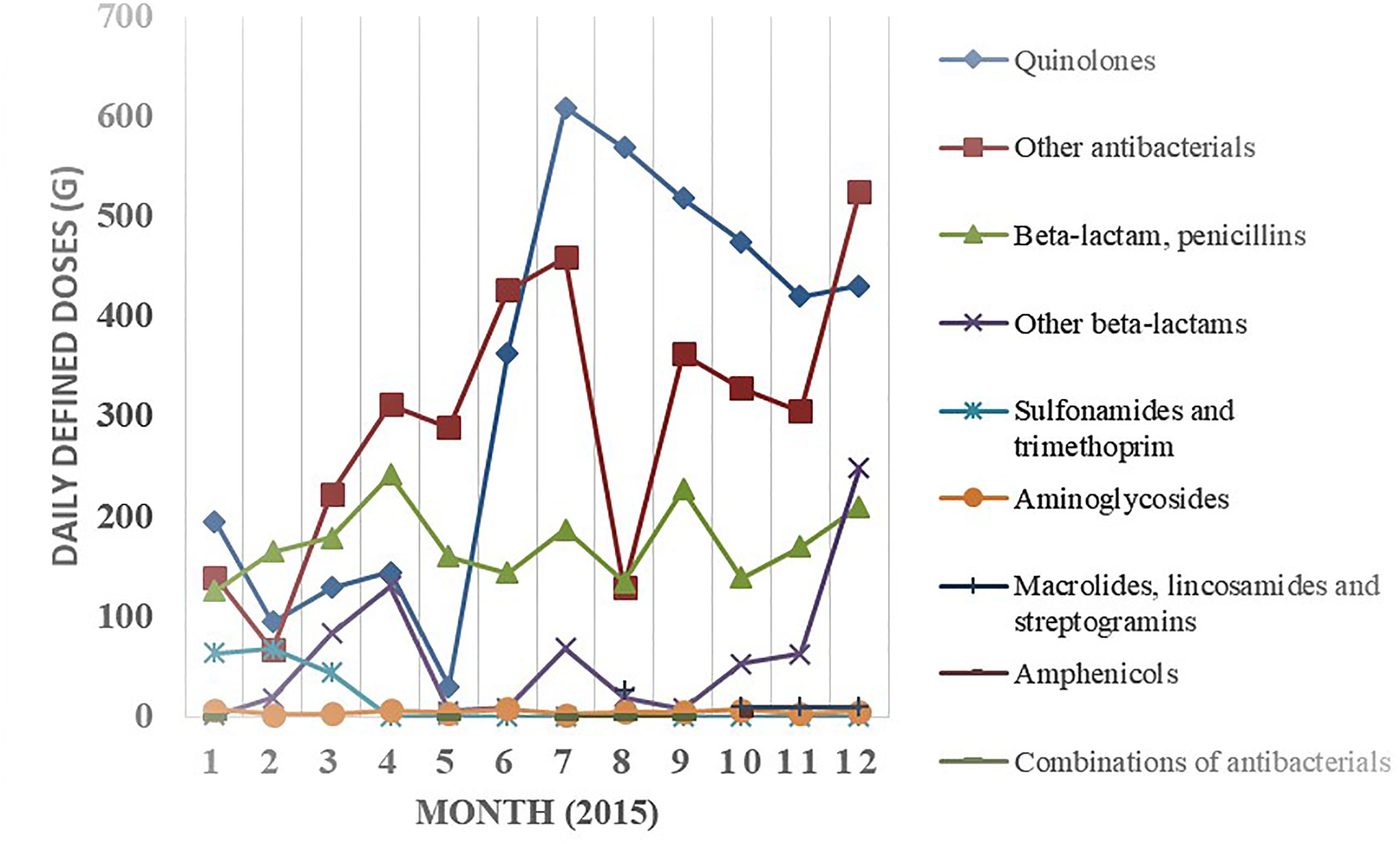
Figure 2 Monthly consumption variations per ATC level 3 classification of antibacterials at Muhimbili National Hospital, Tanzania, 2015. Monthly trends for these classes are shown in Supplementary Table 3.
There was generally an increasing trend over the months per class of antibacterial at ATC levels 3 (Figure 2). There are peaks of utilized amounts in April, July and September of the study period. These increases are notable for individual antibacterials, including the top three antibacterials: ciprofloxacin, metronidazole, and amoxicillin (Figure 3).
