- 1Consultant, Warsaw, Poland
- 2Parent’s Guide to Cord Blood® Foundation, Brookeville, MD, United States
Introduction: This article explains the current regulatory system in Poland regarding Advanced Therapy Medicinal Products given under Hospital Exemptions (ATMP-HE).
Methods: The relevant sections of Polish legislation are translated into English and their interaction is described.
Results: We analyze the impact of these regulations from the perspective of three stakeholder groups: manufacturers, physicians, and patients. Amendments enacted between 2018 and 2023 have substantially changed Polish implementation of the ATMP-HE pathway. In Poland, most ATMP-HE treatments have been therapies employing Mesenchymal Stromal Cells (MSC).
Discussion: Comparison to other European countries shows that Poland is within the mainstream of EU practices regarding ATMP-HE implementation. One notable issue is that Poland has relatively low per capita spending on healthcare, and ATMP-HE in Poland must be funded from outside the government healthcare system. Conclusions. The original intention of the legislation that created ATMP-HE was to allow access to experimental therapies for patients with unmet needs. It remains to be seen if that mission can be fulfilled amidst conflicting pressures from various stakeholder groups.
1 Introduction
The European Medicines Agency (EMA) is an agency of the European Union (EU) which is responsible for the scientific evaluation, supervision, and safety monitoring of medicines in the EU (1). The medical regulations from the EMA provide guidelines for member states, but leave flexibility within those guiding limits for the path traveled by individual nations. For example, only the authorities in individual member states can authorize clinical trials of advanced therapy medicinal products (ATMP), or grant final market approval of ATMP within their borders (1). Hospital exemptions (HE) are another category of medical treatment where the role of the EMA overlaps with, but does not replace, the regulatory role of competent authorities in each EU member state. The European parliament adopted Regulation 1394/2007/EC that amended Directive 2001/83/EC and created a hospital exemption pathway for ATMPs (2). The hospital exemptions created in Regulation 1394/2007/EC were intended to provide expanded access to experimental therapies for patients with unmet needs. While on the one hand the ATMP-HE pathway allows access to experimental products that are not yet approved, on the other hand it creates a safe space for the use of those products by imposing quality controls on the product manufacturing and safety monitoring of the clinical delivery (2).
Since the establishment of the ATMP-HE pathway in 2007, its application has evolved with the development of new therapies. While the language of Regulation 1394/2007/EC constrains the manufacturing conditions, it does not restrict the patients’ indications for use. A traditional justification for HE therapies has been “compassionate use” therapies for patients that have incurable conditions for which there is no therapy with marketing authorization. Subsequently, newer cell and gene therapies like CAR-T have achieved market authorization, and currently the ATMP-HE pathway is also used to allow patients to access these new therapies in circumstances where they do not qualify for the standard treatment protocols (3–5).
One source of creative tension in the application of the ATMP-HE pathway is that each EU member country has developed their own method of interpreting and applying the ATMP-HE regulations. As a result, the landscape of what therapies are covered by ATMP-HEs and how these treatments are offered may differ significantly from one country to another, as previous authors have noted (3–15). Studies of the sociology of science have pointed out that scientists and regulators may feel pressures to modify universal standards to their own national circumstances, either because of a need to adapt to local realities like pre-existing practices, or out of a desire to be competitive with other nations (16–18). Some members of the cell and gene therapy (CGT) community have argued that the ATMP-HE regulations in various countries should be more harmonized (5, 13, 14), whereas others feel that the current system encourages innovation, localization, and cost savings (10, 12, 15).
Another source of tension and outright controversy is that ATMP-HE have become somewhat politicized. The arena of regenerative medicine is plagued by the existence of illegal clinics which advertise direct to consumers that their alleged stem cell products will cure anything that ails a patient (19–21). There has been a rallying cry among alliances of pharmaceutical companies and societies of CGT professionals that there is a need to stamp out “unproven” therapies (21). Those patients that receive ATMP-HE composed of Mesenchymal Stromal Cells (MSC) are often receiving treatments that are very similar to what is offered in illegal clinics, except they are subject to the ATMP-HE requirements on quality control of the manufacturing process and supervision of the clinical safety. Nonetheless, the fact that ATMP-HE products are not “proven” therapies has led some authors to place them in the same bucket as “unproven” commercialization (14). For this reason, the use of ATMP-HE should be evaluated in the context of community standards for the safety and efficacy of MSC therapies (22–24).
2 Methods
The purpose this paper is to explain in detail the current requirements and application of the ATMP-HE regulations in Poland. This paper starts by providing English translations of the key sections of Polish law that govern the availability and application of ATMP-HE programs. In addition, we explain how these laws are interpreted and applied in the context of the Polish healthcare system. We make note of several amendments to these laws which have been adopted recently and which are expected to significantly alter ATMP-HE practices in Poland going forward.
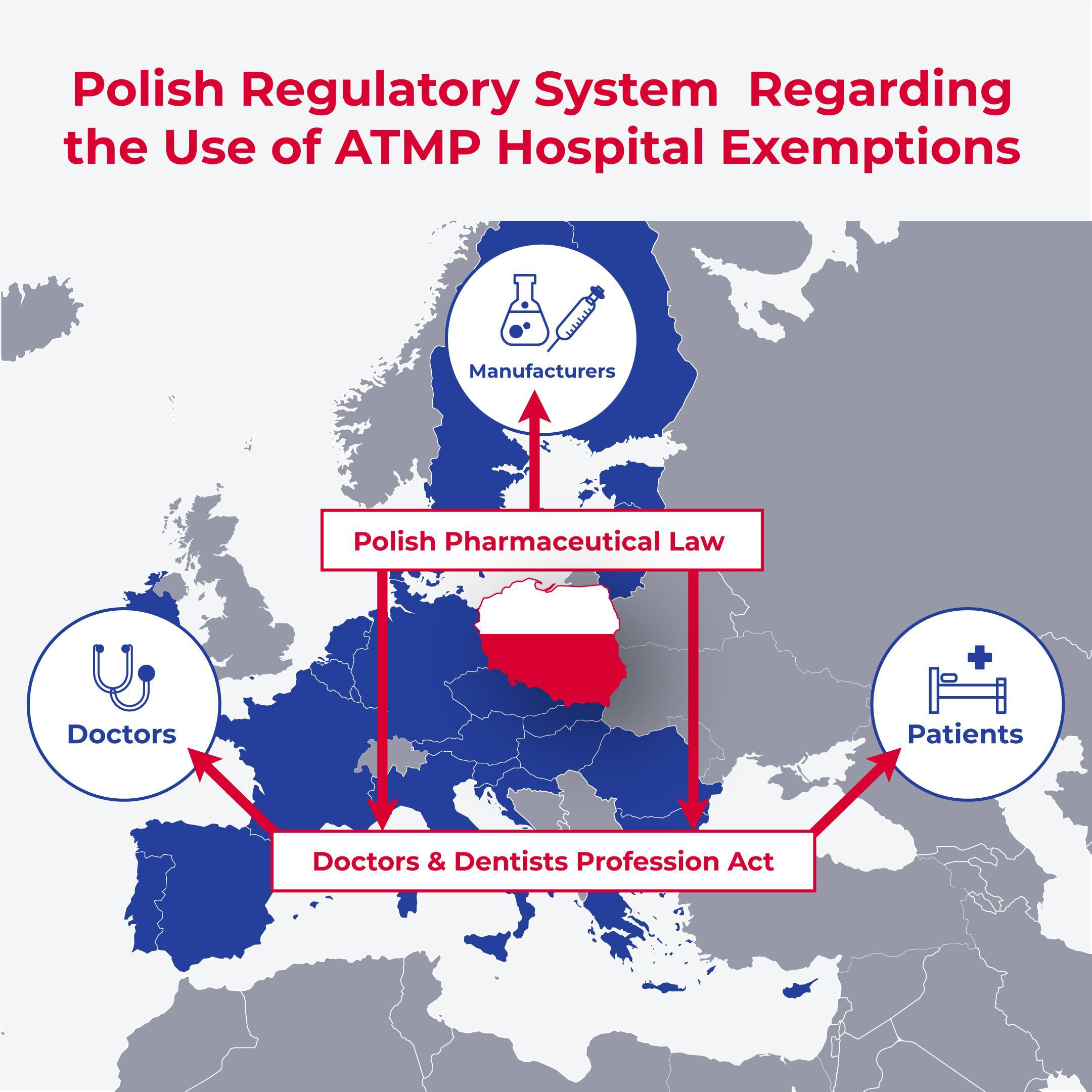
This is the first paper on ATMP-HE which analyzes the impact of the regulatory system from the perspective of three main stakeholder groups: manufacturers, physicians, and patients in Poland. This approach can be generalized to other countries. The breakdown into stakeholder groups helps to illustrate that there are multiple national regulations that filter ATMP-HE policies before they are applied. For example, interactions between healthcare providers and patients are always regulated by national authorities. These layers contribute to any variations that are seen between ATMP-HE practices in different countries.
