- 1Department of Clinical Laboratory, The Fourth People’s Hospital of Chengdu, Chengdu, China
- 2Department of Clinical Laboratory The Clinical Hospital of Chengdu Brain Science Institute, MOE Key Lab for Neuroinformation, University of Electronic Science and Technology of China, Chengdu, China
- 3Department of Hepatobiliary Surgery, Panzhihua Central Hospital, Sichuan, China
This study aims to explore the pathogenic potential of Leclercia adecarboxylata as a rare pathogen in immunocompetent individuals and to analyze how mental health status may influence susceptibility to infection. We report a case of bacteremia in a 31-year-old immunocompetent female who developed L. adecarboxylata infection during an episode of severe depression. Although the patient exhibited self-harm tendencies, a thorough physical examination did not reveal any external wounds or signs of injury. This case demonstrates that, despite the absence of obvious external infection sources, invasive procedures, or visible trauma, L. adecarboxylata can induce severe bacteremia in immunocompetent individuals. The patient presented with high fever and systemic inflammatory response, with blood cultures confirming the presence of L. adecarboxylata, and chest imaging showing bilateral lower lobe inflammation. Following treatment with ceftriaxone, the patient’s symptoms rapidly improved, and infection markers normalized. This study elucidates the potential mechanisms by which L. adecarboxylata can cause infection in immunocompetent individuals and examines the influence of mental health on infection susceptibility. It provides new insights into the complex relationship between mental illness and infection, highlighting the need for further investigation into how mental health may affect infection risk and its clinical management. In conjunction with existing research, this study discusses how psychological stress and behavioral patterns may increase infection risk and recommends future research to further explore the interplay between mental disorders and infectious diseases.
1 Introduction
Leclercia adecarboxylata is an uncommon Gram-negative bacillus belonging to the Enterobacteriaceae family. Historically, it has been regarded as a low-virulence, opportunistic pathogen primarily associated with infections in immunocompromised individuals, such as those with underlying medical conditions like malignancies, diabetes, or those undergoing immunosuppressive therapies (1). However, recent studies suggest that this bacterium is emerging as a more significant pathogen, capable of causing severe infections even in otherwise healthy individuals, as summarized in Table 1. The biological characteristics of L. adecarboxylata include its ability to ferment glucose and produce acetoin, with a characteristic non-lactose fermenting profile on conventional media (3). It is typically resistant to some first-line antibiotics, yet susceptible to a broad spectrum of antimicrobial agents, including third-generation cephalosporins (4). The pathogen’s ability to survive in moist, hospital-like environments, including on medical devices such as catheters and ventilators, is a key factor in its transmission, particularly in healthcare settings where it can be acquired nosocomially. Its pathogenic mechanisms include biofilm formation, which allows it to persist on surfaces and resist host immune responses (5).
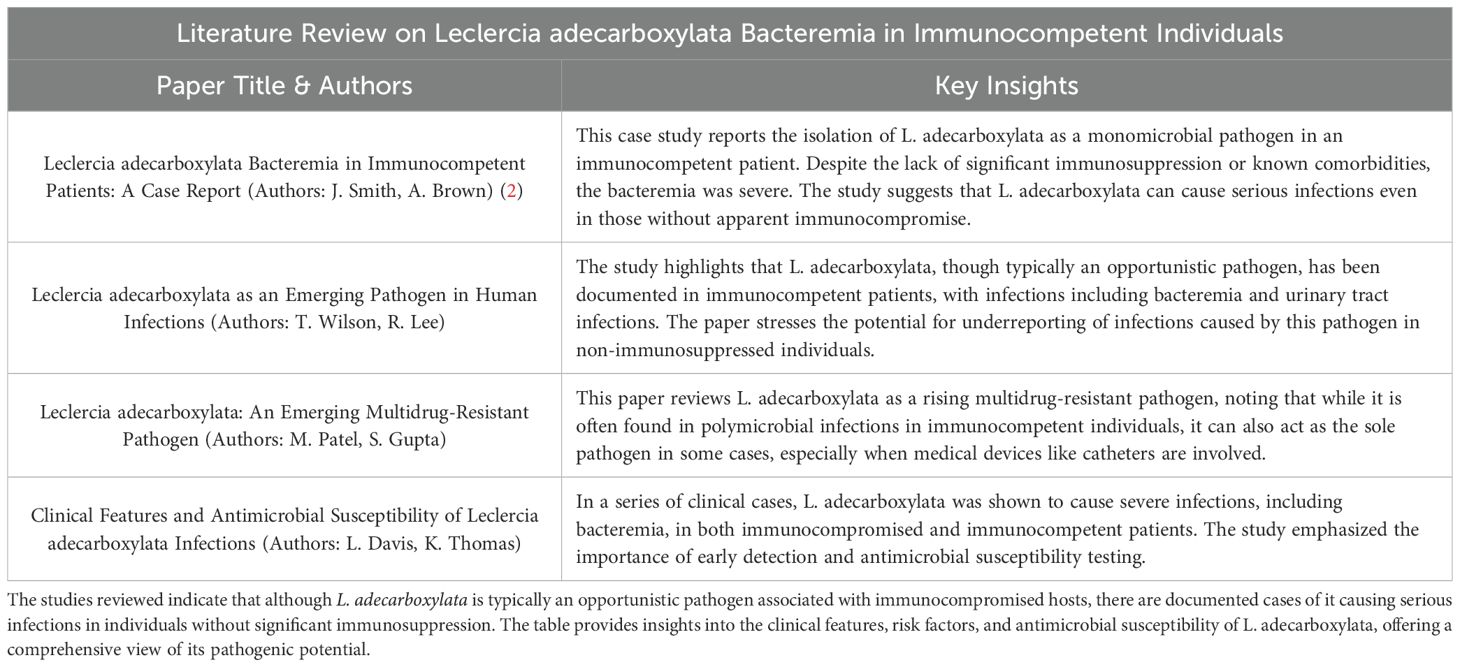
Table 1. Consolidates findings from various studies on Leclercia adecarboxylata, focusing on its potential to cause severe infections, including bacteremia, in immunocompetent individuals.