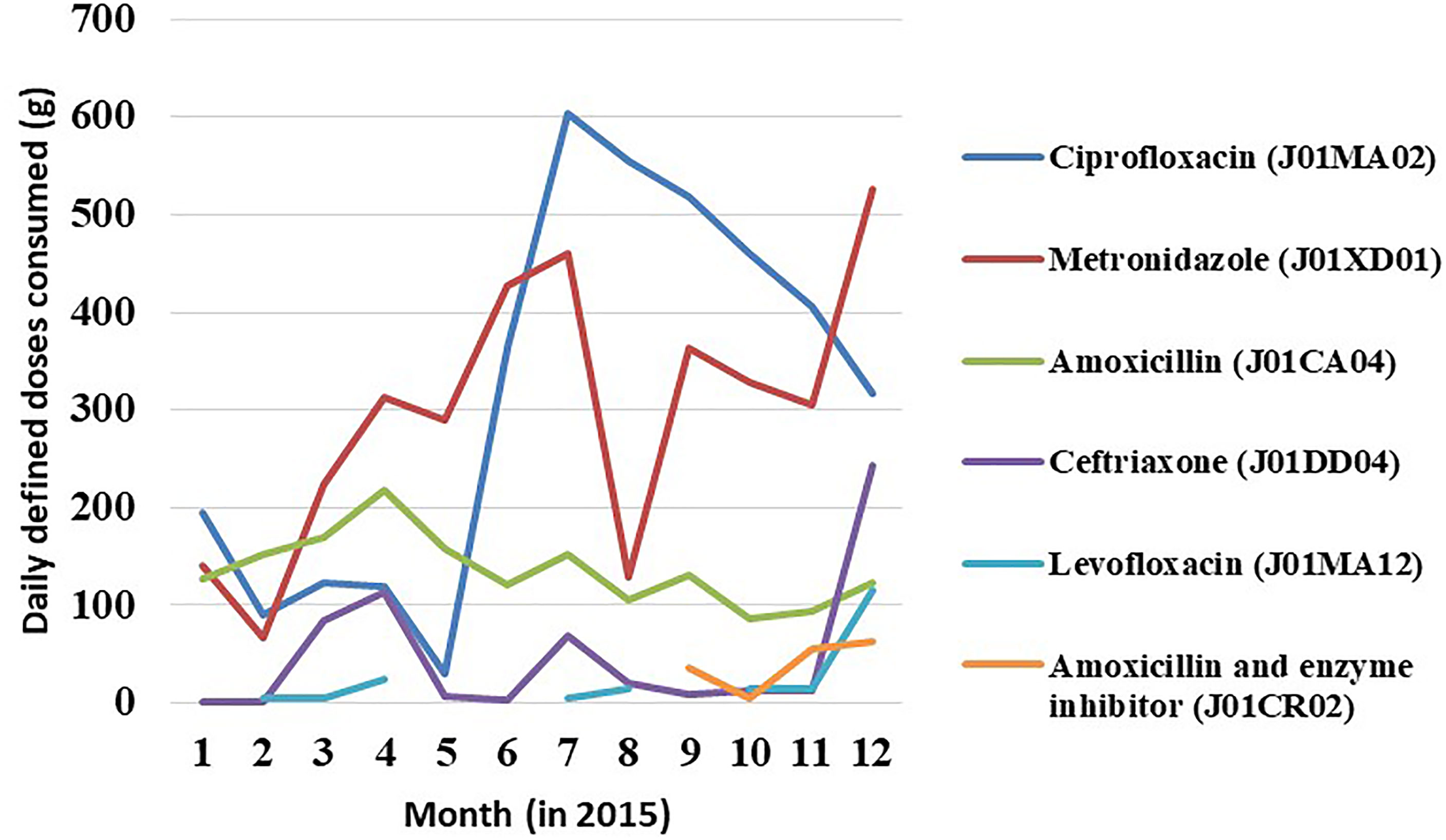
Figure 3 Top 5 antibacterials over 12 months in 2015. Other 13 antibacterials are indicated in Supplementary Table 1.
The monthly trends in the wards show similar peaks in April, July and September of the study period (Table 3).
