- 1School of Pharmacy, Hubei University of Chinese Medicine, Wuhan, China
- 2Basic Medical School, Hubei University of Science and Technology, Xianning, China
The gut microbiome has emerged as a pivotal area of research due to its significant influence on the immune system and cognitive functions. Cognitive disorders, including dementia and Parkinson’s disease, represent substantial global health challenges. This review explores the relationship between gut microbiota, immune modulation, and cognitive decline, with a particular focus on the gut-brain axis. Research indicates that gut bacteria produce metabolites, including short-chain fatty acids (SCFAs), which affect mucosal immunity, antigen presentation, and immune responses, thereby influencing cognitive functions. A noteworthy correlation has been identified between imbalances in the gut microbiome and cognitive impairments, suggesting novel pathways for the treatment of cognitive disorders. Additionally, factors such as diet, environment, and pharmaceuticals play a role in shaping the composition of the gut microbiome, subsequently impacting both immune and cognitive health. This article aims to clarify the complex interactions among gut microbiota, immune regulation, and cognitive disorders, evaluating their potential as therapeutic targets. The goal is to promote microbiome-based treatments and lay the groundwork for future research in this field.
1 Introduction
Cognitive dysfunction, characterized by a notable deterioration or impairment in cognitive abilities, has emerged as a critical global health concern, impacting millions of individuals worldwide (1, 2). The prevalence of cognitive dysfunction is on the rise, primarily attributed to the rapid aging of populations (3). Research indicates that approximately 15.5% of individuals aged 60 and older experience cognitive dysfunction, a figure that escalates to 33.1% among those aged 90 and above (4). Furthermore, a study focusing on individuals aged 60 and older in China revealed an overall prevalence rate of 33.59% (5). The financial burden associated with the treatment of Alzheimer’s patients is substantial, with social and economic costs exceeding one trillion yuan (6, 7). These statistics underscore the profound societal and economic ramifications of cognitive impairment, highlighting the urgent need for further research in this critical area.
The human gut microbiota constitutes a complex microbial ecosystem that plays a crucial role in the immune system regulation (8). Research has established a significant connection between gut microbiota and immune function, encompassing the modulation of mucosal immunity, effects on antigen presentation, and the production of metabolites that influence immune responses, all of which can ultimately impact cognitive function (9–11). Furthermore, the interaction between the microbiome and the host’s immune cells can either promote tolerance or provoke inflammation (12). This underscores the dual role of the microbiome in maintaining immune balance while also having the potential to contribute to disease conditions (13–17).
The gut-brain axis encompasses a variety of signaling pathways that interconnected the neural, endocrine, and immune systems, facilitating the bidirectional communication between the gastrointestinal system and the central nervous system (18–20). Increasing evidence suggests that the gut microbiome significantly influences brain function, behavior, and potentially cognitive processes (21–23). Short-chain fatty acids (SCFAs) and other microbial metabolites can traverse the blood-brain barrier, thereby modifying neurotransmission and affecting neuronal activity (24–26). Dysbiosis, characterized by imbalances in gut microbiota, is strongly associated with cognitive decline (27–29). This body of evidence indicates that the gut-brain axis may present promising opportunities for therapeutic interventions.
This review utilized keywords such as “gut microbiome,” “immune regulation,” and “cognitive dysfunction” to synthesize and analyze contemporary literature from databases, including PubMed, Google Scholar, Web of Science, and CNKI. The primary focus was on the impact of dietary composition, environmental influences, and pharmacological treatments on mucosal immunity, systemic immune responses, and inflammatory diseases. Although current research indicates a connection between gut microbiota and cognitive function, our understanding of the mechanisms underlying these interactions remains limited. Additionally, the role of gut microbiota in preventing or mitigating cognitive impairments presents a significant challenge. Consequently, this review aims to bridge this knowledge gap by providing a comprehensive analysis of the relationships among gut microbiota, immune regulation, and cognitive dysfunction. It evaluates the therapeutic potential of targeting gut microbiota as a strategy to combat cognitive decline. The objective is to establish a scientific foundation for innovative treatment approaches that leverage gut microbiota to enhance cognitive health and slow the progression of neurodegenerative diseases. This investigation seeks to elucidate the complex mechanisms through which gut microbiota influences cognitive function and to pave the way for future pioneering research that could lead to effective prevention and treatment of cognitive impairments, ultimately offering hope to millions affected by these conditions.
2 Gut microbiome-immune system crosstalk in health and disease
2.1 Gut microbiota influence on mucosal immune responses
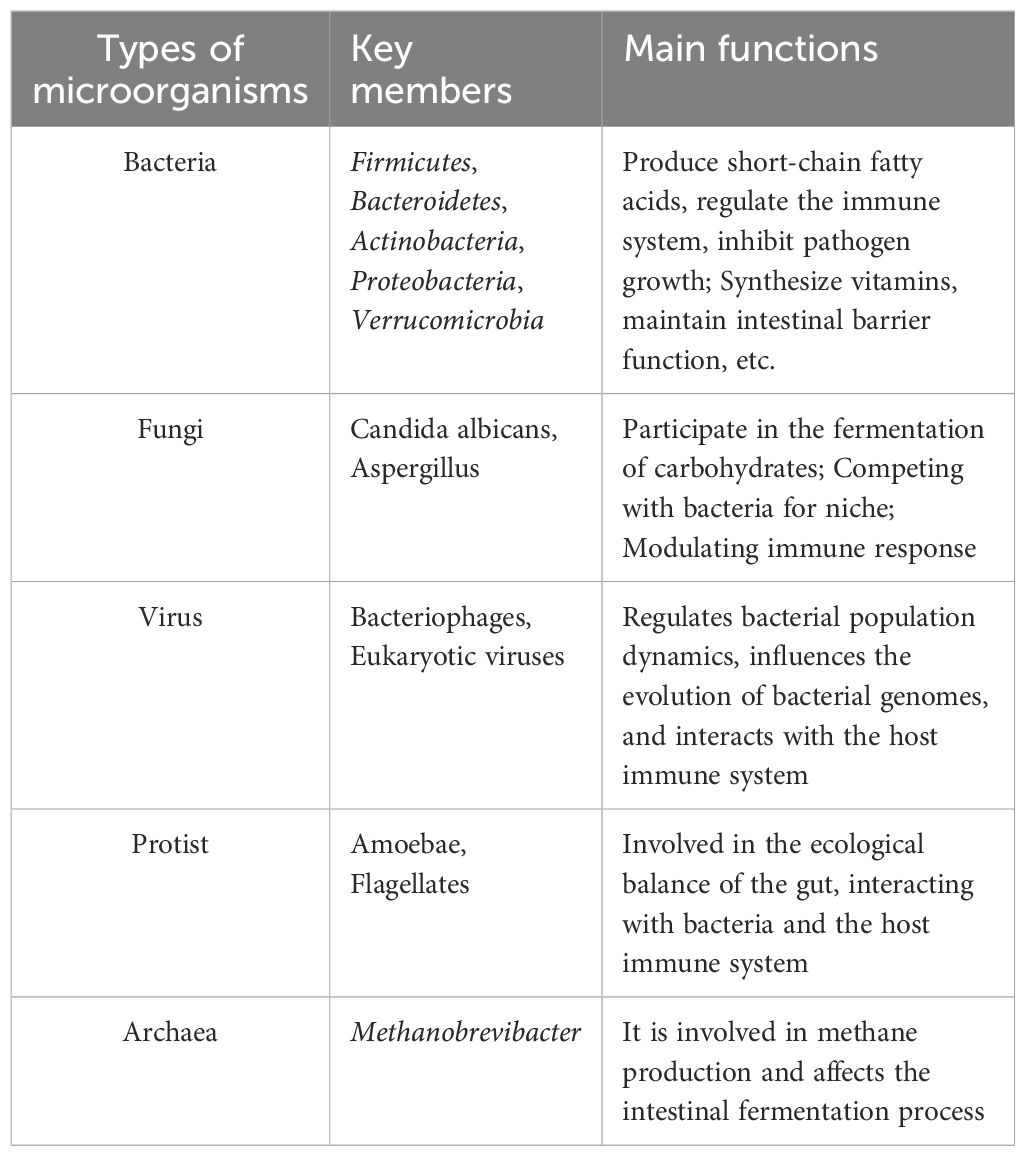
The gut microbiome encompasses the extensive and intricate assemblage of microorganism residing in the gastrointestinal tract of animals, significantly influencing mucosal immunity through sophisticated interactions with immune cells situated in the lower mucosa of the gut (30–32), as shown in Table 1. Recent research highlights the significant influence of gut microbiota on mucosal immunity, demonstrating that specific types of microbiotas can enhance both the development and functionality of immune cells (33). Amoroso et al. have shown that gut microbiota bioregulators can substantially impact mucosal immunity and intestinal inflammation (34). This influence is mediated through mechanisms that interact with host cells, thereby facilitating the maturation and activation of mucosal immune cells. Additionally, Lehmann et al. provide further insights, indicating that gut flora modulates the antigen presentation process by influencing innate lymphocytes (ILC3s), thereby establishing a strong connection with the host’s immune system (35).
In the field of organ transplantation, Dery et al. have provided valuable insights into the influence of gut microbiota on the immune system (36). Their research underscores the critical role that gut microbes play in modulating immune responses among transplant recipients. Furthermore, attention has turned towards probiotics, with Dowdell et al. demonstrating that Enterococcus and Lactococcus strains, sourced from Thai fermented sausages, exhibit significant probiotic activity (37). These strains have shown protective effects against Clostridium difficile infections, indicating that specific beneficial microbiota can substantially enhance host immune responses.
The therapeutic potential of gut microbiota in the treatment of colitis has attracted significant interest. Chiang et al. investigated the modulation of gut microbiota as a strategy for managing colitis, emphasizing fibroblast growth factor 19 (FGF19) as a promising therapeutic agent (38). In the context of cancer immunotherapy, research by Halsey et al. and Inamura underscores the vital role of gut microbiota in mediating therapeutic responses (39, 40). Their findings indicate that monitoring gut microbiota could enhance the effectiveness of immune checkpoint inhibitors.
2.2 Study on the interaction between intestinal flora and immune system
Complex interactions exist between the gut microbiome and the body’s immune and inflammatory responses (41, 42). Recent studies indicate that intestinal microorganisms are crucial for maintaining mucosal barrier function, regulating metabolic processes, and preserving immune balance (43–45). They also play a significant role in the onset, progression, and management of inflammatory bowel disease (IBD) (46). Dysbiosis, characterized by a decrease in beneficial bacteria and an increase in harmful strains, is strongly correlated with the development of IBD (47). For instance, patients with IBD demonstrate a reduction in butyrate-producing bacteria, which disrupts intestinal equilibrium (48). Furthermore, metabolites produced by gut microbiota, such as short-chain fatty acids (SCFAs), enhance gut barrier integrity by activating G protein-coupled receptors and promoting the generation and differentiation of regulatory T cells (TREGs), thereby supporting intestinal homeostasis (49–51). T cell subsets encompass helper T cells (CD4+ T cells) and cytotoxic T cells (CD8+ T cells), both of which play a pivotal role in cognitive function by modulating the blood-brain barrier and neuroinflammatory processes (52, 53). Furthermore, the immune cell repertoire also comprises B cell subsets and natural killer cells (NK cells), whose activities are intricately linked to memory functions (54).