In the discussion section we compare ATMP-HE practices in Poland to several other European countries for which we have accessed the regulations, as well as to previous publications on ATMP-HE variations among EU countries.
3 Results
3.1 Legal basis of using ATMP-HE under Polish Law
The existence of Hospital Exemptions in the European Union was established by Article 28 of EU Regulation 1394/2007/EC, which introduced modifications to the previous Article 3 Directive 2001/83/EC on medicinal products for human use (2). The new Article 28 implemented special conditions that allow patients to be treated with advanced therapy medicinal products that have not received marketing authorization. Article 28 also outlined the criteria necessary to apply for this exemption. This exemption is called ATMP Hospital Exemption or ATMP-HE.
The exact language of Article 28 of Regulation 1394/2007/EC that creates ATMP-HE pathway states as follows in English: “Any advanced therapy medicinal product, as defined in Regulation (EC) No 1394/2007/EC, which is prepared on a non-routine basis according to specific quality standards, and used within the same Member State in a hospital under the exclusive professional responsibility of a medical practitioner, in order to comply with an individual medical prescription for a custom-made product for an individual patient. Manufacturing of these products shall be authorized by the competent authority of the Member State. Member States shall ensure that national traceability and pharmacovigilance requirements as well as the specific quality standards referred to in this paragraph are equivalent to those provided for at Community level in respect of advanced therapy medicinal products for which authorization is required pursuant to Regulation (EC) No 726/2004/EC of the European Parliament and of the Council of 31 March 2004 laying down Community procedures for the authorization and supervision of medicinal products for human and veterinary use and establishing a European Medicines Agency” (2, 25).
After the 2007 EU regulations establishing ATMP-HE, regulations in Poland regarding the use of medicinal products were modified on 18 March 2011. This was done through the Act that established the President of the Office for Registration of Medicinal Products, Medical Devices and Biocidal Products. Amendments were made by adding Article 3 Section 4 Point 7 to Poland’s Pharmaceutical Law (26). The current language of this law and its amendments date from June 2018 (27). Prior to the Amendment of the Pharmaceutical Law in June 2018, there was no obligation for hospitals in Poland to offer ATMP-HE, which was a major legislative defect.
Currently, the Pharmaceutical Law of Poland reads as follows: “an advanced therapy medicinal product - hospital exception - is an advanced therapy medicinal product within the meaning of Art. 2 sec. 1 lit. and Regulation (EC) No. 1394/2007/EC of the European Parliament and of the Council of 13 November 2007 on advanced therapy medicinal products and amending Directive 2001/83/EC and Regulation (EC) No. 726/2004/EC (Official Journal EU L 324 of 10.12.2007, p. 121, as amended13), hereinafter referred to as ‘Regulation 1394/2007’, which is prepared in the territory of the Republic of Poland on a non-routine basis in accordance with quality standards and applied as part of hospital medical services within the meaning of Art. 2 sec. 1 point 11 of the Act of 15 April 2011 on medical activity (Journal of Laws of 2022, items 633, 655, 974 and 1079) in the territory of the Republic of Poland under the sole responsibility of a physician in order to make an individually prescribed medicinal product for a given patient.” (27).
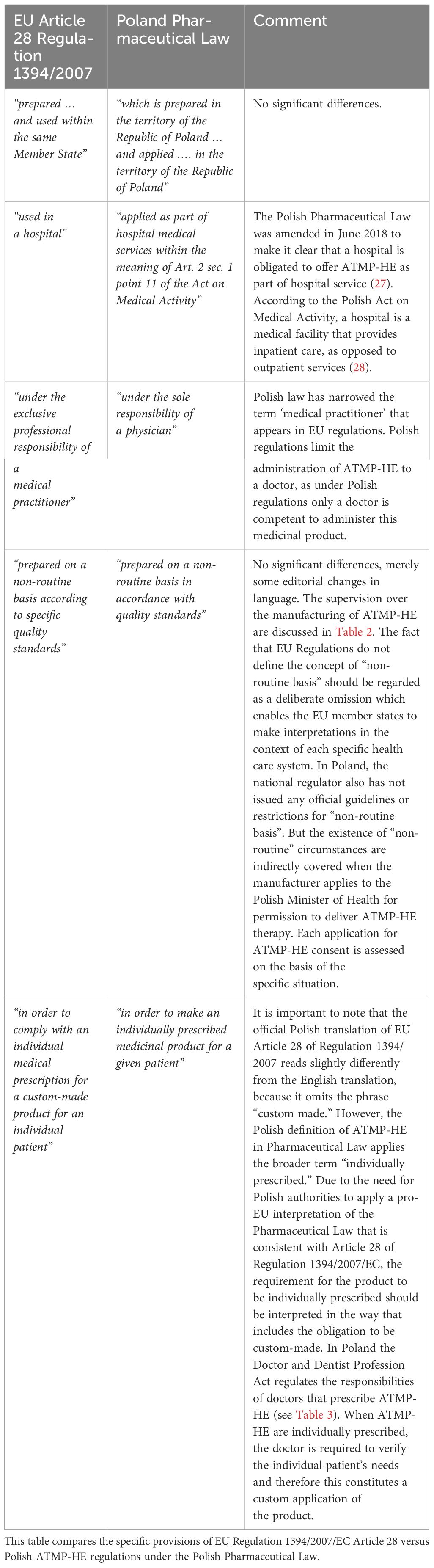
Table 1 presents an analysis that compares the concepts of EU Article 28 of Regulation 1394/2007/EC versus Poland’s Pharmaceutical Law implementing the ATMP-HE provision (2, 25–27). There are differences in the Polish language that appears instead of the three EU quotes “custom-made product for an individual patient”, “used in a hospital”, and “under the exclusive professional responsibility of a medical practitioner” (23–27). We discuss these in turn. First, the Polish Pharmaceutical Law does not include the term “custom-made”, only indicating a similar but broader term “individually prescribed” (26, 27). In Poland the requirement to customize the treatment is implicitly included when the doctor individually prescribes the ATMP-HE product. Second, while some EU member states interpret “used in a hospital” loosely to include clinics, under the current Polish system of providing healthcare services, ATMP-HE may only be administered in hospitals and not in outpatient facilities (28). Third, the EU phrase “medical practitioner” has become “doctor” because in Poland only doctors may prescribe ATMP-HE under the regulations of the Doctor and Dentist Profession Act (29, 30). The responsibilities of doctors prescribing ATMP-HE in Poland are discussed more below.
3.2 Principles of using ATMP-HE under Polish Law: perspective of manufacturers
Products to be administered under ATMP-HE regulations in Poland must be manufactured according to specific quality standards. The relevant language of Article 28 of EU Regulation 1394/2007/EC reads as follows: “Manufacturing of these products shall be authorized by the competent authority of the Member State. Member States shall ensure that national traceability and pharmacovigilance requirements as well as the specific quality standards referred to in this paragraph are equivalent to those provided for at Community level in respect of advanced therapy medicinal products for which authorization is required pursuant to Regulation (EC) No 726/2004/EC of the European Parliament and of the Council of 31 March 2004 laying down Community procedures for the authorization and supervision of medicinal products for human and veterinary use and establishing a European Medicines Agency” (2, 25). These requirements are adopted into article 38a., 38aa, and 38ab of Polish Pharmaceutical Law (26, 27).