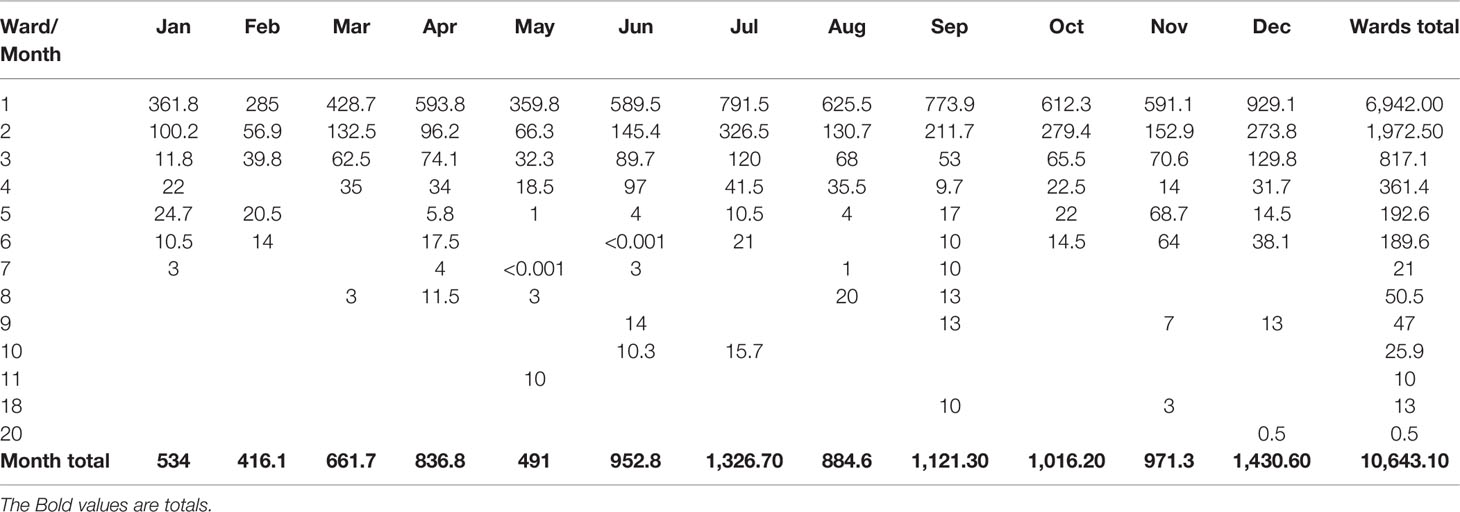
Table 3 Monthly consumption of antibacterials per ward at Muhimbili National Hospital, Tanzania, 2015.
Linear regression curve estimate indicated a significant increase of antibacterials over the 12 months (p-value = 0.002 and R-square 0f 0.64 (Figure 4).
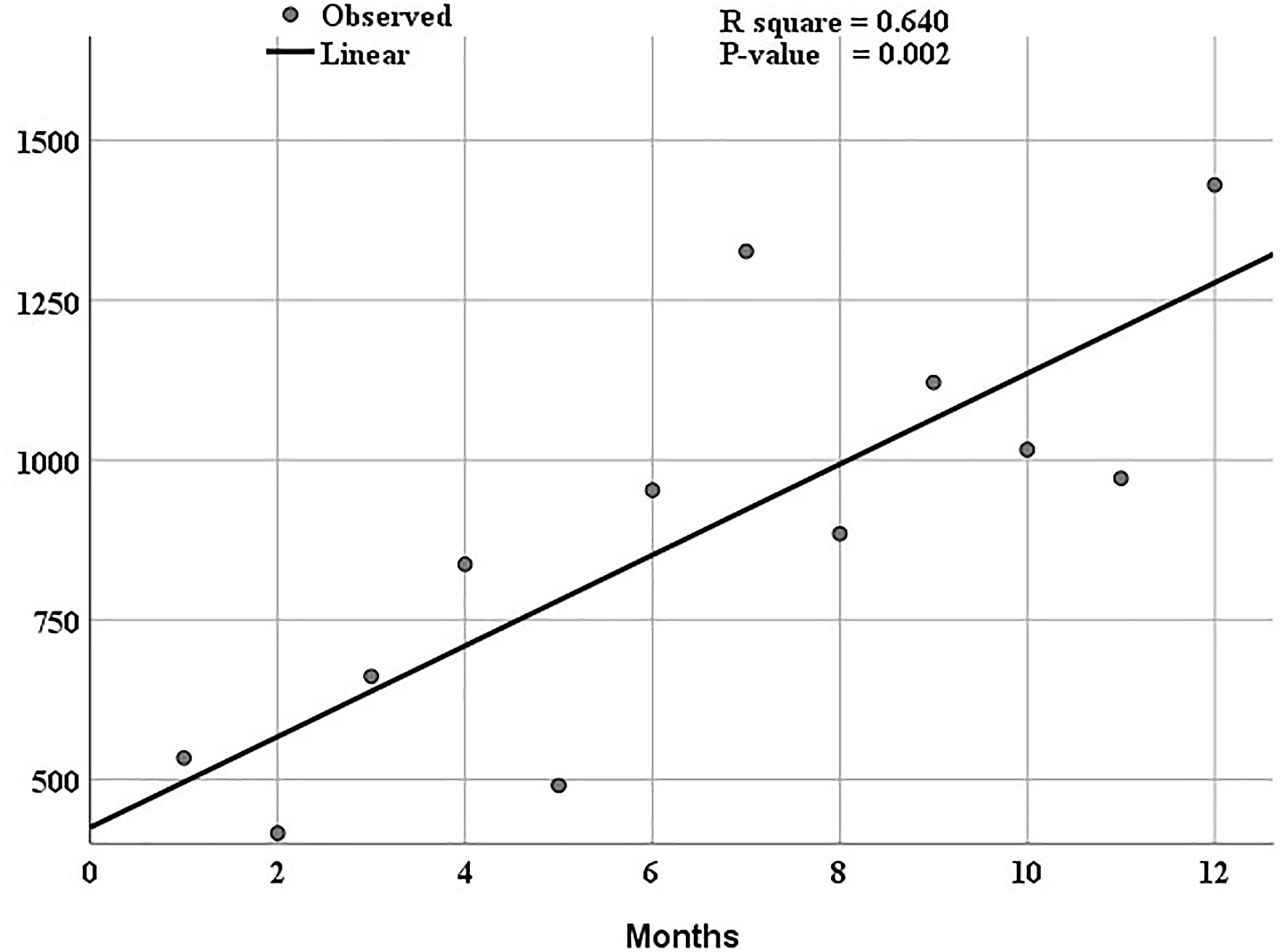
Figure 4 The linear curve estimation of the overall utilization of antibacterials shows an increasing trend over twelve months from January 2015 to December 2015.
