
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Trop. Dis. , 21 July 2021
Sec. Tropical Disease Epidemiology and Ecology
Volume 2 - 2021 | https://doi.org/10.3389/fitd.2021.655690
This article is part of the Research Topic Highlights in Disease Ecology, Prevention and Control View all 4 articles
 Tesema Abera Yada1
Tesema Abera Yada1 Yadeta Dessie1
Yadeta Dessie1 Rasha Darghawth2
Rasha Darghawth2 Tara Wilfong1
Tara Wilfong1 Mohammed Abdurke Kure3*
Mohammed Abdurke Kure3* Kedir Teji Roba3
Kedir Teji Roba3Background: Anemia and malnutrition remain a public health challenge in developing worlds. Anemia during a nonpregnant state is one of the neglected medical conditions affecting reproductive-age women around the world. Globally, it is estimated that one-third of all reproductive-age women are anemic. Although it has negative consequences and extensive burden, anemia in nonreproductive-age women is rarely studied in Africa. In Ethiopia, studies investigating anemia and malnutrition among nonpregnant reproductive-age women are limited. Therefore, this study was aimed to assess intestinal parasitic infection, malnutrition, and predictors of anemia among nonpregnant reproductive-age women in Olenchity General Hospital, central Ethiopia.
Methods: A facility-based cross-sectional study design was employed among 405 nonpregnant reproductive-age women in Olenchity General Hospital, central Ethiopia from February 14 to March 24, 2018. Data were collected using a pretested interviewer-administered questionnaire. Blood samples were collected and tested to determine hemoglobin levels by using a hematology analyzer machine. Collected data were entered into EpiData version 3.02 and exported to SPSS version 20 (IBM SPSS Statistics, 2012) for further analysis. Multivariable logistic regression analysis was done to identify factors independently associated with anemia after controlling for possible confounders. Statistical significance was declared at p-value <0.05.
Result: Overall, the magnitude of anemia was found to be 47.4% [95% CI (42.7, 52.6)], of which 34.8% were mild, 11.4% were moderate, and 1.2% were severely anemic. The prevalence of intestinal parasitic infection, wasting, and overweight was 34.6%, 26.2%, and 8.1%, respectively. Having no formal education [AOR=2.25, CI (1.02, 4.97)], using three to five sanitary pads per day during menses [AOR=1.66 CI (1.02, 2.68)], history of chewing khat [AOR= 4.45, CI (1.18, 16.83)], being from households with mild food insecurity [AOR=3.41, CI (1.10, 10.58)], and intestinal parasitic infection [AOR=2.28, CI (1.39, 3.47)] were factors independently associated with anemia.
Conclusion: The magnitude of anemia, malnutrition, and intestinal parasitic infection among nonpregnant reproductive-age women was found to be a considerable public health problem. Therefore, attention should be given to nonpregnant reproductive-age women visiting different healthcare services to reduce risks of anemia and malnutrition for possible future pregnancies and to ensure women’s health. Deworming of nonpregnant reproductive-age women is also very crucial to reduce the risks of anemia.
Anemia is a condition in which the number of red blood cells or the hemoglobin level falls lower than the normal value (hgb < 12 g/dl) (1). It is a serious public health challenge affecting both nonpregnant and pregnant reproductive-age women (2, 3). It has negative consequences on the health and wellbeing of women and increases the risk of adverse pregnancy outcomes (4, 5). Globally, nearly half of a billion reproductive-age women are affected by anemia. For instance, in 2011 alone, around 496 million nonpregnant reproductive-age women and 32.4 million pregnant women aged 15–49 years were anemic (6, 7). The highest magnitude of this problem is concentrated in South and Central Asia as well as in West Africa (8), of which 19.4 million women were suffering from severe anemia. Anemia is a serious global public health problem that particularly affects young children and pregnant women. For instance, secondary analysis of the World Health Organization (WHO) in Asian and African countries estimates that 42% of children less than 5 years of age (9) and 40% of pregnant women are anemic (10). It also recommends that combating malnutrition in all its forms is one of the greatest global health challenges (11). Females were consistently at a greater risk of anemia than men across almost all geographic regions and in most age groups (12).
Furthermore, anemia continues to be a widespread and significant global health problem that remains to be adequately addressed, particularly in low- and middle-income countries (LMICs) where progress has been slow and uneven (13). For instance, among United Nations (UN) regions, the prevalence of anemia ranges from 12.2% to 36.9%, with the highest report being from the African region while the lowest stemming from Northern America (8). Moreover, according to the WHO report in 2008 alone, around 500 million nonpregnant reproductive-age women and 56 million pregnant women suffered from anemia (14).
Furthermore, researchers have revealed that anemia and malnutrition during the preconception period are directly or indirectly affecting pregnancy and birth outcomes (15, 16). They are also associated with an increased risk of stillbirth, neonatal mortality, and morbidity (6, 17). This burden is often attributed to low dietary intake, blood loss, intestinal worm infestation during the reproductive age, and increased physiological needs during pregnancy (18, 19). Likewise, anemia impairs the health and wellbeing of women and increases the risk of maternal and neonatal adverse outcomes (8). For instance, iron deficiency anemia determines the cognitive development of children and also has consequences in adults due to the aggregate effect with other causes of nutritional deficiencies (13, 16). Moreover, research reports indicated that global economic losses due to iron deficiency related to physical productivity are around 2.32 USD per capita or 0.57% of GDP (20).
Worldwide, researchers have found that iron deficiency anemia is the most common cause of anemia during the reproductive-age years. However, other risk factors such as chronic disease, intestinal parasitic infection, malaria, and poor economic status also play an important role (21, 22). Similarly, anemia can be caused by poor absorption of iron, low dietary intake, and blood loss (23). Moreover, although anemia can occur at any time in life, there are critical times in which it can be more detrimental such as early childhood and during pregnancy. Iron deficiency anemia during pregnancy and even for a period after childbirth increases the risk of maternal death (2, 21). Anemia is also associated with an increased risk of preterm birth, low birth weight infants (24), and fetal mortality (13, 25). Overall, since anemia has a negative effect and extensive burden on a woman’s general health and remains a public health problem, a WHO policy brief recommended that further actions are required to reach the World Health Assembly target of a 50% reduction of anemia in women of reproductive age by 2025 (2).
In Ethiopia, according to the national demographic health report (Ethiopian Demographic and Health Survey, 2016), the magnitude of anemia in nonpregnant reproductive-age women was 24% (26), which is considered a moderate public health problem in the country. In addition, studies conducted among Ethiopian women indicated that one in every five women had iron deficiency anemia (27). Moreover, a similar report from the Ethiopia Demographic and Health Survey (EDHS, 2016) revealed that one in every three Ethiopian women suffers from anemia (26). Although early management before pregnancy is helpful to reduce risks of anemia during pregnancy and missed opportunities for nonpregnant women attending healthcare services, anemia in nonpregnant reproductive-age women is neglected in Ethiopia. Moreover, despite its negative consequences and extensive burden, anemia among nonpregnant women is rarely studied in Ethiopia. Therefore, this study aimed to examine the magnitude of intestinal parasitic infection, malnutrition, and predictors of anemia among nonpregnant reproductive-age women in Oromia Regional State, Ethiopia.
A facility-based cross-sectional study was conducted in Olenchity General Hospital from February 14 to March 24, 2018. Olenchity General Hospital is found in Olenchity town of Boset District, Oromia Regional State, Ethiopia. Boset District is located 123 km from the capital city of Addis Ababa. The District is located at an elevation of 1,436 m above sea level. Olenchity town has two small administrative divisions called kebeles. According to a 2007 Census report, Boset District has an estimated population of 115,598 with 60,587 males and 55,011 females. According to the Central Statistics Agency (CSA), in the 2017/2018 fiscal year, the hospital provides health services for approximately 292,239 population, and an estimated 54,245 nonpregnant reproductive-age women and 10,141 pregnant women are expected to get services from Olenchity General Hospital annually (28).