The gut microbiota plays a crucial role in modulating inflammatory responses by influencing the activity of innate lymphocytes (ILCs) and T cells (41). For instance, Lactobacillus metabolizes tryptophan from the intestinal flora into indole-3 acetaldehyde, a metabolite that activates the aromatic hydrocarbon receptor (AhR) (55). This activation leads to the induction of IL-22 expression, which in turn stimulates epithelial cells to produce antimicrobial peptides, thereby supporting mucosal homeostasis. Furthermore, alterations in gut microbiota composition are associated with an increased susceptibility to inflammatory bowel disease (IBD) (56). Notably, certain bacteria, such as adhesive invasive Escherichia coli (AIEC), are prevalent in IBD patients, where they adhere to and invade intestinal epithelial cells, promoting the expression of inflammatory factors and contributing to the pathogenesis of IBD (57).
The gut microbiota played a crucial role in influencing immune and inflammatory responses by a variety of mechanisms. These mechanisms include the regulation of immune cell function, the preservation of intestinal barrier integrity, and the production of metabolites that modulate immune responses. These findings open new avenues for innovative therapeutic strategies aimed at the prevention, diagnosis, treatment, and prognosis of disorders related to the immune system.
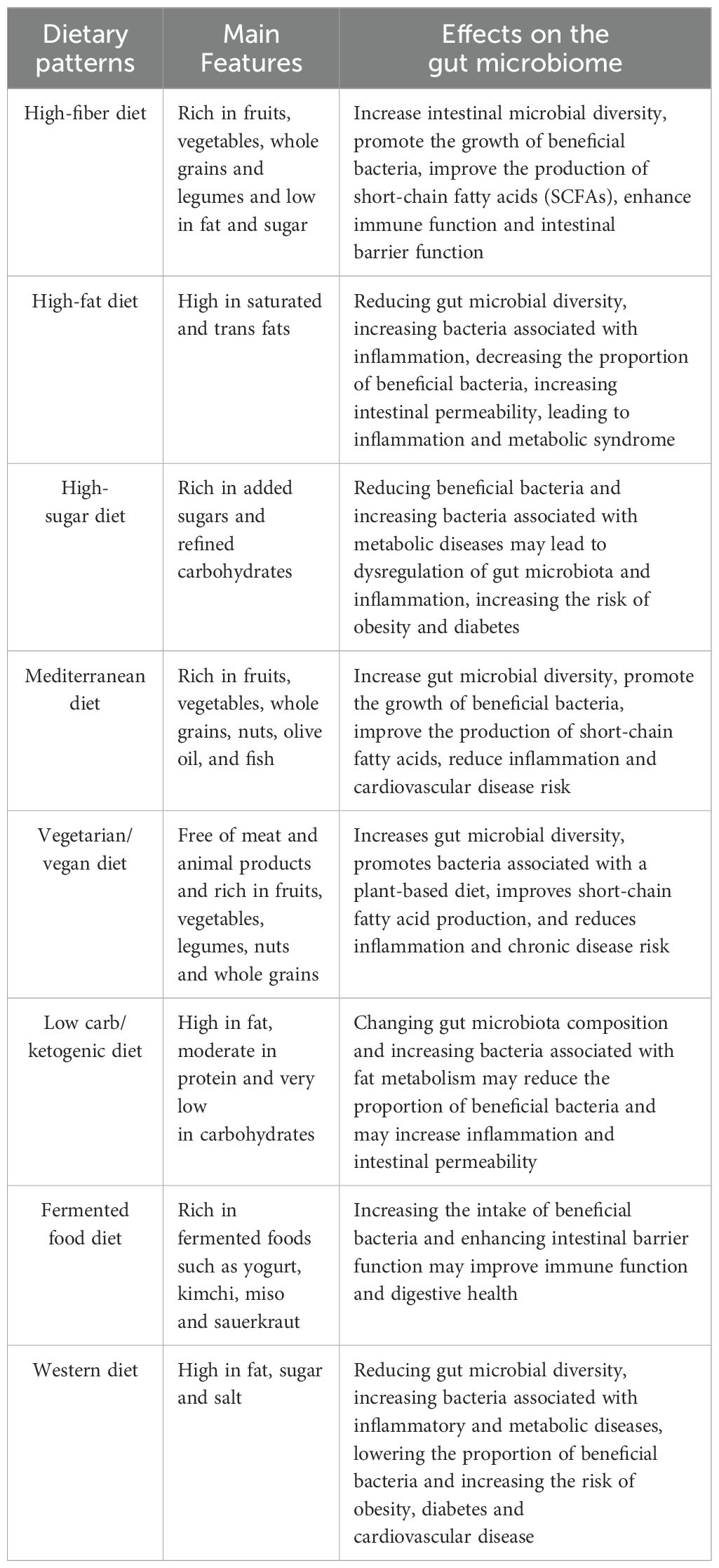
3 Influence of diet on gut microbiota and immunomodulation
Diet significantly influences the gut microbiota, which in turn profoundly affects the body’s immune status (58). Experimental data indicate that a high-fiber diet promotes the growth of beneficial bacteria, particularly short-chain fatty acid-producing bacteria (59–61). The metabolites of these bacteria can modulate immune cell function and elicit anti-inflammatory effects through the activation of G protein-coupled receptors, such as GPR43. For instance, Holscher posits that augmenting dietary fiber consumption can markedly enhance the proliferation of beneficial gut microbiota while concurrently reducing inflammatory marker levels (62). Conversely, a high-fat, high-sugar Western diet can disrupt the gut microbiota, leading to diminished microbial diversity and facilitating the colonization of pathogens, which may result in inflammation and an increased risk of autoimmune diseases (63). Recent studies have shown that participants adhering to a low-fiber, high-fat diet experienced a significant reduction in gut microbiota diversity and an increase in bacterial species associated with inflammatory bowel disease (64).
Short-chain fatty acids (SCFAs), especially butyric acid, have been demonstrated to activate immune cells through the GPR109A receptor, promoting the production of anti-inflammatory cytokines and thereby aiding in the maintenance of intestinal immune tolerance (65). Additionally, dietary fiber intake is closely associated with the composition of the gut microbiota; a high-fiber diet enhances the α-diversity of the SCFA-producing microbiome within the gut (66). Beyond their local effects, SCFAs also modulate the immune response in distal organs via the circulatory system.
The gut microbiota is notably influenced by a high-fat diet (HFD), which also affects immune function (67–69). Research has shown that HFD induces ferroptosis in intestinal regulatory T cells (Treg), a critical initial event leading to the disruption of immune tolerance and the onset of colitis. The ferroptosis of Treg cells results in a reduction of their immunosuppressive capabilities, thereby exacerbating the inflammatory response (70). Furthermore, HFD-induced dysbiosis of the intestinal microbiota increases intestinal barrier permeability, which promotes further activation of resident immune cells and elevates the production of reactive oxygen species (ROS) due to lipid peroxidation and Treg cell death (71). Importantly, the ferroptosis of Treg cells can be counteracted by antioxidant supplementation, such as α-tocopherol, which significantly alleviates colitis symptoms associated with a high-fat diet. These findings reveal novel mechanisms for modulating gut microbiota and immune responses through dietary interventions, suggesting potential therapeutic strategies for the prevention and management of diet-related chronic inflammatory diseases, as shown in Table 2. For example, a randomized controlled trial demonstrated that antioxidant vitamin E supplementation improved clinical symptoms while significantly reducing bowel inflammation in patients with colitis (72).
4 Exploring the correlation between gut microbes and cognitive dysfunction
The dietary modulation of the gut microbiome not only enhances immune functionality but also influences cognitive processes via the “gut-brain axis,” thereby facilitating a holistic regulation encompassing the gut microbiome, immune response, and cognitive function. The close association between gut microbes and cognitive function has emerged as a significant area of research in Alzheimer’s disease (73). Recent studies indicate that gut microbes influence host cognitive function through a gut-brain axis, which encompasses multiple complex mechanisms, including the production of neuroactive metabolites, modulation of immune responses, and maintenance of gut barrier function (74–76). In the pathophysiology of Alzheimer’s disease, alterations in the abundance of specific intestinal flora are closely linked to disease progression. For instance, amyloid-positive patients with Alzheimer’s disease demonstrate a lower relative abundance of Proctococcus and Bacillus subtilis, coupled with a higher abundance of E. coli/Shigella (77). The results indicate that alterations in gut microbiota and their equilibrium may be crucial in the development of Alzheimer’s disease. The imbalance of gut microbiota can result in elevated concentrations of pro-inflammatory cytokines (including IL-1β and TNF-α), which are conveyed to the central nervous system via the “gut-brain axis,” instigating neuroinflammatory responses. Lipopolysaccharides (LPS) generated by intestinal microbiota have the capacity to traverse the blood-brain barrier through systemic circulation, subsequently activating microglial cells, which can culminate in neuronal injury and a deterioration of cognitive abilities (78–80). Additionally, the gut microbiota may influence normal brain functioning by modulating nutrient absorption and metabolism (81).