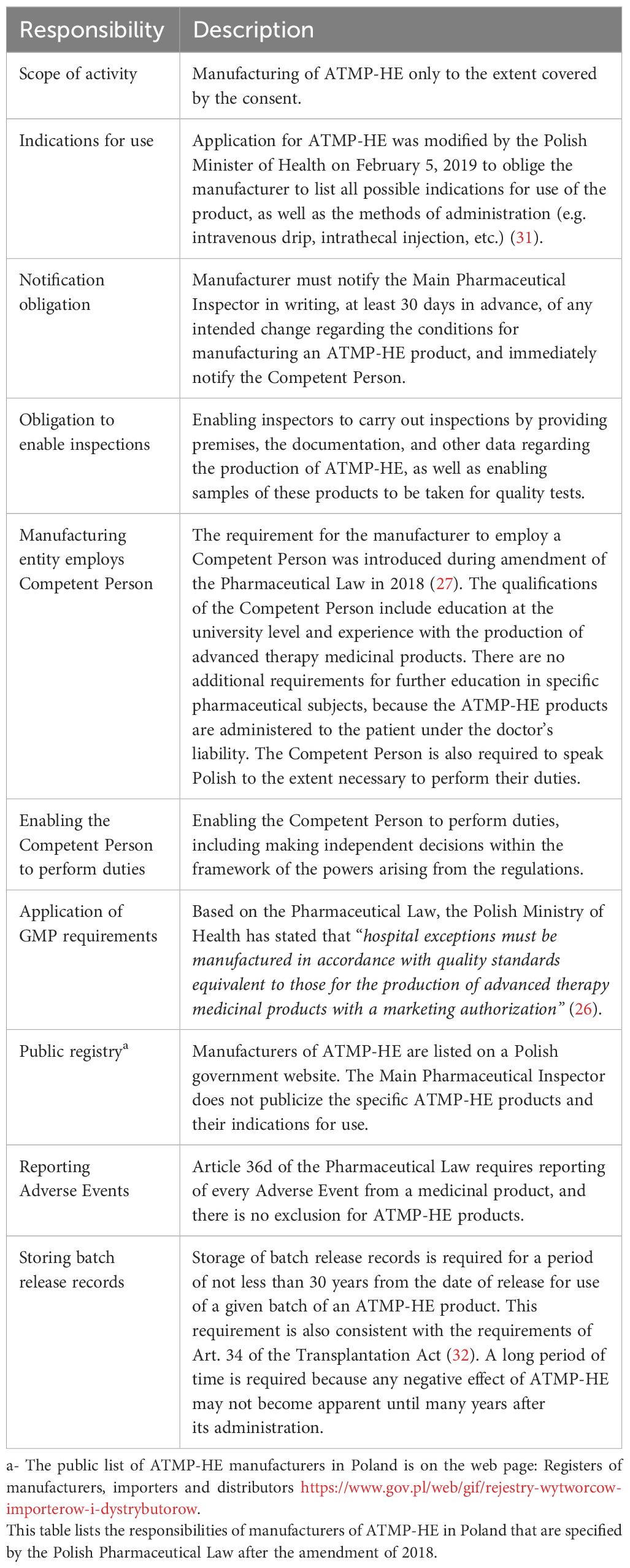
Table 2 describes the manufacturer responsibilities specified by the Polish Pharmaceutical Law (26, 27). The first step in the chain of quality control is that the manufacturer in Poland must obtain consent for the manufacture of ATMP-HE. Under Polish Pharmaceutical Law, the Main Pharmaceutical Inspector is the authority that is competent to issue consent, refuse to grant it, declare its expiry, or withdraw and change this consent by way of a decision. The manufacturer submits an application to the Main Pharmaceutical Inspector that includes, among others: entrepreneur’s data, list of ATMP-HE, specification of the type and indications of the ATMP-HE, specification of the place of manufacturing in accordance with GMP, scope of activity at the site of manufacture, data of the competent person including specific information about her qualifications, and proof of payment of the fee. If necessary, the application should also include a copy of the manufacturer’s permit for tissue and cell banking.
Second, prior to granting or denying consent for manufacture of ATMP-HE, an inspection of the manufacturing facility is conducted by manufacturing inspectors of the Main Pharmaceutical Inspectorate. The purpose of the inspection is to ensure that the entity applying for consent meets the requirements of Good Manufacturing Practice (33). The inspector will determine that: the entity has appropriate premises, technical equipment, and control necessary for the production, control, and storage of ATMP-HE, and that it employs a Competent Person. The qualifications of the Competent Person are listed in Table 2. Once these steps have been completed and the consent is granted, the consent is issued for an indefinite period. Follow up inspections are held at least once every two years. Additionally, it is possible to carry out ad hoc inspections. It is important to note that the role of the Main Pharmaceutical Inspectorate is purely to ensure the quality of the product and they play no role in judging the medical applications of the product. “Main Pharmaceutical Inspector does not supervise the selection of therapy and treatment of patients using advanced therapy medicinal products - hospital exceptions (ATMP-HE). … Therefore, it only supervises the conditions of production of the above-mentioned products by inspecting manufacturing sites” (34).
Third, Article 38ab of Polish Pharmaceutical Law spells out circumstances under which the consent to manufacture ATMP-HE may be withdrawn by the Main Pharmaceutical Inspectorate. These circumstances fall into the categories of obligatory and optional. It is obligatory to withdraw the consent if the manufacturer does not meet some of the statutory requirements. It is optional to withdraw the consent in cases where the possible negative effect on the patient could be disproportionate to the degree of violation of the law. These mechanisms strengthen effective supervision over the area of ATMP-HE production because they introduce rules for withdrawing ATMP-HE consent.
Fourth, we must discuss how Polish regulations interpret the preparation of an ATMP-HE product on a “non-routine basis”, since this is not defined under the umbrella EU regulations (2, 25). The absence of a definition for “non-routine basis” should be regarded as a deliberate omission by the EU regulator which enables the EU member states to make interpretations in the context of each specific healthcare system. In Poland, the national regulator also has not issued any official guidelines or restrictions for “non-routine basis” (26, 27). Each application for ATMP-HE consent is assessed based on the patient’s specific situation.
3.3 Principles of using ATMP-HE under Polish Law: perspective of physicians
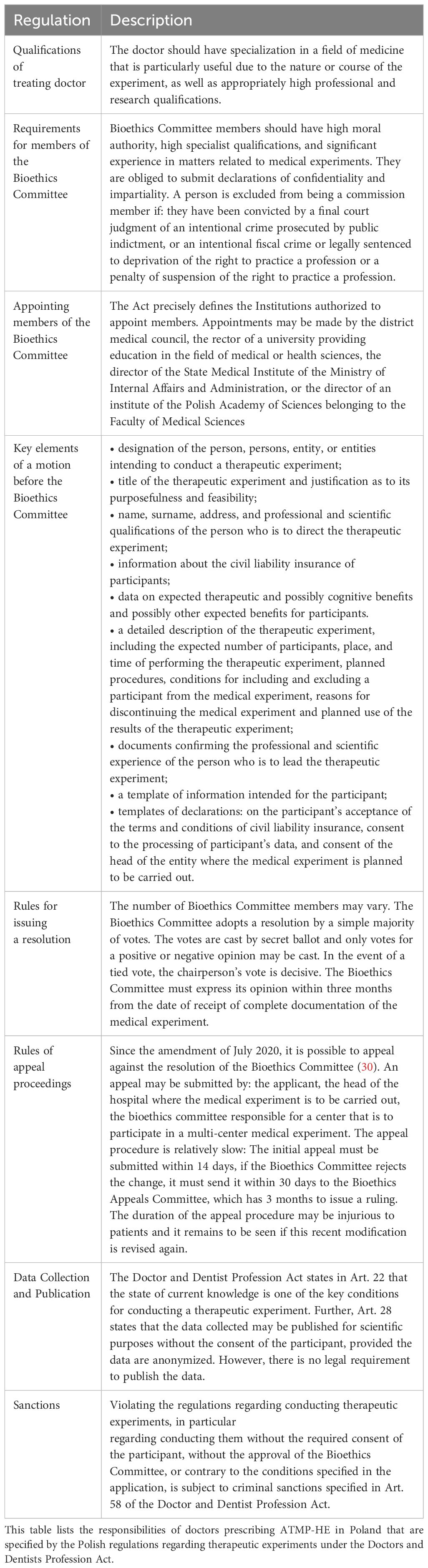
The Polish Pharmaceutical Law states that ATMP-HE must be administered “under the exclusive professional responsibility of a physician in order to comply with an individual medical prescription for a given patient” (26, 27). Unlike the wording of the EU directive which assigns responsibility to a “medical practitioner,” in Poland the entire responsibility for administering ATMP-HE rests on the patient’s doctor. The responsibilities of doctors in Poland are spelled out under the Doctor and Dentist Profession Act (29, 30). A doctor in Poland practices a strictly regulated profession, the doctor works within a registered medical entity, and the doctor bears criminal, professional, civil, and sometimes administrative liability. When ATMP-HE are considered as a form of treatment, it is the patient’s doctor that initiates the request to the Bioethics Committee, and once approval is granted the patient’s doctor is responsible for the administration of the therapy. The rules for doctors and the role of the Bioethics Committee are both very important, working in partnership, to regulate the administration of ATMP-HE in Poland.