All nonpregnant reproductive-age women (women aged 15 to 49 years) who visited Olenchity General Hospital for healthcare services were considered as the source population. All nonpregnant reproductive-age women (NPRAW) who attended Olenchity General Hospital for healthcare services in different departments such as the Expanded Program of Immunization (EPI) unit, family planning (FP) unit, Outpatient Department (OPD), Inpatient Departments (IPD), and chronic follow-up clinics were considered for enrollment. Women who were not using family planning and unknown pregnancy status were tested for urine human chorionic gonadotropin (HCG) hormone to rule out the pregnancy. All women with the following preconditions (postpartum period of fewer than 2 weeks, breastfeeding and less than 6 months, nonpregnant and being treated for anemia, and critically ill during data collection period) were excluded from the study. The sample size for this study was calculated using the statistical software of Epi Info version 7.0 (USA, 2016) by considering the following assumptions. The proportion of anemia among nonpregnant reproductive women (p=18.1%) was taken from a previous study report in Pakistan (29); with 95% of confidence level, 4% tolerable margin of error, and a 15% non-response rate added, the final sample size for the study was 420.
A systematic sampling technique was used to collect information from eligible study participants. First, the Olenchity General Hospital was selected purposely because it is the only public hospital found in Boset District of Oromia Regional State. According to the previous information obtained from the 3-month (one-quarter) hospital registry, an estimated 13,561 NPRAW visited the Olenchity General Hospital for healthcare services in different departments and units. These departments and units include the EPI unit, OPD, IPD, FP unit, and chronic follow-up clinics. When this quarterly report was reduced to a monthly report, the total number of NPRAW was 4,520. Likewise, when we divided this number of women by five units/department (EPI, OPD, IPD, FP, and chronic follow-up clinics), the total population was 904 (4,520/5 = 904). Based on the above information, we used a systematic sampling technique to select the study participants. Charts of the clients at each unit were used as a sampling frame. Accordingly, we estimated the sampling interval (Kth value) by dividing the total population (N=904) by the calculated sample size (n=420); thus, K=904/420 =2. Then, the total sample size (n=420) was proportionally allocated to all respective service units of the hospital. Finally, every second eligible woman was interviewed and data were collected until the required sample size was obtained.
Data were collected using a semi-structured interviewer-administered questionnaire adapted from Ethiopian Demographic and Health Survey (26) data collection tools and other related literature. Dietary data questionnaires were adapted from Food and Nutrition Technical Assistance (FANTA), Food and Agriculture Organization (FAO), and World Food Program (WFP) (30–32). Most of the questionnaires were close-ended questions. However, the questions assessing causes and source of information about anemia were open-ended to capture detailed information. The questionnaire was designed to capture socio-demographic variables (age, residence, marital status, educational status, family income, occupation, types of latrine), menstrual history-related variables (age at first menses, amount flow, duration of flow, frequent utilization of sanitary pad), and dietary diversity-related variables (household food security status and anthropometric assessments). Before the data collection process, the questionnaires were coded and a skipping pattern was arranged. The questionnaire’s template was prepared using statistical software of EpiData version 3.1. Then, the entered data were exported to SPSS version 20 for analysis (IBM SPSS statistics, 2012).
The data were collected by four diploma nurses and two laboratory technicians. Similarly, one Bachelor of Science (BSc) nurse and one senior laboratory technologist were also assigned to each respective unit/department to monitor and supervise the data collection processes and data collectors.
The 5 ml of venous blood was drawn under an aseptic technique in disposable vacutainer tubes by an experienced laboratory technologist. Vacutainer tubes were labeled at the time of sample collection. The blood samples drawn from the study participants were centrifuged at 3,000 revolutions per minute (RPM) for at least 20 min at room temperature. The hemoglobin (hgb) level was done by the hematology analyzer machine (DIRUI BCC-3000B). Women with a hemoglobin concentration of <12.0 g/dl were labeled as anemic. Accordingly, we categorized the status of anemia based on hemoglobin results as: mild anemia (hgb level=10–11.9 g/dl), moderate anemia (hgb level= 7–10.9 g/dl), and severe anemia (hgb level< 7.0 g/dl) (33).
Sample collection of a cup with a lid and bamboo stick was provided to all study participants. During stool sample collection, each participant was instructed to avoid urine or dust contamination of sample stool. Microscopic analysis of stool samples was performed on all fresh stool samples obtained from each study participant. Samples were placed on clean glass slides, labeled for identification, covered with a coverslip, and examined microscopically using the direct wet mount technique. Then, it was observed using low-power (×10) and high-power (×40) objectives for the identification of protozoan trophozoites, cyst, helminths ova, and larvae (30–32).
Anthropometric measurements were documented using a digital weight scale, which has an attached height scale (Adult Scale ASTOR). The height of each participant was recorded to the nearest tenth of a centimeter, and the weight of the participants was recorded to the nearest tenth of the kilogram (kg). During measurements, any heavy clothes, hats, and shoes were removed. Accordingly, the body mass index (BMI) was categorized as: Underweight (BMI<18.5 kg/m2), Normal weight (18.5–24.9 kg/m2), Overweight (25.0–29.9 kg/m2), and Obese (BMI ≥30.0 kg/m2) (34). Similarly, the standard Mid Upper Arm Circumference (MUAC) tape of the United Nations Children’s Fund (UNICEF) was utilized. All MUAC measurements were recorded to the nearest tenth of a centimeter. MUAC measurement of <22 cm was considered as undernutrition, and MUAC measurement > 22 cm was considered as normal (30–32).
Dietary diversity was assessed based on the number of individual food groups consumed over 24 h. The Women’s Dietary Diversity Score (WDDS) was based on nine food groups. Accordingly, food groups of ≤3 were considered a low dietary diversity, 4 and 5 a medium dietary diversity, and ≥6 a high dietary diversity (FAO, 2011). The Food Consumption Score (FCS) was calculated by the frequency of consumption of different food groups by a household during the 7 days preceding the survey. FCS between 0 and 28 was considered poor, 28.5–42 borderline, and >42 acceptable (32, 35, 36).
In this study, the outcome variable of interest was anemia. This outcome variable was dichotomized as a binary outcome (Yes and No). If a woman’s hgb level < 12 g/dl, she was considered to be anemic, and if the hgb level was 12 g/dl and above, she was considered as non-anemic. In SPSS analysis, this binary outcome was recoded as “1 and 0”. Thus, “hgb level < 12g/dl was recoded as 1 and hgb level ≥12g/dl was recoded as 0”.
In this study, the independent variables were socioeconomic status (income, working status, household (HH) food insecurity), socio-demographic factors (age, educational status, residence), menstrual bleeding history, type of family planning utilization, number of pregnancies, number of children, birth interval, previous anemia diagnosis, supplementation of IFA (iron and folic acid) during pregnancy, presence of clinical anemia, BMI status, parasitic infections, chronic illness, access to food rich in iron, latrine accessibility, HHs energy sources, and access to information.
Household food security: is when all occupants of the house, at all times, have physical, social, and economic access to sufficient, safe, and nutritious food that meets their dietary needs and food preferences for an active and healthy life. Household food insecurity: is the inability of households to access enough food, always to lead an active and healthy life. Nine standardized questions were administered to assess household food insecurity (access). If the condition exists, questions to determine frequency were administered; categories included rarely (once or twice), sometimes (three to ten times), or often (more than ten times) during the past 4 weeks. Finally, the results were summarized into one variable based on a formula devised by FANTA, 2007, and are classified as a food secured or unsecured (includes all stages of food insecurity; mild, moderate, and severe) (32). Kebele: is the smallest administrative unit localized for a group of people or cluster contained in the District (in Ethiopian context).