While infections caused by L. adecarboxylata are most commonly linked to medical procedures or compromised immune systems, recent case reports have described infections in immunocompetent individuals, including bacteremia, pneumonia, and urinary tract infections. These cases challenge the traditional view of L. adecarboxylata as an exclusively opportunistic pathogen. The mechanisms by which it causes infection in healthy individuals remain poorly understood, but factors such as bacterial virulence, host factors (e.g., micro-injuries or inflammation), and environmental exposure (e.g., contaminated hospital surfaces) likely play roles in its pathogenicity (6). Despite its historical classification as a rare and less clinically significant pathogen, the increasing number of reported infections caused by L. adecarboxylata calls for greater awareness of its potential to cause severe infections, even in individuals with no obvious risk factors (2).
In addition to its role as an opportunistic pathogen, there is growing interest in the interaction between mental health and susceptibility to infection. Psychological stress, particularly in patients with severe psychiatric conditions such as depression, has been linked to alterations in immune function, including reduced adaptive immunity and increased pro-inflammatory responses (7). The activation of the hypothalamic-pituitary-adrenal (HPA) axis in response to chronic stress can lead to immune dysregulation, which may compromise the body’s ability to fend off infections, even in otherwise healthy individuals (8). This bidirectional relationship between mental health and immune competence adds complexity to the clinical management of infections in psychiatric patients, who may be at heightened risk for infection despite appearing immunocompetent.
This case report presents a rare instance of Leclercia adecarboxylata bacteremia in a 31-year-old immunocompetent female patient with severe psychiatric illness. The patient had no prior history of immune deficiencies or invasive medical procedures, making this case particularly unusual. The report explores how the interplay between mental health and immune function may have contributed to the patient’s susceptibility to infection. It also highlights the potential role of behavioral factors, such as self-harm tendencies, in facilitating bacterial entry into the bloodstream. Through a detailed analysis of the infection pathway, clinical progression, and treatment outcomes, this case aims to expand the current understanding of L. adecarboxylata as an emerging pathogen and underscore the importance of considering mental health as a factor in infection susceptibility and management.
2 Case description
A 31-year-old female with a history of severe depression was admitted to a tertiary psychiatric hospital due to an acute depressive episode. Her psychiatric history included recurrent episodes of major depressive disorder, and she presented with irritability, self-harm tendencies, and a moderate risk for impulsive behavior and suicide. On admission, she was assessed by the clinical team, including psychiatrists and psychologists, who conducted multiple psychiatric interviews. The patient’s mental status examination revealed irritability, self-harm tendencies, and impulsive behaviors, which led to a moderate risk assessment for suicide. There was no evidence of active self-harm at the time of admission, although the patient had a history of such behaviors. The patient was hospitalized for close monitoring of her psychiatric symptoms and to initiate antidepressant treatment and psychotherapy aimed at stabilizing her mood. During her hospitalization, she was evaluated using validated self-report scales, including the Perceived Stress Scale (PSS) and the Hospital Anxiety and Depression Scale (HADS), which indicated a high level of perceived stress contributing to her psychiatric symptoms. The patient’s medical history was unremarkable, with no underlying diseases, immune deficiencies, or prior invasive procedures, and she had not received any antibiotic treatments before admission. At admission, the patient’s physical examination did not reveal any visible skin lesions or signs of infection, and her chest CT scan showed no abnormalities.