Since ATMP-HE products have not gone through the full pipeline of clinical trials required for market authorization, their use is subject to the provisions of a therapeutic experiment. The obligations for doctors administering experimental therapy are set forth in Chapter 4 of the Doctor and Dentist Profession Act as follows: “A therapeutic experiment is the introduction by a doctor of new or only partially tested diagnostic, curative or preventive methods for the purpose of obtaining a direct health benefit for the treated person. It may be conducted if the medical methods used so far are ineffective or not sufficiently effective” (29, 30). It must be emphasized that the law provides for many obligations related to the commencement of a therapeutic experiment by a doctor, for instance: appropriate purpose of the experiment; appropriate qualifications and proper specialization of the doctor conducting experiment; obtaining informed consent from the patient; and obtaining positive opinion on the therapeutic experiment from a proper Bioethics Committee (35–37).
Table 3 outlines the specific Polish ATMP-HE regulations provided by the Doctor and Dentist Profession Act, in particular regarding the Bioethics Committee (29, 30). The main principle that should be followed when determining whether a therapeutic experiment is permissible in each case is expressed in Article 22 of the Doctor and Dentist Profession Act. Therapeutic experiments may be carried out if the expected therapeutic benefit may be significant, and the risks associated with achieving this benefit are justified in the light of the current state of knowledge and consistent with the ethical principles of the medical profession. It is worth noting that the current state of medical knowledge is constantly evolving. The amendment of the Doctor and Dentist Act of 2020 created a mechanism to appeal the decision of the Bioethics Committee (30). This policy is consistent with Art. 42 and 42a of the Polish Code of Medical Ethics (38). Art. 28 of the Doctor and Dentist Profession Act states that the data collected may be published for scientific purposes without the consent of the participant, provided the data are anonymized, but there is no legal requirement to publish the outcome data. Retrospective studies of outcomes have been published for ATMP-HE patients in Poland that were treated with MSC for the indications cerebral palsy, spina bifida, and amyotrophic lateral sclerosis (39–41).
3.4 Principles of using ATMP-HE under Polish Law: perspective of patients
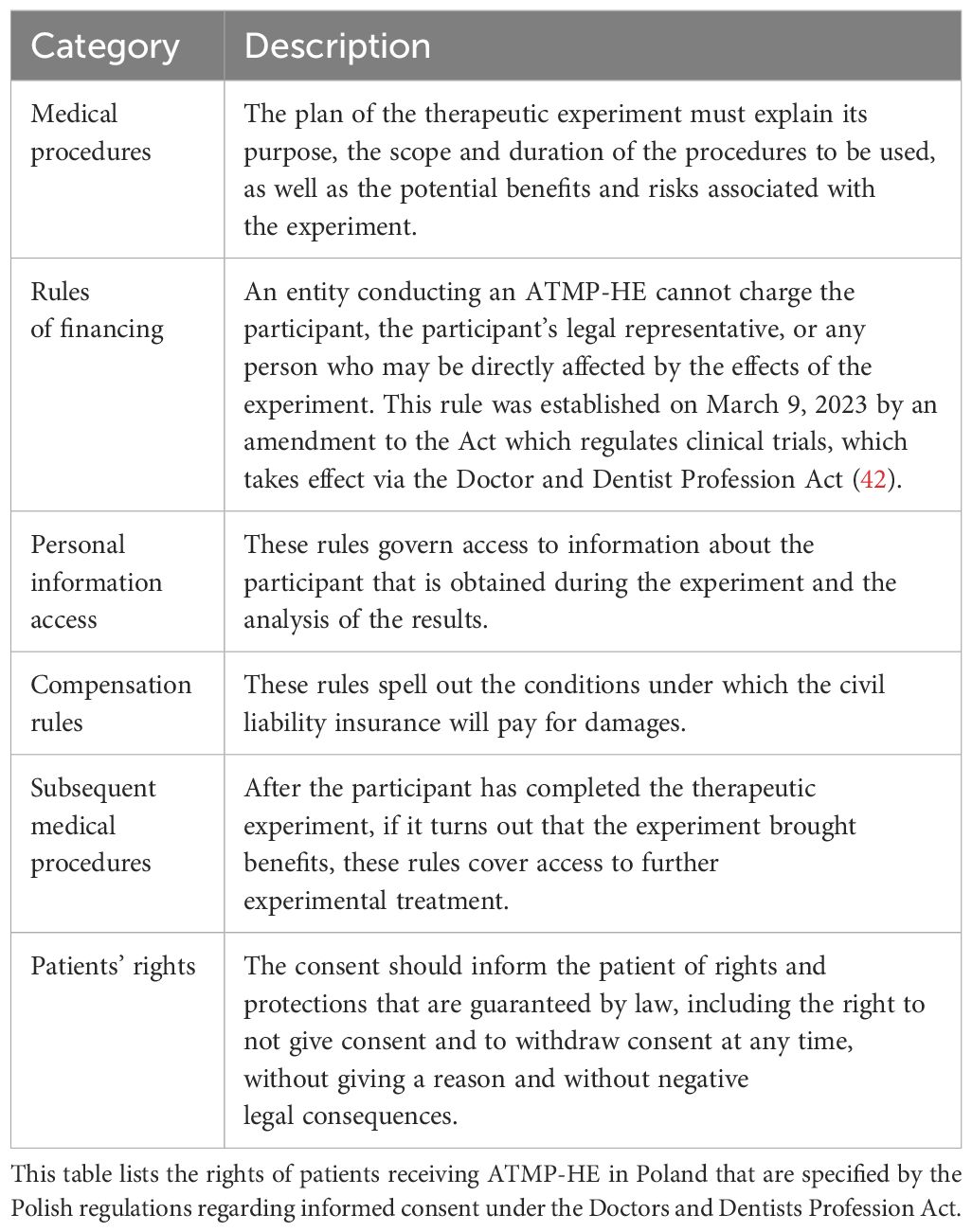
Table 4 sets out the features required when a patient gives Informed Consent for ATMP-HE therapy. The provisions of Informed Consent for a medical procedure are part of the Doctor and Dentist Profession Act (29, 30). The consent for an experimental procedure contains more provisions than a standard medical consent for a procedure that has market approval. The regulations for ATMP-HE also include safety rules which require that the experiment should be stopped if there is a threat to the participant’s health that exceeds the expected benefits. An update to the original Informed Consent requirements made by Amendment of the Doctor and Dentist Profession Act in 2020 has strengthened the provisions for patient protection (30): Experiments should not be approved if there is evidence from global reports, such as from clinical trials or compassionate use programs conducted elsewhere, that they are not likely to be successful. The participant or the representative acting on their behalf may withdraw consent at any stage of the experiment. Also, participation in the experiment must not delay or deprive the patient from receiving preventive, diagnostic, or therapeutic procedures that are medically necessary.
Financial restrictions have also been added to the Doctor and Dentist Profession Act which are intended to protect patients receiving experimental therapy in Poland. One such financial rule is that the entity conducting the ATMP-HE must offer the participants civil liability insurance. This was introduced July 16, 2020 by amendment to Article 23c, section 1, of the Doctor and Dentist Profession Act. “A medical experiment may be conducted after the entity conducting the medical experiment has concluded a civil liability insurance contract for the participant and any other person who may be directly affected by the effects of the experiment” (30). This provision became effective January 1, 2021 (with exceptions for therapeutic experiments which the Bioethics Committee had begun to consider or had issued an opinion on before that date). An exception to this insurance obligation occurs if the case is urgent and there is a direct threat to the life of the experiment participant.
Another financial restriction was introduced on 9 March 2023 by an amendment to the Act which regulates clinical trials (42). This indirectly alters the enforcement of the Doctor and Dentist Profession Act. This newest restriction prohibits the entity conducting the ATMP-HE experiment from charging fees on participants, the representatives of participants, or people who may be directly affected by the experiment. The justification for this amendment states that this limitation is intended to protect patients against “abuses by medical entities accompanied by insufficient supervision by bioethics committees,” because patients themselves are unable to verify the validity of experimental therapy (42). However, it is allowed to obtain funding for ATMP-HE experimental therapies from specialized third parties, such as non-profit foundations, that professionally deal with such activities and therefore have greater knowledge than individual patients (42).