First, the data collection tool was prepared in the English language. Then, it was translated to a local language (Amharic and Afan Oromo) that can be understandable by study participants. Finally, the questionnaire was translated back to the English version to ensure its consistency with the previous initial version. Data collectors along with supervisors were trained for 2 days regarding the data collection procedure. The pretest was conducted on 25 participants (5% of total sampled participants) in Adama General Hospital located in the adjacent District. The results were used for the correction of the questionnaires. Supervisors and the principal investigator checked for completeness and consistency of the collected data. Codes were given for the completed questionnaires. Double data entry verification was done. Hematological data quality was assured following the Hospital’s Standard of Procedure. A standardized procedure was strictly followed during the blood and stool sample collection, storage, and analytical process. To obtain accurate measurements like maternal height, weight, and MUAC, 2 days of training was given for the data collectors using the standard manual of the hospital.
The collected data were checked, coded, and entered into EpiData version 3.02 and exported to SPSS version 20 for analysis (IBM SPSS statistics, 2012). Descriptive statistics were done using frequency tables. Bivariable logistic regression analysis was carried out to investigate the association between anemia and each independent variable. Variables with a p-value less than 0.25 were included in the final model of multivariable analysis. The multivariable logistic regression was done to control for any potential confounders and to identify the true effect of the selected predictor variables on anemia. The multi-collinearity was checked using a variance inflation factor (VIF) and tolerance, and no collinearity effects were detected. The model adequacy was checked using the Hosmer and Lemeshow goodness-of-fitness tests, and the result was found to be insignificant (p-value = 0.475), which indicates the model was fitted. Finally, the strength of associations between anemia and predictor variables was assessed and computed using the adjusted odds ratio (AOR) with 95% confidence, and the significance of the association was declared at a p-value of less than 0.05.
Ethical clearance was obtained from the Institutional Health Research Ethical Review Committee (IHRERC) of the College of Health and Medical Sciences, Haramaya University. A copy of the ethical letter was submitted to the Boset District Health Bureau. A letter of cooperation was written to Olenchity General Hospital. Consent to participate in the study was obtained from all study participants before the data collection. The informed, voluntary, written, and signed consent was obtained from each participant. In addition, informed, voluntary, written, and signed assent was also obtained from the guardians and parents of women age less than 18 years. Study participants were informed about their right to withdraw from the study at any stage. Confidentiality of the information was assured. The data collectors interviewed the participants in separated areas, and tests were done following standard laboratory protocol.
A total of 405 study participants were enrolled in the study with a response rate of 96.4%. The remaining six (1.5%) declined to participate in the study and nine (2.2%) were not willing to provide blood samples to determine their hemoglobin level. The mean age of the participants was 25.7 (SD ± 7.23), and more than half (53.6%) of them were in the age range of 15 to 24 years. The vast majority (73.8%) of study participants were from the Oromo ethnic group, and more than three-quarters of women were from an urban setting. About 155 (38.3%) of participants attended grade 12 or above, and the majority (288, 77.4%) were using pit latrine toilets. Concerning the service area, one-third (134, 33%) of participants were from the inpatient department (pediatrics, surgical, medical, and gynecology wards) (Table 1).
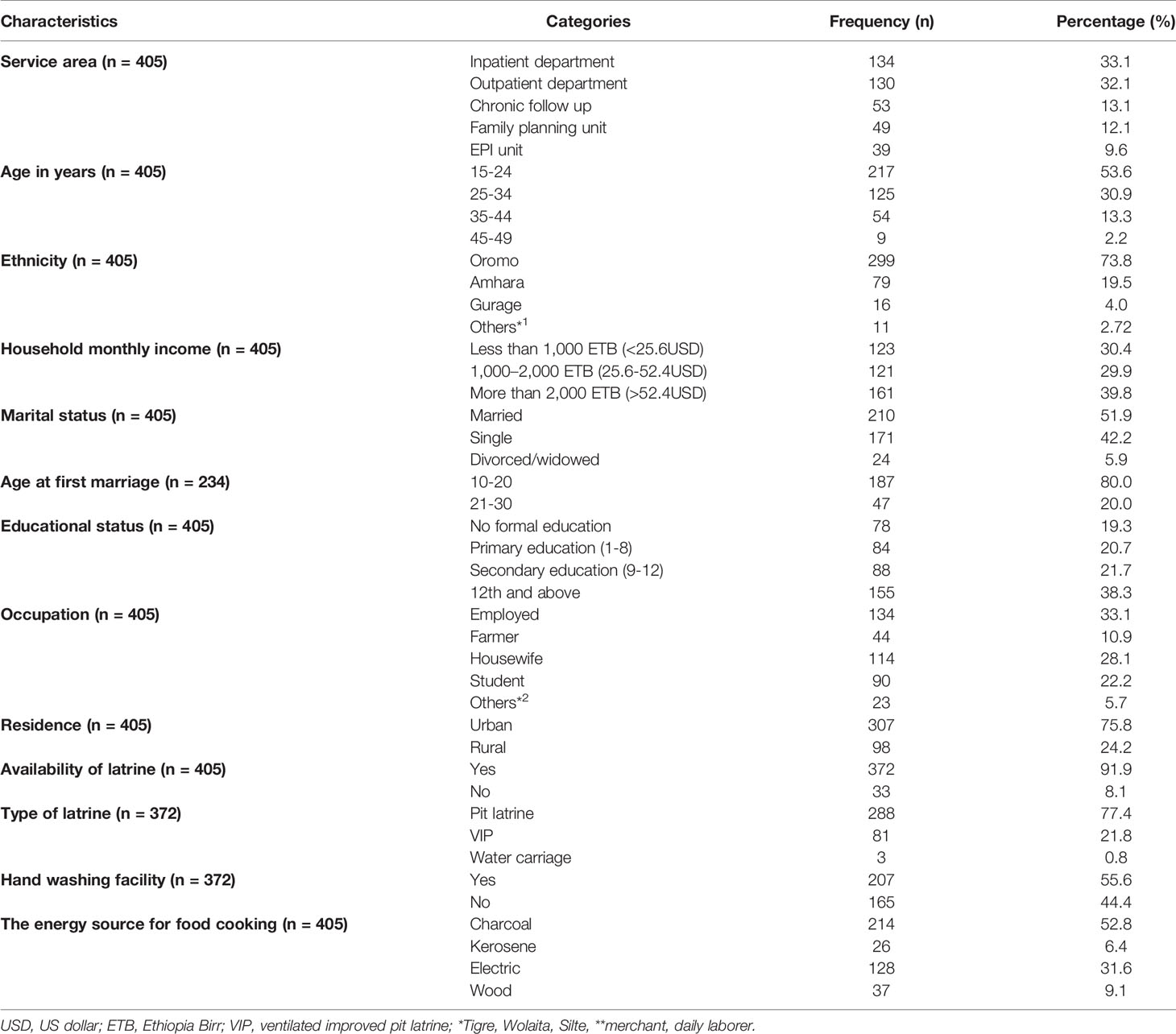
Table 1 Socio-demographic characteristics of nonpregnant reproductive-age women attending healthcare services in Olenchity General Hospital, central Ethiopia, 2018.
Of the 405 women enrolled in the study, the majority (82.5%) of them had experienced their first menses between the ages of 12 and 15 years and about 62% of them reported they had a regular menstrual cycle. More than two-thirds (67.7%) of women had an average menstrual flow while the rest had light and heavy menstrual flow (23.7% and 8.6%, respectively). More than half (64%) of them have used one to two sanitary pads per day during the menstrual period (Table 2).