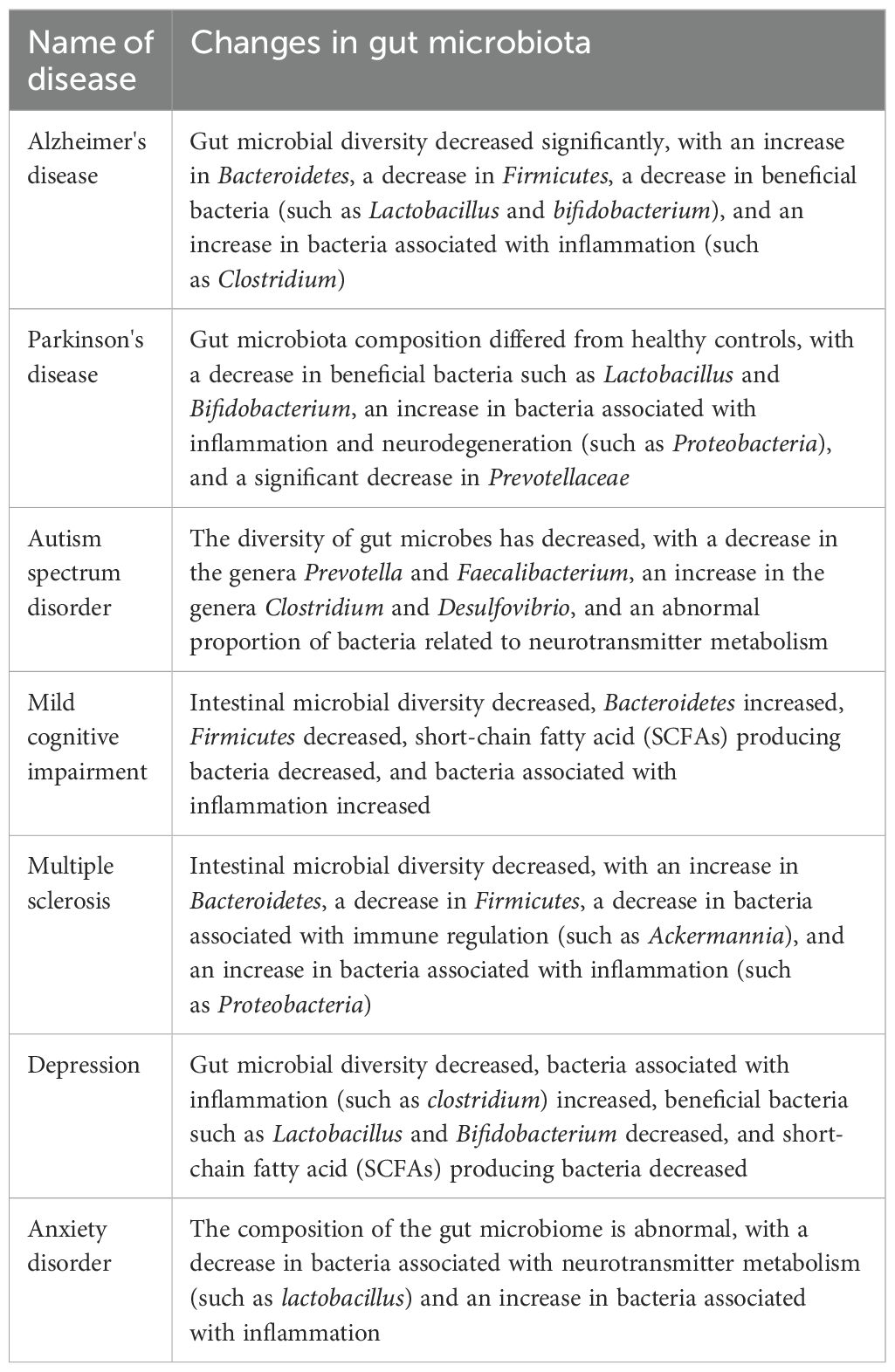
The neuroendocrine system plays a crucial role in the gut-brain axis (82). Gut-brain hormones, including leptin, may influence the perception of mental illness severity (83). Variations in leptin levels secreted by adipocytes can affect appetite regulation and energy metabolism, potentially leading to cognitive dysfunction in individuals with severe mental illnesses due to fluctuations in leptin levels (84). Furthermore, the neuroendocrine system regulates both the composition and function of gut flora, significantly impacting the gut-brain axis (83). For instance, under stress, the neuroendocrine system can modify the intestinal environment, resulting in an imbalance of gut flora that adversely affects cognitive function (84, 85). The gut microbiota can enter the bloodstream through short-chain fatty acids—such as acetic acid, propionic acid, and butyric acid—produced by the fermentation of dietary fiber, thereby influencing neural signaling in the brain (86). Notably, butyric acid, a metabolite of the gut microbiota, has been demonstrated to enhance neurogenesis and synaptic plasticity, positively impacting learning and memory processes (87). Short-chain fatty acids (SCFAs) can stimulate the secretion of mucus from intestinal epithelial cells through the modulation of the gut-brain axis. They enhance the integrity of the intestinal barrier, preventing the translocation of intestinal endotoxins, such as lipopolysaccharides, into the bloodstream. Furthermore, SCFAs influence the synthesis and metabolism of neurotransmitters and play a role in regulating neuroinflammation, as illustrated in Figure 1. They are crucial for maintaining the equilibrium of gut microbiota and impacting the metabolites produced by these microbial communities. Additionally, SCFAs promote neurogenesis and synaptic plasticity, facilitating the proliferation and differentiation of neural stem cells while improving synaptic transmission efficiency. Moreover, they exhibit antioxidant properties and support mitochondrial function, counteracting free radicals to safeguard the normal physiological activities of neurons and mitochondria. Additionally, the gut microbiota stimulates gut-associated lymphoid tissue (GALT), which influences the maturation and differentiation of immune cells, thereby regulating the systemic immune response (88). The composition of the gut microbiota is correlated with disease severity, and autoimmune diseases such as multiple sclerosis (MS) suggest that it may modulate the inflammatory state of the central nervous system (CNS) by affecting the immune response (89).
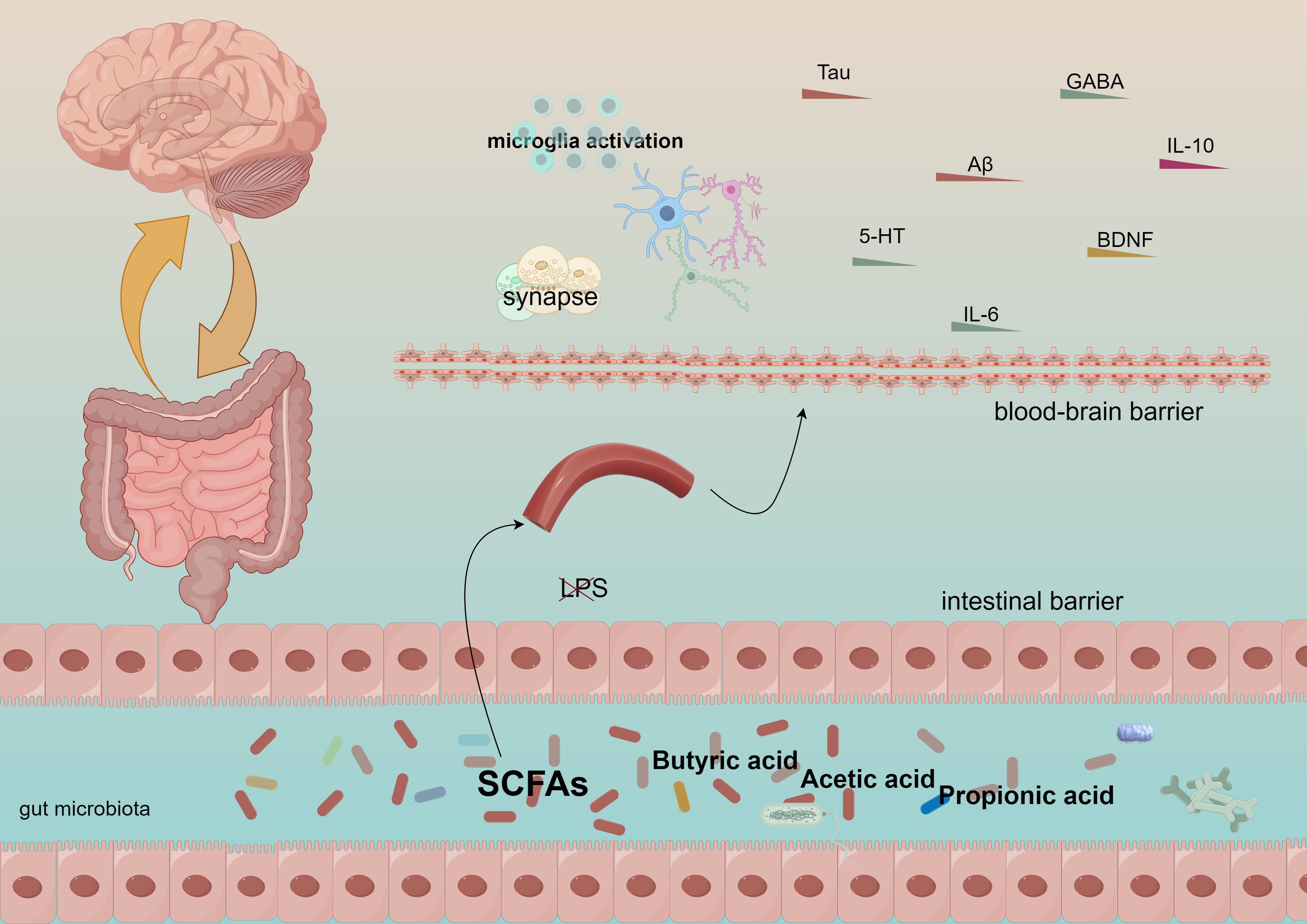
Figure 1. Short-chain fatty acids generate acetic acid, propionic acid, and butyric acid, which traverse the intestinal barrier and the blood-brain barrier, subsequently influencing the immune system and cognitive functions.
The mechanism of bidirectional gut-brain axis regulation refers to the brain’s role in regulating intestinal function while simultaneously influencing the composition and function of the gut microbiota (83). Stress and emotional states, mediated through the vagus nerve and hypothalamic-pituitary-adrenal (HPA) axes, impact the gut microbiota, which in turn affects cognition and mood (89, 90). Diet is another crucial factor shaping the composition of the gut microbiota; a high-fiber diet promotes the proliferation of beneficial bacteria and exerts anti-inflammatory effects, while a high-fat, high-sugar diet may disrupt this balance, triggering inflammation and autoimmune disorders that can impair cognitive function, as illustrated in Figure 2.