4 Discussion
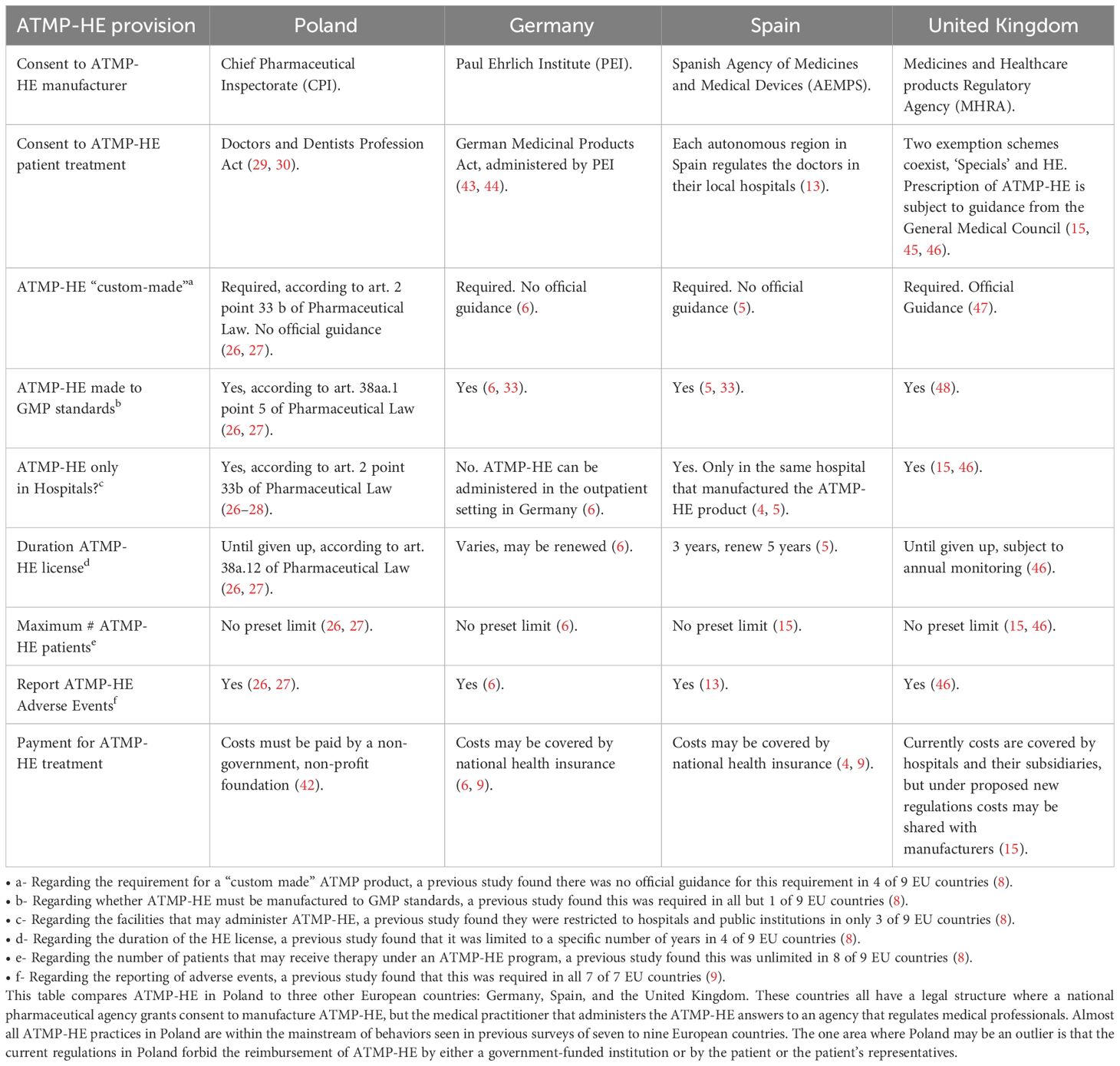
Table 5 lists several features of ATMP-HE regulations in Poland as compared to three other European countries: Germany, Spain, and the United Kingdom. Together, these four countries are a good illustration of the interplay between unifying concepts versus national differences in the way ATMP-HE are managed in different healthcare systems. Footnotes to Table 5 cite the breakdown of these parameters in previous studies of ATMP-HE practices in Europe (3–15). It is worth pointing out that many aspects of healthcare in general are not fully harmonized at the EU level. Regarding ATMP-HE specifically, the Article which creates this pathway intentionally uses broad language which allows for differences in the national interpretations of the guidelines (2). Hence, any national regulations that fall within the guidelines cannot be called an improper application, when the original directive is imprecise. It is clear from the columns and footnotes of Table 5 that ATMP-HE practices in Poland are well within the spectrum of regulatory variations seen among EU countries. For example, if Poland is included, then half of the EU countries surveyed (5 of 10) do not have a guidance to interpret the EU requirement that ATMP-HE must be manufactured under “non-routine” and/or “custom-made” conditions (8). Another example is that that the language of EU Regulation 1394/2007/EC does not restrict the number of patients that may participate in a single ATMP-HE program. This is echoed at the national level, where almost all surveyed EU countries (9 of 10) allow an “unlimited” number of patients to be treated under an ATMP-HE program (8). Thus, in this regard Poland follows the rule and is not an exception. The one aspect in which Poland may be an outlier is the types of payments that are allowed to reimburse the manufacturers of ATMP-HE products. Some countries allow the cost of ATMP-HE to be covered by their national healthcare system, either directly or indirectly through a non-profit connected to the government, whereas Poland requires payment from outside their healthcare system (9).
It is very important to note that there have been several significant changes to Polish regulations in the past few years, so that current ATMP-HE practices in Poland differ dramatically from cumulative surveys of previous cases (14). In 2018, the Pharmaceutical Law was modified to clarify that ATMP-HE must be administered within hospital healthcare services, both in the sense that hospitals are required to allow ATMP-HE, and in the sense that outpatient facilities cannot offer ATMP-HE (27, 28). Those 2018 modifications to the Pharmaceutical Law also required manufacturers to employ a Competent Person, and spelled out the qualifications and duties of the Competent Person (27). In 2019, the template used when requesting Bioethics Committee approval of ATMP-HE began requiring a description of all indications for use of the product as well as the method of administration (31). In 2020, amendments to the Doctor and Dentist Profession Act created new functions for the Bioethics Committee: the amendment tasked the committee to consider the evidence from previous compassionate use programs when deciding if a treatment is likely to be beneficial, but this amendment also created pathways to appeal decisions of the Bioethics Committee (30). Effective at the beginning of 2021, an amendment to the Doctors and Dentists Profession Act required that participants in ATMP-HE programs must be covered by liability insurance (30). In 2023, further amendments to the section of the Doctors and Dentists Profession Act covering experimental therapies have prohibited ATMP-HE from charging fees on participants (42).
The EU funded a 2018 survey of public perceptions on ATMP therapies under a research initiative called RESTORE (49). This survey of the European public was conducted in 28 countries that were representative of 85.3% of the EU population. Respondents ranked “Healthcare” as the most important topic facing society, ahead of seven other issues including data protection, green energy sources, and migration. Regarding ATMP, the top three findings of the survey were (1): 83% of the surveyed EU citizens support more public funding of technologies in the field of ATMPs (2); 74% of respondents are in support of cross-border ATMP healthcare for patients with rare diseases; and (3) 61% support the reimbursement of very expensive ATMPs within the European health care system despite the current lack of long-term efficacy data (49). Drilling deeper into country-by-country responses to this 2018 survey, citizens in Poland were outliers on some of the issues. Polish people were most likely (50%) to be aware of commercial clinics offering unproven ATMP therapies (49). Polish respondents gave the highest approval (80%) for taxpayer funding of cross-border ATMP healthcare (49). In the published outcomes of ATMP-HE in Poland, patient responses were statistically significant on some metrics and the patients and their families reported satisfaction with their improved quality of life (39–41). Despite the documented enthusiasm of the Polish public for access to ATMP therapies, market uptake of approved ATMP therapies will require that the products be affordable. In the past, many ATMP which received early approvals in EU countries were subsequently withdrawn due to inadequate reimbursements (50, 51).