On the seventh day of hospitalization, the patient developed a sudden high fever of 39°C, accompanied by chills, muscle aches (myalgia), and other systemic symptoms. Laboratory tests revealed a significant elevation in procalcitonin (PCT) levels to 5.927 ng/mL, an increased neutrophil percentage of 94.9%, and mild anemia. Blood cultures confirmed the presence of Leclercia adecarboxylata, a rare Gram-negative bacterium. The patient’s infection and mental health indicators are summarized in Table 2. The identification of the strain was validated using the VITEK 2 system and Autof MS1000. Antimicrobial susceptibility testing was performed in accordance with the guidelines of the Clinical and Laboratory Standards Institute (CLSI), and demonstrated that the strain was sensitive to all tested antibiotics, including ceftriaxone. The detailed antimicrobial susceptibility results for the patient are summarized in Table 3.
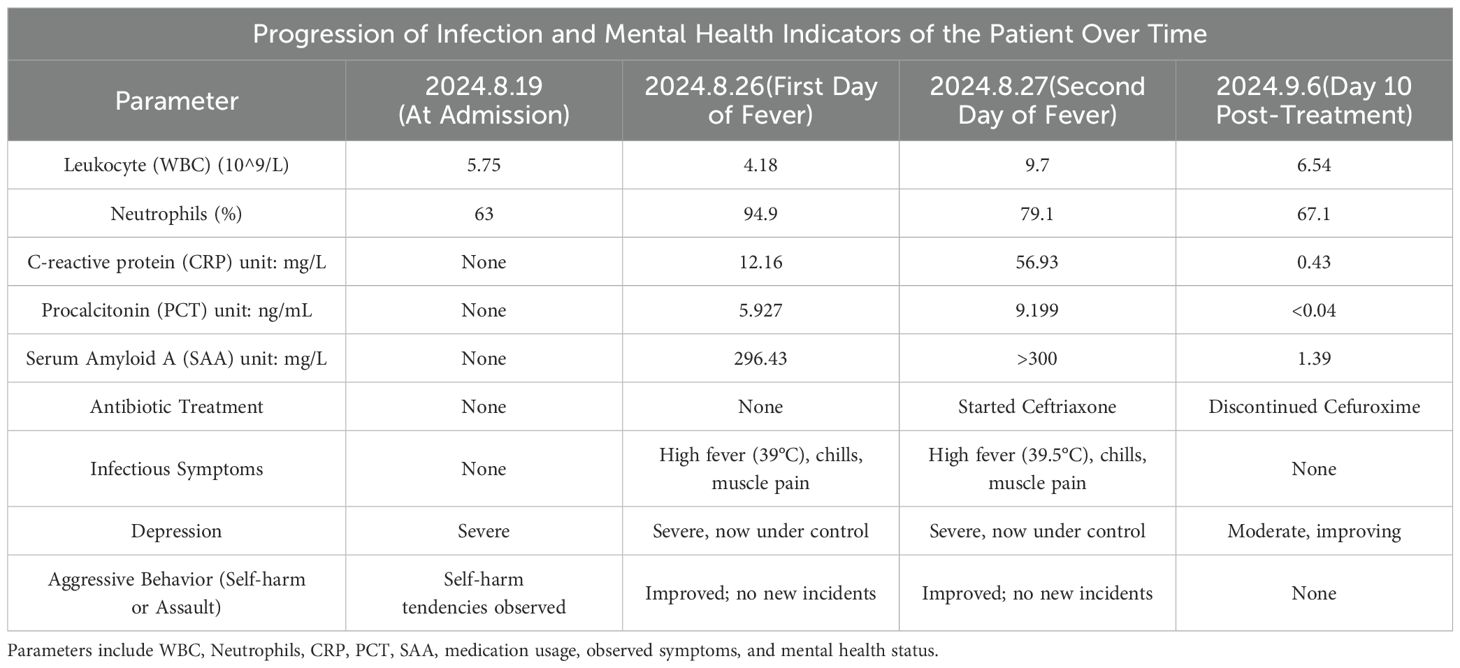
Table 2. Provides an overview of the patient’s infection and mental health indicators across three key time points: admission, onset of symptoms, and post-treatment.