The ARIMA model in time series analysis indicated an increasing trend six months after the end of the study period to June 2016 (Figure 5). The series decomposition data did not show seasonality, but three utilization peaks are noted in the utilization patterns. The predicted total antibacterials in 2016 are shown in Supplementary Table 4.
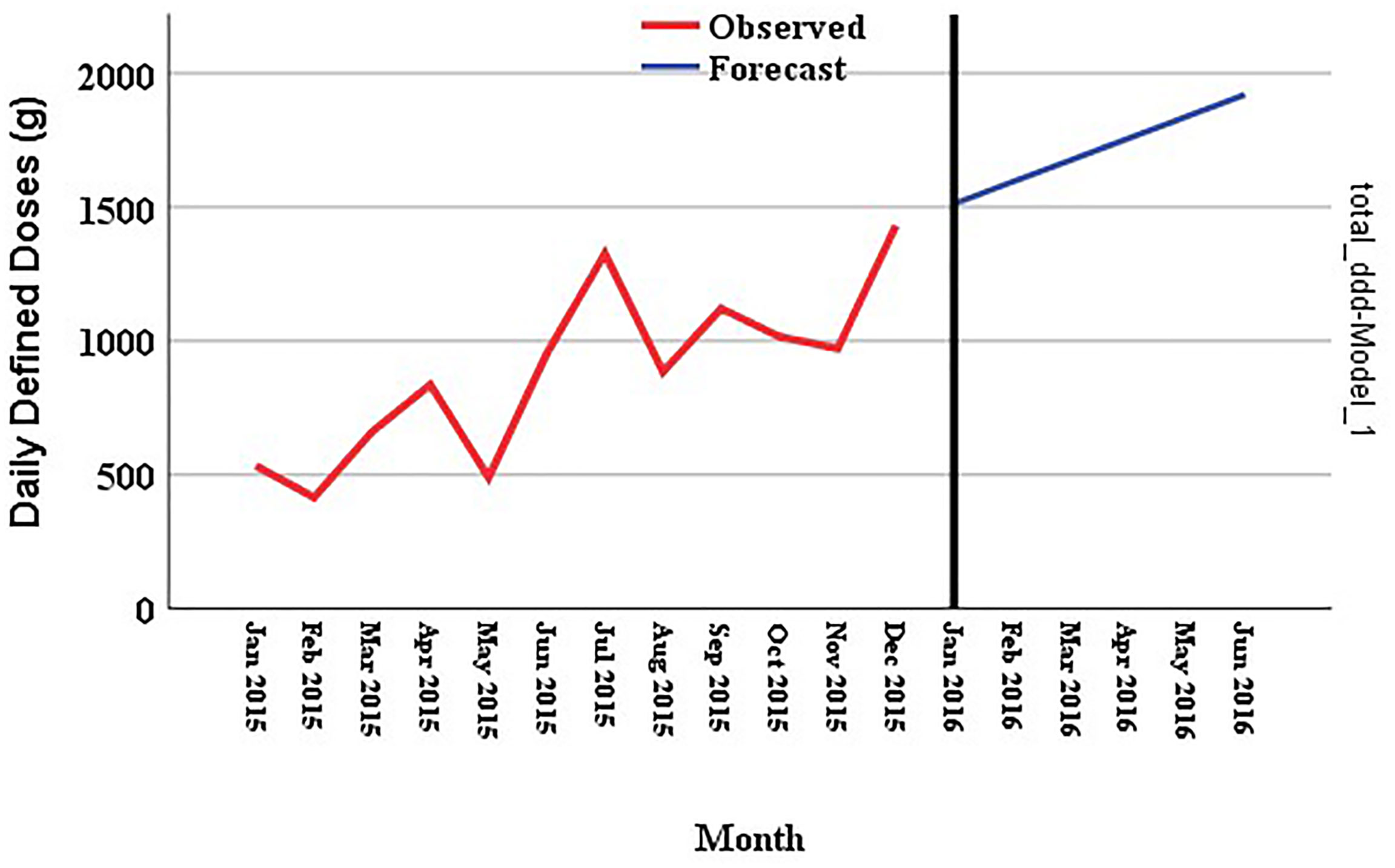
Figure 5 Trends of total utilized antibacterials over twelve months from January 2015 to December 2015. The autoregressive integrated moving average (ARIMA, 0, 1, 0) model forecasted the utilization to June 2016.