Affordability of healthcare is a serious concern in Poland. Within the EU, Poland has one of the lowest levels of annual spending per capita on healthcare (49). In 2018 the per capita spending on healthcare was 830 Euro in Poland, whereas for the other countries in Table 5 the spending was 4627 Euro in Germany, 3646 Euro in UK, and 2310 Euro in Spain (49). Not only do these countries spend between 2.8 and 5.6 times more on healthcare than Poland, but we see from Table 5 that they also have regulatory frameworks that allow ATMP-HE to be directly or indirectly reimbursed by the government. Surveys of ATMP-HE access have found that only a handful of ATMP-HE have ever been registered in most EU countries, but some ATMP-HE programs have been used to treat hundreds and possibly thousands of patients (7, 9, 51). Until recently in Poland, thousands of patients paid out of pocket to access ATMP-HE at hospitals and clinics. Many of these patients traveled from other countries to take advantage of the ATMP-HE programs in Poland. One manufacturer has compiled a registry of over 3450 patients treated, from 35 countries, primarily with MSC, in both clinical trials and ATMP-HE programs (52). But, with the overhaul of Polish regulations during the years 2018 – 2023, this direct-to-consumer access to ATMP-HE has stopped. At present, manufacturers that wish to provide ATMP-HE in Poland are reorganizing to run these programs exclusively in hospitals and funded solely by third party payers (27, 42).
The economic impact of ATMP-HE regulations in Poland is neutral from the perspective of public expenditures on the healthcare system. Whether the ATMP-HE are financed directly by patients or through non-profit foundations, in either case the costs do not burden the budget of the National Health Fund, which is underfinanced. In addition, Polish regulations specify that ATMP-HE can only be used if existing registered therapies cannot meet a patient’s needs, so there is no competition with approved therapies. At the same time, the effective ATMP-HE programs are an economic benefit to society as a whole, since any improvement in the quality of life for patients with disabilities lessens their burden on their families and society. The decision to prevent patients from spending their own money on these treatments has limited their autonomy to pay for a health service which is not paid for by public healthcare programs. This decision may be in legal conflict with provisions that protect individual rights. It could be argued that the existing provisions of the Doctor and Dentist Profession Act, which require the Bioethics Committees to only approve therapies that are likely to be beneficial, should prevent abuse if implemented correctly. In the meantime, the need to reorganize ATMP-HE programs in Poland around third party payers has limited patient access, because some treatments have been suspended temporarily. For example, Poland had the only ATMP-HE program that provided MSC infusions to children with autism, and this program is currently not recruiting.
The motivation of the original EU Regulation 1394/2007/EC was to provide expanded access to experimental therapies for patients with unmet needs. This can be illustrated with two diagnoses that carry a high cost of disability and which have been treated in Poland with ATMP-HE that employ MSC. One example is the adult orthopedic condition knee osteoarthritis, which has a prevalence of 3.6% among the 448 million people in the EU, or 16 million patients (53, 54). Another example is the pediatric neurologic condition autism, which has a prevalence of 1.4% among the 80 million children under age 18 in the EU, or 1.12 million patients (55, 56). Merely for these two conditions, large numbers of patients across Europe might be eligible for expanded access to MSC therapies via ATMP-HE. These ATMP could be manufactured in a network of regional centers of excellence, as some have proposed (12, 57). Thus, for these diagnoses alone the number of patients with unmet needs vastly exceeds the number of enrollments available in clinical trials or the number of openings that have been available in ATMP-HE programs. Nonetheless, the European Federation of Pharmaceutical Industries and Associations (EFPIA), along with other organizations that represent pharmaceutical companies, has issued a joint position paper calling for modification of EU regulations on ATMP-HE (58). Modifications that improve the quality of care are welcome, but the list of proposed revisions must be considered carefully to avoid limiting patient access unnecessarily. For example, if there is a strict prohibition that no patient may obtain ATMP-HE when a similar clinical trial exists, regardless of the enrollment size of the trial, then many patients will be cut off from legal access to MSC treatment. It remains to be seen if the stakeholders in ATMP-HE, both within Poland and in other EU countries, can find a middle ground between protecting patients from exploitation versus allowing patients with incurable conditions and unmet needs to have access to experimental therapies.
5 Conclusions
To date there is no full harmonization of ATMP-HE regulations among EU countries, beyond the overall guidelines provided in the original EU regulation that created ATMP-HE (2–15). We have demonstrated that the Polish implementation of the EU directive is within the mainstream of practices among EU countries regarding manufacturing of products and management of ATMP-HE programs. In addition, between the years 2021 and 2023 Poland has implemented very strong policies for patient protection. The regulations that govern the conduct of therapeutic experiments now require that ATMP-HE participants must have civil liability insurance, and prohibit patients or their representatives from paying to participate in ATMP-HE. It is remarkable that while the public in Poland has among the lowest EU levels of government spending on healthcare, they have among the highest EU levels of public awareness of ATMP and desire to access ATMP.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Author contributions
JP: Conceptualization, Data curation, Formal analysis, Funding acquisition, Writing – original draft. FV: Conceptualization, Data curation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
JP is an independent legal advisor to companies that manufacture ATMP products for use in Poland.
The remaining author declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. EMA. About Us. Available online at: https://www.ema.europa.eu/en/about-us/who-we-are (Accessed Dec. 31, 2023).
2. European Parliament and the Council of the European Union. Regulation (EC) No 1394/2007/EC of the European Parliament and of the Council of 13 November 2007 on advanced therapy medicinal products and amending Directive 2001/83/EC and Regulation (EC) No 726/2004 (OJ L No. 324; “Regulation 1394/2007”). Available online at: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex:32007R1394 (Accessed Dec. 31, 2023).
3. Cuende N, Ciccocioppo R, Forte M, Galipeau J, Ikonomou L, Levine BL, et al. Patient access to and ethical considerations of the application of the European Union hospital exemption rule for advanced therapy medicinal products. Cytotherapy. (2022) 24:686–90. doi: 10.1016/j.jcyt.2022.03.007
4. Juan M, Delgado J, Calvo G, Trias E, Urbano-Ispizua A. Is hospital exemption an alternative or a bridge to european medicines agency for developing academic chimeric antigen receptor T-cell in europe? Our Exp ARI-0001. Hum Gene Ther. (2021) 32:1004–7. doi: 10.1089/hum.2021.168
5. Trias E, Juan M, Urbano-Ispizua A, Calvo G. The hospital exemption pathway for the approval of advanced therapy medicinal products: an underused opportunity? The case of the CAR-T ARI-0001. Bone Marrow Transplantation. (2022) 57:156–9. doi: 10.1038/s41409-021-01463-y
6. Schnitger A. The Hospital Exemption, a regulatory option for unauthorised advanced therapy medicinal products. University of Bonn (2014). Available at: https://www.dgra.de/media/pdf/studium/masterthesis/master_schnitger_a.pdf. Master thesis.