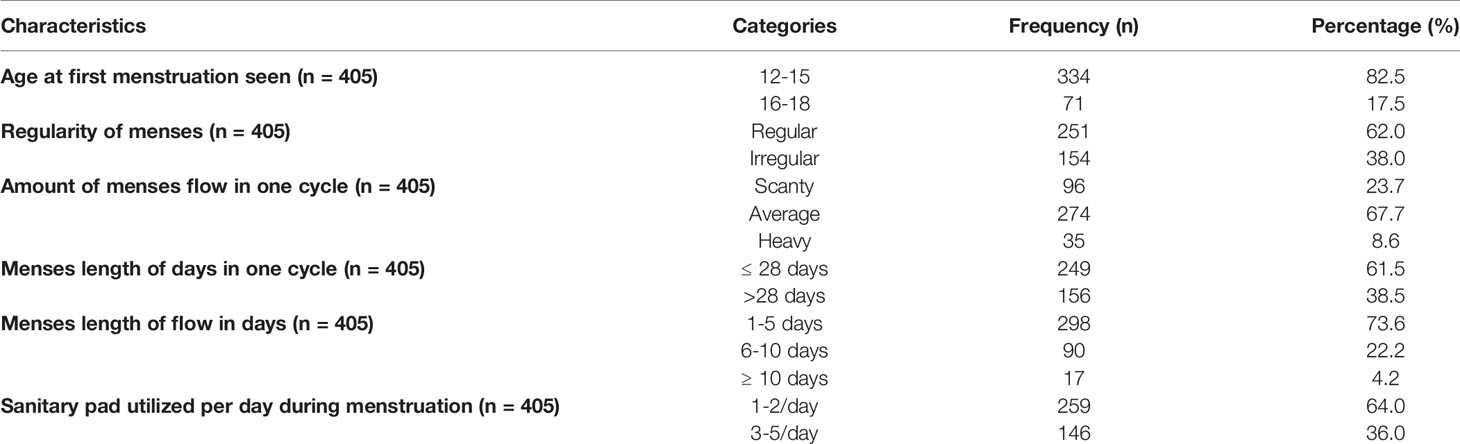
Table 2 Conditions related to the menstrual cycle among nonpregnant reproductive-age women attending healthcare services in Olenchity General Hospital, central Ethiopia, 2018.
Of the 405 women enrolled in the study, nearly two-thirds (60.4%) of them had ever heard about anemia and malnutrition. More than half (61.6%) of the responses were constituted to healthcare workers followed by attending school (15.1%), mass media (7.8%), and family members (6.9%) (Figure 1). In this study, insufficient dietary intake was the most common cause of anemia mentioned by the participants (46.4%) followed by excessive blood loss (22.2%), blood loss during pregnancy (10.4%), and heavy bleeding during menses (8.7%) (Figure 2).
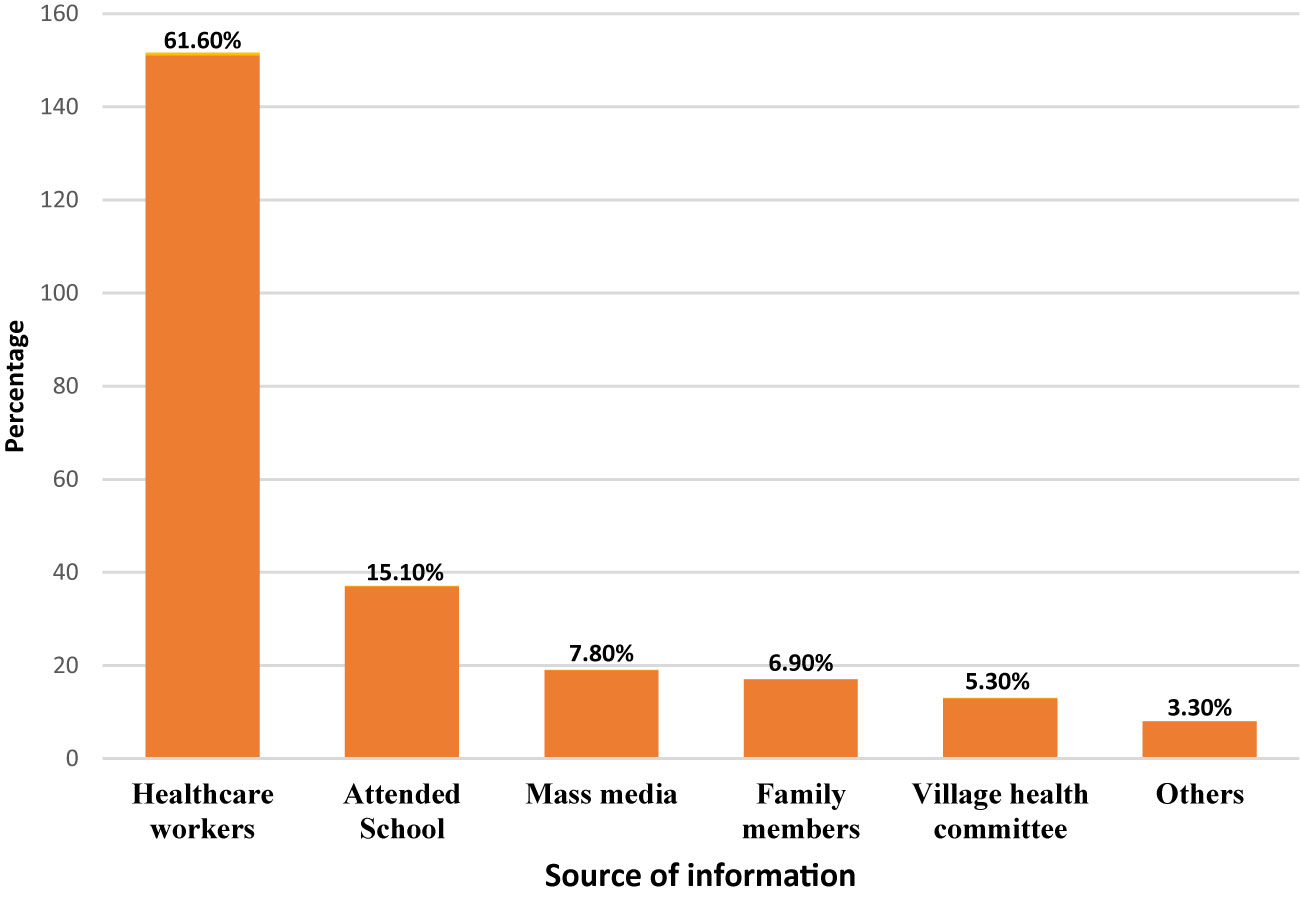
Figure 1 Source of information about anemia and malnutrition reported by nonpregnant reproductive-age women attending healthcare services in Olenchity General Hospital, central Ethiopia, 2018.