Utilization studies are an integral part of ASP and can help mitigate the emergence of AMR at hospital and country levels. These surveillances play a crucial role in guiding ASP to rational and optimal use of antimicrobials [19]. Countries that utilize more antibacterials have shown higher rates of AMR [20]. Countrywide surveillance of antibacterials use has shown an increasing trend in Tanzania and globally [21–23]. Using the WHO ATC/DDD approach, this study investigated one-year antibacterial utilization and seasonality trends at MNH in Tanzania using the WHO ATC/DDD approach.
This study provides preliminary data for implementing ASP at the hospital level. Eighteen unique antibacterials were used in 2015. The amount of antibacterials used reached 10,643.1 DDDs in 2015.
The Tanzania Standard Treatment Guidelines (STG) recommends the minimal use of broad-spectrum antibacterials. However, there was a high rate (66%) of the utilization of broad-spectrum antibacterials in this study. This may be due to antibacterials being frequently prescribed empirically without microbiological testing (15) in Tanzania. The prescribing and dispensing tendency at the hospital is more empirical because of the lack of appropriate technology such as culture sensitivity testing (15). Therefore, prescribers tend to provide empiric treatment, which may be inappropriate on some occasions.
The overuse of broad-spectrum antibacterials will eventually lead to a lack of alternative antibacterials choices, causing trivial bacterial infections to persist. This situation will cause mortality to even trivial infections (15). Study shows a rate of broad-spectrum antibacterial use in Tanzanian hospitals and prolonged surgical antibacterial prophylaxis being a common practice (13, 15, 20). The use of broad-spectrum antibacterials has also been noted in Ethiopia and Sudan (21, 22).
Concerning dosage forms, capsules comprised the majority (53.8%) of all DDDs antibacterials while injectables were at the rate of 25.6% and tablets and syrup at 20.6% of DDDs. This lower rate of injectables is an encouraging finding. Higher rates of injectables (60-85%) have been noted in Ethiopia (21). Similar rates of injectable antibacterials (26.5%) were observed in Ethiopia (23).
High amounts of antibacterials were dispensed in April and September during the study period. Uneven supply of antibacterials in the wards may be due to disease distribution in the community, financial constraints or inappropriate estimation and quantification of antibacterial needs by the hospital. The antibacterial utilization peaks in April and September may also correspond to peaks of the rainy season in Tanzania. Increased rates of infectious diseases have been reported elsewhere (24). The highest percentage of antibacterials was in the ICUs. The hospital caters to all ICU medications instead of the other medical wards where patients’ caretakers may obtain the antibacterial supplies from pharmacies outside the hospital. In addition, the varying high utilization peaks observed in April and September may coincide with the months in which there was bulk supply from the Medical Stores Department, the central medical warehouse of the country. The lower utilization periods coincide with moments where patients seek alternative supplies of antibacterials such as private pharmacies to meet their needs. Since the data was only for 2015, the seasonal decomposition algorithms did not detect any seasonality in the use of antibacterials in the study period.
This study showed high rates of use of ciprofloxacin (35.5%), metronidazole (33.5%) and amoxicillin (15.4%). These antibacterials are among those widely used in national surveillance in Tanzania (25, 26). Overuse of these antibacterials could lead to the emergence of the AMR epidemic against them (27–29) since these are used empirically without evidence of culture and sensitivity (14, 15). Fluoroquinolones are highly potent with antibacterial activity against gram-positive and negative organisms, including pseudomonal and staphylococcal species (30). Because of the potential risk of AMR development to fluoroquinolones, these groups should be used sparingly and according to the STGs (30). Countries like Norway have managed to reduce the utilization of fluoroquinolones in recent years (30).
For oral medications, ciprofloxacin and amoxicillin were the most used for the study period. For injectable medications, metronidazole and ceftriaxone were the most utilized medicines. The choice of medicines over the other for the conditions where two or more options can be used depends on both availability and sometimes selection preferences of prescribers.
Our study indicated high use of quinolones, azoles, and penicillins, contrary to a hospital-based study in Finland from 2003 to 2013, which revealed an increase in penicillins, cephalosporins and carbapenems (31). Frequent use of cephalosporins was observed in Ethiopia (21). High use of metronidazole was also noted in a study in Karthoum (22) and Lusaka Zambia (32) and Pakistan (33).
In our study, cephalosporins were the third most utilized group considering ATC level 3 as opposed to the study in Zambia (32) and Pakistan (33), where there was high use of cephalosporin prompting ASP measures in that settings.