7. Coppens DGM, Hoekman J, De Bruin ML, Slaper-Cortenbach ICM, Leufkens HGM, Meij P, et al. Advanced therapy medicinal product manufacturing under the hospital exemption and other exemption pathways in seven European Union countries. Cytotherapy. (2020) 22:592–600. doi: 10.1016/j.jcyt.2020.04.092
8. Coppens DGM, Gardarsdottir H, De Bruin ML, Meij P, Leufkens HGM, Hoekman J. Regulating advanced therapy medicinal products through the Hospital Exemption: an analysis of regulatory approaches in nine EU countries. Regenerative Med. (2020) 15:2015–28. doi: 10.2217/rme-2020-0008
9. Hills A, Awigena-Cook J, Genenz K, Ostertag M, Simon Butler S, Eggimann A-V, et al. An assessment of the hospital exemption landscape across European Member States: regulatory frameworks, use and impact. Cytotherapy. (2020) 22:772–9. doi: 10.1016/j.jcyt.2020.08.011
10. Wang R, Anozie A, Leutloff J, Chin B, Rex M, Kumar A. Hospital exemptions for ATMPs: friend or foe for pharma? Value Health. (2022) 25:S143. doi: 10.1016/j.jval.2021.11.691
11. Zimmermann P, Tano M, Siorat V, Ribault M, Parent de Curzon O, Degrassat-Théas A, et al. The reform of the french compassionate use program: the state and perspective before the change. Value Health. (2022) 25:S143. doi: 10.1016/j.jval.2021.11.690
12. Priesner C, Hildebrandt M. Advanced therapy medicinal products and the changing role of academia. Transfusion Med Hemotherapy. (2022) 49:158–62. doi: 10.1159/000524392
13. Sánchez-Guijo F, Avendaño-Solá C, Badimón L, Bueren JA, Canals JM, Delgadillo J, et al. Role of Hospital Exemption in Europe: position paper from the Spanish Advanced Therapy Network (TERAV). Bone Marrow Transpl. (2023) 58:727–8. doi: 10.1038/s41409-023-01962-0
14. Dulak J, Pecyna M. Unproven cell interventions in Poland and the exploitation of European Union law on advanced therapy medicinal products. Stem Cell Rep. (2023) 18:1–11. doi: 10.1016/j.stemcr.2023.05.017
15. Bicudo E, Brass I. Advanced therapies, hospital exemptions & marketing authorizations: the UK’s emerging regulatory framework for point-of-care manufacture. Cell Gene Ther Insights. (2023) 9:101–20. doi: 10.18609/cgti.2023.015
16. Sleeboom-Faulkner M, Chekar CK, Faulkner A, Heitmeyer C, Marouda M, Rosemann A, et al. Comparing national home-keeping and the regulation of translational stem cell applications: An international perspective. Soc Sci Med. (2016) 153:240–9. doi: 10.1016/j.socscimed.2016.01.047
17. Sleeboom-Faulkner M. Regulatory brokerage: Competitive advantage and regulation in the field of regenerative medicine. Soc Stud Sci. (2019) 49:355–80. doi: 10.1177/0306312719850628
18. Sipp D, Sleeboom-Faulkner M. Downgrading of regulation in regenerative medicine. Science. (2019) 365:644–6. doi: 10.1126/science.aax6184
19. Weiss DJ, Turner L, Levine AD, Ikonomou L. Medical societies, patient education initiatives, public debate and marketing of unproven stem cell interventions. Cytotherapy. (2018) 20:165–8. doi: 10.1016/j.jcyt.2017.10.002
20. Snyder J, Turner L. Selling stem cell ‘treatments’ as research: prospective customer perspectives from crowdfunding campaigns. Regenerative Med. (2018) 13:375–84. doi: 10.2217/rme-2018-0007
21. Ikonomou L, Cuende N, Forte M, Grilley BJ, Levine AD, Munsie M, et al. International Society for Cell & Gene Therapy Position Paper: Key considerations to support evidence-based cell and gene therapies and oppose marketing of unproven products. Cytotherapy. (2023) 25:920–9. doi: 10.1016/j.jcyt.2023.03.002
22. Moll G, Ankrum JA, Kamhieh-Milz J, Bieback K, Ringdén O, Volk HD, et al. Intravascular mesenchymal stromal/stem cell therapy product diversification: time for new clinical guidelines. Trends Mol Med. (2019) 25:149–63. doi: 10.1016/j.molmed.2018.12.006
23. Moll G, Hoogduijn MJ, Ankrum JA. Editorial: safety, efficacy and mechanisms of action of mesenchymal stem cell therapies. Front Immunol. (2020) 11:243. doi: 10.3389/fimmu.2020.00243
24. Moll G, Ankrum JA, Olson SD, Nolta JA. Improved MSC minimal criteria to maximize patient safety: A call to embrace tissue factor and hemocompatibility assessment of MSC products. Stem Cells Trans Med. (2022) 11:2–13. doi: 10.1093/stcltm/szab005
25. Dziennik Urzędowy Unii Europejskiej. ROZPORZĄDZENIE (WE) NR 1394/2007 PARLAMENTU EUROPEJSKIEGO I RADY z dnia 13 listopada 2007 r. w sprawie produktów leczniczych terapii zaawansowanej i zmieniające dyrektywę 2001/83/WE oraz rozporządzenie (WE) nr 726/2004 (English: European Parliament Regulation 1394/2007/EC). Available online at: https://eur-lex.europa.eu/legal-content/PL/TXT/PDF/?uri=CELEX:32007R1394&from=IT (Accessed Dec. 31, 2023).
26. Dziennik Ustaw Rzeczypospolitej Polskiej Nr. 45 poz. 271. Prawo farmaceutyczne (English: Journal of Laws of the Republic of Poland No. 45, item 271. Pharmaceutical Law (2008). Available online at: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=wdu20080450271 (Accessed Dec. 31, 2023).
27. Dziennik Ustaw Rzeczypospolitej Polskiej 2018 poz. 1375. Ustawa z dnia 7 czerwca 2018 r. o zmianie ustawy - Prawo farmaceutyczne oraz niektórych innych ustaw. (English: Journal of Laws of the Republic of Poland 2018 item 1375. Act of June 7, 2018 amending the Pharmaceutical Law Act and certain other acts.) (2018). Available online at: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20180001375 (Accessed Dec. 31, 2023).
28. Dziennik Ustaw Rzeczypospolitej Polskiej 2011 Nr. 112 poz. 654. Ustawa z dnia 15 kwietnia 2011 r. o działalności leczniczej. (English: Journal of Laws of the Republic of Poland 2011 No. 112 item 654. Act of April 15, 2011 on medical activities.) (2011). Available online at: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=wdu20111120654 (Accessed Dec. 31, 2023).
29. Dziennik Ustaw Rzeczypospolitej Polskiej Nr. 28 poz. 152. Ustawa z dnia 5 grudnia 1996 r. o zawodach lekarza i lekarza dentysty (English: Journal of Laws of the Republic of Poland No. 28, item 152. Act of 5 December 1996 on the Professions of Doctor and Dentist (1996). Available online at: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU19970280152/U/D19970152 (Accessed Dec. 31, 2023).
30. Dziennik Ustaw Rzeczypospolitej Polskiej 2020 poz. 1291. Ustawa z dnia 16 lipca 2020 r. o zmianie ustawy o zawodach lekarza i lekarza dentysty oraz niektórych innych ustaw (English: Journal of Laws of the Republic of Poland 2020 item 1291. Act of July 16, 2020 amending the Act on the professions of doctor and dentist and certain other acts) (2020). Available online at: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20200001291 (Accessed Dec. 31, 2023).
31. Dziennik Ustaw Rzeczypospolitej Polskiej 2019 poz. 313. Rozporządzenie Ministra Zdrowia z dnia 5 lutego 2019 r. w sprawie wzoru wniosku o wydanie zgody na wytwarzanie produktu leczniczego terapii zaawansowanej - wyjątku szpitalnego oraz wniosku o zmianę tej zgody. (English: Journal of Laws of the Republic of Poland 2019 item 313. Regulation of the Minister of Health of February 5, 2019 on the template of the application for consent to the production of an advanced therapy medicinal product - hospital exception and the application for changing this consent) (2019). Available online at: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20190000313 (Accessed Dec. 31, 2023).
32. Dziennik Ustaw Rzeczypospolitej Polskiej 2015 poz. 793. Obwieszczenie Marszałka Sejmu Rzeczypospolitej Polskiej z dnia 15 maja 2015 r. w sprawie ogłoszenia jednolitego tekstu ustawy o pobieraniu, przechowywaniu i przeszczepianiu komórek, tkanek i narządów. (English: Journal of Laws of the Republic of Poland 2015 item 793. Announcement of the Marshal of the Parliament of the Republic of Poland of May 15, 2015 on the publication of the uniform text of the Act on the collection, storage and transplantation of cells, tissues and organs.) (2015). Available online at: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20150000793 (Accessed Dec. 31, 2023).
33. European Commission. The Rules Governing Medicinal Products in the European Union Volume 4. Good Manufacturing Practice. Good Manufacturing Practice for Advanced Therapy Medicinal Products. Guidelines of 2017-11-22 Effective 2018-05-22. Available online at: https://health.ec.europa.eu/system/files/2017-11/2017_11_22_guidelines_gmp_for_atmps_0.pdf (Accessed Dec. 31, 2023).
34. Główny Inspektorat Farmaceutyczny. Informacja dot. nadzoru GIF w zakresie wytwarzania produktów leczniczych terapii zaawansowanej – wyjątków szpitalnych. (English: Chief Pharmaceutical Inspectorate. Information regarding GIF supervision in the production of advanced therapy medicinal products - hospital exceptions.) (2020). Available online at: https://www.gov.pl/web/gif/informacja-dotyczaca-nadzoru-gif-w-zakresie-wytwarzania-produktow-leczniczych-terapii-zaawansowanej–wyjatkow-szpitalnych (Accessed Dec. 31, 2023).
35. Bosek L, Gałązka M. Szczególne świadczenia zdrowotne. System Prawa Medycznego. Tom 2 (English: Health services regarding blood and its components. In: Bosek L, Wnukiewicz-Kozłowska A, editors. Medical law system. Special health services, vol. 2 . C.H.Beck Publishing House, Munich, Germany (2018). p. 62–6.