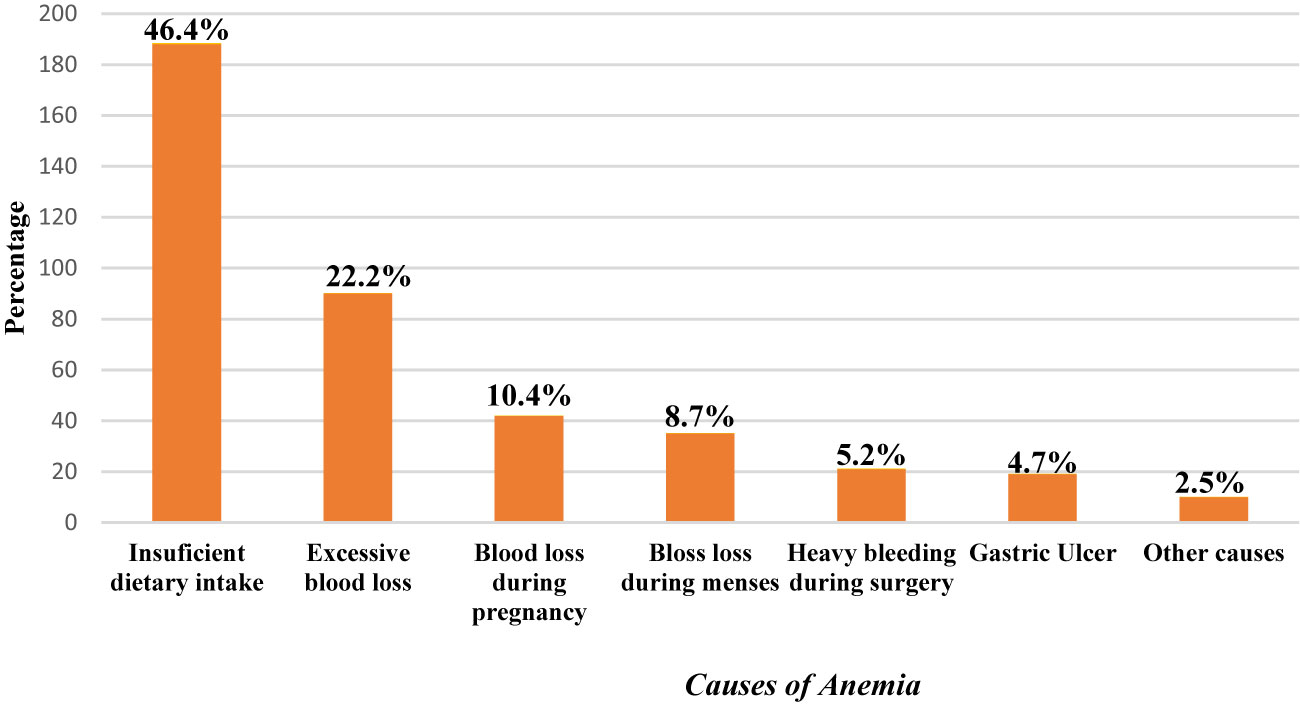
Figure 2 Causes of anemia reported by nonpregnant reproductive-age women attending healthcare services in Olenchity General Hospital, central Ethiopia, 2018.
This study found that 312 (77%) of the women were food secure based on the Household Food Insecurity and Access Scale (HFIAS). Concerning the food consumption score, about 235 (58%) of women had an acceptable (>42) FCS and nearly half, which is 189 (46.7%), of them obtained a medium dietary diversity score (Table 3).
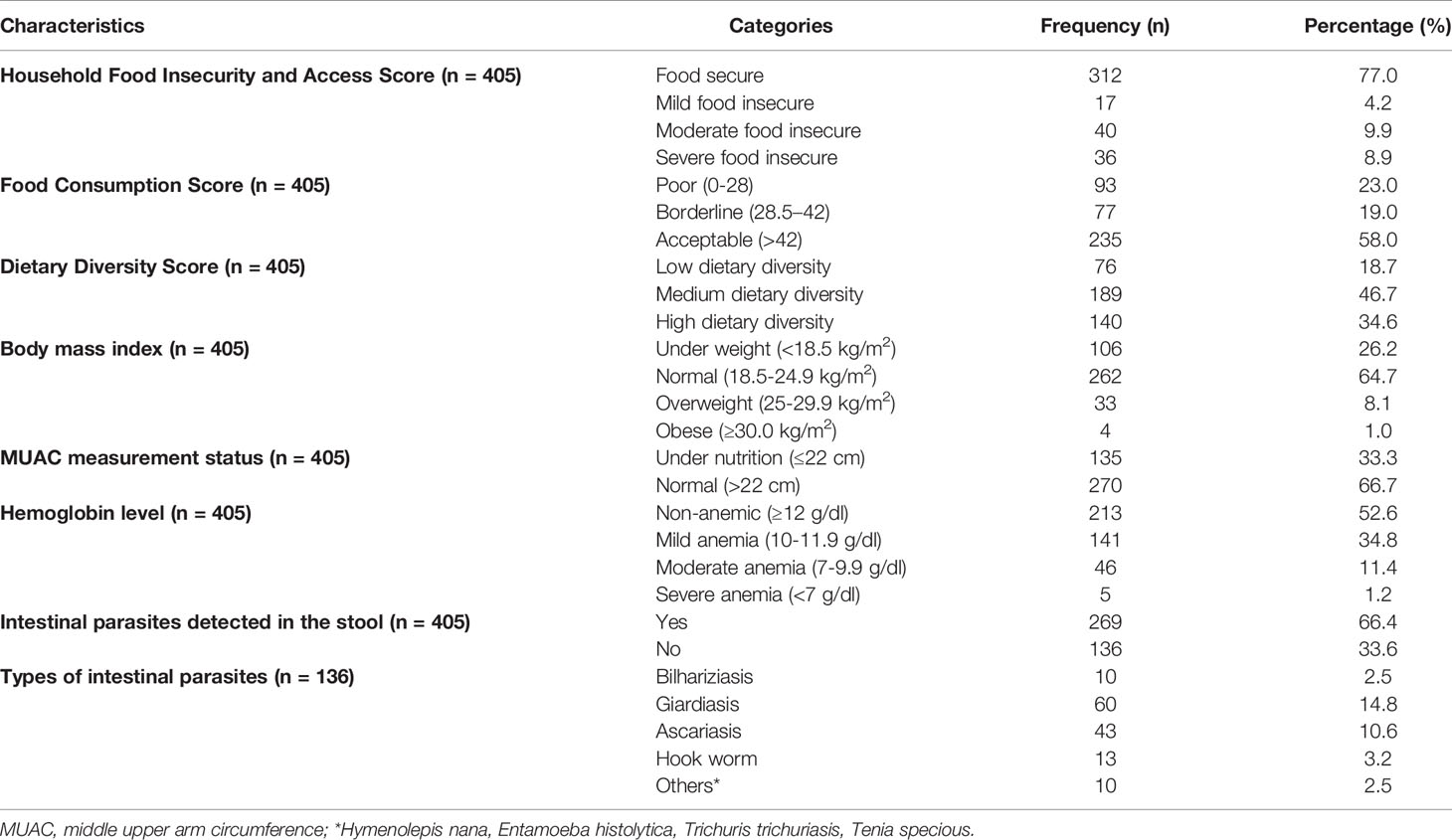
Table 3 Dietary diversity, household food insecurity status, and anthropometric and biochemical measurements among nonpregnant reproductive women attending Olenchity General Hospital, central Ethiopia, 2018.
In this study, the prevalence of anemia was found to be 47.4% [95% CI (42.7, 52.6)]. Around 34.8% of the women had mild anemia, 11.4% had moderate anemia, and 1.2% were severely anemic. About 26.2% of nonpregnant women were underweight (BMI <18.5 kg/m2), and 8.1% were overweight. From the total of 405 nonpregnant women whose stool samples were sent for microscopic examination, one-third (33.6%) tested positive for intestinal parasitic infection, of which 14.8% were positive for Giardiasis, 10.6% for Ascariasis, 3.2% for hookworm, and 3.5% for other parasitic infections (Table 3).
In bivariable analysis, variables like no formal education [COR=2.47, 95% CI (1.42, 4.31)], rural resident [COR=1.58, 95% CI (1.04, 2.51)], menses flow of 6–10 days [COR=1.69, 95% CI (1.05, 2.72)], irregular menses [COR=1.59, 95% CI (1.06, 2.38)], and using three to five sanitary pads/day [COR=1.89, 95% CI (1.26, 2.86)] were significantly associated with anemia. In the final model of multivariable logistic regression analysis, having no formal education, using three to five sanitary pads per day, an intestinal parasitic infection, history of chewing khat, and households with mild food insecurity were remained statistically associated with anemia. Accordingly, nonpregnant women with no formal education were more than two times likely to be anemic than women with an educational status of grade 12 and above [AOR=2.25, CI (1.02, 4.97)]. Women who used three to five sanitary pads per day during the menstrual period were nearly two times more likely to be anemic compared to those who utilized one to two pads/day [AOR=1.66, 95% CI (1.02, 2.68)]. Likewise, being positive for intestinal parasitic infections increases the odds of anemia by 2.28 [AOR=2.28, 95% CI (1.39, 3.47)]. In addition, women who had a history of chewing khat were four times more likely to be anemic than nonusers [AOR=4.45, 95% CI (1.18, 16.83)]. Finally, the odds of anemia were about three times higher among women from mildly food insecure households compared to women from food-secure households [AOR= 3.41, 95% CI (1.10, 10.58)] (Table 4).