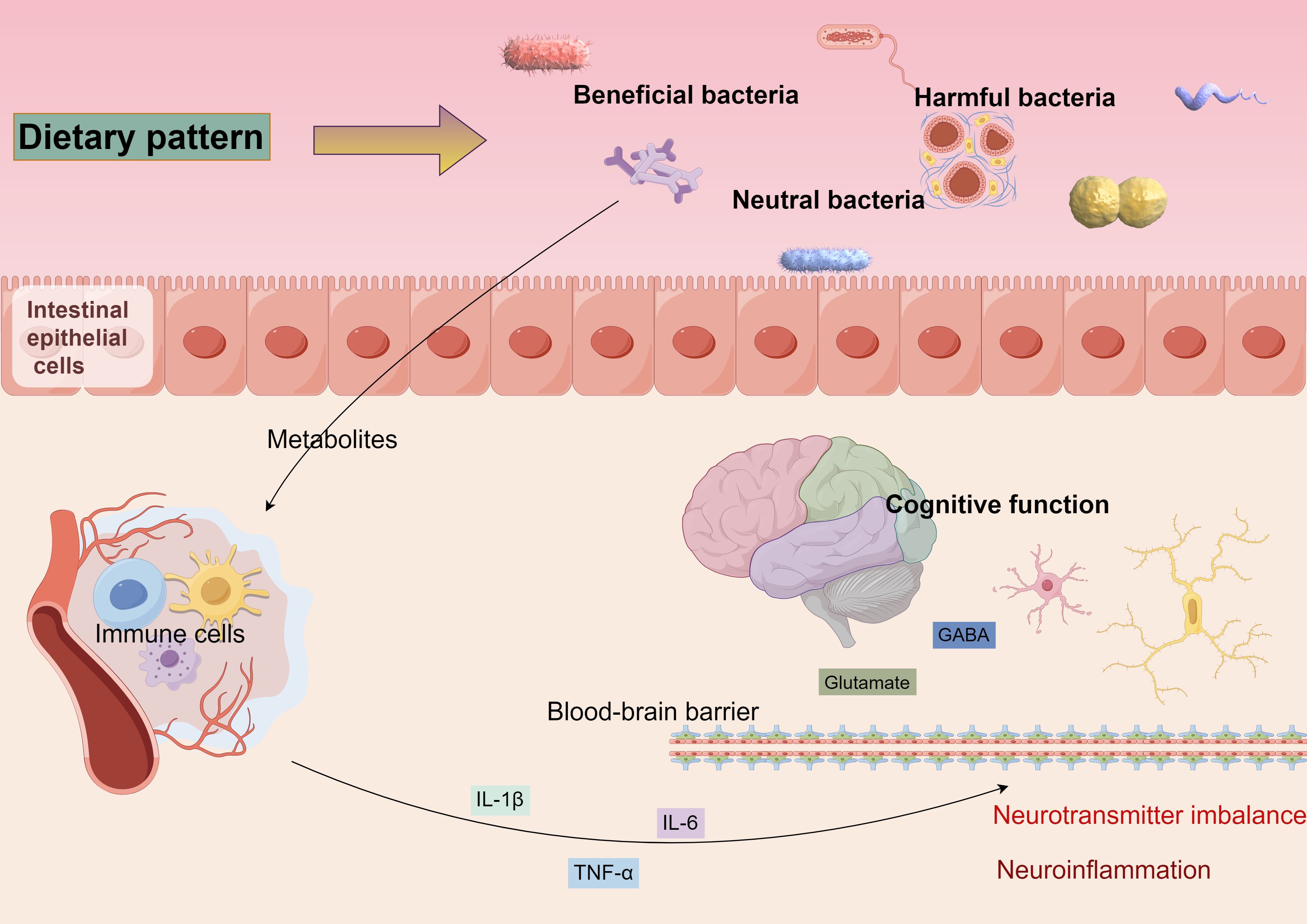
Figure 2. Diverse dietary patterns can alter the equilibrium of beneficial, detrimental, and neutral microbiota, leading to modifications in gut flora. These alterations can impact the integrity of the intestinal barrier, resulting in metabolites entering the bloodstream that activate the immune response. This activation prompts immune cells to secrete inflammatory mediators, which may traverse the blood-brain barrier, instigating neuroinflammation and disrupting neurotransmitter homeostasis, ultimately contributing to cognitive function alterations.
Research on the gut-brain axis offers new strategies for addressing cognitive dysfunction. Modulating the gut microbiota through probiotics, prebiotics, or fecal microbial transplantation (FMT) may enhance cognitive function (91). Furthermore, the development of drugs targeting specific gut microbial metabolites or immunomodulatory pathways represents a promising direction for future cognitive dysfunction treatments. In conclusion, the relationship between gut microbiota and cognitive dysfunction is a complex interplay involving multifactorial and multi-mechanism interactions. Future studies should further investigate the specific mechanisms by which gut microbiota influences cognitive function through the gut-brain axis and develop novel therapeutic strategies to enhance human health and cognitive performance.
5 The role of gut microbes in neurodegenerative diseases
Neurodegeneration is a multifactorial process influenced by genetic, environmental, and lifestyle factors, resulting in a progressive loss of neuronal structure and function (92). This deterioration gives rise to various neurodegenerative disorders, such as Alzheimer’s disease (AD), Parkinson’s disease (PD), and amyotrophic lateral sclerosis (ALS), which significantly debilitate individuals (93). The pathological features of these conditions encompass abnormal protein accumulation, mitochondrial dysfunction, oxidative stress, and neuroinflammation, ultimately leading to severely impaired cognitive and motor functions.
In recent years, researchers have recognized that the gut microbiota, a diverse community of microorganisms residing in the digestive tract, may influence the host’s nervous system through the gut-brain axis, potentially regulating neurodegenerative processes (94). The gut-brain axis encompasses complex interactions among the nervous, endocrine, and immune systems, with the gut microbiota communicating with the central nervous system through these pathways, thereby influencing the host’s behavioral and cognitive functions (74). Clinical studies have demonstrated that the abundance of the Mycobacterium anisopliae phylum in the gut of AD patients is decreased compared to that of the healthy population, while the abundance of the Mycobacterium thickum phylum is increased (95). Furthermore, the gut microbiota of patients with PD exhibits a reduced abundance of certain spore-producing bacteria, such as Christensenaceae, which is negatively correlated with the severity of motor dysfunction (96). Dysbiosis, characterized by disturbances in the composition and function of the gut microbiota, has now been associated with neurodegenerative pathologies (83), as illustrated in Table 3. Research has demonstrated that dysbiosis of the gut microbiota can result in neuroinflammation and compromise the integrity of the blood-brain barrier, disrupt the metabolism of neurotransmitters and neuromodulators, induce immune system dysfunction, increase oxidative stress levels, lead to the overproduction of reactive oxygen species (ROS), and impair neuronal and mitochondrial functions. For instance, the gut microbiota profiles of AD and PD patients differ significantly from those of healthy individuals, suggesting a possible causal relationship between microbial imbalance and disease progression (97). In AD patients, the abundance of inflammation-associated bacteria, such as Enterobacteriaceae, is elevated in the gut, whereas the abundance of bacteria with anti-inflammatory effects, such as Bifidobacteria, is diminished (98). Similar alterations have also been observed in patients with PD, indicating a potential relationship between changes in gut microbiota composition and the development of neurodegenerative diseases (99).
Clinical data further confirm that gut barrier dysfunction is associated with disease progression in ALS patients (100). The disruption of gut barrier function can cause or exacerbate neuroinflammation by allowing microbial sub-metabolites to enter the brain via the circulatory system. Inflammation plays a crucial role in neurodegeneration (76). Pro-inflammatory cytokines, such as tumor necrosis factor beta (TNF-β), interleukin 1β (IL-1β), and interleukin 6 (IL-6), disrupt the blood-brain barrier (BBB), enabling peripheral immune cells to infiltrate the central nervous system and aggravate neuroinflammation (101). This inflammatory environment leads to neuronal damage and death, which is strongly associated with the pathological processes of neurodegenerative diseases, such as AD and PD. This is further substantiated by clinical data indicating early alterations in the microbiome of patients with Alzheimer’s disease (74). In addition, reduced estrogen levels following menopause can result in alterations to the gut microbiome’s composition, heightening the risk of systemic and neuroinflammation. Furthermore, an increased presence of pro-inflammatory gut microbiota in males may more profoundly trigger these neuroinflammatory mechanisms, thereby hastening neuronal impairment and cognitive deterioration (102).
The anti-inflammatory effects of short-chain fatty acids (SCFAs) have been corroborated by clinical studies (103). For instance, a clinical trial demonstrated that cognitive function could be significantly improved by supplementing derivatives of butyric acid in patients with mild to moderate AD (87). Additionally, the production of neurotransmitters, such as gamma-aminobutyric acid (GABA), the primary inhibitory neurotransmitter in the central nervous system, and glutamate, the main excitatory neurotransmitter, is also influenced by the gut microbiota (81). By modulating the metabolic pathways of these neurotransmitters, the gut microbiota may significantly impact neurotransmission and synaptic plasticity, subsequently affecting cognitive and emotional functions. In summary, the gut microbiota may play a pivotal role in the development of neurodegenerative diseases by influencing the gut-brain axis through metabolite production and signaling, Figure 3. Future studies should further explore the mechanisms of interaction between the gut microbiota and neurodegenerative diseases and evaluate potential strategies to prevent or treat these conditions by modulating the gut microbiota.

Figure 3. An intact gut, characterized by its tight junctions and well-regulated immune cell populations, is essential for the synthesis of short-chain fatty acids (SCFAs) and the mitigation of inflammation within the organism. Conversely, when the intestinal barrier is compromised, there is an elevation in immune mediators and metabolites, which subsequently activates an immune response in the intestinal mucosa and promotes inflammatory processes. These alterations, through their impact on hippocampal neurons, may ultimately contribute to cognitive impairments.
6 Exploring the potential of using the gut microbiota as a therapeutic target
The strong correlation between gut microbiota and human health is at the forefront of medical research, with these microbes playing crucial roles in digestion, immune system regulation, and cognitive function (104, 105). Consequently, they represent potential therapeutic targets for the treatment of immune-related diseases and cognitive dysfunction. In addressing these conditions, new strategies for adapting the composition and function of gut microbiota have been developed, Figure 4.