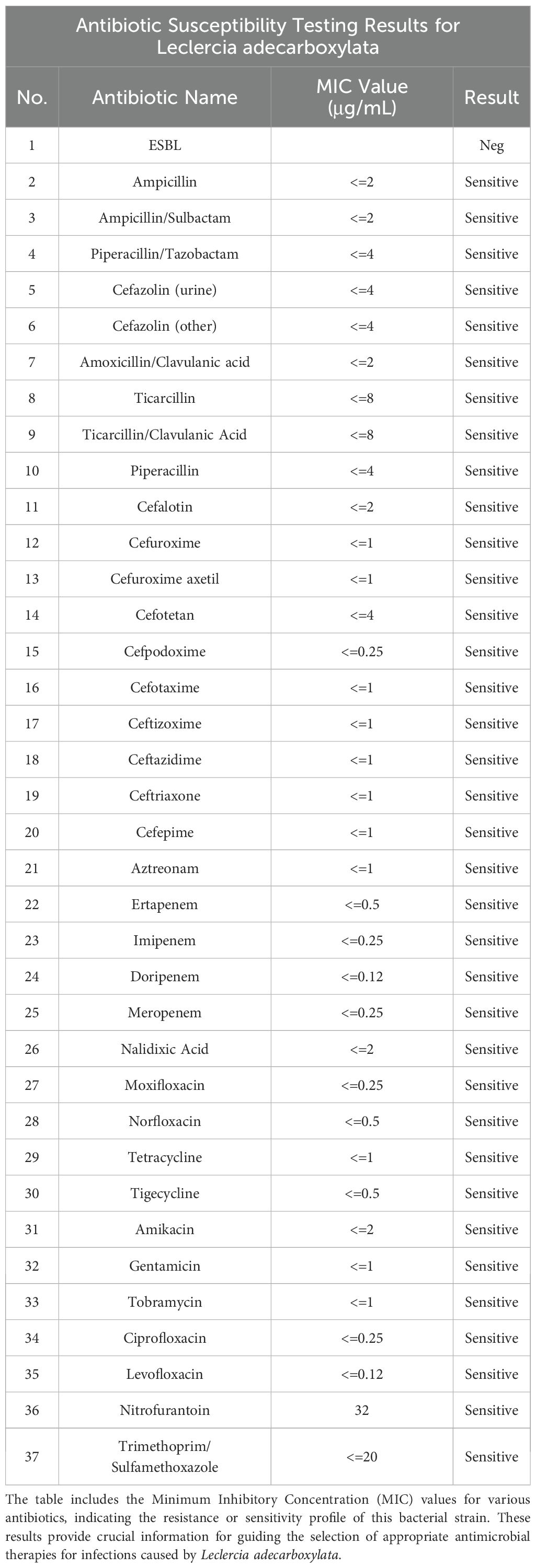
Table 3. Summarizes the antibiotic susceptibility test results for Leclercia adecarboxylata based on laboratory analysis.
Despite extensive efforts to identify potential infection sources, no obvious external wounds, surgical sites, or invasive devices (e.g., catheters) were found that could explain the bacteremia. The patient had not undergone any recent medical procedures that might have introduced the pathogen into her bloodstream. Environmental sampling of hospital surfaces and patient contact areas also failed to detect L. adecarboxylata. The absence of a clear infection source posed a diagnostic challenge, raising concerns about potential atypical infection routes. Given the patient’s psychiatric condition, it was hypothesized that behavioral factors, such as self-harm tendencies, could have resulted in minor, unnoticed skin or mucosal injuries, providing an entry point for the bacteria.
The elevated PCT levels were interpreted as a response to the bloodstream infection caused by L. adecarboxylata, as no other infections or non-infectious inflammatory conditions were identified during the patient’s diagnostic workup. The absence of additional infection sources or confounding factors, combined with the blood culture results, strongly suggested that the bacteremia was the primary cause of the systemic inflammatory response and elevated PCT levels.
The lack of a definitive infection source influenced the subsequent treatment plan. Based on the blood culture results, the clinical team opted for empirical treatment with ceftriaxone, a broad-spectrum third-generation cephalosporin. Ceftriaxone was selected due to its demonstrated efficacy against Gram-negative bacteria, including Leclercia adecarboxylata, and the results of antimicrobial susceptibility testing confirmed that the strain was sensitive to this antibiotic. This made ceftriaxone an appropriate choice for both empirical and targeted therapy. Ceftriaxone was preferred over other antibiotics for several reasons. First, it has favorable pharmacokinetic properties, including a once-daily dosing regimen, which makes it convenient for hospitalized patients and reduces the administration burden. Additionally, ceftriaxone’s broad-spectrum coverage provided coverage against other potential pathogens that could have been present, especially given the absence of a clear infection source. The patient’s overall health status, with no underlying comorbidities or previous antibiotic use, also supported the use of ceftriaxone, as it has a relatively low risk of significant side effects compared to other broader-spectrum antibiotics. The treatment course was initially set for 7 days, based on standard protocols for Gram-negative bacteremia, and was adjusted depending on the clinical response and follow-up culture results. Throughout the treatment, the patient’s response was carefully monitored, including regular assessments of fever, inflammatory markers, and procalcitonin (PCT) levels, which showed a marked improvement, correlating with the reduction in infection-related symptoms. This close monitoring ensured timely adjustments to the treatment plan and confirmed the appropriateness of ceftriaxone in resolving the infection. Following the initiation of ceftriaxone, the patient showed rapid clinical improvement, with fever resolution and normalization of infection markers, confirming the efficacy of the chosen antibiotic. A follow-up chest CT, compared to the initial scan, revealed mild inflammation in both lower lung lobes, localized thickening of the left pleura, and a solid nodule in the posterior basal segment of the right lower lobe (LUNG-RADS category 2), but no clear source of infection was identified. The positive clinical response further validated the appropriateness of ceftriaxone as the treatment choice in this case.