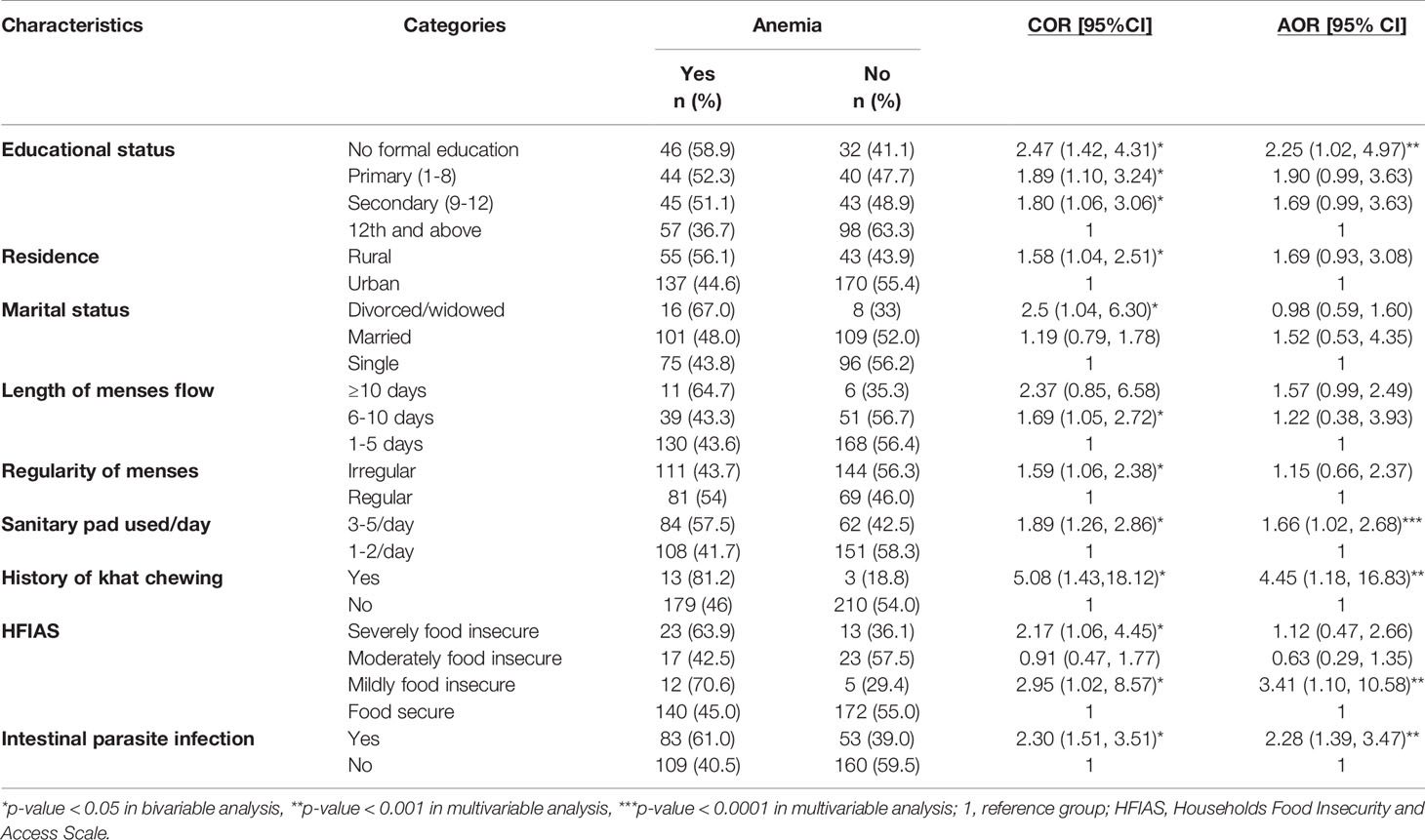
Table 4 Bivariable and multivariable logistic regression analysis of predictors of anemia among nonpregnant reproductive-age women attending healthcare services in Olenchity General Hospital, central Ethiopia, 2018 (N = 405).
In this study, anemia in NPRAW was found to be a severe public health problem. Overall, the prevalence of anemia was found to be 47.4%. This report was higher compared to previous studies done in other parts of Ethiopia with 27.4% in central Ethiopia (33) and 16.1% in Southwest Ethiopia (37, 38). This difference in magnitude might be because of socio-demographic differences of the study population and the geographical location of the study setting. The finding of this study also showed that the prevalence of anemia is higher (56.1%) among rural residents compared to urban dwellers. This is consistent with a study conducted in Bangladesh, which showed a higher prevalence of anemia among rural dwellers (39). This is likely due to many contributing factors that render women living in rural settings to be more likely to have anemia. For instance, most rural-dwelling Ethiopian women are uneducated or have a lower educational status compared to urban women. Moreover, difficulty in accessing basic preventive and curative healthcare services, poor eating habits due to various cultural and social norms, less access to information regarding anemia, and fewer economic opportunities compared to urban-dwelling women are also common.
Furthermore, the literature suggests that the etiology of anemia is complex and context-specific. Anemia may have multiple causes; even in the same individual, hematological manifestations of a particular cause can be masked by another. In our study, almost half (46.4%) of the study participants were aware that insufficient dietary intake is a cause of anemia, while awareness (based on participant reporting rates) was considerably lower for other factors such as accidental blood loss (22.2%), blood loss during pregnancy (10.5%), and heavy bleeding during menses (8.7%). Similar findings were also reported in previous studies (40, 41). This is because, in developing countries like Ethiopia, low dietary availability and an imbalanced diet are the major cause of anemia (42).
In the final model analysis, the report showed that women with no formal education had an increased risk of anemia compared to their counterparts. This finding is also supported by previous studies conducted in Southwest Ethiopia and India (25, 40). Nonpregnant women with no formal education have less access to information and likely lower socioeconomic status leading to an increased risk of anemia. Moreover, the findings of this study also indicated that women who use three to five sanitary pads per day during menstruation have an increased likelihood of being anemic. This is similarly observed in studies conducted in different parts of the world (41, 43). This might be attributed to greater blood loss during a menstrual period, which leads to a significant decrement in iron stores.
In this study, intestinal parasitic infection was significantly associated with anemia. Women who had intestinal parasitic infections were more likely to be anemic than women without intestinal parasitosis. This is also supported by previous studies done in Ethiopia (44, 45). The possible explanation is because the intestinal parasites have a detrimental effect on the intestinal mucosa affecting the absorption of iron and other micronutrients (19).
We also found that women from mildly food-insecure households had increased odds of anemia compared to women from food-secure households. A similar association was also observed in studies done in Pakistan, India, and Tanzania (29, 46, 47). This is because insufficient dietary intake exposes the individual to a higher risk of both being anemic and malnourished. Although the number of women who had a history of chewing khat was small, this behavior was found to be a predictor of anemia. A strong association between khat chewing and anemia was also observed in previous studies reported from elsewhere (37, 48, 49). The possible explanation is that khat is a psycho-stimulant substance that results in an overall loss of appetite and a consequently limited intake of food, resulting in a greater potential of getting anemic and micronutrient deficiency.
Strength of the study: in this study, we used validated tools to collect data from the participants. Limitation of the study: since the study was employed at snapshot, the causal association could not be determined. The study was conducted only in government public hospitals; NPRAW attending healthcare services at private health hospitals/clinics were not enrolled in the study.