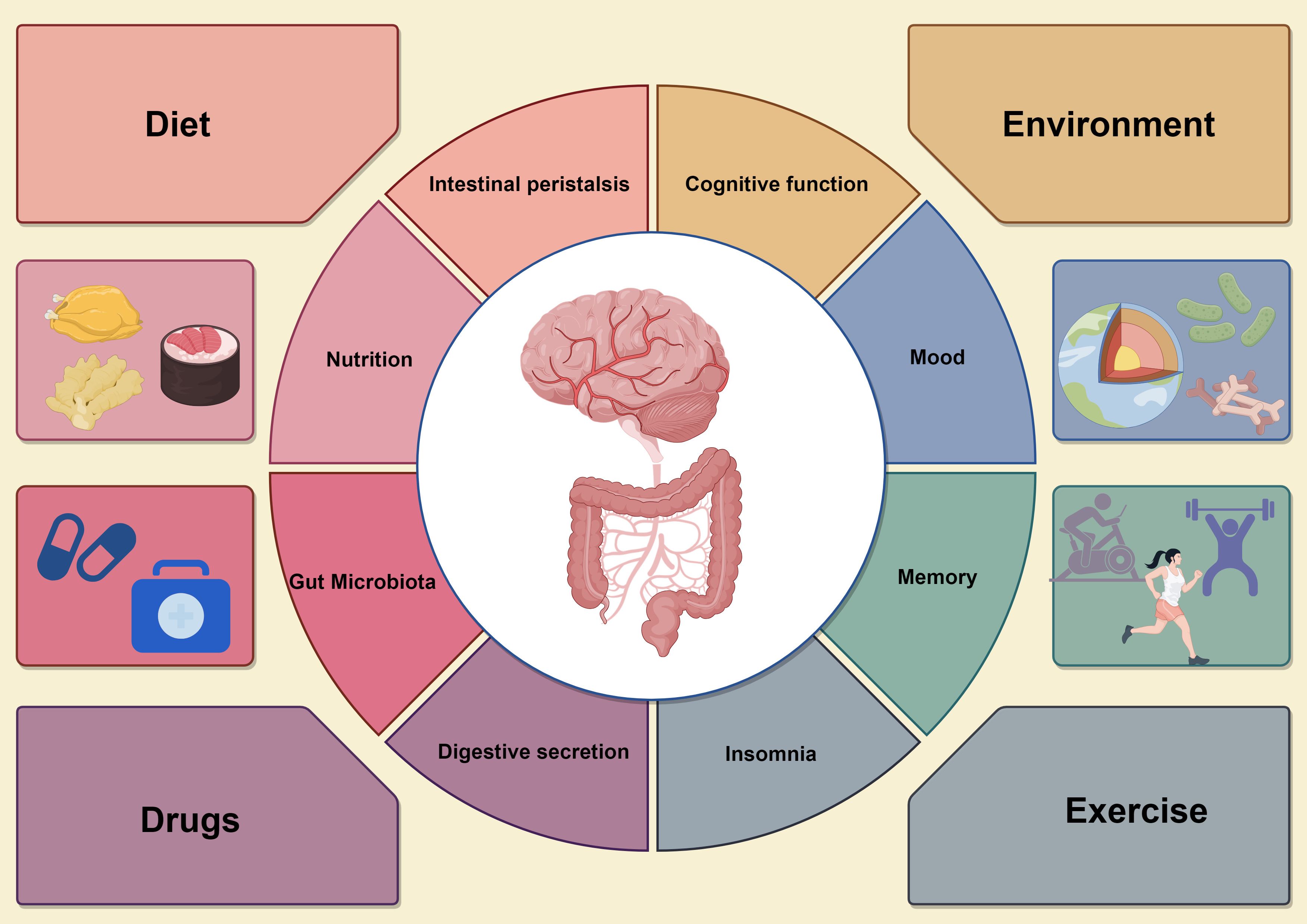
Figure 4. The circular diagram on the left shows the various effects of the gastrointestinal system, including microbiome balance, immune response, intestinal barrier integrity, and short-chain fatty acid (SCFA) production, all which support gut health. In contrast, the circular graph on the right illustrates how gut health affects neurological function, particularly cognitive processes, emotions, and neuroinflammatory responses. Dysbiosis in the gut microbiota can lead to increased pro-inflammatory mediators, impairing brain function and causing cognitive deficits. The four surrounding factors represent interventions to improve gut microbiota, such as dietary changes, probiotics and prebiotics supplementation, careful antibiotic use, and lifestyle changes like exercise and stress management. These strategies enhance both gut and brain health, promoting overall physical and mental well-being by optimizing gut microbiota composition and function.
6.1 Dietary effects on gut microbiota
The impact of dietary patterns on gut microbes represents a comprehensive area of research that encompasses the function of the microbiome and its influence on host health through metabolites. Recent studies have demonstrated that gut microbial assemblages can undergo significant changes, which subsequently affect their function and metabolite production. For instance, different dietary habits, such as fiber-rich diets and high-fat diets, can lead to notable alterations in gut microbial composition (106). Fiber-rich diets have been shown to promote the production of short-chain fatty acids (SCFAs) by gut microbes, metabolites that play a crucial role in gut health and systemic immune regulation (66). Researchers have investigated the protein expression of gut microbes through controlled dietary interventions and have found that the composition and function of the microbiota can change rapidly in response to dietary modifications. These changes may have significant implications for drug metabolism, particularly concerning the capacity of certain microbial communities to metabolize drug components, thereby influencing drug bioavailability and efficacy.
Moreover, dietary patterns, by altering the metabolic pathways of gut microbes, may also be linked to various disease risks, including the association between gut microbes and colorectal cancer (CRC) risk (107). Fine-tuning gut microbes through dietary interventions may serve as a relevant tool for disease prevention and treatment. Thus, the impact of dietary patterns on gut microbes is a multifaceted process that affects gut health, overall immune response, and drug efficacy, influencing not only the type and abundance of gut microbes but also their metabolic activities. Future studies should further investigate the specific mechanisms by which dietary patterns affect the composition and function of gut microbes to provide more effective dietary guidance for the prevention and treatment of related diseases in clinical practice.
6.2 Influence of environmental factors on gut microbiology
In exploring the complex relationship between environmental factors and changes in gut flora, modern scientific research has revealed that various environmental factors—including diet, drugs, and environmental pollutants—affect the structure and function of the gut microbial community (108). Diet, being the most direct environmental factor, influences host health by altering the species composition of gut microbes and their metabolic activities, which subsequently impact host well-being. For instance, studies involving controlled diets have demonstrated that quantitative analysis of microbial protein expression reveals regulation of gut microbes by dietary patterns, evidenced by altered expression of microbial proteins, which in turn affects host metabolism (106). In addition to diet, regulating gut microbial composition is also significantly influenced by drugs. Research has shown that gut microbes not only influence the efficacy and toxicity of drugs through their metabolism but can also participate in the catabolism of drugs, thereby affecting drug metabolic pathways in the host. This interaction underscores the increasing importance of the gut microbial community as a critical consideration in individualized medical and therapeutic strategies.
Pollutants in the environment can adversely affect host health by altering the composition of gut flora (109). Recent studies have indicated that pollutants are associated with an increased risk of developing various diseases, including colorectal cancer, by disrupting the balance of the gut microbial community (108). Further research has demonstrated that gut microbiota, modified by specific environmental factors, can interact with host genetic factors to influence disease development. Notably, the establishment of gut flora during early infancy is significantly influenced by the mode of birth and early feeding practices, which have long-term implications for future health and development. Changes in the composition of gut flora at this stage can set the foundation for individual immune regulation and cognitive function (110).
In summary, environmental factors exert a multidimensional impact on the composition and function of gut microorganisms, leading to significant effects on host health. Future studies exploring the relationship between environmental factors, gut microbes, and host health, as well as the prevention and treatment of various diseases, are anticipated to yield new strategies.
6.3 Effects of drugs on gut microbiology
Drugs passing through the gastrointestinal tract may be altered by interactions with microorganisms, thereby affecting the efficacy and safety of the drug (111). A study by Malfatti et al. demonstrated that gut microorganisms can influence the biodistribution of drugs, particularly impacting the metabolism of acetaminophen (112). Furthermore, individual differences in microbial communities can lead to variations in drug response; Gurry et al. identified functional heterogeneity by examining the fermentation capacity of intestinal microbes in healthy populations, indicating that the composition of individual microbial populations may influence the impact of microbes on drug efficacy (113). The metabolic pathways of drugs within the organism are intricate, and their metabolism is characterized by complexity. The involvement of microorganisms can further diversify these metabolic pathways. Certain drugs can generate new metabolites that are subsequently metabolized by gut microbes. These microbial metabolites may exhibit varying biological activities, with some potentially enhancing the efficacy of the drug, while others may be toxic.
Gut microbes can establish a competitive relationship with drugs that influence drug absorption. As described by Madhusoodanan, microorganisms can compete for the intestinal absorption of the host by metabolizing drugs, which subsequently affects the blood concentration and efficacy of these medications (114). This phenomenon underscores the importance of microbiota in drug efficacy. The interactions between gut microbes and drugs significantly impact drug metabolism, absorption, efficacy, and even safety. Consequently, considering variations in the composition of individual gut microbiota during drug development may prove invaluable for personalized medicine. In the future, this approach could facilitate the creation of more precise drug treatment regimens that target the interaction mechanisms between specific drugs and gut microbes.
7 Conclusion
The gut microbiota is a crucial component of the intestinal microbiome and serves as a significant modulator of immune responses and cognitive functions. This review aims to synthesize the latest findings by examining the interactions between gut microbes and the host immune system, as well as their impact on cognitive impairment. The gut microbiota profoundly influences mucosal immunity and is essential for the development of immune tolerance and inflammation. Previous studies suggest the potential of microbiota-modulating therapies in shaping the immune response; however, the precise mechanisms by which microbial signaling translates into immune cell function require further investigation. Future research could provide therapeutic insights by elucidating the molecular pathways involved through genomics and proteomics techniques.
The role of short-chain fatty acids (SCFAs) in immunomodulation warrants further investigation, particularly regarding their interactions with other microbial metabolites, which remain unclear. SCFAs, such as butyric acid, are recognized for their contributions to anti-inflammatory effects. A deeper understanding of these metabolic interactions is crucial for the development of novel immunotherapies. The relationship between gut microbiota and cognitive disorders, often referred to as the gut-brain axis, is increasingly gaining attention. Metabolites like SCFAs are believed to influence brain function and behavior; however, the neural circuits and signaling molecules mediating these effects are not yet fully understood. Studies that integrate neuroimaging with microbiome analyses could provide valuable insights into how microbiological factors affect brain activity and cognitive performance. In the realm of neurodegenerative diseases, the notion of microbiota-induced inflammation as a contributing factor is receiving growing recognition. Nonetheless, the temporal relationship between microbial imbalances and neurodegenerative processes is complex and varies among individuals. Longitudinal studies that track changes in gut microbiota alongside neurological assessments may elucidate the temporal dynamics between microbial imbalances and neurodegenerative processes.
Gut microbiota therapy holds significant promise; however, challenges remain. The heterogeneity of individual responses to probiotics and other microbiota interventions suggests that a one-size-fits-all approach may not be effective. Personalized strategies that consider an individual’s unique microbiome profile, genetic background, and lifestyle factors are crucial for the success of these therapies. Furthermore, the influence of gut microbiota on drug metabolism introduces a new dimension to drug therapy, as variations in an individual’s response to the same medication may partially stem from differences in their gut microbiota. This necessitates a reassessment of how clinical trials and personalized treatment plans are designed. Additionally, environmental factors, including diet and exposure to pollutants, play a significant role in shaping the gut microbiota, and further investigation into how these factors can be manipulated to improve health outcomes is warranted.
Future research must investigate the molecular mechanisms by which the gut microbiota influences cognitive function through the gut-brain axis, focusing on specific microbial species, metabolites, and signaling pathways. Longitudinal studies are crucial to elucidate the causal relationship between alterations in the gut microbiota and cognitive function. Additionally, large-scale, randomized controlled clinical trials are necessary to enhance the efficacy and safety of interventions for cognitive dysfunction and to assess the modulation of the gut microbiota. Given the heterogeneity of gut microbiota among individuals, future studies should consider personalized therapeutic strategies tailored to individual gut microbiota profiles. Furthermore, it is vital to explore how the gut microbiota impacts drug metabolism and efficacy to inform personalized drug therapy. The development of new preventive and therapeutic strategies should also examine the influence of lifestyle factors—such as diet, exercise, and sleep—as well as environmental factors on the gut microbiota, and how these elements affect cognitive function through the gut-brain axis.