The third most used antibacterial in our study was amoxicillin. In a countrywide study, amoxicillin was the top antibacterial in the study undertaken over seven years (24). This high trend has also been noted in Pakistan (33. The countrywide use in the latter study may have been due to the allowance of amoxicillin sales in specialized accredited drug dispensing outlets (ADDO).
The increased trends in consumption may imply the need for rational use of antibacterials in Tanzania. Other studies evaluating rational use using WHO rational indicators show overutilization in other sub-Saharan countries like Ethiopia (34, 35).
It was found that the trend of antibacterials utilization was increasing over the months at the MNH wards studied. Moreover, the broad spectrum antibacterials such as the third generation, amphenicols and aminoglycosides were high. This presents a high public health concern because it may lead to high antibacterial resistance during treatment. With the limited resources prevailing in sub-Saharan countries such as Tanzania, this is an excellent threat to treatment and should be taken seriously by prescribers. Drugs that are more susceptible to resistance should only be used in a unique situation when there is no option. Also, it was observed that capsules were a convenient dosage form for most patients admitted in the ward.
There was a significantly increasing trend of overall utilization in the study period. Our data can be verified by an ARIMA model, which we try to forecast the next six months’ utilization beyond the end of our study period. The model shows that if the same patterns continued in 2016, then the model predicts a further increase in the utilization of these antibacterials to the year 2016. This prediction model can devise ASP interventions based on the data to inform the future utilization and devise appropriate ASP measures to control the utilization. This study only serves as a benchmark for future intervention using the hospital data.
The series decomposition could not detect seasonality because we modeled our data with only 12 months, which is insufficient for detecting monthly seasonality. Nevertheless, we noted peaks of high utilization, which correspond to the peaks in the supply chain by the central Government warehouse. These troughs below the peaks depict moments where patients need to source medicine supplies outside the hospital pharmacy. Further studies are required to complement our analysis by using both testing data to build the ARIMA model and validation data to evaluate the accuracy of the forecasted trends.
Our results have implications concerning the impact of overuse of antibacterials on AMR occurrence since the increased use of antibacterials has been linked to overuse (4). The second implication is that the forecast trends can be used to highlight the interventions in the future by the ASP team. The ASP team can easily use the forecasted trends to formulate mitigations to prevent overuse and an AMR. Furthermore, our study can inform the hospital ASP team to reduce high dependence on broad-spectrum antibacterials for minor infections and save these for complicated infections.
The limitations of this study were that the DDD methodology does not give any information on the possible antibacterial combinations, which may be necessary for the context of possible misuse and overuse of antibacterials. Thus, the data presented here cannot judge antibacterial therapy’s appropriateness, but only the quantities utilized antibacterials. Despite these limitations, this approach allows a general overview of utilization in a hospital setting, estimating the risk of AMR emergence and setting ASP intervention targets. The trend of utilization over time can help identify inconsistencies, improve awareness of drug use and serve as a basis for more in-depth or ASP intervention studies.
Antibacterial utilization trends showed significant monthly increases in 2015 at MNH wards in Tanzania. The use of wide-spectrum antibacterials dominated the majority of prescriptions. The hospital should review if the use of ciprofloxacin can be regulated to avoid a situation of AMR against this potent antibacterial. This calls for continued surveillance and implementation of hospital-based antimicrobial stewardship programs to correlate antibacterial utilization patterns with AMR levels and conserve the utility of antibacterials.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Muhimbili University of Health and Allied Sciences (MUHAS), Research Ethics Committee. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fitd.2021.768842/full#supplementary-material
1. Ebrahim M, Gravel D, Thabet C, Abdesselam K, Paramalingam S, Hyson C. Antimicrobial Use and Antimicrobial Resistance Trends in Canada: 2014. Canada Commun Dis Rep (2016) 42:227–31. doi: 10.14745/ccdr.v42i11a02
2. Bennani H, Mateus A, Mays N, Eastmure E, Stärk KDC, Häsler B. Overview of Evidence of Antimicrobial Use and Antimicrobial Resistance in the Food Chain. Antibiotics (2020) 9:49. doi: 10.3390/antibiotics9020049
3. Llor C, Bjerrum L. Antimicrobial Resistance: Risk Associated With Antibiotic Overuse and Initiatives to Reduce the Problem. Ther Adv Drug Saf (2014) 5:229–41. doi: 10.1177/2042098614554919
4. Sartelli M C, Hardcastle T, Catena F, Chichom-Mefire A, Coccolini F, Dhingra S, et al. Antibiotic Use in Low and Middle-Income Countries and the Challenges of Antimicrobial Resistance in Surgery. Antibiotics (2020) 9:497. doi: 10.3390/antibiotics9080497
5. Aslam B, Wang W, Arshad MI, Khurshid M, Muzammil S, Rasool MH, et al. Antibiotic Resistance: A Rundown of a Global Crisis. Infect Drug Resist (2018) 11:1645–58. doi: 10.2147/IDR.S173867
6. Capozzi C, Maurici M, Panà A. Antimicrobial Resistance: It Is a Global Crisis, “A Slow Tsunami”. Ig Sanita Pubbl (2019) 75:429–50.