This study revealed that anemia among nonpregnant women is a severe public health problem in central Ethiopia. More than six out of 10 NPRAW who had intestinal parasitic infections were suffering from some degree of anemia and malnutrition. Therefore, education on the most common causes of anemia should be a top priority. In addition, iron and folic acid supplementation, deworming, and food fortification are also very crucial. Heavy menses is also a contributing factor that may require the attention of health professionals. Since this study shows many NPRAW in Ethiopia have either preventable or treatable anemia, healthcare professionals should give more emphasis to reproductive-age women to mitigate these burdens. We also recommend the Federal Ministry of Health and other stakeholders to incorporate anemia in NPRAW as one reproductive health indicator. Further, longitudinal studies are also needed to better understand and characterize the contributing factors for anemia.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical clearance was obtained from the Institutional Health Research Ethics Review Committee (IHRERC) of the College of Health and Medical Sciences, Haramaya University. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
All authors have made a significant contribution to the conception, study design, data collection, data analysis, and interpretation of the findings. The authors also took part in writing the manuscript, reviewed the draft, and finally agreed on the journal to which the article has to be published. All the authors read and approved the final draft of the manuscript and also agreed to be accountable for all contents of the manuscript under circumstances.
This study was funded by Haramaya University. The funding organizations had no role in the study design, data collection, data analysis, and writing up of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors thank the Institutional Health Research Ethics Review Committee coordinating office of College of Health and Medical Sciences, Haramaya University, and Boset District health office staffs of Olenchity hospital for their unreserved contributions for this research paper; without their effort, this work could not be productive.
BMI, body mass index; EDHS, Ethiopian Demographic Health Survey; EMNS, Ethiopian Micro-Nutrient Survey; EPI, Expanded Program of Immunization; FANTA, Food and Nutrition Technical Assistance; HFIAS, Household Food Insecurity Access Scale; Hgb, hemoglobin; IDA, iron deficiency anemia; MUAC, mid-upper arm circumference; NPRAW, nonpregnant reproductive age women; UNICEF, United Nation Children’s Fund; WHO, World Health Organization.
1. Wirth JP, Woodruff BA, Engle-Stone R, Namaste SM, Temple VJ, Petry N, et al. Predictors of Anemia in Women of Reproductive Age: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) Project. Am J Clin Nutr (2017) 106(suppl_1):416S–27S. doi: 10.3945/ajcn.116.143073
2. World Health Organization. Global Nutrition Targets 2025: Anaemia Policy Brief (WHO/NMH/NHD/14.4). Geneva: World Health Organization (2014). Available at: https://apps.who.int/nutrition/publications/globaltargets2025_policybrief_anaemia/en/index.html.
3. Kang Y, Dang S, Zeng L, Wang D, Li Q, Wang J, et al. Multi-Micronutrient Supplementation During Pregnancy for Prevention of Maternal Anaemia and Adverse Birth Outcomes in a High-Altitude Area: A Prospective Cohort Study in Rural Tibet of China. Br J Nutr (2017) 118(6):431–40. doi: 10.1017/S000711451700229X
4. Stephen G, Mgongo M, Hussein Hashim T, Katanga J, Stray-Pedersen B, Msuya SE. Anaemia in Pregnancy: Prevalence, Risk Factors, and Adverse Perinatal Outcomes in Northern Tanzania. Anemia (2018) 2018:1–8. doi: 10.1155/2018/1846280
5. Ali AA, Rayis DA, Abdallah TM, Elbashir MI, Adam I. Severe Anaemia is Associated With a Higher Risk for Preeclampsia and Poor Perinatal Outcomes in Kassala Hospital, Eastern Sudan. BMC Res Notes (2011) 4(1):1–5. doi: 10.1186/1756-0500-4-311
6. Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, Regional, and National Trends in Haemoglobin Concentration and Prevalence of Total and Severe Anaemia in Children and Pregnant and non-Pregnant Women for 1995–2011: A Systematic Analysis of Population-Representative Data. Lancet Global Health (2013) 1(1):e16–25. doi: 10.1016/S2214-109X(13)70001-9
7. World Health Organization. Iron Deficiency Anaemia: Assessment, Prevention, and Control. A Guide for Programme Managers. In: Arch Dis Child: First Published as (2015), vol. 10. Geneva: WHO (2001).
9. World Health Organization. Global Health Observatory Data Repository: Anaemia in Children< 5 Years By Region. (2016).
10. World Health Organization. Global Health Observatory Data Repository: Prevalence of Anaemia in Women (2016). Available at: http://apps.who.int/gho/data/view.main (Accessed May 2, 2018). GSWCAH28REG.
11. WHO U, Mathers C. Global Strategy for Women’s, Children’s and Adolescents’ Health (2016-2030). Organization (2016) 201:4–103.
12. Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R, et al. A Systematic Analysis of Global Anemia Burden From 1990 to 2010. Blood (2014) 123(5):615–24. doi: 10.1182/blood-2013-06-508325
13. Balarajan Y, Ramakrishnan U, Özaltin E, Shankar AH, Subramanian SV. Anaemia in Low-Income and Middle-Income Countries. Lancet (2011) 378:2123–35. doi: 10.1016/S0140-6736(10)62304-5
14. World Health Organization. The Global Prevalence of Anaemia in 2011. WHO Rep (2015) 48:1–3. Available at: https://apps.who.int/iris/handle/10665/177094.
15. Hussein N, Kai J, Qureshi N. The Effects of Preconception Interventions on Improving Reproductive Health and Pregnancy Outcomes in Primary Care: A Systematic Review. Eur J Gen Pract (2016) 22(1):42–52. doi: 10.3109/13814788.2015.1099039
16. Dean SV, Lassi ZS, Imam AM, Bhutta ZA. Preconception Care: Nutritional Risks and Interventions. Reprod Health (2014) 11(S3):S3. doi: 10.1186/1742-4755-11-S3-S3
17. Young MF. Maternal Anaemia and Risk of Mortality: A Call for Action. Lancet Global Health (2018) 6(5):e479–80. doi: 10.1016/S2214-109X(18)30185-2
18. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and Child Undernutrition and Overweight in Low-Income and Middle-Income Countries. Lancet (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
19. Casey GJ, Montresor A, Cavalli-Sforza LT, Thu H, Phu LB, Tinh TT, et al. Elimination of Iron Deficiency Anemia and Soil Transmitted Helminth Infection: Evidence From a Fifty-Four Month Iron-Folic Acid and De-Worming Program. PloS Negl Trop Dis (2013) 7(4):e2146. doi: 10.1371/journal.pntd.0002146
20. Klemm RD, Sommerfelt AE, Alfred Boyo CB, Kotecha P, Steffen M, Franklin N. Are We Making Progress on Reducing Anemia in Women? Cross-Country Comparison of Anemia Prevalence, Reach, and Use of Antenatal Care and Anemia Reduction Interventions. USAID Micronutrient and Child Blindness Project (2011) 1–69.
21. Nguyen PH, Gonzalez-Casanova I, Nguyen H, Pham H, Truong T, Nguyen S, et al. Multicausal Etiology of Anemia Among Women of Reproductive Age in Vietnam. Eur J Clin Nutr (2015) 69(1):107–13. doi: 10.1038/ejcn.2014.181
22. Sadeghian M, Fatourechi A, Lesanpezeshki M, Ahmadnezhad E. Prevalence of Anemia and Correlated Factors in the Reproductive Age Women in Rural Areas of Tabas. J Family Reprod Health (2013) 7(3):139.