In summary, the role of the gut microbiota in immunomodulation and cognitive function represents a complex and dynamic field with significant potential for enhancing human health. This review explores the mechanisms through which the gut microbiota contributes to cognitive dysfunction via the immune system, while also addressing the limitations of the study and suggesting directions for future research. It is essential for upcoming research to integrate insights from diverse disciplines, including immunology, neurology, psychology, and nutrition, to fully leverage the potential of the gut microbiota in healthcare through a multidisciplinary approach. By deepening our understanding of the interactions between the gut microbiota and cognitive dysfunction, we anticipate the development of novel prevention and treatment strategies to tackle global public health challenges.
Author contributions
RZ: Writing – original draft, Writing – review & editing. ND: Investigation, Writing – original draft. XF: Investigation, Writing – original draft. WL: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The authors gratefully acknowledge financial support from Department of Education of Hubei Province (B2022190).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Pérez Palmer N, Trejo Ortega B, Joshi P. Cognitive impairment in older adults: epidemiology, diagnosis, and treatment. Psychiatr Clin North Am. (2022) 45:639–61. doi: 10.1016/j.psc.2022.07.010
2. Liu E, Zhang Y, Wang JZ. Updates in Alzheimer's disease: from basic research to diagnosis and therapies. Transl Neurodegener. (2024) 13:45. doi: 10.1186/s40035-024-00432-x
3. Casagrande M, Forte G, Favieri F, Corbo I. Sleep quality and aging: A systematic review on healthy older people, mild cognitive impairment and alzheimer's disease. Int J Environ Res Public Health. (2022) 19:8457. doi: 10.3390/ijerph19148457
4. Liang Y, Gao Y, Wang R, Grande G, Monastero R, Dong Y, et al. Migraine, cognitive decline, and dementia in older adults: A population-based study. J Alzheimers Dis. (2022) 88:263–71. doi: 10.3233/jad-220013
5. Jia L, Du Y, Chu L, Zhang Z, Li F, Lyu D, et al. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: a cross-sectional study. Lancet Public Health. (2020) 5:e661–71. doi: 10.1016/s2468-2667(20)30185-7
6. Huang Y, Li X, Liu Z, Huo J, Guo J, Chen Y, et al. Projections of the economic burden of care for individuals with dementia in mainland China from 2010 to 2050. PloS One. (2022) 17::e0263077. doi: 10.1371/journal.pone.0263077
7. Kelley AS, Mcgarry K, Bollens-Lund E, Rahman OK, Husain M, Ferreira KB, et al. Residential setting and the cumulative financial burden of dementia in the 7 Years before death. J Am Geriatr Soc. (2020) 68:1319–24. doi: 10.1111/jgs.16414
8. Inaba R, Vujakovic S, Bergstrom K. The gut mucus network: A dynamic liaison between microbes and the immune system. Semin Immunol. (2023) 69:101807. doi: 10.1016/j.smim.2023.101807
9. Jacobson A, Yang D, Vella M, Chiu IM. The intestinal neuro-immune axis: crosstalk between neurons, immune cells, and microbes. Mucosal Immunol. (2021) 14:555–65. doi: 10.1038/s41385-020-00368-1
10. Hosseinkhani F, Heinken A, Thiele I, Lindenburg PW, Harms AC, Hankemeier T. The contribution of gut bacterial metabolites in the human immune signaling pathway of non-communicable diseases. Gut Microbes. (2021) 13:1–22. doi: 10.1080/19490976.2021.1882927
11. Fung TC, Olson CA, Hsiao EY. Interactions between the microbiota, immune and nervous systems in health and disease. Nat Neurosci. (2017) 20:145–55. doi: 10.1038/nn.4476
12. Duess JW, Sampah ME, Lopez CM, Tsuboi K, Scheese DJ, Sodhi CP, et al. Necrotizing enterocolitis, gut microbes, and sepsis. Gut Microbes. (2023) 15:2221470. doi: 10.1080/19490976.2023.2221470
13. González Olmo BM, Butler MJ, Barrientos RM. Evolution of the human diet and its impact on gut microbiota, immune responses, and brain health. Nutrients. (2021) 13. doi: 10.3390/nu13010196
14. Stoeva MK, Garcia-So J, Justice N, Myers J, Tyagi S, Nemchek M, et al. Butyrate-producing human gut symbiont, Clostridium butyricum, and its role in health and disease. Gut Microbes. (2021) 13:1–28. doi: 10.1080/19490976.2021.1907272
15. Shao T, Hsu R, Rafizadeh DL, Wang L, Bowlus CL, Kumar N, et al. The gut ecosystem and immune tolerance. J Autoimmun. (2023) 141:103114. doi: 10.1016/j.jaut.2023.103114
16. Campbell C, Kandalgaonkar MR, Golonka RM, Yeoh BS, Vijay-Kumar M, Saha P. Crosstalk between gut microbiota and host immunity: impact on inflammation and immunotherapy. Biomedicines. (2023) 11(2):294. doi: 10.3390/biomedicines11020294
17. Geuking MB, Köller Y, Rupp S, Mccoy KD. The interplay between the gut microbiota and the immune system. Gut Microbes. (2014) 5:411–8. doi: 10.4161/gmic.29330
18. Barrio C, Arias-Sánchez S, Martín-Monzón I. The gut microbiota-brain axis, psychobiotics and its influence on brain and behaviour: A systematic review. Psychoneuroendocrinology. (2022) 137:105640. doi: 10.1016/j.psyneuen.2021.105640
19. Karakan T, Ozkul C, Küpeli Akkol E, Bilici S, Sobarzo-Sánchez E, Capasso R. Gut-brain-microbiota axis: antibiotics and functional gastrointestinal disorders. Nutrients. (2021) 13(2):389. doi: 10.3390/nu13020389
20. Naufel MF, Truzzi GM, Ferreira CM, Coelho FMS. The brain-gut-microbiota axis in the treatment of neurologic and psychiatric disorders. Arq Neuropsiquiatr. (2023) 81:670–84. doi: 10.1055/s-0043-1767818
21. Ding M, Lang Y, Shu H, Shao J, Cui L. Microbiota-gut-brain axis and epilepsy: A review on mechanisms and potential therapeutics. Front Immunol. (2021) 12:742449. doi: 10.3389/fimmu.2021.742449
22. Petra AI, Panagiotidou S, Hatziagelaki E, Stewart JM, Conti P, Theoharides TC. Gut-microbiota-brain axis and its effect on neuropsychiatric disorders with suspected immune dysregulation. Clin Ther. (2015) 37:984–95. doi: 10.1016/j.clinthera.2015.04.002
23. Dos Santos A, Galiè S. The microbiota-gut-brain axis in metabolic syndrome and sleep disorders: A systematic review. Nutrients. (2024) 16(3):390. doi: 10.3390/nu16030390
24. Chen H, Meng L, Shen L. Multiple roles of short-chain fatty acids in Alzheimer disease. Nutrition. (2022) 93:111499. doi: 10.1016/j.nut.2021.111499
25. Fock E, Parnova R. Mechanisms of blood-brain barrier protection by microbiota-derived short-chain fatty acids. Cells. (2023) 12(4):657. doi: 10.3390/cells12040657
26. Tang CF, Wang CY, Wang JH, Wang QN, Li SJ, Wang HO, et al. Short-chain fatty acids ameliorate depressive-like behaviors of high fructose-fed mice by rescuing hippocampal neurogenesis decline and blood-brain barrier damage. Nutrients. (2022) 14(9):1882. doi: 10.3390/nu14091882
27. Nagpal R, Neth BJ, Wang S, Craft S, Yadav H. Modified Mediterranean-ketogenic diet modulates gut microbiome and short-chain fatty acids in association with Alzheimer's disease markers in subjects with mild cognitive impairment. EBioMedicine. (2019) 47:529–42. doi: 10.1016/j.ebiom.2019.08.032
28. Huang Y, Wang YF, Miao J, Zheng RF, Li JY. Short-chain fatty acids: Important components of the gut-brain axis against AD. BioMed Pharmacother. (2024) 175:116601. doi: 10.1016/j.biopha.2024.116601
29. Li JM, Yu R, Zhang LP, Wen SY, Wang SJ, Zhang XY, et al. Dietary fructose-induced gut dysbiosis promotes mouse hippocampal neuroinflammation: a benefit of short-chain fatty acids. Microbiome. (2019) 7:98. doi: 10.1186/s40168-019-0713-7
30. Allaire JM, Crowley SM, Law HT, Chang SY, Ko HJ, Vallance BA. The intestinal epithelium: central coordinator of mucosal immunity. Trends Immunol. (2018) 39:677–96. doi: 10.1016/j.it.2018.04.002
31. Zhou B, Yuan Y, Zhang S, Guo C, Li X, Li G, et al. Intestinal flora and disease mutually shape the regional immune system in the intestinal tract. Front Immunol. (2020) 11:575. doi: 10.3389/fimmu.2020.00575
32. Wang X, Yuan W, Yang C, Wang Z, Zhang J, Xu D, et al. Emerging role of gut microbiota in autoimmune diseases. Front Immunol. (2024) 15:1365554. doi: 10.3389/fimmu.2024.1365554
33. Pardo-Camacho C, González-Castro AM, Rodiño-Janeiro BK, Pigrau M, Vicario M. Epithelial immunity: priming defensive responses in the intestinal mucosa. Am J Physiol Gastrointest Liver Physiol. (2018) 314:G247–g255. doi: 10.1152/ajpgi.00215.2016
34. Amoroso C, Perillo F, Strati F, Fantini MC, Caprioli F, Facciotti F. The role of gut microbiota biomodulators on mucosal immunity and intestinal inflammation. Cells. (2020) 9(5):1234. doi: 10.3390/cells9051234
35. Lehmann FM, Von Burg N, Ivanek R, Teufel C, Horvath E, Peter A, et al. Microbiota-induced tissue signals regulate ILC3-mediated antigen presentation. Nat Commun. (2020) 11:1794. doi: 10.1038/s41467-020-15612-2
36. Dery KJ, Kadono K, Hirao H, Górski A, Kupiec-Weglinski JW. Microbiota in organ transplantation: An immunological and therapeutic conundrum? Cell Immunol. (2020) 351:104080. doi: 10.1016/j.cellimm.2020.104080