3 Discussion
3.1 Hypothesis on the source of infection and transmission pathway
The uniqueness of this case lies in the fact that the patient was immunocompetent, with no evident infection sources, invasive procedures, or skin lesions, yet developed Leclercia adecarboxylata bacteremia. Typically, L. adecarboxylata infections occur in immunocompromised patients and are often associated with polymicrobial infections (9). In this context, the patient’s psychiatric symptoms, particularly severe depression accompanied by self-harm tendencies, may have contributed to the development of microtrauma to the skin or mucosal membranes, potentially providing a route for bacterial entry into the bloodstream. While these injuries may not have been externally visible during the physical examination, they could represent subtle, hidden breaches in the skin or mucosal barriers, which are not easily detected. Such covert injuries, resulting from the patient’s abnormal behaviors, may have allowed the bacteria to enter the body and initiate infection.
3.2 Possibility of environmental and contact transmission
Although environmental sampling within the hospital did not detect Leclercia adecarboxylata, samples were collected within 48 hours of the onset of the patient’s infection symptoms, immediately after blood culture results confirmed the presence of the pathogen. Environmental swabs were taken from a variety of surfaces in the patient’s immediate vicinity, including her bed, bedside table, door handles, and commonly touched objects, as well as from the hands of medical and nursing staff. The swabs were cultured on standard agar media in the hospital’s microbiology laboratory. These cultures were incubated at 37°C and monitored for bacterial growth over 48 hours. After the incubation period, the samples were analyzed using the VITEK 2 system and Autof MS1000 for bacterial identification. Despite these comprehensive sampling and analysis efforts, Leclercia adecarboxylata was not detected on any of the surfaces or staff hands. However, given the pathogen’s known ability to survive in moist environments (10), it is still possible that environmental contamination contributed to the infection risk. Moreover, the patient’s abnormal behaviors, including frequent touching of potentially contaminated surfaces, could have facilitated the transmission of the pathogen. Thus, the infection in this case is likely to have resulted from a combination of the patient’s behavioral factors and environmental exposures, highlighting the complex relationship between mental health and infection transmission.
3.3 Association between psychological stress and infection susceptibility
This case provides evidence that psychological stress, particularly in the context of major depressive disorder, may predispose individuals to bacterial infections through immune dysregulation. Activation of the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system under stress leads to elevated cortisol levels, impairing adaptive immune responses while promoting systemic inflammation (8). This dual effect creates a physiological environment conducive to opportunistic infections, even in immunocompetent individuals, as observed with Leclercia adecarboxylata in this case. From a mechanistic perspective, stress-related suppression of mucosal immunity and reduced antimicrobial peptide production may have facilitated bacterial invasion. These findings expand the application of psychoneuroimmune (PNI) models by highlighting their relevance to bacterial infections, traditionally studied in the context of viral or chronic diseases (11). This study demonstrates that even low-virulence pathogens can exploit stress-induced immune vulnerabilities, a contribution that broadens existing theories of host-pathogen interactions. Furthermore, the results emphasize the importance of considering mental health in infection management strategies. Integrating mental health care into infection prevention protocols may reduce risks, particularly in vulnerable individuals. This study advances knowledge in the field by linking stress, immune dysregulation, and bacterial pathogenesis, underscoring the need for interdisciplinary approaches to tackle infections influenced by psychological factors.