7. Ayukekbong JA, Ntemgwa M, Atabe AN. The Threat of Antimicrobial Resistance in Developing Countries: Causes and Control Strategies. Antimicrob Resist Infect Control (2017) 6:47. doi: 10.1186/s13756-017-0208-x
8. Poyongo BP, Sangeda RZ. Pharmacists’ Knowledge, Attitude and Practice Regarding the Dispensing of Antibiotics Without Prescription in Tanzania: An Explorative Cross-Sectional Study. Pharmacy (2020) 8:238. doi: 10.3390/pharmacy8040238
9. Ndaki PM, Mushi MF, Mwanga JR, Konje ET, Ntinginya NE, Mmbaga BT, et al. Dispensing Antibiotics Without Prescription at Community Pharmacies and Accredited Drug Dispensing Outlets in Tanzania: A Cross-Sectional Study. Antibiotics (2021) 10:1025. doi: 10.3390/antibiotics10081025
10. Dutta A, Chakraborty S. Practice of Rational Drug Uses in a Rural Area of 24 Pgs(s) in West Bengal. J Adv Pharm Technol Res (2010) 1:358. doi: 10.4103/0110-5558.72421
11. Horumpende PG, Sonda TB, van Zwetselaar M, Antony ML, Tenu FF, Mwanziva CE, et al. Prescription and Non-Prescription Antibiotic Dispensing Practices in Part I and Part II Pharmacies in Moshi Municipality, Kilimanjaro Region in Tanzania: A Simulated Clients Approach. PloS One (2018) 13:e0207465. doi: 10.1371/journal.pone.0207465
12. George SS, Varghese SR, Samuel CJ. Evaluation of Antibiotic Prescribing Patterns Among Medical Practitioners in North India (2013). ijbamr.com. Available at: http://ijbamr.com/word_file/Abstract 19.docx (Accessed March 18, 2016).
13. Sonda TB, Horumpende PG, Kumburu HH, van Zwetselaar M, Mshana SE, Alifrangis M, et al. Ceftriaxone Use in a Tertiary Care Hospital in Kilimanjaro, Tanzania: A Need for A Hospital Antibiotic Stewardship Programme. PloS One (2019) 14:e0220261. doi: 10.1371/journal.pone.0220261
14. Sangeda RZ, Kibona J, Munishi C, Arabi F, Manyanga VP, Mwambete KD, et al. Assessment of Implementation of Antimicrobial Resistance Surveillance and Antimicrobial Stewardship Programs in Tanzanian Health Facilities a Year After Launch of the National Action Plan. Front Public Heal (2020) 8:454. doi: 10.3389/fpubh.2020.00454
15. Horumpende PG, Mshana SE, Mouw EF, Mmbaga BT, Chilongola JO, de Mast Q. Point Prevalence Survey of Antimicrobial Use in Three Hospitals in North-Eastern Tanzania. Antimicrob Resist Infect Control (2020) 9:149. doi: 10.1186/s13756-020-00809-3
16. Bada MZ. Antimicrobial Utilizing Pattern in a Governmental Hospital in Palestine Measured Using WHO ATC / DDD Methodology. Nablus: An Najah National University, Palestine. (2014).
17. World Health Organization. Introduction to Drug Utilization Research. (2003). Available at: https://www.who.int/publications/i/item/8280820396 [Accessed July 12, 2021].
18. World Health Organization. Guidelines for ATC Classification and DDD Assignment (2021). Available at: https://www.whocc.no/filearchive/publications/2021_guidelines_web.pdf (Accessed January 16, 2021).
19. Hospital Muhimbili National. Muhimbili National Hospital (MNH) (2021). Available at: http://www.mnh.or.tz (Accessed August 14, 2021).