37. Dowdell P, Chankhamhaengdecha S, Panbangred W, Janvilisri T, Aroonnual A. Probiotic Activity of Enterococcus faecium and Lactococcus lactis Isolated from Thai Fermented Sausages and Their Protective Effect Against Clostridium difficile. Probiotics Antimicrob Proteins. (2020) 12:641–8. doi: 10.1007/s12602-019-09536-7
38. Chiang JYL, Ferrell JM. Targeting the gut microbiota for treating colitis: Is FGF19 a magic bullet? EBioMedicine. (2020) 55:102754. doi: 10.1016/j.ebiom.2020.102754
39. Halsey T, Ologun G, Wargo J, Jenq RR. Uncovering the role of the gut microbiota in immune checkpoint blockade therapy: A mini-review. Semin Hematol. (2020) 57:13–8. doi: 10.1053/j.seminhematol.2020.05.002
40. Inamura K. Roles of microbiota in response to cancer immunotherapy. Semin Cancer Biol. (2020) 65:164–75. doi: 10.1016/j.semcancer.2019.12.026
41. Zhang X, Irajizad E, Hoffman KL, Fahrmann JF, Li F, Seo YD, et al. Modulating a prebiotic food source influences inflammation and immune-regulating gut microbes and metabolites: insights from the BE GONE trial. EBioMedicine. (2023) 98:104873. doi: 10.1016/j.ebiom.2023.104873
42. Wang Y, Ma L, He J, Gu H, Zhu H. Identification of cancer stem cell-related genes through single cells and machine learning for predicting prostate cancer prognosis and immunotherapy. Front Immunol. (2024) 15:1464698. doi: 10.3389/fimmu.2024.1464698
43. Ma L, Ni Y, Wang Z, Tu W, Ni L, Zhuge F, et al. Spermidine improves gut barrier integrity and gut microbiota function in diet-induced obese mice. Gut Microbes. (2020) 12:1–19. doi: 10.1080/19490976.2020.1832857
44. Morrison DJ, Preston T. Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism. Gut Microbes. (2016) 7:189–200. doi: 10.1080/19490976.2015.1134082
45. Castellanos JG, Longman RS. Innate lymphoid cells link gut microbes with mucosal T cell immunity. Gut Microbes. (2020) 11:231–6. doi: 10.1080/19490976.2019.1638725
46. Li G, Lin J, Zhang C, Gao H, Lu H, Gao X, et al. Microbiota metabolite butyrate constrains neutrophil functions and ameliorates mucosal inflammation in inflammatory bowel disease. Gut Microbes. (2021) 13:1968257. doi: 10.1080/19490976.2021.1968257
47. Fritsch J, Garces L, Quintero MA, Pignac-Kobinger J, Santander AM, Fernández I, et al. Low-fat, high-fiber diet reduces markers of inflammation and dysbiosis and improves quality of life in patients with ulcerative colitis. Clin Gastroenterol Hepatol. (2021) 19:1189–1199.e30. doi: 10.1016/j.cgh.2020.05.026
48. Chen G, Ran X, Li B, Li Y, He D, Huang B, et al. Sodium butyrate inhibits inflammation and maintains epithelium barrier integrity in a TNBS-induced inflammatory bowel disease mice model. EBioMedicine. (2018) 30:317–25. doi: 10.1016/j.ebiom.2018.03.030
49. Luu M, Riester Z, Baldrich A, Reichardt N, Yuille S, Busetti A, et al. Microbial short-chain fatty acids modulate CD8(+) T cell responses and improve adoptive immunotherapy for cancer. Nat Commun. (2021) 12:4077. doi: 10.1038/s41467-021-24331-1
50. Mann ER, Lam YK, Uhlig HH. Short-chain fatty acids: linking diet, the microbiome and immunity. Nat Rev Immunol. (2024) 24:577–95. doi: 10.1038/s41577-024-01014-8
51. Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly YM, et al. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science. (2013) 341:569–73. doi: 10.1126/science.1241165
52. Wang Y, Wang J, Liu Y, Wang X, Ren M. Multidimensional pan-cancer analysis of HSPA5 and its validation in the prognostic value of bladder cancer. Heliyon. (2024) 10:e27184. doi: 10.1016/j.heliyon.2024.e27184
53. Wang Y, He J, Zhao Q, Bo J, Zhou Y, Sun H, et al. Evaluating the predictive value of angiogenesis-related genes for prognosis and immunotherapy response in prostate adenocarcinoma using machine learning and experimental approaches. Front Immunol. (2024) 15:1416914. doi: 10.3389/fimmu.2024.1416914
54. Pang ZQ, Wang JS, Wang JF, Wang YX, Ji B, Xu YD, et al. JAM3: A prognostic biomarker for bladder cancer via epithelial-mesenchymal transition regulation. Biomol BioMed. (2024) 24:897–911. doi: 10.17305/bb.2024.9979
55. Wang G, Si Q, Yang S, Jiao T, Zhu H, Tian P, et al. Lactic acid bacteria reduce diabetes symptoms in mice by alleviating gut microbiota dysbiosis and inflammation in different manners. Food Funct. (2020) 11:5898–914. doi: 10.1039/c9fo02761k
56. Cai J, Sun L, Gonzalez FJ. Gut microbiota-derived bile acids in intestinal immunity, inflammation, and tumorigenesis. Cell Host Microbe. (2022) 30:289–300. doi: 10.1016/j.chom.2022.02.004
57. Perna A, Hay E, Contieri M, De Luca A, Guerra G, Lucariello A. Adherent-invasive Escherichia coli (AIEC): Cause or consequence of inflammation, dysbiosis, and rupture of cellular joints in patients with IBD? J Cell Physiol. (2020) 235:5041–9. doi: 10.1002/jcp.29430
58. Malesza IJ, Malesza M, Walkowiak J, Mussin N, Walkowiak D, Aringazina R, et al. High-fat, western-style diet, systemic inflammation, and gut microbiota: A narrative review. Cells. (2021) 10(11):3164. doi: 10.3390/cells10113164
59. Albuquerque A, Garrido N, Charneca R, Egas C, Martin L, Ramos A, et al. Influence of sex and a high-fiber diet on the gut microbiome of alentejano pigs raised to heavy weights. Vet Sci. (2023) 10(11):641. doi: 10.3390/vetsci10110641
60. Jiang T, Wu H, Yang X, Li Y, Zhang Z, Chen F, et al. Lactobacillus mucosae strain promoted by a high-fiber diet in genetic obese child alleviates lipid metabolism and modifies gut microbiota in apoE(-/-) mice on a western diet. Microorganisms. (2020) 8(8):1225. doi: 10.3390/microorganisms8081225
61. Barbian ME, Owens JA, Naudin CR, Denning P, Patel RM, Jones RM. A high fiber diet or supplementation with Lactococcus lactis subspecies cremoris to pregnant mice confers protection against intestinal injury in adult offspring. Gut Microbes. (2024) 16:2337317. doi: 10.1080/19490976.2024.2337317
62. Holscher. Dietary fiber HD. and prebiotics and the gastrointestinal microbiota. Gut Microbes. (2017) 8:172–84. doi: 10.1080/19490976.2017.1290756
63. Clemente-Suárez VJ, Beltrán-Velasco AI, Redondo-Flórez L, Martín-Rodríguez A, Tornero-Aguilera JF. Global impacts of western diet and its effects on metabolism and health: A narrative review. Nutrients. (2023) 15(12):2749. doi: 10.3390/nu15122749
64. Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K, et al. Influence of diet on the gut microbiome and implications for human health. J Transl Med. (2017) 15:73. doi: 10.1186/s12967-017-1175-y
65. Liu H, Wang J, He T, Becker S, Zhang G, Li D, et al. Butyrate: A double-edged sword for health? Adv Nutr. (2018) 9:21–9. doi: 10.1093/advances/nmx009
66. Makki K, Deehan EC, Walter J, Bäckhed F. The impact of dietary fiber on gut microbiota in host health and disease. Cell Host Microbe. (2018) 23:705–15. doi: 10.1016/j.chom.2018.05.012
67. Sittipo P, Lobionda S, Lee YK, Maynard CL. Intestinal microbiota and the immune system in metabolic diseases. J Microbiol. (2018) 56:154–62. doi: 10.1007/s12275-018-7548-y
68. Frazier K, Kambal A, Zale EA, Pierre JF, Hubert N, Miyoshi S, et al. High-fat diet disrupts REG3γ and gut microbial rhythms promoting metabolic dysfunction. Cell Host Microbe. (2022) 30:809–823.e6. doi: 10.1016/j.chom.2022.03.030
69. Tong Y, Gao H, Qi Q, Liu X, Li J, Gao J, et al. High fat diet, gut microbiome and gastrointestinal cancer. Theranostics. (2021) 11:5889–910. doi: 10.7150/thno.56157
70. Yan J, Zeng Y, Guan Z, Li Z, Luo S, Niu J, et al. Inherent preference for polyunsaturated fatty acids instigates ferroptosis of Treg cells that aggravates high-fat-diet-related colitis. Cell Rep. (2024) 43:114636. doi: 10.1016/j.celrep.2024.114636
71. Ma Y, Xie H, Xu N, Li M, Wang L, Ge H, et al. Large yellow tea polysaccharide alleviates HFD-induced intestinal homeostasis dysbiosis via modulating gut barrier integrity, immune responses, and the gut microbiome. J Agric Food Chem. (2024) 72:7230–43. doi: 10.1021/acs.jafc.4c00616
72. Zeng L, Deng Y, He Q, Yang K, Li J, Xiang W, et al. Safety and efficacy of probiotic supplementation in 8 types of inflammatory arthritis: A systematic review and meta-analysis of 34 randomized controlled trials. Front Immunol. (2022) 13:961325. doi: 10.3389/fimmu.2022.961325
73. Kesika P, Suganthy N, Sivamaruthi BS, Chaiyasut C. Role of gut-brain axis, gut microbial composition, and probiotic intervention in Alzheimer's disease. Life Sci. (2021) 264:118627. doi: 10.1016/j.lfs.2020.118627
74. Loh JS, Mak WQ, Tan LKS, Ng CX, Chan HH, Yeow SH, et al. Microbiota-gut-brain axis and its therapeutic applications in neurodegenerative diseases. Signal Transduct Target Ther. (2024) 9:37. doi: 10.1038/s41392-024-01743-1
75. Appleton J. The gut-brain axis: influence of microbiota on mood and mental health. Integr Med (Encinitas). (2018) 17:28–32.