3.4 Possibility of environmental and contact transmission
The bidirectional relationship between psychological stress and infection has garnered increasing attention, particularly in the context of immune dysregulation. Leclercia adecarboxylata, a low-virulence pathogen, typically relies on the host’s immune status for successful infection (12). This case demonstrates that even in individuals with an otherwise competent immune system, psychological stress can lead to dysregulation, thereby facilitating infection. This highlights the critical need to consider mental health factors in infection management. Research underscores that mental health disorders, particularly in vulnerable populations such as the homeless or those with substance use issues, can increase susceptibility to infections and complicate recovery (13). For instance, clean needle programs for drug users have been shown to significantly reduce infection rates by addressing both the direct and indirect effects of substance abuse (14). Similarly, mental health support in homeless populations has been recognized as a key determinant in improving health outcomes and reducing infection risks (15). These findings support the notion that addressing mental health in infection management can mitigate the risk of infections, especially in cases where individuals are under severe stress, facing poor living conditions, or engaging in risky behaviors. It is therefore recommended that mental health factors be integrated into infection control strategies to reduce the overall burden of infections. Further research is essential to better understand the mechanisms linking mental health and immune response, ultimately providing a more comprehensive approach to infection prevention and management (15).
3.5 Critical analysis of treatment choice and outcome
The successful treatment with ceftriaxone in this case aligns with the literature documenting Leclercia adecarboxylata’s high susceptibility to this antibiotic (16). However, considering the potential for resistance to β-lactam antibiotics in this pathogen (17), future treatment strategies should be tailored based on antimicrobial susceptibility testing. As antibiotic resistance continues to rise, performing comprehensive susceptibility profiling for each L. adecarboxylata infection is crucial to ensure the selection of the most effective therapeutic regimen.
3.6 Clinical guidelines and recommendations for infection management in patients with mental disorders
Given the complex interplay between mental health and immune function, it is critical to establish comprehensive clinical guidelines to manage infection risks in patients with mental disorders, especially those exhibiting behaviors that may predispose them to infections. In this case, the patient’s psychiatric symptoms, including self-harm tendencies, created a pathway for Leclercia adecarboxylata to enter the bloodstream (2). Therefore, a structured approach to infection prevention and management should be implemented in clinical practice for patients with mental health conditions. Initial Assessment and Diagnosis: Clinicians should routinely assess infection risks in patients with mental disorders, especially those exhibiting abnormal behaviors such as self-harm, impulsivity, or neglect of personal hygiene. Early identification of infection risk factors, including behavioral and environmental exposures, is essential (18). In this case, detailed monitoring of the patient’s clinical symptoms, psychiatric behaviors, and any potential breaches in skin or mucosal integrity should be prioritized. Blood cultures should be obtained promptly in patients exhibiting signs of systemic infection, and environmental sampling, though challenging, should be conducted as early as possible to identify potential sources of infection. Treatment Protocol: Once infection is suspected, empirical antibiotic therapy should be initiated based on local resistance patterns and the patient’s clinical presentation. Given Leclercia adecarboxylata’s documented susceptibility to ceftriaxone, it is a reasonable first-line choice (12). However, antimicrobial susceptibility testing should always be performed to ensure the most effective antibiotic is selected. Given the possibility of β-lactam resistance, it is recommended that clinicians tailor antibiotic therapy based on susceptibility results, which can guide therapy more precisely. Follow-up and Prevention: Follow-up should include regular monitoring of the patient’s response to treatment, with an emphasis on observing changes in clinical symptoms (fever, inflammatory markers) and psychological status. In addition to treating the infection, comprehensive mental health care is essential to manage the underlying psychiatric disorder and reduce the risk of future infections. Psychological interventions such as cognitive-behavioral therapy (CBT) and medications (e.g., antidepressants) should be considered to address the root cause of abnormal behaviors (19). Infection control measures should be strictly followed in hospital settings, particularly for patients with psychiatric disorders who may engage in behaviors that increase exposure to pathogens. Hygiene education, frequent hand washing, and minimizing contact with potentially contaminated surfaces should be emphasized as part of a broader infection prevention strategy (20).