23. Pasricha S-R, Caruana SR, Phuc TQ, Casey GJ, Jolley D, Kingsland S, et al. Anemia, Iron Deficiency, Meat Consumption, and Hookworm Infection in Women of Reproductive Age in Northwest Vietnam. Am J Trop Med Hygiene (2008) 78(3):375–81. doi: 10.4269/ajtmh.2008.78.375
24. Figueiredo AC, Gomes-Filho IS, Silva RB, Pereira PP, Da Mata FA, Lyrio AO, et al. Maternal Anemia and Low Birth Weight: A Systematic Review and Meta-Analysis. Nutrients (2018) 10(5):601. doi: 10.3390/nu10050601
25. Asres Y, Yemane T, Gedefaw L. Determinant Factors of Anemia Among Nonpregnant Women of Childbearing Age in Southwest Ethiopia: A Community-Based Study. Int Scholarly Res Notices (2014) 2014:1–8. doi: 10.1155/2014/391580
26. Central Statistical Agency (CSA) [Ethiopia], ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA. CSA and ICF. (2016).
27. Haidar JA, Pobocik RS. Iron Deficiency Anemia Is Not a Rare Problem Among Women of Reproductive Ages in Ethiopia: A Community-Based Cross Sectional Study. BMC Hematol (2009) 9(1):1–8. doi: 10.1186/1471-2326-9-7
28. CSA. (2007). Summary and Statistcal Report of the 2007 Population and Housing Census Federal Democractic Republic of Ethiopia Population Census Commission December 2008 Addis Ababa.
29. Habib MA, Raynes-Greenow C, Soofi SB, Ali N, Nausheen S, Ahmed I, et al. Prevalence and Determinants of Iron Deficiency Anemia Among non-Pregnant Women of Reproductive Age in Pakistan. Asia Pacific J Clin Nutr (2018) 27(1):195. doi: 10.6133/apjcn.042017.14
30. Karki KB, Thapa P, Dhimal M, Bista B, Joshi A, Dhakal P, et al. Anemia and its Determinants Among Women of Reproductive Age in Mid-Western Tarai of Nepal 2015. Government Nepal Nepal Health Res Council (2015) 1–29. Available at: http://hdl.handle.net/123456789/789.
31. Hassan EO, El-Hussinie M, El-Nahal N. The Prevalence of Anemia Among Clients of Family Planning Clinics in Egypt. Elsevier Sci Inc (1999) 60:93–9. doi: 10.1016/S0010-7824(99)00066-9
32. FANTA. (2007). Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide VERSION 3.
33. WHO/UNICEF/UNU. Iron Deficiency Anaemia: Assessment, Prevention, and Control. Geneva: World Health Organization (2001). (WHO/NHD/01.3). (2001).
34. WHO. Physical Status: The Use and Interpretation of Anthropometry Report of a WHO Expert Committee. World Health Organ Tech Rep (1995) 854):1–452. Available at: https://apps.who.int/iris/handle/10665/37003.
35. Castell GS, Rodrigo CP, de la Cruz JN, Bartrina JA. Household Food Insecurity Access Scale (HFIAS). Nutricion Hospitalaria (2015) 31(3):272–8. doi: 10.3305/nh.2015.31.sup3.8775
36. McDonald C, McLean J, Kroeun H, Talukder A, Lynd L, Green T. Household Food Insecurity and Dietary Diversity as Correlates of Maternal and Child Undernutrition in Rural Cambodia. Eur J Clin Nutr (2015) 69(2):242–6. doi: 10.1038/ejcn.2014.161
37. Samson G, Enquselassie F. Correlates of Anemia Among Women of Reproductive Age in Ethiopia: Evidence From Ethiopian DHS 2005. Ethiop J Health Dev (2011) 25(1):22–30. doi: 10.4314/ejhd.v25i1.69842
38. Asres Y, Yemane T, Gedefaw L. Determinant Factors of Anemia Among Nonpregnant Women of Childbearing Age in Southwest Ethiopia. Hindawi Publishing Corporation Int Scholarly Res Notices (2014) 2014. doi: 10.1155/2014/391580
39. Kamruzzaman, Rabbani G, Saw A, Sayem A, Hossain G. Differentials in the Prevalence of Anemia Among Non-Pregnant, Ever-Married Women in Bangladesh: Multilevel Logistic Regression Analysis of Data From the 2011 Bangladesh Demographic and Health Survey. BMC Women’s Health (2015) (2015) 15:54. doi: 10.1186/s12905-015-0211-4
40. Siddiqui MZ, Goli S, Reja T, Doshi R, Chakravorty S, Tiwari C, et al. Prevalence of Anemia and Its Determinants Among Pregnant, Lactating, and Nonpregnant Nonlactating Women in India. SAGE Open (2017) 1–10. doi: 10.1177/2158244017725555
41. Lebso M, Anato A, Loha E. Prevalence of Anemia and Associated Factors Among Pregnant Women in Southern Ethiopia: A Community Based Cross-Sectional Study. PloS One (2017) 12(12):e0188783. doi: 10.1371/journal.pone.0188783
42. Gebreegziabher T, Stoecker BJ. Iron Deficiency was Not the Major Cause of Anemia in Rural Women of Reproductive Age in Sidama Zone, Southern Ethiopia: A Cross-Sectional Study. PloS One (2017) 12(9):e0184742. doi: 10.1371/journal.pone.0184742
43. Nelson AL, Ritchie JJ. Severe Anemia From Heavy Menstrual Bleeding Requires Heightened Attention. Am J Obstetrics Gynecol (2015) 213(1):97.e1–6. doi: 10.1016/j.ajog.2015.04.023
44. Haidar JA, Pobocik RS. Iron Deficiency Anemia is Not a Rare Problem Among Women of Reproductive Ages in Ethiopia. BMC Blood Disord (2009) 9:7. doi: 10.1186/1471-2326-9-7
45. Kumera G, Gedle D, Alebel A, Feyera F, Eshetie S. Undernutrition and its Association With Socio-Demographic, Anemia and Intestinal Parasitic Infection Among Pregnant Women Attending Antenatal Care at the University of Gondar Hospital, Northwest Ethiopia. Maternal Health Neonatol Perinatol (2018) 4(1):18. doi: 10.1186/s40748-018-0087-z
46. Wilunda C, Massawe S, Jackson C. Determinants of Moderate-to-Severe Anaemia Among Women of Reproductive Age in Tanzania: Analysis of Data From the 2010 Tanzania Demographic and Health Survey. Trop Med Int Health (2013) 18(12):1488–97. doi: 10.1111/tmi.12199
47. Mastiholi SC, Somannavar MS, Vernekar SS, Kumar SY, Dhaded SM, Herekar VR, et al. Food Insecurity and Nutritional Status of Preconception Women in a Rural Population of North Karnataka, India. Reprod Health (2018) 15(1):90. doi: 10.1186/s12978-018-0535-2
48. Kedir H, Berhane Y, Worku A. Khat Chewing and Restrictive Dietary Behaviors are Associated With Anemia Among Pregnant Women in High Prevalence Rural Communities in Eastern Ethiopia. PloS One (2013) 8(11):e78601. doi: 10.1371/journal.pone.0078601
Keywords: Ethiopia, predictors, reproductive age, non-pregnant women, malnutrition, anemia, intestinal parasitic infection
Citation: Yada TA, Dessie Y, Darghawth R, Wilfong T, Kure MA and Roba KT (2021) Magnitude of Intestinal Parasitosis, Malnutrition, and Predictors of Anemia Among Nonpregnant Reproductive-Age Women Attending Healthcare Services in Olenchity General Hospital, Central Ethiopia. Front. Trop. Dis 2:655690. doi: 10.3389/fitd.2021.655690
Received: 14 April 2021; Accepted: 29 June 2021;
Published: 21 July 2021.
Edited by:
James Rudge, University of London, United KingdomReviewed by:
Emmanuel Abraham Mpolya, Nelson Mandela African Institution of Science and Technology, TanzaniaCopyright © 2021 Yada, Dessie, Darghawth, Wilfong, Kure and Roba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed Abdurke Kure, bWFtZWVsZW1vQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.