76. Kearns.Gut-Brain Axis R. and neuroinflammation: the role of gut permeability and the kynurenine pathway in neurological disorders. Cell Mol Neurobiol. (2024) 44:64. doi: 10.1007/s10571-024-01496-z
77. Liu L, Huh JR, Shah K. Microbiota and the gut-brain-axis: Implications for new therapeutic design in the CNS. EBioMedicine. (2022) 77:103908. doi: 10.1016/j.ebiom.2022.103908
78. Chen C, Liao J, Xia Y, Liu X, Jones R, Haran J, et al. Gut microbiota regulate Alzheimer's disease pathologies and cognitive disorders via PUFA-associated neuroinflammation. Gut. (2022) 71:2233–52. doi: 10.1136/gutjnl-2021-326269
79. Liu YJ, Tang B, Wang FC, Tang L, Lei YY, Luo Y, et al. Parthenolide ameliorates colon inflammation through regulating Treg/Th17 balance in a gut microbiota-dependent manner. Theranostics. (2020) 10:5225–41. doi: 10.7150/thno.43716
80. Yao ZY, Li XH, Zuo L, Xiong Q, He WT, Li DX, et al. Maternal sleep deprivation induces gut microbial dysbiosis and neuroinflammation in offspring rats. Zool Res. (2022) 43:380–90. doi: 10.24272/j.issn.2095-8137.2022.023
81. Chen Y, Xu J, Chen Y. Regulation of neurotransmitters by the gut microbiota and effects on cognition in neurological disorders. Nutrients. (2021) 13(6):2099. doi: 10.3390/nu13062099
82. Vogt NM, Kerby RL, Dill-Mcfarland KA, Harding SJ, Merluzzi AP, Johnson SC, et al. Gut microbiome alterations in Alzheimer's disease. Sci Rep. (2017) 7:13537. doi: 10.1038/s41598-017-13601-y
83. Cussotto S, Sandhu KV, Dinan TG, Cryan JF. The neuroendocrinology of the microbiota-gut-brain axis: A behavioural perspective. Front Neuroendocrinol. (2018) 51:80–101. doi: 10.1016/j.yfrne.2018.04.002
84. Stranahan AM. Visceral adiposity, inflammation, and hippocampal function in obesity. Neuropharmacology. (2022) 205:108920. doi: 10.1016/j.neuropharm.2021.108920
85. Wastyk HC, Fragiadakis GK, Perelman D, Dahan D, Merrill BD, Yu FB, et al. Gut-microbiota-targeted diets modulate human immune status. Cell. (2021) 184:4137–4153.e14. doi: 10.1016/j.cell.2021.06.019
86. Dalile B, Van Oudenhove L, Vervliet B, Verbeke K. The role of short-chain fatty acids in microbiota-gut-brain communication. Nat Rev Gastroenterol Hepatol. (2019) 16:461–78. doi: 10.1038/s41575-019-0157-3
87. Fernando W, Martins IJ, Morici M, Bharadwaj P, Rainey-Smith SR, Lim WLF, et al. Sodium butyrate reduces brain amyloid-β Levels and improves cognitive memory performance in an alzheimer's disease transgenic mouse model at an early disease stage. J Alzheimers Dis. (2020) 74:91–9. doi: 10.3233/jad-190120
88. Marchesi JR, Adams DH, Fava F, Hermes GD, Hirschfield GM, Hold G, et al. The gut microbiota and host health: a new clinical frontier. Gut. (2016) 65:330–9. doi: 10.1136/gutjnl-2015-309990
89. Zheng D, Liwinski T, Elinav E. Interaction between microbiota and immunity in health and disease. Cell Res. (2020) 30:492–506. doi: 10.1038/s41422-020-0332-7
90. Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. (2015) 28:203–9.
91. Zhao Z, Ning J, Bao XQ, Shang M, Ma J, Li G, et al. Fecal microbiota transplantation protects rotenone-induced Parkinson's disease mice via suppressing inflammation mediated by the lipopolysaccharide-TLR4 signaling pathway through the microbiota-gut-brain axis. Microbiome. (2021) 9:226. doi: 10.1186/s40168-021-01107-9
92. Madore C, Yin Z, Leibowitz J, Butovsky O. Microglia, lifestyle stress, and neurodegeneration. Immunity. (2020) 52:222–40. doi: 10.1016/j.immuni.2019.12.003
93. Garofalo M, Pandini C, Bordoni M, Pansarasa O, Rey F, Costa A, et al. Alzheimer's, parkinson's disease and amyotrophic lateral sclerosis gene expression patterns divergence reveals different grade of RNA metabolism involvement. Int J Mol Sci. (2020) 21(24):9500. doi: 10.3390/ijms21249500
94. Mincic AM, Antal M, Filip L, Miere D. Modulation of gut microbiome in the treatment of neurodegenerative diseases: A systematic review. Clin Nutr. (2024) 43:1832–49. doi: 10.1016/j.clnu.2024.05.036
95. Chin VK, Yong VC, Chong PP, Amin Nordin S, Basir R, Abdullah M. Mycobiome in the gut: A multiperspective review. Mediators Inflamm. (2020) 2020:9560684. doi: 10.1155/2020/9560684
96. Romano S, Savva GM, Bedarf JR, Charles IG, Hildebrand F, Narbad A. Meta-analysis of the Parkinson's disease gut microbiome suggests alterations linked to intestinal inflammation. NPJ Parkinsons Dis. (2021) 7:27. doi: 10.1038/s41531-021-00156-z
97. Wallen ZD, Demirkan A, Twa G, Cohen G, Dean MN, Standaert DG, et al. Metagenomics of Parkinson's disease implicates the gut microbiome in multiple disease mechanisms. Nat Commun. (2022) 13:6958. doi: 10.1038/s41467-022-34667-x
98. Seo DO, Holtzman DM. Current understanding of the Alzheimer's disease-associated microbiome and therapeutic strategies. Exp Mol Med. (2024) 56:86–94. doi: 10.1038/s12276-023-01146-2
99. Cryan JF, O'riordan KJ, Sandhu K, Peterson V, Dinan TG. The gut microbiome in neurological disorders. Lancet Neurol. (2020) 19:179–94. doi: 10.1016/s1474-4422(19)30356-4
100. Wright ML, Fournier C, Houser MC, Tansey M, Glass J, Hertzberg VS. Potential role of the gut microbiome in ALS: A systematic review. Biol Res Nurs. (2018) 20:513–21. doi: 10.1177/1099800418784202
101. Roseborough AD, Zhu Y, Zhao L, Laviolette SR, Pasternak SH, Whitehead SN. Fibrinogen primes the microglial NLRP3 inflammasome and propagates pro-inflammatory signaling via extracellular vesicles: Implications for blood-brain barrier dysfunction. Neurobiol Dis. (2023) 177:106001. doi: 10.1016/j.nbd.2023.106001
102. Popescu C, Munteanu C, Anghelescu A, Ciobanu V, Spînu A, Andone I, et al. Novelties on neuroinflammation in alzheimer's disease-focus on gut and oral microbiota involvement. Int J Mol Sci. (2024) 25(20):11272. doi: 10.3390/ijms252011272
103. He Z, Ma Y, Yang S, Zhang S, Liu S, Xiao J, et al. Gut microbiota-derived ursodeoxycholic acid from neonatal dairy calves improves intestinal homeostasis and colitis to attenuate extended-spectrum β-lactamase-producing enteroaggregative Escherichia coli infection. Microbiome. (2022) 10:79. doi: 10.1186/s40168-022-01269-0
104. Wang Y, Zhu H, Zhang L, He J, Bo J, Wang J, et al. Common immunological and prognostic features of lung and bladder cancer via smoking-related genes: PRR11 gene as potential immunotherapeutic target. J Cell Mol Med. (2024) 28:e18384. doi: 10.1111/jcmm.18384
105. Wang Y, Wang J, He J, Ji B, Pang Z, Wang J, et al. Comprehensive analysis of PRPF19 immune infiltrates, DNA methylation, senescence-associated secretory phenotype and ceRNA network in bladder cancer. Front Immunol. (2023) 14:1289198. doi: 10.3389/fimmu.2023.1289198
106. Bolte LA, Vich Vila A, Imhann F, Collij V, Gacesa R, Peters V, et al. Long-term dietary patterns are associated with pro-inflammatory and anti-inflammatory features of the gut microbiome. Gut. (2021) 70:1287–98. doi: 10.1136/gutjnl-2020-322670
107. Bodén S, Zheng R, Ribbenstedt A, Landberg R, Harlid S, Vidman L, et al. Dietary patterns, untargeted metabolite profiles and their association with colorectal cancer risk. Sci Rep. (2024) 14:2244. doi: 10.1038/s41598-023-50567-6
108. Gacesa R, Kurilshikov A, Vich Vila A, Sinha T, Klaassen MAY, Bolte LA, et al. Environmental factors shaping the gut microbiome in a Dutch population. Nature. (2022) 604:732–9. doi: 10.1038/s41586-022-04567-7
109. Ooi DS, Tan CP, Tay MJ, Ong SG, Tham EH, Siah KTH, et al. Developmental Origins of Health and Disease: Impact of environmental dust exposure in modulating microbiome and its association with non-communicable diseases. J Dev Orig Health Dis. (2020) 11:545–56. doi: 10.1017/s2040174420000549
110. Milani C, Duranti S, Bottacini F, Casey E, Turroni F, Mahony J, et al. The first microbial colonizers of the human gut: composition, activities, and health implications of the infant gut microbiota. Microbiol Mol Biol Rev. (2017) 81(4):e00036-17. doi: 10.1128/mmbr.00036-17
111. Walsh J, Griffin BT, Clarke G, Hyland NP. Drug-gut microbiota interactions: implications for neuropharmacology. Br J Pharmacol. (2018) 175:4415–29. doi: 10.1111/bph.14366
112. Malfatti MA, Kuhn EA, Murugesh DK, Mendez ME, Hum N, Thissen JB, et al. Manipulation of the gut microbiome alters acetaminophen biodisposition in mice. Sci Rep. (2020) 10:4571. doi: 10.1038/s41598-020-60982-8
113. Gurry T, Nguyen LTT, Yu X, Alm EJ. Functional heterogeneity in the fermentation capabilities of the healthy human gut microbiota. PloS One. (2021) 16:e0254004. doi: 10.1371/journal.pone.0254004
Keywords: gut microbiota, immune modulation, cognitive dysfunction, gut-brain axis, short-chain fatty acids
Citation: Zhang R, Ding N, Feng X and Liao W (2025) The gut microbiome, immune modulation, and cognitive decline: insights on the gut-brain axis. Front. Immunol. 16:1529958. doi: 10.3389/fimmu.2025.1529958
Received: 20 November 2024; Accepted: 07 January 2025;
Published: 22 January 2025.
Edited by:
Fraser D. Russell, University of the Sunshine Coast, AustraliaReviewed by:
YaXuan Wang, First Affiliated Hospital of Harbin Medical University, ChinaJibin Liu, Nantong Tumor Hospital, China
Copyright © 2025 Zhang, Ding, Feng and Liao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xicui Feng, MzE2NDkwMjQ0NkBxcS5jb20=; Wenli Liao, bGlhb3dlbmxpQGhidXN0LmVkdS5jbg==
 Ruyi Zhang
Ruyi Zhang Ning Ding
Ning Ding Xicui Feng
Xicui Feng Wenli Liao2*
Wenli Liao2*