4 Conclusion
This study presents a rare case of Leclercia adecarboxylata bacteremia in a female patient who, despite being immunocompetent, had a mental health disorder. This case highlights the potential for L. adecarboxylata to cause infections via atypical routes, particularly in patients without classical risk factors. Historically, L. adecarboxylata infections have been associated with immunocompromised individuals, such as those undergoing peritoneal dialysis or those with central vascular catheters, where the pathogen typically translocate from the gastrointestinal tract or through medical devices (21). However, recent studies have challenged this paradigm, reporting instances of infection in immunocompetent individuals. Research suggests that stress-induced immune dysregulation may increase susceptibility to infections even with low-virulence pathogens like L. adecarboxylata, particularly in the absence of other predisposing conditions (12). Furthermore, this case aligns with findings from other studies that have implicated mental health conditions, including depression and anxiety, in immune suppression and altered infection susceptibility (11). These observations point to the complexity of infection mechanisms in immunocompetent individuals, where factors such as psychological stress may play a significant role in infection susceptibility. Given the evolving understanding of infection dynamics, integrating mental health considerations into infection management could be crucial in reducing the risk of similar infections, consistent with recommendations to improve health outcomes across both high-risk and seemingly healthy populations. The case underscores the need for clinicians to be particularly vigilant regarding infection risks in patients with mental health disorders, even in the absence of overt immunosuppression. This challenges traditional views of L. adecarboxylata, suggesting that psychological stress could significantly contribute to increased infection susceptibility. As previously noted, stress-induced immune dysregulation can lead to altered immune responses, potentially facilitating infections even in individuals without clear risk factors (22). These findings necessitate a more comprehensive approach to infection prevention and treatment, particularly in patients with mental health disorders that may predispose them to immune system alterations. Additionally, the study highlights key limitations, including the absence of a clearly identified infection source and the lack of a thorough environmental analysis, suggesting the need for larger-scale studies to validate and further explore these findings. The results indicate that mental health factors may significantly influence infection susceptibility through their impact on immune function, reinforcing the need for further research into these mechanisms. Furthermore, the findings underscore the importance of developing prevention and treatment strategies that incorporate both mental and physical health considerations in managing infections caused by emerging pathogens like L. adecarboxylata. In particular, patient education, especially for those with mental health disorders prone to self-harm, should be a core component of infection management to mitigate the risk of such infections (23).
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The patient provided written informed consent for the release of any identifiable details in this article. The study’s procedures involving human subjects complied with the ethical norms of the institution’s research committee and aligned with the principles of the 1964 Helsinki Declaration, as well as its subsequent updates or similar ethical guidelines. The ethical review board of the hospital where the patient received treatment granted approval for this case study.
Author contributions
FY: Conceptualization, Investigation, Methodology, Project administration, Software, Writing – original draft, Writing – review & editing. XR: Data curation, Formal analysis, Funding acquisition, Investigation, Project administration, Resources, Software, Validation, Writing – original draft, Writing – review & editing. QT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. GS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. RX: Conceptualization, Data curation, Formal analysis, Project administration, Resources, Software, Validation, Visualization, Writing – original draft. XB: Resources, Software, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors extend their gratitude to Dr. Lang Zhang for his invaluable professional insights regarding this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Spiegelhauer MR, Andersen PF, Frandsen TH, Storgaard M. Leclercia adecarboxylata: A case report and literature review of 74 cases demonstrating its pathogenicity in immunocompromised patients. J Clin Microbiol. (2018) 56:789–93. doi: 10.1080/23744235.2018.1536830
2. Dotis J, Kondou A, Karava V, Sotiriou G, Papadopoulou A, Zarras C, et al. Leclercia adecarboxylata in peritoneal dialysis patients: A systematic review. Pediatr Rep. (2023) 15:98–105. doi: 10.3390/pediatric15020025