20. Nyongole O, Akoko L, Mwanga A, Mchembe M, Kamala B, Mbembati N. Antibiotic Use in Urological Surgeries: A Six Years Review at Muhimbili National Hospital, Dar Es Salaam-Tanzania. Pan Afr Med J (2015) 22:226. doi: 10.11604/pamj.2015.22.226.6253
21. Demoz GT, Kasahun GG, Hagazy K, Woldu G, Wahdey S, Tadesse DB, et al. Prescribing Pattern of Antibiotics Using WHO Prescribing Indicators Among Inpatients in Ethiopia: A Need for Antibiotic Stewardship Program. Infect Drug Resist (2020) 13:2783–94. doi: 10.2147/IDR.S262104
22. Abdalla SN, Yousef BA. Prescribing Patterns of Antimicrobials in the Internal Medicine Department of Ibrahim Malik Teaching Hospital in Khartoum, 2016. Pan Afr Med J (2019) 34. doi: 10.11604/pamj.2019.34.89.17023
23. Gashaw T, Sisay M, Mengistu G, Amare F. Investigation of Prescribing Behavior at Outpatient Settings of Governmental Hospitals in Eastern Ethiopia: An Overall Evaluation Beyond World Health Organization Core Prescribing Indicators. J Pharm Policy Pract (2018) 11:26. doi: 10.1186/s40545-018-0152-z
24. Chowdhury FR, Ibrahim QSU, Bari MS, Alam MMJ, Dunachie SJ, Rodriguez-Morales AJ, et al. The Association Between Temperature, Rainfall and Humidity With Common Climate-Sensitive Infectious Diseases in Bangladesh. PloS One (2018) 13:e0199579. doi: 10.1371/journal.pone.0199579
25. Sangeda RZ, Saburi HA, Masatu FC, Aiko BG, Mboya EA, Mkumbwa S, et al. National Antibiotics Utilization Trends for Human Use in Tanzania From 2010 to 2016 Inferred From Tanzania Medicines and Medical Devices Authority Importation Data. Antibiotics (2021) 10:1249. doi: 10.3390/antibiotics10101249
26. Mbwasi R, Mapunjo S, Wittenauer R, Valimba R, Msovela K, Werth BJ, et al. National Consumption of Antimicrobials in Tanzania: 2017–2019. Front Pharmacol (2020) 11:585553. doi: 10.3389/fphar.2020.585553
27. Smith A. Metronidazole Resistance: A Hidden Epidemic? Br Dent J (2018) 224:403–4. doi: 10.1038/sj.bdj.2018.221
28. Fasugba O, Gardner A, Mitchell BG, Mnatzaganian G. Ciprofloxacin Resistance in Community- and Hospital-Acquired Escherichia Coli Urinary Tract Infections: A Systematic Review and Meta-Analysis of Observational Studies. BMC Infect Dis (2015) 15:545. doi: 10.1186/s12879-015-1282-4
29. Sangeda RZ, Baha A, Erick A, Mkumbwa S, Bitegeko A, Sillo HB, et al. Consumption Trends of Antibiotic for Veterinary Use in Tanzania: A Longitudinal Retrospective Survey From 2010-2017. Front Trop Dis (2021) 2:694082. doi: 10.3389/fitd.2021.694082
30. Andreassen V, Waagsbø B, Blix HS. Bruk Av Ciprofloksacin Ved Et Lokalsykehus. Tidsskr Den Nor legeforening (2020) 140. doi: 10.4045/tidsskr.20.0146
31. Laine N, Hoppu K, Airaksinen M, Saxen H. Antimicrobial Consumption in a Tertiary Children’s Hospital in Finland (2003–2013). Eur J Hosp Pharm (2016) 23:266–71. doi: 10.1136/ejhpharm-2015-000766
32. Masichid AM, Vega AD, Callahan P, Herbert A, Fwoloshi S, Zulu PM, et al. Antimicrobial Usage at a Large Teaching Hospital in Lusaka, Zambia. PloS One (2020) 15:e0228555. doi: 10.1371/journal.pone.0228555
33. Atif M, Azeem M, Saqib A, Scahill S. Investigation of Antimicrobial Use at a Tertiary Care Hospital in Southern Punjab, Pakistan Using WHO Methodology. Antimicrob Resist Infect Control (2017) 6:41. doi: 10.1186/s13756-017-0199-7
34. Sisay M, Mengistu G, Molla B, Amare F, Gabriel T. Evaluation of Rational Drug Use Based on World Health Organization Core Drug Use Indicators in Selected Public Hospitals of Eastern Ethiopia: A Cross Sectional Study. BMC Health Serv Res (2017) 17:161. doi: 10.1186/s12913-017-2097-3
Keywords: seasonality, AMR, ASP, Tanzania, defined daily dose, anatomical therapeutic and chemical classification, antibiotics, antibacterials utilization
Citation: Sangeda RZ, Urassa MI, Buma D, Musiba GN, Chiwanga FS, Chambuso M and Horumpende PG (2022) Seasonality and Annual Utilization Patterns of Antibacterials at Muhimbili National Hospital, Dar es Salaam, Tanzania: A 2015 Monthly Survey. Front. Trop. Dis 2:768842. doi: 10.3389/fitd.2021.768842
Received: 01 September 2021; Accepted: 20 December 2021;
Published: 18 January 2022.
Edited by:
Eric Sampane-Donkor, University of Ghana, GhanaReviewed by:
Gerald Mboowa, Makerere University, UgandaCopyright © 2022 Sangeda, Urassa, Buma, Musiba, Chiwanga, Chambuso and Horumpende. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Raphael Zozimus Sangeda, c2FuZ2VkYUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.