36. Czyżewska K. Eksperyment medyczny w przepisach prawa. (English: Medical experiment in legal regulations.) Health Manager News (2023). Available online at: https://www.termedia.pl/mz/Eksperyment-medyczny-w-przepisach-prawa,50882.html (Accessed Dec. 31, 2023).
37. Serwach M. Nowe zasady przeprowadzania eksperymentów medycznych na ludziach. (English: New rules for conducting medical experiments on humans.) Medycyna Praktyczna (2021). Available online at: https://www.mp.pl/etyka/medycyna_eksperymentalna/276264,nowe-zasady-przeprowadzania-eksperymentow-medycznych-na-ludziach (Accessed Dec. 31, 2023).
38. D UCHWAŁA NADZWYCZAJNEGO II KRAJOWEGO ZJAZDU LEKARZY z dnia 14 grudnia 1991 r. w sprawie Kodeksu Etyki Lekarskiej (English: RESOLUTION OF THE EXTRAORDINARY SECOND NATIONAL CONVENTION OF DOCTORS regarding the Code of Medical Ethics) (1991). Warsaw, Poland: Wolters Kluwer. Available online at: https://sip.lex.pl/akty-prawne/akty-korporacyjne/kodeks-etyki-lekarskiej-286454095 (Accessed Dec. 31, 2023).
39. Boruczkowski D, Zdolińska-Malinowska I. Wharton’s Jelly mesenchymal stem cell administration improves quality of life and self-sufficiency in children with cerebral palsy: results from a retrospective study. Stem Cells Int. (2019) 2019:7402151. doi: 10.1155/2019/7402151
40. Boruczkowski D, Zdolińska-Malinowska I. A retrospective analysis of safety and efficacy of wharton’s jelly stem cell administration in children with spina bifida. Stem Cell Rev Rep. (2019) 15:717–29. doi: 10.1007/s12015-019-09902-6
41. Barczewska M, Maksymowicz S, Zdolińska-Malinowska I, Siwek T, Grudniak M. Umbilical cord mesenchymal stem cells in amyotrophic lateral sclerosis: an original study. Stem Cell Rev Rep. (2020) 16:922–32. doi: 10.1007/s12015-020-10016-7
42. Dziennik Ustaw Rzeczypospolitej Polskiej. USTAWA z dnia 9 marca 2023 r. o badaniach klinicznych produktów leczniczych stosowanych u ludzi. (English: Journal of Laws of the Republic of Poland. Act of 9 March 2023 regarding clinical studies of medicinal products for human use.) (2023). Available online at: https://orka.sejm.gov.pl/proc9.nsf/ustawy/2843_u.htm (Accessed Dec. 31, 2023).
43. Bundesministerium der Justiz. Arzneimittelgesetz: AMG (English: Federal Ministry of Justice. Medicinal Products Act: AMG). Available online at: https://www.gesetze-im-internet.de/englisch_amg/ (Accessed Dec. 31, 2023).
44. Paul-Ehrlich-Institut (PEI) Authorisation of ATMP. (2019). Available online at: https://www.pei.de/EN/regulation/approvals/authorisation-atmp/authorisation-atmp-node.html (Accessed Dec. 31, 2023).
45. UK Medicines and Healthcare products Regulatory Agency (MHRA). Guidance. Advanced therapy medicinal products: regulation and licensing (2015). Available online at: https://www.gov.uk/guidance/advanced-therapy-medicinal-products-regulation-and-licensing (Accessed Dec. 31, 2023).
46. UK Medicines and Healthcare products Regulatory Agency (MHRA).GUIDANCE ON THE UK’S ARRANGEMENTS UNDER THE HOSPITAL EXEMPTION SCHEME (2015). Available online at: https://assets.publishing.service.gov.uk/media/5a7dcbbde5274a5eaea66623/Guidance_on_the_UK_s_arrangements_under_the_hospital_exemption_scheme.pdf (Accessed Dec. 31, 2023).
47. United Kingdom Medicines and Healthcare products Regulatory Agency (MHRA). Guidance on “non-routine”. Available online at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/397739/Non-routine_guidance_on_ATMPs.pdf (Accessed Dec. 31, 2023).
48. Black A.United Kingdom Specialist Pharmacy Service (2020). Out of Specification Advanced Therapy Medicinal Products - Guidance for Healthcare Organisations. Available online at: https://www.sps.nhs.uk/wp-content/uploads/2020/02/Out-of-Specification-Advanced-Therapy-Medicinal-Products-V1.2-March-2020.pdf (Accessed Dec. 31, 2023).
49. Goldsobel G, von Herrath C, Schlickeiser S, Nicola Brindle N, Stähler F, Reinke P, et al. RESTORE survey on the public perception of advanced therapies and ATMPs in europe—Why the european union should invest more! Front Med. (2021) 8:739987. doi: 10.3389/fmed.2021.739987
50. Abou-El-Enein M, Elsanhoury A, Reinke P. Overcoming challenges facing advanced therapies in the EU market. Cell Stem Cell. (2016) 19:293–7. doi: 10.1016/j.stem.2016.08.012
51. Eder C, Wild C. Technology forecast: advanced therapies in late clinical research, EMA approval or clinical application via hospital exemption. J Market Access Health Policy. (2019) 7:1600939. doi: 10.1080/20016689.2019.1600939
52. Famicord. List of life saving transplantations. Available online at: https://famicord.eu/about-us/list-of-life-saving-transplantations (Accessed Dec. 31, 2023).
53. European Union.Facts and figures on life in the European Union. Available online at: https://european-union.europa.eu/principles-countries-history/key-facts-and-figures/life-eu_en (Accessed Dec. 31, 2023).
54. Spitaels D, Mamouris P, Vaes B, Smeets M, Luyten F, Hermens R, et al. Epidemiology of knee osteoarthritis in general practice: a registry-based study. BMJ. (2020) 10:e031734. doi: 10.1136/bmjopen-2019-031734
55. UNICEF. How many children are there in the European Union (EU)? Available online at: https://data.unicef.org/how-many/how-many-children-under-18-are-there-in-the-eu/ (Accessed Dec. 31, 2023).
56. Sacco R, Camilleri H, Eberhardt J, Umla-Runge K, Newbury-Birch D. The Prevalence of Autism Spectrum Disorder in Europe. In: Carotenuto M, editor. Autism Spectrum Disorders - Recent Advances and New Perspectives. IntechOpen, London, UK (2022). doi: 10.5772/intechopen.108123
57. Delgadillo J, Kerkelä E, Waters A, Akker E, Lechanteur C, Baudoux E, et al. A management model in blood, tissue and cell establishments to ensure rapid and sustainable patient access to advanced therapy medicinal products in Europe. Cytotherapy. (2023) 25:1259–64. doi: 10.1016/j.jcyt.2023.08.001
58. European Federation of Pharmaceutical Industries and Associations (EFPIA). Reform of the EU General Pharmaceutical Legislation Joint Position Paper on the Hospital Exemption Scheme for ATMPs. Available online at: https://www.efpia.eu/media/1wwnhpem/arm-efpia-europabio-eucope-isct-joint-paper-on-hospital-exemption-scheme-july-2023.pdf (Accessed 2024-04-12).
Keywords: advanced therapy medicinal products (ATMPs), cell and gene therapy (CGT), hospital exemptions (HE), mesenchymal stromal cells (MSC), regulatory affairs, national licensing provisions, risk -benefit, unproven cell and gene interventions
Citation: Pachocki J and Verter F (2024) Polish regulatory system regarding ATMP hospital exemptions. Front. Immunol. 15:1379134. doi: 10.3389/fimmu.2024.1379134
Received: 30 January 2024; Accepted: 16 April 2024;
Published: 13 May 2024.
Edited by:
Guido Moll, Charité University Medicine Berlin, GermanyReviewed by:
Martin Hildebrandt, Technical University of Munich, GermanyDavid García-Bernal, University of Murcia, Spain
Copyright © 2024 Pachocki and Verter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jan Pachocki, amFucGFjaG9ja2lAZ21haWwuY29t; Frances Verter, ZnZlcnRlckBoaXMuY29t
†These authors have contributed equally to this work and share first authorship
‡ORCID: Frances Verter, orcid.org/0000-0001-5345-4514
 Jan Pachocki
Jan Pachocki Frances Verter
Frances Verter