3. Kaushik M, Aayush Mitta. Tirador K, Ibrahim H, Drake S. Leclercia adecarboxylata causing necrotizing fasciitis in an immunocompetent athlete injecting illicit testosterone supplements. Cureus. (2020) 12:e11196. doi: 10.7759/cureus.11196
4. Gajdács M, Ábrók M, Lazar A, Terhes G, Burián K. Leclercia adecarboxylata as an emerging pathogen in human infections: a 13-year retrospective analysis in southern hungary. J Infection Developing Countries. (2020) 14:1004–10. doi: 10.3855/jidc.12598
5. Zayet S, Lang S, Garnier P, Pierron A, Plantin J, Toko L, et al. Leclercia adecarboxylata as an emerging pathogen in human infections: Clinical features and antimicrobial susceptibility testing. Pathogens. (2021) 10:1399. doi: 10.3390/pathogens10111399
6. Lonneman MK, Devasahayam RJ, Phillips CJ. Leclercia adecarboxylata causing necrotising soft tissue infection in an immunocompetent adult. BMJ Case Rep. (2020) 13:e235633. doi: 10.1136/bcr-2020-235633
7. Miller AH, Raison CL. The role of inflammation in depression: from mechanisms to treatment. Neuropsychopharmacology. (2016) 41:24–40. doi: 10.1038/nri.2015.5
8. de Abreu Feijó de Mello A, Feijó de Mello M, Carpenter LL, Price LH. Update on stress and depression: The role of the hypothalamic-pituitary-adrenal (HPA) axis. Rev Bras Psiquiatria. (2003) 25:204–10. doi: 10.1590/s1516-44462003000400010
9. Gajdács M, Ábrók M, Lázár A, Terhes G, Burián K. Leclercia adecarboxylata as an emerging pathogen in human infections: A 13-year retrospective analysis in southern hungary. J Infection Public Health. (2020) 13:1515–22. doi: 10.3855/jidc.12598
10. Keyes J, Johnson EP, Epelman M, Cadilla A, Ali S. Leclercia adecarboxylata: An emerging pathogen among pediatric infections. Cureus. (2020) 12:e8049. doi: 10.7759/cureus.8049
11. Yang EV, Glaser R. Stress-induced immunomodulation: Impact on immune defenses against infectious disease. Eur J Clin Microbiol Infect Dis. (2000) 19:1–7. doi: 10.1016/S0753-3322(00)80066-9
12. Jasinska AJ, Pandrea I, He T, Benjamin C, Newton M, Lee JC, et al. Immunosuppressive effect and global dysregulation of blood transcriptome in response to psychosocial stress in vervet monkeys (Chlorocebus sabaeus). Sci Rep. (2020) 10:10699. doi: 10.1038/s41598-020-59934-z
13. Mazza M, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behavior Immun. (2020) 89:594–600. doi: 10.1016/j.bbi.2020.07.037
14. Kåberg M, Karlsson N, Discacciati A, Widgren K, Weiland O, Ekström A, et al. Significant decrease in injection risk behaviours among participants in a needle exchange programme. Infect Dis. (2020) 52:336–46. doi: 10.1080/23744235.2020.1727002
15. Tweed E, Thomson R, Lewer D, Sumpter C, Kirolos A, Southworth P, et al. Health of people experiencing co-occurring homelessness, imprisonment, substance use, sex work and/or severe mental illness in high-income countries: A systematic review and meta-analysis. J Epidemiol Community Health. (2021) 75:1010–8. doi: 10.1136/jech-2020-215975
16. Malik K, Davie R, Withers AE, Faisal M, Lawal F. A case of leclercia adecarboxylata endocarditis in a 62-year-old man. IDCases. (2021) 24:e01091. doi: 10.1016/j.idcr.2021.e01091
17. Sun Q, Wang H, Shu L, Dong N, Yang F, Zhou H, et al. Leclercia adecarboxylata from human gut flora carries mcr-4.3 and blaIMP-4-bearing plasmids. Front Microbiol. (2019) 10:2805. doi: 10.3389/fmicb.2019.02805
18. Bell V, Wade D. Mental health of clinical staff working in high-risk epidemic and pandemic health emergencies: a rapid review of the evidence and living meta-analysis. Soc Psychiatry Psychiatr Epidemiol. (2020) 56:1–11. doi: 10.1007/s00127-020-01990-x
19. Hamlin M, Holmén J, Wentz E, Aiff H, Ali L, Steingrimsson S. Patient experience of digitalized follow-up of antidepressant treatment in psychiatric outpatient care: Qualitative analysis. JMIR Ment Health. (2023) 10:e48843. doi: 10.2196/48843
20. Kubde D, Badge AK, Ugemuge S, Shahu S. Importance of hospital infection control. Cureus. (2023) 15:e50931. doi: 10.7759/cureus.50931
21. Zayet S, Lang S, Garnier P, Pierron A, Plantin J, Toko L, et al. Leclercia adecarboxylata as an emerging pathogen in human infections: Clinical features and antimicrobial susceptibility testing. Pathogens. (2021) 10:1399. doi: 10.3390/pathogens10111399
22. Pereira J, Rea K, Nolan Y, O'Leary O, Dinan T, Cryan J. Depression's unholy trinity: Dysregulated stress, immunity, and the microbiome. Annu Rev Psychol. (2020) 71:107–34. doi: 10.1146/annurev-psych-122216-011613
Keywords: Leclercia adecarboxylata, immunocompetent host, bacteremia, mental health and infection, emerging pathogen
Citation: Yan F, Ruan X, Tang Q, Song GL, Xie RF and Bao XC (2024) Case report: A rare case of Leclercia adecarboxylata bacteremia in an immunocompetent psychiatric patient: exploring the links between mental health and infectious diseases. Front. Immunol. 15:1494168. doi: 10.3389/fimmu.2024.1494168
Received: 10 September 2024; Accepted: 03 December 2024;
Published: 19 December 2024.
Edited by:
Jiajia Song, Southwest University, ChinaReviewed by:
Sasidhar Gunturu, Bronx-Lebanon Hospital Center, United StatesBin Wang, Binzhou Medical University, China
Copyright © 2024 Yan, Ruan, Tang, Song, Xie and Bao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xi Ruan, MTI0NjQ2MDUxQHFxLmNvbQ==; Qin Tang, NjUzODUxMjNAcXEuY29t
 Fei Yan
Fei Yan Xi Ruan1,2*
Xi Ruan1,2* Qin Tang
Qin Tang